0022-538X/06/$08.00⫹0 doi:10.1128/JVI.00473-06
Copyright © 2006, American Society for Microbiology. All Rights Reserved.
Epstein-Barr Virus BNRF1 Protein Allows Efficient Transfer from the
Endosomal Compartment to the Nucleus of Primary B Lymphocytes
R. Feederle,
1,2† B. Neuhierl,
1† G. Baldwin,
2H. Bannert,
1B. Hub,
1J. Mautner,
3U. Behrends,
3and H. J. Delecluse
1,2*
German Cancer Research Center, Department of Virus Associated Tumours, Heidelberg, Germany1; Cancer Research UK Institute for
Cancer Studies, University of Birmingham, Department of Pathology, Birmingham, United Kingdom2; and
Clinical Cooperation Group, Children’s Hospital, Hematology-Oncology, Technical University Munich, Munich, Germany3
Received 7 March 2006/Accepted 18 July 2006
Epstein-Barr virus (EBV) is a tumor virus with marked B lymphotropism. After crossing the B-cell mem-brane, the virus enters cytoplasmic vesicles, where decapsidation takes place to allow transfer of the viral DNA to the cell nucleus. BNRF1 has been characterized as the EBV major tegument protein, but its precise function is unknown. We have constructed a viral mutant that lacks the BNRF1 gene and report here its in vitro phenotype. A recombinant virus devoid of BNRF1 (⌬BNRF1) showed efficient DNA replication and production of mature viral particles. B cells infected with the⌬BNRF1 mutant presented viral lytic antigens as efficiently as B cells infected with wild-type or BNRF1trans-complemented⌬BNRF1 viruses. Antigen presentation in B cells infected with either wild-type (EBV-wt) or⌬BNRF1 virus was blocked by leupeptin addition, showing that both viruses reach the endosome/lysosome compartment. These data were confirmed by direct observation of the mutant virus in endosomes of infected B cells by electron microscopy. However, we observed a 20-fold reduction in the number of B cells expressing the nuclear protein EBNA2 after infection with a⌬BNRF1 virus compared to wild-type infection. Likewise,⌬BNRF1 viruses transformed primary B cells much less efficiently than EBV-wt or BNRF1trans-complemented viruses. We conclude from these findings that BNRF1 plays an important role in viral transport from the endosomes to the nucleus.
The herpesviruses form a large family of viruses that share a common architecture but are characterized by different cell tropisms, host ranges, and life cycles (26). All herpesviruses possess an envelope wrapped around the nucleocapsid that contains the double-stranded viral DNA. The virtual space between the nucleocapsid and the envelope, the tegument, contains several proteins of viral and cellular origin (e.g., actin, tubulin, and heat shock proteins) (11, 15). Viral tegument proteins have been found to have multiple functions such as gene transactivation, protein phosphorylation, suppression of host protein synthesis, virion morphogenesis, and viral DNA packaging. Most of the knowledge about this protein class comes from the study of herpes simplex virus (HSV), for which about 20 tegument proteins have been identified (for a review see reference 15). One group of proteins, whose most promi-nent representative is VP16, includes transactivators of viral immediate-early genes and host shutoff proteins that are in-volved in the initiation of a successful infection (4, 14). An-other group of tegument proteins is involved in organizing the architecture of the tegument by acting as a nucleation factor that allows incorporation of other tegument proteins in the matrix around the viral nucleocapsid (29, 30). This is best exemplified by the interactions of VP22 with VP16 (7) and VP16 with vhs (28). HSV tegument proteins also have been shown to be involved in viral transport within the infected cell
either during virus maturation or during the last phases of HSV infection (6, 15). For example, HSV tegument protein VP1/2 has been shown to play an important role during teth-ering of the nucleocapsid to the nuclear membrane and release of the viral DNA to the nucleus (2).
Much less is known about the Epstein-Barr virus (EBV) tegument proteins. Some positional homologues such as BOLF1, BBLF1, BGLF1, and BPLF1 have been identified, but no or only scanty information is available about their function (11, 15). Other EBV tegument proteins have no homologues in HSV, suggesting that the viruses have followed different evo-lution routes (11). This is particularly clear for the HSV key transactivator VP16, for which no EBV counterpart is known. BNRF1, also designated EBV major tegument protein, is rep-resentative of this group of orphan EBV tegument proteins. BNRF1 has been shown to be part of the infectious virus, but its function during viral infection is unknown (3, 11). Here we describe the phenotype of an EBV viral mutant devoid of the BNRF1 gene. We found that BNRF1 plays no obvious role in DNA replication or viral maturation but is important for effi-cient infection and transformation of primary B cells. BNRF1 was found to be required for viral transfer from the endosome/ lysosome compartment to the nucleus.
MATERIALS AND METHODS
Eukaryotic and prokaryotic cells.Raji is an EBV-positive Burkitt’s lymphoma cell line (24). B95.8 is an EBV-immortalized marmoset monkey lymphoblastoid cell line (LCL) (16). Peripheral blood mononuclear cells were isolated from fresh buffy coat by density gradient centrifugation, and CD19-positive B cells were isolated using M-450 CD19 (Pan B) Dynabeads (Dynal) followed by detachment of the B cells from Dynabeads using Detachabead (Dynal). All cells were grown
* Corresponding author. Mailing address: German Cancer Research Center, ATV-F100, Im Neuenheimer Feld 242, 69120 Heidelberg, Ger-many. Phone: 49/6221/424870. Fax: 49/6221/424852. E-mail: h.delecluse @dkfz.de.
† These two authors equally contributed to this work.
9435
on November 8, 2019 by guest
http://jvi.asm.org/
in RPMI 1640 medium supplemented with 10% fetal calf serum (FCS; Invitro-gen). LCLs and mini-LCLs were established as described previously (1) and maintained as suspension cultures in RPMI 1640 supplemented with 2 mM
L-glutamine, 1% nonessential amino acids, 1 mM sodium pyruvate, 50g/ml
gentamicin, 10% FCS. BJ5183 is arecA-positive,recBC-negative K-12
Esche-richia colistrain. DH10B is arecA-negativeE. coliK-12 strain that tolerates large plasmids.
