Recombinant Porcine Reproductive and Respiratory Syndrome
Virus Expressing Membrane-Bound Interleukin-15 as an
Immunomodulatory Adjuvant Enhances NK and
␥␦
T Cell
Responses and Confers Heterologous Protection
Qian M. Cao,
aYan-Yan Ni,
aDianjun Cao,
aDebin Tian,
aDanielle M. Yugo,
aC. Lynn Heffron,
aChristopher Overend,
aSakthivel Subramaniam,
aAdam J. Rogers,
aNicholas Catanzaro,
aTanya LeRoith,
aPaul C. Roberts,
a*
Xiang-Jin Meng
aaDepartment of Biomedical Sciences and Pathobiology, Virginia-Maryland College of Veterinary Medicine,
Virginia Polytechnic Institute and State University (Virginia Tech), Blacksburg, Virginia, USA
ABSTRACT
Cytokines are often used as adjuvants to improve vaccine
immuno-genicity, since they are important in initiating and shaping the immune response.
The available commercial modified live-attenuated vaccines (MLVs) against porcine
reproductive and respiratory syndrome virus (PRRSV) are unable to mount sufficient
heterologous protection, as they typically induce weak innate and inadequate T cell
responses. In this study, we investigated the immunogenicity and vaccine efficacy of
recombinant PRRSV MLVs incorporated with the porcine cytokine interleukin-15
(IL-15) or IL-18 gene fused to a glycosylphosphatidylinositol (GPI) modification signal
that can anchor the cytokines to the cell membrane. We demonstrated that both
cy-tokines were successfully expressed on the cell membrane of porcine alveolar
mac-rophages after infection with recombinant MLVs. Pigs vaccinated with recombinant
MLVs or the parental Suvaxyn MLV had significantly reduced lung lesions and viral
RNA loads in the lungs after heterologous challenge with the PRRSV NADC20 strain.
The recombinant MLVs SUV-IL-15 and SUV-IL-18 recovered the inhibition of the NK
cell response seen with Suvaxyn MLV. The recombinant MLV SUV-IL-15 significantly
increased the numbers of gamma interferon (IFN-
␥
)-producing cells in circulation at
49 days postvaccination (dpv), especially for IFN-
␥
-producing CD4
⫺CD8
⫹T cells and
␥␦
T cells, compared to the Suvaxyn MLV and 18. Additionally, MLV
SUV-IL-15-vaccinated pigs also had elevated levels of
␥␦
T cell responses observed at 7 dpv,
49 dpv, and 7 days postchallenge. These data demonstrate that the recombinant
MLV expressing membrane-bound IL-15 enhances NK and T cell immune responses
after vaccination and confers improved heterologous protection, although this was
not statistically significant compared to the parental MLV.
IMPORTANCE
Porcine reproductive and respiratory syndrome (PRRS) has arguably
been the most economically important global swine disease, causing immense
economic losses worldwide. The available commercial modified live-attenuated
vac-cines (MLVs) against PRRS virus (PRRSV) are generally effective against only
homolo-gous or closely related virus strains but are ineffective against heterolohomolo-gous strains,
partially due to the insufficient immune response induced by the vaccine virus. To
improve the immunogenicity of MLVs, in this study, we present a novel approach of
using porcine IL-15 or IL-18 as an adjuvant by directly incorporating its encoding
gene into a PRRSV MLV and expressing it as an adjuvant. Importantly, we directed
the expression of the incorporated cytokines to the cell membrane surface by fusing
the genes with a membrane-targeting signal from CD59. The recombinant MLV virus
expressing the membrane-bound IL-15 cytokine greatly enhanced NK cell and
␥␦
T
cell responses and also conferred improved protection against heterologous
chal-lenge with the PRRSV NADC20 strain.
Received4 January 2018Accepted9 April 2018
Accepted manuscript posted online11 April 2018
CitationCao QM, Ni Y-Y, Cao D, Tian D, Yugo DM, Heffron CL, Overend C, Subramaniam S, Rogers AJ, Catanzaro N, LeRoith T, Roberts PC, Meng X-J. 2018. Recombinant porcine reproductive and respiratory syndrome virus expressing membrane-bound interleukin-15 as an immunomodulatory adjuvant enhances NK and γδ T cell responses and confers heterologous protection. J Virol 92:e00007-18. https://doi.org/10.1128/JVI.00007-18.
EditorTom Gallagher, Loyola University Medical Center
Copyright© 2018 American Society for Microbiology.All Rights Reserved.
Address correspondence to Xiang-Jin Meng, xjmeng@vt.edu.
*Present address: Paul C. Roberts, Influenza, SARS and Other Viral Respiratory Disease Section, NIAID, NIH, Rockville, Maryland, USA.
crossm
on November 6, 2019 by guest
http://jvi.asm.org/
KEYWORDS
modified live-attenuated vaccine, MLV, membrane-bound IL-15,
adjuvant, immunogenicity, NK cells,
␥␦
T cells
P
orcine reproductive and respiratory syndrome (PRRS) is arguably the most
eco-nomically important global swine disease, causing immense economic losses
worldwide, with an estimated annual loss of $664 million in the United States alone (1,
2). The causative agent, PRRS virus (PRRSV), is an enveloped RNA virus that belongs to
the family
Arteriviridae
in the order
Nidovirales
(3). The genome of PRRSV is a
single-stranded positive-sense RNA molecule of approximately 15 kb, consisting of at least 10
open reading frames (ORFs): ORF1a, ORF1b, ORF2a, ORF2b, ORF3 to ORF5, ORF5a, ORF6,
and ORF7 (4, 5). As is the case for all arteriviruses, the structural proteins of PRRSV are
expressed from a set of 3
=
-coterminal subgenomic mRNAs (sgmRNAs) using the
dis-continuous mRNA transcription mechanism (6, 7).
Sequence analyses revealed that PRRSV can be divided into two genotypes,
Euro-pean type 1 and North American type 2 (8). There is also high genetic diversity within
each genotype, which is often caused by mutations and recombination among strains
(9). Type 2 PRRSV was systematically classified into 9 genetically distinct lineages based
on the ORF5 gene sequences of 8,624 PRRSV strains (10). The Suvaxyn PRRSV modified
live-attenuated vaccine (MLV) used in this study is derived from PRRSV isolate ISU-55,
which was isolated in the early 1990s and belongs to genetic lineage 5 of type 2 PRRSV
(8, 11, 12). A heterologous PRRSV strain, NADC20, used as the challenge virus in this
study, belongs to genetic lineage 9 and shares approximately 87% amino acid
se-quence identity in ORF5 with the PRRSV Suvaxyn MLV.
Current commercially available PRRSV vaccines include both MLVs and inactivated
vaccines with limited efficacy (13–15). MLVs are generally effective against homologous or
closely related strains but are largely ineffective against heterologous strains (16). The
ineffectiveness of the commercial vaccines is due mainly to the significant antigenic
variations among circulating viruses and is also due to a compromised immune response
induced by PRRSV upon exposure or vaccination. Since innate cytokines or costimulatory
molecules are critically important in activating antigen-presenting cells (APCs) and shaping
adaptive immunity, the use of these molecules as vaccine adjuvants has been explored in
numerous studies (17), but none were tested for their adjuvant effects on PRRSV MLVs.
Interleukin-15 (IL-15), which has been shown to promote the development and function
of cytotoxic T cells and NK cells (18), is thus a good candidate to augment the immune
response of PRRSV MLVs. Additionally, IL-18, a gamma interferon (IFN-
␥
)-inducing factor
similar to IL-12, has also been reported to effectively enhance Th1 immunity and NK cell
function (19, 20). Furthermore, the coding regions of bioactive IL-15 and IL-18 are both
⬍
500 bp, thus making them suitable for insertion into the PRRSV genome for
more-stable expression without affecting the viability of recombinant viruses.
As a glycosylphosphatidylinositol (GPI)-anchored protein, porcine CD59 is
constitu-tively expressed on leukocytes and is usually concentrated in the lipid raft, which is
thought to function as a platform for many cell-to-cell contact events (21). In order to
decrease the adverse systemic effects of soluble cytokines in circulation, we
incorpo-rated the gene sequence of porcine IL-15 (pIL-15) or IL-18 (pIL-18) fused with the
GPI-anchoring signal from porcine CD59 into the PRRSV Suvaxyn MLV infectious clone.
These recombinant PRRSV MLVs were rescued and used to infect porcine alveolar
macrophages (PAMs), and the expression of pIL-15 and pIL-18 on the cell surface was
characterized. Nursery pigs were vaccinated with recombinant PRRSV MLVs expressing
cytokines, followed by challenge with a heterologous PRRSV strain, NADC20. The
adjuvant effects of the membrane-bound cytokines on anti-PRRSV protective immunity,
including NK cell and T cell responses, were investigated.
RESULTS
The GPI modification signal from pCD59 and the transmembrane region from
influenza virus HA successfully target cytokine expression to the cell plasma
membrane surface.
We generated expression plasmids in which the coding regions of
on November 6, 2019 by guest
http://jvi.asm.org/
mature pIL-15 or pIL-18 were individually fused with a short N-terminal signal sequence
from hemagglutinin (HA) of influenza virus (influenza virus A/WSN/33; GenBank
acces-sion no.
