“A STUDY ON HAIR DYE CONTACT DERMATITIS-ITS
CLINICAL PRESENTATIONS AND ALLERGENS”
Dissertation Submitted
In Partial fulfillment of the University regulations for
MD DEGREE IN
DERMATOLOGY, VENEREOLOGY AND LEPROSY
(BRANCH XX)
MADRAS MEDICAL COLLEGE
THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY,
CHENNAI INDIA.
CERTIFICATE
It is Certified that this dissertation titled “A STUDY ON HAIR DYE
CONTACT DERMATITIS-ITS CLINICAL PRESENTATIONS AND
ALLERGENS” is a bonafide work done by Dr. SUDHA K, Post graduate
student of the Department of Dermatology, Venereology and Leprosy,
Madras Medical College, Chennai – 3, during the academic year 2016 –
2019. This work has not previously formed the basis for the award of any
degree.
Prof. Dr. U.R. DHANALAKSHMI
MD., D.D., D.N.B.,
Professor and Head
Department of Dermatology Madras Medical College &
Rajiv Gandhi Govt. General Hospital Chennai-3.
Prof. Dr. R. JAYANTHI.,
M.D., F.R.C.P (Glasg)
Dean
DECLARATION
The dissertation entitled “A STUDY ON HAIR DYE CONTACT
DERMATITIS-ITS CLINICAL PRESENTATIONS AND ALLERGENS” is
a bonafide work done by Dr. SUDHA. K at Department of Dermatology,
Venereology and Leprosy, Madras Medical College, Chennai – 3, during the
academic year 2016 – 2019 under the guidance of Prof. Dr. S. NIRMALA
M.D., Professor, Head of Department, Department of occupational and
contact dermatitis, Madras Medical College, Chennai -3.
This dissertation is submitted to The Tamil Nadu Dr. M.G.R. Medical
University, Chennai towards partial fulfillment of the rules and regulations
for the award of M.D Degree in Dermatology, Venereology and Leprosy
(BRANCH – XX)
Prof. Dr. S. NIRMALA, M.D,
Professor and Head of Department
Department of Occupational and Contact Dermatitis Madras Medical College
DECLARATION
I, Dr. SUDHA.K solemnly declare that this dissertation titled
“A STUDY ON HAIR DYE CONTACT DERMATITIS-ITS CLINICAL
PRESENTATIONS AND ALLERGENS” is a bonafide work done by me at
Madras Medical College during 2016-2019 under the guidance and
supervision of Prof. U. R. DHANALAKSHMI, M.D., D.D., D.N.B.,
Professor and Head of Department, Department of Dermatology, Madras
Medical College, Chennai-600003.
This dissertation is submitted to The Tamil Nadu Dr. M.G.R. Medical
University, Chennai towards partial fulfillment of the rules and regulations
for the award of M.D Degree in Dermatology, Venereology and Leprology
(BRANCH – XX).
PLACE :
SPECIAL ACKNOWLEDGEMENT
My sincere thanks to Prof. Dr. R. JAYANTHI., M.D., F.R.C.P
(Glasg) Dean, Madras Medical College, Chennai-3 for allowing me to do
ACKNOWLEDGEMENT
I am grateful to the Professor and Head of the Department of Dermatology,
Prof. Dr. U.R. DHANALAKSHMI, M.D., D.D., D.N.B., for her advice, guidance and encouragement for my study.
I would like to express my sincere and heartfelt gratitude to Prof. Dr. S. KALAIVANI, M.D., D.V., Director and Professor, Institute of Venereology, for her kindness and support throughout the study.
I sincerely thank my guide Prof. Dr. S. NIRMALA M.D., Professor and Head of Department, Department of Occupational and Contact Dermatitis for her valuable support. She has been a source of constant motivation and encouragement throughout the study. I am extremely grateful to her for guiding me throughout the study.
I sincerely thank Prof. Dr. R. PRIYAVATHANI ANNIE MALATHY, M.D., D.D., D.N.B., M.N.A.M.S., Professor of dermatology for her help and support.
I thank Prof. Dr. S. KUMARAVEL, M.D., D.D., Professor of Dermatology for his advice and encouragement.
I thank Prof. Dr. A. RAMESH M.D., D.D., D.N.B., Professor of Dermatology for his advice and encouragement.
I am grateful to Prof. Dr. J. MANJULA, M.D., D.N.B., Professor, Department of Dermatology for her invaluable guidance, help and encouragement.
I thank Prof. Dr. AFTAB JAMEELA WAHAB, MD., D.D., Professor of Dermatology for his advice and encouragement.
I wish to thank Dr. S. VIJAYA BASKAR, M.D., D.C.H., Additional professor, Institute of Venereology for his guidance.
I humbly thank my Co-Guide DR.K. DEEPA M.D.(DVL) Assistant professor, Department of Dermatology for her valuable guidance throughout my work. I would like to express my sincere and heartfelt gratitude for the time which they devoted for my research project.
I also thank my Assistant Professors Dr. P. PRABHAKAR, M.D.D.V.L., Dr. C. VIDHYA, M.D.DVL., Dr.R.HEMAMALINI, M.D.D.V.L., Dr.H.DHANASELVI, M.D.D.V.L., Dr.K.GAYATHRI, M.D.D.V.L., Dr.E.BALASUBRAMANIAN, M.D.D.V.L and Dr.R.SNEKAVALLI M.D.D.V.L., Dr S.TAMILSELVI M.D.D.V.L, Dr T. VANATHI, M.D.D.V.L, Dr. DURGAVATHY, M.D., D.D., Institute of Venereology for their able guidance.
CONTENTS
SL.NO. TITLE
PAGE NO.
1. INTRODUCTION 1
2. REVIEW OF LITERATURE 3
3. AIMS & OBJECTIVES 28
4. MATERIALS AND METHODS 29
5. OBSERVATIONS & RESULTS 35
6. CLINICAL IMAGES
7. DISCUSSION 70
8. CONCLUSION 77
9. BIBLIOGRAPHY
10. ANNEXURES
ABBREVIATIONS
MASTER CHART
KEY FOR MASTER CHART
PROFORMA
INFORMATION SHEET
CONSENT FORM
ETHICS COMMITTEE APPROVAL CERTIFICATE
PLAGIARISM SCREENSHOT
1
INTRODUCTION
Tremendous advancements in this cosmetic world have increased our ability to enhance youth and beauty. The desire for every individual to project a more youthful look, has led to the innovation of various hair coloring products. Various commercially available hair dyes can cause both irritant and allergic contact dermatitis. Allergic contact dermatitis is a delayed type of hypersensitivity reaction manifesting as pruritic dermatitis, which is elicited when the skin meets an allergen to which an individual has been previously sensitized (1). Allergic contact dermatitis (ACD) may clinically present with blisters, oozing, oedema (acute), scaling(subacute), lichenification (chronic). Paraphenylenediamine (PPD), the most common ingredient used in hair dye is the common cause of dermatitis (2). It may involve mainly the scalp and forehead.
2
hypoallergenic dye. A careful history and clinical examination help in identifying allergic contact dermatitis to hair dye. In India, very few studies have been conducted for the demographic profile and for the pattern of clinical presentations of hair dye dermatitis which is mandatory to know the burden of the disease.