Plasmids and BNRF1 targeting vector.The BNRF1 open reading frame was first PCR amplified and cloned into the pUC19 SmaI restriction site (p2406). In a second step, the internal BNRF1 BstEII-XhoI fragment from p2406 was exchanged against the SacI-HindIII fragment from pCP15 carrying the kanamy-cin gene. This targeting vector (p2407) introduced a 1.4-kb deletion into the
BNRF1 gene and a frameshift in the BNRF1 3⬘fragment. A BNRF1 expression
plasmid was constructed by inserting the 4.78-kb PmlI fragment encompassing
BNRF1 into the EcoRV site of pcDNA3.1(⫹). p2670 is a pRK5 expression
plasmid that carries the B95.8 BALF4 gene (BALF4 encodes the gp110 glyco-protein).
Recombinant EBV plasmid.p2089 is a plasmid comprising the EBV wild-type genome, the F-factor origin of replication, the chloramphenicol and the hygro-mycin resistance genes, and the gene encoding the green fluorescence protein
(GFP) (5). To generate a BNRF1-negative mutant, the recBCDE. colistrain
BJ5183 (9) was transformed with the recombinant EBV plasmid p2089. The BNRF1 targeting vector was cleaved with BamHI and EcoRI to generate a linearized fragment of 6,761 bp consisting of the modified BNRF1 gene flanked by EBV-specific sequences. The linearized plasmid was transformed into BJ5183 carrying p2089 to induce homologous recombination via EBV flanking regions.
Bacterial clones were selected in the presence of chloramphenicol (15g/ml)
and kanamycin (10g/ml). Plasmid DNA from antibiotic-resistant clones was
prepared and analyzed with different restriction enzymes to identify clones with the correct recombination pattern. Recombinant DNA from wild-type EBV (EBV-wt) was digested in parallel and provided an appropriate control. Plasmid
DNA from a properly recombined clone was then electroporated intorecA E. coli
strain DH10B (Invitrogen) for further propagation of the recombinant EBV plasmid. 293 cells were transfected with the recombined DNA using Lipo-fectamine (Invitrogen) as described previously (10). Selection of stable 293 cell clones carrying the EBV recombinant plasmid was performed using hygromycin
(100g/ml). Cell clones surviving selection were first checked for GFP
fluores-cence and successively expanded for further investigation. The cell clone that
delivered the highest viral titers is referred to as 293/⌬BNRF1 in this work. To
confirm the integrity of the viral genome in the 293/⌬BNRF1 cells, circular DNA
molecules were extracted using a denaturation-renaturation method as described previously (8).
Virus induction and infection of target cells.For induction of the EBV lytic
phase, 293/EBV-wt (which carries p2089) and 293/⌬BNRF1 cells were
trans-fected in six-well cluster plates with expression plasmids carrying the BZLF1 and
the BALF4 genes (0.5g/well) using lipid micelles (Lipofectamine; Invitrogen).
In some experiments, 1 microgram of the BNRF1 expression plasmid was added. Three days after transfection, virus supernatants were harvested, filtered through
a 0.8-m filter, and kept frozen at⫺74°C. Primary B cells were infected at a
multiplicity of infection (MOI) of 10 and seeded into U-bottom 96-well
micro-titer plates at a cell density of 104cells per well (two plates per supernatant). In
each well, gamma-irradiated human embryonic lung fibroblasts served as the feeder layer. To inhibit endosome/lysosome fusion, primary B cells were
pre-treated with chloroquine (ICN Biomedicals) at a final concentration of 150M
for 45 min on ice prior to addition of viral supernatant. After incubation for 50 min at 37°C cells were washed and fixed for electron microscopy.
Electron microscopy.Cells were washed three times in phosphate-buffered saline (PBS) and fixed with 2% glutaraldehyde in the same buffer for 20 min at 4°C. Samples were postfixed in 2% osmium tetroxide in cacodylate buffer for 1 h at 4°C, stained with 0.5% uranyl acetate for 16 h at 25°C, washed twice in distilled water, dehydrated in ethanol, and embedded in Epon 812. Thin sections were examined by using a Zeiss electron microscope.
Gardella gel electrophoresis and Southern blot analysis. Preparation of genomic DNA, Gardella electrophoresis, and Southern blot analysis were per-formed as previously described (10). Gardella gel electrophoresis followed by Southern blotting was used to detect either viral DNA in replicating cells or viruses in cell-free virus supernatants. Following electrophoresis the gel was
blotted onto a Hybond N⫹membrane (Amersham) and hybridized with a
radioactively labeled plasmid encompassing EBV-specific sequences.
EBV binding assay. To assess EBV binding to target cells, EBV-wt or
⌬BNRF1 virus-containing supernatant was incubated at a MOI of 10 viruses per
cell with purified B cells. After incubation for 3 h on ice, cells were washed three
times in PBS after which they were dried on glass slides for immunostaining. DNA extracted from infected samples was used for quantitative real-time PCR.
Immunostains.Cells were washed three times in PBS and fixed on glass slides for 20 min using pure acetone (for gp350 stain) or acetone-methanol (1:1, vol/vol) (for EBNA2 stain) at room temperature. Slides were incubated for 30 min with a purified mouse monoclonal antibody directed against EBV glyco-protein gp350/220 (ATCC 72A1 hybridoma) or EBNA2 (clone PE2). Slides were washed three times in PBS and incubated for 30 min with a secondary goat anti-mouse antibody conjugated with the Cy-3 fluorochrome (Dianova). After several washes in PBS, slides were embedded with 90% glycerol and immuno-fluorescence was evaluated by using a immuno-fluorescence microscope coupled to a charge-coupled device camera (Leica).
qPCR-mediated DNA amplification.Virus titers in supernatants from lytically induced cells or bound viruses on purified B cells were assessed by quantitative real-time PCR. Supernatants were first digested with DNase I (1 IU/ml super-natant) at 37°C for 1 hour. After DNase I heat inactivation (10 min at 70°C), supernatants were mixed (1:1, vol/vol) with lysis buffer (0.1 mg/ml proteinase K in water) and incubated for 60 min at 50°C, after which the enzyme was heat inactivated (75°C for 20 min). Water-diluted supernatants (1:10) or genomic DNA (75 ng) extracted from B cells after virus binding was subjected to quan-titative PCR (qPCR) using primers and a 6-carboxyfluorescein–6-carboxy tetra-methylrhodamine-labeled probe specific to the BALF5 gene as previously de-scribed (12). The human Burkitt’s lymphoma cell line Namalwa, which contains two EBV genome copies per cell, was used to calculate the standard curve.
