Dissertation
Submitted to
THE TAMILNADU Dr. M.G.R MEDICAL
UNIVERSITY
In partial fulfilment of the requirements for
the award of the degree of
M.D PHARMACOLOGY
Branch VI
May 2018
DRUG PRESCRIBING PATTERN WITH COST ANALYSIS
AND MONITORING OF ADVERSE DRUG REACTIONS IN
Dissertation
Submitted to
THE TAMILNADU Dr. M.G.R MEDICAL
UNIVERSITY
In partial fulfilment of the requirements for
the award of the degree of
M.D PHARMACOLOGY
Branch VI
May 2018
DRUG PRESCRIBING PATTERN WITH
COST ANALYSIS AND MONITORING OF ADVERSE DRUG
REACTIONS IN DEPARTMENT OF DERMATOLOGY: A
Acknowledgement
In the first place, I would like to express my gratitude to my professor, mentor and guide Dr. Reneega Gangadhar, for her valuable and constant guidance, supervision and support throughout the study. Her patience and understanding during times of
difficulties in the study period helped me a lot under such circumstances. Her constant
motivation has helped me to overcome all the challenges and difficulties that I came
across this research work. Her encouragement from the inception of this research to
its culmination has always been profound. It has been an extraordinary experience
working under her.
I am very much grateful and thankful to my Co-Guide Dr. Padma Prasad .M.K,
Associate Professor, Department of Dermatology for his immense help with his ideas,
valuable contributions, patience and generous encouragement during the research
work and preparation of the manuscript. Dr. Ganesh .V, Associate Professor, Department of Pharmacology for his support and guidance all throughout the study.
I extend my thanks to my Assistant professors Dr. Sarath Babu .K for his valuable suggestion, support and encouragement during the preparation of the manuscript and
Dr. V. M. Sandeep for his valuable inputs during all the stages of my study.
I extend my sincere heartfelt thanks to Dr. Velayuthan Nair, Chairman and
Dr. Rema V. Nair, Director, for permitting me to carry out the study in the hospital and providing facilities to accomplish my dissertation work. Then I would also like to
thank the Principal of the Institution Dr. Padmakumar for his valuable support extended to me.
I express my special thanks to my colleague Dr. Sushmita Ann. S. J, for giving me uncountable constructive ideas and encouragement to do the study. I also thank
my senior Post Graduates Dr. Prathab Asir. A, Dr. Anandhalakshmi. A and Dr. Arjun. G. Nair and my junior Post Graduates Dr.Priyanka. R , Dr. Ramakrishnan Nair and Dr. Charmilla. V for their help and support.
Abbreviations
AB Antibody
ADP Adenosine Diphosphate
ADR Adverse drug reaction
AG Antigen
AGA Androgenetic Alopecia
CDSCO Central Drug Standard Control Organization
CYP3A4 CytochromeP450 3A4
DNA Deoxyribonucleic acid
DUS Drug utilization study
EDL Essential Drug List
FDE Fixed Drug Eruptions
hdIVIg High-dose intravenous immunoglobulin
IFN-α Interferon α
IgG Immunoglobulin G
IHEC Institutional Human Ethics Committee
IL-10 Interleukin -10
IL-12 Interleukin -12
INR Indian rupee
NSAIDs NonsteroidalAntiinflammatory Drugs
OPD Outpatient Department
PUVA Psoralen and ultraviolet A
TNF-α Tumour Necrosis Factor α
UMC Uppsala Monitoring Centre
UV Ultraviolet radiation
Contents
Table of Contents
Sl. No Page No
1. Introduction 1
2. Review of literature 6
3. Aims and objectives 53
4. Materials and Methods 54
5. Observation & Results 59
6. Discussion 73
7. Conclusion 77
8. References I- XI
9. Annexure
I IHEC certificate XII
II Consent form XIII
III Case Record form XIV
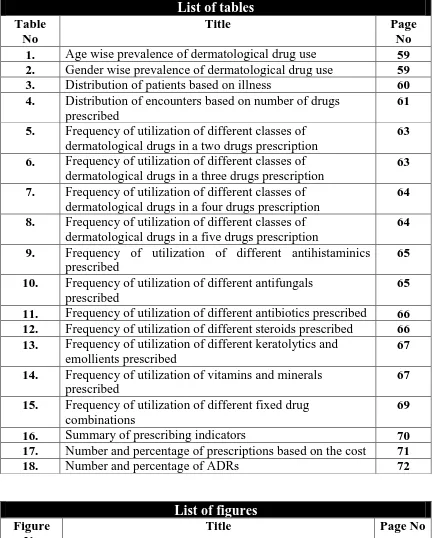
List of tables
Table No
Title Page
No 1. Age wise prevalence of dermatological drug use 59 2. Gender wise prevalence of dermatological drug use 59 3. Distribution of patients based on illness 60 4. Distribution of encounters based on number of drugs
prescribed
61 5. Frequency of utilization of different classes of
dermatological drugs in a two drugs prescription
63 6. Frequency of utilization of different classes of
dermatological drugs in a three drugs prescription
63 7. Frequency of utilization of different classes of
dermatological drugs in a four drugs prescription
64 8. Frequency of utilization of different classes of
dermatological drugs in a five drugs prescription
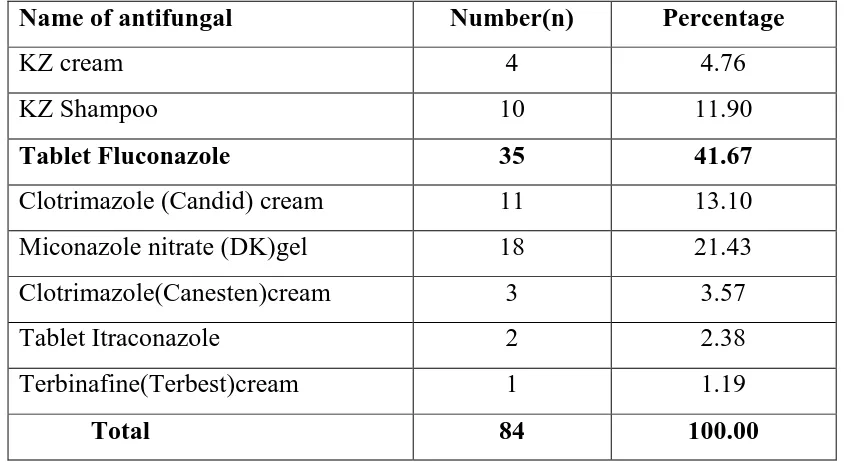
64 9. Frequency of utilization of different antihistaminics
prescribed
65 10. Frequency of utilization of different antifungals
prescribed
65 11. Frequency of utilization of different antibiotics prescribed 66 12. Frequency of utilization of different steroids prescribed 66 13. Frequency of utilization of different keratolytics and
emollients prescribed
67 14. Frequency of utilization of vitamins and minerals
prescribed
67 15. Frequency of utilization of different fixed drug
combinations
69 16. Summary of prescribing indicators 70 17. Number and percentage of prescriptions based on the cost 71 18. Number and percentage of ADRs 72
List of figures
Figure No
Title Page No
1. Distribution of encounters based on number of drugs prescribed
61 2. Distribution of various classes of dermatological drugs
prescribed
62 3. Percentage of drugs prescribed from WHO essential drug
list
68 4. Causality assessment of ADRs of dermatological drugs
by WHO-UMC causality assessment scale
[image:9.595.102.537.73.611.2]Introduction
1 | P a g e
INTRODUCTION
Skin constitutes as the largest organ of human body and thus it is exposed to injury by various extrinsic factors such as environmental, chemical, infectious agents as well as intrinsic factors such as metabolic, genetic and immunological. Metaphorically skin acts as a mirror to various internal diseases , constituting that many systemic diseases are identified by their dermatological manifestations.1
In Developing countries skin diseases have a greater impact on the quality of life of people,it is more so in a country like India which has a wide variation of climate, religion, customs & socioeconomic status in different parts of the country.2In India patients in the second and third decades of age group (3.7% to 51.17% ) form the largest part of population suffering from various skin diseases.3The most prevalent dermatological conditions include scabies, pyoderma, dermatitis, urticaria, fungal skin infection, acne, alopecia and less common are eczematous disorder like psoriasis, skin cancer and cutaneous adverse drug reaction.4
Introduction
2 | P a g e steroids, salicylic acid, anti-histaminic,vitamins and minerals, analgesics usually depends upon prescriber’s choice . 5
A prescription is a written communication from a registered medical practitioner or other licensed practitioners to a pharmacist providing with salient instructions regarding the dispensing of prescribed medication. It designates a medication to be administered to a particular patient by combined skill and services of both the physician and the pharmacist Drug prescribing practice is a science and an art itself. It conveys the message from the prescribing physician to the patient. 6
Medication problem is tragic and costly for patients and professionals alike.7 Rational use of drug is defined by WHO as" patients receive medicines appropriate to their clinical needs in doses that meet their own individual requirements for an adequate period of time, at the lowest cost to them and their community".8A recent observation is that many doctors are frequently adopting polypharmacy which has lead to a steep rise in the cost of the treatment as well as adverse drug effects. 8