J02176.1
) and a C-terminal GPI modification signal from pCD59. Additionally,
we also tested the influenza virus HA transmembrane (HATM) region as an alternative
to the GPI modification signal for targeting cytokine expression to the cell surface, since
the HATM region, containing the transmembrane domain, the cytoplasmic tail, and a
portion of the short stalk region, was shown previously to direct fusion proteins to the
lipid raft of the cell surface (22–24). The resulting plasmids were designated
pIL-15-CD59GPI, pIL-15-HATM, pIL-18-pIL-15-CD59GPI, and pIL-18-HATM, respectively. Their plasma
membrane-targeting abilities in cells transfected with each of these plasmids were
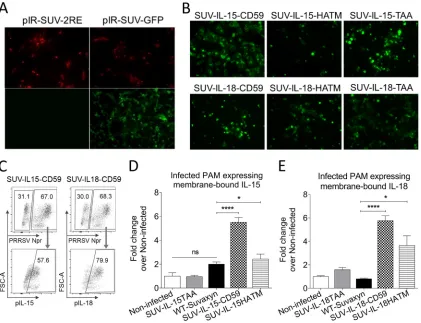
characterized. As expected, substantial cell surface expression of IL-15 (Fig. 1A and B)
or IL-18 (Fig. 1C and D) was detected in cells transfected with plasmids containing
cytokines fused to either the CD59 GPI signal or the HATM region, while only minimal
surface expression of cytokines was found in cells transfected with the control plasmid
pIL-15-TAA or pIL-18-TAA with only an N-terminal signal sequence preceding the
cytokine genes. These results suggest that both the GPI-anchoring signal from pCD59
FIG 1Characterization of the cell plasma membrane-targeting abilities of the GPI modification signal from pCD59 and the HA transmembrane (HATM) region. Porcine kidney PK-15 cells were transfected with individual expression plasmids, fused or not fused with the respective membrane-targeting sequence. Cell surface cytokines were stained with anti-IL-15- or anti-IL-18-specific antibody and analyzed by flow cytometry. (A and C) Representative histograms showing the frequencies of cells expressing membrane-bound cytokines in individual transfections. (B and D) Above-mentioned frequencies on average for each group. Asterisks indicate a statistically significant difference between the designated groups (**,P⬍0.01;
***,P⬍0.001).
on November 6, 2019 by guest
http://jvi.asm.org/
[image:3.585.42.426.74.455.2]and the transmembrane region from HA can serve as appropriate plasma
membrane-targeting sequences for the expression of selected cytokines.
Successful rescue of vaccine virus from a DNA-launched infectious clone of
PRRSV Suvaxyn MLV.
The complete genomic sequence of the PRRSV Suvaxyn MLV
was determined by using primers based on the reported partial sequence of parental
strain ISU-55 of the Suvaxyn MLV and the conserved sequences of type 2 PRRSV strains.
5
=
rapid amplification of cDNA ends (RACE) and 3
=
RACE were used to determine the
extreme 5
=
- and 3
=
-end sequences of the PRRSV Suvaxyn MLV genome. A
DNA-launched infectious clone of PRRSV Suvaxyn MLV was successfully generated according
to similar strategies reported previously (25). The PRRSV Suvaxyn MLV genome fused
with ribozyme fragments was successfully assembled in a modified vector,
pIRES-EGFP2, downstream of a cytomegalovirus (CMV) promoter, which is used for
in vitro
transcription (Fig. 2A). The resulting full-length clone of the PRRSV Suvaxyn MLV was
designated pIR-SUV. The viable infectious MLV virus was successfully rescued from this
DNA-launched infectious clone in BHK-21 cells and MARC-145 cells, as previously
described (25) (data not shown). The sequence of the rescued MLV virus was confirmed
by reverse transcription-PCR (RT-PCR) amplification and sequencing analysis of the
supernatant of MARC-145 cells infected with the rescued Suvaxyn MLV virus.
Successful construction and rescue of viable recombinant PRRSV MLVs
ex-pressing pIL-15 or pIL-18.
To determine whether porcine cytokines could be
incor-porated into the PRRSV genome, thus being expressed by the virus in the
membrane-bound form, we first generated a new DNA-launched PRRSV MLV infectious clone that
allows for foreign gene insertion and expression. Two unique restriction enzyme sites,
SbfI and PacI, were introduced into the nonoverlapping region between ORF1b and
ORF2a of the infectious clone pIR-SUV (Fig. 2B). Therefore, any foreign gene sequence
can be inserted into this modified PRRSV MLV infectious clone between the SbfI and
PacI sites and subsequently transcribed into sgmRNAs guided by body
transcription-regulating sequence 2 (TRS2) that is embedded in ORF1b and originally responsible for
ORF2a transcription. In order to compensate for ORF2a transcription, a synthetic body
TRS with a flanking sequence of a total of 40 bp (Fig. 2C) was inserted immediately after
the PacI site and upstream of the start codon of ORF2a. The resulting PRRSV MLV
infectious clone was designated pIR-SUV-2RE (Fig. 2B). Viable infectious viruses were
successfully rescued from pIR-SUV-2RE (Fig. 3A). Subsequently, we demonstrated that
pIR-SUV-2RE can also be used as a PRRSV expression cassette for foreign gene insertion,
as a green fluorescent protein (GFP) sequence was cloned into the vector (Fig. 2D), and
a GFP-expressing PRRSV was successfully rescued (Fig. 3A).
The nucleotide sequence of mature pIL-15 or pIL-18 with a short N-terminal signal
sequence from HA as well as the above-mentioned C-terminal pCD59-GPI signal or
C-terminal HATM region, respectively, was incorporated into pIR-SUV-2RE (Fig. 2D).
Recombinant MLV viruses, designated CD59, SUV-IL-18-CD59,
SUV-IL-15-HATM, and SUV-IL-18-SUV-IL-15-HATM, were successfully rescued (Fig. 3B). Two additional control
recombinant MLV viruses, SUV-IL-15TAA and SUV-IL-18TAA, without a
membrane-targeting signal (Fig. 2D), were also rescued similarly (Fig. 3B). The rescued viruses were
sequenced and confirmed to be genetically stable for at least 8 serial passages in cell
culture. The SUV-IL-15-CD59 and SUV-IL-18-CD59 viruses replicated at lower levels
in
vitro
(0.5 to 1 log units lower at passages 4 to 6) than the parental Suvaxyn virus (data
not shown).
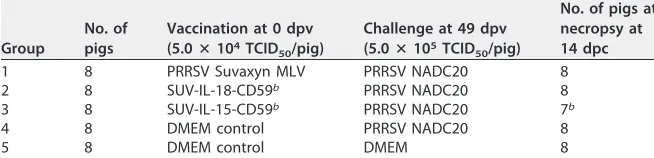
Recombinant PRRSV MLVs successfully express membrane-bound pIL-15 or
pIL-18 on the plasma membrane of infected porcine alveolar macrophages.
In
order to determine if the inserted cytokine can be expressed by the recombinant MLVs
on the plasma membrane of infected cells, PAM cells were infected with each of the
recombinant PRRSV MLVs at a multiplicity of infection (MOI) of 0.1. At 20 h postinfection
(hpi), surface cytokine expression as well as the intracellular viral N protein were
detected by flow cytometry, as described previously (26). Infected PAMs can be divided
into PRRSV N-positive or -negative cells, and the frequencies of cells expressing
membrane-bound cytokines in the PRRSV N-positive population were compared
on November 6, 2019 by guest
http://jvi.asm.org/
FIG 2Construction of DNA-launched infectious clones of the PRRSV Suvaxyn MLV and recombinant PRRSV MLVs with foreign genes incorporated in the vicinity of the ORF1b/2 junction region. (A) Construction of a DNA-launched full-length clone of the PRRSV Suvaxyn MLV. The 5 genomic fragments, overlapping each other, all contain unique restriction enzyme sites for full-length viral genome assembly and are assembled into a modified pIRES-EGFP2 vector downstream of a CMV promoter. The resulting infectious clone of the PRRSV Suvaxyn MLV is designated pIR-SUV. (B) pIR-SUV contains a nonoverlapping region of one single nucleotide between ORF1b and ORF2a. pIR-SUV-2RE serves as a PRRSV MLV expression cassette for foreign gene insertion. The two introduced unique restriction enzyme sites, SbfI and PacI, are indicated by boldface type and underlining with italic type, followed by the introduced synthetic body TRS with flanking sequences. The conserved junction motif for the synthetic body TRS is boxed. The asterisks beneath the underlined sequences indicate stop codons of the corresponding ORFs. (C) Hairpin structure of the synthesized body TRS and its flanking region. (D) Nucleotide sequences of GFP-inserted recombinant PRRSV and cytokine-incorporated recombinant PRRSV MLVs in the vicinity of the ORF1b/2 junction region. The recombinant PRRSV MLV SUV-IL-15-CD59 contains a GPI modification signal at the C terminus, while SUV-IL-15-HATM contains the HATM region. The recombinant PRRSV MLVs CD59 and SUV-IL-18-HATM have an additional N-terminal signal peptide sequence from HA. SUV-IL-15-TAA and SUV-IL-18-TAA contain only the cytokine-coding regions.
on November 6, 2019 by guest
http://jvi.asm.org/
[image:5.585.42.378.73.544.2](Fig. 3C). As expected, compared to noninfected cells, there was a significant increase
in the plasma membrane surface expression level of IL-15 (Fig. 3D) or IL-18 (Fig. 3E) on
PAM cells infected by recombinant SUV-IL-15-CD59 or SUV-IL-18-CD59. In contrast, only
a few cells expressing membrane-bound cytokines were detected among cells infected
with the Suvaxyn SUV-IL-15TAA and SUV-IL-18TAA viruses, which contain cytokine
genes but without the membrane-targeting signal. Interestingly, the HATM region
appeared to be less efficient in terms of tethering cytokines onto the plasma
mem-brane, as shown by the results for cells infected with the recombinant SUV-IL-15HATM
and SUV-IL-18HATM viruses. Given the fact that PAMs, as the natural host cells for
PRRSV, rapidly die or undergo apoptosis within 24 to 30 h postinfection
in vitro
, in this
study, we chose the GPI modification signal from pCD59, with a higher potency for
expressing membrane-bound cytokines, in subsequent investigations of the
recombi-nant PRRSV MLVs.
