i
COMPARATIVE STUDY OF Ischial containment socket AND
Quadrilateral socket for functional Ability
IN PERSONS WITH UNILATERAL TRANSFEMORAL AMPUTATION
Dissertation submitted to the Tamil Nadu Dr. MGR Medical University,
Chennai, in partial fulfillment of requirements for the MD Branch XIX
ii
D E C L A R A T I O N
I hereby declare that “Comparative study of Ischial containment socket
and Quadrilateral socket for functional ability in persons with unilateral
transfemoral amputation” is my bona fide work in partial fulfillment of the
requirement of the Tamil Nadu Dr. MGR Medical University, Chennai, for
the MD Branch XIX (Physical Medicine and Rehabilitation) examination in
April 2016.
Dr. Nitha. J
Candidate Number 201329052
Department of Physical Medicine and Rehabilitation
Christian Medical College
iii
C E R T I F I C A T E
This is to certify that “Comparative study of Ischial containment socket
and Quadrilateral socket for functional ability in persons with unilateral
transfemoral amputation” is the bona fide work of Dr. Nitha. J, Candidate
Number 201329052 in partial fulfillment of the requirement of the Tamil
Nadu Dr. MGR Medical University, Chennai, for the MD Branch XIX
(Physical Medicine and Rehabilitation) examination in April 2016, done
under my supervision and guidance.
Dr. Henry Prakash
Professor
Department of Physical Medicine and Rehabilitation
Christian Medical College
iv
C E R T I F I C A T E
This is to certify that “Comparative study of Ischial containment socket
and Quadrilateral socket for functional ability in persons with unilateral
transfemoral amputation” is the bona fide work of Dr. Nitha.J, Candidate
Number 201329052, in partial fulfillment of the requirement of the Tamil
Nadu Dr. MGR Medical University, Chennai, for the MD Branch XIX
(Physical Medicine and Rehabilitation) examination in April 2016, done
under my supervision and guidance.
Dr. George Tharion
Professor and Head of the Department
Department of Physical Medicine and Rehabilitation
Christian Medical College
v
C E R T I F I C A T E
This is to certify that “Comparative study of Ischial containment socket
and Quadrilateral socket for functional ability in persons with unilateral
transfemoral amputation” is the bona fide work of Dr. Nitha.J, Candidate
Number 201329052, in partial fulfillment of the requirement of The Tamil
Nadu Dr. MGR Medical University, Chennai, for the MD Branch XIX
(Physical Medicine and Rehabilitation) examination in April 2016, done
under my supervision and guidance.
Dr. Alfred Job Daniel
Principal
Christian Medical College
vi
ACKNOWLEDGEMENT
Even though my name appears primarily on the covers of this thesis, a great many
people have contributed to its production. I owe my humble gratitude to all these
people who have made this thesis possible and made this work a cherishable
experience.
I would like to express my deep gratitude to my guide Dr. Henry Prakash whose
advice and guidance have enabled me to successfully complete the study. I am also
thankful to him for reading my reports, helping me understand and enrich my ideas.
I would like to thank Dr. George Tharion, Professor and Head of the Department of
PMR for his support and encouragement for this study. His insightful comments and
constructive criticisms were deeply thought provoking.
I wish to thank various people without whom this study would not have been possible
– All who have been involved with the study from the department of Prosthetics and
Orthotics, for their valuable suggestions, time and efforts. Particularly, I would like
to acknowledge Mr. Vinoth Jacob, from P&O for his unstinted support and
cooperation. Special thanks to Mr. Mansur Ali and Mr. Dinesh from P&O for their
support in the completion of the thesis. The doctors in charge of the Amputee Clinic
who helped me enroll my patients, my teachers and friends in the department who
vii
A special thanks to Mrs. Joyce the neutral assessor and gait analyst, who have helped
me with the data acquisition.
I would like to express my great appreciation to the patients who took part in the
study without whom none of this would have been possible.
Most importantly, none of this would have been possible without the love and
patience of my family. I am deeply thankful to my 2 year old son Aadith, who
without any complaints for the limited time I spent with him, has loved me and made
my life meaningful. Special thanks to my loving husband and my ever caring parents,
who have stood by me always.
ix
x
CONTENTS
ORGINALITY REPORT PDF……….ix
CONTENTS ... x
LIST OF FIGURES ... xv
LIST OF TABLES ... xvii
LIST OF EQUATIONS ... xviii
ABSTRACT ... xx
1 INTRODUCTION ... 1
2 AIMS & OBJECTIVES ... 3
2.1 AIM ... 3
2.2 OBJECTIVE ... 3
3 REVIEW OF LITERATURE ... 3
3.1 AMPUTATION ... 3
3.1.1 STATISTICS ... 4
3.1.2 ETIOLOGY OF AMPUTATION ... 4
3.2 REHABILITATION OF PERSONS WITH TRANSFEMORAL AMPUTATION ... 5
3.2.1 PRE-OPERATIVE PERIOD ... 6
3.2.2 TRANSFEMORAL AMPUTATION ... 6
xi
3.2.4 PRE-PROSTHETIC TRAINING ... 8
3.3 PROSTHESIS ... 9
3.3.1 HISTORY ... 9
3.3.2 BIOMECHANICAL PRINCIPLES OF TRANSFEMORAL PROSTHESIS ... 10
3.4 COMPONENTS OF TRANSFEMORAL PROSTHESIS ... 17
3.5 SUSPENSION SYSTEMS ... 18
3.6 SOCKET ... 19
3.7 QUADRILATERAL SOCKET ... 20
3.8 ISCHIAL CONTAINMENT SOCKET ... 21
3.8.1 EVOLUTION ... 21