In many developing countries, an important portion of government and household expenditure is the drug cost and improper use of drugs results in major health hazard and increases treatment costs.9
Introduction
3 | P a g e utilization studies 10.In 1985 WHO convened a major conference in Nairobi on the rational use of drug and from that time onwards efforts have been made to improve the drug use pattern and prescription behaviour.11
According to a WHO report ,based on a "community based surveillance of anti-microbial use and resistance in the resource constrained settings" antibiotic use & antimicrobial resistance is increasing in India from 5 pilot projects , three from India (Delhi, Mumbai and Vellore) and two from South Africa .12Henceforth the pattern of drug use in hospital setting needs to be monitored systematically in order to analyse their rationality and to provide feedback to drug prescribers .This is essential to increase the therapeutic benefits and reduce the adverse effects. 13
Introduction
4 | P a g e had shown that of the total medical expenditure percapita,medicines alone accounted for 74% expenses in the rural and 67% in urban areas. 15
Adverse drug reaction(ADR) are unintended effects of drugs occurring during use of drugs. Majority of ADRs are minor reactions and are self limiting but sometimes they are severe and potentially life threatening .14Therefore ADR monitoring is mandatory.16
Therefore periodic auditing of prescriptions and pharmacovigilance is essential inorderto increase the therapeutic efficacy, decrease adverse effects and provide feedback to prescribers. Setting up Hospital formulary depending on geographic profile of disease and availability of drugs is also the need of the hour.4 At present there is an increasing trend for irrational prescribing of dermatology drugs .Inappropriate drug has a direct impact as well as indirect impact on the cost to health system and individuals.Therefore periodic evaluation of drug utilization patterns are essential inorder to enable suitable modification in prescription of drugs to increase therapeutic benefits and decrease adverse effects as well as to minimize the expenditure cost of drugs being used.8
Till now very few systematically analyzed data are available on the drug utilization pattern, and adverse drug reaction profile in dermatology Outpatient department (OPD) in India.4
Introduction
Review of Literature
6 | P a g e
Review of literature
:Dermatology is the study of skin and its associated structures including hair, nail and of their diseases. Skin is considered as the boundary between ourselves and the world around us.16 It is one of the many specialties that has evolved from general internal medicine.17
Skin as an organ has certain roles:
1.It acts as a barrier, preventing the entry of noxious chemicals and infectious organisms, and also preventing the exit of water and other chemicals.
2.It reflects internal changes and reacts to external changes also.
3.It can sweat, grow hair, erect its hairs, change colour, smell, grow nails, and secrete sebum.
4.When confronted with insults from outside, it usually adapts easily and returns to a normal state.
Review of Literature
7 | P a g e
History
Contributions of Heberden, Cullen, and Hebra, laid the foundations on which the pioneer specialist dermatologists of the following century were able to build .20 In India, therapeutics of dermatoses were known and practised by our ancient physicians for centuries, Charaka Samhita contains one chapter on the subject.21 Another Indian literature Atreya Punarvasu has described eighteen dermatoses.22Later on Ayurvedic dermatology was influenced by the Unani system. During the British era , Dr. Vandyke Carter, Surgeon Major, HMS Indian Medical Services, was requisitioned to take stock of the various dermatological situation in India.This, perhaps, was the first scientific endeavor to study dermatoses in the Indian subcontinent, where hardly any statistics were available.23
Epidemiology:
Review of Literature
8 | P a g e
Classification of Dermatological condition18:
Dermatological conditions are categorised into : 1. Disorders of keratinization
2. Papulosquamous disorders 3. Eczema and dermatitis
4. Reactive erythemas and vasculitis 5. Bullous diseases
6. Connective tissue disorders
7. Disorders of blood vessels and lymphatics 8. Sebaceous and sweat gland disorders 9. Regional dermatology
10. Infections 11. Infestations
Review of Literature
9 | P a g e
Treatment
From diagnosis to assessing the effectiveness of therapy,dermatology is a visually oriented specialty.27
Non Pharmacological interventions 27:
Depression, anxiety and anger are commonly observed emotional reactions in individuals with skin disease. Negative emotional states such as stress, anxiety, depression, and anger can elicit or exacerbate skin disease.Worsening of skin disease, stress and negative emotional states increase the release of proinflammatory cytokines and produce negative effects on barrier function. These type of patients require :
1. Lifestyle modification- Healthy diet , using precautionary measures at work place ,using sunshades or umbrella
2. Cosmetic intervention
3. Cognitive behaviour Pshycotherapy
Pharmacological interventions28,29 :
1. Glucocorticoids 2. Retinoids
3. Vitamin Analogs 4. Photochemotherapy 5. Antihistamines
Review of Literature
10 | P a g e
7. Antimalarial agents
8. Cytotoxic and Immunosuppressive drugs 9. Anti-Inflammatory drugs
10. Biological agents 11. Sunscreens
12. Intravenous Immunoglobulin 13. Emollients
14. Coolants
15. Capsaicin &Podophyllin 16. Topical Anesthetics
17. Opioid receptor antagonist
18. Anxiolytics &Tricyclic antidepressants 19. Selective serotonin reuptake inhibitors 20. Antipsychotic agents
21. Keratolytic agents
22. Drugs for Androgenetic Alopecia 23. Drugs for Hyperpigmentation
Glucocorticoids 28,29
Review of Literature
11 | P a g e
conditions for which topical corticosteroids were being prescribed 30 and the most common adverse effect reported in a Study by Shakya Shrestha S et al was shedding of skin 7(35%).31
Mechanism of action28,29
Glucocorticoids impair immunological competence.They suppress all types of hypersensitization and allergic phenomena. Corticosteroids penetrate cells and binds to high affinity cytoplasmic receptor proteins which results in structural change in the steroid receptor complex that allows its migration into nucleus and binding to glucocorticoid response elements on the chromatin. This further results in transcription of specific m-RNA and regulates protein synthesis. Furthermore glucocorticoids cause greater suppression of cell mediated immunity in which T-cells are primarily involved.This is the basis of use in autoimmune disease. Glucocorticoids also cause attenuation of increased capillary permeability,local exudation,cellular infiltration,phagocytic activity and late responses like capillary permeability, local exudation, collagen deposition, fibroblastic activity and scar formation.The cardinal signs of inflammation such as redness,heat,swelling and pain are suppressed.
