“A STUDY ON ASSOCIATION BETWEEN SERUM
BILIRUBIN AND SEVERITY OF DIABETIC RETINOPATHY
IN A TERTIARY CARE CENTRE IN TAMILNADU”
Dissertation submitted by
DR.V.RAGHURAM
In partial fulfillment of the requirements for the degree of
MASTER OF SURGERY
IN
OPHTHALMOLOGY
THE TAMILNADU DR.M.G.R.MEDICAL UNIVERSITY
APRIL 2015
DEPARTMENT OF OPHTHALMOLOGY
DECLARATION BY THE CANDIDATE
I hereby declare that this dissertation entitled “A STUDY ON
ASSOCIATION BETWEEN SERUM BILIRUBIN AND SEVERITY OF
DIABETIC RETINOPATHY IN A TERTIARY CARE CENTRE IN
TAMIL NADU” is a bonafide and genuine Research work carried out by
me under the guidance of DR. D. SUNDAR,M.S.,D.O. Professor and Head
of the Department of Ophthalmology, PSG institute of Medical Sciences &
Research. Coimbatore in partial for the award of M.S. Degree in Ophthalmology
to be held in 2015. This dissertation has not been submitted in part of full to any
other University or towards any other degree before this below mentioned date.
CERTIFICATE BY THE GUIDE
This is to certify that the dissertation entitled “A STUDY ON
ASSOCIATION BETWEEN SERUM BILIRUBIN AND SEVERITY OF
DIABETIC RETINOPATHY IN A TERTIARY CARE CENTRE IN
TAMIL NADU” is a bonafide and genuine Research work done by
DR.V.RAGHURAM in partial fulfillment of therequirement forthedegreeof MASTER OF SURGERY IN OPHTHALMOLOGY as per regulations of PSG
INSTITUTE OF MEDICAL SCIENCES AND RESEARCH,
COIMBATORE. I have great pleasure inforwarding this to the University.
Place : Coimbatore DR. D. SUNDAR M.S.,D.O.
Date : Professor and Head,
Department of Ophthalmology
PSG Institute of Medical Sciences
ENDORSEMENT BY THE HEAD
OF THE DEPARTMENT
This is to certify that the dissertation entitled “A STUDY ON
ASSOCIATION BETWEEN SERUM BILIRUBIN AND SEVERITY OF
DIABETIC RETINOPATHY IN A TERTIARY CARE CENTRE IN
TAMIL NADU” is a bonafide and Genuine Research work done by
DR.V.RAGHURAM under the guidance of DR. D. SUNDAR MS,DO
Professor, Department of Ophthalmology, PSG Institute of Medical Sciences &
Research.
ENDORSEMENT BY THE PRINCIPAL
This is to certify that the dissertation entitled “A STUDY ON
ASSOCIATION BETWEEN SERUM BILIRUBIN AND SEVERITY OF
DIABETIC RETINOPATHY IN A TERTIARY CARE CENTRE IN
TAMIL NADU” is a bonafide and genuine research work done by
DR.V.RAGHURAM under the guidance of DR.D.SUNDAR,MS,DO, Professor and Head, Department of Ophthalmology, PSG Institute of Medical Sciences &
Research.
Place : Coimbatore DR S RAMALINGAM
Date : Principal
PSG Institute of Medical Sciences & Research
COPYRIGHT
DECLARATION BY THE CANDIDATE
I hereby declare that PSG Institute of Medical Sciences and Research,
Coimbatore, shall have the rights to preserve, use and disseminate this
dissertation in print or electronic format for academic/research purpose.
Place : Coimbatore Signature of Candidate
ACKNOWLEDGEMENT
I would like to thank the Head of the Department and my guide for this
thesis Dr. D SUNDAR for his valuable guidance and support throughout the
study.
I would like to extend my heartfelt thanks to Dr.JEEVAMALA for his
valuable comments and guidance.
I am greatly endebted to Dr. DIVYA for their immense support and
encouragement while pursuing this study.
I express my gratitude to Dr.JENIT OSBORN Community
Medicine department for his wonderful statistical guidance in the study.
I would like to thank my fellow colleagues for their considerate
cooperation without which I would have stumbled along the way.
I would like to thank my spouse Mrs.HARATHI RAGHURAM and my
parents for their encouragement and motivation which was much required
during the period.
Most of all I would like to thank the patients who cooperated with me
CONTENTS
SL
TITLE PAGE
NO.
1. INTRODUCTION 1
2. AIM 4
3. REVIEW OF LITERATURE 5
4. MATERIALS AND METHODS 80
5. OBSERVATIONS AND RESULTS 83
6. DISCUSSION 96
7. CONCLUSION 105
BIBLIOGRAPHY
ANNEXURES
ANNEXURE - I CASE SHEET PROFORMA
ANNEXURE - II MASTER CHART
INTRODUCTION
According to VISION 2020 initiative for the elimination of
avoidable blindness globally one of the disease which is given priority is
diabetic retinopathy. In order to prevent this avoidable cause of blindness
the World Health Organization (WHO) has advised all its member
countries to establish various prevention programs to prevent and control
the blindness caused by diabetic retinopathy.
The incidence of Diabetic Retinopathy(DR) is high in most of the
countries with rapid developing economies and they are the leading cause
for preventable blindness1 in these countries than in other countries.
Generally in patients with type 1 diabetes after 5 years they may
show signs of diabetic retinopathy may have signs of retinopathy after 5
years of diabetes, these changes can be seen in almost 25% of the diabetic
patients. which can increase to 60% by the end of 10 years. The chance
of developing retinopathy after 25 years is ,nearly 97% in type 1 diabetic
patients2,3 .but in case of Type 2 diabetic patients during the diagnosis
people affected by diabetes will reach 438 million which is almost twice
the present affected population which is nearly 285 million.
The burden of DR is likely to be significant, because the incidence
of diabetic retinopathy is likely to increase with increase duration of
diabetes mellitus. Due to the vast development in the healthcare and the
better management of the diabetic complications due to cardiac and renal
complications the life exptectancy of the diabetic patients is high. So the
chance of developing DR is high.
The exact cause of diabetic microvascular disease is unknown.
Exposure to hyperglycemia over an extended period results in a number
of biochemical and physiological changes like increased platelet
adhesiveness, increased red blood cell aggregation, defective fibrinolysis
and upregulation of Vascular Endothelial Growth Factor(VEGF) .
Although there are no pathogens in DR, analysis of inflammatory
molecules in vitreous, serum and retina form diabetic patients or
experimental animals indicate that DR is associated with significant
increases in pro-inflammatory cytokines, chemokines and adhesion
molecules the presence of TNF-α has been noticed in vitreous, serum and
ocular fibrovascular membranes from patients with DR and its level has
model of diabetes mellitus. Interleukin-1β (IL-1β) is significantly
increased in vitreous, retina and serum from diabetic patients and rats.