3.8.2 DIMENSIONS ... 27
3.8.3 NSNA (NORMAL SHAPE-NORMAL ALIGNMENT TECHNIQUE)... 31
3.8.4 CAT-CAM(CONTOURED ADDUCTED TROCHANTERIC-CONTROLLED ALIGNMENT METHOD) ... 31
3.8.5 NARROW M-L (NARROW MEDIO-LATERAL SOCKET) ... 32
3.8.6 SCAT-CAM (SKELETAL CONTOURED ADDUCTED TROCHANTERIC CONTROLLED ALIGNMENT METHOD) ... 32
3.9 OTHER SOCKET DESIGNS FOR TRANSFEMORAL PROSTHESIS ... 32
3.9.1 FLEXIBLE SOCKETS ... 33
3.9.2 MARLO ANATOMICAL SOCKET ... 34
xii
3.10 KNEE JOINTS ... 36
3.11 FOOT-ANKLE ASSEMBLIES ... 39
3.12 FABRICATION AND ALIGNMENT OF TRANSFEMORAL PROSTHESIS ... 41
3.13 PROSTHETIC TRAINING ... 45
3.14 NORMAL GAIT ... 45
3.14.1 GAIT ANALYSIS ... 46
3.15 TRANSFEMORAL PROSTHETIC GAIT ... 47
3.16 ENERGY EFFICIENCY ... 50
3.17 JUSTIFICATION OF THE STUDY ... 51
4 METHODOLOGY ... 53
4.1 STUDY DESIGN ... 53
4.2 INTERVENTION ... 53
4.3 SETTINGS AND LOCATION ... 55
4.4 ETHICS COMMITTEE APPROVAL ... 56
4.5 PARTICIPANTS ... 56
4.6 INCLUSION CRITERIA ... 57
4.7 EXCLUSION CRITERIA ... 57
4.8 SAMPLE SIZE ... 57
4.9 OUTCOME MEASURES ... 58
4.9.1 PRIMARY OUTCOME MEASURES ... 58
xiii
4.9.1.2 TIMED UP AND GO TEST (TUG)... 59
4.9.1.3 SOCKET COMFORT SCORE (SCS) ... 60
4.9.1.4 SOCKET PREFERENCE ... 61
4.9.2 SECONDARY OUTCOME MEASURES ... 61
4.9.2.1 PHYSIOLOGICAL COST INDEX (PCI) ... 61
4.9.2.2 GAIT ANALYSIS ... 62
4.10 STATISTICAL ANALYSIS ... 64
4.11 FLOW DIAGRAM ... 65
5 RESULTS ... 66
5.1 DEMOGRAPHIC DATA ... 66
5.1.1 AMBULATION STATUS ... 67
5.1.2 AGE ... 67
5.1.3 SIDE OF AMPUTATION ... 67
5.1.4 ETIOLOGY ... 68
5.1.5 GENDER ... 68
5.1.6 BODY MASS INDEX... 68
5.1.7 DURATION OF PROSTHETIC USE ... 69
5.1.8 RESIDUAL LIMB LENGTH INDEX ... 69
5.2 PRIMARY OUTCOME MEASURE ... 70
5.2.1 6 MINUTE WALK TEST ... 70
xiv
5.2.3 SOCKET COMFORT SCORE ... 75
5.2.4 SOCKET PREFERENCE ... 77
5.3 SECONDARY OUTCOME MEASURES ... 78
5.3.1 ENERGY EFFICIENCY ... 78
5.3.2 GAIT VELOCITY ... 79
5.3.3 GAIT CADENCE ... 82
5.3.4 STRIDE LENGTH ... 83
5.3.5 SINGLE LIMB SUPPORT ... 85
5.3.6 STANCE SWING RATIO ... 86
6 DISCUSSION... 87
7 CONCLUSION ... 94
8 LIMITATIONS... 95
9 SCOPE OF FUTURE RESEARCH ... 96
10 BIBLIOGRAPHY ... 97
xv
LIST OF FIGURES
Figure 3-1 - FORCE VECTORS ACTING ON SINGLE LIMB SUPPORT ... 11
Figure 3-2 – PELVIS ACTING AS LEVER ... 12
Figure 3-3 - ALIGNMENT STABILITY ... 15
Figure 3-4 HIP ABDUCTOR INSUFFICIENCY ... 22
Figure 3-5 QUADRILATERAL SOCKET ... 22
Figure 3-6 LATERAL TRUNK LEAN ... 23
Figure 3-7 PROTO ISCHIAL CONTAINMENT SOCKET ALIGNMENT ... 25
Figure 3-8 ISCHIAL CONTAINMENT SOCKET ... 26
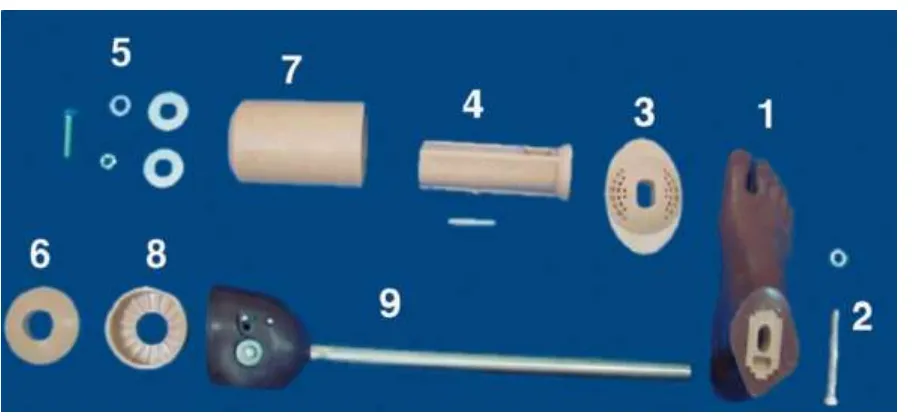
Figure 3-9 – COMPONENTS IN TRANSFEMORAL KIT OF ICRC ... 41
Figure 4-1 ISCHIAL CONTAINMENT FABRICATION PROCEDURE ... 55
Figure 4-2 – TIMED UP & GO TEST ... 60
Figure 4-3- GAIT ANALYSIS... 63
Figure 5-1 ETIOLOGY OF AMPUTATION ... 68
Figure 5-2-6MWT TEST IN QUADRILATERAL & ISCHIAL CONTAINMENT SOCKET ... 71
Figure 5-3 – RELATION OF 6MWT VS AGE ... 71
Figure 5-4- 6MWT VS ETIOLOGY ... 72
Figure 5-5- 6MWT VS DURATION OF PROSTETIC USE ... 72
Figure 5-6- TUG TEST IN QUADRILATERAL & ISCHIAL CONTAINMENT SOCKET ... 74
Figure 5-7- TUG VS ETIOLOGY ... 74
Figure 5-8- TUG VS AGE ... 75
Figure 5-9- TUG VS DURATION OF PROSTHETIC USE ... 75
Figure 5-10- SCS IN QUADRILATERAL & ISCHIAL CONTAINMENT SOCKET ... 77
Figure 5-11 – SOCKET PREFERENCE IN TRANSFEMORAL AMPUTEE PERSONS ... 77
xvi
Figure 5-13- GAIT VELOCITY IN QUADRILATERAL & ISCHIAL CONTAINMENT SOCKET ... 81
Figure 5-14 – GAIT VELOCITY VS ETIOLOGY ... 81
Figure 5-15- GAIT VELOCITY VS AGE ... 81
Figure 5-16- GAIT CADENCE IN QUADRILATERAL & ISCHIAL CONTAINMENT SOCKET ... 83
Figure 5-17 – STRIDE LENGTH IN QUADRILATERAL & ISCHIAL CONTAINMENT SOCKET ... 83
Figure 5-18 – STRIDE LENGTH VS AGE ... 84
xvii
LIST OF TABLES
Table 3-1PHASES OF AMPUTEE REHABILITATION ... 5
Table 3-2 COMPARISON OF QUAD & IC SOCKET ... 30
Table 5-1 DEMOGRAPHIC DATA OF PATIENTS... 66
Table 5-2 AGE DISTRUBUTION OF PATIENTS ... 67
Table 5-3 DURATION OF PROSTHETIC USE ... 69
Table 5-4 CORRELATION OF THE 6 MINUTE WALK TEST WITH AGE, ETIOLOGY AND DURATION OF PROSTHETIC USE IN QUAD AND IC GROUPS ... 70
Table 5-5 CORRELATION OF THE TIMED UP AND GO TEST WITH AGE, ETIOLOGY AND DURATION OF PROSTHETIC USE IN QUAD AND IC GROUPS ... 73
Table 5-6 CORRELATION OF THE SOCKET COMFORT SCORE WITH AGE, ETIOLOGY AND DURATION OF PROSTHETIC USE ... 76
Table 5-7 CORRELATION OF THE PHYSIOLOGICAL COST INDEX WITH AGE, ETIOLOGY AND DURATION OF PROSTHETIC USE ... 79
Table 5-8 CORRELATION OF THE GAIT VELOCITY WITH AGE, ETIOLOGY AND DURATION OF PROSTHETIC USE ... 80
Table 5-9 CORRELATION OF THE GAIT CADENCE WITH AGE, ETIOLOGY AND DURATION OF PROSTHETIC USE IN THE QUAD AND IC GROUPS. ... 82
Table 5-10 CORRELATION OF THE STRIDE LENGTH WITH AGE, ETIOLOGY AND DURATION OF PROSTHETIC USE IN THE QUAD AND IC GROUPS ... 84
Table 5-11 SINGLE LIMB SUPPORT OF AMPUTATED AND NORMAL SIDE LIMBS WITH QUAD AND IC SOCKET ... 85
xviii
LIST OF EQUATIONS
xix
TITLE OF THE STUDY
Comparative study of ischial containment socket and
quadrilateral socket for functional ability in persons with
unilateral transfemoral amputation
PLACE OF STUDY
Dept. of Physical Medicine and Rehabilitation
xx
ABSTRACT
TITLE
Comparative study of ischial containment socket and quadrilateral socket for
functional ability in persons with unilateral transfemoral amputation
.