Pharmacokinetic:
Review of Literature
12 | P a g e
intracellular receptors and regulation of protein synthesis. The synthetic derivatives are more resistant to metabolism and are longer acting comparatively.
Adverse reaction:
a. Local adverse effects :
1. Thinning of epidermis - atrophy 2. Telangiectasia, Striae
3. Easy bruising 4. Hypopigmentation 5. Delayed wound healing
6. Fungal and bacterial infections
7. Chronic use may cause - skin atrophy , striae , telangiectasia , purpura and acniform eruptions
b. Systemic adverse effects :
1. Adrenal pituatory suppression can occur if large amounts are applied topically
2. Cushing's syndrome
Review of Literature
13 | P a g e
Therapeutic uses :
1. Eczematous skin disease
2. Pemphigus vulgaris , exfoliative dermatitis 3. Napkin rash
4. Steven Johnson syndrome 5. Lichen planus
6. Discoid Lupus erythematosus 7. Alopecia areata
Retinoids
Review of Literature
14 | P a g e
Mechanism of action:
Retinoids selectively activates retinoic acid receptors and retinoid-x receptors which controls genes of diffrentiation within the dermis . It causes inhibition of activator protein-1, a transcription factor composed of c-Jun and c-Fos that normally activates the synthesis of matrix metalloproteinases in response to UV radiation. It also increases the level of CD25,low affinity IL-2 receptors on malignant lymphocytes of T-cell origin.
Pharmacokinetic:
Trans retinoic acid is used topically, while 13-cis retinoic acid is given orally for acne. Retinoic acid is rapidly metabolized and excreted in bile and urine. It is used as 0.025%-0.05% gel or cream. Bexarotene is metabolized by CYP3A4.
Adverse reaction:
1. Erythema,desquamation,burning and stinging sensation 2. Photosensitivity reaction
3. Retinoid toxicities such asmucocutaneous side effects such as -chelitis, xerosis, blepharoconjunctivitis , cutaneous photosensitivity , photophobia , myalgia , arthralgia , headache , alopecia,nail fragility and increased susceptibility to staphylococcal infections
4. Retinoid dermatitis 5. Serum lipid elevation
Review of Literature
15 | P a g e
Therapeutic uses:
1. Non-inflammatory (comedonal) acne , acne vulgaris 2. Fine wrinkles and dyspigmentation
3. Photoaging 4. Psoriasis
5. Cutaneous lesions of Kaposi sarcoma 6. Early stage of cutaneous T-cell lymphoma
Contraindication:
Systemic retinoids and Topical retinoids are contraindicated in women who are pregnant, contemplating pregnancy or breast-feeding. Furthermore Systemic retinoids are relatively contraindicated in : Leukopenia , alcoholism, hyperlipidemia , hypercholestrolemia , hypothyroidism and significant hepatic or renal disease.
Vitamin Analog
Review of Literature
16 | P a g e
Mechanism of action:
- carotene has an anti-oxidant effect that decreases the production of free radicals or singlet oxygen. While calcipotriene exerts its effect through the vitamin D receptor, by binding with the vitamin D receptor ,the drug-receptor complex associates with the retinoid receptor- and binds to vitamin D response elements on DNA.
Pharmacokinetics:
Calcipotriene - on absorption through skin, gets inactivated rapidly andhence therapeutic response occurs only after 4-8 weeks. Topical calcipotriene has the ability to cross the placenta. It gets rapidly metabolized by the liver to inactive metabolites and excreted via bile. Only 20–30% of supplemental beta carotene is absorbed unchanged . Photosensitivity protecting action occurs after at least 2–4 weeks . It is principally metabolized in the small intestine and in the liver , to vitamin A . Excretion is by fecal route and urine in the form of metabolites.
Therapeutic use:
1. Psoriasis
2. Reduces photosensitivity in patients with erythropoietic protoporphyria
Adverse reaction:
Review of Literature
17 | P a g e
Photochemotherapy
In 2005, Man et al reported a twofold increased risk of basal cell carcinoma after 4 years of follow-up in a cohort of 1,908 patients treated with phototherapy, but no increased risk of squamous cell carcinoma or melanoma.34Phototherapy and Photochemotherapy are treatment methods in which UV or visible radiations is used to induce a therapeutic response either alone or in the presence of a photosensitizing drug.28 A study by Patrizi et al had stated that photochemotherapy is one of the frequently used treatment for dermatological diseases such as psoriasis, acne, and Atopic dermatitis, as well as for sleep disorders and some psychiatric illnesses.35
Psoralens and UVA28,29
Psoralens are lipophilic molecules which are derived from fusion of a furan with a coumarin.
Mechanism of action:
Review of Literature
18 | P a g e
Therapeutic uses:
1. Vitiligo
2. Cutaneous T-Cell lymphoma 3. Psoriasis
4. Atopic dermatitis 5. Alopecia aqreata 6. Lichen planus
7. Urticaria pigmentosa
Adverse reaction:
1. Phototoxic reactions 2. Pruritis
3. Hypertrichosis 4. GI disturbance 5. CNS disturbance 6. Bronchoconstriction 7. Hepatic toxicity
8. Herpes simplex recurrence 9. Retinal damage
10. Photoaging
11. Nonmelanoma skin cancer 12. Melanoma
Review of Literature
19 | P a g e
Method of drug administration:
Photosensitizing agents such as methoxsalen or trioxsalen or bergapten can be administered as oral, topical lotion or bath water
Photopheresis28
It is a process by which extracorporeal peripheral blood mononuclear cells are exposed to UVA radiation in the presence of methoxsalen.
Mechanism of action:
Mechanism of extracorporeal photopheresis include apoptosis of T cells, generation of clone-specific suppressor T cells, Shifting of T cells phenotype, production of an immune response against the pathogenic T cells and release cytokines.
Adverse reaction:
1. Phototoxic reactions
2. Temporary dyspigmentation 3. Potential scarring
Therapeutic use:
Actinic keratosis
Method of drug adminstration:
Review of Literature
20 | P a g e
Photodynamic therapy28
This therapy uses photosensitizing drugs and visible light for dermatological disorders. Two drugs are approved for topical photodynamic therapy ,it includes - aminolevulinic acid and methyl aminolevulinate.
Mechanism of action:
Aminolevulinic acid and methyl aminolevulinate are prodrugs which get converted to protoporphyrin IX within living cells.In the presence of UVA2 of wavelength of 320-340 nm and oxygen, protoporphyrin produces singlet oxygen which will oxidize cell membranes,proteins and mitochondrial structure leading to apoptosis.
Therapeutic use:
1. Precancerous actinic keratoses 2. Thin , non-melanoma skin cancer 3. Acne
4. Photorejuvenation
Adverse reaction:
1. Phototoxic reaction 2. GI disturbance 3. Hypotension
4. Congestive heart failure
Review of Literature
21 | P a g e
Antihistamines
Histamines are potent vasodilators and a stimulant of nociceptive itch receptors.Oral antihistamines, H1 receptor antagonists have anticholinergic activity and sedative property which aid in treatment of pruritus. First-generation antihistamine includes hydroxyzine, diphenhydramine, promethazine, cyproheptadine and doxepin. Second generation antihistamine includes cetrizine, levocetirizine, loratadine, desloratadine and fexofenadine.28,29 In a study on antihistamines , Kolasani BP et al had reported that the top three disorders, for which antihistamines were prescribed, were psoriasis followed by eczema and allergic contact dermatitis. They also noted that hydroxyzine had higher sedation, whereas levocetirizine had the least sedation, pheniramine had the highest anticholinergic side effects, and cetirizine/levocetirizine had a minimal or no anticholinergic side effects comparatively.36
Mechanism of action:
Histamine gets released from mast cells following AG:AB reaction on their surface in immediate type of hypersensitivity reactions.H1 antagonists effectively controls this manifestation by inhibiting the histamine release.
