“ A STUDY ON INFLUENCE OF SERUM LEPTIN OVER ASTHMA CONTROL AND ASTHMA RELATED QUALITY OF
LIFE ’’
DISSERTATION SUBMITTED
BY
DR.G.THARINI
IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF MEDICINE (M.D)
IN
TUBERCULOSIS AND RESPIRATORY DISEASES
THE TAMIL NADU DR. M.G.R MEDICAL UNIVERSITY
UNDER THE GUIDANCE OF
PROFESSOR, DR.K.ANUPAMA MURTHY M.D (CHEST),
APRIL 2017
DEPARTMENT OF RESPIRATORY MEDICINE
P.S.G INSTITUTE OF MEDICAL SCIENCES & RESEARCH,
CERTIFICATE BY THE GUIDE
This is to certify that the dissertation entitled “ A STUDY ON INFLUENCE OF SERUM LEPTIN OVER ASTHMA CONTROL AND ASTHMA RELATED QUALITY OF LIFE ” is a bonafide and genuine research done by DR.G.THARINI in the Department of Respiratory Medicine ,PSG Institute of Medical Sciences and Research, Coimbatore in partial fulfillment of the regulations of Dr.MGR Medical University for the award of M.D degree in Tuberculosis and Respiratory diseases.
PLACE : COIMBATORE DATE :
ENDORSEMENT BY THE HEAD OF THE DEPARTMENT
This is to certify that the thesis entitled “ A STUDY ON INFLUENCE OF SERUM LEPTIN OVER ASTHMA CONTROL AND ASTHMA RELATED QUALITY OF LIFE ” is a bonafide and genuine research done by DR.G.THARINI under the guidance and supervision of DR.K.ANUPAMA MURTHY ,M.D, Professor and Head, Department of Respiratory Medicine, PSG Institute of Medical Sciences and Research, Coimbatore in partial fulfillment of the regulations of Dr.MGR Medical University for the award of MD degree in Tuberculosis and Respiratory diseases.
PLACE : COIMBATORE DATE :
ENDORSEMENT BY THE PRINCIPAL
This is to certify that the thesis entitled “ A STUDY ON INFLUENCEOF SERUM LEPTIN OVER ASTHMA CONTROL AND ASTHMA RELATED QUALITY OF LIFE ” is a bonafide and genuine research done by DR.G.THARINI under the guidance and supervision of DR.K.ANUPAMA MURTHY ,M.D, Professor and Head, Department of Respiratory Medicine, PSG Institute of Medical Sciences and Research, Coimbatore in partial fulfillment of the regulations of Dr.MGR Medical University for the award of MD degree in Tuberculosis and Respiratory diseases.
DR.S.RAMALINGAM, M.D, Principal, PSG Institute of Medical Sciences and Research, Coimbatore.
PLACE : COIMBATORE
DECLARATION BY STUDENT
I hereby declare that this dissertation entitled “ A STUDY ON INFLUENCE OF SERUM LEPTIN OVER ASTHMA CONTROL AND ASTHMA RELATED QUALITY OF LIFE ’’ is a bonafide and genuine research carried out by me under the direct guidance and supervision of DR.K.ANUPAMA MURTHY ,MD, Professor and Head, Department of Respiratory Medicine ,PSG Institute of Medical Sciences and Research, Coimbatore. The dissertation is submitted to the Tamilnadu Dr.MGR Medical University in partial fulfillment of the university regulation for the award of MD degree in Tuberculosis and Respiratory Diseases. This dissertation has not been submitted in part or full to any other university or for any other Degree or Diploma before this below mentioned date.
PLACE : SIGNATURE OF THE CANDIDATE
COPY RIGHT
DECLARATION BY THE CANDIDATE
I hereby declare that PSG Institute of Medical Sciences and Research ,Coimbatore shall have the rights to preserve, use and disseminate this dissertation in print or electronic format for academic/research purpose.
PLACE : SIGNATURE OF THE CANDIDATE
DATE : DR.G.THARINI
ACKNOWLEDGEMENT
I wholeheartedly thank my dear professor and head, DR.K.ANUPAMA MURTHY for guiding me through out the study with her vast experience, timely suggestions, and correcting all my mistakes which I have committed. Her endless enthusiasm and patience was the cornerstone in successfully completing my dissertation.
I express my sincere Gratitude to my co guide and Professor Dr. R.KARTHIKEYAN for guiding and encouraging me throughout the
study. He has been a great source of motivation in all my difficult times encountered during my residentship.
I thank my co-guide Dr.B.APPALARAJU, Professor Department of microbiology for his guidance and support.
I am greatful to DR.G.SUMITHRA, Assistant Professor, Department of biochemistry for her guidance and support.
I am greatful to our Principal and PSG Management for allocating the funds required to carry out the research project.
I would like to thank my colleagues ,who have unburdened me by sharing work.
I thank the paramedical staff of our department for their support.
I wish to dedicate this work to my family for their unending love.
ABBREVIATIONS
FENO - Fraction Of Exhaled Nitric Oxide
FEV1 - Forced Expiratory Volume (1 st Second)
PEFR - Peak Expiratory Flow Rate IL – 6 - Interleukin 6
TNF α - Tumor Necrosis Factor – Alpha VEGF - Vascular Endothelial Growth Factor RSV - Respiratory Syncitial Virus
PAMP - Pathogen Associated Molecular Patterns DAMP - Damage Associated Molecular Patterns TSLP - Thymic Stromal Lymphopoietin
ELISA - Enzyme Linked Immune Sorbent Assay BMI - Body Mass Index
COPD - Chronic Obstructive Pulmonary Disease NSCLC - Non Small Cell Lung Carcinoma
AQLQ - Asthma Quality of life Questionnaire ACQ - Asthma Control Questionnaire
ACT - Asthma Control Test ICS - Inhaled Corticosteroids
CONTENTS
Sl.No CONTENTS Page No.
1. INTRODUCTION 1
2. REVIEW OF LITERATURE 9
3. AIM OF OUR STUDY 34
4. MATERIALS AND METHODS 35
5. RESULTS 45
6. DISCUSSION 65
7. LIMITATIONS 74
8. CONCLUSION 75
9. RECOMMENDATIONS 76
10. BIBLIOGRAPHY
ANNEXURES
PROFORMA
CONSENT FORM
INTRODUCTION
Bronchial Asthma is a heterogenous disease characterized by chronic airway inflammation. It is defined by history of respiratory symptoms such as wheeze, shortness of breath, cough and chest tightness that vary over time and intensity with variable, expiratory airflow limitation1.