Antiserum against BNRF1. The 3,217-bp Ecl136II-NruI BNRF1 fragment
from p2406 was cloned in the Ecl136II site of the pET21(⫹) vector (Novagen)
for expression of a His-tagged BNRF1 fusion protein. The plasmid was
trans-formed intoE. colistrain BL21(DE3), and protein extracts were obtained by
lysing the cells in 20 mM Tris-HCl, pH 7.9, 0.5 M NaCl, 10% glycerol, 1 mM phenylmethylsulfonyl fluoride, 5 mM imidazole. The BNRF1 fusion protein was purified from a 10% sodium dodecyl sulfate-polyacrylamide gel after elution in 4 M sodium acetate. One female chinchilla bastard rabbit was immunized
sub-cutaneously with 150g BNRF1 recombinant protein in the presence of
incom-plete Freund’s adjuvant followed by two subsequent boosts. The specificity of the polyclonal antiserum was assessed by Western blot analysis.
Western blot analysis.Cells were lysed in 50 mM Tris-HCl, pH 7.5, 150 mM NaCl, 1% NP-40, 0.5% sodium deoxycholate, 0.1% sodium dodecyl sulfate
(SDS). A virus pellet, obtained after ultracentrifugation (2 h at 30,000⫻g) of 5
ml virus supernatant, and 20g of proteins denatured in Laemmli buffer for 5
min at 95°C were separated on a 10% SDS-polyacrylamide gel and electroblotted onto a nitrocellulose membrane (Hybond ECL; Amersham). After preincuba-tion of the blot in 1% dry milk powder in PBS, the polyclonal serum against BNRF1 was applied at a 1:10,000 dilution for 1 hour at room temperature. After extensive washings in 0.1% Tween in PBS, the blot was incubated for 1 hour with protein A coupled with horseradish peroxidase. Bound antibody was revealed using the ECL detection reagent (Amersham).
T-cell antigen recognition assay.Mini-LCLs are primary B cells transformed by the mini-EBV, a recombinant plasmid that contains the EBV latent genes but not all lytic genes and therefore cannot replicate (13). Mini-LCLs were
estab-lished as described previously (18). Cells (1⫻105
/well) were incubated with serial dilutions of viral supernatant or purified recombinant proteins for 24 h; excess virus and, where added, inhibitors were removed by washing; and the cells were fixed by treatment with 1% paraformaldehyde for 5 min at room
temper-ature followed by extensive washing. T cells (1⫻105
) were then incubated with the B cells and placed in culture for 24 h. We used an enzyme-linked immu-nosorbent assay system (R&D Systems) to quantify T-cell cytokines released in the culture medium following interactions between B cells and T cells. The
CD4⫹T-cell clones specific for BLLF1 (clone 1D6), BNRF1 (clone 1H7), and
BALF4 (clone A9) have been isolated from an EBV-seropositive donor and cultivated as described previously (1). These T-cell clones are all HLA-DR B1*1301 restricted. To inhibit lysosomal processing, leupeptin (Sigma-Aldrich)
was added to the target cells at a final concentration of 200g/ml together with
the virus supernatant.
RESULTS
Construction of ⌬BNRF1 virus.The complete genome of the B95.8 strain of EBV cloned onto an F-factor replicon (p2089) was moved into arecA-positive,recBC-negativeE. coli strain (BJ5183) (5). This bacterial strain allows homologous recombination between targeting vectors and sequences present
on November 8, 2019 by guest
http://jvi.asm.org/
on the F plasmid to take place with high efficiency (5, 9). The targeting vector was constructed by deleting the central parts of the BNRF1 open reading frame and performing insertional mutagenesis with the aid of the kanamycin resistance gene. The BNRF1 mutant resulted from homologous recombination between the linearized targeting vector and the wild-type EBV genome within BJ5183. Properly recombined clones were sub-jected to double selection with chloramphenicol and kanamy-cin and analyzed with several restriction enzymes to confirm the successful disruption of the target gene. Restriction anal-ysis using the BamHI enzyme was performed to allow distinc-tion between the wild type and BNRF1 (Fig. 1A contains a partial restriction map). As expected, this analysis showed that the 10.7-kb and 9.2-kb fragments that carry the BNRF1 gene in the wild-type EBV genome are fused together to produce a 19-kb single fragment in the mutant (Fig. 1B).
The⌬BNRF1 mutant was stably transfected into 293 cells that were previously shown to be permissive for EBV replica-tion (5). Fifteen hygromycin-resistant GFP-positive clones car-rying the recombinant EBV genome were expanded for further analysis. All clones were found to be permissive for lytic DNA replication (data not shown), and we chose the cell clone that delivered the highest viral titers (here referred to as 293/ ⌬BNRF1). We then confirmed the structural integrity of the virus present in 293/⌬BNRF1 by transforming this plasmid back into E. coli DH10B cells. Restriction enzyme analysis confirmed that the 293/⌬BNRF1 cells carry a recombinant genome with an intact structure (Fig. 1B). We then confirmed that the⌬BNRF1 genome lacks a functional BNRF1 gene by performing a Western blot assay both on induced 293/⌬BNRF1 cells and on free viruses using a BNRF1-specific polyclonal
antiserum (Fig. 1C). The BNRF1 protein could be detected neither in 293/⌬BNRF1 cells nor in mature⌬BNRF1 virions. In contrast, 293/EBV-wt cells and 293/⌬BNRF1 cells comple-mented intranswith a BNRF1 expression plasmid clearly ex-pressed the protein. Expression of the BNRF1 gene in lytically induced 293/⌬BNRF1 cells therefore led to the incorporation of its protein product in mature virions to levels found in wild-type EBV particles. These results showed that the 293/ ⌬BNRF1 cells represent an appropriate genetic system to as-sess the function of the BNRF1 protein.