Pharmacokinetics:
Review of Literature
22 | P a g e
for a longer period ,which can result due to induction of microsomal P-450 enzymes.Patients with hepatic impairment can result in elimination of antihistamine slowly.
Therapeutic uses:
1. Hypersensitive type I reactions 2. Urticaria
3. Itching and Angioedema
Adverse reactions:
1. Sedation, diminished alertness and concentration 2. Light headedness
3. Motor incoordination 4. Fatigue
5. Dryness of mouth
6. Altered bowel movements 7. Urinary hesitancy
8. Blurring of vision
Review of Literature
23 | P a g e
Antimicrobial Agents
Antibiotics :
Commonest dermatological disorder treated with either topical or systemic antibiotics is acne vulgaris. Commonly used topical antimicrobials in acne include clindamycin, erythromycin, mupirocin, benzoyl peroxide, sulfacetamide/sulfur combinations, metronidazole and azelaic acid. Other agents include tetracycline, doxycycline, minocycline and trimethoprim-sulfamethoxazole. Tetracyclines are the most commonly employed antibiotics for dermatological manifestations.28,29 According to a study by Shamna AM et al beta-lactam drugs (penicillin, cephalosporin) and macrolides were the most frequently prescribed antimicrobial agents for skin and soft tissue infections Moreover the antibiotic class of drugs which were mostly accounted included cephalosporins (34.69%) followed by fluoroquinolones and others in which type A reactions were more compared to type B and 59.18% of them were predictable.37
Mechanism of action:
Antibiotics have four different mechanism:
Review of Literature
24 | P a g e
Therapeutic uses:
1. Pyoderma due to gram positive organisms like staphylococcus aureus and streptococcus pyogenes
2. Impetigo due to Staphylococcus aureus and Streptococcus pyogenes 3. Superficial infections caused by wounds and injuries
4. Deeper bacterial infections like folliculitis, erysipelas, cellulitis and necrotizing fasciitis
Adverse reactions :
1. Dizziness
2. Hyperpigmentation of skin and mucosa 3. serum-sickness like reaction
4. drug-induced lupus erythematosus
5. Allergic contact dermatitis especially on disrupted skin
Antifungals
A Meta-analysis by Chia-Hsuin Chang et al had reported that with the the risk of liver injury requiring termination of treatment with antifungals ranged from 0.11% (continuous itraconazole 100 mg/day) to 1.22% (continuous fluconazole 50 mg/day) and the risk of having asymptomatic elevation of serum transaminase but not requiring treatment discontinuation was less than 2.0% .38 Antifungals belonging to azole group and amphotericin-B can be used systemically as well as topically. Other antifungals
Review of Literature
25 | P a g e
azoles-miconazole and econazole , allylamines- naftifine and terbinafine , griseofulvin, triazoles.28,39Another study by Mandeep Kaur et al had reported that by comprising all factors , ketoconazole and fluconazole were the most effective drugs that were used and terbinafine was the less commonly used drug for treatment of dermatological conditions.40
Mechanism of action 28,39
Azole group of antifungals binds to cytochrome P-450 dependent 14- demethylase enzyme which results in hinderance of ergosterol synthesis . Furthermore inhibition of fungal respiration under aerobic condition occurs. Griseofulvin causes disruption of mitotic spindle and arrests the fungal mitosis at metaphase . It also has the property to bind to newly synthesised keratin making it resistant to fungal invasion. Terbinafine on the other hand inhibits fungal enzyme squalene epoxidase which converts squalene to lanosterol which can affect the fungal cell membrane integrity and function. Terbinafine also inhibits squalene epoxidase and decreases ergosterol biosynthesis.
Therapeutic uses :
1. Localized tinea corporis and uncomplicated tinea pedis 2. Localized cutaneous candidiasis and tinea versicolor 3. Tinea capitis
4. Onychomycosis
Review of Literature
26 | P a g e
Adverse reaction:
1. Headache,nausea,vomiting,photosensitivity and peripheral neuritis 2. Hepatotoxicity
3. Griseofulvin can cause disulfiram-like reaction with ethanol 4. Epigastric distress
5. Itraconazole on high dose can cause hypokalemia,hypertension and oedema
Antiviral Agents
Common dermatological viral infections include Human papillomavirus, Herpes simplex virus, Condyloma accuminatum,Molluscum contagiosum and varicella zoster virus.28,39A study done by Forbes J H et al, had reported that the most commonly prescribed antiviral was aciclovir (69.0%), followed by famciclovir (27.8%) and valaciclovir (3.5%) .41An Observational study by Jayanthi CR et al had reported that among the distribution of various ADRs across therapeutic classes Antivirals accounts for 6.7%.42Antiviral drugs given for dermatological manifestation include acyclovir, penciclovir, valacyclovir, famciclovir, docosnal trifluoridine and cedofovir.28,39
Mechanism of action:
Review of Literature
27 | P a g e
Therapeutic use:
1. Herpes simplex virus 2. Varicella zoster 3. Mucocutaneous HSV 4. Condylomata
5. Herpes labialis
Adverse reactions:
1. Phlebitis
2. Rash and mild hypotension 3. Renal toxicity
Antimalarial agents
In a retrospective study done by Gina C A et al had reported that a significant subgroup of patients whose skin lesions had been unresponsive to a single antimalarial benefitted from combination therapy with hydroxychloroquine and quinacrine or chloroquine and quinacrine.43Antimalarials commonly used in dermatology include Chloroquine, Hydroxychloroquine and Quinacrine.28,39
Mechanism of action:
Stabilization of lysosomes
Inhibition of antigen presentation
Review of Literature
28 | P a g e Inhibition of pro-inflammatory cytokine synthesis
Photoprotection
Inhibition of immune complex formation
Anti-thrombotic
Therapeutic uses:
1. Cutaneous lupus erythematosus 2. Cutaneous dermatomyositis 3. Polymorphous light eruption 4. Porphyria cutaneous tarda 5. Sarcoidosis
Adverse reactions:
1. Nausea 2. Vomiting 3. Dizziness 4. Headache 5. Urticaria 6. Blurred vision
7. Hypotension and T-wave abnormalities in ECG 8. GIT distress
Review of Literature
29 | P a g e
Cytotoxic and Immunosuppressive drugs
In a study by Callen JP , Cytotoxic and Immunosuppresive drugs such as methotrexate, azathioprine, cyclophosphamide, chlorambucil, cyclosporine, and other related drugs were reported to have potential benefits in the treatment of severe recalcitrant cutaneous disease.44
Cytotoxic and Immunosuppressive drugs include antimetabolites such as methotrexate, azathioprine and fluorouracil , alkylating agents such as cyclophosphamide and calcineurin inhibitors such as cyclosporine, tacrolimus and pimecrolimus.29
Mechanism of action:
Methotrexate acts by supressing immunocompetent cells in the skin and also decreases the expression of cutaneous lymphocyte associated antigen positive T cell and endothelial cell. Other antimetabolites act by interfering with DNA synthesis by blocking the methylation of deoxyuridylic acid to thymidylicacid. Calcineurin inhibitors acts by inhibiting calcineurin, a phosphatase that normally dephosphorylates the cytoplasmic subunit of nuclear factor of activated T cell.29
Therapeutic uses:
1. Pityriasis lichendosis et varioliformis 2. Lymphomatoid papulosis
Review of Literature
30 | P a g e
4. Pemphigus Vulgaris 5. Pityriasis rubra pilaris 6. Lupus erythematosus 7. Dermatomyositis
8. Cutaneous T cell lymphoma 9. Psoriasis
10.Pyoderma gangrenosum 11.Behcets disease
12.Actinic keratoses 13.Actinic cheilitis 14.Bowen's disease 15.Keratocanthoma 16.Wart
17.Prokeratoses 18.Atopic dermatitis
Adverse reactions:
1. Bone marrow supression 2. Hepatic fibrosis
3. Abnormal Liver function test 4. Inflammation of the treated area 5. Hepatitis
6. Lymphoproliferative malignancy
Review of Literature
31 | P a g e
Anti-Inflammatory drugs
Some common anti inflammatory drugs administered for dermatological manifestation include: Mycophenolate mofetil, Imiquimod, Vinblastine, Dapsone & Thalidomide.28 In a study by Totri CR et al on prescribing practices for systemic agents had reported that the most commonly used second-line agent was anti-inflammatory drug mycophenolate mofetil (30.4%) The main factors that discouraged their use were the side-effect profiles (82.6%) and perceived risks of long-term toxicity (81.7%).45
Mechanism of action:
They can modulate inflammatory cytokines such as TNF-, IFN-, 10, IL-12, cyclooxygenase-2. It can also modulate T cells by altering their patterns of cytokine release and can increase keratinocyte migration and proliferation. It also has the property to inhibit adherence of antibodies to neutrophils and decrease the release of eicosanoids and block their inflammatory effects.