The various risk factors for Diabetic Retinopathy are duration of
Diabetes mellitus, glycemic control, associated systemic hypertension
,nephropathy, anemia.
There are various other factors like nitric oxide synthase
dysregulation (NOS) , oxidative stress and formation of advanced
glycation end products which can also been shown to induce
inflammation by a variety of mechanisms.
Bilirubin is the orange-yellow pigment which is derived from
senescent red blood cells4. They are extracted and biotransformed mainly
in liver and excreted in bile and urine.Various studies has been carried
out to study the antioxidant 5,6 role of serum bilirubin and its association
with the microvascular complications of diabetes but its role with
retinopathy needs to be furthur observed, if proved about the protective
action7,8 of serum bilirubin against diabetic retinopathy it will play a
AIM
Aim:
To study association between serum bilirubin & severity
REVIEW OF LITERATURE
HISTORY OF DIABETES:
Diabetes was the term which was first told to as by a famous
physician Aretaeus of Cappadocia in Rome. During the 2nd century AD.
Greek verb ”diabaino” which means „to pass through‟ was used to define
the condition where the amount of urine passed by the patient was
increased11. In Indian texts they have mentioned about a disease
“Madhumeha” which would be similar to the term “Diabetes mellitus”,
these factors suggesting that diabetes must have been present even before
2500 BC in India. Although, there is no evidence as to how prevalent the
condition was, some of the recent articles suggest that a that it could
have been quite common in India even during ancient times12.
Although diabetes was a well known disease since 2nd century
A.D, but doctors have attempted or documented to link it with an eye
pathology before the middle of 19th century.
Epidemiology
Worldwide the growth and prevalence of diabetes mellitus is very
rapid.by the end of year 2030 it is estimated to reach 438million.in that
the major proportion of diabetes mellitus is expected to occur in
developing countries of the world14. In terms of estimated increase the
major number of increase is expected to be in the Asia region countries of
the top ten countries in the world that includes India, Pakistan and
Bangladesh. So India is apparently the diabetes capital of the world and is
likely to remain so for 30 years.
The main reason for the rapid rise in number of cases is predicted
to be a result of an aging global population due to medical care,
Etiologic based classification of diabetes mellitus
I. Diabetes type 1 (β-cell destruction, usually leading to absolute
insulindeficiency)
A. Immune-mediated
B. Idiopathic
II. Diabetes type 2 (may range from predominantly insulin
resistancewith relative insulin deficiency to a predominantly insulin
secretorydefect with insulin resistance)
III. Gestational diabetes mellitus (GDM).
IV. Various specific types of diabetes
A. Genetic defects of β-cell function characterized by mutations in :
1. Hepatocyte nuclear transcription factor (HNF) 4α (MODY 1)
2. Glucokinase (MODY 2)
3. HNF – 1α (MODY 3)
4. Insulin promoter factor (IPF) 1 (MODY 4)
5. HNF – 1β (MODY 5)
B. Genetic defects in insulin action.
1. Type A insulin resistance
2. Leprechaunism
3. Rabson-Mendenhall syndrome
4 Lipodystrophy syndromes.
C. Diseases of the exocrine pancreas – pancreatitis, pancreatectomy,
neoplasia, cystic fibrosis, hemochromatosis, fibrocalculous
pancreatopathy.
D. Endocrinopathies – acromegaly, Cushing’s syndrome, glucagonoma,
pheochromocytoma, hyperthyroidism, somatostatinoma, aldosteronoma
E. Drug or chemical induced – Vacor, pentamidine, nicotinic acid,
glucocorticoids, thyroid hormone, diazoxide, beta-adrenergic agonists,
thiazides, phenytoin, α– interferon, protease inhibitors, clozapine, beta
blockers.
F. Infections – congenital rubella, cytomegalovirus, coxsackie.
G. Uncommon forms of immune-mediated diabetes – “stiff-man”
syndrome, anti-insulin receptor antibodies.
H. Other genetic syndromes sometimes associated with diabetes –Down’s
syndrome, Friedreich’s ataxia, Huntington’s chorea,
Laurence-Moon-Biedl syndrome, myotonic dystrophy, porphyria, Prader-Willi syndrome.
TYPE 1 DIABETES MELLITUS
Immune Mediated Diabetes (Type 1A)
Only 5-10% accounts for this type of diabetes, cellular mediated
autoimmune destruction of the β-cells of pancreas is the main cause of
this group of DM. Islet cell auto antibodies, autoantibodies to insulin,
autoantibodies to glutamic acid decarboxylase (GAD65) and
autoantibodies to the tyrosine phosphatases IA-2 and IA-2B are the
various markers responsible for the immune destruction of the β-cells. In
85-90% of individuals one or more of the auto antibodies are present.
this disease has strong association with HLA,DQA and DQB genes.
Destruction rate of the β-cell destruction is quite variable in this form of
the diabetes.
They are usually rapid in children than adults. Diabetic
Ketoacidosis can be the first manifestation in some patients, particularly
Some of the other autoimmune disorders associated with immune
mediated diabetic mellitus are such as- Myasthenia gravis ,Grave’s
disease, pernicious anemia, Hashimoto’s thyroiditis, Addison’s disease,
vitiligo, celiac sprues and
Idiopathic Diabetes (Type 1B)
These are the forms of type 1 diabetes which has no known
etiologies. These patients will present with permanent insulinopenia and
they are more are prone to diabetic ketoacidosis, but they have not
evidence of any autoimmunity. The number of patients with this
presenation are very less. They are more commonly seen in patients with
african or Asian ancestry. These individuals are more prone to develop
episode of ketoacidosis and they are prone to develop deficiency of
TYPE 2 DIABETES MELLITUS
Almost 90-95% accounts for this form of diabetes, these are the
individuals who will develop resistance to insulin and usually have
relative (rather than absolute) insulin deficiency.
They are multifactorial and they can be caused due to various
factors.
Obesity is seen commonly in patients with type-2 diabetes mellitus
and they will itself lead to some degree of insulin resistance. Later
diabetic Ketoacidosis seldom will occurs spontaneously usually most of
the time this form of diadetes with not be diagnosed for years, since the
development of hyperglycemia is gradually.
Nevertheless, these patients are at higher risk of developing
diabetics related macrovascular and microvascular complications.
Various factor plays a vital role to develop this form of diabetes like
obesity, and lack of physical activity they will occurs more frequently in
women with prior history of GDM (Gestational diabetes mellitus), and
GESTATIONAL DIABETES MELLITUS (GDM)
This is also known as development of Glucose intolerance during
pregnancy. Insulin resistance related to the metabolic changes of late
pregnancy will lead to increase the requirement of insulin and it can lead
to IGT. Approximately 4% of pregnancies will develop GDM. Most
women will reduce to normal glucose tolerance level postpartum, but
have a substantial chance of developing diabetes mellitus later in life is
(30-60%)13.
