A
AN
NT
TI
IB
BI
IO
OT
TI
IC
CS
S
S
SU
UR
RV
VE
EI
IL
LL
LA
AN
NC
CE
E
P
PR
RO
OG
GR
RA
AM
M:
:
S
SU
UR
RV
VE
EY
Y
O
ON
N
T
TH
HE
E
R
RE
ES
SI
IS
ST
TA
AN
NC
CE
E
P
PA
AT
TT
TE
ER
RN
NS
S
O
OF
F
M
MI
IC
CR
RO
OO
OR
RG
GA
AN
NI
IS
SM
MS
S
T
TO
O
A
AN
NT
TI
IB
BI
IO
OT
TI
IC
CS
S
I
IN
N
N
NO
OS
SO
OC
CO
OM
MI
IA
AL
L
I
IN
NF
FE
EC
CT
TI
IO
ON
NS
S
Dissertation Submitted to
The Tamil Nadu Dr. M.G.R Medical University, Chennai
In partial fulfillment for the requirement of the Degree of
M
M
A
A
S
S
T
T
E
E
R
R
O
O
F
F
P
P
H
H
A
A
R
R
M
M
A
A
C
C
Y
Y
(
(P
Ph
ha
ar
r
ma
m
ac
cy
y
P
Pr
ra
ac
ct
ti
ic
c
e)
e
)
S
Su
ub
bm
mi
it
tt
te
ed
d
b
by
y:
:
R
Re
eg
g
N
No
o.
.
2
26
61
10
07
72
29
90
0
APRIL 2012
D
De
ep
pa
ar
rt
tm
me
en
nt
t
o
of
f
P
Ph
ha
ar
rm
ma
ac
cy
y
P
Pr
ra
ac
ct
ti
ic
ce
e
K
K
M
M
C
C
H
H
C
C
O
O
L
L
L
L
E
E
G
G
E
E
O
O
F
F
P
P
H
H
A
A
R
R
M
M
A
A
C
C
Y
Y
K
KOOVVAAIIEESSTTAATTEE,,KKAALLAAPPAATTTTIIRROOAADD,,
C
Dr. A. Rajasekaran, M.Pharm., Ph.D
Principal,
KMCH College of Pharmacy, Kovai Estate, Kalappatti Road, Coimbatore - 641 048. (T.N)
CERTIFICATE
This is to certify that the dissertation work entitled “ANTIBIOTICS SURVEILLANCE PROGRAM: SURVEY ON THE RESISTANCE
PATTERNS OF MICROORGANISMS TO ANTIBIOTICS IN
NOSOCOMIAL INFECTIONS” submitted by Mr. Sheril K.C, is a bonafide work carried out by the candidate under the guidance of Mr. K. Chandrasekaran M. Pharm., and submitted to the Tamil Nadu Dr. M.G.R. Medical University, Chennai, in partial fulfillment for the Degree of Master of Pharmacy in
Pharmacy Practice at the Department of Pharmacy Practice, KMCH College of Pharmacy, Coimbatore, during the academic year 2010-2012.
K Chandrasekaran, M. Pharm.,
Asst. Professor & Clinical Pharmacist, Department of Pharmacy Practice, KMCH College of Pharmacy Coimbatore.
CERTIFICATE
This is to certify that the dissertation work entitled “ANTIBIOTICS SURVEILLANCE PROGRAM: SURVEY ON THE RESISTANCE
PATTERNS OF MICROORGANISMS TO ANTIBIOTICS IN
NOSOCOMIAL INFECTIONS” submitted by Mr. Sheril K.C, to the Tamil Nadu Dr. M.G.R. Medical University, Chennai, in partial fulfillment for the Degree of Master of Pharmacy in Pharmacy Practice is a bonafide work carried out by the candidate under my guidance at the Department of Pharmacy Practice, KMCH College of Pharmacy, Coimbatore, during the academic year 2010-2012.