OBJECTIVE
To compare ischial containment socket with quadrilateral socket in transfemoral
amputee persons in terms of functional ability and socket preference.
METHODOLOGY
This is an interventional study where transfemoral amputee persons ambulant with
prosthetic limb fitted with quadrilateral socket were enrolled after informed consent.
First assessment was done with the quadrilateral socket during the initial visit. Then
they were provided with ischial containment socket. The knee component, pylon and
the foot piece were retained without alteration. Each patient was given two weeks’
time to acclimatize to the new socket. At the end of two weeks all the assessments
were repeated with the ischial containment socket.
OUTCOME MEASURES
Functional ability was measured with the 6-minute walk test (6MWT) and Timed Up
xxi
final socket preference. The secondary outcome measures were energy efficiency
with Physiological Cost Index and gait parameters. The outcome measures were
statistically analyzed with the paired T test.
RESULTS
The ischial containment socket (IC) was preferred by 87 % of patients who were
already community ambulant with quadrilateral socket (QUAD). The socket comfort
score significantly improved with the ischial containment socket. The ischial
containment socket is superior to quadrilateral socket in terms of comfort. The
comfortable walking speed of transfemoral amputee persons improved with the
ischial containment socket. The gait velocity and stride length showed statistically
significant improvement with ischial containment socket. The 6MWT, TUG and PCI
showed better results with ischial containment socket even though the improvement
was not statistically significant. Observable variations in gait deviations were not
seen with the socket change.
CONCLUSION
The ischial containment socket is an evolutionary transfemoral socket design, which
provides better comfort for transfemoral amputee persons. The ischial containment
socket might potentially improve walking ability and endurance in unilateral
1
1
INTRODUCTION
Amputation is a lifesaving as well as a life changing event. Once the decision for
elective amputation is made, the primary focus should be preparing the individual
physically and mentally for the surgical procedure. Such amputations should be
followed by a goal oriented extensive rehabilitation phase. Functional rehabilitation
of amputee person’s, especially ones with higher levels of amputation like
transfemoral levels is a challenge. To restore all the functional activities at their near
normal physiological level should be the ultimate goal.
The residual limb is fitted with prosthesis. The expected role of prosthesis is
substituting the functions of normal limb, which is independent ambulation in lower
limb amputee persons. The prosthesis should provide comfort as well as cosmesis.
Prosthetic rehabilitation should make the person capable of leading a normal and
successful life as far as possible.
Understanding of the complex biomechanics of human locomotion as well as
developments in material science has contributed in the advancement in field of
prosthetic design and fabrication. The prosthetic technology has evolved from the
plug fit wooden sockets to osseo-integrated prosthesis, microprocessor knee and
2
A socket is a part of the prosthesis which attaches to the residual limb. For
transfemoral residual limb a few socket designs have been developed over the last
few decades. The Quadrilateral socket has been the socket design of choice for
transfemoral prosthesis from its inception in 1950’s till last two decades. The Ischial
containment socket emerged in 1980’s with sound biomechanical concepts while
addressing the short comings of quadrilateral socket. Even though the biomechanical
principles of the ischial containment socket is better; the quadrilateral socket
continued to be the preference in most of the nations.(1) The skill needed to fabricate
an ischial containment socket is more than the conventional quadrilateral socket.
This study aims at comparing the ischial containment socket with quadrilateral socket
in terms of functional abilities and socket preference. Does the theoretical advantage
of ischial containment socket, correlate with the functional outcome of transfemoral
amputee persons?
In this study transfemoral amputee persons who have been ambulant with
quadrilateral socket were recruited and were given prosthesis, where the quadrilateral
socket was replaced with an ischial containment socket. Outcome measures were
assessed with quadrilateral as well as ischial containment socket, followed by
statistical analysis. The outcome measures used in this study were 6 minute walk test,
timed up and go test, socket comfort score, socket preference, gait parameters and
physiological cost index. At the end of the study patients were given an option to
3
2
AIMS & OBJECTIVES
2.1
AIM
To evaluate the theoretical advantage of ischial containment socket over quadrilateral
socket in rehabilitation of transfemoral amputee persons.
2.2
OBJECTIVE
To compare ischial containment socket with quadrilateral socket in transfemoral
amputee persons in terms of functional ability and socket preference.
3
REVIEW OF LITERATURE
3.1
AMPUTATION
Amputation is the removal of a limb or a part of the limb by trauma, medical illness,
or surgery. History of amputation dates back to Hippocrates era. Then the surgical
principle was lost in Dark Ages and reintroduced in 1529 by Ambroise Pare, when he
first used ligatures to control bleeding. The introduction of tourniquet by Morel and
antiseptic technique by Lord Lister contributed in the further development of
amputation techniques. The discovery of chloroform as an anesthetic agent made the
surgery more reasonable. The surgical technique of amputation advanced rapidly
4
3.1.1
STATISTICS
Global burden of disease refers disability as “loss of health where health is
conceptualized in terms of functioning capacity in a set of health domains such as
mobility, cognition, hearing and vision”.(3) According to WHO statistics the global
disability prevalence is 15 % that is about one in seven of world population is
disabled.(4) As per the Census of India 2011, 2.1 percent of Indian population is
estimated to have disability.(5) Even though amputation being a major contributor to
disability, its exact burden on disability or its global incidence is unknown. The
available data shows considerable variations among countries and within countries.
3.1.2
ETIOLOGY OF AMPUTATION
Globally the main three causes for amputation are trauma, diseases and congenital
malformation. Trauma is the major cause of amputation globally.(6) Diabetes
contributes 30-90 percent of lower extremity amputations.(7) In India the major
cause for amputation is trauma.(8,9) The next important cause is diseases. Chronic
diabetes and peripheral vascular disease is the most common non traumatic cause for
lower limb amputations.(10) The study conducted by Pooja et.al from Kolkata
observed that 70 percent of amputation was due to trauma and 27 percent due to
vascular disease. Traumatic amputations are more with young and active individuals,
with male predominance.(8) Lower limb amputations constitute about 95% of all
major amputations. The most common level of amputation is transtibial level.
5
3.2
REHABILITATION OF PERSONS WITH TRANSFEMORAL
AMPUTATION
Rehabilitation of an amputee person includes a multidisciplinary approach, involving
surgeon, physiatrist, psychologist, physiotherapist, occupational therapist and
prosthetic technicians. Adequate rehabilitation should aim at restoring the acceptable
functional capacities allowing individuals to achieve their goals, allow participation
in society and to improve quality of life with or without prosthesis.(11) The
rehabilitation process should start when the decision for amputation is made,
covering pre and post-surgical period. The patient should be informed about the
anticipated functional outcomes according to the level of amputation and medical
[image:26.612.68.548.421.697.2]conditions.(12)The phases of amputee rehabilitation are as follows(6,13,14)
TABLE 3-1PHASES OF AMPUTEE REHABILITATION
PHASES GOALS
1. Preoperative Preparing psychologically and physically for amputation,
determining the level of amputation, discussing the expected
functional outcomes, alleviating anxiety and stress,
sensitizing about phantom pain and phantom sensation.