The BNRF1 protein has no influence on lytic DNA replica-tion.The EBV lytic cycle leads to the production of viruses and requires both viral DNA replication and structural protein synthesis. These events were analyzed in induced 293 cells carrying wild-type or⌬BNRF1 EBV genomes. Previous anal-ysis of several 293/EBV-wt cell clones has shown that the permissivity for EBV lytic replication markedly varies between them. 293/EBV-wt clones produce between 106and 108viral
DNA equivalents per ml, with an average of 107viral DNA
equivalents per ml (data not shown), a value also observed for B95.8. These results probably reflect the percentage of cells induced in a given clone. Evaluation of late gene expression by immunostaining of fixed, lytically induced 293/EBV-wt showed that between 5% and 20% of cells produce the late protein gp350 and that the high producers are found in cell clones that contain a high proportion of gp350-positive cells (data not shown).
[image:3.585.136.449.70.269.2]We first used qPCR to determine viral titers in supernatants from induced cells. Supernatants from both B95.8 and 293/ EBV-wt were used as controls in this analysis. We used a highly permissive 293/EBV-wt cell clone that is representative of FIG. 1. Construction of a⌬BNRF1 recombinant virus. (A) Schematic representation of the EBV restriction map depicting the genome region encompassing the BNRF1 gene in its wild-type and mutated configurations. Insertion of the BNRF1 targeting vector leads to the replacement of 9.2-kb and 10.7-kb BamHI fragments by a 19-kb fragment. The locations of the BamHI restriction sites (B) are indicated. (B) Restriction analysis of wild-type and mutant EBV recombinant genomes. Recombinant⌬BNRF1 genomes cloned inE. colior rescued from 293/⌬BNRF1 cells inE. coliwere cut with BamHI and separated on an agarose gel. EBV-wt genomes cloned inE. coliwere used as a control. The results of this analysis conformed to the predictions (see panel A). (C) Western blot analysis using a BNRF1-specific antiserum. Extracts from lytically induced 293/EBV-wt and complemented or noncomplemented 293/⌬BNRF1 cells or from their respective viral supernatants were separated on a polyacrylamide gel electrophoresis gel and blotted with a polyclonal antiserum against BNRF1. The producer cell lines and viruses from 293/EBV-wt ortrans-complemented 293/⌬BNRF1 express BNRF1 at comparable levels. As expected, 293/⌬BNRF1 cells and their viruses do not produce the BNRF1 protein.
on November 8, 2019 by guest
http://jvi.asm.org/
high-producer wild-type cell clones to assess replication in 293/ ⌬BNRF1. qPCR analysis showed that viral supernatants from induced 293/⌬BNRF1 andtrans-complemented 293/⌬BNRF1 both contain approximately 107 DNA equivalents per ml,
whereas the B95.8 and 293/EBV-wt cell clones used as positive controls produce approximately 107and 108DNA equivalents
per ml, respectively. This analysis therefore suggests that the
293/⌬BNRF1 clone has an average permissivity for viral rep-lication and that BNRF1 does not interfere with DNA lytic replication. The ability of⌬BNRF1 virus to support lytic rep-lication was further assessed by evaluating linear DNA repli-cation in 293/⌬BNRF1 by Gardella gel electrophoresis in the absence or presence of BNRF1 (Fig. 2A). As expected from results of the qPCR analysis, induced 293/⌬BNRF1 cells were FIG. 2. BNRF1 is not required during EBV lytic replication. (A) Gardella gel analysis was applied to lytically induced producer cells as well as to free viruses from these cell lines. Similar amounts of linear EBV molecules are visible in induced B95.8 and 293/⌬BNRF1 cells with or without
trans-complementation. Induced 293/EBV-wt cells are used as positive controls for high-producer cells (108viruses/ml). C, circular DNA; L, linear
DNA;*, cross-hybridization with BNRF1 expression plasmid. (B) Lytically induced producer cell lines carrying EBV-wt or⌬BNRF1 viruses were stained with an antibody specific to gp350. Three days after infection, the same number of gp350-positive cells were visible in induced 293/⌬BNRF1 cells and in BNRF1trans-complemented 293/⌬BNRF1 cells. (C) Electron microscopy was used to analyze virus production. The⌬BNRF1 mutants do not show obvious morphological abnormalities. Both insets show viruses with an electron-dense core just after cell egress. Similar numbers of viruses are readily visible in both 293/EBV-wt and 293/⌬BNRF1 cells (arrows). Cy, cytoplasm; Nu, nucleus.
on November 8, 2019 by guest
http://jvi.asm.org/
found to contain as many linear viral copies as B95.8 but less linear DNA than their wild-type counterparts in proportions that reflect the differences in viral titers. Complementation with BNRF1 had no influence on linear DNA replication in induced 293/⌬BNRF1 cells. We conclude from these data that BNRF1 plays no substantial role in lytic DNA replication.
We then studied late gene expression by evaluating the pro-portion of induced cells using a gp350-specific immunostain. We found that roughly 10% of induced 293/⌬BNRF1 cells express gp350, a result found in average 293/EBV-wt clones (Fig. 2B). In addition, complementation of 293/⌬BNRF1 cells with BNRF1 did not modify the proportion of cells undergoing replication upon induction. There is therefore no evidence to suggest that 293/⌬BNRF1 cells are less permissive to induction than their wild-type counterparts. We finally used electron microscopy to analyze lytic replication at the single-cell level. Similar numbers of virions were visible in both 293/⌬BNRF1 and 293/EBV-wt cells (Fig. 2C). Virions within the producer cell and virions shortly after egress did not show any major morphological variations between⌬BNRF1 viruses and their wild-type counterparts (Fig. 2C and inset). Altogether these results suggest that BNRF1 is not required for production of EBV particles.