3
REVIEW OF LITERATURE
Dyes are colorants which are soluble in water and/or organic solvents, having a particle size of <0.01micrometer with affinity to colour substrates (3). They have been widely used in industrial products, among which hair dyes are the frequently used cosmetics. Hair dyes include a variety of ingredients known to cause allergic contact dermatitis like 2,7 naphthalene diol, 2-aminomethyl-p-aminophenol hydrochloride, 2- chloro-p-phenylenediamine, N-phenyl-p-phenylenediamine, O-aminophenol, p-aminophenol (4). Although many of these agents can cause allergic contact dermatitis, paraphenylenediamine (PPD) remains the most common agent for contact sensitivity (5). Due to its protein binding capacity, low molecular weight and ability to penetrate hair shafts, PPD is an effective constituent in hair dyes (5).
4
CLASSIFICATION OF HAIR DYES:
Based on their chemical composition, hair dyes can be broadly classified into 3 main categories
A) Vegetable hair dyes B) Metallic hair dyes C) Synthetic hair dyes
- Direct hair dyes - Oxidative hair dyes
1. VEGETABLE DYES:
Henna is the only available vegetable hair dye. It is obtained from the dried leaves and stem of Lawsonia intermis. Natural henna gives a brownish orange color. Its active principle is Lawsone (2, hydroxy-1,4 naphthoquinone) (2). Black henna commercially available in recent times is a mixture of natural henna and PPD is added to intensify the color and to decrease the frequency of application (2).
5
2. METALLIC DYES:
Metallic dyes contain metals like lead acetate and salts of bismuth, silver, copper, nickel and cobalt. They give various range of colours. The disadvantage is that they tend to make hair brittle and are used rarely.
3. SYNTHETIC ORGANIC DYES: They are of 2 types- direct and oxidative (11).
A) Direct hair dyes include - temporary and semi-permanent dyes. B) Oxidative dyes include - permanent dyes.
BASED ON PERSISTENCE OF COLOR CLASSIFIED AS: 1. Temporary
2. Semi-permanent 3. Demi-permanent 4. Permanent
1. TEMPORARY – contains pigments which are of high molecular weight and therefore cannot penetrate the cuticle layer.
2. SEMIPERMANENT – contains no or little developer (hydrogen peroxide and ammonia), less damaging to hair strands, contains low molecular weight pigments than temporary dyes, enters the hair shaft partially.
6
4. PERMANENT – contains ammonia, mixed with a developer or oxidizing agent. Duration of contact – 30- 45 mins.
CHEMICAL COMPOSITION OF PERMANENT HAIR DYE:
The process of hair coloring in permanent hair dye involves mixing of two components-
a) Precursor along with coupler b) Oxidizing agent.
Precursors/primary intermediates:
Belong to aryl amine groups, includes phenylenediamine (PPD), para-toluene diamine (PTD), ortho-aminophenol, Para-aminophenol.
Coupler:
They are meta-substituted derivative of aniline. Based on the colour they produce, they can be divided into,
1. blue coupler – 1,3 diaminobenzenes and its derivatives 2. red coupler – phenols and naphthol’s
7
Formation of hair colour involves three steps: STEPS:
First step - Oxidation of p-phenylenediamine to the quinonimines (C6H4(NH)2):
Second step - Involves the attack of this quinonimines on the coupler. In organic chemistry, this reaction is called electrophilic aromatic substitution:
Third and final step - The product from the quinonimines-coupler reaction oxidizes to the final hair dye.
The dye formed in the above reaction bonds to hair permanently. The main reason for a permanent colour on hair is by producing larger dye molecules, which is locked inside the hair.
ROLE OF AMMONIA IN HAIR DYE:
Ammonia is generally used in permanent hair dyes which must be mixed with a developer or an oxidizing agent to obtain the permanent change of colour. It is an alkaline agent which opens up the cuticle layer and facilitates the penetration of both developer and colorants together into the cortex (13). Semi-permanent dyes contain ethanolamine and sodium carbonate for an alkaline pH.
ANATOMY OF HAIR SHAFT AND THE SCIENCE BEHIND COLORING PRODUCTS:
8
1. Hair shaft cuticle – made up of thin flat keratinocytes. Forms a protective barrier around the entire hair shaft.
2. Hair shaft cortex – gives shape and support to the hair structure, as it contains bundles of keratin fibres, arranged in a vertical rod like fashion. 3. Hair shaft medulla – air filled space at the Centre of the shaft which has
no known biological function.
Hair colour is attributed to the presence of melanin in the keratinocytes of the cortex (14).
Modification of hair colour can be obtained by two methods: 1. Removal of melanin pigment in cortex via bleaching 2. Addition of artificial pigment present in hair dye
Temporary dyes weakly adhere to the cuticle, but do not penetrate the cortex. This adherence is via van der Waals forces (weak attractions between atoms, molecules and surfaces due to change in polarizations of nearby particles)(15). As they only coat the hair, they are easily washed off by single shampooing.
Permanent dyes pass through the cuticle, penetrate deeper into the shaft and gets deposited completely into the cortex, by forming covalent and ionic bonds. They are colourless and undergoes oxidation to give various shades of brown to black colour (16).
9
DIFFERENCES BETWEEN PERMANENT AND SEMIPERMANENT DYES:
TEMPORARY /
SEMI-PERMANENT DYES PERMANENT DYES
1. Washed off easily after
shampooing (once in temporary,4 to 12 shampoos in
semi-permanent).
1. Not easily removed by shampooing
2. These are direct dyes and requires no chemical reactions to give color
2. These are colorless precursors and require an oxidizing agent to give color.
3. Contains alkalizing agent other than ammonia like monoamine ethanolamine and sodium carbonate.
3. Contains ammonia as alkalizing agent.
4. Hydrogen peroxide concentration is lower than in permanent
counterpart.
4. Hydrogen peroxide concentration is higher.
5. Less damaging to hair 5. More damaging to hair 6. Alkalizing agents are less effective
in removing the natural pigment of hair and therefore they cannot give a lighter shade.
6. Alkalizing agent removes the natural pigment of hair effectively.
Role of developers:
Hydrogen peroxide in developers serves the following functions,
1. It causes swelling of hair cuticle and thereby allows diffusion of precursors (colourless) into the hair cortex.
2. Bleaches the natural melanin pigment.
10
EPIDEMIOLOGICAL PROFILE:
PPD has been considered as an important allergen to produce contact dermatitis for many decades. It can cause acute, subacute and chronic dermatitis. The median prevalence of PPD positivity among dermatitis patients was found to be 4.3% in Asia,4% in Europe and 6.2% in North America (17,18,19). The sensitization prevalence to PPD ranged between 2% and 12%. It was observed that the prevalence was relatively higher in Asian men than in women. This could be due to frequent dyeing of facial hair than scalp hair in men, thereby increasing the risk of sensitization. In a study, it was reported that there was fourfold rise in PPD prevalence over the last decade (20). Allergic contact dermatitis occurs in only small proportion of patients who are already sensitized, the prevalence varying from 1.7% to 6% (21)(22). But, the true incidence in a community is very difficult to be estimated because its diagnosis depends on several factors like demography, index of suspicion of the physician, availability of patch testing etc. The key stone in the management and prevention of allergic contact dermatitis lies in the early diagnosis of ACD and identification of the culprit allergen.
