Reduced Susceptibility to VIRIP-Based HIV-1 Entry Inhibitors
Has a High Genetic Barrier and Severe Fitness Costs
Janis A. Müller,aAnna Glöckle,aAli Gawanbacht,aMatthias Geyer,bJan Münch,aFrank Kirchhoffa
aInstitute of Molecular Virology, Ulm University Medical Center, Ulm, Germany
bInstitute of Structural Biology, University of Bonn, Bonn, Germany
ABSTRACT VIRIP has been identified as natural HIV-1 inhibitor targeting the gp41 fusion peptide. An optimized analogue (VIR-576) was effective in a phase I/II clinical trial and initial studies showed that HIV-1 resistance to VIRIP-based inhibitors has a high genetic barrier. Partially resistant CXCR4 (X4)-tropic HIV-1 NL4-3 variants could be obtained, however, after more than 15 months of passaging in MT-4 cells in the presence of another derivative (VIR-353). Sequence analyses identified the accumula-tion of seven mutaaccumula-tions across the HIV-1 envelope glycoprotein but outside the gp41 fusion peptide. The authors suggested that the three initial alterations con-ferred resistance, while subsequent changes restored viral fitness. Here, we intro-duced these mutations individually and in combination into X4- and CCR5 (R5)-tropic HIV-1 constructs and determined their impact on VIR-353 and VIR-576 susceptibility, viral infectivity, replication fitness, and fusogenicity. We found that es-sentially all seven mutations contribute to reduced susceptibility to VIRIP-based in-hibitors. HIV-1 constructs containing ⱖ4 changes were substantially more resistant to both VIRIP-based inhibitors and the VRC34.01 antibody targeting the fusion pep-tide. However, they were also much less infectious and fusogenic than those harbor-ing only the three initial alterations. Furthermore, the additional changes attenuated rather than rescued HIV-1 replication in primary human cells. Thus, the genetic bar-rier to HIV-1 resistance against VIRIP-based inhibitors is higher than previously sug-gested, and mutations reducing viral susceptibility come at a severe fitness cost that was not rescued during long-term cell culture passage.
IMPORTANCE Many viral pathogens are critically dependent on fusion peptides (FPs) that are inserted into the cellular membrane for infection. Initially, it was thought that FPs cannot be targeted for therapy because they are hardly accessible. However, an optimized derivative (VIR-576) of an endogenous fragment of ␣ 1-antitrypsin, named VIRIP, targeting the gp41 FP reduced viral loads in HIV-1-infected individuals. Characterization of HIV-1 variants selected during long-term cell-culture passage in the presence of a VIRIP derivative suggested that just three mutations in the HIV-1 Env protein might be sufficient for VIRIP resistance and that four subse-quent changes restored viral fitness. Here, we show that all seven mutations contrib-ute to reduced viral susceptibility to VIRIP-based inhibitors and demonstrate that the additional changes strongly impair rather than rescue HIV-1 infectivity, fusogenicity, and replication fitness. High genetic barrier to resistance and severe fitness cost sup-port further clinical development of this class of antiviral agents.
KEYWORDS HIV-1, VIRIP, antiretroviral resistance, fusion inhibitor, gp41 fusion peptide, viral envelope
M
ost viral pathogens contain an lipid bilayer envelope derived from the host cell and infect their target cells by direct fusion at the cell surface (e.g., HIV) or by receptor-mediated endocytosis and subsequent fusion within intracellular vesicles (e.g.,Received27 April 2018Accepted14 June 2018
Accepted manuscript posted online20 June 2018
CitationMüller JA, Glöckle A, Gawanbacht A, Geyer M, Münch J, Kirchhoff F. 2018. Reduced susceptibility to VIRIP-based HIV-1 entry inhibitors has a high genetic barrier and severe fitness costs. J Virol 92:e00733-18.https://doi .org/10.1128/JVI.00733-18.
EditorGuido Silvestri, Emory University
Copyright© 2018 American Society for Microbiology.All Rights Reserved. Address correspondence to Jan Münch, jan.muench@uni-ulm.de, or Frank Kirchhoff, frank.kirchhoff@uni-ulm.de.
VIRUS-CELL INTERACTIONS
crossm
on November 6, 2019 by guest
http://jvi.asm.org/
influenza virus) in a pH-dependent or -independent manner (1, 2). Fusion is mediated by viral glycoproteins (also referred to as “fusion proteins”) that are embedded into the viral envelope and almost invariantly depend on the insertion of highly hydrophobic viral fusion peptides (FPs) into the host cell membrane (3). Most enveloped viruses encode type I fusion proteins, such as HIV-1 gp41 or influenza virus hemagglutinin (4). These molecules are typically trimeric and mediate membrane fusion by forming a six-helix bundle that pulls the viral and cellular membranes together (5). This process is preceded by the exposure of external hydrophobic FPs that penetrate into the cellular membrane and connect the virion with the cell. In comparison, type II fusion proteins contain internal FPs that are less well characterized (3, 6, 7). Notably, however, both types of FPs are essential for virus infection and share some features, e.g., they are hydrophobic and between 15 and 30 amino acid residues in length.
Since FPs are essential for infection by many viral pathogens, including immuno-deficiency, influenza, mumps, measles, hepatitis B and C, SARS (severe acute respiratory syndrome), Ebola, and presumably Zika viruses, they represent a potential target for antiviral drug development. Initially, it was thought that FPs can hardly be targeted for therapy because they are poorly accessible and rapidly penetrating the cellular mem-brane (8). Thus, it came as surprise that several lines of evidence suggested that an endogenous fragment of ␣1-antitrypsin, named VIRIP (VIRus Inhibitory Peptide), di-rectly targets the viral gp41 FP to inhibit HIV-1 entry (9). Synthetic peptides corre-sponding to the HIV-1 FP have membrane-perturbing activity that can be quantified in hemolysis assays (10). The potency of various VIRIP derivatives in preventing hemolysis and thus to interfere with insertion of the HIV-1 gp41 FP into the cellular membrane correlated significantly with their antiviral activity (9). In addition, structural nuclear magnetic resonance analyses revealed that the large hydrophobic surfaces of the FP and VIRIP or VIR-576 show a remarkable complementarity that is consistent with a highly specific interaction (9, 11). The structural data also revealed that altered amino acids in improved VIRIP derivatives further enforce hydrophobic contacts and revealed that newly introduced cysteine residues stabilize a conformation required for tight FP interaction (9). The correlation between antiviral activity and simulated free energy of the interaction between various VIRIP derivatives and the gp41 FP allowed improving the antiviral activity in a virtual screening approach (11). In further support of direct targeting of the viral FP, replacement of the HIV-1 gp41 FP by that of a simian immunodeficiency virus (SIV) significantly reduced viral sensitivity to inhibition by VIRIP derivatives (9). Recently, it has been shown that a bispecific peptide consisting of VIRIP and a peptide targeting the gp41 six-helix bundle exerts synergistic antiviral activity (12).
The HIV-1 gp41 FP is highly conserved, and VIRIP-based agents inhibited all virus strains tested, including divergent groups and subtypes, as well as multidrug-resistant variants (9). Broad antiviral efficacy, lack of cross-resistance and good compatibility made VIRIP derivatives interesting for clinical application. In fact, one derivative (VIR-576) that showed about 2 orders of magnitude improved antiviral efficacy was tested in a phase I/II clinical study in treatment naive HIV-1-infected individuals with high viral loads (11). Intravenous infusion of VIR-576 reduced the mean plasma viral load by up to 98% without causing severe adverse effects, providing proof of concept that inhibitors of viral FPs can be safe and effective in patients.
One interesting feature of VIRIP-based inhibitors was the high barrier to HIV-1 resistance. Initial attempts to generate resistant HIV-1 variants by weekly cell culture passage in the presence of VIR-576 for 2 months failed (9). Long-term serial passage of HIV-1 for more than 15 months in the presence of increasing concentrations of the VIR-353 derivative in MT-4 cells, however, allowed the selection of virus variants showing reduced susceptibility to inhibition (13). Sequence analyses at the end of cell culture passaging revealed seven amino acid changes across the viral Env glycoprotein. Three changes are located in the external glycoprotein gp120, and four are in the transmembrane protein gp41 but outside the FP. The authors reported that the combination of two mutations in gp120 (A433T and V489I) and one mutation in gp41
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
(V570I) that emerged first during cell culture passage are most relevant for VIR-353 resistance, whereas four subsequent changes (L545M, T244S, A612T, and N625K) restored viral replication fitness (14). However, this conclusion was mainly based on the ability of HIV-1 constructs to cause cytotoxic effects in MT-4 cells. In addition, only X4 HIV-1 was examined, and no experiments were performed using primary T cells and the clinically validated VIR-576 derivative.