Recombinant PRRSV MLVs SUV-IL-15 and SUV-IL-18, but not the parental
PRRSV Suvaxyn MLV, activate NK cells after vaccination.
To evaluate the
immuno-modulatory effects of the membrane-bound cytokines expressed by the recombinant
PRRSV MLVs as adjuvants, we conducted a vaccination-challenge study with 3-week-old
piglets. Groups of pigs (Table 1) were vaccinated with the parental PRRSV Suvaxyn MLV,
FIG 3Rescue and characterization of recombinant PRRSV MLVs expressing membrane-bound cytokines. All the recombinant PRRSVs were rescued as live infectious viruses, as confirmed by an IFA with a PRRSV-specific monoclonal antibody. (A, top) MARC-145 cells were infected with passage 1 virus rescued from pIR-SUV-2RE or passage 1 virus rescued from pIR-SUV-GFP and stained with an anti-PRRSV N monoclonal antibody (SDOW17). (Bottom) GFP fluorescence in fresh cells after infection with the SUV-2RE or SUV-GFP virus. (B). Similarly, recombinant MLVs incorporated with the IL-15 or IL-18 gene were rescued and confirmed by an IFA. (C to E) PAMs were infected with the indicated viruses, followed by surface staining with anti-IL-15 or anti-IL-18 antibodies and intracellular staining of anti-PRRSV N protein at 20 hpi. (C) Representative FACS data showing that the PRRSV N-positive cells were further analyzed for the surface expression of cytokines. In the noninfected control group, frequencies of cytokine-expressing cells in the PRRSV N-negative population were calculated. FSC-A, forward scatter area. (D and E) The frequencies of cells expressing surface IL-15 (D) and IL-18 (E) in individual infections were compared with those in noninfected cells. Asterisks indicate statistical significance between the designated groups, as determined by one-way ANOVA (*,P⬍0.05;****,P⬍0.0001; ns, not significant).
on November 6, 2019 by guest
http://jvi.asm.org/
[image:6.585.43.464.71.394.2]the recombinant MLV SUV-IL-15-CD59, the recombinant MLV SUV-IL-18-CD59, and
Dulbecco’s modified Eagle’s medium (DMEM) via a combination of intranasal and
intramuscular routes. At 49 days postvaccination (dpv), the animals were challenged
with a high dose of a heterologous PRRSV (strain NADC20) to determine the protective
efficacy of the recombinant PRRSV MLVs.
We found that porcine NK cells (CD3
⫺CD16
⫹) in the circulation can be further
categorized into two subgroups, CD8
⫺NK and CD8
⫹NK cells, according to CD8
expression (Fig. 4A), although the functional difference between these two subgroups
is not well known (20, 27). At 7 dpv, the frequencies of NK cells were decreased in pigs
vaccinated with the PRRSV Suvaxyn MLV compared to those in nonvaccinated pigs, and
these decreases were observed mainly in the subpopulation of CD8
⫹NK cells (Fig. 4B).
However, we did not find such a reduction of NK cells in recombinant PRRSV MLV
SUV-IL-15- or SUV-IL-18-vaccinated pigs.
Additionally, at 7 dpv, there was an increase in the frequency of IFN-
␥
-producing
CD8
⫺NK cells in the recombinant SUV-IL-15-vaccinated group compared to that in the
parental Suvaxyn MLV group (Fig. 4C). Later, at 49 dpv, Suvaxyn MLV-vaccinated but
not recombinant MLV SUV-IL-15- or SUV IL-18-vaccinated pigs had significantly lower
numbers of total IFN-
␥
-producing NK cells and IFN-
␥
⫹CD8
⫹NK cells than did the
nonvaccinated pigs (Fig. 4D). These data suggest that the Suvaxyn MLV inhibited the
proliferation and IFN-
␥
production of NK cells, whereas the recombinant MLVs
SUV-IL-15 and SUV-IL-18 greatly ameliorated this inhibition.
Recombinant MLV SUV-IL-15 facilitates long-term
␥␦
T cell responses and
greatly increases the number of IFN-
␥
-producing T cells during late stages of
vaccination.
To evaluate T cell responses after vaccination, we first analyzed the
surface expression of CD107a as an indicator of lymphocyte degranulation. At 7 dpv,
the total numbers of CD107a-expressing T cells were comparable among all groups
(data not shown). However, the Suvaxyn MLV-vaccinated and recombinant MLV
SUV-IL-15-vaccinated pigs had substantially increased numbers of CD107a
⫹␥␦
T cells
compared to those in nonvaccinated pigs (Fig. 5B). We also found increased total
numbers of
␥␦
T cells in these 2 vaccinated groups (Fig. 5C), which may partially explain
the enhanced CD107a expression from
␥␦
T cells at 7 dpv. Similarly, at 49 dpv, total
numbers of CD107a-expressing T cells were comparable among different groups (Fig.
5D), but only the recombinant MLV SUV-IL-15-vaccinated group had increased numbers
of both total T cells (Fig. 5C) and CD107a-expressing
␥␦
T cells (Fig. 5E) compared to
those in the Suvaxyn MLV-vaccinated group.
We also evaluated IFN-
␥
production in T cells after vaccination. At 7 dpv, the
numbers of IFN-
␥
-producing T cells were comparable among different groups (data not
[image:7.585.41.368.106.185.2]shown). In contrast, at 49 dpv, the group vaccinated with the recombinant MLV
SUV-IL-15, but not with the Suvaxyn MLV or the recombinant MLV SUV-IL-18, had a
TABLE 1Experiment design for the vaccination-challenge study in pigs to evaluate the immunogenicity and efficacy of the recombinant PRRSV MLVs expressing membrane-bound cytokinesa
Group
No. of pigs
Vaccination at 0 dpv (5.0ⴛ104TCID
50/pig)
Challenge at 49 dpv (5.0ⴛ105TCID
50/pig)
No. of pigs at necropsy at 14 dpc
1 8 PRRSV Suvaxyn MLV PRRSV NADC20 8
2 8 SUV-IL-18-CD59b PRRSV NADC20 8
3 8 SUV-IL-15-CD59b PRRSV NADC20 7b
4 8 DMEM control PRRSV NADC20 8
5 8 DMEM control DMEM 8
aPigs were vaccinated with the respective recombinant PRRSV MLVs by a combination of intranasal (half) and intramuscular (half) inoculation routes. The pigs were subsequently challenged with a heterologous PRRSV strain, NADC20, by intramuscular inoculation. PRRSV Suvaxyn MLV is the commercial vaccine virus rescued from a DNA-launched PRRSV infectious clone, pIR-Suvaxyn. SUV-IL-15-CD59 and SUV-IL-18-CD59 are recombinant PRRSV MLVs expressing plasma membrane-bound IL-15 and IL-18, respectively. TCID50, 50%
tissue culture infective dose.
bOne pig died from intestinal hemorrhage unrelated to this study.
on November 6, 2019 by guest
http://jvi.asm.org/
significant increase in the total number of IFN-
␥
-producing T cells compared to other
groups (Fig. 5F). Moreover, there were substantially increased numbers of IFN-
␥
⫹CD8
⫹T cells and IFN-
␥
⫹␥␦
T cells among T cells in recombinant MLV SUV-IL-15-vaccinated
pigs compared to those in the Suvaxyn MLV-vaccinated pigs (Fig. 5G). These results
demonstrate that the recombinant MLV SUV-IL-15, but not the recombinant MLV
SUV-IL-18, greatly enhanced both the proliferation and anti-PRRSV functions of
␥␦
T
cells, as indicated by the increased levels of expression of the degranulation marker
CD107a and intracellular IFN-
␥
production. More importantly, the recombinant MLV
expressing IL-15 was able to activate IFN-
␥
-producing CD8
⫹T cells at a late stage of
vaccination.
Recombinant MLV SUV-IL-15 enhances CD107a surface expression in
␥␦
T cells
after heterologous PRRSV challenge.