K Chandrasekaran, M. Pharm.,
DECLARATION
I do hereby declare that the dissertation work entitled “ANTIBIOTICS SURVEILLANCE PROGRAM: SURVEY ON THE RESISTANCE
PATTERNS OF MICROORGANISMS TO ANTIBIOTICS IN
NOSOCOMIAL INFECTIONS” submitted to the Tamil Nadu Dr. M.G.R.
Medical University, Chennai, in partial fulfillment for the Degree of Master of Pharmacy in Pharmacy Practice, was done by me under the guidance of Mr. K. Chandrasekaran, M.Pharm., at the Department of Pharmacy Practice, KMCH College of Pharmacy, Coimbatore,during the academic year 2010-2012.
EVALUATION CERTIFICATE
This is to certify that the dissertation work entitled “ANTIBIOTICS SURVEILLANCE PROGRAM: SURVEY ON THE RESISTANCE
PATTERNS OF MICROORGANISMS TO ANTIBIOTICS IN
NOSOCOMIAL INFECTIONS” submitted by Mr. Sheril K.C, Reg. No: 26107290 to the Tamil Nadu Dr. M.G.R. Medical University, Chennai in partial fulfillment for the Degree of Master of Pharmacy in Pharmacy Practice is a bonafide work carried out by the candidate at the Department of Pharmacy Practice, KMCH College of Pharmacy, Coimbatore and was evaluated by us during the academic year 2010-2012.
Examination Center: KMCH College of Pharmacy, Coimbatore.
Date:
Internal Examiner External Examiner
ACKNOWLEDGEMENT
I pay obeisance to the Almighty for blessing me with all the confidence, courage, Inspiration, and curiosity to complete this project.
It is my privilege to submit my deepest sense of gratitude and respectful regard to my beloved Guide Mr. K. Chandrasekaran M.Pharm., Assistant Professor & Clinical Pharmacist, Department of Pharmacy practice, KMCH College of Pharmacy, Coimbatore, for his excellent guidance, constant encouragement and inspiration given throughout the tenure of the dissertation work.
I express my sincere thanks and gratitude to my Principal, Dr. A. Rajasekaran, M.Pharm., Ph.D KMCH College of Pharmacy for providing me with a cooperative and creative environment to work excellently.
I am overwhelmed by the generous help, and enthusiastic encouragement offered by
Dr. P. Chinnaswami, Ph.D, M.Sc, FICS, MAACC, FIFCC (Clinical chemistry),
Medical Laboratory, KMCH.
I express my sincere thanks to Mr. D. Gandhiraj, M.Sc, Med, (Micro) Microbiology Department, KMCH, and all the staffs of Microbiology Department for their help and co-operation.
My heartfelt thanks to my Lecturers, Dr. SUCHANDRA SEN, M.Pharm., Ph.D., A. VIJAYAKUMAR, M.Pharm., Mr. V. SIVAKUMAR, M.Pharm., Mr. S.
PALANISWAMY, M.Pharm., (Ph.D)., Mrs. K. GEETHA, M.Pharm., (Ph.D).,
Mr. C. DANDAPANI, M.Pharm., and all other teaching and non-teaching staffs for their encouraging suggestions and judicious help.
I extend my sincere thanks to our beloved chairman Dr. Nalla. G. Palaniswami MD., AB (USA)., and Madam Trustee Dr. Thavamani D. Palaniswami, MD., of Kovai Medical Center Research and Educational Trust, Coimbatore for providing me with all the facilities to carry out a work of this kind in a corporate hospital.
I am deeply obliged with warm gratitude towards my Mom, Shelin and Sherun for their faith in me and for the prayers they have offered for me for the completion of this project work in a fruitful manner.
It’s my privilege to express my deep sense of gratitude and love to all my dear
classmates, seniors, juniors and friends for their memorable company and encouragement.
Last but not the least, I thank one and all who are directly or indirectly involved in this study and the Almighty to complete this herculean task successfully.