To better assess the prospects of VIRIP-based inhibitors, we examined the impact of these mutations on VIR-353 and VIR-576 sensitivity, as well as the infectiousness, fusogenicity, and replication of X4 and R5 HIV-1 constructs in TZM-bl indicator cells and human peripheral blood mononuclear cells (PBMCs). We confirmed that the amino acid changes reduce sensitivity to both VIRIP derivatives in a cumulative manner. However, essentially all alterations contributed to resistance, although even the combination of all seven reduced the susceptibility of R5 HIV-1 to VIR-576 in primary cells only⬃4-fold. Furthermore, the four late changes not only reduced HIV-1 sensitivity to inhibition but also strongly impaired viral infectivity, fusion, and replication fitness. Our data show that the genetic barrier to HIV-1 resistance to VIRIP-based inhibitors is higher than previously reported. Reduced susceptibility to inhibition came at the cost of impaired Env function. Mutations emerging late during long-termin vitropassage did not restore viral infectivity and replication fitness. Thus, further development of inhibitors of viral FPs seems warranted.
RESULTS
Generation of mutant HIV-1 constructs.Esté and colleagues reported the accu-mulation of seven mutations in the HIV-1 Envelope (Env) glycoprotein during long-term cell culture passage of HIV-1 NL4-3 in the presence of increasing concentrations of VIR-353 (13, 14) (Fig. 1A). The amino acid changes were scattered throughout both the external gp120 and the gp41 transmembrane glycoproteins (Fig. 1B). Analysis of their localization in the prefusion HIV-1 gp41/gp120 structure (15) revealed that four (T244S, V489I, L545M, and V570I) of the seven mutations align to the interface of gp41 and gp120 (Fig. 1C). The initial mutation M1 (V570I) is located inside the flexible loop B of heptad repeat 1 (HR1) connecting the A and C helices in the prefusion state of gp41, while the subsequent mutation M2 (A433T) is hidden in the structure of gp120, suggesting potential allosteric effects on VIR-353 accessibility. Notably, all subsequent mutations (M3 to M7) are located in relative close proximity around the FP sequence at the N terminus of gp41 (Fig. 1D). All mutations are of conservative nature, presumably to preserve Env function in the resistance mutants.
To further investigate their impact on HIV-1 susceptibility to VIRIP-based inhibitors as well as viral infectivity and replication fitness, we introduced the seven mutations individually (M1, M2, . . ., M7; named according to their appearance in time) and in accumulating combinations (M1-2, M1-3, . . ., M1-7) in the Env protein of the well-characterized X4-tropic HIV-1 NL4-3 strain. To assess possible coreceptor dependencies, we also inserted all mutations into a derivative of NL4-3 containing the V3 loop region of HIV-1 92TH014.12, which efficiently utilizes CCR5, the main entry cofactor of HIV-1in vivo (16). For analyses of HIV-1 infection and susceptibility to inhibition in primary human CD4⫹T cells, we also generated corresponding sets of viral reporter constructs expressing the firefly luciferase or enhanced green fluorescent protein (eGFP) reporter genes.
High genetic barrier to VIR-353/576 resistance of HIV-1. To determine the susceptibility of the parental and mutant HIV-1 constructs to VIR-353, we pretreated TZM-bl reporter cells with various concentrations of the inhibitor and subsequently exposed them to virus stocks that were generated by transient transfection of HEK293T cells and adjusted for infectivity. TZM-bl cells express CD4, as well as CCR5 and CXCR4, and contain the -galactosidase reporter gene under the control of the HIV-1 long terminal repeat (17). Three days later, infection levels were quantified by a
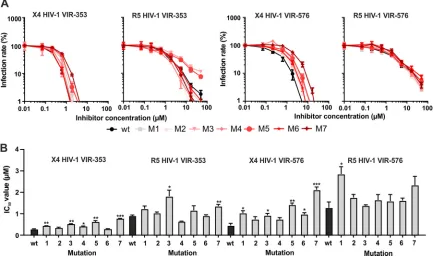
-galactosidase assay. The first four accumulating mutations (M1, M1-2, M1-3, and M1-4) had modest effects on the susceptibility of X4 HIV-1 NL4-3 to VIR-353 (Fig. 2A,
High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
left), increasing the 50% inhibitory concentration (IC50) from 0.27 to 0.86M (Fig. 2B,
left). In comparison, the addition of the fifth mutation (T244S) clearly enhanced VIR-353 resistance and the combination of all seven changes resulted in a 23-fold increased IC50
of 6.26M (Fig. 2A and B, left).
Analysis of the R5-tropic HIV-1 derivatives confirmed that the mutations in Env reduce viral susceptibility to VIR-353 inhibition in a cumulative manner increasing the IC50from 0.90 to 8.07M (Fig. 2A and B, mid left). Similar to the results obtained with
the X4 HIV-1 NL4-3 construct, the initial two alterations (V570I and A433T) had modest effects. In comparison, subsequent changes of V489I, L545M, and T244S clearly reduced susceptibility to VIR-353 inhibition. However, R5-tropic HIV-1 constructs were slightly less sensitive to VIR-353 inhibition than their X4-tropic counterparts. Most notably, R5 HIV-1 constructs containingⱖ4 amino acid changes showed a plateau in their
dose-FIG 1Time line of occurrence and localization of mutations in HIV-1 Env selected in the presence of VIR-353. (A) Manifestation of Env mutations during long-term passage of HIV-1 NL4-3 in the presence of increasing concentrations of VIR-353 in MT-4 cells (13). Mutations are numbered in the order of occurrence (M1 to M7) on a linear axis indicating the number of passages. (B) Localization of amino acid changes in the linear HIV-1 Env sequence. Abbreviations: SP, signal peptide; C, conserved; V, variable; FP, fusion peptide; HR, heptad repeat; TM, transmembrane; CD, cytoplasmic domain. (C) Localization of amino acid changes in the HIV-1 Env monomeric prefusion structure (created by The PyMOL Molecular Graphics System, version 2.0 [Schrödinger, LLC] using PDB file4TVP[15]). A ribbon diagram is shown with gp120 colored light blue, gp41 in rainbow colors, and the FP (amino acids 510 to 532) in pink. Note that the initial eight residues of the FP are not resolved in the crystal structure, suggesting its conformational flexibility. Residues that change upon long-term exposure to VIR-353 are displayed in surface representation. (D) Close-up view of the mutations in close proximity to the gp41 FP. Residues 518 to 532 of the gp41 FP are shown in the surface representation. Particularly, M5 (T244S), M3 (V489I), and M7 (N625K) directly contact the fusion peptide, but M4 (L545M) is also very close.
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:4.585.42.476.70.458.2]response curves, and less than 90% inhibition was achieved even at the maximal dose of peptide (Fig. 2A, middle left). Altogether, the results show that the mutations selected by serial passage of X4-tropic HIV-1 (13) also reduce the susceptibility of R5 virus to inhibition. However, not only the three initial alterations, as previously sug-gested (14), but also subsequent mutations contributed to the reduced susceptibility of HIV-1 to VIR-353 inhibition.
Esté and colleagues utilized VIR-353 (13, 14), which was one of most potent VIRIP derivatives described in the initial study (9). A later clinical study, however, was conducted with another derivative (VIR-576), which is dimeric and further differs in two amino acid residues from VIR-353 (11). To determine whether the mutations in HIV-1 Env selected in the presence of VIR-353 also affect viral susceptibility against the clinically validated VIRIP derivative, we examined the effect of VIR-576 on TZM-bl cell infection by the various HIV-1 constructs. Our results showed that X4 HIV-1 constructs carrying mutations reducing viral susceptibility to VIR-353 inhibition are also less sensitive to VIR-576 (Fig. 2A and B, middle right). Again, the impact of the initial three mutations was modest (an IC50increase from 0.45 to 1.38M), and each of the four
subsequent amino acid changes contributed to resistance development. The combi-nation of all seven substitutions resulted in⬃25-fold reduced susceptibility of X4 HIV-1 to VIR-575 inhibition (IC5011.14M).
Unexpectedly, the effects of all Env alterations on VIR-576 inhibition of the R5 HIV-1 NL4-3 derivative were relatively modest (Fig. 2A, right). Even the combination of all seven changes reduced viral susceptibility only⬃4-fold (IC504.85M) compared to the
parental R5 HIV-1 strain (IC50 1.28 M) (Fig. 2B, right). Again, R5 HIV-1 constructs
showed substantially flatter inhibition curves than X4 constructs (Fig. 2A) and hence higher IC90values despite similar or even lower IC50s (Fig. 2B). Altogether, the results
showed that the mutations reduced the susceptibility of HIV-1 to both VIR-353 and VIR-576 in a cumulative manner and that not only the three initial but also subsequent
FIG 2Effect of cumulative Env mutations on X4 and R5 HIV-1 inhibition by VIR-353 and VIR-576 in TZM-bl indicator cells. (A) TZM-bl reporter cells were preincubated with increasing concentrations of VIR-353 (left) or VIR-576 (right). Cells were subsequently infected with X4 or R5 HIV-1 NL4-3 construct mutants carrying the indicated cumulative mutations (M1 to M1-7) in Env normalized for the same infectivity. (B) The dose-response curves shown in panel A were used to calculate the IC50s. Shown are mean values (⫾the SD) obtained from triplicate infections.Pvalues indicate differences from the parental HIV-1 NL4-3 constructs (*,P⬍0.05;**,P⬍0.01;***,P⬍0.001).