To investigate the protective immune response
against heterologous challenge with PRRSV strain NADC20, we analyzed both
PRRSV-specific T cells and NK cells at 7 days postchallenge (dpc). Different from the time point
of 49 dpv, the numbers of IFN-
␥
⫹T cells in the circulation were comparable among the
groups, whereas the numbers of CD107a-expressing T cells at 7 dpc in recombinant
MLV SUV-IL-15-vaccinated pigs increased significantly compared to those in Suvaxyn
MLV-vaccinated pigs or to those in the unvaccinated and nonchallenged DMEM/DMEM
control pigs (Fig. 6A and B). More specifically, the numbers of both activated
␥␦
T cells
(CD107a
⫹or IFN-
␥
⫹) and total
␥␦
T cells in the recombinant MLV SUV-IL-15 vaccination
group were elevated compared to those in the Suvaxyn MLV vaccination group (Fig. 6C
and D). Interestingly, a similarly increased CD107a
⫹or IFN-
␥
⫹␥␦
T cell response in the
DMEM group was also observed. Unlike the MLV SUV-IL-15 group, however, the total
number of
␥␦
T cells in the DMEM group was not increased compared to that in the
FIG 4NK cell responses after vaccination at 7 dpv and 49 dpv. PBMCs collected at 7 dpv and 49 dpv were restimulated with PRRSV NADC20. Cells were surface stained with anti-pig CD107a, CD3, CD8, and CD16 antibodies and intracellularly stained with IFN-␥antibody. (A) Gating strategies for NK cells. Porcine NK cells were pregated from PBMCs as CD3⫺CD16⫹cells based on lymphocyte morphology. They were further
divided into CD8⫹and CD8⫺subpopulations. CD107a and IFN-␥expression levels were then evaluated
in NK cells. Shown here are representative graphs. FSC-A, forward scatter area; SSC-A, side scatter area. (B) NK cells in circulation at 7 dpv. (C) Total IFN-␥-producing NK cells and IFN-␥-producing CD8⫹NK
or CD8⫺NK cells among CD3⫺PBMCs at 7 dpv. (D) IFN-␥-producing NK cells at 49 dpv. Data on the
CD107a expression levels of NK cells are not shown. Asterisks indicate statistical significance between the designated groups, as determined by one-way ANOVA (*,P⬍0.05;**,P⬍0.01).
on November 6, 2019 by guest
http://jvi.asm.org/
[image:8.585.41.375.71.331.2]Suvaxyn MLV group or to that in the DMEM/DMEM group. There was no significant
difference in either CD107a expression or IFN-
␥
production from T cells in the
recom-binant MLV SUV-IL-18-vaccinated group compared to the Suvaxyn MLV-vaccinated
group.
Regarding the NK cell response, the nonvaccinated challenged-only pigs had the
fewest NK cells in circulation among the groups (Fig. 6E). The numbers of
CD107a-FIG 5T cell responses after vaccination at both 7 dpv and 49 dpv. PBMCs were collected from each pig at 7 dpv and 49 dpv. (A) Gating strategy for T cells. PBMCs were pregated as CD3⫹T cells and further divided
into CD4⫹, CD8⫹, CD4⫹CD8⫹(double-positive), and␥␦T cell subpopulations. CD107a and IFN-␥expression
levels were evaluated in these T cell populations. Only representative graphs are shown. FSC-A, forward scatter area; SSC-A, side scatter area. (B) Different subpopulations of T cells expressing surface CD107a at 7 dpv. (C) Frequencies of␥␦T cells among PBMCs at 7 dpv and 49 dpv. (D) Total CD3⫹T cells expressing
CD107a at 49 dpv. (E) Different T cell subpopulations expressing CD107a at 49 dpv. (F) Total T cells producing IFN-␥at 49 dpv. (G) Different T cell subpopulations producing IFN-␥at 49 dpv. Asterisks indicate statistical significance between the designated groups, as determined by one-way ANOVA (*,P⬍0.05;**, P⬍0.01;***,P⬍0.001).
on November 6, 2019 by guest
http://jvi.asm.org/
[image:9.585.40.377.69.541.2]expressing NK cells in this challenged-only group were also lower than those in the
other groups (except for the recombinant MLV SUV-IL-18 group), even though the
numbers of IFN-
␥
-producing NK cells were comparable among different groups (Fig.
6F). These results suggested that PRRSV NADC20, similar to PRRSV Suvaxyn MLV, likely
inhibited the proliferation of NK cells and impaired their degranulating activity.
Furthermore, the total circulating cells, regardless of cell type, were also evaluated
for the surface expression of CD107a and IFN-
␥
before and after PRRSV NADC20
challenge (Fig. 7A and B). At 49 dpv, recombinant MLV SUV-IL-15 significantly increased
the number of IFN-
␥
-producing cells in the peripheral blood compared to those in the
parental Suvaxyn MLV-vaccinated group as well as the nonvaccinated group,
suggest-ing an overall enhanced immunogenicity by the recombinant MLV expresssuggest-ing IL-15
after vaccination. However, after heterologous challenge with PRRSV NADC20, there
was no significant difference in numbers of IFN-
␥
-producing cells among the groups,
while numbers of CD107a-expressing cells were increased in both recombinant MLV
SUV-IL-15-vaccinated pigs and the unvaccinated challenged-only pigs.
Pigs vaccinated with recombinant MLV SUV-IL-15 have significantly reduced
numbers of lung lesions and viral RNA loads in lungs, similar to those of Suvaxyn
MLV-vaccinated pigs after heterologous challenge with PRRSV.
In order to measure
FIG 6Anti-PRRSV immune responses after heterologous PRRSV NADC20 challenge. PBMCs collected at 7 dpc were evaluated for CD107a-expressing and IFN-␥-producing lymphocytes. (A and B) Total CD3⫹T
cells expressing CD107a (A) or IFN-␥(B) among PBMCs. (C)␥␦T cells expressing CD107a or IFN-␥among PBMCs. (D) Frequencies of␥␦T cells among PBMCs. (E) Frequencies of NK cells among PBMCs. (F) Frequencies of total NK cells expressing CD107a or IFN-␥. Asterisks indicate statistical significance, as determined by one-way ANOVA (*,P⬍0.05;**,P⬍0.01).
on November 6, 2019 by guest
http://jvi.asm.org/
[image:10.585.49.358.68.435.2]the replication level of the challenge virus NADC20, viral RNA loads in the sera and lung
tissues were compared among different groups. Pigs vaccinated with the recombinant
MLVs SUV-IL-15 and SUV-IL-18 had serum viral RNA titers similar to those of pigs
vaccinated with the parental Suvaxyn MLV against heterologous virus challenge at both
7 dpc and 14 dpc (Fig. 8A and B). In the lung tissues at 14 dpc, there were lower viral
RNA loads in the recombinant MLV SUV-IL-15-vaccinated group than in the parental
Suvaxyn MLV- and MLV SUV-IL-18-vaccinated groups (Fig. 9A). All three vaccinated
groups had significantly lower viral RNA copy numbers than those in the unvaccinated
FIG 7CD107a-expressing or IFN-␥-producing cells regardless of cell type in the peripheral blood at 7 dpv, 49 dpv, and 7 dpc. PBMCs were collected at the indicated time points, and all the cells were evaluated for CD107a expression (A) and IFN-␥production (B). Asterisks indicate statistical significance, as determined by two-way ANOVA (*,P⬍0.05).
FIG 8Serum viral RNA loads after challenge with the PRRSV NADC20 strain at 7 dpc (A) and 14 dpc (B). Viral RNAs were extracted from serum samples at 7 and 14 dpc for the quantification of PRRSV RNA copy numbers in sera by qRT-PCR. The detection limit is calculated as 2 log10copies for each real-time PCR. Samples below the detection
limit were considered negative and labeled as 2 log10copies. Asterisks indicate statistical significance between the
designated groups, as determined by one-way ANOVA (**,P⬍0.01;***,P⬍0.001;****,P⬍0.0001).
on November 6, 2019 by guest
http://jvi.asm.org/
[image:11.585.118.293.74.322.2] [image:11.585.46.400.507.688.2]challenged-only group, indicating that the parental Suvaxyn MLV effectively reduced
lung viral RNA loads against heterologous PRRSV challenge. The microscopic lung
lesion scores for the recombinant MLV SUV-IL-15-vaccinated group were lower than
those for the Suvaxyn MLV-vaccinated, recombinant MLV SUV-IL-18-vaccinated, or
unvaccinated challenged-only group (Fig. 9B). There was no significant difference in the
gross lung lesions among three vaccinated groups (data not shown). The results
suggested that the recombinant MLV SUV-IL-15 exhibited enhanced protection,
al-though not statistically significant, against heterologous challenge, as evidenced by the
low lung viral RNA loads and low lung lesion scores compared to the parental Suvaxyn
MLV. It is important to point out that the parental Suvaxyn MLV is a commercial vaccine;
thus, any incremental improvement of the efficacy of an existing vaccine is an
achieve-ment, as significant improvement of the efficacy of a commercial vaccine is usually very
challenging.
Recombinant MLVs SUV-IL-15 and SUV-IL-18 express IL-15 or IL-18
in vivo
.