11
Epidemiological studies to assess the adverse effects of hair dyes could not be specifically summarized, since people indulge in various occupations like Hair dressers, barbers, cosmetic persons use multiple products during work. In a review by Khumalo et al, prevalence of contact dermatitis was seen in up to 80% of hair dressers in smaller studies and 16.4% in larger studies (26). The most common presentation was Hand dermatitis which may be not only due to sensitizing and irritant effects of hair dye ingredients, but also due to unsafe packaging, inadequate protection and ignorance of safe handling of these chemicals (26).
PATHOGENESIS OF CONTACT DERMATITIS TO HAIR DYE:
Hair dye can cause both irritant and allergic contact dermatitis. Irritant dermatitis is characterized by damage to cutaneous integrity with epidermal lesions varying in severity and inflammation in underlying dermis. There is no prior sensitization or immunological reactions needed in irritant contact dermatitis. CD may be acute or chronic. In chronic ICD, barrier function is disturbed and in acute ICD mediators like TNF-α.IL-1, IL-6, IL-8, IFN-γ, IL-2 AND GM-CSF are involved.
12
ACD consists of two distinct phases: 1. Induction or sensitization phase 2. Elicitation phase.
Induction phase: an allergen (hap ten) penetrates the epidermal layer, picked up and processed by an antigen presenting cell. Most allergens in ACD requires minimal processing as they are of low molecular weight. The processed antigen is presented to T lymphocytes present in lymph nodes which gets differentiated into memory and effector T lymphocytes. These are released into the blood stream. When the same individual is exposed to the same antigen, he develops elicitation phase. The resultant inflammatory reaction develops clinically in 24-48 hrs. Activated keratinocytes present antigen to the specific memory T cells in the epidermis and elicit a rapid inflammatory response. Once acquired, sensitivity persists. activated keratinocytes secrete IL-1 and express HLA DR on their surface and augments the function of Langerhans cells.
CLINICAL FEATURES:
13
who use hair dyes for beard and moustache, lesions occur over the face, neck, upper chest, upper arms or rarely it may be generalized. Various other presentations are air borne contact dermatitis like picture (involving eyelids, retro auricular folds and flexures especially cubital fossa), prurigo like lesions on extremities (in severe cases).
Most commonly young to middle aged individuals are affected. It has also been reported that Allergic contact dermatitis to hair dye occurs in children, though rare in the age group of 12-15 years (28). This is due to sensitization after temporary henna tattoos exposure. Adverse effects of hair dye can rarely present as non-eczematous conditions like lymphomatoid contact dermatitis to PPD containing hair dye (29) and body dysmorphic syndrome (30).
Jain et al, in his study using 200 hair dye users has concluded that hair dye is toxic to human lens and this observation was confirmed on animal experiments (31).
I t has been found that long term PPD exposure has been associated with renal impairment (20). In one study conducted by Hamdouk in a group of 72 hairdressers, it was found 14% had renal impairment, 26.4% had proteinuria and 41.1% had hematuria. It can also lead to hypertension, skin changes and bronchospasm (32).
14
sensitizers causing contact dermatitis (CD) (34). In India, in recent times permanent hair dyes had arouse as a major cause of suicidal poisoning (35). Such poisoning usually presents with severe rhabdomyolysis, cervico- facial oedema and renal failure. Studies conducted in recent times shows positive associations of hair dye use to various malignancies like bladder cancer, leukaemia, myelo-dysplastic syndromes (23).
EVALUATION: PATCH TEST:
Patch test was introduced by Joseph Jadassohn in 1896.
For irritant contact dermatitis:
Para-phenylene diamine, the main ingredient found in many permanent and some semi-permanent hair dyes would cause irritant contact dermatitis as well. Patch testing containing PPD allergen can be tried to identify the cause.
For allergic contact dermatitis:
15
immune response in an already sensitized individual by applying defined concentration of suspected allergen and evaluating the degree of response. A positive reaction to patch test confirms that the person has allergic contact dermatitis.
16
INDICATIONS OF PATCH TEST:
1. Eczematous disorders where contact allergy is suspected or is to be excluded.
2. Eczematous disorders failing to respond to treatment as expected 3. Chronic hand and foot eczema
4. Persistent or intermittent eczema of the face, eyelids, ears and perineum. 5. Stasis eczema
Patch test is used to investigate drug reactions like drug rash, eosinophilia and systemic symptoms (DRESS), maculopapular rash and fixed drug eruption (FDE) (40).
Before application, patient should be informed of 1) test objectives 2) avoiding wetting the test site3) avoiding activities causing excessive sweating 4) local symptoms like itching 5). Patients should be instructed not to be exposed to sun or other sources of UV light.
17
Battery or series and types of chambers:
Indian battery series 1 and 2(ISB 1&2) were used for patch testing in our centre.
The allergens used in the series are prepared with better penetration and without local irritant side effects. Each allergen is prepared in a suitable vehicle and the most commonly used is petrolatum. This allows good occlusion, has low cost and keeps the allergens stable. Other vehicles that could be used are water, solvents (acetone, ethanol, methylethylacetone) and hydrophilic gel. When the allergens are in liquid form filter papers are used while testing.
PATCH TEST CHAMBERS: Finn chambers:
18
Durat et al study shows substances with same chemical structure cross react and should not be tested next to each other (41). In the battery series, substances are kept in an order according to their chemical structures to avoid cross reactivity and co sensitization (42). After application, adhesive tapes can be used to prevent detachment due to increased sweating and false negative results(43).
19
ANTIGENS USED IN INDIAN BATTERY SERIES: 1. Vaseline
2. Wood alcohol 3. Balsam of Peru 4. Formaldehyde
5. Mercaptobenzothiazole 6. Potassium bichromate 7. Nickel sulphate
8. Cobalt sulphate 9. Colophony 10.Epoxy resin
11.Paraben mix
12.Para-phenylenediamine 13.Parthenium
14.Neomycin sulphate 15.Benzocaine
16.Chlorocresol 17.Fragrance mix 18.Thiuram mix 19.Nitrofurazone 20.Black rubber mix
READINGS AND INTERPRETATION:
ICDRG (international contact dermatitis research group scoring system)
- Negative
?+ doubtful Faint erythema only
+ Weak positive Palpable erythema, infiltration, possibly papules ++ Strong positive Erythema, infiltration, papules, vesicles
+++ Extremely positive Intense erythema, infiltration and coalescing vesicles
20
FALSE POSITIVE REACTIONS:
• Excessive concentration of allergen • Contaminants
• Irritant vehicle
• Recent dermatitis at patch test site • Presence of dermatitis at distant sites • Adhesive tape reactions
• Artefacts
• Angry back reaction- recent dermatitis at the test area or even other areas lowers the threshold for irritant reactions and causes nonspecific irritant reactions. Also called excited skin Syndrome.