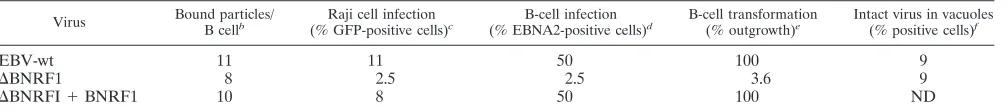
Analysis of the ⌬BNRF1 infection phenotype in cell lines and primary B cells.Next we evaluated the ability of⌬BNRF1 viruses to infect various EBV target cells. The central experi-ment here was represented by the infection of purified primary B cells, which are the main target of EBV infection in vivo. The results of the B-cell infection experiments with mutant and wild-type supernatants at a MOI of 10 viruses per cell are summarized in Table 1. Approximately 50% of primary B cells infected with wild-type viruses showed nuclear expression of EBV nuclear antigen 2 (EBNA2) 3 days after infection (Fig. 3A). The infection rate, however, dropped to 2.5% in B cells infected with⌬BNRF1 viruses but could be restored bytrans -complementation with BNRF1 (Fig. 3A). Similarly, the pro-portion of B cells expressing GFP was higher after infection with wild-type viruses than after infection with the mutant (data not shown). This reduced infection rate clearly translated into the ability of viruses to immortalize B cells. Whereas cell outgrowth was observed in 192 of 192 wells containing 104B
cells infected at a MOI of 10 with both wild-type andtrans -complemented⌬BNRF1 mutants, only 7 of 192 (3.6%) of the wells infected with ⌬BNRF1 contained immortalized B-cell clones (Table 1). Southern blot analysis with a probe specific to the BNRF1 gene confirmed that the immortalized B-cell lines carry the mutant virus with a rearranged BNRF1 locus (Fig.
3B). This set of experiments therefore provided definite evi-dence that BNRF1 is important for primary-B-cell infection.
We then extended our infection experiments to the Raji B-cell line. Infection of cell lines is less informative than in-fection of primary cells, but these experiments can be valuable in the present context as it has been suggested that EBV infection of primary B cells and Raji cells follows different pathways (17, 20, 27). Infection of Raji cells at a MOI of 10 showed that⌬BNRF1 viruses have a reduced ability to infect these cells (2.5% GFP-positive cells) (Table 1).trans -comple-mentation of the ⌬BNRF1 mutant brought back infection efficiency to levels similar to those seen with wild-type viruses (8% versus 11% GFP-positive cells, respectively). BNRF1 therefore plays a role during Raji infection, but the reduction in infection efficiency in Raji cells is much less pronounced than in B cells (3.2-fold versus 20-fold reduction compared to wild-type virus).
[image:5.585.44.548.81.137.2]BNRF1 knockout viruses are imported into cellular vesicles but are impaired in their ability to reach the nucleus.From our previous experiments it was clear that BNRF1 is required for efficient infection. We therefore set out to determine which of the infection steps were affected by the BNRF1 deletion. Successful viral infection requires binding and fusion to the cell membrane, transfer to the nucleus, and expression of the viral genome in the target cell’s nucleus. We therefore assessed the ability of⌬BNRF1 viruses to perform these functions. In a first step, we performed a binding assay using primary B cells as a target. Immunostaining of viruses bound to the cell surface showed no major difference between wild type and mutants (Fig. 3C). However, this method does not allow any precise quantitative evaluation, and therefore we estimated the aver-age number of viruses bound per cell by quantitative PCR of DNA extracted from viruses bound to the B cells. This analysis showed that⌬BNRF1 viruses bind nearly equally well to pri-mary B cells as their complemented or wild-type counterparts (Table 1). Because this moderately decreased ability to bind to target cells cannot make up for the 20-fold reduction in trans-formation efficiency, we analyzed virus entry using electron microscopy. This analysis showed the presence of viral parti-cles in cytoplasmic cellular vesiparti-cles in both B cells infected with either⌬BNRF1 or wild-type viruses (Fig. 4). We then repeated this experiment in the presence of chloroquine, a weak base previously shown to inhibit de-envelopment and egress of EBV particles into the cytoplasm (20). This treatment leads to an accumulation of virions in cellular vesicles thereby allowing easy quantitation of the number of viruses present in these structures. Analysis of 100 cells infected either with⌬BNRF1 TABLE 1. Analysis of BNRF1 mutant infection phenotypea
Virus Bound particles/
B cellb
Raji cell infection
(% GFP-positive cells)c
B-cell infection
(% EBNA2-positive cells)d
B-cell transformation
(% outgrowth)e
Intact virus in vacuoles
(% positive cells)f
EBV-wt 11 11 50 100 9
⌬BNRF1 8 2.5 2.5 3.6 9
⌬BNRFI⫹BNRF1 10 8 50 100 ND
a
All experiments were performed at a MOI of 10 virus particles per cell, and mean values obtained from three independent experiments are given.
b
Resting B cells were incubated for 3 h on ice with virus supernatant, and the number of bound particles was determined by real-time PCR.
c
GFP expression was scored 3 days after Raji cell infection.
d
Primary B cells were stained for EBNA2 expression 3 days postinfection.
e
Outgrowth of LCL clones was visually scored 4 weeks after infection.
f
Electron microscopy data were from 100 randomly selected chloroquine-treated cells. ND, not determined.
on November 8, 2019 by guest
http://jvi.asm.org/
or wild-type viruses showed no difference in the proportion of viral particles found in cellular vesicles (Table 1). ⌬BNRF1 viruses are therefore able to enter target cells, suggesting that BNRF1 does not play a major role during internalization.