As
expected, the IL-15 expression level in the lung tissues of recombinant MLV
SUV-IL-15-vaccinated pigs was significantly higher than those in any of the other groups at 14
dpc (Fig. 9C). Similarly, the IL-18 expression level in lung tissues was also significantly
FIG 9Viral RNA loads, microscopic lesions, and cytokine expression in lung tissues after heterologous challenge with PRRSV NADC20 at 14 dpc. (A) Viral RNA loads in lung homogenates were determined by qRT-PCR. The detection limit is calculated as 2 log10copies for each real-time PCR. Samples below the detection limit were
considered negative and labeled as 2 log10copies. (B) Microscopic lung lesion scores at 14 dpc. (C and D) IL-15 (C)
or IL-18 (D) expression levels in lung tissue homogenates at 14 dpc were quantified by qRT-PCR and normalized to the value for the housekeeping geneYWHAZ, shown as fold changes over the values for the DMEM (unvacci-nated challenged-only) group. Asterisks indicate statistical significance between the desig(unvacci-nated groups, as deter-mined by one-way ANOVA (*,P⬍0.05;**,P⬍0.01;***,P⬍0.001).
on November 6, 2019 by guest
http://jvi.asm.org/
[image:12.585.47.403.71.435.2]higher in the recombinant MLV SUV-IL-18-vaccinated group than in the other groups
(Fig. 9D). These data indicate that the recombinant MLVs carrying the cytokine genes
successfully expressed IL-15 or IL-18 in pigs.
DISCUSSION
PRRSV infection usually induces insufficient activation of the immune response,
including a weak cell-mediated immune response and a strikingly delayed neutralizing
antibody response (28). This is partially due to virus inhibition of type I interferons
(29–31), tumor necrosis factor alpha (TNF-
␣
) (32), or other innate cytokines and
costimulatory molecules (26, 33, 34) that play an important role in priming APCs and in
bridging adaptive immunity (28, 32, 35, 36). This immune suppression by PRRSV has
remained a major challenge for developing effective MLVs against PRRSV (14, 37).
Therefore, novel strategies that can improve the efficacies of PRRSV MLVs are needed
for the effective control of PRRSV.
Previous studies evaluated the use of cytokines as adjuvants to improve the
immunogenicity and efficacy of the vaccines, either by codelivering the cytokines along
with vaccines in their bioactive form or, alternatively, by fusing their DNA sequences
with certain vaccines (38–40). In this study, for the first time, we investigated the
immunogenicity and the protective efficacy of recombinant PRRSV MLVs expressing
membrane-bound porcine cytokines as adjuvants. We present a novel approach of
using porcine IL-15 and IL-18 as adjuvants by incorporating their genes into
recombi-nant PRRSV MLVs, in attempts to induce cytotoxic NK cells during the innate immune
response as well as to enhance the adaptive T cell response. In the meantime, we also
attempted to direct cytokine expression to the plasma membrane of infected cells by
the recombinant PRRSV MLV, aiming to reduce cytokine diffusion into the circulation,
thus avoiding excessive systemic inflammation. Furthermore, these membrane-bound
cytokines are more likely to stimulate immune cells and facilitate cytotoxic lysis due to
their proximity to viral antigen presentation on the same cell.
By using a DNA-launched infectious clone of the commercial PRRSV Suvaxyn MLV as
the backbone, we successfully generated a panel of recombinant Suvaxyn MLVs
expressing cytokines. We further demonstrated that the recombinant MLVs can readily
infect MARC-145 cells and PAMs
in vitro
and express the cytokines of interest during
virus infection. Both the GPI signal and HATM region can direct cytokine protein
expression to the cell plasma membrane surface by expression plasmids. However, the
GPI modification signal from CD59, but not the HATM region, can tether the cytokines
onto the plasma membrane much more efficiently when they are expressed by the
recombinant PRRSV MLVs in PAMs. We speculate that since the sequence from CD59 is
of porcine origin, it has already been adapted for expression in PAMs and/or can be
expressed by the recombinant PRRSV with a higher efficiency than the HATM region.
When the recombinant MLVs were inoculated into pigs, the MLVs incorporated with the
cytokine gene fused to the GPI signal expressed IL-15 and IL-18
in vivo
, as demonstrated
by the elevated levels of IL-18 or IL-15 expression in the lung tissues, as measured by
RT-quantitative PCR (qRT-PCR) for gene transcription.
Among the circulating lymphocytes,
␥␦
T cells are a prominent subset in pigs,
especially in young pigs (27). Unfortunately, how
␥␦
T cells respond to PRRSV infection
has rarely been studied. Consistent with data from previous studies, we found that
␥␦
T cells are the most abundant porcine T cell subpopulation by making up more than
40% of the T cells across the entire time period of the animal study (data not shown).
We also found that
␥␦
T cells were much more responsive to PRRSV infection than
CD8
⫹, CD4
⫹CD8
⫹(double-positive [DP]), and CD4
⫹T cells. This is reflected by the
substantially expanded and activated
␥␦
T cells at an early stage of vaccination with the
Suvaxyn MLV or with the recombinant MLV SUV-IL-15. This is further demonstrated by
the significantly increased number of CD107a
⫹␥␦
T cells in the unvaccinated
challenged-only group 7 days after PRRSV NADC20 challenge.
It is also worth mentioning that CD8
⫹T cells and DP T cells are two primary T cell
populations that are capable of expressing surface CD107a as an indicator of
on November 6, 2019 by guest
http://jvi.asm.org/
cyte degranulation/cytotoxicity, followed by the
␥␦
T cell population, in response to
PRRSV infection (Fig. 5A and D and 6C). In contrast to
␥␦
T cells, together they compose
less than 30% of the total T cells (data not shown). CD4
⫹T cells, as expected, were the
least capable of expressing CD107a. These observations suggested that CD8
⫹T, DP T,
and
␥␦
T cells are likely major players in lymphocyte degranulation against PRRSV
infection. Whether
␥␦
T cells exert this cytotoxicity toward PRRSV-infected cells in a
major histocompatibility complex (MHC)-unrestricted manner or not is unclear.
Mean-while, NK cells were also capable of expressing surface CD107a at a considerable level
compared to T cells, suggesting their important role in degranulation and cytotoxicity
as well.
Early after vaccination with the parental Suvaxyn MLV, we observed significant
decreases in the numbers of total NK cells and IFN-
␥
⫹NK cells in pigs at 7 dpv. Similarly,
numbers of total NK cells and CD107a
⫹NK cells were significantly reduced in the
unvaccinated challenged-only pigs after PRRSV NADC20 challenge. NK cell-mediated
cytotoxicity was suppressed in PRRSV-infected PAMs, as reported previously (41), and
the results of our study reinforce the fact that PRRSV greatly impairs NK cell activation.
However, the PRRSV MLVs SUV-IL-15 and SUV-IL-18 greatly restored the proliferation of
NK cells and their functions, suggesting that IL-15 and IL-18 expressed by recombinant
MLVs as adjuvants can enhance the anti-PRRSV innate immune response.
At a late stage of vaccination, the total number of IFN-
␥
-producing T cells and,
moreover, the total number of cells in the circulation producing IFN-
␥
were significantly
increased only in the MLV SUV-IL-15 group compared to any of the other groups. This
suggests that the MLV SUV-IL-15 is able to elicit a long-term protective immune
response with enhanced IFN-
␥
production. When we analyzed the different T cell
subsets at 49 dpv, we noticed that the CD8
⫹and
␥␦
T cell responses in MLV
SUV-IL-15-vaccinated pigs were significantly more robust than those in Suvaxyn
MLV-vaccinated pigs but were not statistically different compared to those in unMLV-vaccinated
animals. This observation further implies that the parental Suvaxyn MLV may have
inhibitory effects, especially on inducing long-term CD8
⫹and
␥␦
T cell responses,
whereas the recombinant MLV SUV-IL-15 was able to overcome and/or offset this
suppression by enhancing IFN-
␥
production not only from these two T cell
subpopu-lations but also overall in the circulation. Again, these results from vaccination with the
Suvaxyn MLV substantiate the accumulating evidence for the compromised host
immune response induced by PRRSV.
After heterologous challenge with PRRSV NADC20, we found increases in the
numbers of both total T cells and total cells among peripheral blood mononuclear cells
(PBMCs) expressing surface CD107a only in the MLV SUV-IL-15 group, compared to
those in the Suvaxyn MLV or DMEM/DMEM control group. To a large extent, such an
increase seems to be attributed to the activated
␥␦
T cells. Interestingly, we also found
an increased
␥␦
T cell response in the unvaccinated challenged-only group at a level
similar to that in the MLV SUV-IL-15-vaccinated group. However, we noticed that the
number of total
␥␦
T cells was not increased in this group but was substantially
elevated in the MLV SUV-IL-15 group compared to the Suvaxyn MLV group or the
uninfected DMEM/DMEM control. Based on these observations, we postulate that the
␥␦
T cells typically responded, in a yet-to-be-defined manner, to the high level of PRRSV
replication in pigs of the challenged-only group at 7 dpc. In fact, it has been
demon-strated that porcine
␥␦
T cells may directly respond to pathogen-associated molecular
patterns (PAMPs) in the absence of APCs by recognition via Toll-like receptors (TLRs)
(42, 43) and can exert antiviral functions quickly after viral infection by producing IFN-
␥
and perforin and upregulating MHC class II (44, 45). On the other hand, it is important
to note that the MLV SUV-IL-15 enhanced both the proliferation and the antiviral
function of
␥␦
T cells at 7 dpv, 49 dpv, and 7 dpc, especially compared to the uninfected
(unvaccinated and unchallenged) DMEM/DMEM control group. Therefore, whether the
␥␦
T cell response that we observed in the unvaccinated challenged-only group at 7
dpc was sustainable and/or protective against NADC20 challenge is debatable, as
␥␦
T
cells were not profoundly proliferating in this group compared to the uninfected
on November 6, 2019 by guest
http://jvi.asm.org/
DMEM/DMEM control group. Clearly, further in-depth study is warranted to investigate
the role of
␥␦
T cells in anti-PRRSV immunity.