Severe impact of asthma found to be widely spread all over the world . Globally the prevalence of asthma is estimated to be 300 million people of all age groups belonging to different ethnic backgrounds1,3. According to the recent estimates, 14% of the world’s children experience asthma symptoms. The adults who were found to have symptoms of asthma were 8.6 % and those who were taking treatment for asthma for asthma were 4.5 %.4 In India, there is wide geographical variations in prevalence of asthma.In developing countries, Rural population was found to be more affected than urban population with marked geographical differences. Bronchial asthma is the major cause of school and work absence, affecting children and adults. The increase in atopic sensitization and other allergic diseases like atopic dermatitis and allergic rhinitis contribute for increase of prevalence of asthma. Western countries are found to have higher incidence of Asthma in children, “hygiene hypothesis” contributes as one of the causes of asthma in children living in developed countries2.
causes. The phenotypes in adults include Allergic asthma , non allergen mediated asthma , late onset asthma which is more common in females, asthma with fixed airflow limitation or chronic remodeled asthma.One other important phenotype is obesity and asthma1. As the communities adapt to western lifestyle, the rate of asthma is found to increase along with the world’s population, that is urban population which increased by 14% i.e 45% to 59% in 2025. Likely it is going to witness a significant raise of asthmatic population worldwide over coming twenty years. It is found to have additional 100 million cases with asthma by 20253.Thereby understanding the current issues we need to further probe into the newer and earlier diagnostic modalities of bronchial asthma .Understanding the various phenotypes and newer diagnostic modalities helps in imparting knowledge to the patients regarding the risks of exacerbations, hospitalizations, need for good compliance to treatment, prevention of disease to have better quality of life which is beneficial to the individual and the community2.
useful for diagnosis of bronchial asthma. Research involving other biomarkers is essential to have a better understanding of the biology of asthma ,i.e understanding the association between the role of biomarkers in pathogenesis of asthma ,diagnosis and screening, assessing the severity, quality of life, disease control, prognosis, identification of endotypes and for application into clinical trials and safety monitoring6 .
proinflammatory cytokines such as leptin-levels , adiponectin-levels and ghrelin-levels were found to contribute in pathogenesis of bronchial asthma during disease control times and during severe disease without involving obesity7.
active metabolic tissue that secretes adipokines such as leptin,adiponectin and also a member of non specific inflammatory cytokines such as IL6 and
TNF α .Immunomodulation of these adipokines suggest the link between
obesity and asthma8.
The pathogenesis of bronchial asthma is associated with activation of neutrophils and eosinophils by eosinophil activating factor granulocyte monocyte colony stimulating factor or interferon gamma which facilitates into the site of allergic reaction. The influx of inflammatory cells leads to inflammatory reaction in airways leading to release of proinflammatory cytokines. The pathogenesis of this disease involves recruitment of many inflammatory cells and cytokines like IL4,IL5,IL13 in the airways following exposure to allergens,viral infections, triggering factors2.
PATHOGENESIS OF BRONCHIAL ASTHMA
Leptin is one of the proinflammatory cytokine is shown in literature and it is involved in the pathogenesis of bronchial asthma . Leptin is a 16 KD A proinflammatory cytokine without any glycolysation. This polypeptide is represented in the obese gene. Structurally, Leptin belongs to the long chain helical cytokine family. Other pro inflammatory
cytokines including TNF α are known to increase leptin synthesis in
The leptin production is related to the food intake. Serum leptin levels are found to reduce during fasting whereas after the intake of food there is high concentration of serum leptin due to the expression of the obesity gene. Other factors such as insulin and steroids stimulates leptin secretion. Leptin concentrations are also higher during infectious conditions and sepsis.The expression of leptin is upregulated by various
proinflammatory cytokines that includes TNF α,Interleukin 1,leukemia inhibiting factor.
Other than Bronchial asthma, Leptin plays an important role in lung diseases such as obstructive sleep apnoea and hypoapnoea syndrome, obesity hypoventilation syndrome, chronic obstructive pulmonary disease, lung malignancy and infectious disease of the lungs.
The release of VEGF is directly proportional to the severity of asthma. Activation of leptin receptors in the airway smooth muscles increases the release of vascular endothelial growth factor which indicates severity of disease. Bronchial asthma not only manifests as local inflammation, but also systemic inflammation takes place.10
Despite adequate evidence between bronchial asthma and serum leptin levels, we still find gaps in knowledge. Moreover we found out that leptin has not been studied in the perspectives of outcomes of asthma management, specifically disease control and quality of life.
Our study intends to study association between serum leptin ,control of asthma and disease specific quality of life.
REVIEW OF LITERATURE
the most common pathogens. These are found in airways of chronic stable asthmatics. Their presence of all these causes increase in tissue mast cells. Exposure of the lung to air pollution exacerbates pre existing asthma. Airpollution causes local oxidative stress, induces or modifies airway inflammation, leading to sensitization of the airways to the allergens, impairs lung development or injures the smaller airways. Other early life exposures such as fetus, newborn and early childhood exposures influence the risk of bronchial asthma. However Dietary deficiencies of vitamin D and vitamin E,Parental smoking are some of the other contributing factors. Occupational exposures contributes 17 % of adult onset asthma. This occurs due to immunological sensitization of airway epithelium to the substances used in occupation. (occupational asthma caused by sensitizer ) or high concentration irritant exposure, Irritant induced occupational asthma2 .
causing visious cycle in atopic phenotype, IL – 13 sustains airway inflammation .However the role of Th2 cells in non allergic asthma is not understood 2.
Thereby the biomarkers have a potential role in diagnosing, monitoring the disease progression, and creating individually tailored regimens. Along with clinical and hematological investigations, pulmonary function tests is often used in diagnosing bronchial asthma and differentiating bronchial asthma from other obstructive airway disease. This heterogenecity, pathogenesis, lack of consensus to judge therapeutic efficacy and lack of effective clinical trials to judge drug efficacy have been obstacle in developing new treatment targeting different phenotypes. We had done a thorough literature review to understand the various investigation tools and biomarkers used in the diagnosis of bronchial asthma.
Induced sputum Eicosanoid concentration in asthma was studied by Ian D, Richard et al during 1999,including 36 subjects,10 of them were normal and 26 subjects were asthmatics. They measured induced sputum eicosanoids and cysteinyl – leukotrienes by ELISA method and concluded that there was higher concentration of eicosanoids and cysteinyl leukotrienes in asthmatics compared to normal subjects18.
subjects who had controlled asthma and created mild exacerbation by decreasing the inhaled steroid dosage from from 800 micrograms of beclomethasone to 200 micrograms of budesonide. They were monitored weekly twice and PEFR was measured for 8 weeks after steroid reduction. During each visit, FENO, Methacholine challenge test were measured and spirometry and sputum induction was performed. They found that 8 subjects did not develop exacerbation during the study and seven subjects developed mild exacerbation at weeks 4,6 and 8.There was an increase in sputum eosinophil count in subjects with subsequent exacerbations and there was decrease in airway function, by monitoring PEFR and FEV1,Thereby they concluded that change in eosinophil count is a potential marker for explaining poor control of asthma19.
levels of serum leptin was 3.53 ng/mL and 2.26 ng / Ml .subgroup analysis showed that the difference in leptin levels was more in boys when compared to female children,3.09 ng/ml in asthmatic boys and 1.52ng/ml in non asthmatic boys. Health boys were found to have low sr leptin concentration when compared with non asthmatic healthy girls (p = 0.019) .Atopic asthma patients had high concentration of serum leptin when compared with non atopic asthmatics who had the same body mass.A weak relationship was found between serum leptin levels and serum total IgE levels in the overall group of asthmatic children(p=0.019) and this relationship was much more confined to boys. However they did not show any relationship between serum leptin levels and skin prick test, weight at birth, duration of giving breast feeds , pulmonary function tests and passive-smoking.
infusion of leptin lead to increase in serum leptin concentrations which was increased much more after ovalbumin challenge and sensitization.