High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:5.585.44.474.74.338.2]mutations clearly contribute to reduced susceptibility to inhibition. To some extent the effects were independent of the viral coreceptor tropism. However, efficient (⬎90%) inhibition was more difficult to achieve for R5 than for X4 HIV-1 constructs. Remarkably, even the combination of all seven mutations conferred only partial resistance, espe-cially in the case of R5 HIV-1 and the clinically validated VIR-576 derivative.
Effect of single mutations on HIV-1 susceptibility to VIRIP-based inhibitors.Our analysis of combined mutations did not support the previous conclusion that predom-inantly the first three mutations are involved in resistance development (14). To directly examine the effect of each of the seven mutations on VIR-353/576 susceptibility, we introduced them individually into the X4 and R5 HIV-1 constructs. Infection experi-ments showed that all individual changes had only modest effects on HIV-1 suscepti-bility to VIR-353 inhibition (Fig. 3A). In case of X4 HIV-1, mutations M5 (T244S) and M7 (N625K) had the most significant impact increasing the IC50of VIR-353 from 0.27M to
0.61 or 0.77M, respectively (Fig. 3B, left). These two alterations had also the strongest (i.e., 3.1- and 4.7-fold) effect on susceptibility of X4 HIV-1 to VIR-576 inhibition (Fig. 3A and B, middle right). Altogether, the effects of individual mutations on susceptibility to both VIRIP derivatives correlated significantly (R2⫽0.82;P⫽0.0019). In comparison,
the impact of individual amino acid changes on inhibition of R5 HIV-1 by VIR-353 and VIR-576 was even weaker (Fig. 3A), and the IC50s of the mutant viruses were usually not
significantly different from those of the parental virus (Fig. 3B). Notably, however, the M3 (V489I) and M5 (T244S) changes clearly reduced the IC90of VIR-353 against R5 HIV-1
from 7.5M to⬎50 and 30M, respectively. Most notably, our results showed that also individually the three initial amino acid changes selected during cell culture passage do not have stronger effects on VIRIP resistance than subsequent alterations.
Env mutations reduce sensitivity of HIV-1 to VIRIP derivatives in primary human cells.TZM-bl reporter cells provide a convenient and commonly used means for quantitative analyses of HIV-1 infection. However, they were derived from the cervical HeLa cancer cell line (18) that is usually not susceptible to HIV infection and
FIG 3Effect of individual amino acid substitutions in Env on X4 and R5 HIV-1 inhibition profiles in TZM-bl indicator cells. (A) TZM-bl reporter cells were preincubated with increasing concentrations of VIR-353 (left) or VIR-576 (right). Cells were subsequently infected with X4 or R5 HIV-1 NL4-3 construct mutants carrying the indicated individual mutations (M1 to M7) in Env normalized for the same infectivity. (B) Dose-response curves as shown in panel A were used to calculate the IC50s. Shown are mean values (⫾the SD) obtained from triplicate infections.Pvalues indicate differences from the parental HIV-1 NL4-3 constructs (*,P⬍0.05;**,P⬍0.01;***,P⬍0.001).
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:6.585.41.475.74.334.2]might not faithfully reflect effects in primary human cells (19). To confirm the impact of the mutations in a physiologically more relevant setting, we performed inhibition assays using primary human peripheral blood mononuclear cells (PBMCs) and X4 or R5 HIV-1 NL4-3 constructs expressing the firefly luciferase reporter gene. Prestimulated PBMCs were incubated with the inhibitor and exposed to infectivity normalized virus stocks, and the levels of luciferase activity in the cellular extracts were determined 3 days later. In agreement with the results obtained in TZM-bl cells, the mutations in Env resulted in a significant shift of the inhibition curves for both VIR-353 and VIR-576, irrespective of the viral coreceptor tropism (Fig. 4A). In contrast to the results obtained in TZM-bl cells, however, we did not observe that the curves obtained for R5 HIV-1 strains were flattened compared to X4 viruses. Moreover, even the X4 and R5 HIV-1 constructs containing the combination of all seven amino acid changes were fully inhibited at the highest dose of peptide. Examination of the IC50s showed that they
increased sequentially with the number of alterations but usually remained below 3M (Fig. 4B). The IC50s derived for VIR-353 and VIR-576 measured in PBMCs correlated well
FIG 4VIR-353 and VIR-576 inhibition profiles of HIV-1 luciferase reporter constructs in human PBMCs. (A) Stimulated PBMCs were preincubated with increasing concentrations of VIR-353 (left) or VIR-576 (right) and subsequently infected with infectivity normalized amounts of X4 or R5 HIV-1 NL4-3 firefly luciferase expressing reporter constructs carrying the indicated cumulative mutations (M1 to M1-7). (B) IC50s were calculated from the dose-response curves in panel A and tested for significance as described in the legend to Fig. 2. (C) Linear correlation analysis of IC50s determined by infection of PBMCs (see B) and TZM-bl cells (Fig. 2). Highlighted dot marks the mutant carrying all mutations.
High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:7.585.43.500.73.488.2]with those detected in TZM-bl reporter cells (Fig. 4C). However, while up to 25-fold increases in IC50s were measured in the indicator cell line, only between 3.5- and
10-fold effects were measured in PBMCs. The results obtained in PBMCs confirmed that essentially all mutations affect viral susceptibility to inhibition by VIRIP derivatives in a cumulative manner and that even the combination of all seven substitutions confers only partial resistance.
VIR-353/576 resistance is associated with impaired HIV-1 infectivity.To deter-mine possible effects of the resistance conferring mutations in Env on HIV-1 virion infectivity, we infected TZM-bl reporter cells or human PBMC with luciferase reporter HIV-1 constructs adjusted for equal quantities of reverse transcriptase (RT) activity. The resistance conferring mutations severely impaired the infectivity of the X4-tropic HIV-1 strain in TZM-bl cells in a cumulative manner (Fig. 5A, upper left). HIV-1 constructs containing ⱖ4 amino acid substitutions were most severely attenuated and 5- to 10-fold less infectious than the parental virus. The results were confirmed in human PBMCs (Fig. 5A, lower left), and infectivity in both cell types correlated well (Fig. 5B, upper). Individually, all but the M2 (A433T) mutation reduced virion infectivity with changes that evolved early and later during passaging, showing similar attenuating effects (Fig. 5A, right). Mutations in gp41 (M1, M4, M6, and M7) impaired HIV-1 infectivity in PBMC cultures more significantly than those located in gp120 (M2, M3, and M5). In the context of the R5 HIV-1 constructs, the mutations had similar effects on virion infectivity, and analyses of HIV-1 IRES-eGFP constructs in both TZM-bl cells and PBMCs confirmed the results obtained using luciferase reporter viruses (data not shown). In all cases, X4 and R5 HIV-1 constructs containingⱖ4 changes were substan-tially less infectious than those containing just the three initial changes. Thus, reduced susceptibility of HIV-1 to VIRIP derivatives came at the cost of reduced virion infectivity, and the final changes that emerged duringin vitropassage (13, 14) did not restore viral infectiousness.
VIR-353/576 resistance is associated with delayed and/or attenuated HIV-1 replication.Our results from VIR-353/576 inhibition and HIV-1 infectivity assays did not support the previous conclusion (14) that mutations selected late during long-term
FIG 5Infectivity of HIV-1 NL4-3 mutants carrying VIR-353 and VIR-576 resistance mutations. (A) TZM-bl cells (upper) or prestimulated PBMCs (lower) were infected with X4 HIV-1 NL4-3 luciferase reporter constructs containing cumulative or individual amino acid changes in Env that were normalized for RT activity. Infection rates were determined 3 days postinfection by measuring luciferase activities and normalized to wild-type HIV-1 (100%). Values represent mean values obtained from triplicate infections (⫾the SD).*,
P⬍0.05;**,P⬍0.01;***,P⬍0.001. (B) Correlation between HIV-1 infections levels determined in PBMCs and TZM-bl indicator cells.
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:8.585.42.465.70.301.2]passage in cell culture restore viral fitness rather than affecting VIR-353 sensitivity. To directly determine the effects on HIV-1 replication fitness in relevant target cells, we analyzed viral replication kinetics in infected PBMC cultures. The parental X4 HIV-1 NL4-3 strain replicated with rapid kinetics, and RT activities of released virus already peaked at 3 days postinfection (Fig. 6A). HIV-1 constructs containing up to three cumulative mutations showed similar kinetics, while additional amino acid changes were associated with a marked delay. Individually, most amino acid substitutions had little if any effect on HIV-1 replication kinetics and efficiency (Fig. 6B). Exceptions were the M4 (L545M) and M6 (A612T) mutations in gp41 that delayed virus replication and reduced virion infectivity. In the context of R5 HIV-1 constructs, all mutations reduced viral replication capacity, and viruses containingⱖ4 substitutions were usually more strongly attenuated than those containingⱕ3 changes (Fig. 6C).