FALSE NEGATIVE RESULTS:
21
Insufficient concentration of allergen
Improper adhesion of patch
Readings done too early
Pretreatment at the patch test site with topical steroids
UV exposure of patch test site and if the patient is on immunosuppressants
COMPLICATIONS OF PATCH TEST:
Pruritus
Folliculitis
Flare of dermatitis
Irritant reactions due to inappropriately diluted allergen
Sensitization
Hyper or hypo pigmentation
Scarring and anaphylaxis
OPEN TEST:
22
SEMI-OPEN TEST:
This method is designed to evaluate substances with irritating properties like detergents, shampoos, dyes, glues, pharmaceuticals and cosmetics. A small amount of the substance is applied to 2*2cm area. After it is dried completely, the area is covered with adhesive tape for 2 days. The site is read after 48 and 96 hours.
REPEATED OPEN APPLICATION TEST (ROAT):
ROAT was first described by Hannuksela and Sato in 1986.It is used to refine the positive, negative or doubtful responses, obtained in the closed test (46). Suspected commercial products (cosmetics or drugs), are applied twice a day for 7 days to sites like anterior portion of arm, antecubital fossa or scapular region. Positive response in 2-4 days indicates presence of sensitizing substance.
PHOTO PATCH TEST:
23
PATCH TESTS IN SPECIAL SITUATIONS: Patch tests in patients using immunomodulatory drugs:
The frequency of positivity for drug reactions varies from 7.5 to 54%, according to different studies, the patients selected, type of rash and drug involved (47).
In 2008, Rosmarin et al. described allergic contact dermatitis in hands in patients using
Anti-TNFα. The authors patch tested the patient and found positive results to various substances (48). Wee et al. patch tested 38 patients using different immunosuppressive drugs. Among them, 16 (44%) tested positive with intensity varying between (+) and (+ + +) (49).
Patch tests in children:
The most affected areas are the extremities and the most common allergens are metals, footwear, topical medication and cosmetics. The size of the child's back does not allow the placement of many allergens. The use of chambers designed at present is well established in this age group (50).
24
COMPOUND ALLERGY:
Compound allergy refers to the condition where patch test is positive when done with a finished product but when patch tested with individual ingredients, it turns out to be negative. So, the finished product and its constituents should be patch tested if there is a strong suspicion.
QUENCHING:
This phenomenon is investigated mostly in fragrance material aldehyde. A combination of chemicals may lead to a quenching effect, as there may be potentiation of allergic and irritant responses. It may be due to one of the compounds having anti-inflammatory properties like triclosan having quenching effect on nickel ACD.
MULTIPLE PATCH TEST REACTIONS:
This is a quite common and may be due to non- specific hyperreactivity, multiple primary hypersensitivities and cross-reactions (true and false). Cross reactions is the phenomenon where sensitization to one primary compound (primary allergen), extends to one or more compounds (secondary allergen) as a result of similarity in structure.
Chemicals that cross react with PPD:
25
CHEMICAL PRODUCT
Para-aminobenzoic acid Sunscreens
Sulfonamides, sulfonylureas Medications
Para-toluene diamine sulfate Semi-permanent hair dyes
Azo dyes Clothes, ballpoint pen ink, shoes
Benzocaine, tetracaine, procaine Local anesthetics Para-amino salicylic acid Antibiotics
IN VITRO TEST:
Lymphocyte activation test (LAT) – described by Kneiling et al. Titrated amount of PPD with IL-2 supplementation are cultured with freshly isolated peripheral blood mononuclear cells. Proliferation of cells determined by minimum of three-and-a-half-fold raise in the uptake of [3H]-thymidine added to it confirms the individual is allergic to PPD.
COMPLICATIONS:
26
MANAGEMENT: General measures:
avoidance of hair dye product causing dermatitis.
In case of acute dermatitis, hair is washed thoroughly with soap less shampoo to remove excess hair dye.
Frequent application of emollients
In acute stage, saline compresses help in anti-pruritic action, reducing oozing and removal of crust.
Potassium permanganate soaks in severe infected lesions.
Systemic antibiotics will be needed if secondary bacterial infection occurs
Avoidance of over the counter topical preparations as they may contain irritants like alcohol and propylene glycol
Those who manifest with photosensitivity must be advised about regular use of sunscreens over sun exposed areas. Additional protection by using appropriate clothing’s and wide brim hats are to be advised.
Usage of topical steroids in lotion formulation gives symptomatic relief. Super potent steroids in face and prolonged usage of steroids are better avoided. Short course of systemic steroids are used in severe cases
systemic anti -histamines may be required to alleviate itching.
People should inform their hair dressers about their allergy.
27
In case of occupational exposure, wearing of protective garments like sleeved clothes, protective gloves.
PPD free alternative hair dyes:
28
AIMS & OBJECTIVES
STUDY OBJECTIVES:
29
MATERIALS & METHODS
STUDY DESIGN
PROSPECTIVE STUDY
STUDY PLACE
Department of occupational and contact dermatitis Madras medical college
Chennai
STUDY PERIOD
June 2017 to May 2018
ELIGIBILITY
INCLUSION CRITERIA
1. Patients attending or referred to occupational and contact dermatoses OPD with a clinical suspicion of contact dermatitis to hair dye.
2. All patients with more than 18 years of age.
EXCLUSION CRITERIA
1. Patients less than 18 years of age. 2. Pregnant women
30
METHODOLOGY
This study was carried out as a clinical, epidemiologic and etiological survey of hair dye contact dermatitis from June 2017 to May 2018.
The sampling procedure is summarized as follows.
I. All patients attending occupational and contact dermatitis outpatient department having signs and symptoms of hair dye contact dermatitis between the study period are selected for the study as per the criteria mentioned above and enrolled in the study.
II. The sample size for the study 43.
III. All the subjects were interviewed in person.
IV. Detailed case history of each patient with reference to a. Age
b. Sex
c. Duration and course of the disease d. Type of work
e. Address
f. Educational Status
g. Age at which first used Hair dye h. Type of Hair Dye Used
31
V. One of the senior and experienced professors helped to exclude conditions like psoriasis, lichen planus and dermatophytosis clinically.
VI. Symptomatology assessment
Symptoms like itching, watery discharge, burning sensation and signs, sites of involvement, morphology of lesions like oozing, scaling, crusting, vesicles, hyperkeratotic, discoid lesions, pigmentation and history of other skin. The presence of associated skin findings of atopy was noted.
VII. Risk factor assessment
VIII. History of endogenous factors like atopy is noted.
IX. History of exogenous factors like hair dye application is noted. X. PATCH TEST
Patch test was done for all patients with kit containing Indian standard series which is approved by contact and occupational dermatosis forum of India and has twenty allergens.
Patient ‘s upper back was chosen for application of patch test
Before patch testing once again it was confirmed whether the patient is on systemic steroids or other immunosuppressants.
The patch made of non-allergenic, non-irritant, non-occlusive tape and aluminum chambers named as Finn chamber.
32
The kit is available as two strips with each strip containing two columns of antigen of five each.