Taken together, the recombinant MLV expressing membrane-bound IL-15, but not
the parental Suvaxyn MLV or the recombinant MLV expressing IL-18, is able to enhance
the immunogenicity of the MLV mainly by recovering the early response of NK cells,
increasing the numbers of IFN-
␥
-producing T cells in the long term, and facilitating a
quick and robust
␥␦
T cell response against PRRSV NADC20 challenge.
At necropsy at 14 dpc, we found that the commercial Suvaxyn MLV significantly
reduced viral RNA loads in the serum and lung tissues against heterologous PRRSV
NADC20. The recombinant MLV SUV-IL-15 group had lower viral RNA loads in lung
tissues and lower microscopic lung lesion scores than those of the Suvaxyn MLV group
and the recombinant MLV SUV-IL-18 group. We believed that this incremental
enhance-ment of vaccine protection is attributed largely to the above-enhance-mentioned improved
immune response in recombinant MLV SUV-IL-15-vaccinated pigs. These data
demon-strate that the recombinant MLV expressing membrane-bound IL-15 can not only
augment immunogenicity after vaccination but also confer improved protection
against the heterologous PRRSV NADC20 strain. Additionally, it appears that PRRSV is
generally less efficient in stimulating IFN-
␥
production from T cells, since the numbers
of IFN-
␥
⫹T cells were increased only in the recombinant MLV SUV-IL-15-vaccinated
pigs at as late as 49 dpv. Therefore, it will be interesting in the future to evaluate the
use of other cytokines or chemokines as potential adjuvants expressed by recombinant
PRRSV MLVs.
In summary, in this study, we present a novel strategy of utilizing the discontinuous
transcription mechanism of PRRSV to express membrane-bound cytokines as vaccine
adjuvants upon infection with recombinant PRRSV MLVs. This is achieved by directly
incorporating the cytokine genes and fusing them to a selected plasma
membrane-targeting signal into a PRRSV MLV genome. Our results demonstrate that the cytokines
of interest are successfully expressed on the cell plasma membrane surface by the
recombinant PRRSV MLVs
in vitro
and
in vivo
. Therefore, this would potentially eliminate
the need for administering soluble adjuvants along with the vaccines. The
cytokine-incorporated MLVs could serve as potential vaccines with an improved immune
re-sponse and cross-protection against heterologous PRRSVs.
MATERIALS AND METHODS
Cells and viruses.BHK-21 and MARC-145 cells were cultured in DMEM supplemented with 10% fetal bovine serum (FBS) and antibiotics. PBMCs were isolated from heparinized blood of PRRSV-negative pigs and cryopreserved for later use. Upon thawing, PBMCs were cultured with RPMI 1640 medium supple-mented with 10% FBS, 25 mM HEPES, and antibiotics. The PRRSV Suvaxyn MLV used in this study (kindly provided by Zoetis Inc., Kalamazoo, MI) is a vaccine virus that was attenuated by serial passagesin vitro of wild-type PRRSV strain ISU-55. PRRSV ISU-55 was isolated from lungs of a diseased pig during a PRRS outbreak in Iowa in the early 1990s (46). PRRSV strain NADC20, of genetic lineage 9 (47), was kindly provided by Kelly Lager of the USDA National Animal Disease Center, Ames, IA.
Construction of expression vectors for membrane-bound IL-15 and IL-18.Porcine IL-15 (486 bp) and mature IL-18 (471 bp) were commercially synthesized by Integrated DNA Technologies Inc. (Cor-alville, IA) as gBlock fragments, designated pIL-15 and HAsp-pIL-18, respectively, both of which contain two flanking restriction enzyme sites (NheI and XhoI) at each of the two ends as well as a C-terminal Flag tag. Additionally, HAsp-pIL-18 has an engineered N-terminal signal peptide of 51 bp from HA of influenza virus A/WSN/33 (GenBank accession no. J02176.1), whereas pIL-15 retains its own signal peptide. Furthermore, the GPI modification signal from pCD59 (114 bp) and the HA transmembrane region (210 bp) were also commercially synthesized as pCD59-GPI or HATM. All the sequences for gBlock fragments and primers used in this study will be provided upon request.
To construct plasmids for expressing cytokines with the GPI signal, the cytokine gBlock fragment (IL-15 or IL-18) was digested with NheI and XhoI, and the GPI modification signal from pCD59 or the HATM region was amplified from gBlock with specific primers (primers pCD59_XhoI-F and pCD59_ NotI-R and primers HA_XhoI-F and HA_NotI-R, respectively) containing XhoI and NotI restriction sites and subsequently digested with the corresponding enzymes. These two flanking fragments were then included in a three-fragment ligation with NheI- and NotI-digested vector pIHA (26). The resulting constructs, pIL-15-CD59GPI, pIL-18-CD59GPI, pIL-15-HATM, and pIL-18-HATM, contained either a GPI modification signal or a HA transmembrane region at the C terminus. To construct plasmids for expressing cytokines without a GPI signal as controls, two primer sets with an engineered stop codon (primer set IL-15TAA-F and IL-15TAA-R and primer set HAsp-IL-18-TAA-F and HAsp-IL-18-TAA-R) were used to amplify the cytokine gBlock fragment and subsequently cloned into NheI- and NotI-digested
on November 6, 2019 by guest
http://jvi.asm.org/
vector pIHA. The resulting plasmids were designated pIL-15TAA and pIL-18TAA. Each of the cytokine coding regions was fused to a Flag tag prior to the membrane-targeting signal (or prior to the stop codon in pIL-15TAA and pIL-18TAA). The specificity of the rabbit antibody against porcine IL-18 or porcine IL-15 was confirmed by simultaneous staining of the Flag-tagged cytokines with a rat anti-Flag antibody (data not shown).
Determination of the full-length genomic sequence of the PRRSV Suvaxyn MLV and sequence analyses.The sequences of the ORF2 to ORF7 genes, but not ORF1, of the wild-type PRRSV ISU-55 isolate were reported previously (8, 11). To determine the complete genomic sequence of the PRRSV Suvaxyn MLV, total RNAs were isolated from the Suvaxyn MLV virus by using Tri reagent (MRC, Cambridge, UK). Reverse transcription and cDNA synthesis were performed at 42°C for 60 min in a 20-l reaction mixture containing 100 U of Superscript II reverse transcriptase (Invitrogen, Carlsbad, CA), 10 mM deoxyribo-nucleoside triphosphate, 100 mM dithiothreitol (DTT), 1 U of RNasin (Promega, Madison, WI), and 0.5g of oligo(dT) primers (Invitrogen, Carlsbad, CA). A total of 10 overlapping PCR fragments covering the entire genome of the Suvaxyn MLV were amplified and subsequently cloned into a pCR-2.1 vector (Invitrogen). Three individual clones of each fragment were sequenced. The consensus sequences were assembled and used for sequence analysis utilizing Lasergene software (version 10; DNAStar Inc., Madison, WI). The sequence of the extreme 5=end of the viral genome was determined by using the GeneRACER kit (Invitrogen, Carlsbad, CA) with two reverse primers, SV5RACE1 and SV5RACE2. The sequence of the extreme 3=end of the viral genome was determined by nested PCR using the same forward primer, SV10F, and two reverse primers, SV3RACE adaptorT and SV3RACE primer.
Construction of a DNA-launched infectious clone of the PRRSV Suvaxyn MLV.After determining the complete genomic sequences at the extreme 5=end and 3=end of the viral genome, a total of 5 overlapping fragments (AX, XP, PN, NE, and EX) with unique restriction enzyme sites were amplified from the viral cDNA of the PRRSV Suvaxyn MLV. Twenty poly(A) nucleotides were introduced immediately downstream of the 3=end of the viral genome. Nested PCR was used to introduce the ribozyme elements to the 5=and 3=ends of the viral genome for the construction of the DNA-launched infectious clone, as previously described (47). Two restriction sites, AscI and XbaI, were engineered upstream and down-stream of the viral genome for genome assembly. A total of 6 individual clones for each fragment were selected for sequencing, and the clone containing the consensus sequence was used for the assembly of the full-length clone. Fragment ACYC-XA from plasmid pACYC-177 was amplified by using primers pACYC-Xbalf (5=-AAACCCGATATCAAACCCTCTAGAGCCCTTCGCCCTTCCGGCTGGCT-3=) and pACYC-AscIr (5=-GGTTTCATATGGGGTTTGTTTAAACGGGTTTGGCGCGCCGGATCCTCCGGCGTT-3=), incorporating the unique restriction sites AscI, XhoI, PmeI, NdeI, EcoRV, and XbaI, which were then used to ligate the fragment upstream of the viral genome. Among the five fragments, each of the PN, NE, and EX fragments was used to sequentially replace the fragments with the same restriction enzyme sites on the modified expression vector pIRES-EGFP2. A three-fragment ligation was used to assemble fragments AX and XP into the vector using the restriction sites AscI and PmeI, resulting in the assembly of a full-length genome of the PRRSV Suvaxyn MLV, which was then used to replace the PRRSV VR2385 genome in the pIR-VR2385-CA DNA-launched infectious clone (47) with the restriction sites AscI and XbaI. The final full-length DNA-launched infectious clone of the PRRSV Suvaxyn MLV was designated pIR-SUV.