OTHER TYPES OF DM
Other etiologies of diabetes mellitus include specific genetic
defects in insulin secretion or action, metabolic abnormalities that impair
insulin secretion, mitochondrial abnormalities and a host of conditions
that impair glucose tolerance. MODY (Maturity Onset Diabetes of
Young) is a subtype of diabetes mellitus characterized by autosomal
dominant inheritance, early onset of hyperglycemia, and impairment of
insulin secretion.
Diabetes mellitus can result from pancreatic exocrine disease when
the majority of pancreatic islets (>80%) are destroyed. Hormones that
diabetes mellitus, is often a feature of endocrinopathies, such as
acromegaly and Cushing’s disease.
IMPAIRED GLUCOSE TOLERANCE (IGT) AND IMPAIRED
FASTING GLUCOSE (IFG)
The expert committee recognized an intermediate group of subjects
whose glucose levels, although not meeting criteria for diabetes, are
nevertheless too high to be considered normal15.
This group is defined as having fasting plasma glucose (FPG)
levels between 100 mg /dl (5.6 mmol/l) to 125 mg% (7.0 mmol/l) or 2 hr
values of oral 15glucose tolerance test (OGTT) of ≥ 140 mg/dl (7.8
mmol/l) but < 200 mg/dl (11.5 mmol/l). Thus categories of FPG values
are as follows:
FPG < 100mg/dl (5.6 mmol/l) = Normal fasting glucose
FPG 100 – 125 mg/dl (5.6-6.9 m mol/L) = IFG (Impaired fasting
glucose)
FPG ≥ 126 mg/dl (7.00 m mol/L) = Diabetes Corresponding
2h post load glucose 140-199 mg/dl (7.8 – 11.1 mmol/L) = IGT
(Impaired glucose tolerance)
2 h post load glucose ≥ 200 mg/dl (11.1 m mol/L) = Diabetes.
Patients with IFG and IGT are now referred to as having
‘Prediabetes’ indicating relatively high risk for development of diabetes
DIAGNOSTIC CRITERIA FOR DIABETES MELLITUS 14,15
Criteria for the Diagnosis of Diabetes Mellitus
• Along with the presence of diabetes symptoms plus(RBS) random
blood glucose concentration ≥11.1
mmol/L (200 mg/dL)a or
•The level of (FBS)Fasting plasma glucose ≥ 7.0 mol/L (126 mg/dL)b or
• The level of (PPBS)Two-hour plasma glucose ≥ 11.1 mmol/L (200
mg/dL) during an oral glucose tolerance test c
a ( RBS).Random is defined as without regard to time since the last
meal
b. (FBS)Fasting is defined as no caloric intake for atleast 8 h.
c. (PPBS)The test should be performed using a glucose load
containing the equivalent of 75g anhydrous glucose dissolved in
water.
SCREENING FOR DIABETES
Most of the time the diagnose of diabetes is not done until
complications appear and almost one third of all diabetic patients may be
undiagnosed. But yet there is no randomized trials demonstrating benefits
of early diagnosis of diabetes through screening of asymptomatic
individuals. But the wide spread use of screening test such as FPG for
high risk T-2 diabetes mellitus individuals is justified15.
(source:Adapted from American Diabetic Association,2004)
Risk factors for Type 2 Diabetes Mellitus
• Presence of Family history of diabetes (i.e. parent or sibling with type 2
diabetes)
• Presence of Obesity (BMI≥25 kg/m2)
• Physical inactivity
• Various Race/ethnicity (e.g. African, American, Hispanic American,
Native American, Asian American, Pacific Islander)
• Previously identified IFG or IGT
•Presence of History of GDM or delivery of baby > 4kg (>9 Ib)
• Presence of associated Hypertension (blood pressure ≥ 140/90 mHg)
• Presence of HDL cholesterol level ≤ 35mg/dL (0.90mmol/L) and / or a
triglyceride level ≥ 250mg/dL (2.82 mol/L)
• Presence of Polycystic ovary syndrome or acanthosis nigricans.
The most suitable test for diabetes are FPG test and oral glucose
tolerance test (OGTT).but mostly FPG test is easier and faster to perform
so they are commonly used in clinical settings.It is more acceptable to
patients and less expensive. An FPG>126 mg/dl is an indication for
retesting, which should be repeated on a different day to confirm
diagnosis. The indicator to repeat the FPG test is if the value is <126
mg/dl and there is a high suspicion for diabetes,in this condition an
OGTT should be performed. A 2hr post load valueif the value is
≥200mg/dl the test is positive for diabetes and it has to be confirmed on
an alternate day.
The HbA1C remains a important tool to monitor glycemic level,
but for the screening or diagnosis of diabetes nowdays they are not
recommended.
VARIOUS LEVEL OF CARE IN DIABETES
Medical care of diabetes and carefull education of the course and
Medical history
The patient must be asked about the detailed history of the signs
and Symptoms.the results of laboratory tests done previously must
be taken into account, and all previously done and various results
related to the diabetes must be noted.
Detailed history about the patients eating patterns, present status of
nutritional, and detailed weight history, growth and development
in children and adolescents, history of hormonal imbalance must be
noted.
Detailed history about the physical activities and exercise must be
noted.
History of any signs of acute complications such as diabetic
ketoacidosis and hypoglycemia.
Prior or current infections, particularly skin, foot, dental, and
genitourinary infections.
Detailed history of any treatment of eye, kidney, nerve,
genitourinary (including sexual), bladder,heart, peripheral vascular,
foot and cerebrovascular complications associated with diabetes.
Note the presence of risk factors that can lead to associated
complications like atherosclerosis; smoking, hypertension, obesity,
Family history of diabetes and other endocrine disorders.
Use of tobacco and alcohol must be noted.
Contraception and reproductive and sexual history.
Physical examination
This is a vital examination and calculation of BMI is vital. Height
and weight of the patients are usually noted and comparison to
norms in children and adolescents.
Detailed history of Sexual maturation staging (during pubertal
period).
Blood pressure determination, including orthostatic measurements
when indicated, and comparison to age-related norms.
evaluation of eyes to ruleout retinopathy
evaluation of oral is done.
palpation of Thyroid.
Neurological examination and Cardiovasular examination.
Abdominal examination (e.g. for hepatomegaly).
Signs of diseases that can cause secondary diabetes (e.g.
hemochromatosis, pancreatic disease).
Laboratory evaluation
HBA1C.
Complete lipid profile evaluation including total cholesterol,
triglycerides, LDL and HDL.
In all the patients who have been diagnosed with type 1 diabetic
patients for morethan 5 years and in all patients with type 2
diabetes they have to be tested for microalbuminuria.
The level of Serum creatinine in adults must be evaluated. (in
children if proteinuria is present).
Evaluation of thyroid prolife test will be needed (TSH) in all type
1 diabetic patients; in type 2 if clinically indicated.
If clinically indicated then Electrocardiogram can be done.
Urine analysis is done for ketones, protein, sediment.