These two strips with the allergens were stuck to the patient’s upper back
The antigens are numbered over the adhesive plaster with an indelible ink
The corners of the patch were also marked on all the four sites which would give us an idea whether the patch was displaced or not.
The patients were advised not to take shower for the duration of test, and avoid activities like exercise which would induce sweating and dislodge the patches
The patients were advised not to expose the patches to sun or other sources of UV light.
The patients were asked to come after 48 hours for reading
The patches were removed and patient is made to wait for next one hour for the erythema and edema developed due to pressure of the strips to subside
After removal of the patches, allergens are numbered over the body as their positions cannot be distinguished once the pressure effects have subsided
33
- Negative
?+ Doubtful, Faint erythema only
+ Weak positive reaction
Palpable erythema, infiltration and papules ++ Strong positive reaction
Erythema, infiltration, papules and vesicles
+++ Extreme positive reaction. Intense erythema, infiltration and coalescing vesicles
IR Irritant reaction NT Not tested
True allergic reactions were distinguished from irritant reaction by presence of itching and infiltration, extension beyond the margins
The patch test readings are noted and the person is advised to avoid the particular allergen
Patients were advised skin care and importance of regular application of emollient
Patients were advised protection measures like wearing gloves according to the occupation.
Patients were given appropriate treatment according to disease severity
34
STATISTICAL ANALYSIS
The collected data was entered for analysis in Microsoft Excel. This data was exported to Statistical Package for Social Sciences software (SPSS) version 22.0. Mean, standard deviations and range were employed to describe continuous variables, while frequency distributions were obtained for dichotomous variables.
ETHICAL ISSUES
All the Participants were made aware about the nature and purpose of the study.
It was also informed to all the participants that all data provided by the patients were kept confidential and will be used only for the study purpose.
Willingness and signature of the participants was taken on a previously designed consent form.
Written consent was obtained from all the subjects who participated in the study before data are collected.
Detailed description of the study and the aspects of patient confidentiality were explained to the subject and voluntary participation is sought.
35
RESULTS
Table 1: Age distribution of the study subjects (n=44)
Age group Frequency
N
Percent %
31 - 40 years 8 18.2
41 - 50 years 20 45.5
51 - 60 years 16 36.4
Total 44 100.0
Mean (± S.D) Age: 48.55 ± 7.02 years
Minimum: 34 years Maximum: 60 years
[image:49.595.125.492.506.752.2]Comments: About 63% of the subjects were aged between 31 to 50 years while the remaining were aged more than 50 years.
Fig 1: Age distribution of the study subjects (n=44)
18%
46% 36%
36
Table 2: Gender distribution of the study subjects (n=44)
Group Frequency
N
Percent %
Female 13 29.5
Male 31 70.5
Total 44 100.0
Comments: About 70% of the subjects were males.
Fig 2: Gender distribution of the study subjects (n=44)
30%
70%
37
Table 3: Distribution of the study subjects according to locality (n=44)
Locality Frequency
N
Percent %
Rural 9 20.5
Urban 35 79.5
Total 44 100.0
Comments: About 80% of the subjects were from urban locality.
Fig 3: Distribution of the study subjects according to locality (n=44)
20%
80%
38
Table 4: Distribution of the study subjects according to occupation (n=44)
Occupation Frequency
N
Percent %
Professional 1 2.3
Semi-professional 1 2.3
Clerk/shop owner 8 18.2
Housewife 9 20.5
Skilled 13 29.5
Semi-skilled 4 9.1
Unskilled 8 18.2
Total 44 100.0
Comments: About 30% of the subjects were skilled workers while 20% of the subjects were housewives and 18% were unskilled workers.
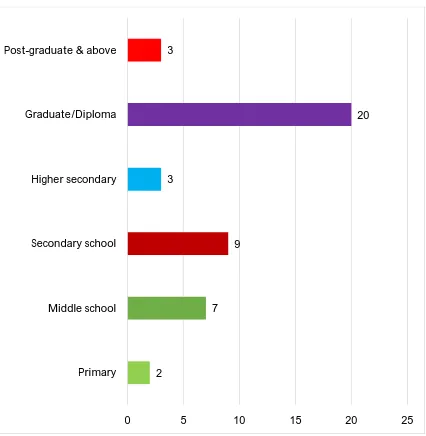
Table 5: Distribution of the study subjects according to education (n=44)
Education Frequency
N
Percent %
Primary 2 4.5
Middle school 7 15.9
Secondary school 9 20.5
Higher secondary 3 6.8
Graduate/Diploma 20 45.5
Post-graduate & above 3 6.8
Total 44 100.0
[image:52.595.80.534.464.680.2]39
Fig 4: Distribution of the study subjects according to education (n=44)
2
7 9 3
20 3
0 5 10 15 20 25 Primary
40
Table 6: Distribution of the study subjects according to previous history of contact dermatitis (n=44)
Previous history
Frequency N
Percent %
Present 3 6.8
Absent 41 93.2
Total 44 100.0
[image:54.595.93.514.493.748.2]Comments: Only about 7% of the subjects had previous history of contact dermatitis.