Construction of cytokine gene-incorporated recombinant PRRSV MLV infectious clones. In order to generate the PRRSV MLV expression cassette, an upstream fragment of 3,906 bp was amplified from the original pIR-SUV infectious clone backbone with forward primer Suv-NS_F1 containing the NotI restriction site and reverse primer Suv-NS_R1 containing the SbfI and PacI restriction enzyme sites. Nested PCR was used to amplify the downstream fragment of 576 bp with two forward primers (Suv-NS F2-1 and Suv-NS F2-2) containing the PacI restriction enzyme site and a synthetic TRS of 40 nucleotides (nt) (IDT, Coralville, IA) and a reverse primer (Suv-NS_R2) containing the ScaI site. These two flanking fragments were then included in a three-fragment ligation with the NotI- and ScaI-digested pIR-SUV infectious clone to generate a new PRRSV MLV infectious clone, designated pIR-SUV-2RE, which contains two unique enzyme sites, SbfI and PacI, and a synthetic TRS that allows for foreign gene insertion and expression.
To insert pIL-15 and pIL-18 together with the GPI signal in pIR-SUV-2RE, a primer set comprising IL-18_SbfI-F1, IL-18-R1, IL-18-F2, and CD59_PacI-R and a primer set comprising IL-15_SbfI-F1, IL-15-R1, IL-15-F2, and CD59_PacI-R were used for overlapping PCR to amplify the cytokine fused with GPI from expression plasmids pIL-15-GPI and pIL-18-GPI. The amplified regions and pIR-SUV-2RE were separately digested with SbfI and PacI and subsequently ligated together to generate recombinant PRRSV MLV SUV-IL-15 and SUV-IL-18 infectious clones. The control recombinant MLVs SUV-GFP, SUV-IL-15TAA, and SUV-IL-18TAA were generated similarly with primer sets GFP-F and GFP-R, IL-15_SbfI-F1 and IL15_PacI-R, and IL18mtr_SbfI-F and IL18_PacI-R.
Rescue of recombinant PRRSV MLVs and indirect immunofluorescence assay.BHK-21 cells were transfected with the respective DNA-launched PRRSV recombinant MLV infectious clone plasmid DNAs. The supernatant of transfected cells at 26 h posttransfection (hpt) was used to infect MARC-145 cells, as described previously (26). Transfected or infected cells were examined by an indirect immunofluores-cence assay (IFA) using PRRSV anti-N monoclonal antibody (MAb) SDOW17, as described previously (48). To further verify the stability and authenticity of the introduced mutations, viral RNA from the fourth and fifth passages of the recombinant PRRSV MLVs in MARC-145 cells was extracted from the supernatants by using the ZR viral RNA kit (Zymo Research) and subjected to RT-PCR amplification (Superscript III one-step RT-PCR system) and DNA sequencing analyses of the inserted genes between ORF1b and ORF2a.
Antibodies. The following antibodies against porcine antigens were used for multiparameter fluorescence-activated cell sorter (FACS) analysis. Anti-CD8␣IgG2a (clone 76-2-11), anti-CD8␣IgG1 (clone
on November 6, 2019 by guest
http://jvi.asm.org/
PT36A), anti-CD4 IgG2b (clone 74-12-4), anti-CD3 IgG2b (clone 8E6-2b3c), and anti-␥␦T cell IgG1 (clone PGBL31A) were purchased from Washington State University (Pullman, WA). Phycoerythrin (PE)-conjugated anti-human/porcine CD107a and mouse anti-porcine CD3-biotin (clone PPT3) were pur-chased from Southern Biotech (Birmingham, AL). Other primary antibodies included mouse anti-pig CD16 IgG1 (clone G7; Bio-Rad, Hercules, CA) and peridinin chlorophyll protein (PerCP)-Cy5.5 mouse anti-pig IFN-␥(clone P2G10; BD eBioscience, San Jose, CA). The secondary antibodies used for FACS analysis, fluorescein isothiocyanate (FITC)-conjugated anti-mouse IgG2b, PE-Cy7 anti-mouse IgG1, allophycocyanin-conjugated streptavidin, and allophycocyanin-conjugated anti-mouse IgG2a, were pur-chased from BioLegend (San Diego, CA). Rabbit polyclonal antibodies against porcine IL-15 or pIL-18 were purchased from MyBioSource (San Diego, CA). The SDOW17 antibody against the PRRSV N protein used for IFAs was purchased from Research Technology Innovation Inc. (Brookings, SD).
Flow cytometry.Cells were dispensed into 96-well U-bottom plates (BD Falcon, Bedford, MA) and stimulated with PRRSV strain NADC20 at a MOI of 1 in a final volume of 150l. As described previously (26, 49), GolgiPlug and GolgiStop (Thermo Scientific, Waltham, MA) were added at a final dilution of 1:1,000 at 12 hpi. PE-CD107a was also added at 5l per well and incubated for four additional hours, according to the manufacturer’s instructions. Cells were washed and suspended in FACS buffer (phosphate-buffered saline [PBS] containing 2% FBS at 4°C). They were divided into different panels and incubated with anti-porcine CD3, CD4, and CD8 antibodies of different isotypes as panel 1 or separately with anti-porcine CD3 and anti-␥␦ antibodies as panel 2. This was followed by incubation with isotype-matched PE-Cy7-, FITC-, and allophycocyanin-conjugated secondary antibodies. As panel 3, NK cells were incubated with anti-porcine CD3, CD8, and CD16 antibodies of different isotypes, followed by isotype-matched PE-Cy7-, FITC-, and APC-conjugated secondary antibodies. After staining of these surface markers, cells were fixed with 3.2% paraformaldehyde for 10 min at room temperature, followed by permeabilization in 0.2% saponin for 10 min at room temperature. Cells were incubated with PerCP-Cy5.5 mouse anti-porcine IFN-␥for 15 min and subsequently washed with FACS buffer with 0.2% saponin. The fluorescence of each panel was assessed with a BD FACSAria II instrument.
Vaccination and challenge study in pigs.The animal study was approved by the Virginia Tech Institutional Animal Care and Use Committee (IACUC) (approval no. 16229). A total of 40 pigs were divided into 5 groups of 8 pigs each and vaccinated with recombinant PRRSV MLVs or the cell culture medium DMEM (Table 1). At 49 dpv, all the pigs were challenged with either a heterologous PRRSV strain, NADC20, or cell culture medium as a control. PRRSV NADC20 was inoculated into pigs via the intramus-cular route, as this has been widely used in studies reported previously (47, 48, 50). At 14 dpc, all pigs were necropsied. At necropsy, the gross lung pathological lesions were recorded in a blind fashion by a board-certified veterinary pathologist (T.L.). Samples of lung tissues were also collected during necropsy for histological examination in a blind fashion by a board-certified veterinary pathologist (T.L.) and quantification of viral RNA loads. Weekly serum samples and PBMCs were also collected from each pig for a total of 9 weeks.
Quantitation of viral RNA loads in sera and lung tissues.Viral RNAs were extracted from serum samples at 7 and 14 dpc by using the ZR viral RNA kit (Zymo Research, Irvine, CA), and the total RNAs from the lung tissues were extracted by using Tri reagent (MRC, Cambridge, UK), both according to the manufacturers’ protocols. The quantification of PRRSV RNA copy numbers in sera and in lung tissues was performed by qRT-PCR using a SYBR green one-step qRT-PCR kit (Bioline), as described previously (48, 50). The RNA standard used for qRT-PCR was derived from thein vitrotranscription of a PRRSV full-length cDNA clone, pACYC-VR2385, by using the mMessage mMachine T7 kit (Ambion). Each qRT-PCR was performed in triplicate.
Gross pathological and histological evaluations of lung lesions.All pigs were humanely eutha-nized by an intravenous overdose of pentobarbital (Fatal-Plus; Vortech Pharmaceutical Ltd., Dearborn, MI). At necropsy, the lungs were scored for gross pathology in a blind manner, as described previously (12). Five sections of lung tissues were collected from each pig, fixed in 10% neutral buffered formalin, and processed for routine histopathological evaluation. The criteria for evaluating gross pathology and histopathology have been well established and were described previously (12).
Statistical analyses. One-way analysis of variance (ANOVA) was used to evaluate the data for statistical differences. The data were analyzed by using GraphPad Prism (version 6.0).
ACKNOWLEDGMENTS
This study was supported by Virginia Tech Internal Funds. Qian M. Cao is a recipient
of the Stamp Scholar fellowship.
We thank Melissa Makris for her expert assistance in flow cytometry analyses and
Karen Hall, Mariah Weiss, and Virginia Tech TRACSS staff for their assistance in animal
care.
REFERENCES
1. Lunney JK, Benfield DA, Rowland RR. 2010. Porcine reproductive and respiratory syndrome virus: an update on an emerging and re-emerging viral disease of swine. Virus Res 154:1– 6.https://doi.org/ 10.1016/j.virusres.2010.10.009.