LIST OF ABBREVIATIONS
AMR - Antimicrobial Resistance BSI - Blood Stream Infections
BW - Birth Weight
CAP - Community Acquired Pneumonia
CAUTIs - Catheter Associated Urinary Tract Infections CDC - Center for Disease Control and Prevention EARSS - European Antimicrobial Resistance Surveillance
System
HAI - Hospital Acquired Infections HCAP - Health Care Associated Pneumonia ICU - Intensive Care Unit
MDR-TB - Multi Drug Resistant Tuberculosis MLST - Multi Locus Sequence Typing
MRSA - Methicillin Resistant Staphylococcus Aureus NDM-1 - New Delhi Metallo beta lactamase
NICU - Neonatal Intensive Care Unit NIs - Nosocomial Infections
NNIS - National Nosocomial Infection Surveillance PABA - Para Amino Benzoic Acid
pBSI - Primary Blood Stream Infection PDR - Potentially Drug Resistance PFGE - Pulsed Field Gel Electrophoresis RICU - Respiratory Intensive Care Unit SICU - Surgical Intensive Care Unit
SOFA - Sepsis Related Organ Failure Assessment SSTI - Skin and Soft Tissue Infections
TBSAB - Total Body Surface Area Burn VRE - Vancomycin Resistant Enterococci WHO - World Health Organization
INDEX
S.No
CONTENTS
PAGE
No.
1. 2. 3. 4. 5. 6. 7 8. 9 10 INTRODUCTIONREVIEW OF LITERATURE
AIM AND OBJECTIVES
PLAN OF STUDY
METHODOLOGY
RESULTS AND DISCUSSION
TABLES & GRAPHS
SUMMARY AND CONCLUSION
BIBLIOGRAPHY
ANNEXURES
Annexure I : Permission letter from Hospital Authority Annexure II : Permission letter from Ethics Committee Annexure III : Patient Data Collection Form
1
INTRODUCTION
The emergence of resistance to antimicrobial agents is a global public health problem, particularly in pathogens causing nosocomial infections. Antimicrobial resistance results in increased illness, deaths, and health-care costs. The distribution of pathogens causing nosocomial infections, especially antimicrobial-resistant pathogens, changes with time and varies among hospitals and among different locations in the same hospital.1
The increasing number of immunocompromised patients and increased use of indwelling devices, as well as widespread use of antimicrobial agents in hospital settings, particularly in intensive care units (ICUs), contributes to antimicrobial resistance among pathogens causing nosocomial infections.
ANTIMICROBIAL RESISTANCE (AMR):
AMR is the expression of the ability of microbes to resist the actions of
naturally occurring or synthetically produced compounds inimical to their
survival. In a clinical context, AMR refers to a reduction in clinical efficacy so that
either the benefits for the individual of treatment with an antimicrobial drug or the
benefits to general public health are compromised. (WHO)2
CAUSE:
Inadequate national commitment to a comprehensive and coordinated
response, ill defined accountability and insufficient engagement of communities;
2 Inadequate systems to ensure quality and uninterrupted supply of medicines Inappropriate and irrational use of medicines, including in animal
husbandry:
Poor infection prevention and control practices;
Depleted arsenals of diagnostics, medicines and vaccines as well as
insufficient research and development on new products.3
An important cause of increasing antibiotic resistance is the selection of resistant bacterial strains by mutation and transfer of mobile resistance genes as a result of excessive antibiotic prescribing by hospital doctors. Increasing antibiotic resistance also caused by transmission of resistant bacteria within hospitals by cross colonization of patients via the hands of health care staff and subsequent spread between hospitals by transfer of colonized patients.
The use of antimicrobial agents is a powerful selective force that promotes the emergence of resistant strains. Thereby, the growth of antimicrobial resistance led a signal to reduce unnecessary antibiotic use and to improve treatment protocols to maximize the lifespan of these drugs. To reduce antimicrobial resistance, multiple and often conflicting recommendations have been made, which includes reduction of all antimicrobial classes, increased use of prophylactic antimicrobials to reduce colonization, rotation of different antibiotic classes in a temporal sequence, and simultaneous use of different antimicrobials for different patients.