The serum IgE levels and methacholine responsiveness to challenge test were increased in leptin when compared to saline infusion mice. This study showed that serum leptin levels were higher in the time of allergic airway sensitization and it hence plays a major role between asthma and obesity.
sputum strategy(SS) group. the minimum treatment to maintain control was identified in 107 patients (Phase 1) and the treatment was continued for two years. Out of the 126 exacerbations, majority of them were mild. Among the 102 exacerbations, the sputum examination was done before treatment was initiated ,out of them 70 were non eosinophilic.
In the sputum strategy group ,the time for first exacerbation was 213 days ,which is relatively longer in those who considered to need treatment with long acting beta agonists by 490 days with a relative risk ratio .Patients who used inhaled corticosteroids with a daily dosage of fluticasone 250 mcg were found to be benefitted. They concluded that patients who had moderate as well as severe asthma were benefitted via monitoring sputum cell counts by reducing the incidence of eosinophilic exacerbations & also via reduction of the severe characteristic clinical features of eosinophilic-mediated as well as non-eosinophilic mediated exacerbations that too with not even increasing the whole corticosteroid dose.
European study of asthma, spain during the year of 1996 conducted a large randomized control study on the total sr. IgE concentration levels in association with asthma independent feature of the specific IgE concentration levels ,to common aeroallergens,
They faced a respiratory questionnaire and spirometry, total and serum specific IgE to mites, moulds and pets were recorded. Dose dependent methacholine challenge test was done in 1,626 subjects, those who had asthma attacks showed association with total IgE .Those who had negative specific IgE had association between Serum IgE and asthma. Subjects who have current wheezing and bronchial hyper responsiveness without attacks of asthma also showed adjusted association with serum IgE.The above findings prove that increased levels of serum IgE was associated with asthma even in the subjects who had negative specific IgE to common aeroallergens22.
Guiquan Jia , Richard.W. Erickson,et al 24 during 2012 conducted a prospective study including 67 asthma patients who remained symptomatic despite maximum inhaled corticosteroid treatment. They aimed to analyze whether periostin can be used as a systemic biomarker of eosinophilic airway inflammation in asthmatic patients, They measured FENO, peripheral blood eosinophilia, periostin and serum IgE levels and compared with airway eosinophilia in asthma patients. Sputum was collected in these patients and performed bronchoscopy and matched peripheral blood samples from 67 asthma patients. They concluded that serum periostin levels were high in asthma patients with evidence of eosinophilic airway inflammation compared to those with relatively less airway inflammation. Periostin is a systemic biomarker of airway eosinophilia in asthma patients and has potential utility for patient selection and asthma therapeutics targeting T helper 2 inflammation.
periostin levels were significantly higher in serum than sputum with a (p<0.001). Eosinophilic asthma patients(n=37) had higher serum and sputum periostin than non eosinophilic asthma. Both serum and sputum periostin levels were significantly associated with proportion of sputum eosinophils (r=0.422,p<0.001 ,r=0.364,p=0.005 respectively)but they were not associated with asthma control. Peripheral blood eosinophilia was assessed in 67 matched samples and it had a greater AUC about 0.820 compared with serum periostin p=0.086,for the detection of eosinophilic asthma.They concluded that in poorly controlled asthmatics, sputum and serum periostin levels significantly related to sputum eosinophil proportions while their ability to predict the presence of eosinophil asthma is significant.
In the past and present there are quite number of studies that have examined the potential role of leptin in respiratory diseases. Data resources are available that have identified foetal and adult lung tissue as leptin responsive and leptin producing organs and association between leptin and asthma. Leptin’s response in pulmonary homeostasis have also become evident. Research articles on serum leptin levels and other disorders like Obstructive sleep apnoea and hypoapnoea syndrome (OSAHS),COPD and lung cancer have also come to light10.
and it is associated with abnormal inflammatory response of the lungs to noxious particles or gases. There is some relationship between obesity and chronic bronchitis or obesity and emphysema, patients with low body mass index have high mortality rates. The mechanism underlying this concept is not clearly understood. Some studies in the literature has shown that some abnormalities in the leptin feedback mechanism might play a role in impaired energy balance that is responsible for the cachexia in COPD patients. However there is no evidence for presence of high serum leptin levels in malnourished stable patients and malnourished COPD patients and there is no statistically significant relationship between circulating
peripheral lung of COPD patients. Leptin is also found to be over expressed in submucosa of proximal airways of COPD patients10 .
Lung cancer and serum leptin levels : As the body mass index increases, there is higher death rates due to cancer and there is a well established relationship between obesity and risks of developing cancer. Functional polymorphism in the promoter region of leptin gene is found to have three fold increase in the risk of developing Non Small Cell Lung Carcinoma (NSCLC).Due to higher concentration of serum leptin in obese subjects, leads to polymorphism of the leptin gene and causes cancer. Leptin has an influence over the innate and adaptive immunity and causes neutrophils, mononuclear cells, macrophages, dendritic cells and T cells that induces chronic inflammation and leads to lung carcinogenesis. However further research is needed as literature shows only some experimental evidence between lung cancer and serum leptin levels.
Leptin ,it is 16Kilo Dalton chain of aminoacids (protein) which constitutes total number of 167 aminoacids. It represents the product of Ob gene which is located in humans in chromosome seven. White adipose tissue is the source of synthesis of this protein. Other tissues such as placenta, pancreas and gastric fundus mucosa are also sources for leptin synthesis. Leptin is demonstrated in the peripheral lung tissue of humanbeings, which includes both broncho-epithelial cells of the alveolar type 2 pneumocytes as well as macrophages generated in the lung tissue. The serum leptin levels directly correlate with the food intake as there is transient Ob gene expression following food intake. Other factors such as insulin and glucocorticoids influence leptin levels. Leptin levels are higher in sepsis and infection, it is upregulated by various pro inflammatory
cytokines such as TNF α,IL– 1 and leukemia inhibiting factor. Testosterone inhibits leptin production ,however ovarian sex steroids increases leptin levels. Chronic inflammatory conditions causes reduction in leptin levels in contrast to acute inflammatory conditions10.