OTHER OPINIONS
Eye exam, if indicated.
Family planning for women of reproductive age.
Diabetes educator, if not provided by physician or practice staff.
Behavioral specialist, as indicated.
Foot specialist, as indicated.
Other specialities and services as appropriate.
Recommendations for Adults Diagnosed with Diabetes
Summary of recommendations for adults with diabetes
Glycemic control
HBA1C < 7.0%
Fasting plasma glucose = 90 – 130 mg/dl (5.0 – 7.2 mmol/l)
Postprandial plasma glucose < 180 mg/dl (< 10.0 mmol/l)
Blood Pressure < 130/80 mmHg
Lipids
LDL < 100 mg/dl (<2.6 mmol/l)
Complications of Diabetes :
Diabetes has both acute and long term complications14.
They are:
Acute
Diabetic ketoacidosis
Hyperglycemic Hyperosmolar state
Hypoglycemia
Long term
Retinopathy
Neuropathy
Nephropathy
Ischemic heart disease
Cerebrovascular disease
Peripheral vascular disease
Others
Infections
Tuberculosis
Candidiasis – oral / volvovaginal
Mucor mycosis
Necrotising fasciitis
Periodontitis
Duputrens contracture
OPHTHALMIC MAINFESTATIONS OF DIABETES16:
1.Ocular conditions directly associated with Diabetes
• Cataract
• Anterior Ischemic Optic Neuropathy
• Diabetic papillopathy
• Extraocular movements disorders
2.Ocular conditions for which diabetes is a known risk factor
• Ocular Ischemic syndrome
• Glaucoma – Primary open angle and Neovascular
3.Ocular conditions for which diabetes is a possible risk factor
• Central Retinal vein occlusion
• Central Retinal arteriolar emboli
• Central Retinal artery occlusion
• Corneal disease
4.Conditions masquerading as diabetic retinopathy in diabetics
• Age related macular degeneration
• Hypertensive retinopathy
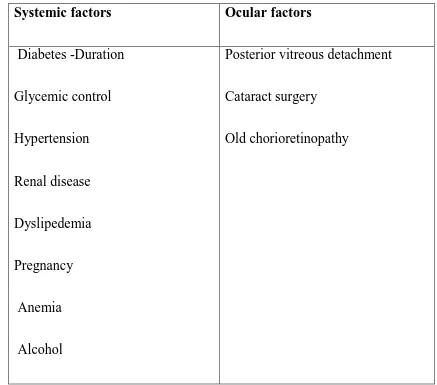
Table – 1 :Various associated Factors with development of diabetic
retinopathy
Systemic factors Ocular factors
Diabetes -Duration
Glycemic control
Hypertension
Renal disease
Dyslipedemia
Pregnancy
Anemia
Alcohol
Posterior vitreous detachment
Cataract surgery
Old chorioretinopathy
Out of all the risk factors associated with diabetic retinopathy the
duration of diabetics is a vital factor and many studies may been done on
RISK FACTORS
1. Duration of Diabetes: Presence of diabetes for Prolonged duration is
a major risk factor in the incidence of Diabetic retinopathy and it has
been observed that almost 50% of the patients develop diabetic
retinopathy after 10 years duration of diabetes and 90% of them
develop after 30 years duration if they have been diagnosed as diabetic
before the age of 30 years.but in rare cases diabetic retinopathy
develops within 5 years of onset of DM or even before puberty. In
around 5% of type 2 DM patients diabetic retinopathy is noted at
presentation itself17.
2. Control of Blood Glucose: The development of diabetic retinopathy
can prevented by good glycemic control.the one of the important and
independent risk factor is the glycosylated Hemoglobin at
baseline.Intensive therapy is recommended by the DCCT to achieve
near normal glycemic status as early as possible in IDDM patients18,19.
3. Hypertension: Most commonly the patients with DM suffer from concomitant hypertension.Nearly 17% of the patients with type1 DM
has been found to have prevalence of hypertension at baseline and
almost 25% were found to have hypertension after 10 years in The
(WESDR)20.In case of type 2 DM patients, the prevalence of
hypertension has been noted to be around 38% to 68% in
cross-sectional studies.it has been observed that progress and the level of
DR is rapid and severe in patients with hypertension they are more
prone to develop associated diffuse DME.
4. Renal Disease: The relationship between microalbuminuria or proteinuria and retinopathy has been observed and reported in various
studies presence of associated renal disease will also act as a risk
factor for diabetic retinopathy21.
Various others risk factor are also present along with the above
factors. they are serum lipids levels, pregnancy, anemia, genetic
Ocular Factors acts as a protective factor in reducing the severity
of Diabetic Retinopathy 17,24,25
1. Glaucoma :Severity of DR is reduced in a glaucomatous
eye.Underlying mechanism is unclear though there are several
suggested possibilities:
• They can be due to complete decrease in the metabolic activity in
retina with due to the loss of ganglion cells secondary to chronic
glaucoma.
• Loss of retinal vascular perfusion secondary to elevated intraocular
pressure.
2. Myopia : Myopia of atleast 5 Dioptres is known to reduce the severity
and prevalence of DR.
3. Carotid arery stenosis : Cases of internal carotid artery narrowing
unilaterally resulting from atherosclerosis has been found to be
protecting the eye on the same from diabetic retinopathy changes.
4. Retinochoroidal scarring : Scarring of retinochoroid in Eyes due to
trauma and inflammatory diseases etc has shown to reduce
prevalence of DR and the degree of DR Changes. This is due to the
decreased retinal metabolism and a decreased need for oxygen would
Epidemiology of Diabetic Retinopathy 26,27
The large numbers of people affected with DR is an indication of
the severity of the problem. Prevalence of Diabetic retinopathy was found
to be 50.3% in USA20, 33.6% in UK28, 29.0% in Australia29 and 17.6% in
India30.
PATHOLOGY OF DIABETIC RETINOPATHY
The pathogenesis of diabetic retinopathy can be described in the
following ways:
1. Biochemical pathways.
2. Retinal vascular changes.
3. Pathological correlates.
1. BIOCHEMICAL PATHWAYS
Even though the cellular mechanisms through which
undergo a series of additional reactions leading to inter and intrachain
cross linking with considerable alteration of protein function.
ii) Accelerated oxidative stress in the cells leads to formation of
excess of toxic end products of oxidation‟ peroxides, superoxides, nitric
oxide and oxygen free radicals” which may remain elevated due to
chronic changes in metabolic pathway.
iii) Changes in the enzymatic pathways due to prolonged
hyperglycemia.
The following are the important biochemical factors implicated in
the pathogenesis32.
1. Vascular endothelial growth factor (VEGF)
They are expressed by vascular endothelial cells of the retina,
pericytes and pigment epithelial cells in response to hypoxia. Stimulates
angiogenesis and increases capillary permeability leading to
neovascularisation and retinal edema respectively.