3 resistant strains, improved surveillance, and aggressive control of transmission of epidemic resistant bacteria.
MECHANISM:
The four main mechanisms by which microorganisms exhibit resistance to antimicrobials are:
1. Drug inactivation or modification: for example, enzymatic deactivation of penicillin G in some penicillin-resistant bacteria through the production of β-lactamases
2. Alteration of target site: for example, alteration of PBP—the binding target site of penicillins in MRSA and other penicillin-resistant bacteria
3. Alteration of metabolic pathway: for example, some sulfonamide-resistant bacteria do not require para-aminobenzoic acid (PABA), an important precursor for the synthesis of folic acid and nucleic acids in bacteria inhibited by sulfonamides, instead, like mammalian cells, they turn to using preformed folic acid.
4. Reduced drug accumulation: by decreasing drug permeability and/or increasing active efflux (pumping out) of the drugs across the cell surface.4
SOME FACTS ABOUT AMR:
4 Resistance to earlier generation antimalarial medicines such as chloroquine and sulfadoxine-pyrimethamine is widespread in most malaria-endemic countries. Falciparum malaria parasites resistant to artemisinins are emerging in South-East Asia; infections show delayed clearance after the start of treatment (indicating resistance).
A high percentage of hospital-acquired infections are caused by highly resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci.
New resistance mechanisms, such as the beta-lactamase NDM-1, have emerged among several gram-negative bacilli. This can render powerful antibiotics, which are often the last defense against multi-resistant strains of bacteria, ineffective.5
“Antimicrobial Resistance” chosen as World health day (April 7th
) 2011 theme by WHO6
The three key, inter-related elements of the Strategy to control AMR are:
Surveillance: to monitor “how we are doing” and provide the data on
resistant organisms, illness due to them and antimicrobial usage necessary to inform action;
Prudent antimicrobial use: to reduce the pressure for resistance by
5 Infection control: to reduce the spread of infection in general (and thus
some of the need for antimicrobial agents) and of antimicrobial resistant micro-organisms in particular.
NOSOCOMIAL INFECTIONS:
An infection acquired in hospital by a patient who was admitted for a
reason other than that infection. An infection occurring in a patient in a hospital
or other health care facility in whom the infection was not present or incubating at
the time of admission. This includes infections acquired in the hospital but
appearing after discharge, and also occupational infections among staff of the
facility.
Nosocomial infections are one of the occupational biohazards that affect the health of individuals with or without predisposing factors. These are the infections acquired during hospital stay, which are found in 5 to15% (two million cases are estimated annually) of hospitalized patients and can lead to complication in 25to 33% of those admitted in ICU.
6 According to the data published by the US Centers for Disease Control and Prevention (CDC) as part of their national nosocomial infection surveillance (NNIS) System, well over half of all intensive care unit isolates from documented infections are caused by methicillin-resistant S. aureus. The type, as well as severity, of S. aureus infections and its response to antibiotic treatment are dictated by the specific suite of virulence and antibiotic resistance associated genes carried by the strain of the S. aureus causing the infection.
NOSOCOMIAL INFECTION SITES:
ROLE OF HOSPITAL PHARMACIST IN INFECTION CONTROL:
The hospital pharmacist is responsible for:
Obtaining, storing and distributing pharmaceutical preparations using
practices which limit potential transmission of infectious agents to patients
Dispensing anti-infectious drugs and maintaining relevant records (potency,
7 Obtaining and storing vaccines or sera, and making them available as
appropriate
Maintaining records of antibiotics distributed to the medical departments
Providing the Antimicrobial Use Committee and Infection Control
Committee with summary reports and trends of antimicrobial use
Having available the following information on disinfectants, antiseptics and
other anti-infectious agents:
o Active properties in relation to concentration, temperature, length of action, antibiotic spectrum
o Toxic properties including sensitization or irritation of the skin and mucosa
o Substances that are incompatible with antibiotics or reduce their potency
o Physical conditions which unfavourably affect potency during storage: temperature, light, humidity
o Harmful effects on materials.