most common is allergic asthma whereas ,adults have heterogenous collection of phenotypes20. There is also existing data that suggests high serum leptin concentrations are associated with greater asthma severity11. Pathophysiology of asthma and leptin has correlation as leptin activates the sympathetic nervous system.Though the action of leptin on sympathetic nerves of lungs is unknown, leptin increases the sympathetic nervous system activity of adrenal medulla and sympathetic nerves in various organs. However, the effect of leptin on human airway smooth muscle cells and airway remodeling is associated with asthma according to some researchers10. Leptin and its receptors are expressed in human airway epithelial cells , systemic leptin or visceral fat expression of leptin may be associated with greater asthma prevalence or severity particularly pre pubertal , peripubertal, post pubertal girls, and women. Further modulation of leptin independent of BMI needs to be established for asthma prevention and treatment.
thickness, physical activity. About 5876 subjects were included in the study after excluding pregnant women and those who had missing values for covariates. Among the participants, 4.9% currently had asthma and 95.1% never had. Mean concentration of sr.leptin levels were 11.3μg/l. After classifying the subjects as over fifty years and less than fifty years, the association between current asthma and leptin was stronger in women and when compared between premenopausal and post menopausal women, leptin levels were higher in pre - menopausal females when compared with that of post- menopausal females. The results of this large study shows that leptin was high in females, especially those who were obese and also those who were asthmatics, However this study did not give any evidence that serum leptin were associated in this context13.
compared between obese asthma patients and control group. Spirometry and skin prick tests were undergone. Here it showed that in obese individuals Erythrocyte Sedimentation rate, and Complementary Reactive Proteins and , Tumor necrosis Factor α and , Interleukin 6 and leptin levels were higher in obese asthmatics than control group. This study identified that inflammatory markers were higher in obese asthmatics and likely leptin is thought to play a vital role in the pathogenesis of asthma disease27.
Andrea Lessard, et al conducted a study during 2010.They found higher serum leptin (p <0.00001) and lower adiponectin (p=0.0002) levels in obese asthmatics. Sputum leptin was correlated with BMI and serum leptin ,and concluded that airway inflammation occurring in obese asthmatics may present a different involving leptin. Sputum leptin levels are found to arise from the systemic circulation and it is also found to have a variety of other contributing mechanisms28.
tightness, coughing, shortness of breath at rest ,during exercise or being woken from sleep due to breathlessness. Allergic rhinitis by questioning ,whether there was any previous history of allergic rhinitis suspected ,results were ,out of the 1957 subjects had information on leptin and adiponectin, Leptin / adiponection ratio positively associated with the level of asthma, especially females. However this estimation was non significant after adjusting for fatness measures and multiple other comparisons. Thus asthma levels correlated positively with serum leptin levels. The possibility of association with fatness could not be ruled out30.
associated with allergic rhinitis and allergic broncho pulmonary aspergillosis patients12.
A prospective study by Agori Tsaroucha M.D ,Zoe Daniil et al, during 2013,conducted a prospective study to assess the circulating concentration of leptin, adiponectin and ghrelin in thirty two female patients who belonged to postmenopausal age group and thirty seven female asthmatics during exacerbations and 8 weeks later and 22 controls. The relationship between the three peptides and the indexes of pulmonary function, atopy and airway inflammation were studied. Compared with controls the stable asthma patients had higher amount of leptin and lower ghrelin concentrations. Patients with severe asthma had higher values of leptin and low values of adiponectin versus patients with mild to moderate asthma.The leptin concentration as well as leptin adiponectin ratio were useful biomarkers for discriminating asthma patient’s with controls on one hand and severe from mild to moderate asthmatics on the other hand. Leptin concentration was higher in atopic asthma patients than non atopic asthma patients and also positive correlation was established between serum leptin and total IgE levels in .They concluded that leptin ,adipnectin and ghrelin may play a significant role in the pathogenesis of asthma during stable and exacerbations independent of obesity7.
adiponectin is an anti inflammatory cytokine. The effects of adipokines on lungs has shown to induce or cause exacerbation of bronchial asthma. Higher serum adiponectins has shown to cause lower clinical severity of asthma and in contrast exogenous administration of leptin has shown to induce bronchial hyper responsiveness in mice. The macrophages present in the alveoli of obese asthma patients were sensitive to leptin levels, thereby augmenting inflammation. Based on this mechanism, Higher serum leptin is present in obese asthma patients according to the literature as we searched through. The prevalence of asthma in these associations are stronger in women, post pubertal girls and prepubertal boys20.
Doaa Mohammad Youssef et al conducted a study to evaluate the levels of serum leptin in children and their effect on Th1 / Th2 balance in obese children and non obese children who had asthma. They also aimed to identify the relationship between serum leptin levels and clinical outcomes in asthma. Fifty atopic children who were physician diagnosed moderate to severe persistent asthma and twenty controls were studied. The children with asthma were divided into two groups, obese and non obese groups .Peripheral blood sample was obtained from all the fifty children and serum leptin levels, IFN – γ and IL – 4 levels were determined. Asthma symptoms were analysed and the results was associated with parameters studied. The found out that serum leptin levels were higher in obese children compared to non obese children and also children with asthma had higher levels of serum leptin compared to children without asthma. Additional findings were obese asthmatics showed low levels of FEV1 percentage predicted and
high levels of asthma symptom score than the non obese group.The obese asthma group showed a significant correlation between leptin levels and IFN – γ levels. Thus they concluded that though the pathogenesis of asthma involves leptin in both obese children and non obese children, the effects of leptin is more pronounced in the obese children. The obese children with asthma who had high levels of serum leptin exhibited T helper one polarization - with higher amount of Interfern – γ and greater severity of
asthma.
Some of the barriers to reduce the burden of asthma as of literature review are poverty, poor education and poor infra structure. Environmental barriers such as tobacco smoking, indoor and out door air pollution and also occupational exposures. The lack of symptom based approach to treatment rather than disease based approach to the management of respiratory diseases also remains a barrier to reduce the burden of asthma. Inherent barriers in the organization of health care services such as geography, type of professional responding, public and private care, education and training systems, tendency of care to be acute than routine. Limited availability and usage of medications , poor supply of drugs, cost, cultural attitudes towards drug delivery systems such as inhalers .Inadequate resources and requirement of respiratory specialists and related organizations to care for a wide variety of diseases which resulted in failure to adequately promote awareness of asthma.
Our understanding about the nature of illness is being evolving with time from an isolated disease to many complex phenotypical disease, many natural concepts , physiology, response for the therapy. Earlier treatment of asthmatic individuals by corticosteroids and other antiasthmatic medications has shown various ranges of victory, inspite of the fact that primary studies showed that type 2 inflammation as a cause involved in pathogenesis of asthmatic individuals and the therapeutics targeted towards the same, the treatment options are not successful.Almost whole factors finally causes improved interest in carrying out phenotype of bronchial asthma approach to large asthma patient cohort groups identified variable asthmatic individual characteristics. It has also been identified that the significance of the initial occurrence of age of asthmatic disease as well as blood eosinophils in evaluating clinically appropriate phenotypic asthmatics. Research on this similar molecular studies about phenotyping of asthma, made us understand that all the asthmatics did not have the same type II inflammatory pattern. Further research is mandatory to understand and clarify the additional clinical and molecular phenotypes, validated predictive biomarkers for diagnosis and monitoring disease progression and identify the new areas of possible interventions54.
leptin levels with disease control and disease specific quality of life we conducted the study .The results of such research analysis would help in designing and optimizing treatment strategies to improve the health related outcomes of the patient and the community.