2.Amputation
surgery
Myoplasty techniques for better femur adduction, Nerve
handling, Rigid dressing application
3. Acute
post-surgical
Optimization of analgesics. Emotional support, mobilization
6
4.Preprosthetic Residual limb shaping, restoring sense of control, improving
muscle power and maintaining full range of motion
5.Prosthetic
Fabrication
Consensus on prosthetic prescription, prosthetic measurement
and fabrication
6.Prosthetic
Training
Functional use of prosthesis
7. Community
integration
Resuming social roles, developing healthy coping strategies,
recreational activities
8.Vocational
Rehabilitation
Job modifications and training
9.Follow up Lifelong medical, functional and prosthetic assessment and
emotional support
3.2.1
PRE-OPERATIVE PERIOD
The functional rehabilitation in the preoperative period includes maintaining ROM,
stretching out the contracted muscles, conditioning the normal side, increasing the
endurance, practicing the single limb gait. This preoperative initiation of
rehabilitation can reduce the time spent in postoperative rehabilitation.(12)
3.2.2
TRANSFEMORAL AMPUTATION
Trans femoral amputations forms about 30% of total major amputations.(6) Trans
femoral amputations can be classified as supracondylar, long, medium and short
7
Gottschalk modification - Gottschalk found that the prosthetic shape or alignment is
not sufficient to keep hip in adduction. Hence he modified the transfemoral
amputation surgical principle by preserving the adductor magnus if possible and
attaching it to distal end of femur with drill holes, while femur is maintained in
adduction.(16) Even though the biomechanical principle was good, it didn’t evolve as
a standard surgical practice.
3.2.3
ACUTE POST SURGICAL MANAGEMENT
In the acute post-surgical period pain management and wound care is most important.
The residual limb can be fitted with immediate post-operative prosthesis or
prefabricated prosthesis.
IMMEDIATE POST OPERATIVE PROSTHESIS (IPOP) – It is applied in the
operation room itself. It consists of a rigid dressing made of POP or fiberglass, a
connector, pylon and a foot piece. Early ambulation in the second or third
post-operative day is the most important advantage of this technique. The other
advantages are reduction of edema, protection from trauma, lower rate of
complications, early definitive prosthesis fitting and shorter rehabilitation time. IPOP
is an emotional enhancer since the presence of prosthetic limb aids with better body
image. The disadvantages are mechanical stress, tissue necrosis and wound
dehiscence along with reduced access to wound inspection. To apply an IPOP skilled
8 PREFABRICATED POSTOPERATIVE PROSTHETIC SYSTEMS (PFPS)
Prefabricated prosthesis are designed for early gait re-education following surgery.
They provide a psychological boost and decrease the time interval for definitive
prosthesis. They are similar to IPOP methods but use pneumatic technology for
socket holding. The residual limb with soft dressing will be lined by air cell, or air
bags which can be inflated and serves as the socket residual limb interface. This can
be inflated up to 20-40 mm of Hg, thus providing excellent external compression.
The advantages are early weight bearing, easy removal and replacement for wound
inspection. It reduces the limb swelling by pneumatic compression. The
disadvantages are expensive, bulky along with difficult donning and doffing.(18–20)
3.2.4
PRE-PROSTHETIC TRAINING
The goal of early post-operative period is functional rehabilitation.
PHYSICAL TRAINING
-
Individualized exercise schedule should be instructed toimprove or maintain the range of motion of all the limbs, to improve the strength of
the limbs and to improve endurance for daily activities.(6)
TRANSFERS AND MOBILITY- In the early phase amputee persons are taught bed mobility, transfers, and mobilization to a chair or wheelchair. Subsequently gait
training is initiated inside the parallel bar and progressed to elbow crutches. The
pre-prosthetic training provides the patient a safe return home with the temporary
9
The residual limb will continue to shrink and hence definitive prosthesis fitting will
require 6- 8 months post amputation.(12)
3.3
PROSTHESIS
Prosthesis is a device which substitutes for a missing body part.
3.3.1
HISTORY
Humans for centuries have discovered ingenious ways to replace the lost body part.
The history of prosthesis dates back to Greek and Roman times, with little
advancement in the Dark Ages. In the year 2000, researchers in Cairo, Egypt,
unearthed the oldest documented prosthesis – 3000 year old toe made of wood and
leather. In 1500’s German’s made prosthetic limbs utilizing iron, springs and leather.
French surgeon Ambrose Paré invented transfemoral prosthesis with peg leg and foot
piece, adjustable harness, knee lock control and other engineering features that are
used in today's devices. Lorrain, a French locksmith used leather, paper and glue in
place of heavy iron in making prosthesis, which later became a major contribution in
prosthetic technology. In 1863, Dubois Parmlee invented an advanced prosthesis with
a suction socket, polycentric knee and multi-articulated foot. Following the U.S Civil
War and World War 2 the number of amputations increased astronomically. This
eventually led to the formation of the American Orthotic & Prosthetic Association
(AOPA) for better prosthetic design and technology.(21) Prosthetic devices which
10
with new technologies and advancement of prosthetic design. In the last century new
sophisticated prosthesis were developed, with microprocessors and computerized
technologies. The socket fitting also got revolutionized with the introduction of
osseo-integrated prosthesis. (2,21)
3.3.2
BIOMECHANICAL PRINCIPLES OF TRANSFEMORAL PROSTHESIS
The requirements for a good transfemoral prosthesis is basically three in number—
comfort, function, and appearance. The user of the prostheses will not be able to wear
it unless it is comfortable. It should enable the wearer to perform functions with ease.
In addition to the above the prosthesis should be cosmetically acceptable and natural
to the wearer as well. The prosthesis should provide adequate support and a naturally
appearing gait. Hence to ensure that all the 3 functionalities are suitably met, the
correct bio mechanical principles are to be used.
MEDIO-LATERAL STABILITY
Two specific deviations of gait observed in transfemoral amputee persons were.
a) Exaggerated lateral movement of the torso from side to side.
b) Increased step width.
Hence achieving a narrow based gait and adequate medio-lateral stability is crucial
for a transfemoral prosthesis.(22) A normal person walks with a step width
measuring about 2-4 inches whereas in the case of an amputee person’s step width is
11
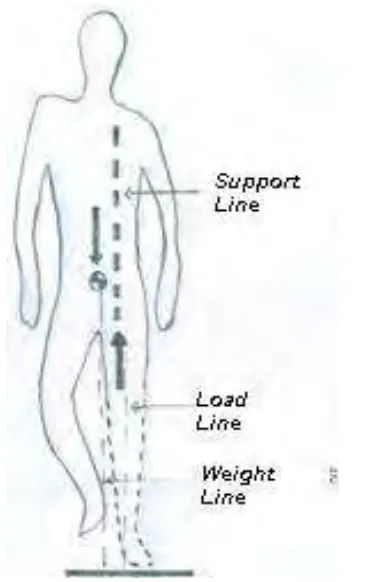
FIGURE 3-1 - FORCE VECTORS ACTING ON SINGLE LIMB SUPPORT
DEFINITIONS (22, 23)
The center of gravity of the body can be defined as a point within the body at which the effect of all body weight can be assumed to be concentrated. As per the
laws of physics the body weight must be assumed as acting vertically down from this
center of gravity. “The weight line of the body is a line through the center of gravity along which the body weight can be assumed to
act vertically downward at all times.” The total force exerted on the sole of the foot is known as
the floor reaction force which is the load which the leg transmits upwards. The load line can be defined as the line along which the force
between the foot and the floor acts. The support line is defined as a vertical or plumb line, passing through the support point, along
which the effective supporting force between the
socket rim and the residual limb can be assumed
to act.(Figure 3.1)
ROLE OF HIP ABDUCTORS
During midstance the pelvis drops 5 degree in the unsupported side. Further pelvic
drop is prevented by the eccentric contraction of hip abductors. In normal persons
12
FIGURE 3-2 – PELVIS ACTING AS LEVER
controlling the pelvic drop. In case of the transfemoral amputee persons, the residual
femur during weight bearing shift’s laterally since the femur floats in soft tissue mass
without any bony attachment distally.(24) There occurs increase in pressure in the
perineal area due to drop of pelvis towards the normal side, which is uncomfortable,
hence the amputee persons compensates by leaning over the prosthesis which results
in amputee persons’ list or walking with wide base. The gluteus medius has to be
maintained in functional position for providing comfortable and normal gait for the
amputee persons.(25)
THE PELVIC LEVER
As illustrated by the Figure 3.2, while the amputee
person is bearing weight on the prosthesis during
stance phase, the pelvis acts as a lever. The body
weight is supported by the pelvic lever by
balancing action of the hip abductors, using the
ischium as fulcrum. The body weight is balanced
by the tension in the hip abductors whereas the
lever action of the pelvis prevents the dropping of
the pelvis towards the unsupported side.(23)
However this is possible only if the residual limb
13 DISTRIBUTION OF LATERAL PRESSURE
Distribution of counter pressure uniformly over the lateral side of the socket ensures
stabilisation of the residual limb. If the length of the residual limb is average, then
stabilisation can be achieved by fitting the residual limb over the entire lateral wall.