As summarized in Fig. 7A, essentially each of the seven cumulative changes in the HIV-1 Env protein contributed to decreased sensitivity to inhibition by VIR-353/576 but also to decreased viral infectivity and replication. However, the impact of the three initial mutations on VIRIP resistance and Env function was modest, while almost full effects were observed by the combination of five amino acid changes. Mutations M1-4 were associated with an intermediate phenotype. On average, the two final alterations, M6 and M7, further increased the IC50by⬃1.5-fold. They did not further disrupt viral
infectivity and marginally enhanced it in some experiments. Altogether, our results FIG 6Replicative fitness HIV-1 NL4-3 constructs containing mutations involved in VIR-353 and VIR-576 resistance. Stimulated PBMCs from two donors were inoculated with X4 (A and B) or R5 (C) HIV-1 constructs containing cumulative (M1 to M1-7) (A and C) or individual (M1 to M7) (B) mutations in the Env glycoprotein. Infections were performed using RT activity-normalized virus stocks and performed in triplicates. Aliquots of supernatants were taken at the indicated days and analyzed for RT activity. SDs are not shown for clarity but were generally below 10%.
High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:9.585.55.359.71.416.2]clearly demonstrate that not only the first three but also subsequent changes contrib-ute to VIR-353/576 resistance and that the concomitant decrease in HIV-1 infectivity and replication fitness was not restored by changes emerging late during in vitro
passage.
As outlined above, most mutations (M3 to M7) are located in close proximity to the gp41 FP domain (Fig. 1D), suggesting that they might affect its accessibility. To test this, we took advantage of the neutralizing antibody VRC34.01. This antibody targets an epitope that includes the N-terminal eight residues of the gp41 FP, and prevents viral entry by inhibiting conformational changes in gp120 and gp41 required for virion fusion with the cell (20). VRC34.01 had modest effects on infection by wild-type (wt) HIV-1 NL4-3, reducing infection by⬃50% at a concentration of 10g/ml (Fig. 7B). The three initial alterations moderately increased HIV-1 susceptibility, while all viral con-structs containing ⱖ5 mutations were fully resistant (Fig. 7B). Thus, the amino acid changes selected in the presence of VIR-353 affect HIV-1 inhibition by an antibody targeting the viral FP.
VIR-353/576-resistant HIV-1 derivatives show impaired fusogenicity.The resis-tance mutations were distributed over a surface area of the Env glycoprotein, and none of them mapped directly to the gp41 FP (Fig. 1) proposed to be the primary target of VIRIP or its derivatives (9). Most mutations, however, are located in close proximity to the FP domain and/or in gp41 domains thought to be involved in viral fusion (15). Thus, we examined whether altered fusion kinetics might underlie the reduced susceptibility of the mutant HIV-1 constructs to VIR-353 and VIR-576 inhibition and impaired infec-tivity. To analyze this, we used an enzyme-based colorimetric fusion assay first de-scribed by Cavrois et al. (21). Virus particles containing cumulative, as well as individual, mutations in Env and additionally the-lactamase-Vpr (BlaM-Vpr) hybrid protein were generated by cotransfection of HEK293T cells. Kinetics studies of the parental X4 HIV-1 strain showed that 2 h of incubation was sufficient for maximal fusion (Fig. 8A) and hence used in subsequent studies. Analyses of fusion kinetics of RT normalized X4 HIV-1 constructs showed that the initial M1 mutation slightly delays fusion kinetics, while the subsequent M2 mutation alone or in combination with M3 restored it to wild-type levels (Fig. 8B). The quadruple HIV-1 mutant, however, displayed clearly delayed fusion kinetics and efficacy, and subsequent mutations had further attenuating effects. Alto-gether, HIV-1 constructs containing ⱕ3 amino acid changes showed near wild-type fusion kinetics and efficiencies, while those harboring ⱖ4 substitutions were poorly fusogenic (Fig. 8B). Analysis of HIV-1 constructs containing individual mutations
FIG 7Impact of cumulative mutations in Env on HIV-1 sensitivity to VIR-353/576 inhibition, infectivity, replication and sensitivity to an antibody targeting the FP. (A) IC50and infectivity values are provided relative to the parental X4 and R5 HIV-1 constructs (100%) and represent mean values of triplicate measurements. Replication indicates the relative RT activity detected for the mutant HIV-1 constructs at the peak of wt virus replication (100%). Shaded areas highlight the effect of the three initial and three final mutations selected duringin vitropassage. (B) Effect of cumulative X4 HIV-1 Env mutations on anti-FP antibody VRC34.01 inhibition profile in TZM-bl indicator cells. TZM-bl reporter cells were incubated with the indicated increasing concentrations of VRC34.01. Cells were subsequently infected with infectivity-normalized X4 HIV-1 NL4-3 mutants carrying the indicated cumulative mutations in Env. Infection rates were determined 3 days later. Shown are mean values (⫾the SD) obtained from triplicate infections.
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:10.585.45.465.72.219.2]showed that most mutations in gp41 affected virion fusion, with M4 strongly impairing and M7 clearly enhancing viral fusion (Fig. 8C). While the M7 change may have modest restorative effects, however, it clearly did not allow efficient fusion if combined with the remaining six mutations (Fig. 8B). In agreement with the results obtained in infectivity and replication assays, these data further support that reduced susceptibility to VIRIP-based inhibitors comes at a cost of impaired Env function.
DISCUSSION
HIV-1 is highly variable and capable of rapidly developing resistance to most antiretroviral drugs (22). Thus, despite the availability of effective antiretroviral therapy, anti-HIV agents associated with a high genetic barrier for resistance are still of signif-icant interest. VIRIP-based HIV-1 inhibitors that target virus-cell fusion seem to consti-tute a much higher obstacle to resistance than other antiretroviral agents (23). Initial attempts failed to generate VIR-576-resistant HIV-1 in cell culture under conditions readily allowing the selection of viruses resistant to other antiretroviral agents (9). In vitro selection of HIV-1 variants showing reduced susceptibility to VIR-353 was achieved, however, by extensive serial passage of the lab-adapted X4 NL4-3 HIV-1 over more than 15 months in the presence of increasing concentrations of this VIRIP FIG 8Fusion kinetics of VIR-353 and VIR-576 resistant X4 HIV-1 constructs. (A) Time course for assay optimization. Jurkat cells were inoculated with X4 HIV-1 containing the BlaM-Vpr hybrid protein for 1 h on ice, virus was washed off and cells were incubated at 37°C for the indicated time period. Fusion was determined after overnight staining with CCF2 by flow cytometry analysis. (B and C) Jurkat cells were inoculated for 1 h with RT-activity normalized X4 HIV-1 containing cumulative (M1 to M1-7) (B) or individual (M1 to M7) (C) mutations, and fusion was determined as described for panel A. Fusion values at baseline (0 h) were subtracted. The lower panel show calculated areas under the curve (defined as maximal fusion by Cavrois et al. [21]). The upper panel is representative for two independent experiments and lower panel indicates averages (⫾the SD).*,P⬍0.05;**,P⬍0.01;***,P⬍0.001.
High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:11.585.50.362.70.421.2]derivative (13). Here, we show that essentially all seven amino acid changes across the viral Env glycoprotein previously identified contribute to partial HIV-1 resistance to VIRIP derivatives VIR-353 and VIR-576. We further demonstrate that significant VIR-353/ 576 resistance is associated with grossly impaired HIV-1 infectivity and replication fitness in PBMC cultures, presumably due to reduced fusogenic activity of the viral Env protein. Thus, our data confirm thatin vitro-selected mutations significantly reduce viral susceptibility of X4 HIV-1 to VIR-353 (13) and further show that this also holds true for R5 HIV-1 and the clinically validated VIR-576 derivative. Our results do not confirm the previous conclusion (14), however, that predominantly the first three alterations se-lected duringin vitropassage contribute to resistance while subsequent ones restored viral fitness. We found that the first three mutations have only modest effects on VIR-353/576 sensitivity and viral infectivity. The next four amino acid changes further reduced HIV-1 susceptibility to infection but also resulted in strongly impaired viral infectivity and delayed and/or attenuated replication in PBMC cultures. Thus, the genetic barrier to VIR-353/576 resistance is higher (ⱖ5 mutations) than previously suggested (3 mutations). Perhaps most importantly, VIRIP-resistant forms of HIV-1 obtained after 83 passages in cell culture (13) were poorly infectious and fusogenic. Thus, viral fitness was not restored after long-termin vitroculture. Our results support further clinical development of VIRIP-based HIV-1 inhibitors since a substantial number of mutations is required for partial resistance, and a clinical benefit will most likely be maintained since they come at a severe fitness cost.