[image:6.585.135.449.70.561.2]T cells specific for EBV lytic proteins recognize B cells infected by a⌬BNRF1 virus.EBV-infected B cells efficiently present virion protein components to T cells (25). Following virus uncoating, structural proteins of the viral envelope are FIG. 3.⌬BNRF1 viruses show a reduced ability to infect B cells. (A) Primary B cells were infected with EBV-wt or⌬BNRF1 mutant virus at a MOI of 10 and stained for EBNA2 expression 3 days after infection. One-half of cells infected with wild-type EBV stained positive for EBNA2. In contrast, only 2.5% EBNA2-positive cells were detected after infection with⌬BNRF1.trans-complementation of 293/⌬BNRF1 with a BNRF1 expression plasmid restored the full infection ability. (B) Southern blot analysis of LCLs obtained by infection of primary B cells with wild-type EBV,⌬BNRF1, ortrans-complemented⌬BNRF1 virus. Genomic DNA was cut with EcoRI and separated by agarose gel electrophoresis. Hybridization with a BNRF1-specific probe detected a 7.4-kb BNRF1 signal corresponding to the mutated BNRF1 gene in both 293/⌬BNRF1 LCLs and their complemented counterparts. As expected, LCLs infected with EBV-wt carry an intact BNRF1 gene. (C) A binding assay was used to evaluate the ability of the⌬BNRF1 mutant to bind to resting B cells. Cells were incubated with supernatants containing mutant or wild-type viruses at a MOI of 10. The panel shows an immunostain with an antibody specific to gp350. Bound viruses are seen as red dots at the surface of the cell.
on November 8, 2019 by guest
http://jvi.asm.org/
degraded in the endosomal/lysosomal compartment and peptides derived from structural proteins of EBV are effi-ciently presented on major histocompatibility complex (MHC) class II molecules for recognition by CD4⫹T helper (Th) cells (1). The cells release soluble gamma interferon upon activa-tion, which can be detected and quantified in supernatants. Detection of a Th-cell response against an EBV-infected B cell therefore means that the virus has at least reached the endo-some/lysosome compartment. In addition, the immune re-sponse is proportional to the amount of antigen being pre-sented. It therefore allows quantitative evaluation of the infection process.
We analyzed the ability of B cells infected by ⌬BNRF1 viruses to present BALF4-, BLLF1-, and BNRF1-specific an-tigens. To this aim, limiting amounts of viral supernatants were pulsed onto mini-LCLs and antigen presentation by MHC class II molecules was monitored with CD4⫹T-cell clones specific for peptides derived from the BLLF1, BALF4, and BNRF1 proteins. Mini-LCLs were obtained by transformation of pri-mary blood B cells with mini-EBV plasmids that lack most EBV viral lytic genes and therefore do not interfere with their recognition (13). As shown in Fig. 5A, mini-LCLs pulsed with EBV-wt,⌬BNRF1, or BNRF1trans-complemented⌬BNRF1 viruses were recognized to the same extent by all CD4⫹T-cell clones, with the exception of the mini-LCL pulsed with ⌬BNRF1, which, as expected, was not recognized by the BNRF1-specific T cells. We confirmed the specificity of the observed immune reaction by showing that mini-LCLs are able to present purified BALF4, BNRF1, and BLLF1 proteins (data not shown).
To confirm that antigen presentation required internaliza-tion of the viral particles and processing of virion proteins in the lysosomal compartment, mini-LCLs were pulsed with EBV-wt and⌬BNRF1 viruses in the absence or presence of leupeptin, an inhibitor of lysosomal proteases, and subse-quently probed with the T cells. In both cases, leupeptin strongly reduced antigen presentation, demonstrating that EBV-wt and⌬BNRF1 viral particles efficiently target the en-dosome/lysosome compartment (Fig. 5B).
These results confirm that the⌬BNRF1 viruses lack BNRF1 but also show that both EBV-wt and the ⌬BNRF1 mutant reach the endosome with similar efficiencies. Antigen process-ing from both EBV-wt and⌬BNRF1 viruses can then further
proceed after fusion of the endosome with the lysosomal com-partment.
DISCUSSION
EBV and HSV are two members of the same virus family, but they classically access the nuclear compartment of their target cells by following different routes. HSV accesses the nucleus by crossing through the cytoplasm, whereas EBV first enters the endosomal compartment by receptor-mediated en-docytosis, from which it is transported to the nucleus (19, 20). The apparent mutual exclusion suffers, however, many excep-tions. Indeed, earlier work suggested that infection of the Raji Burkitt’s lymphoma B-cell line takes place in a mainly vesicle-independent manner (27). It has been argued that abnormal-ities in the cytoskeletons of malignant cells might be respon-sible for the discrepancy. Whether this reflects adaptation to in vitro growth or an intrinsic property of malignant cells remains to be determined. The EBV infection pathway could therefore be influenced by differentiation or growth. It has also been shown that EBV infects epithelial foreskin cells using a non-endocytic mechanism (17). Here again it remains to be deter-mined whether such a mechanism is representative of a phys-iological infection pathway, as foreskin cells are unlikely to be in vivo targets for EBV infection. Interestingly, recent reports also showed that HSV1 can use the endosome to reach the nuclei of HeLa cells, human epidermal keratinocytes, and CHO cells expressing gD receptors (21–23).
[image:7.585.135.450.68.183.2]We have used a genetic system to gather information on BNRF1’s function during EBV cell infection. As expected, the ⌬BNRF1 virus lacked BNRF1, but transfection of a BNRF1 expression plasmid in a 293/⌬BNRF1 producer cell line led to the reappearance of the BNRF1 protein within the mature virus as assessed by Western blot analysis. This complemented virus was indistinguishable from EBV wild-type virus, thereby demonstrating that the alterations introduced in ⌬BNRF1 were limited to the BNRF1 gene. Assessment of lytic DNA replication by Gardella gel analysis of both producing cells and newly formed virions showed no difference between the ⌬BNRF1 virus and cellular clones carrying EBV-wt.⌬BNRF1 titers were similar to the ones observed in average permis-sive wild-type producer cell lines. We could readily identify ⌬BNRF1 viruses by examining induced 293/⌬BNRF1 cells FIG. 4.⌬BNRF1 and EBV-wt viruses are visible in vesicles of infected primary B cells. Electron microscopy was used to follow EBV infection in the endosomal compartment of primary B cells. B cells were infected for 2 h at 4°C to allow binding, followed by a 30-min incubation at 37°C to allow virus entry. The picture shows two examples of⌬BNRF1 viruses located in primary B-cell vesicles. EBV-wt served as a positive control.
on November 8, 2019 by guest
http://jvi.asm.org/
with an electron microscope. The viruses did not show major structural alterations, confirming that BNRF1 is not required for virus production. Importantly, trans-complementation of ⌬BNRF1 did not influence lytic replication. We therefore con-clude that, in our experimental settings, BNRF1 plays no role during lytic DNA replication.