Fig 5: Distribution of the study subjects according to previous history of contact dermatitis (n=44)
7%
93%
41
Table 7: Distribution of the study subjects according to duration of contact dermatitis (n=44)
Duration
Frequency N
Percent %
<1 month 25 56.8
1m to 1 year 14 31.8
>1 year 5 11.4
Total 44 100.0
[image:55.595.102.517.190.517.2]42
Fig 6: Distribution of the study subjects according to duration of contact dermatitis (n=44)
25
14
5
0 5 10 15 20 25 30
Frequency
43
Table 8: Distribution of the study subjects according to duration of dye usage (n=44)
Duration of dye use
Frequency N
Percent %
<1 year 10 22.7
1 to 5 years 21 47.7
6 to 10 years 9 20.5
>10 years 4 9.1
Total 44 100.0
Mean (± S.D) duration of dye use: 5.38 ± 4.0 years Minimum: 2 months maximum: 30 years
44
Fig 7: Distribution of the study subjects according to duration of contact dermatitis (n=44)
10
21
9
4 0
5 10 15 20 25
Frequency
45
Table 9: Distribution of the study subjects according to brand of dye (n=44)
Dye brand
Frequency N
Percent %
Black henna 4 9.1
Black rose 12 27.3
Godrej 21 47.8
Garnier 3 6.8
Indica 8 18.2
Supervasmol 3 6.8
V care 1 2.3
46
Table 10: Distribution of the study subjects according to frequency of dye application (n=44)
Frequency of dye use Frequency N
Percent %
Weekly once 3 6.8
Once in 2 weeks 5 11.4
Once in 3 weeks 3 6.8
Once in a month 18 40.9
Once in 2 months 10 22.7
Once in 3 months 5 11.4
Total 44 100.0
47
Fig 8: Distribution of the study subjects according to frequency of dye application (n=44)
3 5 3
18 10
5
0 5 10 15 20
48
Table 11: Distribution of the study subjects according to quantity of dye application (n=44)
Quantity of dye used Frequency N
Percent %
10 ml 5 11.4
15 ml 2 4.5
20 ml 16 36.4
25 ml 2 4.5
30 ml 19 43.2
Total 44 100.0
49
Fig 9: Distribution of the study subjects according to quantity of dye application (n=44)
5 2
16 2
19
0 5 10 15 20
50
Table 12: Distribution of the study subjects according to previous history of reaction after dye application (n=44)
Reaction after dye use
Frequency N
Percent %
No 25 56.8
Itching/ Pruritis 17 38.7
Raised lesion/pain/darkening of skin 2 4.5
Total 44 100.0
51
Table 13: Distribution of the study subjects according to co-morbidities (n=44)
Co-morbidities*
Frequency N
Percent %
Diabetes mellitus 7 15.9
Hypertension 2 4.6
Cataract 1 2.3
Hypertrophic LP/Prurigo nodularis 1 2.3
Trigeminal neuralgia 1 2.3
Pityriasis capitis 1 2.3
Facial melanosis 1 2.3
Acanthosis Nigricans 1 2.3
No comorbidities 33 75
* Not mutually exclusive
52
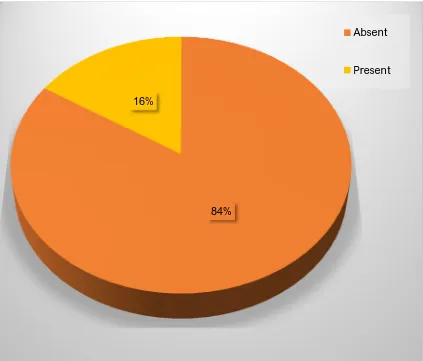
Table 14: Distribution of the study subjects according to history of atopy (n=44)
History of atopy Frequency N
Percent %
Absent 37 84.1
Present 7 15.9
Total 44 100.0
53
Fig 10: Distribution of the study subjects according to history of atopy (n=44)
84% 16%
54
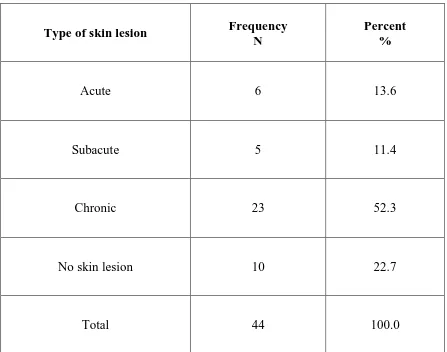
Table 15: Distribution of the study subjects according to type of skin lesion (n=44)
Type of skin lesion Frequency N
Percent %
Acute 6 13.6
Subacute 5 11.4
Chronic 23 52.3
No skin lesion 10 22.7
Total 44 100.0
[image:68.595.86.533.196.548.2]55
Fig 11: Distribution of the study subjects according to type of skin lesion (n=44)
0 5 10 15 20 25
Acute Subacute Chronic No skin lesion
6 5
23
[image:69.595.95.537.218.567.2]56
Table 16: Distribution of the study subjects according to clinical pattern of skin lesion (n=44)
Clinical pattern of skin lesion Frequency N
Percent %
Localized contact dermatitis (scalp and scalp
margins) only 10 22.7
Face (beard, periorbital) and neck 8 18.2
Localized contact dermatitis + Face (beard,
periorbital) and neck involvement 21 47.7
Hands and feet 1 2.3
Air-borne contact dermatitis (ABCD) pattern 3 6.8
Miscellaneous patterns 1 2.3
Total 44 100.0
[image:70.595.89.535.190.647.2]57
Table 17: Distribution of the study subjects according to morphology of skin lesion (n=44)
Morphology of skin lesion Frequency N
Percent %
No skin lesion 10 22.7
Multiple skin coloured papules with or without
erythema 3 6.8
Hyper-pigmented macules 5 11.4
Hyper-pigmented papules 11 25
Hyper pigmented/scaly plaques with or without
erythema 9 20.5
Urticarial plaque 1 2.3
Lesions with Crusted erosions/oozing/Fissuring 4 9.1
Hyper pigmented patch 9 20.5
Depigmented macules/papules/Leukoderma 1 2.3
Hypo-pigmented patch 2 4.6
Seborrheic melanosis 1 2.3
Angioedema 1 2.3
58
Table 18: Distribution of the study subjects according to patch test result (n=44)
Patch test Frequency
N
Percent %
Positive* 39 88.6
Negative 3 6.8
Reading not taken
(patient not returned) 2 4.6
Total 44 100.0
*1 subject had allergic contact dermatitis to tape
[image:72.595.88.532.180.521.2]59
Fig 12: Distribution of the study subjects according to patch test result (n=44)
89% 7%
4%
[image:73.595.85.528.210.562.2]60
Table 19: Distribution of the study subjects according to patch test result for PPD (n=42)
Patch test for PPD Frequency N
Percent %
Negative 5 11.9
1+ 17 40.5
2+ 5 11.9
Pigmentation 14 33.3
Pigmentation and 1 + 1 2.4
Total 42 100.0
61
Fig 13: Distribution of the study subjects according to patch test result for PPD (n=42)
0 5 10 15 20
Negative 1+ 2+ Pigmentation Pigment and 1 +
5
17 5
[image:75.595.96.538.182.611.2]62
Table 20: Distribution of the study subjects according to patch test result for parthenium (n=42)
Patch test for parthenium Frequency N
Percent %
Negative 38 90.5
1+ 3 7.1
3+ 1 2.4
Total 42 100.0
63
Table 21: Distribution of the study subjects according to patch test result for Benzocaine (n=42)
Patch test for Benzocaine Frequency N
Percent %
Negative 38 90.5
1+ 3 7.1
Doubtful 1 2.4
Total 42 100.0
64
Table 22: Distribution of the study subjects according to patch test result for Colophony (n=42)
Patch test for Colophony Frequency N
Percent %
Negative 38 90.5
1+ 3 7.1
Doubtful 1 2.4
Total 42 100.0
65
Table 23: Distribution of the study subjects according to patch test result for Fragnance mix (n=42)
Patch test for Fragnance mix Frequency N
Percent %
Negative 32 76.2
1+ 10 23.8
Total 42 100.0
66
Table 24: Distribution of the study subjects according to patch test result for Epoxy resin (n=42)
Patch test for Epoxy resin Frequency N
Percent %
Negative 37 88.1
1+ 3 7.1
Doubtful 2 4.8
Total 42 100.0
67
Table 25: Distribution of the study subjects according to patch test result for Mercaptothiazide (n=42)
Patch test for Mercaptothiazide Frequency N
Percent %
Negative 38 90.5
1+ 1 2.4
Doubtful 3 7.1
Total 42 100.0
68
Table 26: Distribution of the study subjects according to patch test result for other antigens (n=42)
Patch test Antigen Result Frequency N
Percent %
Nickel 1+ 3 7.1
Nitrofurazone 1+ 2 4.8
Chlorocresol 1+ 1 2.4
Neomycin
Doubtful 1 2.4
1+ 1 2.4
Cobalt sulphate 1+ 1 2.4
Balsam of Pern 1+ 2 4.8
Black rubber Mix 1+ 2 4.8
Paraben mix 1+ 1 2.4
Potassium bichromate 1+ 3 7.1
69
Table 27: Distribution of the study subjects according to patch test result and gender (n=42)
Patch test Antigen Total positives
Female (n=12) N (%)
Male(n=30) N (%)
PPD 37 11 (91.7) 26 (86.7)
Fragnance mix 10 3 (25) 7 (23.3)
Epoxy resin 5 0 5 (16.7)
Parthenium 4 1 (8.3) 3 (10)
Benzocaine 4 1 (8.3) 3 (10)
Colophony 4 0 4 (13.3)
Mercaptothiazide 4 2 (16.6) 2 (6.7)
Potassium bichromate 3 - 3 (10)
Nickel 3 2 (16.6) 1 (3.3)
Neomycin 2 1 (8.3) 1 (3.3)
Nitrofurazone 2 1 (8.3) 1 (3.3)
Balsam of Pern 2 1 (8.3) 1 (3.3)
Black rubber Mix 2 0 2 (6.7)
Chlorocresol 1 0 1 (3.3)
Paraben mix 1 0 1 (3.3)
Fig 1 : Papules over the neck
Fig 3 : Hyperpigmented papule over nape of neck
[image:86.595.203.415.351.672.2]Fig 5 : Patch test applied
Fig 8a : 1+ for fragrance mix Fig 8b : Pigmentation in
[image:88.595.109.509.70.352.2]and thiuram mix patch test for PPD
Fig 10 : 1+ for parthenium
70
DISCUSSION
Demographic variables:The mean age in the current study was 58.5 years with an SD of 7 years. The minimum age was 34 years while the maximum was 60 years.