Esté et al. reported an up to 80-fold decrease in the susceptibility of X4 NL4-3 HIV-1 against VIR-353 (13). We observed that cumulative mutations reduced the IC50by about
25-fold compared to wild-type virus. This quantitative difference is most likely due to differences in the experimental protocols and target cell types. In essence, the effects of the mutations were consistent for both VIRIP derivatives and types of target cells (TZM-bl and PBMC). However, some quantitative differences were noted. For X4 HIV-1 the effect of the cumulative mutations on VIR-353 and VIR-576 sensitivity was more pronounced in TZM-bl cells than in PBMCs (Fig. 7, left). In comparison, the mutations had a lesser effect on VIR-576 than on VIR-353 sensitivity in the context of R5 HIV-1 (Fig. 7, right). Even the combination of all seven changes increased the IC50of VIR-576 for R5
HIV-1 in PBMCs only by 4-fold. Thus, while they significantly reduced viral susceptibility this effect would not meet the definition of resistance according to the criteria used by Esté et al., i.e., a 5-fold increase of IC50compared to the wild-type virus. These findings
are relevant since most primary HIV-1 strains utilize CCR5 and VIR-576 has been proven effective in patients (11). The reasons for these target cell type and/or VIRIP derivative-dependent differences remain to be determined and might involve differences in CD4 and coreceptor expression levels as well as altered affinity and accessibility of the target region in Env to the inhibitors. For example, TZM-bl cells express very high levels of CD4 and CCR5 (24) and are more susceptible to R5 than to X4 HIV-1 infection (25), while a substantially higher number of CD4⫹ T cells in PBMC cultures express CXCR4 than CCR5. While VIR-353 is monomeric, VIR-576 is a dimer (11). Thus, changes in Env structure and fusion kinetics might have differential effects on the efficiency of inhibi-tion by these two VIRIP derivatives.
Structural, functional, and interaction studies suggest that VIRIP-based inhibitors target the gp41 FP (9, 11, 26). The results of Esté et al. called this into question since none of the seven mutations is located in the FP region (13, 14). Another study selected HIV-1 variants against the VIRIP analogue VIR165 and also identified alterations in the C1 domain of gp120 and the HR1 domain of gp41 instead of the FP (27). Notably, some C1 mutations rendered HIV-1 dependent on the inhibitor (27). Further studies are required to fully clarify the mechanisms underlying VIRIP inhibition and viral evasion. The localization and functional consequences of the mutations suggest that they reduce viral sensitivity to VIRIP-based inhibitors by affecting Env structure, fusion efficiency, and accessibility of the FP rather than by altering their primary target site. We observed that the alterations selected in the presence of VIR-353 also affect HIV-1 susceptibility to the antibody VRC34 that targets an epitope that includes the
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
N-terminal part of the FP (20). Notably, Eggink et al. also suggested that the above-mentioned alterations in the gp120 C1 and gp41 HR1 regions alter VIR165 sensitivity because they change the kinetics of Env conformational changes and thus decrease the accessibility of the FP target region (27).
Essentially, each of the seven mutations increased the IC50of HIV-1 against VIR-353
and VIR-576, supporting that all of them are involved in the mechanism of resistance. The alterations are located in both gp120 and in gp41 and distributed over a space far too large for direct VIR-353/576 interaction. In addition, individually all changes had only modest effects on VIR-353/576 sensitivity, whereas single amino acid changes can confer significant resistance to enfuvirtide (T20) inhibition (28). The initial mutation M1 (V570I) is located inside the flexible loop B of the heptad repeat 1 (HR1) region connecting the A and C helices in the prefusion state of gp41. During fusion, this loop B needs to rearrange into a helix consequently combining helices A and C, which result in the insertion of the FP into the cellular membrane (29). As summarized in Fig. 9, the conservative V570I substitution might affect this rearrangement and thereby slightly reduce viral infectivity, fusion and VIR-353/576 sensitivity.
Mutations in C4 (M2, A433T) and C5 (M3, V489I) might affect gp120 structure and function and the former usually enhanced viral infectivity. Mutation M4 (L545M) had a significant disruptive effect on viral fusion and infectivity both individually and in combination with the M1-3 changes. It has been reported that L545 is involved in trimer formation (15). Similarly to M1 (V570I), M4 (L545M) is localized in the flexible loop B connecting the A and C helices in the prefusion structure (Fig. 9), and a similar substitution (A558T) was identified in an independent study examining HIV-1 resistance to VIR-165 (27). This mutation in HR1 might interfere with six-helix bundle formation, thereby decreasing viral fitness but also susceptibility to VIR-353/576. M6 (A612T) is also localized inside a flexible loop in the prefusion structure of gp41. During the fusion process, this flexible loop forms the linker between the two-heptad repeats. Thus, A612T affects an additional region that is crucial during the fusion process. Finally, M7 (N625K) is located inside the loop E connecting the ␣-helices D and F, which will rearrange into the second heptad repeat HR2. Individually, this mutation impaired viral infectivity, although it accelerated virion fusion and possibly caused a slight recovery of viral fitness in the context of the remaining six mutations. Notably, several alterations (M3-V489I, M4-L545M, M5-T244S, and M7-N625) that are well apart in the linear Env sequence are located in very close proximity to the gp41 FP (Fig. 1C and D) and might clearly affect its accessibility to inhibitors.
If the FP represents the direct target of VIRIP-based inhibitors, why were no alterations selected in this region? Besides in vitro passaging, initial attempts to generate VIRIP-resistant HIV-1 variants involved the generation of HIV-1 mutants con-taining random changes in two to three amino acid positions across the entire gp41 FP region. Most of these HIV-1 mutants showed grossly impaired infectivity, and no resistant virus variants were detected after propagation in CEM-M7 cells in the presence of VIR-576 (9). These previous results show that many changes in the gp41 FP region are not tolerated and suggest that more than two or three amino acid changes might be required for VIRIP resistance, possibly because of relatively large interacting com-plementary surfaces. Notably, replacement of the HIV-1 FP by that of SIVmac/HIV-2,
which differs in nine amino acids from the original FP, conferred⬃5-fold resistance to VIR-576 (9). Thus, it might be easier for HIV-1 to evolve reduced sensitivity to VIR-353/ 576 inhibition by changes across Env altering fusion kinetics and target accessibility rather than by acquisition of changes in the gp41 FP. An indirect mechanism is in agreement with our finding that the mutations outside the FP only confer partial resistance and came at the cost of severely impaired Env function. While mutation of the primary target side of the inhibitor is the most common reason for resistance, mechanisms that are more complex are also well known. For example, mutations in gp120 might render HIV-1-resistant against fusion inhibitors targeting the six-helix bundle formation of gp41 (28). Furthermore, changes outside the V3 loop region of gp120 affecting the coreceptor tropism can reduce viral susceptibility to CCR5
antag-High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
onists (30–32). Thus, amino acid changes outside the identified drug target region can render HIV-1-resistant to entry inhibitors. In addition, it is well known that alterations in the helical regions of gp41 affects fusion kinetics and susceptibility to HIV-1 entry inhibitors (33, 34). The finding that alterations reducing HIV-1 susceptibility to VIR-165 and VIR-353 increase viral sensitivity to inhibition by T20 targeting the HR1 region of gp41 (13, 27) also supports effects on fusion kinetics. Thus, the results of the previous studies are not in disagreement with the gp41 FP being the primary target of VIR-based inhibitors.
Previous studies on other HIV-1 entry inhibitors, i.e., the fusion inhibitor T20 and the CCR5 antagonist Maraviroc, showed that resistance conferring mutations selected in
FIG 9Possible implications of mutations conferring VIR-353 resistance on Env function. The upper panel illustrates an HIV-1 Env gp120-gp41 protomer in the viral membrane in close proximity to the cellular membrane and its receptors. The image was inspired by Sanders and Moore (45). The gp41 subunit has a C-terminal cytoplasmic tail (CT), a transmembrane domain (TM), and an ectodomain (blue/green) that wraps around the N and C termini of gp120 (red) with an N-terminal FP (pink). The gp41 ectodomain consists of six-helix-forming segments (A to F). In the prefusion state, segments B and E have a loop structure, whereas A, C, D, and F appear as helices. Engagement of gp120 with CD4 induces conformational changes, allowing coreceptor interaction and further reorganization of gp120, followed by unwrapping of gp41. Via an intermediate state, gp41 loop B and helix segments A and C rearrange into a long helix A-C (HR1) that inserts the FP into the cellular membrane. Mutations 1 and 4 in loop B might directly influence this initial rearrangement. In the continuing fusion process, loop E similarly rearranges into a long helix consisting of segments D to F (HR2). HR1 and HR2 now align to form the hairpin six-helix (in the protomer: two-helix) bundle that pulls the viral and cellular membranes together to mediate fusion. Mutation 7 is located in loop E that connects HR1 and HR2 and might affect hairpin formation. Mutations 3, 4, 5, and 7 are in close proximity to the FP in the prefusion state and might alter its accessibility. The lower panel summarizes the location, functional effects, and potential mechanistic implications of the mutations in Env selected by passaging HIV-1 in the presence of VIR-353.
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
[image:14.585.44.474.75.470.2]cell culture are frequently also found in HIV-1-infected individuals (35–37). However, T20 and Maraviroc act by mechanisms that are different from that of VIRIP. Resistance to T20 has a low genetic barrier and just requires just one or two mutations in HR1 that are usually not associated with severe fitness costs (38, 39). In the case of Maraviroc, HIV-1 typically acquires resistance by accumulation of two to four mutations in the V3 loop region of gp120 V3 region, allowing CCR5 utilization in an inhibitor-insensitive manner (37). The genetic barrier for VIRIP resistance of HIV-1 seems to be significantly higher and comes at a more severe fitness cost. The VIR-353-resistant HIV-1 derivative remained fully sensitive to T20 and the CXCR4 antagonist Plerixafor (AMD3100) (13, 14). How mutations conferring resistance to VIRIP derivatives affect viral susceptibility to neutralization by antibodies or chemokines and whether the changes selected in cell culture would also occur in HIV-1-infected individuals remains to be determined. Presumably, VIRIP-resistant variants would also emerge in HIV-1-infected individuals, but their occurrence would most likely take substantially longer time periods and come at more severe fitness costs compared to other HIV-1 inhibitors.