A completely different picture emerged from the various experiments we performed to characterize viral infection. ⌬BNRF1 viruses were found to have a 20-fold-reduced ability to infect and transform primary B cells. We therefore analyzed the different steps that lead to infection. Complemented and noncomplemented⌬BNRF1 viruses bound to B cells nearly equally well. We did not find evidence for an altered morphol-ogy of the⌬BNRF1 viruses by electron microscopy, but this does not exclude the possibility that the protein plays a role in the internal architecture of the viruses. Using electron micros-copy, we could identify incoming⌬BNRF1 viruses within ves-icles of infected cells, and we found no difference in the pro-portion of cells containing viral particles compared to EBV-wt infection. Furthermore, we assessed the ability of⌬ BNRF1-infected B cells to induce a T helper cell reaction. This method allows a more quantitative approach because the strength of the immune reaction, as determined by measuring the concen-tration of gamma interferon in the supernatant, is proportional to the amount of antigen presented by B cells. These assays showed that B cells infected with⌬BNRF1, EBV-wt, ortrans -complemented⌬BNRF1 viruses present the gp350 (BLLF1) and gp110 (BALF4) structural proteins with the same
effi-ciency. As expected, B cells infected with⌬BNRF1 virus did not present the BNRF1 protein. We conclude that BNRF1 is not required for viral transport from the cellular membrane to the endosome/lysosome compartment but plays a role at a later stage during infection.
Infection of Raji cells with ⌬BNRF1 and trans -comple-mented viruses showed that the mutant is less infectious than the wild-type virus. Several explanations could be offered for this result. If Raji infection takes place exclusively along an endosome-independent pathway, then these results show that BNRF1 is important for both the endocytic and nonendocytic entry pathway and is therefore likely to act during a step common to both mechanisms. This step would then very likely be the docking of the viral capsid to the nucleus. This would imply that BNRF1 remains associated with the capsid during transport toward the nucleus. Such a role has been attributed to the HSV tegument protein VP1/2 (2). This hypothesis would predict that the reduction in infection efficiency observed in ⌬BNRF1 should be similar both in Raji and B cells. Our results suggest, however, that this does not hold true. Also, if BNRF1 was important for nuclear import, one would expect to see accumulation of capsids at the nuclear envelope. However, using electron microscopy we could not detect any viral capsids around the nuclei of⌬BNRF1-infected B cells.
Another scenario is that Raji cells can be infected both in endocytic and nonendocytic pathways. Previous results showed that the virus mostly enters the cell by directly fusing with the cell membrane but could not exclude the possibility that infec-FIG. 5.⌬BNRF1-infected B cells efficiently present late viral antigens on MHC class II molecules. (A) Mini-LCL cells were incubated with increasing amounts of wild-type,⌬BNRF1, and BNRF1trans-complemented⌬BNRF1 viral supernatants for 24 h, after which the cells were fixed with paraformal-dehyde and used as targets for the BNRF1-, BLLF1-, and BALF4-specific T cells. Gamma interferon (IFN-␥) concentration in the supernatant of T cells was measured 24 h later using an enzyme-linked immunosorbent assay-based method. The different graphs represent IFN-␥concentrations measured in response to incubation of the B cells with increasing amounts of virus super-natant. The immune response against EBV BLLF1 and BALF4 induced by ⌬BNRF1 viruses is indistinguishable from those observed withtrans -comple-mented⌬BNRF1 or EBV-wt viruses (i to iii). As expected, only B cells infected withtrans-complemented⌬BNRF1 or EBV-wt viruses efficiently present BNRF1 (iii). (B) Lysosomal protein processing is essential for effi-cient antigen presentation. Mini-LCLs were incubated with EBV-wt ortrans -complemented or non-complemented⌬BNRF1 virus-containing supernatant (1l/well) in the presence or absence of leupeptin for 24 h. Following fixation with paraformaldehyde, the B cells were incubated with T cells specific for BALF4. Noninfected mini-LCLs were used as a negative control. B cells treated with leupeptin showed a markedly decreased ability to present antigen compared to their nontreated counterparts. This shows that⌬BNRF1 viruses reach the endosome/lysosome compartment.
on November 8, 2019 by guest
http://jvi.asm.org/
[image:8.585.50.267.71.361.2]tion never occurs through the endosome (20, 27). Therefore the possibility that EBV can utilize more than one route of entry during Raji infection cannot be excluded, though the direct-infection pathway might be predominant. This hypoth-esis would fit with our data and suggests that BNRF1’s main function is specific of the endocytic infection process. If par-allels can be established between HSV and EBV, BNRF1 would then be involved during de-envelopment or exclusion of the capsid from the endosome/lysosome compartment. Bio-chemical analysis of the interactions between BNRF1 and the B-cell organelles is now required to further elucidate BNRF1’s precise functions.
ACKNOWLEDGMENTS
This work was supported by Cancer Research UK and the Leukemia Research Fund.
REFERENCES
1.Adhikary, D., U. Behrends, A. Moosmann, K. Witter, G. W. Bornkamm, and J. Mautner.2006. Control of Epstein-Barr virus infection in vitro by T helper
cells specific for virion glycoproteins. J. Exp. Med.203:995–1006.
2.Batterson, W., D. Furlong, and B. Roizman.1983. Molecular genetics of herpes simplex virus. VIII. Further characterization of a temperature-sensi-tive mutant defectemperature-sensi-tive in release of viral DNA and in other stages of the viral
reproductive cycle. J. Virol.45:397–407.
3.Cameron, K. R., T. Stamminger, M. Craxton, W. Bodemer, R. W. Honess, and B. Fleckenstein.1987. The 160,000-Mrvirion protein encoded at the
right end of the herpesvirus saimiri genome is homologous to the 140,000-Mr
membrane antigen encoded at the left end of the Epstein-Barr virus genome.
J. Virol.61:2063–2070.
4.Campbell, M. E., J. W. Palfreyman, and C. M. Preston.1984. Identification of herpes simplex virus DNA sequences which encode a trans-acting polypeptide responsible for stimulation of immediate early transcription. J.
Mol. Biol.180:1–19.