2. Renin – Angiotensin
In diabetes mellitus, Upregulation of renin-angiotensin system has
stimulated by Angiotensin II which is present in the vascular endothelial
cells of the retina.
3. Erythropoetin
Erythropoetin has been produced primarily due to the retinal
ischaemia and possibly due to hyperglycemia, oxidative stress,
inflammatory cytokines. They can promote VEGF in retinal vascular
endothelial cells.
4. Diacylglycerol and Protein Kinase C
Elevated DAG and PKC activity in the retina correlates with
decreased blood flow rate; also implicated in renal abnormalities like
increased albumin excretion and GFR. PKC in retinal cells gets activated
due to hyperglycemia which will ultimately cause the increase of
expression of matrix proteins and vasoactive mediators.they will lead to
both structural and functional retinal vascular changes.
damage can occur in the retinal endothelial cells and pericytes. Which
can be due to sorbitol.
6. Growth hormone and insulin like growth factor (IGF)
The function of the retinal endothelial precursor cells can be
modulated by these factors. which can drive retinal angiogenesis which
can be caused in response to hypoxia.IGF-1 are capable to disrupt the
blood-retinal barrier and they can increase the permeability.
7. Carbonic anhydrase
In diabetic retinopathy the level of intraocular carbonic anhydrase
is elevated. Meanwhile the level of extracellular carbonic anhydrase will
increases the retinal vascular permeability by increasing pH leading to
2. RETINAL VASCULAR CHANGES
Capillary basement membrane thickening
This is usually measured by electron microscope morphometry.
Additional basement membrane abnormalities of diabetes mellitus
include “Swiss Cheese” like vacuolization and deposition of fibrillar
collagen. Basement membrane collagen is extensively glycated which
may be either qualitatively or quantitatively altered by enzymatic or non
enzymatic processes. Basement membrane serves as filtration barrier for
molecules of various size and electrical charges. Alteration in the amount
or degree of sulfation or in the anatomic distribution of highly negatively
charged heparan sulfate proteoglycan molecules within the basement
membrane can affect their permeability properties to various ions33.
Another function of basement membrane is to regulate cell
proliferation and differentiation33. The role of proteolytic enzymes that
degrade basement membrane components is thought to be important in
blood vessel growth, whether in normal development, in tissue repair or
Loss of pericytes
In early diabetic retinopathy, there is loss of the intramural
pericytes and the exact mechanism is unknown. It may be related to the
action of sorbitol pathway since they find aldose reductase specifically in
retinal capillary pericytes but not in endothelial cells. This gives a
satisfactory explanation of pericyte loss not only in retinal
microcirculation but also elsewhere in the body. Another study postulates
that the alterations of PDGF – B secretion or function produced by
prolonged hyperglycemia or galactosemia, may selectively affect the
pericyte viability leading to their loss by apoptosis34.
Microaneurysms
The earliest clinically observable lesion of diabetic retinopathy are
the microaneurysms. Retinal capillary microaneurysms may represent
focal regions of endothelial cell proliferation, where the antiproliferative
effect of pericytes has been lost. This explains the development of
cellular microaneurysms but not acellular ones.
It is assumed that all microaneurysms are initially cellular, but
some become acellular as a result of extensive apoptosis involving
Another explanation of microaneurysms formation is that they may
arise from weak points in the capillary wall following loss of pericytes.
Since the pericytes are contractile elements of the capillary wall, much
like the smooth muscle cells of larger vessels, the tonus exerted by the
myofibrils in the pericytes may counteract the transmural pressures
produced by the flowing blood and when this tonus is lost, the
microvessel wall may dilate focally to produce a microaneurysms. The
point against this reasoning for microaneurysm development is the
presence of microaneurysm in diseases wherein pericyte loss has not been
observed33.
Break down of Blood Retinal Barrier
One possible cause of blood retinal barrier breakdown is opening
of tight junctions (zonulae occludentes) between adjacent microvascular
endothelial processes.Several proteins are closely involved with tight
junction formationand function. The most widely studied of these are
Fenestrae are normally absent in the thick endothelium of retinal
capillaries, but they have been observed in subjects with retinal
neovascularisation in which blood retinal barrier has broken down.
Another possible explanation is an increase in transport by endocytic
vesicles31.
3. CLASSICAL PATHOLOGICAL LESIONS IN DIABETIC
RETINOPATHY 17,24,25
1. MICROANEURYSMS
Retinal microaneurysms are dilatations of retinal capillaries . They
appear as either pouching on the side of the capillary or looping of the
capillaries with ultimate fusion of the base of the loop and dilatation of
the apex of the loop. These can occur at any level between superficial and
deeper retinal capillary networks or even from choroidal circulation35.
Most microaneurysms are found in the posterior pole and in diabetic
retinopathy there is a predisposition in the area temporal to fovea. Almost
always it is possible to identify a variable area of capillary nonperfusion
The aneurysms may reflect:
(i) Out pouching from capillary wall due to loss of pericyte support.
(ii) Active cellular response to retinal hypoxic insult.
The size usually ranges from 12-100 m in diameter. Generally a
size of 125 m is considered as upper limit with sharp margins, smooth
borders, round shape and central light reflex are considered if a lesion is
to be distinguished as a microaneurysm35.
Retinal microaneurysms may follow a variable course. Small
microaneurysms may become larger and leak. Others may develop
hyalinised wall and appear white.
As the area of capillary nonperfusion enlarges, the microaneurysms
may disappear with new microaneurysms appearing later at the edge of
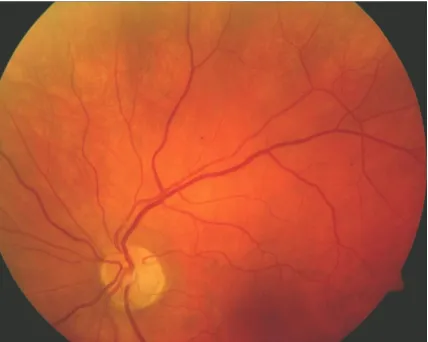
Figure – 1 : Microaneurysms
2. INTRARETINAL HEMORRHAGES
The intraretinal hemorrhages appear secondary to ruptured
microaneurysms, capillaries or venules. Their shape is dependent on the
location of the hemorrhage within the retinal layers35.
Commonly the intraretinal hemorrhages are of two types:
i) Superficial
ii) Deep
i) Superficial
• These are usually flame shaped and occur in the nerve fibre layer
of the retina35.
The shape is due to
• Tighter organization of the cells in the nerve fibre layer.
• Relative paucity of extracellular space due to compact nerve fibre
arrangement.
and ample extracellular space allows the hemorrhage to take a larger
form. Some hemorrhages may have a white centre which probably
represents auto occlusion.