However if the hip abductors are used for pelvic stabilisation with residual limb not
properly supported against lateral wall, then end of residual limb may get subjected
to intense compressive forces causing pain.
The lateral stabilisation of the pelvis by the hip abductors is influenced by
predominately two factors (22)
a) Lever arm between the abductor and support point – The tension in
abductors has greater advantage when the lever arm is at the lengthiest. If the
ischial seat and gluteal musculature support the body weight substantially then
amputee persons is at ease to balance the body weight.
b) Degree of residual limb adduction in socket - Efficiency of muscles is at
the peak when they are at normal rest length. If the movement of femur is
anticipated and pelvic femoral angle maintained, then the hip abductors are
most efficient.
KNEE CONTROL
Knee stability refers to maintain the knee in extension during the stance phase. Knee
instability happens when the prosthetic knee buckles under load. Excessive knee
stability will lead to difficult swing phase initiation and increased energy
14
control. Depending on the age and residual limb condition of amputee persons, a
fine balance needs to be maintained between the degree of involuntary and voluntary
control.
Involuntary Control
If the weight line is anterior to the knee axis, the weight bearing tends to extend the
knee and locks it against the extension stop. Prosthesis can be said to be in a state of
high alignment stability when the socket is placed well forward on knee block or
aligned in hyper extension and knee joint posterior to angle.(22) This is
predominantly required for eliminating the fear of falling. However the limitation is
that the prosthesis being hard, flexibility is limited and normal gait gets
compromised.
Voluntary Control
In order to enable amputee persons to have near normal gait, the use of involuntary
control has to be minimised and voluntary control by residual limb action needs to
be emphasised. The key to voluntary control is effective utilisation of the hip
extensor musculature. For voluntary control, the hip extensors – gluteus maximus
and hamstrings should be able to exert enough force to maintain the knee in
extension. However voluntary control is exercised such that the residual limb should
15
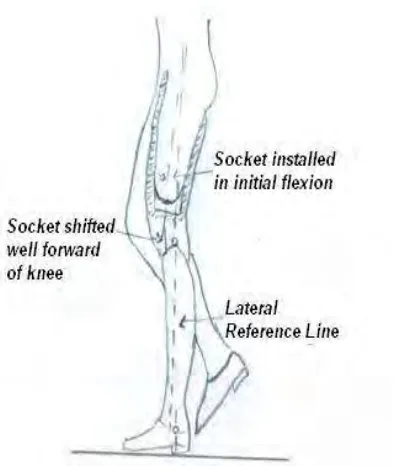
FIGURE 3-3 - ALIGNMENT STABILITY
INITIAL FLEXION
The hip extensors should be at an optimum resting length for exerting extension force
in the knee. For this the glutei has to be kept stretched. The socket is aligned in initial
flexion to increase the resting length.(Figure 3.3) Hence the amputee persons will
have greater knee stability during walking, as the length of the hip extensors is
increased by hip flexion. This enables the residual limb to exert sufficient force
without any conscious effort by the amputee persons, to keep the knee back against
the extension stop.(24) The transfemoral amputee persons walk with increased pelvic
lordosis if the hip extensors are weak, this can be decreased by keeping the socket in
initial flexion.(22,26) The hamstring muscles in the case of amputee persons with a
well-developed musculature tend to force the ischium off the ischial seat. This causes
tremendous pressure on the muscles and
the anterior brim of the socket. This is
reduced to a great extent by the initial
flexion, by allowing the body weight to be
borne by the hamstring musculature. The
flexibility of the prosthetic knee is
enhanced to a great extent by positioning
the socket anterior to the knee axis as this
allows easy transmission of weight from
the prosthesis to normal leg.
16 FOOT POSITION
The feet of the amputee persons should be in medial position alignment to ensure
that weight is borne primarily by the ischial seat and the torso list is minimal.
Normally the center line of feet will be aligned below the ischium for an amputee
person. However this may not apply always, as it is dependent on the ability of
amputee persons to use hip abduction. If an amputee person has a very short
residual limb, then excessive dependence on the abductors may result in pain and
will force him to lean over the prosthesis and walk with wider base. (23)
DYNAMIC ALIGNMENT
The forces acting on the prosthesis in the case of an amputee person varies with the
different phases of gait. The dynamic forces will greatly influence the behaviour of
the prosthesis during the swing phase as well as stance to swing and swing to stance
phase. The pre requisite towards achieving a smooth swing phase is good transition
from the stance to swing phase.(27) When the alignment stability of the prosthesis
is high the initiation of the swing phase will be delayed and the energy required is
high. Swing phase vaulting happens when the prosthesis is too long. The lateral
knee movement along with medial foot movement of the prosthesis caused by poor
dynamic alignment is known as the whip of the prosthesis.(26)
17 ROTATION OF KNEE AXIS
Extensive studies on human locomotion have indicated that during motion, when
the knee is brought forward by hip flexion the femur rotates by 40 on an average.
This medial rotation of the femur will result in lateral displacement of the feet. In
order to overcome this medial rotation of the femur on hip flexion, the knee axis is
also rotated laterally.(22)
ANKLE – FOOT - DYNAMICS
The most unstable phase of an amputee persons’ gait is ‘heel strike’. When the heel
of an amputee person contacts the ground, knee flexor moment is produced causing
the knee to buckle. In normal gait the controlled plantar flexion will stabilize the
knee. In transfemoral prosthesis the stiffness of plantar flexion is the most
significant factor affecting the knee stability. If the ankle is too stiff then, the feet is
not allowed to rotate forward to a flat stable position. This will cause the knee to
buckle on the transfer of weight to prosthesis. On the other hand if the plantar
flexion stiffness is not sufficient then the feet will have a tendency to slap at the
heel contact. Hence the key is to have a proper balance for each amputee
person.(26)
3.4
COMPONENTS OF TRANSFEMORAL PROSTHESIS
Transfemoral prosthesis is constituted by suspension systems, socket, knee joint,
18
3.5
SUSPENSION SYSTEMS
A prosthesis can be suspended using many methods like belts, liners, suction and
vacuum suspension.
Belt Suspension - Three different types of belt suspensions are used for a transfemoral prosthesis i.e. total elastic suspension belt, silesian belt and pelvic band
with hip joint.(12)
Elastomeric Liner Suspension - Liner suspension can be used either with pins / lanyards. The liner suspension with either pin / lanyard type has advantages like
increased shear control, cushioning, and greater suspension and comfort.(28)
However these liners require frequent replacement, add bulk and pose hygiene
challenges.