The X4 HIV-1 mutant carrying the initial three mutations showed IC50s ranging from
0.33 to 1.0M, while the M1-7 construct displayed IC50s ranging from 2.1 to 11.0M.
In addition, the first three mutations reduced X4 HIV-1 infectivity by 55 to 65%, while the combination of all seven resulted in 88 to 91% reduced infectiousness. Finally, the combination of all seven mutations (M1-7), but not the three initial ones (M1-3), was associated with delayed replication kinetics in PBMC cultures and grossly impaired the efficacy of virion fusion. Thus, our results do not support the conclusion of Esté et al. that mutations M1-3 are largely sufficient for resistance, while the last four mutations rescue viral fitness (14). In the previous study, replication fitness was measured by determining cytopathic effects at a single time point in virus-infected MT-4 cells (14) and might not faithfully recapitulate viral replication fitness in primary human target cells. Altogether, our results obtained in TZM-bl and primary cells using both X4 and R5 HIV-1 constructs in infection, fusion, and replication assays support that all seven mutations contributed to maximal VIR-353/576 resistance but also severely impaired Env function and HIV-1 replication fitness.
Previous studies showed that VIRIP-based inhibitors do not show cross-resistance to other antiretroviral agents (9) and were safe and effective in a clinical trial (11). Here, we show that the genetic barrier to resistance against VIRIP-based inhibitors is high and associated with grossly impaired viral infectivity and replication fitness. Nonetheless, VIRIP-based inhibitors have significant drawbacks such as lack of oral availability and relatively low stability and bioavailability. Highly effective, relatively well tolerated, and orally available drugs against HIV/AIDS already exist. Thus, why study resistance to VIRIP-based inhibitors? As outlined above, the high barrier to resistance and distinct mechanism make VIRIP interesting for further investigation. Perhaps more importantly, however, FPs are essential for host cell entry by most enveloped viruses, including major human pathogens, such as the influenza, mumps, measles, hepatitis B and C, SARS, and Zika viruses. For most of these viral pathogens, no specific and effective therapy is available. The FPs of these viruses share some structural and mechanistic features, suggesting that this critical functional domain may represent a common target to prevent viral entry. In fact, recent data show that antibodies against viral FPs block not only HIV-1 (40) but also infection by influenza (orthomyxovirus) and Junin (arenavirus) viruses (41, 42). As mentioned above, viruses encode either type I or II fusion proteins, and both share a number of properties, such as hydrophobicity, length, and membrane-destabilizing activity (7). Thus, studies on VIRIP-based inhibitors might pave the way toward analogous inhibitors of other dangerous enveloped viruses. Several viral pathogens utilizing FPs for infection, such as the Ebola, Lassa, or dengue viruses, are characterized by high acute pathogenicity and lethality. In contrast to HIV, however, they do not cause chronic infection and would only require effective short-term treatment. Thus, injectable peptide drugs showing similar efficacy as VIR-576 in HIV-infected individuals, would represent an enormous progress in the treatment of some human pathogens.
High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
MATERIALS AND METHODS
Proviral constructs, plasmids, and cloning.Mutations were generated using splice overlap exten-sion PCR (M1, V570I 5=-CAACTCACAATCTGGGGCATC-3= and 5=-GATGCCCCAGATTGTGAGTTG-3=; M5, T244S 5=-CATGTACAAATGTCAGCTCAGTACAATG-3=and 5=-CATTGTACTGAGCTGACATTTGTACATG-3=) or a QuikChange II site-directed mutagenesis kit (Agilent) (M2, A433T 5=-GGAGGGGCATACATTGTTTTTCCTAC TTCCTGCC-3=and 5=-GGCAGGAAGTAGGAAAAACAATGTATGCCCCTCC-3=; M3, V489I 5=-TTGGAGAAGTGA ATTATATAAATATAAAGTAATAAAAATTGAACCATTAGGAGTAGCA-3=and 5=-TGCTACTCCTAATGGTTCAATT TTTATTACTTTATATTTATATAATTCACTTCTCCAA-3=; M4, L545M 5=-CTGACGGTACAGGCCAGACAATTAATGT CTGATATAGTG-3=and 5=-CACTATATCAGACATTAATTGTCTGGCCTGTACCGTCAG-3=; M6, A612T 5=-GATTT ATTACTCCAACTAGTATTCCAAGGCACAGCAGTGG-3=and 5=-CCACTGCTGTGCCTTGGAATACTAGTTGGAGT AATAAATC-3=; M7, N625K 5=-ATCTCTGGAACAGATTTGGAATAAGATGACCTGGATGG-3=and 5=-CCATCCAG GTCATCTTATTCCAAATCTGTTCCAGAGAT-3=) according to the manufacturer’s instructions and sequenced (5=-GCAGAAGACAGTGGCAATGA-3=, 5=-ACACATGGAATCAGGCCAGT-3=, 5=-TTTGTTCCTTGGGTTCTTGG-3=, and 5=-TCGATTAGTGAACGGATCCTTAG-3=) to verify correctness. Mutations were introduced into X4-tropic HIV-1 NL4-3 (pBR_NL4-3) and its R5-X4-tropic derivative where the V3-loop region of Env has been replaced by that of HIV-1 92TH014.12 (16). After introduction and verification of all mutations, env
cassettes were cloned back into X4 NL4-3, R5 NL4-3, and corresponding reporter viruses expressing the firefly luciferase or coexpressing Nef and eGFP via an IRES element generated as reported previously (43, 44) using StuI and XhoI. pCMV_BlaM_Vpr and pAdVAntage were used to generate-lactamase incor-porating viruses as described previously (21).
Peptides.VIR-353 (LEAIPCSIPPCFLFNKPFVF) and VIR-576 (LEAIPCSIPPEFLFGKPFVF)x2 were prepared by Fmoc solid-phase synthesis as described previously (9, 11) and subsequently purified by reversed-phase chromatography. Identity and homogeneity of the products were analyzed by reversed-reversed-phase high-pressure liquid chromatography, capillary zone electrophoresis, electrospray mass spectroscopy, and sequence analysis. The peptides were dissolved in 150 mM natrium bicarbonate– 48 mM sodium hydroxide buffer until further use.
Cell culture.HEK293T (American Type Culture Collection [ATCC]) and TZM-bl (obtained through the NIH AIDS Reagent Program, Division of AIDS, NIAID, NIH: TZM-bl from John C. Kappes, Xiaoyun Wu, and Tranzyme, Inc.) cells were cultivated in Dulbecco modified Eagle medium (DMEM) supplemented with 10% heat-inactivated fetal calf serum (FCS), 2 mML-glutamine, 100g/ml streptomycin, and 100 U/ml penicillin. Jurkat cells (ATCC) and PBMCs were maintained in equally supplemented RPMI 1640. PBMCs were isolated from buffy coats from healthy human donors using lymphocyte separation medium (Biocoll separating solution; Biochrom), and culture medium was additionally supplemented with 10 ng/ml interleukin-2 (Miltenyi Biotec). Three days prior to infection, 106PBMCs/ml were stimulated with 1g/ml phytohemagglutinin (Thermo Scientific). All cells were kept in a humidified incubator at 37°C at 5% CO2.
Virus stocks.Virus stocks were generated by transient transfection of HEK293T cells using the calcium phosphate precipitation technique. HEK293T cells were seeded in 2 ml of medium in 6-well plates or in 20 ml medium in 75-cm2flasks (Sarstedt, Nümbrecht, Germany). Before transfection the next day, where cells showed a confluence of 60 to 80% medium was changed. As a transfection mix, 5 or 50
g of proviral DNA, respectively, were diluted in 125 mM CaCl2and water, and an equal volume of 2⫻ HEPES-buffered saline (HBS) was added dropwise. After thorough mixing, the precipitate was added to the media dropwise. Medium was replaced with fresh supplemented DMEM (2.5% [vol/vol] FCS) after 6 to 16 h of incubation. At 24 h after a medium change, the viral supernatant was harvested, briefly centrifuged (3 min, 1,300 rpm) to remove cellular debris, and stored shortly at 4°C or frozen for later usage at⫺80°C.
Infection of cell lines.A total of 10,000 TZM-bl reporter cells (19) were seeded in 96-well microplates with F bottoms in 100l of supplemented DMEM. On the following day, 80l of medium was added, and the cells were infected by adding 20-l virus stocks normalized for RT activity. For inhibition assays, 60l of supplemented medium and 20l of serially diluted VIR353/576 or anti-FP antibody VRC34.01 were added to the cells. After 1 h of incubation at 37°C, the cells were exposed to 20-l infectivity normalized virus stocks. At 3 days postinfection, the supernatant was removed, and Gal-Screen substrate/ buffer A was applied to lyse cells and determine the Tat-driven-galactosidase activity, as described previously (43), in an Orion II microplate luminometer using the software Simplicity 4.02 (Berthold Detection Systems). The enzyme activity was measured as relative light units/second. Averages and standard deviations (SD) were calculated from triple measurements after subtraction of background. IC50s were calculated using GraphPad Prism.