Anti-inflammatory drug such as mycophenolate has the ability to inhibit the enzyme inosine monophosphate dehydrogenase.
Therapeutic uses:
1. Autoimmune blistering disorder
2. Inflammatory disease- psoriasis, atopic dermatitis and pyodermagangrenosum
3. Actinic keratoses
Review of Literature
32 | P a g e
6. Bullous systemic lupus erythematosus 7. Erythema elevatumdiutinum
8. Acne fulminans 9. Pustular psoriasis 10. Lichen planus 11. Pemphigus vulgaris 12. Bullous pemphigoid 13. Leukocytoclasticvasculitis 14. Urticarial vasculitis
Adverse reactions:
1. Progressive multifocal leukoencephalopathy and pure red cell aplasia 2. Irritant reactions such as edema,vesicles,erosions or ulcers
3. Agranulocytosis,peripheral neuropathy and psychosis
4. In utero exposure can cause limb abnormalities and congenital anomalies 5. Irreversible neuropathy
Biological agents
Review of Literature
33 | P a g e
underlying immune and inflammatory disease processes but further research in this field is needed to establish the efficacy, safety and cost-effectiveness of the biological therapies currently available, and to support the development of new treatments options.46
Mechanism of action:
T cell activation inhibited by binding to CD-2 on the surface of T-cell
Apoptosis of memory-effector T cell leading to reduction in CD4 lymphocyte counts
Tumour necrosis factor inhibitors blocks the TNF-
It also inhibits protein synthesis through ADP ribosylation leading to cell death
Therapeutic uses:
1. Psoriasis
2. Psoriatic arthritis
3. Cutaneous T -cell lymphoma
Adverse reactions:
1. Peripheral leukocytosis
2. Thrombocytopenia & rebound psoriasis 3. exacerbation of congestive heart failure
4. Pain, fever, chills , nausea ,vomiting and diarrhoea 5. Hypersensitivity reaction
Review of Literature
34 | P a g e
Sunscreens
Sunscreens can be classified into UVA agents and UVB agents.
UVA agents are : avobenzone, oxybenzone, titanium oxide ,zinc oxide and ecamsule
UVB agents such as : p-aminobenzoic acid esters, cinnamates, octocrylene and salicylates.29
In a study by D Rweyemamu out of 830 drugs prescribed , sunscreens (68) were one of the topical miscellaneous drugs prescribed.47
Mechanism of action:
Sunscreens consists of chemical agents that can absorb incident solar radiation of UVB and/or UVA ranges and physical agents that can block or reflect incident energy and reduce the transmission to skin
Therapeutic uses:
1. Prevents incident sunlight that can cause erythema or redness on skin 2. Reduce actinic keratoses
3. Squamous cell carcinoma of skin
Intravenous Immunoglobulin
Review of Literature
35 | P a g e
David Chandler , there has been reports of clinical improvement in patients with atopic dermatitis treated with adjunctive high-dose intravenous immunoglobulin (hdIVIg) . However, small clinical trials have failed to demonstrate any significant clinical improvement, and have shown significantly lower efficacy of IVIg.46
Mechanism of action:
Suppression of Ig G production
Accelerated catabolism of Ig G
Neutralization of complement mediated reaction
Neutralization of pathogenic antibodies
Downregulation of inflammatory cytokines
Inhibiton of autoreactive T lymphocytes
Inhibiton of immune cell trafficking
Blockade of Fas-ligand/Fas receptor interactions
Therapeutic use:
1. Autoimmune bullous disease 2. Toxic epidermal necrolysis 3. Connective tissue disease 4. Vasculitis
5. Urticaria
6. Atopic dermatitis
Review of Literature
36 | P a g e
Adverse reaction:
1. Fluid overload in congestive heart failure and renal failure patients 2. Renal failure in patients with rheumatoid arthritis or cryoglobulinemia
Emollients
Emollients are bland oily substances which helps in soothening and softening the skin surface. Some commonly used emollients include olive oil, arachis oil, sesame oil, cocoabutter, hard and soft paraffin, liquid paraffin,wool fat,bees wax and spermaceti. 28A study by Purushotham K et al had reported that emollients and skin protective agents were one of the commonly prescribed class of drugs (51%).48
Mechanism of action 49
Emollients acts as an inert oily layer over the surface of the skin. This residual film of oil on the skin surface aids in prevention or at least impedes evaporation of water from the skin surface and reduces the rate at which water is traversing the skin, thus trapping it within the upper layers of stratum corneum, this allows softening and smoothening of the skin surface.
Therpeutic uses:
1. Dry skin conditions in patients with atopic dermatitis, hypothyroidism, uraemia and lymphoma.
Review of Literature
37 | P a g e
Keratolytic agents
Keratolytic agents used in dermatology include salicylic acid,resorcinol,urea and sulfur.28,29 In a study by Anuj Kumar Pathak , keratolytics were grouped under other drugs and these constituted 5.91% of the prescriptions.1 In another study by Doddarangaiah R S , steroids with keratolytic was prescribed in 33.21% of patients .50
Mechanism of action:
Breaking of intercellular junctions
Increasing stratum corneum water content
Increasing desquamation
Therapeutic uses:
1. Psoriasis
2. Seborrheic dermatitis 3. Xerosis
4. Icthyoses 5. Verrucae
Review of Literature
38 | P a g e
Drugs for Androgenetic Alopecia
Androgenetic alopecia (AGA) is a common dermatological condition associated with frequent hair thinning or hair loss affecting both men and women. Commonly used drug for androgenetic alopecia include minoxidil and finasteride.29,39 A study by B.S Chandrasekhar on Topical minoxidil fortified with finasteride showed that 84.44% patients maintained the density well, showing the effectiveness of the combination in maintaining hair growth.51
Mechanism of action:
It enhances follicular size resulting in thicker hair shafts
It stimulates and prolongs anagen phase of the hair cycle resulting in longer and increased number of hairs
Adverse effects:
1. Allergic and contact dermatitis
2. Genital abnormalities in male fetuses if exposed to pregnant women 3. Decreased libido
4. Erectile dysfunction 5. Ejaculation disorder
Review of Literature
39 | P a g e
Drugs for Hyperpigmentation
Melanizing agents include hydroquinone, monobenzone and Azelaic acid. It is effective mostly for hormonally or light induced pigmentation within the epidermis.28,29 Debabrata Bandyopadhyay had stated that hydroquinone remained the gold standard of topical treatment but concerns regarding its side effects still remains.52
Mechanism of action:
It inhibits tyrosinase and other melanin forming enzymes
Decreases the formation of and increases degradation of melanosomes
Therapeutic uses:
1. Melasma
2. Chloasma of pregnancy 3. Widespread vitiligo patients 4. Acne and papulopustular rosacea
Adverse effects:
1. Skin irritation , rashes and allergy 2. Dermatitis
Review of Literature
40 | P a g e
Anti-Seborrheic agent
Rosso J Q Det al reported that the treatment options for seborrheic dermatitis, involving scalp or other sites, included several studies inclusive of multiple agents (number of studies, N=number of actively treated subjects): selenium sulfide 2.5% shampoo (1, N=95), propylene glycol solution 35 to 50% (1, N=37), hydrocortisone 1% cream (3, N>58), ketoconazole 2% shampoo (3, N=181), ketoconazole 2% cream (4, N=89), miconazole 2% cream (1, N=22), bifonazole 1% shampoo (2, N=59), ciclopirox 1% cream (1, N=57), ciclopirox 1.5% shampoo (1, N=102), and lithium succinate 8%/zinc sulfate 0.05% ointment (1, N=82)53. Seborrheic dermatitis occurs in areas which are rich in sebaceous gland and is asscoiated with erythematous and scaling lesions. Anti-seborrheic agents include selenium sulfide , zinc pyrithione , corticosteroids , imidazole antifungals , sulfur , resorcinol , coaltar , ammoniated mercury and salicylic acid.29
Mechanism of action:
It acts as an fungicidal agent to Pityrosporum ovale which is a causative agent for seborrhoea
It reduces epidermal turnover
Adverse reactions:
1. Sensitivity reactions 2. Atrophy
Review of Literature
41 | P a g e
Drugs for Acne vulgaris
Acne vulgaris is a common dermatological manifestation among adolescent boys and girls. It occurs by androgenic stimulation of sebaceous follicles of face and neck leading to colonization by bacteria and yeast such as propionibacterium acne, staphylococcus epidermis and pityrosporum ovale. Some commonly used drugs for acne vulgaris include topical drugs such as benzoyl peroxide , retinoic acid, adapalene ,topical antibiotic and azelaic acid and systemic drugs such as antibiotics which includes tetracycline,minocycline or erythromycin and isoretinoin.29 In a study Nibedita Patro et al reported that out of 3634 drugs prescribed, 1724 (47.44%) were oral and 1910 (52.56%) were topical formulations. In oral formulations, isotretinoin {1174 (68.10%)} was the most frequently prescribed drug, as compared to 550 (31.90%) prescriptions of antibiotics. Doxycycline {298 (54.18%)} was the most frequently prescribed oral antibiotic followed by azithromycin {213 (38.73%)}, minocycline{30 (5.45%)} and clarithromycin {9 (1.64%)}.54
Mechanism of action:
It is efficacious against Propionibacterium acne
It promotes lysis of keratinocytes and comedolytic property
Adverse effects:
Review of Literature
42 | P a g e
5. Contact sensitization
6. Warmth and stinging sensation 7. Cheilitis
8. Epistaxis 9. Pruritis
10.Conjunctivitis 11.Paronychia
12.Rise in serum lipids and intracranial tensions 13.Musculoskeletal symptom
Drug utilization studies
Drug utilization studies play a major role in helping to understand, interpret, and also improve the prescribing, administration, and use of medications in a well managed health care systems.55 The pioneering work of Arthur Engel in Sweden and Pieter Siderius in Holland alerted many investigators to the importance of comparing drug use.
Definition56
Review of Literature
43 | P a g e
Why drug utilization studies ?57
The major objective of DUS is to facilitate a rational use of drugs in the population. The objectives are :
To increase our understanding of how drugs are being used.
To give an early signal of irrational use of a drug
To analyse whether the steps taken to improve drug utility have acquired the required impact.
To help the healthcare system to know, interpret, analyse andimprove the drug prescription, use and administration of medication.
To provide insight into the effectiveness of drug use.
To set priority for sensible distribution of healthcare budgets
Sources of drug utilization data56
Data sources for drug utilization can be obtained from general practitioners , from pharmacy records , from drug regulatory agencies , from drug suppliers and from population through health surveys like surveys conducted among females, elderly out patients or at nationallevel.
Study designs for drug utilization studies56
The study designs in DUS are mainly:
Prospective
Concurrent
Review of Literature
44 | P a g e
Prospective drug utilization study consists of evaluating the patient’s disease and its intended drug therapy before a drug is given.
It generally addresses the generic substitution, drug-disease contraindications, therapeutic interchange and wrongdosage, improper duration of treatment, clinical abuse and drug allergy.
Concurrent drug utilization study consists of monitoring of drug therapy which is on progress, to guarantee positiveresults. It also addresses drug - age precautions, extreme dose, low or high dosage, over or underutilization, drug-drug interactions.
Retrospective drug utilization studies consists of review of drug therapy after the patient has taken the drug. It also notices the prescribing pattern of the drugs, administeration or dispensing of drugs to avoid improper use of drugs. This study includes case report, case series and case control studies.
Assessment of WHO drug use indicators56
A. Core indicators:
a) Prescribing indicators:
Average number of medications per consultation- to measure the degree of polypharmacy.Combination drugs are counted as one.
Percentage of medications prescribed by generic name - to measure the tendency to prescribe by generic name.
Review of Literature
45 | P a g e Percentage of consultations with an antibiotics prescribed.
b) Patient care indicators:
Average consultation time
Average dispensing time
Patient’s awareness about correct dosage
Percentage of drugs actually dispensed
c) Facility indicators:
Availability of copy of Essential Drug List (EDL)
Availability of important drugs
B. Complementary indicators:
Percentage of patients treated without medications
Average drug cost per consultation - to measure cost of drug treatment
Percentage of drug cost spent on injections- to measure the overall impact of infection where commonly overused.
Normal values:
Average number of drug per consultation - 2-3
Percentage of consultation with an injection prescribed - 16-20%
Percentage of drugs prescribed by generic name - 100%
Percentage of drugs prescribed from essential drug list (EDL) - 80-100%
Review of Literature
46 | P a g e
Steps in drug utilization studies58:
1) Recognize the therapeutic areas of practice or drugs to include in the program 2) Design of study
3) Define criteria and standards 4) Design the data collection form 5) Data collection
6) Evaluate results
7) Provide feedback of results
8) Develop and implement interventions
9) Reassess and revise the drug utilization evaluation program
Pharmacovigilance
Nowadays people are using more of efficacious andnewer drugs for diverse medical conditions in large scale. The two important concerns regarding any drug are their safety and efficacy. Hence pharmacovigilance plays a vital role in the rational use of drugs by giving details about the adverse drug reactions occuring due to drugs in the general population.59
Definition59:
Review of Literature
47 | P a g e
Current status of Pharmacovigilance in India
Now a days in India, pharmacovigilance situation has been progressing gradually step by step than what it was present earlier in the past.60 In the world survey , India has been enlisted as the fourth amongproducers of pharmaceuticals. It is rising as one of the nation for the clinical trial hub in the world .59 Many new drugs has been introduced by our country and hence an energetic pharmacovigilance system in the country is essential to guard the people from the possible harm that may arise by some of these new drugs.61 Evidently, the Central Drugs Standard Control Organization (CDSCO) has started a well planned and highly participative National Pharmacovigilance Program. It is based mainly on the recommendations made in the WHO document titled “Safety Monitoring of Medicinal Products Guidelines for Setting up and Running a Pharmacovigilance Centre”.62 In India the rate of pharmacovigilance accounts for less than 1% when compared to the world rate of 5%. This has occured due to lack of knowledgeabout the subject and also deficiency in training.
Pharmacoeconomics65
Review of Literature
48 | P a g e
Its aim is to compare the alternative solutions which are available on the basis of the relationship between necessary resources and results to be obtained. This definition highlights two concepts of fundamental importance for application of the economic principle the possibility of choosing between alternatives and comparing on the basis of costs and effects.