The intraretinal hemorrhages resolve within 6 to 12 weeks. Their
usual site is the posterior pole, however they can occur anywhere in the
fundus. They usually do not cause visual obscuration unless they are
3. HARD EXUDATES
Hard exudates represent an accumulation of lipid, lipid laden
macrophages and/or protein within the sensory retina. These are usually
located within the outer plexiform layer. They have a predilection for the
posterior pole, being intimately associated with retinal thickening.
Ophthalmoscopically, they appear glistening, yellowish-white and waxy.
Hard exudates are arranged in different patterns, in the form of
streaks or clusters or in circinate arrangement around an area of
abnormal leaking capillaries and microaneurysms. They are a hallmark of
clinically significant macular edema.
Hard exudates may either resolve spontaneously or following laser
photocoagulation, being phagocytosed by macrophages. If present
chronically, hard exudates, may organize into hard plaques, eventually
forming a disciform scar.
4. SOFT EXUDATES/COTTON WOOL SPOTS
Extensive arteriolar closure in severe and advanced NPDR leads to
infarcts of the nerve fibre layer. These are referred to as cotton wool
spots/soft exudates.
Pathologically, occlusion (or) decreased flow of an arteriole leads
to axoplasmic stasis and retinal tissue swelling in the nerve fibre layer.
These appear as bright, fluffy, whitish-yellow lesions with fuzzy margins.
They usually resolve in 2-3 months but may take much longer. Residual
nerve fibre layer atrophy and ganglion cell atrophy at the site where a
cotton wool spot existed is referred to as „depression sign of Goldmann‟.
„Strict‟ or „Rapid‟ metabolic control in patients with diabetes leads to
raise in the number of cotton wool spots.
5. VENOUS ABNORMALITIES
• Venous dilatation
• Venous beading
• Venous loops
These changes are associated with capillary nonperfusion and
retinal ischemia and are correlated with an increased probability of
progression to proliferative retinopathy.
Venous dilatation
Venous dilatation is the earliest change described in diabetic
retinopathy. This change represents the preclinical stage of diabetic
retinopathy and may be difficult to assess.
Venous beading
Venous beading represents focal areas of venous dilatation with
apparent thinning of the venous wall. It is associated with venous
dilatation. There is always a degree of capillary nonperfusion in the area
of venous beading. Histopathologically, the walls of beaded veins
become thickened later and undergo hyaline degeneration.
Venous loops
Localized areas of deviation of the vein which may be present on
2. Development of fibrous tissue in the vessel which contracts to create
a loop.
The area peripheral to the loop show capillary nonperfusion. They
have no prognostic value for the development of PDR or increase in the
severity of DR..
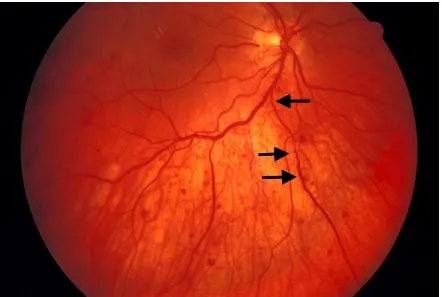
[image:57.595.108.550.267.564.2]
Foveal avascular zone abnormalities
Foveal avascular zone is approximately 350 to 750 μm in
diameter. In diabetic eyes, abnormalities of the foveal avascular zone are
seen. These abnormalities include:
1. Enlargement of FAZ
2. Irregular margins
3. Capillary budding into the FAZ
4. Widening of the intercapillary spaces within the perifoveolar
capillary bed
Intraretinal microvascular abnormalities (IRMA)
IRMA refers to dilated tortuous telangiectatic channels that occur
between diseased arterioles and venules. These are present within areas of
arteriolar and capillary nonprefuson. They appear as fine blood vessels. It
is difficult to differentiate them from early surface neovascularisation
Neovascularisation
It is the hallmark of PDR. It refers to new vessels that arise from
retina or optic disc and proliferate along retinal surface or into vitreous
with or without a fibrous component37. It is most commonly associated
with mid-peripheral capillary non-perfusion. It is most commonly located
posteriorly within 45 degree of the optic disc and/or on the optic disc
itself.
NVD:
New vessels located on or within one disc diameter of the optic
disc. Appear as fine wisps of blood vessels looping across other disc
vessels. They create an advancing edge as they branch earlier forming
proximal loops. It is best appreciated by Goldmann contact lens or non
contact lens like Hruby lens or 78D lens.
NVE:
Neovascularisation anywhere in the retina apart from NVD is
termed NVE. They are seen as wheel like network of fine vessels from
retinal veins/capillaries crossing between arterial and venous sides. Well
intraretinally but eventually break through the retinal internal limiting
membrane and proliferate.
[image:60.595.113.519.187.490.2]
CLASSIFICATION
Various terminologies and clinical classifications have been used
as a clinical scale to distinguish various grades of diabetic retinopathy.
One of the important classifications commonly used is the modified airlie
house classification and abbreviated ETDRS classification. This has been
described below:
CLASSIFICATION OF DIABETIC RETINOPATHY 38
MODIFIED AIRLIE HOUSE CLASSIFICATION
ABBREVIATED ETDRS CLASSIFICATION:
CATEGORY DESCRIPTION MANAGEMENT
NON-PROLIFERATIVE DIABETIC RETINOPATHY (NPDR)
No DR Review in 12 months
Very mild : Microaneurysms only Review most patients in 12 months
Mild : Any or all of: Microaneurysms,
retinal hemorrhages, exudates,
cotton wool spots, up to the level of
moderate NPDR. No IRMA or
significant Beading
Review range 6-12 months,
depending on severity of signs,
stability, systemic factors, patient’s
Moderate:
Severe retinal hemorrhages (more than
ETDRS standard photograph 2A)
Significant venous beading in no more
than 1 quadrant Cotton wool spots
commonly present
Review in approximately 6
months
Severe
4:2:1 rule : one or more of :
Severe hemorrhages in all 4 quadrants
Significant venous beading in 2 or
more quadrants
Moderate IRMA in 1 or more
Quadrants
Review in 4 months
Very Severe
2 or more of the criteria for severe Review in 2-3 months
PROLIFERATIVE DIABETIC RETINOPATHY (PDR)
MILD-MODERATE
HIGH RISK
New vessels on disc (NVD) greater
than ETDRS standard photograph 10A
(about 1/3 disc area)
Any NVD with vitreous or preretinal
Hemorrhage
NVE greater than ½ disc area with
vitreous or preretinal hemorrhage (or
Hemorrhage with presumed obscure
NVD/E)
Immediate treatment
Advanced diabetic eye disease
Tractional retinal detachment,
Significant persistent vitreous
hemorrhage and neovascular glaucoma
Severe NPDR
NVD [PDR]
[image:66.595.146.465.71.341.2]FEATURELESS RETINA
In the late stage of the NPDR, larger arterioles may occlude
completely resulting in extensive capillary non-perfusion. Retina may
appear thin and atrophic and does not show any background lesions. This
may result in underestimation of the actual severity of the disease.