Antibodies.The antibody VRC34.01 that targets the N terminus of the HIV-1 FP (20) was kindly provided by Kai Xu and Peter D. Kwong (Vaccine Research Center, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD).
Fusion assay.Viral fusion was monitored using a virion fusion assay as described previously (21). To generate-lactamase incorporating virus stocks, HEK293T cells were transfected in 6-well plates with 3.3
g proviral DNA, 1.1g of pCMV_BlaM-Vpr plasmid and 0.6g of pAdVAntage vector. To determine fusion kinetics, 500,000 Jurkat cells were incubated with 1.0 ml of RT activity-normalized virus stocks at 4°C on ice for 1 h to allow attachment of viral particles. Subsequently, the cells were washed three times with cold PBS, resuspended in supplemented RPMI 1640, and incubated at 37°C for various time periods. After incubation, the cells were washed three times and stained with 100l of staining solution (containing the-lactamase substrate CCF2/AM) by overnight incubation at room temperature in the dark. Finally, the cells were washed three times with PBS, fixed with 2% paraformaldehyde, and analyzed by flow cytometry using a BD FACSCanto II Cell Analyzer.
Müller et al. Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
Reverse transcriptase assay.A standard virus stock of known p24 antigen concentration and the samples of interest were diluted in PBS (1:3 to 1:5). The samples (5l) were mixed with 25l of RT mixture consisting of 2.5 ml of RT master mix, 10l dithiothreitol, and 2.5l of P32isotope and then incubated at 37°C for 2 to 3 h. Subsequently, 5-l aliquots were dropped on Whatman filters, dried, washed three times with 2⫻SSC (1⫻SSC is 0.15 M NaCl plus 0.015 M sodium citrate) buffer and once with 95% ethanol, and dried again at 65°C. The filters were stored in a cassette with a film at 4°C overnight. Films were developed using a Fuji FLA-3000 scanner and the Basreader FIA3000 program, and the data were analyzed using AIDA software.
Statistical analyses.IC50s were compared using a two-tailed Studentttest. Prism version 7.03 for Windows (GraphPad Software, La Jolla, CA) was used for all calculations.
ACKNOWLEDGMENTS
We thank Daniela Krnavek and Susanne Engelhart for expert technical assistance, Christina Stürzel for help with primer design, and Kai Xu and Peter D. Kwong for providing the VRC34.01 antibody. We are also grateful to Ludger Ständker and Nico Preising (both CFP, Ulm, Germany) and to Wolf-Georg Forssmann (Hanover, Germany) for peptides syntheses and peptides, respectively.
This study was supported by the Deutsche Forschungsgemeinschaft (SFB 1279).
REFERENCES
1. Harrison SC. 2015. Viral membrane fusion. Virology 479 – 480:498 –507.
https://doi.org/10.1016/j.virol.2015.03.043.
2. Garcia NK, Guttman M, Ebner JL, Lee KK. 2015. Dynamic changes during acid-induced activation of influenza hemagglutinin. Structure 23: 665– 676.https://doi.org/10.1016/j.str.2015.02.006.
3. Apellániz B, Huarte N, Largo E, Nieva JL. 2014. The three lives of viral fusion peptides. Chem Phys Lipids 181:40 –55.https://doi.org/10.1016/j .chemphyslip.2014.03.003.
4. Eckert DM, Kim PS. 2001. Mechanisms of Viral Membrane Fusion and Its Inhibition. Annu Rev Biochem 70:777– 810.https://doi.org/10.1146/annurev .biochem.70.1.777.
5. Wilen CB, Tilton JC, Doms RW. 2012. Molecular mechanisms of HIV entry. Adv Exp Med Biol 726:223–242.https://doi.org/10.1007/978-1 -4614-0980-9_10.
6. Worch R. 2014. Structural biology of the influenza virus fusion peptide. Acta Biochim Pol 61:421– 426.
7. Smith AE, Helenius A. 2004. How viruses enter animal cells. Science 304:237–242.https://doi.org/10.1126/science.1094823.
8. Blumenthal R, Dimitrov DS. 2007. Targeting the sticky fingers of HIV-1. Cell 129:243–245.https://doi.org/10.1016/j.cell.2007.04.005.
9. Münch J, Ständker L, Adermann K, Schulz A, Schindler M, Chinnadurai R, Pöhlmann S, Chaipan C, Biet T, Peters T, Meyer B, Wilhelm D, Lu H, Jing W, Jiang S, Forssmann W-G, Kirchhoff F. 2007. Discovery and optimiza-tion of a natural HIV-1 entry inhibitor targeting the gp41 fusion peptide. Cell 129:263–275.https://doi.org/10.1016/j.cell.2007.02.042.
10. Epand RM. 2003. Fusion peptides and the mechanism of viral fusion. Biochim Biophys Acta 1614:116 –121.https://doi.org/10.1016/S0005 -2736(03)00169-X.
11. Forssmann W-G, The Y-H, Stoll M, Adermann K, Albrecht U, Tillmann H-C, Barlos K, Busmann A, Canales-Mayordomo A, Giménez-Gallego G, Hirsch J, Jiménez-Barbero J, Meyer-Olson D, Münch J, Pérez-Castells J, Ständker L, Kirchhoff F, Schmidt RE. 2010. Short-term monotherapy in HIV-infected patients with a virus entry inhibitor against the gp41 fusion peptide. Sci Transl Med 2: 63re3.https://doi.org/10.1126/scitranslmed .3001697.
12. Jiang X, Jia Q, Lu L, Yu F, Zheng J, Shi W, Cai L, Jiang S, Liu K. 2016. A novel bispecific peptide HIV-1 fusion inhibitor targeting the N-terminal heptad repeat and fusion peptide domains in gp41. Amino Acids 48: 2867–2873.https://doi.org/10.1007/s00726-016-2325-x.
13. Gonzalez E, Ballana E, Clotet B, Esté JA. 2011. Development of resistance to VIR-353 with cross-resistance to the natural HIV-1 entry virus inhibi-tory peptide (VIRIP). AIDS 25:1557–1583.https://doi.org/10.1097/QAD .0b013e328348a733.
14. González-Ortega E, Ballana E, Badia R, Clotet B, Esté JA. 2011. Compen-satory mutations rescue the virus replicative capacity of VIRIP-resistant HIV-1. Antiviral Res 92:479 – 483.https://doi.org/10.1016/j.antiviral.2011 .10.010.
15. Pancera M, Zhou T, Druz A, Georgiev IS, Soto C, Gorman J, Huang J, Acharya P, Chuang G-Y, Ofek G, Stewart-Jones GBE, Stuckey J, Bailer RT, Joyce MG,
Louder MK, Tumba N, Yang Y, Zhang B, Cohen MS, Haynes BF, Mascola JR, Morris L, Munro JB, Blanchard SC, Mothes W, Connors M, Kwong PD. 2014. Structure and immune recognition of trimeric pre-fusion HIV-1 Env. Nature 514:455– 461.https://doi.org/10.1038/nature13808.
16. Papkalla A, Münch J, Otto C, Kirchhoff F. 2002. Nef enhances human immunodeficiency virus type 1 infectivity and replication independently of viral coreceptor tropism. J Virol 76:8455– 8459. https://doi.org/10 .1128/JVI.76.16.8455-8459.2002.
17. Wei X, Decker JM, Liu H, Zhang Z, Arani RB, Kilby JM, Saag MS, Wu X, Shaw GM, Kappes JC. 2002. Emergence of resistant human immunode-ficiency virus type 1 in patients receiving fusion inhibitor (T-20) mono-therapy. Antimicrob Agents Chemother 46:1896 –1905.https://doi.org/ 10.1128/AAC.46.6.1896-1905.2002.
18. Qi Q, Wang Q, Chen W, Du L, Dimitrov DS, Lu L, Jiang S. 2017. HIV-1 gp41-targeting fusion inhibitory peptides enhance the gp120-targeting protein-mediated inactivation of HIV-1 virions. Emerg Microbes Infect 6:e59.https://doi.org/10.1038/emi.2017.46.
19. Lauck M, Switzer WM, Sibley SD, Hyeroba D, Tumukunde A, Weny G, Taylor B, Shankar A, Ting N, Chapman CA, Friedrich TC, Goldberg TL, O’Connor DH. 2013. Discovery and full genome characterization of two highly divergent simian immunodeficiency viruses infecting black-and-white colobus mon-keys (Colobus guereza) in Kibale National Park, Uganda. Retrovirology 10: 107.https://doi.org/10.1186/1742-4690-10-107.