Studies on Drug utilization pattern for skin disease in
Dermatology
In a study by Rathod SS et al on prescribing practices of topical corticosteroids in the outpatient dermatology department of a rural tertiary care teaching hospital ,had stated that out of 500 prescriptions - (2,050 drugs) the average number of drugs per prescription being 4.1. About 66% of the prescriptions contained four to five drugs. This reflects a trend toward polypharmacy.64
Review of Literature
49 | P a g e
(106), 71.1% were topical and 28.9% oral preparations. A total of 46 emollient, creams were prescribed. Vitamins, minerals and antioxidants comprised about 70 drugs, out of which 90% were advised by oral route and 10% topically. 22 antiseptics & ectoparasiticides were prescribed and all by topical route. Antiviral agents were 10 in number and were prescribed mainly by oral route. Rest of the drugs were miscellaneous out of which 25.2% of them were oral drugs, 73.3% topical agents and 1.5% were injectables.10In another study by Anand S et al on the prescription pattern for dermatological conditions among specialists and general practitioner had stated that the commonly prescribed class of drugs were antifungals-15.02%, anti-allergics-12.95%, antibiotics-3.92%, steroids 29.16%, scabicides 8.49%,analgesics 3.92% , anti-dandruff preparations 7.62% and vitamins & minerals 0.54%.65
Review of Literature
50 | P a g e
clindamycin for acne treatment was very common. Other than this mupirocin and fusidic acid and other fixed dose combinations of two or more antibiotics or along with steroids were used very frequently. Among antiparasites permethrin, ivermectin for scabies and albendazole and mebendazole as anthelmintics were prescribed in very few cases.1
In a study by Gupta S et al stated that Antifungals (19.4%), Antibiotics (17.6%), Antihistamines (15.9%) and Corticosteroids (9.4%) were the most common class of drugs prescribed in theirhospital. This study had revealed that the commonly prescribed antifungals were terbinafine, ketoconazole, sertaconazole, fluconazole, itraconazole and miconazole, while the commonly prescribed antibacterials were clindamycin, azithromycin, nadifloxacin, cefpodoxime, fusidic acid, neomycin, doxycycline and linezolid. Commonly prescribed H1antihistamines were levocetrizine, hydroxyzine, fexofenadine and loratadine. Topical corticosteroids (glucocorticoids) commonly employed were betamethasone, clobetasol, mometasone, halobetasol, beclomethasone, halometasone. The common insecticide chosen for scabies was permethrin topically.66
Studies related to Pharmacovigilance of drugs used in
dermatology
Review of Literature
51 | P a g e
were the most commonly suspected drugs followed by unknown medicines of 29% for cutaneous ADR.67
Nandha et al in a study had stated that most of the common offending drug class belonged to antimicrobials followed by NSAIDS.66
A study by Saha A et al reported that the commonest cutaneous ADRs were morbilliform eruption (30.18%), followed by fixed drug eruption(24.52%). This study also stated that 17% of cutaneous ADRs were due to Sulfa drugs followed by fluroquinolones(11.30%).68
Lihite RJ et al had stated in his study that the incidence of dermatological adverse drug reactions in outdoor patients accounted for 1.6%.69A Study conducted by Achayra T et al had reported that the severity of adverse cutaneous drug reactions assessment to be 83% moderate and 15% mild in nature using a Hartwig and Siegel’s scale.70
Gohel D on his study on evaluation of dermatological adverse drug reaction in the outpatient department of dermatology at a tertiary care hospital revealed that the incidence of dermatological ADRs in outdoor patients was 3.78% out of which the most common offending drug classes were anti-microbial agents 42 (43.30%) followed by NSAIDs - 26 (26.80%) , corticosteroids 9 (26.80%) and anti-epileptic 5 (5.15%) .71
Review of Literature
52 | P a g e
(16.66%). ADR findings in that study suggested that the cause for most adverse drug reactions were antimicrobials (50%) followed by NSAIDs (22%). Severity assessment by modified Hartwig and Siegel’s scale in the study showed that out of 18 ADRs, 8(44.44%) were mild, 8 (44.44%) were moderateand 2 (11.11%) were severe in nature in nature.72
Studies on cost of drugs used for skin diseases
In a study by Narwane S.P et al had stated that an average total cost per prescription was found to be INR135.60, while average hospital and outside pharmacy costs were INR19.40 and INR116.20 respectively .73In a study by Bijoy KP et al on drug prescribing pattern and economic analysis for skin diseases in dermatology OPD reported that the average cost of drugs per prescription was found to be 196.74 INR.13
Aims and objectives
53 | P a g e
Aims and objectives
To determine the prescribing pattern of drugs, their cost and adverse reactions in the outpatient department of dermatology of a tertiary care hospital.
Objectives :
1. To analyse the pattern of drugs prescribed in dermatology using WHO prescribing indicators.
2. To evaluate the cost of therapy per prescription 3. To assess causality of the adverse drug reactions
WHO prescribing indicators analyzed are :
1. Average number of medications per encounter - to measure the degree of polypharmacy . Combination drugs are counted as one.
2. Percentage of medications prescribed by generic name - to measure the tendency to prescribe by generic name.
Methodology
54 | P a g e
Methodology
Materials and methods:
Study design:
This study was a cross sectional study.
Study setting:
This study was conducted at outpatient clinic of Department of Dermatology at Sree Mookambika Institute of Medical Sciences, Kulasekaram, Kanyakumari district, Tamilnadu.
Period of study:
This study was done for 1 year from February 2016 to January 2017.
Inclusion criteria:
i.Patients attending Dermatology Out Patient Department from February 2016 to January 2017
ii.Patients of both sexes above the age of 18 years
iii.Same patients attending outpatient department with a new dermatological condition during the study period.
Exclusion criteria:
i. Patients already recruited in the study coming for review to the outpatient department , SMIMS
Methodology
55 | P a g e
Institutional Human Ethics Committee(IHEC) Approval:
The study proposal was approved by the Institutional Human Ethics Committee (IHEC) of SMIMS with Ref. No. SMIMS/IHEC/2015/A/06. The certificate of approval for the same has been enclosed (Annexure-I). Confidentiality and anonymity of patients information were maintained during and after the study.
Procedure:
Methodology
56 | P a g e
Outcome parameters :
A. Data obtained from case record form were evaluated for:
i.Pattern of dermatological drugs used as per demographic profile
ii.Frequency in utilization of different classes of dermatological drugs prescribed
iii.Number of patients receiving fixed dose combinations for dermatological treatment
B.Prescribing indicators
The data collected were analysed and compared with values of WHO prescribing indicators given below :
i.Average number of drugs prescribed per encounter (Avg. no. of drugs prescribed per encounter) was calculated to measure the degree of polypharmacy
Average number of drugs prescribed per encounter =
Total number of drugs prescribed
Number of encounters surveyed
Combinations of drugs for one health problem were counted as one.
Methodology
57 | P a g e
% of drugs prescribed by generic name =
Number of drugs prescribed by generic name
Total number of drugs prescribed
iii. Percentage of encounter with an antibiotic prescribed was calculated to measure the overuse of antibiotics
% of encounter with antibiotic prescribed =
Number of encounters with antibiotic prescribed
Number of encounters surveyed
iv. Percentage of drugs prescribed from EDL was calculated to measure the degree to which practices conform to a national drug policy as indicated in the national list of India
% of drug prescribed from EDL =
Number of drugs prescribed from EDL Total number of drugs prescribed
The above data were compared with WHO values given below : 1. Average number of drugs per encounter : 2-3
2. Percentage of drugs prescribed by generic name : 100% 3. Percentage of drugs prescribed from EDL : 80-100%
4.Percentage of encounter with antibiotics prescribed : less than 40%
x 100 x100
Methodology
58 | P a g e
C. Average drug cost per encounter per day
Avg . drug cost per encounter /day =
Total cost of all drugs prescribed
No. of encounter surveyed
D. Number of patients who experienced different ADRs for different classes of dermatological drugs
E. Casuality assessment of ADRs reported in patients prescribed with dermatological drugs by using WHO-UMC causality assessment scale (Appendix - IV).