Careful evaluation has to be done for occluded arterioles and areas of
avascular retina that is thinner and duller compared to healthy retina.
Fluorescein angiography reveals extensive areas of capillary
non-perfusion. This is an important sign as these patients may develop
neovascularisation of iris and angle without showing any retinal
Figure 9: Fundus Color Photograph Showing Neovascularisation
METHODS OF RETINAL EXAMINATION 17,24,25
Various methods can be used to evaluate retinal changes in diabetic
retinopathy.
1.DIRECT OPHTHALMOSCOPY
One of the most commonly used and old method to examine the
retina .Though an easy and convenient method, its two main
disadvantages are the lack of a stereoscopic view of structural changes
which are three dimensional by nature and the difficulty of recording and
transmitting the information or of making any form of quantitative
assessment of the disturbance.
2.INDIRECT OPHTHALMOSCOPY
Indirect ophthalmoscopy is more useful in patients with opacities
in the ocular media. Good illumination and wide field of view make this
the instrument of choice for examining retina in detail upto the periphery.
Indentation will give view of the peripheral retina.
contact lens. It is used during laser photocoagulation and during
vitrectomy. The central zone of 3 mirror contact lens can also be used as
a fundus viewing lens.
By 90D or 78D condensing lenses, the real image of the retina
formed by the condensing lenses may be viewed through slit lamp
microscope. The 90D lens gives a wider field of view but lesser
magnification than the 78D lens. Though it gives an excellent view of the
posterior pole of the fundus, it is less suitable for examining the
periphery of retina. It gives a stereoscopic view of the macula. The
panfundoscopic contact lens gives a panoramic view of the retina.
4. FUNDUS PHOTOGRAPHY
Grading of retinopathy can be done with the help of fundus
photographs and the progression or the effect of treatment can be
assessed by serial photographs.
In this study I used the Zeiss FF450 Plus camera to take fundus
photographs.
5. FLUORESCEIN ANGIOGRAPHY (FFA)
This allows us to examine structures in the retina which are beyond
hemodynamic changes that occur in the retina and the localised
abnormalities of flow and perfusion that are the background for many
pathological disturbances.
Under normal circumstances the contrast medium fluorescein,does
not leak out of the retinal vessels.Abnormal fluorescence in an angiogram
may be due to:
(1) Hyperfluorescence
• The dye leakage from microaneurysms, IRMA, new vessels and
from damaged capillaries
• The dye leakage from optic nerve head in NVD
• Tissue staining will be seen as a result of prolonged retention of
fluorescein
(2) Hypofluorescence
• Result of Blockage of fluorescence is seen by increased density of
pigment (xanthophyll), hard exudates and blood
• Capillary nonperfusion areas are seen as a result of Obstruction of
Figure 11 : Fundus Fluorescein Angiogram
[image:73.595.68.529.418.696.2]
FFA is an excellent method of showing retinal capillaries and a
good guide for laser photocoagulation and to assess the effect of
treatment.Neovascularisation elsewhere occurs usually at the junction
of perfused and non-perfused retina and the most common location is
along the temporal vascular arcades.39
5. ELECTRO DIAGNOSTIC TESTS (ERG)
It is the record of an action potential produced by the retina when it
is stimulated by light of adequate intensity.
It is useful in assessing retinal function in diabetic retinopathy,
when the media is opaque due to cataract or vitreous hemorrhage.
6. ULTRASOUND ‘B’ SCAN
In DR, it is used when the media is opaque to detect whether
there is any vitreous hemorrhage, posterior vitreous detachment,
traction or rhegmatogenous retinal detachment or to detect the
presence of epiretinal membranes.
• Vitreous opacities produce dots or short lines.
7. VISUAL ACUITY
It is the most important test of macular function, particularly for
near. Hypermetropia, with disparity between the subjective and objective
refraction of the eye, is characteristic of a shallow elevation of sensory
retina at macula. In CSMO, near visual acuity is affected.
8. AMSLER GRID
Evaluates the 20 degrees of visual field surrounding fixation. It is
primarily used for screening macular function.
9. PHOTOSRESS TEST
May be useful in demonstrating macular lesions when
ophthalmoscopy is equivocal in early cystoid macular edema.
10. POTENTIAL ACUITY METER
This is done by projecting a standard Snellen’s chart onto the macula
through a small area of an immature cataract and asking the patient to
TREATMENT OF DIABETIC RETINOPATHY40,41
Essential step and the very first step is control of diabetes. This is
very important in preventing development of microvascular
complications. The main modes of treatment of diabetes mellitus are:
1. INSULIN THERAPY
This is the mainstay in youth onset diabetes and maturity onset
diabetes,in whom oral hypoglycaemic agents have failed to maintain
satisfactory blood sugar levels.
Available insulin preparations are:
• Rapid acting preparations – for intravenous, intramuscular and
subcutaneous use with peak activity of 2-4hrs.
• Intermediate acting preparations – such as NPH (Isophane) and Lente
(Zinc) with a 6-12 hr span of peak activity.
• Long acting preparations – such as ultra lente and protamine zinc
insulin (PZI) with 14-24 hrs span of maximal action.
• Human Insulin- synthetic insulin with a structure identical to that of
human hormone has largely replaced animal insulins. It is produced
Regimen of meticulous control
• Intensified multiple subcutaneous insulin injections
• Continuous subcutaneous insulin infusion
• Implantable intraperitoneal pumps
Risk of meticulous control
Acceleration of diabetic retinopathy- though not a common
complication, amelioration of severe retinopathy cannot be expected.
According to DCCT study, the progression of early retinopathy slowed
down.BDR is not a contraindication for meticulous control, but frequent
ophthalmologic surveillance is required to detect accelerated
neovascularisation. The reason for worsening is unknown. Perhaps
retinal glucopenia may stimulate vascular endothelial growth factor
(VEGF).VEGF receptors are present in endothelial cells of retina and of
major vessels.
2.DIET THERAPY
Normal weight persons with diabetes usually require about 35kcal/kg
body weight/day and 0.8-1gm protein/kg body wt/day. A standard
recommendation is for fat content to be 30% or less of total calories and
3. EXERCISE
4. ORAL HYPOGLYCEMIC AGENTS
• SULPHONYL UREAS –Glipizide, Glimepride, Glyburide
• BIGUANIDES – Metformin
• THIAZOLIDINEDIONES – Pioglitazone, Rosiglitazone
• MEGLITINIDES – Nateglinide, Repaglinide
• α – GLUCOSIDASE INHIBITORS – Acarbose, Miglitol
• DPP-IV INHIBITORS - Sitagliptin
SPECIFIC TREATMENT FOR DIABETIC RETINOPATHY
• Laser Photocoagulation
• Surgical – Vitrectomy, Intravitreal Injections
LASER PHOTOCOAGULATION
It is recommended that patients with severe and very severe NPDR
must receive laser treatment when exposed to several risk factors that
Risk factors for laser treatment42:
NON-MODIFIABLE Diabetes Mellitus type I
Opposite eye with PDR
Extensive zones of capillary closure on FFA
MODIFIABLE Glycemic control
Elevated serum lipids
Hypertension
Renal dysfunction
TIMEABLE Pregnancy
Cataract in evolution
Strict glycemic control
Irregular followup
Macular photocoagulation for CSME are of two types17,39:
1. Focal – for leaking microaneurysm
2. Grid – for diffuse macular edema
Since the visual outcome following grid laser is poor, surgical
intervention is preferred instead. Focal laser for CSME should precede
Pan retinal photocoagulation by 6-8 weeks ideally.