The hospital pharmacist may also participate in the hospital sterilization and disinfection practices through:
Participation in development of guidelines for antiseptics, disinfectants, and
8 Participation in guideline development for reuse of equipment and patient
materials
Participation in quality control of techniques used to sterilize equipment in
the hospital including selection of sterilization equipment (type of appliances) and monitoring.7
SURVEILLANCE:
The systematic, ongoing collection, collation, analysis, interpretation and
dissemination of data for public health action.
9
AMR SURVEILLANCE NEEDED TO:
Detect resistant strains of public health importance
Support prompt notification and investigation of outbreaks Inform clinical treatment decisions
Guide policy recommendations
Monitor efficacy of interventions and infection control measures
NEEDFORTHESTUDY:
• Hospital-acquired infections result in significant morbidity and mortality, and contribute to escalating health care costs.
• The emergence of resistance to antimicrobial agents, despite the availability
of newer antibiotics, has become an increasing problem throughout the world, particularly in pathogens causing nosocomial infections.
10
REVIEW OF LITERATURE:
M. Merchant et al., done a prospective study about the incidence of hospital-acquired pneumonia in consecutive admissions to an 1800 bed hospital in Bombay; 991 of them to general medical wards and 895 to a 17bed medical intensive care unit (ICU). The average bed occupancy in general ward was two nurses for 56 patients, and in the ICU three nurses for 17 beds. They found One hundred and sixty eight patients developed nosocomial pneumonia: 18 (1.8%) in general wards and 150 (16.7%) in the ICU. Common isolates included Pseudomonas spp (44”/0) and Klebsiella spp (34%). The most frequently used antibiotics were cefotaxime (34%), amikacin (25%), gentamicin (23%) and ofloxacin (13%). Crude mortality in general ward patients was 88.9 vs 14.6% in patients without pneumonia. The corresponding figures for ICU patients were 67.4 vs 37.1%; 40% of the crude mortality in ICU patients with pneumonia was attributable to the infection. Infected patients stayed an additional 5.8 days in the ICU and 6.7 days in the general ward. Costs of additional stay and antibiotics accounted for 18.6% of the ICU budget. They concluded that the incidence of nosocomial pneumonia was lower than expected, despite occupancy exceeding bed capacity, low nurse:patient ratios, and extensive reuse of disposable respiratory therapy equipment. Nevertheless, nosocomial pneumonia imposes a significant financial burden on the already scarce resources available for intensive care in developing countries like India.8
12
R. Gadepalli et al., analysed risk factors for nosocomial meticillin-resistant Staphylococcus aureus (MRSA) skin and soft tissue infections (SSTIs) in three Indian hospitals. They also determined antimicrobial resistance patterns and genotypic characteristics of MRSA isolates using pulsed-field gel electrophoresis (PFGE), multilocus sequence typing (MLST) and staphylococcal cassette chromosome (SCCmec) typing. Medical records of 709 patients admitted to three tertiary hospitals with nosocomial S. aureus SSTIs were clinically evaluated. Antimicrobial susceptibility testing of patient isolates was performed in accordance with Clinical and Laboratory Standards Institute guidelines, with meticillin and mupirocin resistance confirmed by multiplex polymerase chain reaction. PFGE analysis of 220 MRSA isolates was performed, followed by MLST and SCCmec typing of a selected number of isolates. MRSA was associated with 41%, 31% and 7.5% of infections at the three hospitals, respectively. Multiple logistic regression analysis identified longer duration of hospitalisation [odds ratio (OR): 1.78; OR: 2.83 for _20 days], intra-hospital transfer (OR: 1.91), non-infectious skin conditions (3.64), osteomyelitis (2.9), neurological disorders (2.22), aminoglycoside therapy (1.74) and clindamycin therapy (4.73) as independent predictors for MRSA SSTIs. MRSA isolates from all three hospitals were multidrug resistant, with fifteen clones (IeXV) recognised. A majority of the strains possessed type III cassette. The common sequence type (ST) 239 was considered the signature MLST sequence for PFGE clone III. This major MRSA clone III was closely related to the UK EMRSA-1 and was significantly more resistant to antibiotics. Dissemination of multidrug-resistant MRSA clones warrants continuous tracking of resistant genotypes in the Indian subcontinent.10