2. Holtkamp DJ, Kliebenstein JB, Neumann EJ, Zimmerman JJ, Rotto HF,
Yoder TK, Wang C, Yeske PE, Mowrer CL, Haley CA. 2013. Assessment of the economic impact of porcine reproductive and respiratory syndrome virus on United States pork producers. J Swine Health Prod 21:72– 84.
3. Snijder EJ, Kikkert M, Fang Y. 2013. Arterivirus molecular biology and
on November 6, 2019 by guest
http://jvi.asm.org/
pathogenesis. J Gen Virol 94:2141–2163. https://doi.org/10.1099/vir.0 .056341-0.
4. Meng XJ, Paul PS, Halbur PG. 1994. Molecular cloning and nucleotide sequencing of the 3=-terminal genomic RNA of the porcine reproduc-tive and respiratory syndrome virus. J Gen Virol 75(Part 7):1795–1801.
https://doi.org/10.1099/0022-1317-75-7-1795.
5. Johnson CR, Griggs TF, Gnanandarajah J, Murtaugh MP. 2011. Novel structural protein in porcine reproductive and respiratory syndrome virus encoded by an alternative ORF5 present in all arteriviruses. J Gen Virol 92:1107–1116.https://doi.org/10.1099/vir.0.030213-0.
6. Pasternak AO, Spaan WJ, Snijder EJ. 2006. Nidovirus transcription: how to make sense? J Gen Virol 87:1403–1421. https://doi.org/10.1099/vir.0 .81611-0.
7. Meng XJ, Paul PS, Morozov I, Halbur PG. 1996. A nested set of six or seven subgenomic mRNAs is formed in cells infected with different isolates of porcine reproductive and respiratory syndrome virus. J Gen Virol 77(Part 6):1265–1270. https://doi.org/10.1099/0022-1317 -77-6-1265.
8. Meng XJ, Paul PS, Halbur PG, Lum MA. 1995. Phylogenetic analyses of the putative M (ORF 6) and N (ORF 7) genes of porcine reproductive and respiratory syndrome virus (PRRSV): implication for the existence of two genotypes of PRRSV in the USA and Europe. Arch Virol 140:745–755.
https://doi.org/10.1007/BF01309962.
9. Martin-Valls GE, Kvisgaard LK, Tello M, Darwich L, Cortey M, Burgara-Estrella AJ, Hernandez J, Larsen LE, Mateu E. 2014. Analysis of ORF5 and full-length genome sequences of porcine reproductive and respiratory syndrome virus isolates of genotypes 1 and 2 retrieved worldwide provides evidence that recombination is a common phenomenon and may produce mosaic isolates. J Virol 88:3170 –3181.https://doi.org/10 .1128/JVI.02858-13.
10. Shi M, Lam TT, Hon CC, Murtaugh MP, Davies PR, Hui RK, Li J, Wong LT, Yip CW, Jiang JW, Leung FC. 2010. Phylogeny-based evolutionary, de-mographical, and geographical dissection of North American type 2 porcine reproductive and respiratory syndrome viruses. J Virol 84: 8700 – 8711.https://doi.org/10.1128/JVI.02551-09.
11. Meng XJ, Paul PS, Halbur PG, Morozov I. 1995. Sequence comparison of open reading frames 2 to 5 of low and high virulence United States isolates of porcine reproductive and respiratory syndrome virus. J Gen Virol 76(Part 12):3181–3188. https://doi.org/10.1099/0022-1317-76-12 -3181.
12. Halbur PG, Paul PS, Frey ML, Landgraf J, Eernisse K, Meng XJ, Lum MA, Andrews JJ, Rathje JA. 1995. Comparison of the pathogenicity of two US porcine reproductive and respiratory syndrome virus isolates with that of the Lelystad virus. Vet Pathol 32:648 – 660.https://doi.org/10.1177/ 030098589503200606.
13. Huang YW, Meng XJ. 2010. Novel strategies and approaches to develop the next generation of vaccines against porcine reproductive and respi-ratory syndrome virus (PRRSV). Virus Res 154:141–149.https://doi.org/ 10.1016/j.virusres.2010.07.020.
14. Renukaradhya GJ, Meng XJ, Calvert JG, Roof M, Lager KM. 2015. Live porcine reproductive and respiratory syndrome virus vaccines: current status and future direction. Vaccine 33:4069 – 4080.https://doi.org/10 .1016/j.vaccine.2015.06.092.
15. Renukaradhya GJ, Meng XJ, Calvert JG, Roof M, Lager KM. 2015. Inacti-vated and subunit vaccines against porcine reproductive and respiratory syndrome: current status and future direction. Vaccine 33:3065–3072.
https://doi.org/10.1016/j.vaccine.2015.04.102.
16. Han K, Seo HW, Park C, Chae C. 2014. Vaccination of sows against type 2 porcine reproductive and respiratory syndrome virus (PRRSV) before artificial insemination protects against type 2 PRRSV challenge but does not protect against type 1 PRRSV challenge in late gestation. Vet Res 45:12.https://doi.org/10.1186/1297-9716-45-12.
17. Mbow ML, De Gregorio E, Valiante NM, Rappuoli R. 2010. New adjuvants for human vaccines. Curr Opin Immunol 22:411– 416.https://doi.org/10 .1016/j.coi.2010.04.004.
18. Pulendran B, Dillon S, Joseph C, Curiel T, Banchereau J, Mohamadzadeh M. 2004. Dendritic cells generated in the presence of GM-CSF plus IL-15 prime potent CD8⫹Tc1 responses in vivo. Eur J Immunol 34:66 –73.
https://doi.org/10.1002/eji.200324567.
19. Matikainen S, Paananen A, Miettinen M, Kurimoto M, Timonen T, Julkunen I, Sareneva T. 2001. IFN-alpha and IL-18 synergistically enhance IFN-gamma production in human NK cells: differential reg-ulation of Stat4 activation and gamma gene expression by
IFN-alpha and IL-12. Eur J Immunol 31:2236 –2245. https://doi.org/10 .1002/1521-4141(200107)31:7⬍2236::AID-IMMU2236⬎3.0.CO;2-G. 20. Domeika K, Berg M, Eloranta ML, Alm GV. 2002. Porcine interleukin-12
fusion protein and interleukin-18 in combination induce interferon-gamma production in porcine natural killer and T cells. Vet Immunol Immunopathol 86:11–21.https://doi.org/10.1016/S0165-2427(01)00431-7.
21. Heider S, Dangerfield JA, Metzner C. 2016. Biomedical applications of glycosylphosphatidylinositol-anchored proteins. J Lipid Res 57: 1778 –1788.https://doi.org/10.1194/jlr.R070201.
22. Khan T, Heffron CL, High KP, Roberts PC. 2014. Tailored vaccines target-ing the elderly ustarget-ing whole inactivated influenza vaccines beartarget-ing cy-tokine immunomodulators. J Interferon Cycy-tokine Res 34:129 –139.
https://doi.org/10.1089/jir.2012.0119.
23. Yang Y, Leggat D, Herbert A, Roberts PC, Sundick RS. 2009. A novel method to incorporate bioactive cytokines as adjuvants on the surface of virus particles. J Interferon Cytokine Res 29:9 –22.https://doi.org/10 .1089/jir.2008.0017.
24. Herbert AS, Heffron L, Sundick R, Roberts PC. 2009. Incorporation of membrane-bound, mammalian-derived immunomodulatory proteins into influenza whole virus vaccines boosts immunogenicity and protec-tion against lethal challenge. Virol J 6:42.https://doi.org/10.1186/1743 -422X-6-42.
25. Ni YY, Huang YW, Cao D, Opriessnig T, Meng XJ. 2011. Establishment of a DNA-launched infectious clone for a highly pneumovirulent strain of type 2 porcine reproductive and respiratory syndrome virus: identifica-tion and in vitro and in vivo characterizaidentifica-tion of a large spontaneous deletion in the nsp2 region. Virus Res 160:264 –273.https://doi.org/10 .1016/j.virusres.2011.06.027.
26. Cao QM, Subramaniam S, Ni YY, Cao D, Meng XJ. 2016. The non-structural protein Nsp2TF of porcine reproductive and respiratory syn-drome virus down-regulates the expression of swine leukocyte antigen class I. Virology 491:115–124.https://doi.org/10.1016/j.virol.2016.01.021. 27. Gerner W, Kaser T, Saalmuller A. 2009. Porcine T lymphocytes and NK cells—an update. Dev Comp Immunol 33:310 –320.https://doi.org/10 .1016/j.dci.2008.06.003.
28. Yoo D, Song C, Sun Y, Du Y, Kim O, Liu HC. 2010. Modulation of host cell responses and evasion strategies for porcine reproductive and respira-tory syndrome virus. Virus Res 154:48 – 60. https://doi.org/10.1016/j .virusres.2010.07.019.
29. Wang R, Nan Y, Yu Y, Zhang YJ. 2013. Porcine reproductive and respi-ratory syndrome virus Nsp1beta inhibits interferon-activated JAK/STAT signal transduction by inducing karyopherin-alpha1 degradation. J Virol 87:5219 –5228.https://doi.org/10.