Suction Suspension– In this mode of suspension, air is only allowed to exit & not enter by placing a single side valve near the distal region. On placing the limb in the
socket, the sock is pulled out thereby sliding the limb in the socket. This can be
achieved by use of special nylon socks, elastic bandage or wet fit method. While the
suction suspension is the most secure of all suspensions, it has certain disadvantages
like it is difficult to don.(29) Moreover any weight gain may result in adductor roll,
19 Vacuum Suspension system - Vacuum systems are new and advanced version of the suspension systems which use an active mechanism to expel air from inner socket.
These systems require both gel liner and sealing sleeve and the air is removed and
vacuum achieved through a mechanical / electric pump. This provides for better
suspension, maintains the limb volume and increased tissue oxygenation in the
residual limb.(30) However the disadvantage of the system is that the vacuum seal is
lost if a hole is formed on the sleeve. Moreover the cost as well as the weight of the
device is increased on account of this.
3.6
SOCKET
Introduction
Socket is the human prosthesis interface. Earlier design of the transfemoral socket
was wooden socket with a conical interior shape – plug fit. The weight of the
amputee person was transferred through the thigh muscles. The quadrilateral socket
design which provided ischial-gluteal weight bearing was introduced in 1950s. In
1980s a second generation of transfemoral sockets – the ischial containment socket
emerged due to the work of Long, Mayfield and Sabolich. The socket evolution
continued and newer socket design like Marlo Anatomical System developed. By the
end of 19th century direct bony anchoring of the prosthesis – Osseo-integrated
20
3.7
QUADRILATERAL SOCKET
“The quadrilateral socket is truly more than a cross sectional shape at the ischial level, is a three dimensional receptacle for the residual limb with contour at every level which are justifiable on a sound biomechanical basis” -RADCLIFFE
Quadrilateral (QUAD) socket was introduced in 1950, by University of California at
Berkeley. It has been the standard socket design for transfemoral prosthesis for about
four decades. Quadrilateral socket has four distinct walls, hence the name. The
medio-lateral diameter is increased and the antero-posterior diameter is shortened. It
has posterior shelf on which ischium rests. The primary weight-bearing surface is the
ischial tuberosity and the gluteal muscles. Hence it’s an ischial gluteal weight bearing
prosthesis in which 83 % of the weight is borne by ischium and gluteal
musculatures.(23,33)
The lateral wall is higher than the posterior wall. The lateral wall primarily stabilizes
the femoral shaft and encloses the gluteus maximus, vastus lateralis and tensor fascia
lata. The lateral wall is kept in adduction and this stretches the hip abductors. The
medial wall is perpendicular to provide counter pressure. It stabilizes the residual limb by compressing the abductor muscles against the lateral wall. The posterior
wall contains hamstring medially. The hip is kept in flexion by anterior slant of about
7 -10 degrees. This will stretch the gluteus and hamstrings for maximum power
generation. The anterior wall is higher than the posterior wall. It stabilizes the
21 and it presses against the Scarpa’s triangle.(22,23,33) Distally the socket provides the total contact. Quadrilateral socket provides good stability in the sagittal
plane.(34) The medio-lateral and rotational stability is minimal. The quadrilateral
socket has a better fit with firm, long residual limbs with good adductor
musculature.(24)
3.8
ISCHIAL CONTAINMENT SOCKET
3.8.1
EVOLUTION
The Quadrilateral socket was the socket design of choice till 1980’s.(25) Ivan Long
and Mayfield investigated the performance of the quadrilateral socket in regard to
coronal-plane residual limb-socket biomechanics. They radiologically evaluated 100
transfemoral amputee persons standing erect in quadrilateral socket and found that
majority of them; the femur in residual limb was in abduction. There were gait
deviations like lateral bending of trunk and wide based gait.(35,36)
THE PROBLEM
Considering pelvis as a lever, the ischium as the fulcrum, the hip abductor tension
should be able to balance the weight of the body, preventing the pelvic drop during
stance phase of prosthetic limb. For the maximum physiological efficiency of the
abductors, the normal rest length should be maintained. (Figure 3.4) If not it will lead
to abductor insufficiency. (22) In quadrilateral socket when gluteus medius contracts,
22
FIGURE 3-4 HIP ABDUCTOR INSUFFICIENCY
maintain femur in adduction. The abduction of femur is mainly due to the wider
medio-lateral dimension of quadrilateral
socket. The abduction of the femur causes
more pressure on the distal aspect of the
residual limb.(Figure 3.5) When the
prosthetic side is bearing weight the residual
limb exerts force on the lateral wall which
shifts laterally since the ischium cannot check this displacement. When gluteus
contracts and abducts the femur the pelvis shift medially which makes the lateral
shift worse and cause high shearing force in the soft tissue around the ischial seat and
medial brim.(37) The lateral wall of the socket
is away from the lateral surface of thigh
except in the distal part. This lateral shift of
the socket results in a gap in the proximal
socket – limb interface. The lateral shift of the
socket resulted in compressive forces in the
medial proximal tissues of the limb. This
creates a shearing force in the soft tissue structures between medial brim and medial
structures of pelvis. Thus the quadrilateral socket exerts high pressures in proximal
medial and posterior brim.(37) This in turn results in pain and discomfort in the
[image:43.612.325.510.379.548.2]23
trunk leaning gait.(Figure 3.6)(39) The biomechanical disadvantage of the
quadrilateral socket is more pronounced with shorter residual limb.
Goals of new socket technology were
1. The hip abductor to be maintained in its normal length.
2. The femur to be maintained in physiological position of
adduction.
3. The pressure in the distal lateral aspect of the residual
limb to be distributed for a painless and comfortable gait.
4. The lateral shift of the socket to be controlled
5. Pain and discomfort in the perineal area to be alleviated
6. The gait deviations to be minimized
7. The energy efficiency of the gait to be improved
EMERGENCE OF ISCHIAL CONTAINMENT SOCKET
Initially the alignment modification was tried. The newer alignment techniques were
focused on maintaining the femur in adduction. The head of the femur was aligned to
the center of the medio-lateral dimension of the socket. Ivan Long proposed Long’s
Line-”a straight line from the head of the femur (located approximately at the center
of a narrow socket), through the distal femur, and down to the center of the heel”.
[image:44.612.397.510.186.473.2]24
alignment. The ischial seat, knee joint and foot should be perpendicular to the Long’s
line. The knee joint was placed laterally in order to avoid the knocking of knees.
Alignment modifications were followed by socket design alterations. To maintain hip
adduction the lateral wall was contoured with sloping medially from sub trochanteric
region to distal end of the socket. To achieve this alignment the medio-lateral
dimension was reduced. This lead to the emergence of the narrow medio-lateral
socket concept. The newer socket alignment method came to be known as Proto
ischial containment limb (Figure 3.7).(40) Femoral alignment, balance and gait
improved with new alignment method.(35,38,40)
Even though the alignment modifications were made, during weight bearing the
ischial tuberosity migrated medially. This resulted in the lateral gap in the proximal
brim of the socket along with medial wall digging inside and lateral leaning of pylon.
Hence amputee persons had pain and discomfort in the perineal area.(39) To maintain
the hip in adduction and for better comfort in the perineal region alignment
modification alone was not sufficient. Hence alterations in socket design were tried.