Analysis of data :
Observation & results
59 |P a g e
Observation & results
A descriptive, quantitative and cross-sectional survey was conducted to determine the drug prescribing pattern, cost analysis and ADRs at the outpatient department of dermatology. A sample of 171 patient encounters was assessed prospectively from February 2016 to January 2017. Data were collected from prescriptions.
The baseline demographic characteristics and pattern of dermatological drug use :
[image:73.612.109.512.298.442.2](Table - 1,2,3)
Table-1: Age wise prevalence of dermatological drug use
Age (years) Number of cases (n) Percentage
Less than 20 20 11.70
21-40 80 46.78
41-60 49 28.65
Above 60 22 12.87
Total 171 100.00
The usage of dermatological drugs was maximum in the age group of 21-40 yrs (n=80, 46.78%).The mean age was 38.67
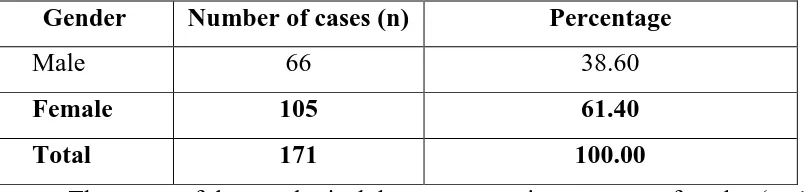
Table-2: Gender wise prevalence of dermatological drug use
Gender Number of cases (n) Percentage
Male 66 38.60
Female 105 61.40
Total 171 100.00
[image:73.612.110.516.518.614.2]Observation & results
[image:74.612.107.528.127.373.2]60 |P a g e
Table-3: Distribution of patients based on illness
Type of illness Number of cases(n) Percentage
Eczema 37 21.64
Tinea 27 15.79
PMLE 10 5.85
Dermatitis 17 9.94
Urticaria 27 15.79
Others 53 30.99
Total 171 100.00
PMLE -Polymorphous Light Eruption
Observation & results
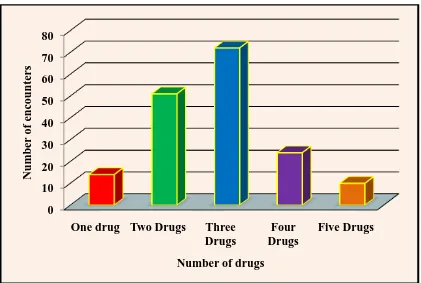
[image:75.612.109.530.95.378.2]61 |P a g e
Figure-1: Distribution of encounters based on number of drugs prescribed
Out of 171 prescriptions, three drugs per prescription were most commonly prescribed (n=72, 42.10%) and least common was five drugs per prescription (n=10, 5.84%)
Table - 4 : Distribution of encounters based on number of drug prescribed
Number of cases (n) Percentage
Single drug 14 8.18%
Two drugs 51 29.82%
Three drugs 72 42.10%
Four drugs 24 14.03%
Five drugs 10 5.84%
Total 171 100.00
Maximum number of patients (n=72, 42.10%) received three drugs for dermatological disorders. Most commonly prescribed monotherapy drug was tablet levocetrizine in 14 patients (8.18%)
0 10 20 30 40 50 60 70 80
One drug Two Drugs Three Drugs Four Drugs Five Drugs Num b er of e n cou n te rs
[image:75.612.107.525.478.641.2]Observation & results
62 |P a g e
[image:76.612.88.561.142.523.2]Utilization of various classes of dermatological drugs
prescribed
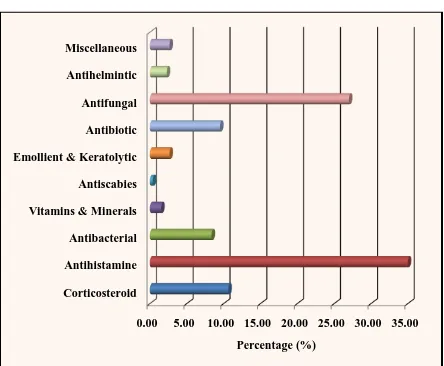
Figure-2: Distribution of various classes of dermatological drugs prescribed
Out of 171 prescriptions, the class of drugs most commonly prescribed was antifungals (27 % ) and least prescribed was antidandruff (1.05%)
0 5 10 15 20 25
Antihistamine Anti fungal Anti biotic Steroids Keratolytic & emollients vitamin & minerals Antiparasite & antiseptic Antidandruff others
Percentage (%)
Clas
s
of
drug
s
12.05
1.05
1.26
5.07
9.09
17.12
9.51
23.25
Observation & results
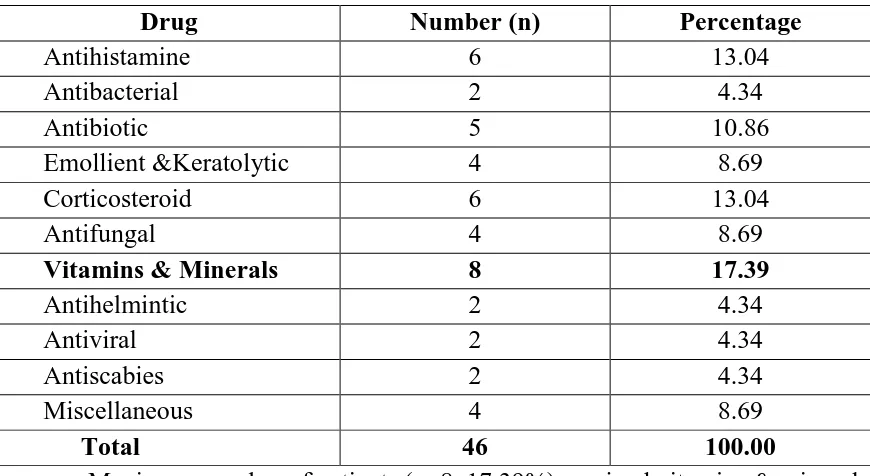
[image:77.612.107.534.117.332.2]63 |P a g e
Table-5: Frequency of utilization of different classes of dermatological drugs in a two drugs prescription
Drug Number (n) Percentage
Corticosteroid 22 22.44
Antihistamine 26 26.53
Antibacterial 5 5.10
Antibiotic 11 11.22
Emollient &Keratolytic 13 13.26
Vitamins & minerals 4 4.08
Antifungal 12 12.24
Antihelmintic 2 2.04
Antimetabolite 1 1.02
Antiviral 2 2.04
Total 98 100.00
Maximum number of patients (n=26, 26.53%) received antihistamine in a two drug prescription pattern.
Table-6: Frequency of utilization of different classes of dermatological drugs in a three drugs prescription
Drug Number (n) Percentage
Corticosteroid 45 20.83
Antihistamine 56 25.92
Antibacterial 9 4.16
Antibiotic 9 4.16
Emollient &Keratolytic 28 12.96
Vitamins & minerals 9 4.16
Antifungal 52 24.07
Antihelmintic 3 1.38
Skin antiseptic & disinfectant 1 0.46
Miscellaneous 4 1.85
Total 216 100.00
[image:77.612.108.524.416.638.2]Observation & results
[image:78.612.108.525.116.318.2]64 |P a g e
Table-7: Frequency of utilization of different classes of dermatological drugs in a four drugs prescription