Panretinal photocoagulation is usually done in 2 or more sessions
done and in the second session, the superior quadrants and also open
macular closure are done. More sessions may be added if required.
ETDRS RESEARCH GROUP PROTOCOL FOR PRP43
Spot size 500microns
Exposure time 0.1s
Intensity Moderate
Number of shots 1200 – 1600
Location Diameter of shot separation, >2DD out of
fovea to the equator
Number of sessions At least 2
Treated lesions directly New vessels 2DD extrapapillary
Indications for new
treatment
Areas of new vessels extrapapillary,
SURGICAL THERAPY
Pars Plana Vitrectomy:
Pars plana vitrectomy is the surgical therapy and its Indications are44,
• Vitreous hemorrhage which is severe and long standing.
• Retinal detachment with traction on the macula
• Conditions with the presence of both tractional and
rhegmatogenous detachment
• Fibrovascular proliferation which is very severe and progressive
• Dense pre-macular hemorrhage
• Macular edema associated with or without posterior hyaloid
traction
• Diffuse macular edema with massive hard exudates
• In case of associated Ghost cell glaucoma
• In case of Anterior hyaloidal fibrovascular proliferation
• In case of associate Fibrinoid syndrome with retinal detachment.
Vitrectomy with Internal Limiting membrane peeling at macula in
cases of diabetic macular edema is done with the main objective being
relieving the traction of ILM on macular area leaving retinal tissue force
to settle and absorb the edema.45,46 Prompt, rather than early vitrectomy,
pre-retinal hemorrhage confined within an incomplete PVD overlying the
area centralis47.
Intravitreal Injections:
Intravitreal Triamcinolone acetonide (IVTA) during vitrectomy or
given alone is reported to cause short term regression of diabetic macular
edema and increase visual acuity. IVTA after 6 months or less leads to
prolonged beneficial improvement of vision48,49.
Anti-VEGF antibodies like Bevacizumab (Avastin), Pegaptanib
(Macugen), Ranibizumab (Lucentis) are widely used nowadays for the
treatment of neovascularisation in DR.
Protein Kinase C (Pkc) Inhibitors like LY333531 (ruboxistaurin,
RBX) and PKC412 (midostaurin) are currently being studied for the
BILIRUBIN
Bilirubin is the orange-yellow pigment which is derived from
senescent red blood cells. They are extracted and biotransformed mainly
in liver and excreted in bile and urine. This is the brief outline about
bilirubin and various other details are explained below.
In the year 1849 Virchow discovered a yellow pigment in blood
extravasatesand ha called it as “hematoidin”.later in the year 1864
Stadeler coined it as “bilirubin”,it was Tarchanoff who demonstrated the
direct association of bile pigments to Hb(hemoglobin).then it was Fisher
and Plieninger in 1942 who synthesized Bilirubin IXα and proposed the
structure of bilirubin.This linear tetrapyrolic structure of bilirubin was
accepted for morethan 30 years.the bilirubin is usually insoluble in water
Bilirubin IXα is produced from the catabolism of protoporphyrin
IX by a microsomal heme oxygenase.the tetra pyrolic product of the ring
opening at the α-methene bridge is the green pigment biliverdin,they are
the pigments which is subsequently reduced to bilirubin by reduced form
of nicotinamide adenine dinucleotide
phosphate(NADPH)-dependent,cytosolic enxyme bilirubin reductase.
Each mole of heme catabolized by this pathway will produces one
mole of carbon monoxide,bilirubin and ferric iron.Daily bilirubin
production from all sources in man averages from 250 to 300 mg.Almost
85% of the total amount of bilirubin produced in the body are derived
from various organs of the body like spleen,liver and bone marrow in
which the reticuloendothelial cells are present in which the heme moiety
of Hb released from senescent erythrocytes are destroyed.
Remaining 15% bilirubin of the body are produced from the RBC
precursor destroyed in bone marrow and due to catabolism of other heme
containing proteins in the body such as Myoglobin,Cytochromes and
Peroxidases.
In the liver cells they are reversibly bound to soluble protein known as
“ligandins”or “Protein Y”.It plays a vital role in processing of various
compounds that binds with it like steroids,bromsulfthalein,indocyanine
green and some carinogens.thus they may increase the net efficiency of
uptake by retarding the reflux of these various substances back to
plasma.the bilirubin present inside the hepatocytes will conjugate with the
glucuronic acid to produce bilirubin monoglucuronide and
diglucuronide.they are finally excreted into the bile.
Generally, all the bilirubin excreted in bile is in the form of
glucosidic conjugates; In that 95% are glucuronides and 5% are
glucosides and xylosides.Also Diglucuronide forms the 90% of the total
glucuronides and minor fraction by monoglucuronides 10%.
In intestine bilirubin glucuronides are not later reabsorbed.they are
generally hydrolysed by catalytic action of β-glucuronidase from the
intestinal epithetial cells,liver and bacteria.
Usually the unconjugated bilirubin are reduced by anaerobic
intestinal microbial flora to form a group of three tetrapyroles which are
colourless they are known as “Urobilinogens”.In all the three
Urobilinogens the carbon bridge are saturated(methylene) form.each one
of them differ from eachother in the degree of hydrogenation of vinyl side
6,8&12 more hydrogen atoms than bilirubin are named as
Stereobilinogen,Mesobilinogen and Urobilinogen respectively.The
amount of urobilinogens reabsorbed from the intestine and enters the
enterohepatic circulation daily is nearly 20%. In that most of the
reabsorbed urobilinogens is taken up by the liver and they are excreted by
bile.
These are the various importance about the bilirubin structure,
ANALYTICAL METHODOLOGY OF BILIRUBIN:
In order to measure the bilirubin and its metabolites in serum,urine
and feces various techniques are used are below,
1.Diazo methods:
In 1916 Van den bergh and Muller applied diazo reaction to
measure the bilirubin in serum and bile.In mid 1950 Billing,Cole and
Lathe described the chemical nature of direct and indirect bilirubin.Later
Knenzle and colleagues were the first to successfully use an open-column
chromatography technique that didn’t involue a depolarization step.
Other methods widely used in the analysis of bilirubin are namely,
2. High performance liquid chromatography:
3. Enzymatic:
4 .Spectophotometric:
These are the various importance of the analytical methods used to