This is similar to the mean age of 58.7 years with an SD of 9.6 years as observed in a study by Lee et al (53) with an objective to evaluate the safety of 15 commercial hair dye products by studying patch test results with commercial hair dye products in patients with allergic contact dermatitis to para-phenylenediamine. The mean age was slightly lower than one observed by Gupta et al (54) study (on 80 patients suspected to have contact allergy from hair dye using the patch test with Indian Standard series including PPD) as the mean age was 62 years ranging from 17 years to 74 years. The current study finding of 63% of the subjects between the age of 31 and 50 years is comparable to 42 % of the patients between 26 to 40 years as reported by Sadagopan et al (55). However the mean age in this study was much higher than 27.5 years as reported by Tomar et al (56).
71
About 80% of the subjects in the current study were from urban locality while Gupta et al (54) observed 58 % were from rural background and 42% were from urban background.
About 52% of the subjects were graduates or postgraduates while 27% of the subjects had Secondary School Education.
Occupation plays an important role in exposure and sensitization to allergens and in the current study, 30% of the subjects were skilled workers while 20% of the subjects were housewives and 18 % were unskilled workers. Gupta et al(54) observed 57% of the males were skilled workers while 19 % were shopkeepers and 91% of the females were housewives and the remaining being students. Tomar et al (56) reported that 46 % of the subjects where students followed by 18 % housewife and 10% were teachers.
72
Roughly about 70% of the subjects were using hair dye for a duration ranging from one year to 5 years. According to Gupta et al (54), 14% where using the dye for less than a month whereas 21% were using the dye for more than 3 years and 52% of the subjects were using the dye for a duration ranging from one month and one year.
Regarding the brand of hair dye in the current study, 48% of the subjects were using Godrej while 27% were using black rose. About 41 percent of the subjects were using hair dye once in a month while 15 % were using once in a week or once in a fortnight. About one-third (37%) of the subjects were using 20 ml of the dye after reconstitution per session while 43% of subjects were using 30ml for each session.
More than one-third (39%) of the subjects had Itching/ pruritis immediately after application of hair dye. About 16% of the subjects had Diabetes mellitus while 5% had hypertension and one subject is reported cataract, Trigeminal Neuralgia, acanthosis nigricans, facial melanosis, and prurigo nodularis. Regarding the history of atopy, 84% of the subjects had a positive history while 16 % reported negative history.
Clinical pattern:
73
periorbital) and neck. Only scalp and scalp margins were involved in localised contact dermatitis in about 22.7 % of the patients. Skin lesions involving face and neck including the periorbital area was observed in 18.2 % of the cases. Airborne contact dermatitis was observed in about 7 % of the patients while involvement of only hands and feet was observed in one subject. These findings can be corroborated with findings of Gupta et al (54) such as the most common presentation of the contact dermatitis was localized to scalp and scalp margins followed by dermatitis of face and neck and hands and feet. Airborne contact dermatitis was observed in 9 subjects. According to Tomar et al (56), the most commonly involved site for the skin lesions was the face followed by fore-head, scalp and neck. The commonest clinical pattern observed by Sharma VK et al(58) was Airborne contact dermatitis followed by hands and feet involvement.
74
Patch test:
Among the 44 subjects who were involved in the patch test about 39 subjects (88.6 %) where found to be positive for the patch test while 3 (6.8%) subjects reported negative results. Two subjects did not turn up for the patch test results. One subject reported an allergic contact dermatitis to the tape used in the patch test.
Lee et al (53) studied the 23 patients who completed the study and 87% had a positive patch test for at least one product. According to Gupta et al (54), out of the 80 subjects, 54 patients (67.5%) showed positive patch test result. Tomar et al(56) observed that patch test was positive in 66% of the patients while Jindal et al(57) observed that patch test was positive in 50% of the patients. Sharma VK et al (58)
observed that 82% of the subjects were positive for patch test.
75
The Korean standard antigen series was used by Lee et al (53) and all the patients showed positive patch test results to Para phenylenediamine (PPD) with 60.9% of patients showing 1+ reaction and 21.7 percent showing 2 + reaction the remaining 17.4% showed a positive 3 + reaction. 26.14% were positive for Nickel sulphate and 17.4 % where positive for neomycin sulphate. Fragrance mix was positive in 13% while potassium dichromate was positive in 13 % and balsam of Peru was reported positive in 13 % of patients.
According to Gupta et al (54), 67.5% showed positive patch test results for PPD. About 8 subjects showed a positive patch test for other allergens like 5 subjects had positivity for fragrance mix, 3 for thiuram mix and one each for paraben mix and colophony.
Sadagopan et al (55) studied 358 contact dermatitis patients with patch test and observed that 39 out of 57 of the construction workers were positive for Potassium dichromate followed by Nickel and Cobalt. He also reported in other occupations, contact dermatitis to parthenium, hair dye, footwear, paint,and Kumkum were also present in significant number.
76
Among the most commonly used commercial hair dye, the ingredients present were PPD and Resorcinol. The next common ingredient found among our patients to cause allergy was fragrance mix.
Jindal et al (57) studied 34 patients with Venous Eczema and 10 controls for patch test with Indian Standard series and 10 topical medication. Patch test was positive in 50% of the patients with the commonest allergen being fragrance mix and PPD in 15% followed by Nickel, wool alcohol, Chino form in 9 %, and 5% in balsam of Peru and Cobalt 3 % in potassium dichromate, epoxy resin, formaldehyde and thiuram mix.