AIM OF OUR STUDY
Primary Aim :
To characterize asthmatic subjects in terms of asthma severity, control and disease specific quality of life.
Secondary Aim :
To correlate serum leptin with asthma control.
To explore the association between serum leptin and various components of asthma related quality of life.
MATERIALS AND METHODS
Study design : Prospective study (observational)
Sample Size and population : Sixty asthmatic subjects
Duration of study : 12 months
Study location : Department of Respiratory
Medicine, PSG IMSR.
INCLUSION CRITERIA
1. Age more than or equal to 18 years.
2. Physician made diagnosis of asthma.
3. Willingness to participate in the study.
EXCLUSION CRITERIA
1. Acute exacerbation of Asthma within 2 weeks prior to recruitment.
2. Steroid dependent asthma.
3. Chronic respiratory illness other than asthma.
4. Clinical evidence of pulmonary and extra pulmonary infections.
5. History suggestive of COPD.
6. Systemic inflammatory disorders, malignancy, decompensated cardiac conditions, uncontrolled Diabetes Mellitus (HbA1c ≥8.5).
7. Hormone replacement therapy.
Data collection and evaluation plan: Eligible candidates as
1. Socio demographic characteristics
2. Disease characteristics
3. Current and past treatment details.
4. Asthma related Quality of life (Asthma related Quality of Life Questionnaire)7
5. Asthma control (Asthma Control Questionnaire)8
6. Asthma control (Asthma Control Test)9
After a detailed interaction with the subjects, they underwent Spirometry with the bronchodilator response.5 ml of venous blood was collected after at least 8 hours of fasting. Thus collected blood samples were centrifuged at 3000 RPM and serum was separated and stored at -20 degree celcius. Subsequently serum leptin levels were estimated by ELISA method. All the data collected were compiled appropriately in a case record form and then transferred in a master sheet for further data analysis.
SOCIODEMOGRAPHIC CHARACTERISTICS ;
Socioeconomic status was defined and categorized according to Modified Prasad’s classification.This classification involves five classes as give below based on the per capita income :
MODIFIED BG PRASAD’s CLASSIFICATION OF SOCIO
ECONOMIC STATUS(January 2015)
CLASS PER CAPITA INCOME
I More than Rs 5797
II Rs 2898 – Rs 5797
III Rs 1932 – Rs 2577
IV Rs 869 – Rs 1546
V Below Rs 869
DISEASE CHARACTERISTICS :
Disease and treatment related variables such as duration of illness in years, duration of use of inhaled corticosteroids, Number of exacerbations during the last one year prior to recruitment were all studied. Associated symptoms of allergic rhinitis was also included. The number of exacerbations over last one year was divided into three groups such as :
1. No exacerbation 2. 1 – 3 exacerbation
JUNIPER’S ASTHMA CONTROL QUESTIONNAIRE :
This asthma control questionnaire has seven questions. It includes the most five important symptoms , two questions about the rescue bronchodilator use and FEV1 predicted by spirometry respectively. The
patients were asked to recall their symptoms over the last seven days and response to each of the question was elicited.
The scoring of ACQ –
For clinical practice the optimal cut off is 0.75
The average of all the seven questions were calculated.
A score of 0.75 or less – 85 % chance of having well controlled asthma.
For clinical trials – The optimal cut off is 1.50
ACQ score of 1.50 or greater – 88 % chance that the asthma is not well controlled16.
For the purpose of this study, all study subjects were categorized as well controlled and inadequately controlled at a cut off value of 1.5.Accordingly,
Well controlled asthma ≤ 1.5
ASTHMA RELATED QUALITY OF LIFE QUESTIONNAIRE
(AQLQ) :
The Asthma related quality of life questionnaire by Elizabeth Juniper is a well validated questionnaire which is used in clinical trials and clinical practice. This questionnaire helps to accurately assess the symptoms of the asthmatics as perceived by them over a duration of last two weeks.
The questionnaire consists of thirty two questions and they are divided into four domains:
AQLQ symptom Score
AQLQ Activity score
AQLQ Emotion score and
AQLQ Environment score.
A detailed interview was conducted with the subjects and the questionnaire was completed.
ASTHMA CONTROL TEST
The asthma control test consists of a numerical score to guide the clinician to determine whether the disease is well controlled or not.
It consists of five questions each having 4 score boxes respectively. The scores of all the five questions are added up.This score is used foe individuals who are more than twelve years.
Step 1 : Write the number of each answer in the score box provided
Step 2 : Add up each score box for the total
Step 3 : To take the completed test score to physician
A score of ≤ 19 indicates - poorly controlled asthma
Score ≥ 19 well controlled asthma.
SERUM LEPTIN ANALYSIS BY ELISA METHOD
This is the Quantitative determination of serum leptin by Enzyme linked immunoassay method.
PRINCIPLE OF THE TEST :
This method consists of a two step or a sandwich type assay. The assay uses two highly specific monoclonal antibodies. A monoclonal antibody that is specific for the proinflammatory cytokine, leptin is fixed already into the micro well plate and another monoclonal antibody specific for another epitope of leptin is conjugated with biotin. In first step ,leptin present in the samples and standards is bound to the immobilized antibody and to the biotinylated antibody thus leading to the formation of a sandwich complex. The extra amount of unbound biotinylated antibody is removed by washing step.
In the second step, streptavidin HRP is added ,which binds specifically to any bound biotinylated antibody. The unbound streptavidin HRP is removed by washing step.
the graph from which the amount of leptin in patient samples and controls can be read directly from the reader.
DEMONSTRATION OF ELISA KIT – THE YELLOW COLOURED
STUDY METHODOLOGY
Recruitment of Eligible subject based on selection criteria
Written informed consent
History & Physical examination
Spirometry with bronchodilator response
Asthma control questionnaire (Juniper’s Questionnaire) AQLQ (Juniper’s Questionnaire)
ACT
Sampling of blood after 8-12hrs of fasting and analyze Sr. Leptin levels by ELISA Method
Data analysis
RESULTS
We present our study results under the following description :
1. Characterization of study population
2. Definition of control of asthma
3. Group analysis comparing clinic physiological variables, serum leptin and quality of life between well controlled and inadequately controlled asthmatics.