5.Delecluse, H. J., T. Hilsendegen, D. Pich, R. Zeidler, and W. Hammer-schmidt.1998. Propagation and recovery of intact, infectious Epstein-Barr
virus from prokaryotic to human cells. Proc. Natl. Acad. Sci. USA95:8245–
8250.
6.Desai, P. J.2000. A null mutation in the UL36 gene of herpes simplex virus type 1 results in accumulation of unenveloped DNA-filled capsids in the
cytoplasm of infected cells. J. Virol.74:11608–11618.
7.Elliott, G., G. Mouzakitis, and P. O’Hare. 1995. VP16 interacts via its activation domain with VP22, a tegument protein of herpes simplex virus, and is relocated to a novel macromolecular assembly in coexpressing cells.
J. Virol.69:7932–7941.
8.Griffin, B. E., E. Bjorck, G. Bjursell, and T. Lindahl.1981. Sequence com-plexity of circular Epstein-Bar virus DNA in transformed cells. J. Virol.
40:11–19.
9.Hanahan, D.1985. Techniques for transformation ofE. coli, p. 109–135.In
D. Glover (ed.), DNA cloning. A practical approach, vol. 1. IRL Press, Oxford, United Kingdom.
10.Janz, A., M. Oezel, C. Kurzeder, J. Mautner, D. Pich, M. Kost, W. Ham-merschmidt, and H. J. Delecluse.2000. Infectious Epstein-Barr virus lacking
major glycoprotein BLLF1 (gp350/220) demonstrates the existence of
addi-tional viral ligands. J. Virol.74:10142–10152.
11.Johannsen, E., M. Luftig, M. R. Chase, S. Weicksel, E. Cahir-McFarland, D. Illanes, D. Sarracino, and E. Kieff.2004. Proteins of purified Epstein-Barr
virus. Proc. Natl. Acad. Sci. USA101:16286–16291.
12.Junying, J., K. Herrmann, G. Davies, D. Lissauer, A. Bell, J. Timms, G. M. Reynolds, S. G. Hubscher, L. S. Young, G. Niedobitek, and P. G. Murray.
2003. Absence of Epstein-Barr virus DNA in the tumor cells of European
hepatocellular carcinoma. Virology306:236–243.
13.Kempkes, B., D. Pich, R. Zeidler, B. Sugden, and W. Hammerschmidt.1995. Immortalization of human B lymphocytes by a plasmid containing 71
kilo-base pairs of Epstein-Barr virus DNA. J. Virol.69:231–238.
14.Kwong, A. D., J. A. Kruper, and N. Frenkel.1988. Herpes simplex virus
virion host shutoff function. J. Virol.62:912–921.
15.Mettenleiter, T. C.2004. Budding events in herpesvirus morphogenesis.
Virus Res.106:167–180.
16.Miller, G., T. Shope, H. Lisco, D. Stitt, and M. Lipman.1972. Epstein-Barr virus: transformation, cytopathic changes, and viral antigens in squirrel
mon-key and marmoset leukocytes. Proc. Natl. Acad. Sci. USA69:383–387.
17.Miller, N., and L. M. Hutt-Fletcher.1992. Epstein-Barr virus enters B cells
and epithelial cells by different routes. J. Virol.66:3409–3414.
18.Moosmann, A., N. Khan, M. Cobbold, C. Zentz, H. J. Delecluse, G. Hollweck, A. D. Hislop, N. W. Blake, D. Croom-Carter, B. Wollenberg, P. A. Moss, R. Zeidler, A. B. Rickinson, and W. Hammerschmidt.2002. B cells immortal-ized by a mini-Epstein-Barr virus encoding a foreign antigen efficiently
re-activate specific cytotoxic T cells. Blood100:1755–1764.
19.Morgan, C., H. M. Rose, and B. Mednis.1968. Electron microscopy of
herpes simplex virus. I. Entry. J. Virol.2:507–516.
20.Nemerow, G. R., and N. R. Cooper.1984. Early events in the infection of human B lymphocytes by Epstein-Barr virus: the internalization process.
Virology132:186–198.
21.Nicola, A. V., J. Hou, E. O. Major, and S. E. Straus.2005. Herpes simplex virus type 1 enters human epidermal keratinocytes, but not neurons, via a
pH-dependent endocytic pathway. J. Virol.79:7609–7616.
22.Nicola, A. V., A. M. McEvoy, and S. E. Straus.2003. Roles for endocytosis and low pH in herpes simplex virus entry into HeLa and Chinese hamster
ovary cells. J. Virol.77:5324–5332.
23.Nicola, A. V., and S. E. Straus.2004. Cellular and viral requirements for
rapid endocytic entry of herpes simplex virus. J. Virol.78:7508–7517.
24.Pulvertaft, R. J. V.1964. Cytology of Burkitt’s lymphoma (African
lym-phoma). Lanceti:238–240.
25.Rickinson, A. B., and E. Kieff.2001. Epstein-Barr virus, p. 2575–2627.In
D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed., vol. 2. Lippincott Williams & Wilkins, Philadelphia, Pa.
26.Roizman, B., and P. E. Pellett.2001. The familyHerpesviridae: a brief
intro-duction, p. 2381–2397.InD. M. Knipe, P. M. Howley, D. E. Griffin, R. A.
Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed., vol. 2. Lippincott Williams & Wilkins, Philadelphia, Pa.
27.Seigneurin, J. M., M. Vuillaume, G. Lenoir, and G. De-The.1977. Replica-tion of Epstein-Barr virus: ultrastructural and immunofluorescent studies of
P3HR1-superinfected Raji cells. J. Virol.24:836–845.
28.Smibert, C. A., B. Popova, P. Xiao, J. P. Capone, and J. R. Smiley.1994. Herpes simplex virus VP16 forms a complex with the virion host shutoff
protein vhs. J. Virol.68:2339–2346.
29.Vittone, V., E. Diefenbach, D. Triffett, M. W. Douglas, A. L. Cunningham, and R. J. Diefenbach.2005. Determination of interactions between tegument
proteins of herpes simplex virus type 1. J. Virol.79:9566–9571.
30.Zhu, Q., and R. J. Courtney.1994. Chemical cross-linking of virion envelope
and tegument proteins of herpes simplex virus type 1. Virology204:590–599.