This lead to the emergence of the ischial containment socket with newer socket
design and alignment technology. It is an evolutionary design rather than a
revolutionary design.(23, 24) The ischial containment socket refers to postero-medial
extension of the proximal brim of the socket, so that the weight is borne against the
25
FIGURE 3-7 PROTO ISCHIAL CONTAINMENT SOCKET ALIGNMENT
Original Source – King. C, 2009 (40)
The postero-medial brim is oblique and sloping and the ischium is contained in it and
hence the name. Along with this there is contouring beneath the ischial tuberosity
resulting in the same amount of ischial weight bearing as quadrilateral socket.(39)
Radcliffe named this newer socket design as Ischial Ramal containment.(24) The
26
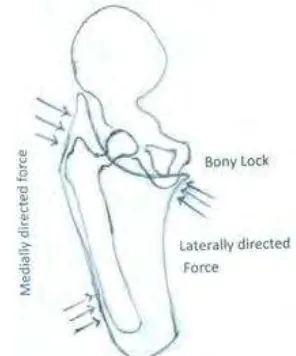
The femur is kept in adduction in the ischial containment socket by two methods.
1. The ischial tuberosity and ramus is held inside the socket. That will bear the forces
which are directed laterally. The lateral surface of the socket proximal to the
trochanter is snugly fit into the soft tissue. The ischium and ramus is held in position
by the medially directed forces borne by the proximal femur in the trochanteric and
sub-trochanteric region. The medially directed forces in the mid and distal femur help
in maintaining proper adduction angle. The ischial containment is like a locking
system in which ischium sits inside the socket and the opposing force is given from
the lateral aspect pushing the femur into adduction. The three point pressure system(
Figure 3.8) - laterally directed forces in the ischial tuberosity, the medially directed
forces in the supra-trochanteric region and the medially directed forces in the lateral
aspect of femur along with the bony lock maintains femur in adduction. The
increased adduction angle in ischial containment socket results in considerable
weight bearing by the femur. (24, 39)
2. The narrow medio-lateral dimension will lock
the femur, maintain the hip in adduction. Since the
medio-lateral dimension is narrow the weight is
borne directly by the skeletal structures, reducing
the motion lost through soft tissue interface. A
wide medio-lateral dimension cannot provide this
[image:47.612.357.505.485.663.2]locking phenomenon since the femur can fall away
27
from the supporting surfaces. The antero-posterior dimension is widened to
compensate the narrow medio-lateral. Increasing the antero-posterior diameter allows
flexors and extensors which form the major muscle bulk around the hip to function
naturally.(23,39)
The rotational stability of the quadrilateral socket depends mostly on muscle
channels. In ischial containment socket the containment of the ischium and narrow
diameter between the greater trochanter and medial ischial surface provides sufficient
rotational stability.(24) Ischial containment is contoured throughout for total contact
socket. Since more area of the residual limb is contained inside and due to the
contour, it provides greater distribution of weight bearing and stabilization forces.
(34) The weight bearing in ischial containment socket is by ischial tuberosity, gluteal
musculature, femur and hydrostatic compression.(23)
The ischial containment is the socket design of choice for short, fleshy and unstable
residual limb. For functionally active amputee persons and high activity sports ischial
containment is the preferred socket design. For elderly debilitated patients walking
with walking aids quadrilateral socket will be sufficient.(24)
3.8.2
DIMENSIONS
MEDIAL-LATERAL DIMENSION
The ischium sits inside the postero-medial socket wall. To prevent the ischial ramus
28
side. This is achieved by reduction in the medio-lateral dimension of subtrochanteric
region. The proximal region is wide enough to accommodate the ischial ramus as
well as greater trochanter. Hence the medio-lateral dimension of ischial containment
at the ischial level is similar to quadrilateral socket. The decrease in the medio-lateral
dimension is mainly 4 cm distal to ischial tuberosity in the subtrochanteric
region.(23). The lateral wall is well above the greater trochanter for medio –lateral
stability. The lateral wall is slanted medially for better adduction.
ANTERIOR-POSTERIOR DIMENSION
The medio-lateral dimension is narrow, in order to accommodate the residual limb
volume the antero-posterior dimension is greater compared to quadrilateral socket.
The major muscle bulk acting in the hip joint is in the sagittal plane. Hence wider
antero-posterior dimension allows the flexors and extensors to function more
effectively (36, 37). Wider the antero-posterior dimension lesser will be the pressure
on Scarpa’s triangle.(39)
MEDIALBRIM
The postero-medial socket wall provides lateral pressure to the ischium in order to
prevent it from slipping medially. Hence the medial wall has to be loaded, while
providing pressure relief for the less pressure tolerant areas like adductor tendon and
pubic ramus. The medial brim extends posterior to enclose ischial ramus and dips
29
ischium from posterior to anterior direction, hence in the transverse plane it looks
internally rotated.(23)
ANTERIOR BRIM
The anterior trim line of ischial containment and quadrilateral socket is similar, up to
or just proximal to the inguinal crease. While sitting the socket should clear the
superior iliac spine. (23)
LATERAL BRIM
The lateral wall is extended proximally snugly fitting to provide counter pressure for
the ischium in the sloping medial wall. The contouring helps to distribute the
pressure over the entire area. In transverse plane posterior to greater trochanter, there
is extreme obliquity compared to quadrilateral socket. This is termed as wallet
hollow. The postero-lateral brim compresses gluteal muscles and helps in gluteal
weight bearing. Lateral brim locks around the greater trochanter & provides rotatory
stability.(23)
POSTERIOR BRIM
The posterior trim line of the ischial containment socket is 4 cm proximal to the
ischial tuberosity, higher than the quadrilateral socket in order to contain the
30
TABLE 3-2 COMPARISON OF QUAD & IC SOCKET
QUAD IC
Ischial containment Ischium is outside the socket resting in the ischial seat
Ischium is contained inside the socket in the postero-medial wall Weight bearing Ischial – Gluteal weight
bearing
Ischial tuberosity, ramus, femur and
hydrostatic compression Medio – lateral stability No bony lock, less
medio-lateral stability
Hip maintained in adduction with bony lock and contoured lateral wall, greater medio-lateral stability Rotational control Lesser rotational control
since ischium slips from the posterior shelf
Increased rotational control due to skeletal lock inside the socket Socket Shape Wider medio-lateral,
narrow antero-posterior
Narrow ML, Wider antero-posterior,
subtrochanteric concave shaped
Alignment Medial wall in line of progression
31
The ischial containment sockets were known in different names. The prosthetic
technique of University of California was named as CAT-CAM. The socket design
followed in Northwestern University was NSNA (Normal Shape-Normal Alignment
technique). In New York University it was known as Narrow Medio-lateral.(25)
3.8.3
NSNA (NORMAL SHAPE-NORMAL ALIGNMENT TECHNIQUE)
Long found that when foot is lined under femur head rather than ischium, the
amputee persons walk with a near normal narrow base. He proposed Long’s Line and
the alignment in NSNA is mainly based on it.
3.8.4
CAT-CAM (CONTOURED ADDUCTED
TROCHANTERIC-CONTROLLED ALIGNMENT METHOD)
The Contoured Adducted Trochanteric-Controlled Alignment Method is an ischial
containment socket developed by Sabolich. This design keeps the femur in adducted
position by undercutting of the trochanter. The ischium sits in special fossa in the
posterior wall, with a three dimensional support in the socket, thus forming a bony
lock.(24)
The prosthetic foot is lateral to the plumb line from the ischial tuberosity. In
variation to NSNA the foot is not always under the distal femur or center of hip joint.