Sharma VK et al (58) reported that the most common test allergen was Nickel sulphate (31%), parthenium (26%), potassium dichromate (15.7%, fragrance mix (11 %), nitrofurazone (10.7%) and Colophony in 9.3%. Mercaptothiazide and neomycin was positive in 7.8% of the subjects.
LIMITATIONS OF THE STUDY
1) Since it’s a hospital-based study with a small sample size, the frequency of manifestations may not reflect the actual population of the community. 2) Readings were not taken at 96 hours to observe late reactions.
3) Resorcinol was not tested in patch test.
77
CONCLUSION
The total number of participants in our study were 43.
Majority of the participants were males (70%) from urban locality (80%) and 30% of them were skilled workers.
ACD to hair dye was more common in persons who have used hair dyes for one to five years with a frequency of once in a month.
More than one third of them had itching immediately after application of hair dye and more than half of them had chronic skin lesions. This indicates the importance of hair dye application subsequently in spite of symptoms.
89% of the patients had positive patch test in which more than half of them showed PPD positivity while one third had pigmentation response alone.
BIBLIOGRAPHY
1. Nelson JL, Mowad CM. Allergic contact dermatitis: patch testing beyond the TRUE test. The Journal of clinical and aesthetic dermatology. 2010 Oct;3(10):36.
2. Handa S, Mahajan R, De D. Contact dermatitis to hair dye: an update. Indian Journal of Dermatology, Venereology, and Leprology. 2012 Sep 1;78(5):583.
3. Platzek T. Risk from exposure to arylamines from consumer products and hair dyes. Front Biosci (Elite Ed). 2010 Jun 1;2:1169-83.
4. Søsted H, Basketter DA, Estrada E, Johansen JD, Patlewicz GY. Ranking of hair dye substances according to predicted sensitization potency: quantitative structure–activity relationships. Contact Dermatitis. 2004 Nov;51(5‐ 6):241-54.
5. Gupta M, Mahajan VK, Mehta KS, Chauhan PS. Hair dye dermatitis and p-phenylenediamine contact sensitivity: a preliminary report. Indian dermatology online journal. 2015 Jul;6(4):241.
6. Xie Z, Hayakawa R, Sugiura M, Kojima H, Konishi H, Ichihara G, Takeuchi Y. Experimental study on skin sensitization potencies and cross‐reactivities of hair‐dye‐related chemicals in guinea pigs. Contact Dermatitis. 2000 May;42(5):270-5.
8. Belhadjali H, Ghannouchi N, Amri C, Youssef M, Amri M, Zili J. Contact dermatitis to henna used as a hair dye. Contact Dermatitis. 2008 Mar;58(3):182-.
9. Kazandjieva J, Grozdev I, Tsankov N. Temporary henna tattoos. Clinics in dermatology. 2007 Jul 1;25(4):383-7.
10. Thami GP, Kaur S, Kanwar AJ. Allergic contact dermatitis to henna. Allergy. 2001 Oct;56(10):1013-4.
11. Clausen T, Schwan‐Jonczyk A, Lang G, Schuh W, Liebscher KD, Springob C, Franzke M, Balzer W, Imhoff S, Maresch G, Bimczok R. Hair preparations. Ullmann's Encyclopedia of Industrial Chemistry. 2000 Jun 15.
12. Corbett JF. An historical review of the use of dye precursors in the formulation of commercial oxidation hair dyes. Dyes and Pigments. 1999 Feb 1;41(1-2):127-36.
13. Lewis D, Mama J, Hawkes J. A review of aspects of oxidative hair dye chemistry with special reference to n-nitrosamine formation. Materials. 2013 Feb 13;6(2):517-34.
14. Wolfram LJ. Human hair: a unique physicochemical composite. Journal of the American Academy of Dermatology. 2003 Jun 1;48(6):S106-14.
15. Correa A, Mohan A, Jackson L, Perry H, Helzlsouer K. Use of hair dyes, hematopoietic neoplasms, and lymphomas: a literature review. I. Leukemias and myelodysplastic syndromes. Cancer investigation. 2000 Jan 1;18(4):366-80.
hair dye use to the risk of malignancy. The Journal of clinical and aesthetic dermatology. 2013 Jan;6(1):39.
17. Thyssen JP, White JM, European Society of Contact Dermatitis. Epidemiological data on consumer allergy to p‐phenylenediamine. Contact Dermatitis. 2008 Dec;59(6):327-43.
18. Chan YC, Ng SK, Goh CL. Positive patch‐test reactions to para‐
phenylenediamine, their clinical relevance and the concept of clinical tolerance. Contact dermatitis. 2001 Oct;45(4):217-20.
19. Chan YC, Ng SK, Goh CL. Positive patch‐test reactions to para‐
phenylenediamine, their clinical relevance and the concept of clinical tolerance. Contact dermatitis. 2001 Oct;45(4):217-20.
20. Handa S, De D, Mahajan R. Epidemiological trends in contact dermatitis to hair dye: Comparing para-phenylenediamine positivity after a decade long interval. Indian Journal of Dermatology, Venereology, and Leprology. 2011 Jul 1;77(4):511.
21. Narendra G, Srinivas CR. Patch testing with Indian standard series. Indian Journal of Dermatology, Venereology, and Leprology. 2002 Sep 1;68(5):281.
22. Bajaj AK, Saraswat A, Mukhija G, Rastogi S, Yadav S. Patch testing experience with 1000 patients. Indian Journal of Dermatology, Venereology, and Leprology. 2007 Sep 1;73(5):313.
23. Uter W, Lessmann H, Geier J, Schnuch A. Contact allergy to ingredients of hair cosmetics in female hairdressers and clients–an 8‐year analysis of IVDK* data. Contact dermatitis. 2003 Nov;49(5):236-40.
2003–2006. JDDG: Journal der Deutschen Dermatologischen Gesellschaft. 2007 Nov;5(11):993-1000.
25. Nayak US. Hair dye dermatitis and para-phenylenediamine contact sensitivity. Indian dermatology online journal. 2015 Jul 1;6(4):246-.
26. Khumalo NP, Jessop S, Ehrlich R. Prevalence of cutaneous adverse effects of hairdressing: a systematic review. Archives of dermatology. 2006 Mar 1;142(3):377-83.
27. Sahoo B. Contact anaphylaxis due to hair dye. Contact Dermatitis. 2000;43:244.
28. Sosted H, Johansen JD, Andersen KE, Menné T. Severe allergic hair dye reactions in 8 children. Contact Dermatitis. 2006 Feb;54(2):87-91.
29. Amarger S, Franck F, Ferrier ML, Souteyrand P, D'Incan M. Proxy lymphomatoid contact dermatitis. InAnnales de dermatologie et de venereologie 2011 (Vol. 138, No. 4, pp. 315-318).
30. Matterne U, Shab A, Weisshaar E. Body dysmorphic disorder in a hairdresser: Contact dermatitis due to voluntary exposure to occupationally relevant allergens. Acta dermato-venereologica. 2010 Jan 10;90(1):97-8.
31. Jain IS, Jain GC, Kaul RL, Dhir SP. Cataractogenous effect of hair dyes: a clinical and experimental study. Annals of ophthalmology. 1979 Nov;11(11):1681-6.