4. Correlation of clinic physiological variables with serum leptin.
Study Population:
belonged to class III, 5(8.3%) of the subjects belonged to class IV, 2 (3.3%) of the subjects belonged to class V. (TABLE 1)
[image:59.595.103.506.377.659.2]Among the study population, 3 (5%) of them were exsmokers with pack years less than 5, none others were current smokers and none of them were alcohol consumers. 42(70%) subjects had family history of bronchial asthma whereas the remaining 18 (30%) subjects had no family history of bronchial asthma.
TABLE 1: SOCIODEMOGRAPHIC CHARACTERISTICS OF
STUDY POPULATION
* BMI-Body Mass Index
SOCIODEMOGRAPHIC VARIABLES N=60
Age (Years) 37.8 ± 15.33 Gender Male 25 (41.7%)
Female 35 (58.3%)
BMI (Kgs/m2) * 24.04 ± 4.16
Socio Economic Status (modified Prasad's scale)
Class I 16 (26.7%)
Class II 30 (50.0%) Class III 7 (11.7%)
Class IV 5 (8.3%)
Class V 2 (3.3%)
When we studied the disease and treatment characteristics of the study population (TABLE: 2) , the mean duration of illness was 11.02 ± 3.37 years. Among the study subjects 48 (80%) of them used inhaled corticosteroids and the mean duration of usage of inhaled corticosteroids was 4.67 ± 6.18 years.
Forty two (70%) subjects had family history of bronchial asthma whereas remaining 18 (30%) of the subjects had no family history of bronchial asthma.
The frequency of exacerbation was enquired for last one year prior to recruitment. The frequency of exacerbation was divided into three groups:
No exacerbation,
One to three exacerbations
More than three exacerbations.
TABLE 2: SUMMARY OF DISEASE AND TREATMENT
CHARACTERISTICS OF STUDY POPULATION
* ICS Inhaled Corticosteroids
DISEASE / TREATMENT RELATED
VARIABLES N=60
Duration of illness 11.02 ± 3.37 Years
ICS Use* 48 (80.0%)
No. of Years of ICS usage 4. 67 ± 6.18
Acute exacerbation
category during one year
prior to recruitment
No Exacerbation 35 (58.3%)
1-3 Exacerbation 16 (26.7%)
>3 Exacerbation 9(15.0%)
FIGURE 1: PIE CHART DISTRIBUTION OF FREQUENCY OF
EXACERBATIONS AMONG THE STUDY POPULATION DURING
LAST ONE YEAR PRIOR TO RECRUITMENT
58% 27%
15%
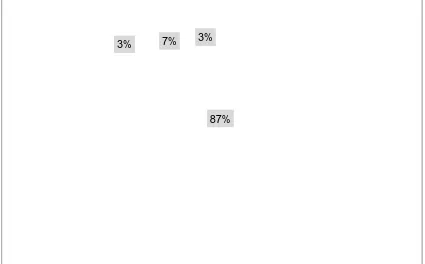
FIGURE 2: PIE CHART DISTRIBUTION OF FREQUENCY OF
COMORBID CONDITIONS AMONG THE STUDY POPULATION
87%
3% 7% 3%
CORRELATION BETWEEN THE TWO SCORING SYSTEM FOR
CONTROL OF ASTHMA:
We used Juniper’s Asthma control questionnaire (ACQ) ,Asthma Quality of life questionnaire(AQLQ) and Asthma Control test(ACT) Questionnaires. Juniper’s Asthma control questionnaire score of <1.5 was defined as well controlled asthma16. Juniper’s Asthma control test of ≥ 19 was defined as well controlled asthma17. Among the study group, 17 (28.3%) of the subjects were considered as well controlled according to Junipers asthma control questionnaire score while 21 (35.0%) of the subjects were considered to have well controlled asthma according to asthma control test questionnaire. These two definitions in the study population did not correlate well. The Pearson’s correlation coefficient was r2 = 0.188; P > 0.05 (Table-3)
Thus we were compelled to use one of the two scoring systems suitable for this project. Accordingly, Juniper’s ACQ was selected for the following reasons :
1. Juniper’s ACQ is most widely used and well validated tool for assessment of control of asthma.
2. Juniper’s ACQ has FEV1 parameter (spirometry) giving
TABLE 3: CORRELATION BETWEEN TWO SCORING SYSTEM
FOR CONTROL OF ASTHMA
JUNIPER'S ASTHMA CONTROL
QUESTIONNAIRE
JUNIPER'S ASTHMA
CONTROL TEST
Score of < 1.5 defines well controlled
asthma
Score of ≥ 19 defines well
controlled asthma
FIGURE 3: GRAPHICAL REPRESENTATION OF THE
CORRELATION BETWEEN TWO SCORING SYSTEM FOR
CONTROL OF ASTHMA (SCATTER PLOT GRAPH).
GROUP ANALYSIS OF STUDY POPULATION BASED ON
CONTROL OF ASTHMA :
Based on the control of asthma as assessed by Juniper’s asthma control questionnaire, the subjects were divided into two groups. Well controlled asthmatics were 17 (28.3 %) and others 43 (71.6 %) were classified as inadequately controlled. An array of variables like sociodemographic characteristics, gender, duration of illness, duration of use of inhaled corticosteroids , dose of inhaled corticosteroids, associated allergic rhinitis, post bronchodilator FEV1 % ,AQLQ total score, symptom,
activity and emotion domains were compared between the two groups. (TABLE 4)
However we found that the dose of inhaled corticosteroids in well controlled asthma was significantly higher 294.12 ± 143.18 mcg per day compared with inadequately controlled asthmatic subjects whose daily mean ICS dosage was 188.37 ± 169.32 mcg per day ( P=0.027) . In the study, among the fifty two subjects who had allergic rhinitis, 13 (21.6%) subjects had well controlled asthma and 39(65%) subjects had inadequately controlled asthma (p= 0.144). The post bronchodilator FEV1(% predicted ) was 80.25 ± 20.41 % in well controlled asthmatics and
82.92 ± 21.58% in inadequately controlled asthmatics ( p=0.670 ). Lung function status in terms of post bronchodilator FEV 1 % predicted was
TABLE 4: GROUP ANALYSIS OF STUDY POPULATION BASED ON CONTROL OF ASTHMA BY ACQ SCORE
VARIABLES
WELL
CONTROLLED
ASTHMA N=17
INADEQUATELY
CONTROLLED
ASTHMA N=43
P VALUE
Age (Years) 37.35 ± 15.910 37.98 ± 15.282 0.880
Male 5 (29.4 %) 20 (46.5%) 0.226
BMI (Kgs/m2)* 23.388 ± 3.837 24.304 ± 4.305 0.440
Duration (years) 13.29 ± 11.03 10.12 ± 8.606 0.240
Duration of ICS (years) 6.544 ± 8.196 3.939 ± 5.116 0.143
ICS dose (mcg)* 294.12 ± 143.486 188.37 ± 169.32 0.027
Allergic rhinitis 13 ± 76.5 % 39 ± 90.7 % 0.144
Post Bronchodilator %
FEV1 (% Predicted)
80.25 ± 20.41 82.92 ± 21.58 0.670
Comparing the Asthma quality of life total score, the mean score was significantly higher among well controlled asthmatics 4.863 ± 1.015, compared with inadequately controlled asthmatics whose average score was 4.300 ± 0.8482 (P=0.029). Similarly Asthma Quality of life questionnaire activity score in well controlled asthmatics was significantly higher 4.8888 ± 1.090 compared with inadequately controlled asthmatics whose mean score was 4.376 ± 0.8482 (p = 0.050). The AQLQ symptom score in well controlled asthmatics was 4.892 ± 1.028 and in inadequately controlled asthmatics 4.265 ± 0.8327 (p = 0.018). The AQLQ emotion score in well controlled asthmatics was 4.752 ± 1.030 and in inadequately controlled asthma was 4.218 ± 0.8594 (p = 0.045).