20. Kong R, Xu K, Zhou T, Acharya P, Lemmin T, Liu K, Ozorowski G, Soto C, Taft JD, Bailer RT, Cale EM, Chen L, Choi CW, Chuang G-Y, Doria-Rose NA, Druz A, Georgiev IS, Gorman J, Huang J, Joyce MG, Louder MK, Ma X, McKee K, O’Dell S, Pancera M, Yang Y, Blanchard SC, Mothes W, Burton DR, Koff WC, Connors M, Ward AB, Kwong PD, Mascola JR. 2016. Fusion peptide of HIV-1 as a site of vulnerability to neutralizing antibody. Science 352:828 – 833.https://doi.org/10.1126/science.aae0474. 21. Cavrois M, De Noronha C, Greene WC. 2002. A sensitive and specific
enzyme-based assay detecting HIV-1 virion fusion in primary T lympho-cytes. Nat Biotechnol 20:1151–1154.https://doi.org/10.1038/nbt745. 22. Beyrer C, Pozniak A. 2017. HIV drug resistance: an emerging threat to
epidemic control. N Engl J Med 377:1605–1607.https://doi.org/10.1056/ NEJMp1710608.
23. Tang MW, Shafer RW. 2012. HIV-1 antiretroviral resistance: scientific principles and clinical applications. Drugs 72:e1– e25.https://doi.org/10 .2165/11599900-000000000-00000.
24. Platt EJ, Wehrly K, Kuhmann SE, Chesebro B, Kabat D. 1998. Effects of CCR5 and CD4 cell surface concentrations on infections by macrophag-etropic isolates of human immunodeficiency virus type 1. J Virol 72: 2855–2864.
25. Derdeyn CA, Decker JM, Sfakianos JN, Wu X, O’Brien WA, Ratner L, Kappes JC, Shaw GM, Hunter E. 2000. Sensitivity of human immunode-ficiency virus type 1 to the fusion inhibitor T-20 is modulated by coreceptor specificity defined by the V3 loop of gp120. J Virol 74: 8358 – 8367.https://doi.org/10.1128/JVI.74.18.8358-8367.2000. 26. Venken T, Krnavek D, Münch J, Kirchhoff F, Henklein P, De Maeyer M, High Barrier and Fitness Costs of VIRIP Resistance Journal of Virology
on November 6, 2019 by guest
http://jvi.asm.org/
Voet A. 2011. An optimized MM/PBSA virtual screening approach ap-plied to an HIV-1 gp41 fusion peptide inhibitor. Proteins 79:3221–3235.
https://doi.org/10.1002/prot.23158.
27. Eggink D, de Taeye SW, Bontjer I, Klasse PJ, Langedijk JPM, Berkhout B, Sanders RW. 2016. HIV-1 escape from a peptidic anchor inhibitor through stabilization of the envelope glycoprotein spike. J Virol 90: 10587–10599.https://doi.org/10.1128/JVI.01616-16.
28. Eggink D, Bontjer I, Langedijk JPM, Berkhout B, Sanders RW. 2011. Resistance of human immunodeficiency virus type 1 to a third-generation fusion inhibitor requires multiple mutations in gp41 and is accompanied by a dramatic loss of gp41 function. J Virol 85: 10785–10797.https://doi.org/10.1128/JVI.05331-11.
29. Guenaga J, Garces F, de Val N, Stanfield RL, Dubrovskaya V, Higgins B, Carrette B, Ward AB, Wilson IA, Wyatt RT. 2017. Glycine substitution at helix-to-coil transitions facilitates the structural determination of a sta-bilized subtype C HIV envelope glycoprotein. Immunity 46:792– 803.
https://doi.org/10.1016/j.immuni.2017.04.014.
30. Marozsan AJ, Kuhmann SE, Morgan T, Herrera C, Rivera-Troche E, Xu S, Baroudy BM, Strizki J, Moore JP. 2005. Generation and properties of a human immunodeficiency virus type 1 isolate resistant to the small molecule CCR5 inhibitor, SCH-417690 (SCH-D). Virology 338:182–199.
https://doi.org/10.1016/j.virol.2005.04.035.
31. McNicholas PM, Mann PA, Wojcik L, Qiu P, Lee E, McCarthy M, Shen J, Black TA, Strizki JM. 2011. Mapping and characterization of Vicriviroc resistance mutations from HIV-1 isolated from treatment-experienced subjects enrolled in a phase II study (VICTOR-E1). J Acquir Immune Defic Syndr 56:222–229.https://doi.org/10.1097/QAI.0b013e3181ff63ee. 32. Ogert RA, Wojcik L, Buontempo C, Ba L, Buontempo P, Ralston R, Strizki
J, Howe JA. 2008. Mapping resistance to the CCR5 coreceptor antagonist vicriviroc using heterologous chimeric HIV-1 envelope genes reveals key determinants in the C2-V5 domain of gp120. Virology 373:387–399.
https://doi.org/10.1016/j.virol.2007.12.009.
33. Steger HK, Root MJ. 2006. Kinetic dependence to HIV-1 entry inhibition. J Biol Chem 281:25813–25821.https://doi.org/10.1074/jbc.M601457200. 34. Suntoke TR, Chan DC. 2005. The fusion activity of HIV-1 gp41 depends on interhelical interactions. J Biol Chem 280:19852–19857.https://doi .org/10.1074/jbc.M502196200.
35. Xu L, Pozniak A, Wildfire A, Stanfield-Oakley SA, Mosier SM, Ratcliffe D, Workman J, Joall A, Myers R, Smit E, Cane PA, Greenberg ML, Pillay D. 2005. Emergence and evolution of enfuvirtide resistance following long-term therapy involves heptad repeat 2 mutations within gp41. Antimi-crob Agents Chemother 49:1113–1119.https://doi.org/10.1128/AAC.49 .3.1113-1119.2005.
36. Ray N, Harrison JE, Blackburn LA, Martin JN, Deeks SG, Doms RW. 2007.
Clinical resistance to enfuvirtide does not affect susceptibility of human immunodeficiency virus type 1 to other classes of entry inhibitors. J Virol 81:3240 –3250.https://doi.org/10.1128/JVI.02413-06.
37. Moore JP, Kuritzkes DR. 2009. A pièce de resistance: how HIV-1 escapes small molecule CCR5 inhibitors. Curr Opin HIV AIDS 4:118 –124.https:// doi.org/10.1097/COH.0b013e3283223d46.
38. Chibo D, Roth N, Roulet V, Skrabal K, Gooey M, Carolan L, Nicholls J, Papadakis A, Birch C. 2007. Virological fitness of HIV in patients with resistance to enfuvirtide. AIDS 21:1974 –1977.https://doi.org/10.1097/ QAD.0b013e3282ef1bc8.
39. Menzo S, Castagna A, Monachetti A, Hasson H, Danise A, Carini E, Bagnarelli P, Lazzarin A, Clementi M. 2004. Genotype and phenotype patterns of human immunodeficiency virus type 1 resistance to enfu-virtide during long-term treatment. Antimicrob Agents Chemother 48: 3253–3259.https://doi.org/10.1128/AAC.48.9.3253-3259.2004. 40. van Gils MJ, van den Kerkhof TLGM, Ozorowski G, Cottrell CA, Sok D,
Pauthner M, Pallesen J, de Val N, Yasmeen A, de Taeye SW, Schorcht A, Gumbs S, Johanna I, Saye-Francisco K, Liang C-H, Landais E, Nie X, Pritchard LK, Crispin M, Kelsoe G, Wilson IA, Schuitemaker H, Klasse PJ, Moore JP, Burton DR, Ward AB, Sanders RW. 2016. An HIV-1 antibody from an elite neutralizer implicates the fusion peptide as a site of vulnerability. Nat Microbiol 2:16199.https://doi.org/10.1038/nmicrobiol .2016.199.
41. York J, Berry JD, Ströher U, Li Q, Feldmann H, Lu M, Trahey M, Nunberg JH. 2010. An antibody directed against the fusion peptide of Junin virus envelope glycoprotein GPC inhibits pH-induced membrane fusion. J Virol 84:6119 – 6129.https://doi.org/10.1128/JVI.02700-09.
42. Prabhu N, Prabakaran M, Ho H-T, Velumani S, Qiang J, Goutama M, Kwang J. 2009. Monoclonal antibodies against the fusion peptide of hemagglutinin protect mice from lethal influenza A virus H5N1 infection. J Virol 83:2553–2562.https://doi.org/10.1128/JVI.02165-08.
43. Schindler M, Würfl S, Benaroch P, Greenough TC, Daniels R, Easterbrook P, Brenner M, Münch J, Kirchhoff F. 2003. Down-modulation of mature major histocompatibility complex class II and up-regulation of invariant chain cell surface expression are well-conserved functions of human and simian immunodeficiency virus nef alleles. J Virol 77:10548 –10556.
https://doi.org/10.1128/JVI.77.19.10548-10556.2003.
44. Schindler M, Munch J, Kirchhoff F. 2005. Human immunodeficiency virus type 1 inhibits DNA damage-triggered apoptosis by a Nef-independent mechanism. J Virol 79:5489 –5498.https://doi.org/10.1128/JVI.79.9.5489 -5498.2005.
45. Sanders RW, Moore JP. 2014. A stamp on the envelope. Nature 514: 437– 438.https://doi.org/10.1038/nature13926.
Müller et al. Journal of Virology