In the geriatric population CAT – CAM offers superior comfort due to less pressure
in the Scarpa’s region.(39) The CAT-CAM socket offers more comfort due to
32
3.8.5
NARROW M-L (NARROW MEDIO-LATERAL SOCKET)
Narrow Medio-Lateral socket is a type of ischial containment socket. Here the
casting techniques are slightly different. The centralization of femur is achieved by
applying laterally directed forces in the medial distal end of residual limb, while
maintaining femur in adduction with a medially directed force applied on the middle
of the femur shaft. This will provide a distraction force displacing the soft tissue
mass in the distal aspect of residual limb, resulting in centralization of femur and
better contour of the end region of the residual limb.(25)
3.8.6
SCAT-CAM (SKELETAL CONTOURED ADDUCTED TROCHANTERIC
CONTROLLED ALIGNMENT METHOD)
Skeletal Contoured Adducted Trochanteric-Controlled Alignment Method is a
modified form of CAT–CAM in which skeletal anatomy is considered more. The
femur is kept in adducted position with Oklahoma fossa and compartment. The
medial brim line is advanced proximally to contain the maximum of the ischium and
the ramus.(39)
3.9
OTHER SOCKET DESIGNS FOR TRANSFEMORAL
PROSTHESIS
The prosthetics and orthotics is a developing field of science. The newer sockets are
being developed with advanced technology to meet the variety of needs of the
33
3.9.1
FLEXIBLE SOCKETS
"To label a socket as flexible I would say that you should be able to deform it by your hands, and the material should not be elastic enough to stretch under the loads it will be subjected to." - KRISTINSSON
The flexible socket design concept is introduced by Ossur Kristinsson. The design
was popularly known as Scandinavian Flexible socket or ISNY (Icelandic Swedish
New York) socket. The socket is formed by a flexible thermoplastic which is
supported by a rigid frame. The flexible socket materials are made of laminating
resins like polyurethane, polyester, acrylic, silicone, lynadure, surlyn along with
nylon stockinet with fiberglass stockinet in between. The rigid frame or socket
retainer should be of enough strength to support the residual limb and to resist
deforming forces. The socket retainer is mainly made of carbon fiber. The
suspension system for flexible sockets is mainly vacuum suspension. If needed other
suspension methods can be incorporated.(41–43) The advantages of flexible socket
design is maximal comfort, better proprioception and ability to accommodate minor
34
3.9.2
MARLO ANATOMICAL SOCKET
Marlo Ortiz Vasquez a Mexican prosthetist developed the Marlo Anatomical Socket
(MAS). Marlo Anatomical socket is an ischial ramal containment socket. It deviates
from ischial containment socket by lowering the posterior and anterior timelines. The
ischial ramus is contained inside the socket which provides the skeletal stability. The
medial and anterior portion of ischial tuberosity and ramus is captured inside the
socket with less of posterior aspect of ischial tuberosity. The posterior trim lines are
lowered so that the gluteus maximus is not included in the socket. The anterior trim
lines are also correspondingly lowered. The lateral trim line above the trochanter is
snugly fit and is lower compared to ischial containment socket. MAS is a total
contact socket and the vertical forces are mainly borne by the ischial ramus along
with quasi hydrostatic suspension. Its mainly designed like a flexible socket with
socket retainer made of carbon. The advantages are better cosmesis, easy donning
and doffing, improved proprioception along with more natural sensation of sitting
since there is no socket material beneath the gluteus maximus.(44) The amputee
persons gait is better with MAS socket due to superior containment of bony structure,
and improved range of motion of the hip.(45) The femur is kept in adduction and the
pelvis stability is improved with MAS socket. In comparison to the ischial
35
3.9.3
OSSEOINTEGRATION
The osseointegration is a newer and alternative method of attaching prosthesis to
human body. The concept of osseointegration dates back to 1960s when it was found
that titanium is bone friendly. Further research by Swedish Professor Branemark lead
to the use of osseointegrated implants in the dental surgery. The concept was
expanded in 1990s and the transfemoral amputee persons were fitted with
osseointegrated system. In this the prosthesis is directly anchored to the bone. This
requires two stage surgical procedures. In the first stage implant which is a threaded
titanium material is inserted into the marrow cavity of residual femur. This is known
as fixture. This fixture will get integrated to the bone with time. The second surgery
is conducted after six months. The abutment which is a titanium extension is inserted
into the fixture and secured with abutment screw. The abutment penetrates the skin
and protrudes out. The rest of the prosthetic components can be directly fixed to the
abutment in the following phase of comprehensive rehabilitation. This leads to a
gradual and progressive weight bearing of the prosthesis. The entire rehabilitation
will take 6 months for proper weight bearing and gait training. So from amputation to
independent walking with the osseointegrated prosthesis will require a minimum of
one year. The osseointegrated prosthesis the hip range of motion is not restricted
unlike the other sockets.(45) The cumulative survival rate, prosthetic use and
mobility is better with osseointegrated prosthesis.(47) Two years follow up of
transfemoral amputee persons with osseointegrated prosthesis showed better quality
36
energy consumption with osseointegrated and conventional transemoral prosthesis.
They found that amputee persons with osseointegrated prosthesis walk with higher
speed and lesser energy expenditure.(49)
The advantages of the osseointegrated prosthesis are. 1. Since there is no socket, the
discomfort, skin irritation, sweating, concentrated pressure and pain occurring in the
human- socket interface can be avoided. 2. The prosthesis can be easily detached
from the abutment. Hence donning and doffing is easy. 3. The suspension is good,
since it is directly anchored to the bone. 4. The hip movements are not restricted
since there is no socket wrapped around the residual limb. 5. The more natural
perception of the prosthetic limb, which is known as osseoperception.(50)
The disadvantages are 1. Need for extensive rehabilitation and longtime interval
between amputation and prosthetic walking. 2. Risk of implant related complications
like infection, implant loosening and failure. 3. Risk of fractures. 4. Permanent
abutment can lead to poor cosmesis. 5. High impact activities like running and
jumping are restricted. 6. Regular skin care for the abutment area is required.
3.10
KNEE JOINTS
Prosthetic knee joint is a complex structure which forms the integral part of the
transfemoral prosthesis. The prosthetic knee can be endoskeltal or exoskeltal. The
knee joint provides adequate support during the stance phase, preventing the failing
37 SINGLE-AXIS KNEE JOINT(12) - This is the basic or simplest knee joint which works
on a simple hinge mechanism. The stance phase stability is dependent on involuntary as
well as voluntary stability. The advantages are being simple, low cost and easy
maintenance. The disadvantage is compromised mechanical stability.
POLYCENTRIC-AXIS KNEE JOINT(26) – In Polycentric knee the instantaneous center
of rotation changes with respect to flexion and extension of thigh and shank component.
The polycentric knee mainly consists of four bar linkage. The advantage is varying
mechanical stability through the entire gait cycle. During flexion of the knee, there is
inherent shortening which aids in better foot clearance. The polycentric knees are
beneficial for amputee persons with weak hip extensors, short residual limbs and knee
disarticulation.
WEIGHT-ACTIVATED STANCE-CONTROL KNEE(26,27) – It consists of a braking
mechanism which prevents knee from buckling. This brake is activated by applying
weight. The weight required to activate this mechanism can be modified according to
each individual.
MANUAL LOCKING KNEE JOINT(12,26) – This has an automatic locking mechanism
which is activated in extension. This can be unlocked manually. This is the most stable
knee during stance phase. The disadvantage is maximal gait deviations and increased
38 FRICTION CONTROL KNEE JOINT(12,27) - A constant mechanical friction is applied
to the knee joint. The friction is adjusted to the normal cadence of the amputee persons.
Alteration in cadence by the amputee persons can result out of phase flexion and
extension of knee joint. The advantages are simple design, dependability and easy to
maintain. The disadvantage is amputee persons have to walk with single cadence.
EXTENSION ASSIST KNEE JOINT(26)– It helps in extending the shank in swing phase
by recoil of a spring mechanism which is being compressed while flexing the knee. It
provides initial stance support since full knee extension is ensured at the end of terminal
swing itself.
PNEUMATIC CONTROL KNEE JOINT (12,26)– Pneumatic knee contains a piston,
which is compressed during the knee flexion. This forces the air in the cylinder to travel
upwards through bottom valve and then back to the central cylinder through another
valve