Thus we found that Asthma Quality Of Life questionnaire total and domains score such as activity, symptoms and emotions in well controlled asthmatics was significantly better compared with inadequately controlled asthmatics. However in our study there was no statistically significant difference in AQLQ environment domain between well controlled asthma 4.852 ± 1.2121 and inadequately controlled asthma 4.302 ± 0.9006 (p = 0.103) (TABLE: 5)
that serum leptin levels was statistically different in both the groups of asthma control (Figure 4 and Table 5 )
FIGURE 4: GRAPHICAL REPRESENTATION (BOX PLOT) OF
SERUM LEPTIN AND ITS RELATIONSHIP WITH CONTROL
CORRELATION BETWEEN SERUM LEPTIN AND
CLINICOPHYSIOLOGICAL VARIABLE :
In the study population, we found that there was significant statistical correlation between serum leptin and some of the clinic physiological variables.
The variables that showed positive statistical significance with serum leptin levels are :
Body mass index correlated modestly with serum leptin (r2 =0.302 ; p = 0.019).There was a statistically significant correlation between serum leptin and AQLQ total score (r2 =0.256 ; p= 0.049).AQLQ activity domain score (r2=0.274 P = 0.034) and AQLQ symptom domain score (r2 =0.253, p= 0.05)(TABLE - 5) .
Other important variables such as age , mean duration of illness ,duration of usage of inhaled corticosteroids, dosage of inhaled corticosteroids ,post bronchodilator FEV1 and asthma quality of life environment score did
TABLE 5: CORRELATION BETWEEN SERUM LEPTIN AND
CLINICOPHYSIOLOGICAL VARIABLE (CONTINUOUS
VARIABLES ONLY)
Variables r2 P Value
Age 0.045 0.734
BMI 0.302 0.019
Duration of illness 0.142 0.279
ICS years 0.145 0.268
ICS dose 0.068 0.607
Post Bronchodilator FEV1 -0.145 0.299
ACQ Score -0.178 0.172
ACT Score 0.144 0.271
AQLQ total 0.256 0.049
AQLQ activity 0.274 0.034
AQLQ Symptom 0.253 0.05
FIGURE 5: GRAPHICAL (SCATTER PLOT) REPRESENTATION
OF CORRELATION BETWEEN BMI AND SERUM LEPTIN
LEVELS.
FIGURE 6: SCATTER PLOT REPRESENTATION OF CORRELATION
BETWEEN SERUM LEPTIN VALUES AND ASTHMA RELATED
OVERALL QUALITY OF LIFE (TOTAL SCORE).
r2 = 0.256
FIGURE 7: SCATTER PLOT REPRESENTATION OF
CORRELATION BETWEEN SERUM LEPTIN VALUES AND
ACTIVITY SCORE OF ASTHMA RELATED QUALITY OF LIFE
r2 = 0.274
FIGURE 8: SCATTER PLOT REPRESENTATION OF
CORRELATION BETWEEN SERUM LEPTIN VALUES AND
SYMPTOM SCORE OF ASTHMA RELATED QUALITY OF LIFE
DISCUSSION
The primary objective of our study was to characterize the asthmatic subjects in terms of sociodemographic ,disease characteristics including control and quality of life. Our secondary aim was to correlate serum leptin with asthma control and to explore the association between serum leptin and various variables and asthma related quality of life. To achieve this we divided the study population into two groups,
1.Well controlled asthmatics (N = 17)
2.Inadequately controlled asthmatics (N=43)
The study population included sixty asthmatic subjects. Among them, seventeen were well controlled asthmatics and forty three were inadequately controlled asthmatics.
expression. Obesity related increase in leptin leads to worsening of asthma10.The mechanism for correlation of serum leptin with body mass index could be due to low grade chronic inflammation in obese patients due to excessive adipose tissue. The adipose tissue is rich in a number of non specific mediators of inflammation such as Tumor necrosis factor α,
Interleukin - 6 and different kinds of adipokines. The activated and hypertrophied adipose tissue leads to the release of proinflammatory cytokines and macrophages or immune modulation of these adipokines leading to the decreased amount of adiponectin and increased leptin leading to chronic inflammation in obesity8.
Our study was conducted with the aim of exploring the role of leptin in stable asthmatics and to identify its relationship with control of asthma. We found that serum leptin had no association with control of asthma. Other salient features of our study as follows: The positive findings were:
High dose of ICS was associated with better control of Asthma. Serum leptin correlated modestly with body mass index.
Serum leptin had modest but statistically significant positive correlation with overall asthma related quality of life possibly through activity and symptoms domains of quality of life.
relationship between serum leptin and asthma severity or control. Similarly Canoz M Erdenen et al compared the relationship of inflammatory cytokines in control group and asthma group27. This study included 54 women in asthma group (24 non obese and 30 obese asthmatics) and 44 controls (20 with normal weight and 22 obese women).Mean age of asthma group was 40.7 ± 9.8 and control group was 36.1 ±11.1 years. Obese asthma patients had a mean BMI of more than thirty while the healthy control group and non obese asthma patients had a mean BMI of about less than twenty five. Anthrometric parameters, Erythrocyte sedimentation rates (ESR), C Reactive protein (CRP), leptin, Tumor necrosing factor,
TNF α, IL 6, were compared between obese asthma patients and control
group. Pulmonary function tests and allergy skin tests were also performed.
The results showed ESR, CRP, TNF α, IL 6 and leptin levels were higher in
obese asthmatics than control group. This study identified that inflammatory markers were higher in obese asthmatics and likely leptin is suggested to play a role in pathogenesis of asthma27.However in both the above studies they did not evaluate the relationship between asthma severity or control.
Stephanie A. Shore et al explained a possible mechanism of the influence of obesity on airway smooth muscle related differences in anatomy of airways and lungs. The mechanical load of obesity affects lung growth causing reduced pulmonary function38. Monika Cembrzynska –
gamma by Bronchoalveolar leucocytes from patients with bronchial asthma.The pathological changes in the asthmatics are associated with increased release of eosinophils and neutrophils by eosinophil activating factor ,granulocyte monocyte colony stimulating factor or interferon gamma, all these are facilitated into the site of allergic reactions. Insitu secretion of proinflammatory cytokines causes development of inflammatory reaction39.
Chun Kwok Wong et al41 found that leptin upregulated the expression of ICAM -1and CD – 18, whereas it suppresses ICAM -3 and L –Selectin. Intra cellular adhesion molecule ICAM- 1 has demonstrated to potentiate inflammatory process in childhood asthma. The interaction of ICAM-1 and integrins were proven to be essential for recruitment of transendothelial migration of eosinophils which is a basic pathogenesis in bronchial asthma.
The findings of our study were consistent with the above and other studies14 showing a significant positive relationship with body mass index and serum leptin. A plausible explanation for this observation could be exaggerated proinflammatory role of alveolar macrophages in obese individuals. The primary alveolar macrophage derived from overweight and obese asthmatics generated higher levels of pro inflammatory cytokines after stimulation with leptin than the macrophage derived from normal weight asthmatics or obese nonasthmatics10.
exacerbation and hence could not study the effects of asthma exacerbation or serum leptin levels.
Another study in the pediatric population between age groups of 2 years to 14 years by Asya Tanju et al11 investigated the association between clinical severity of childhood asthma and serum leptin levels. The authors also explored the predictive value of serum leptin in terms of severity of asthma. In this study, the subjects were divided into three groups such as intermittent asthma, mild persistent asthma and moderate persistent asthma11. The authors concluded that leptin level correlated well with severity of asthma in children and this was associated with severity of inflammation in children. Interestingly this study showed a negative correlation between body mass index and serum leptin levels.
body mass index and serum leptin levels, there was no relationship between leptin and triglyceride, HDL cholesterol, VLDL cholesterol, eosinophils and total serum IgE levels. There was positive correlation between total cholesterol and LDL cholesterol levels. They did not find any relationship between allergic rhinitis, asthma and serum levels of leptin. They concluded that there was no effect of inhaled steroids or intra nasal steroids on serum leptin levels. Thus the relationship between serum leptin and asthma remains controversial. Some studies as cited above, involving adults and children population concluded that there is an association between serum leptin and asthma though the mechanisms could not be explained beyond doubt. F. Erel et al and our study did not establish such association. Almost all studies including ours were limited by smaller sample size which could be a reason for such contradicting results from these studies though role of leptin in asthma cannot be fully denied.
association between serum leptin and various components of asthma related quality of life, we found that serum leptin correlated with Asthma Quality of life total score (r2 = 0.256,p = 0.049),AQLQ Activity score (r2 = 0.274,p = 0.034) and AQLQ symptoms score (r2 =0.253, P =0.050).This is the most unique finding in our study, as per the review of literature we found no study which established the relationship between serum leptin and quality of life.
LIMITATIONS
Other limitations in our study include smaller sample size. The current study could serve as pilot data to extend our investigations in order to understand clearly the actual role of serum leptin in asthma as also the mechanisms involved. Investigating genetic factors associated with serum leptin levels were not analyzed which could have added great value to our study.
CONCLUSION
RECOMMENDATIONS
Relationship between serum leptin and asthma has not yet been established well despite of sound scientific ground to expect a pathogenetic role of leptin in asthma. Such a role if present could only be established through well designed studies with larger sample size and involving various clinical, physiological and laboratory parameters. Simultaneous investigation of these variables along with other biomarkers and genetic studies can enable us to establish mechanisms involving serum leptin in asthma. Therapeutic implications of serum leptin should also be studied in asthma. Thus we recommend large scale observational and interventional studies leading to better understanding of the role of serum leptin in asthma.
BIBLIOGRAPHY
1. Global Initiative For Asthma - GINA Guidelines Updated 2015.
2. Murray and Nadels’s text book of Respiratory Medicine.
3. Mathew Masoli, Denise Fabian, shaun Holtet al. The global Burden of asthma : executive summary of the GINA dissemination committee report, Journal of Allergy 2004 :59:469-478.
4. M Gonzalez-Garcia, A Caballero ,C Jaramill et al. Prevalence, Risk factors and under diagnosis of asthma and wheezing in adults 40 years and older : A population based study, Journal of asthma vol 52,2015 – Issue 8.
5. Xiao Chloe Wan , Prescott G. Wooddruff, Biomarkers in severe asthma, Immunol Allergy Clin N Arm 36 (2016)547-557.
6. SJ Wadsworth ,DD Sin and DR Dorscheid, Clinical update on the use of biomarkers of airway inflammation in the management of asthma Journal of Asthma and Allergy : 30 June 2011 volume 2011 : 4 pages 77-86.
8. Adel Salah , Mostafa Ragab,et al . Leptin and adiponectin are valuble serum markers explaining obesity /bronchial asthma interrelationship, Egyptian Journal of chest diseases and tuberculosis(2015)64,529-533.
9. Juanita H.J. Vernooy , Niki D.J,et al. Leptin as a regulator of pulmonary immune response: Involvement in respiratory diseases. Pulmonary pharmacology and therapeutics, August 2013 Vol.26 (4):464 – 472.
10. Foteini Malli , Andrana et al.The role of leptin in Respiratory system : an over view. Malli et al . Respiratory Research 2010,11:152.
11. Asya Tanju, Ferhat Cekmez et al. Association between clinical severity of childhood asthma and serum leptin levels. Indian J Pediatrics (March 2011) 78 : 291 – 295.
12. S.Kaur,V.K.Gupta,et al. Elevated levels of Mannan binding leptin (MBL) and eosinophilia in patients of bronchial asthma with allergic rhinitis and allergic bronchopulmonary aspergillosis associate a novel ionotropic polymorphism in MBL. Clinical And Experimental Immunology, November 2005.
13. Association between leptin and asthma in adults. Thorax 2006 ;61: 300-305.
15. Alpaydin AO, et al. Asthma control test and Asthma quality of life questionnaire association in adults. J Allergy Asthma Immunol , 2012 Dec:11(4): 301 – 7.
16. Elizabeth Juniper’s ,Asthma quality of life questionnaire(AQLQ, AQLQ (S), Mini AQLQ and Acute AQLQ ) background, administration and analysis, 1991.
17. Elizabeth Juniper’s, Asthma control questionnaire, background, administration and analysis, 2004.
18. Pavord ID, Ward R et al. Induced sputum eicosanoid concentration in asthma. Am J Respir Crit Care Med. 1999 Dec: 160 (6) : 1905 – 9.
19. Anton Jatakanon, Sam Lim et al. Changes in sputum eosinophil counts predict loss of asthma control.AM J Respir Crit Care Med 2000:161:64 – 72.
20. Akshay Sood and Stephanie A. Shore . Leptin , Adiponectin and Resistin basic mechanisms through population studies. Journal of Allergy, Volume 2013.