13 and identified the etiologic and antibiotic resistant patterns associated with CAUTIs in the intensive care units (ICUs) of a large University Hospital in Alexandria, Egypt. They done a prospective active surveillance of CAUTIs in 4 ICUs during a 13-month period from January 1, 2007 through January 31, 2008 in Alexandria University Hospital using the standard Centers for Disease Control National Nosocomial Infection Surveillance (NNIS) case definitions. Rates were expressed as the number of infections per 1000 catheter days. 757 patients were monitored after ICU admission, with either existing indwelling urinary catheters (239), or got catheters inserted after ICU admission (518), for a total duration of 16301 patient days, and 10260 patient catheter days. A total of 161 episodes of infection were diagnosed, for an overall rate of 15.7 CAUTIs per 1000 catheter days. Important risk factors associated with acquiring CAUTI were female gender (Relative risk (RR), 1.7; 95% confidence interval (CI); 1.7-4.3), and previous catheterization within the same hospital admission (RR, 1.6; 95% CI; 1.3-1.96). Patients admitted to the chest unit, patients =40 years, patients with prolonged duration of catheterization, prolonged hospital and ICU stay had a significantly higher risk of acquiring CAUTIs. Out of 195 patients who had their urine cultured, 188 pathogens were identified for 161 infected patients; 96 (51%) were Candida, 63 (33.5%) gram negatives, 29 (15.4%) gram positives. The prevalence of ESBL producers among K. pneumonia and E. coli isolates was 56% (14/25) and 78.6% (11/14), respectively. They concluded that the infection control policies and procedures, CAUTI rates remain a significant problem in Alexandria University hospital. Using the identified risk factors, tailored intervention strategies are now being implemented to reduce the rates of CAUTIs in these 4 ICUs.11
14 Intensive Care Unit (RICU) of a tertiary care institute in northern India. They included 201 patients (1285 patient days) admitted to RICU over a period of one-and-a-half years. A total of 77 infections were identified in 67 patients (33.5%). The infections included pneumonia (23%), sepsis of unknown origin (10.5%), bacteremia (7.5%), urinary tract infections (1.5%), catheter related blood stream infections (1%) and Clostridium difficile colitis (1%). The most commonly identified organisms were the Acinetobacter species (34.8%), Pseudomonas aeruginosa (23.9%) and Escherichia coli (15.2%). The median length of stay in patients with and without infection was 13 days (interquartile range, IQR, 28) and 4 days (interquartile range, IQR, 3), respectively (p < 0.0001). Multivariate analysis showed the following risk factors for ICU acquired infection: the admitting diagnosis of infection (odds ratio [OR] 3.3; 95% confidence intervals [CI] 1.06e10.1), length of stay in the RICU (OR, 1.2; 95% confidence intervals [CI] 1.1e1.33); renal failure (OR, 4.7; 95% CI, 1.52e14.41) and institution of parenteral nutrition (OR, 16.9; 95% CI, 1.07e 269.03). Multivariate analysis showed the following risk factors for death in ICU: APACHE II scores (OR, 1.06; 95% CI, 1.01e1.11), and endotracheal intubation (OR, 5.07; 95% CI, 1.24e20.65). APACHE II scores (OR, 1.06; 95% CI, 1.01e1.11), and endotracheal intubation (OR, 5.07; 95% CI, 1.24e20.65). This study clearly documents a high prevalence rate of infections in the ICU, and the data suggest that occurrence of infections was associated with a prolonged ICU stay but had no significant effect on the final outcome.12
15 and pneumonia (1). Infection contributed to 75% of observed mortality. On logistic regression analysis, infected patients were more likely to die as well as stay longer in the hospital as compared to non-infected patients. Infected patients also had more central venous lines inserted. The mortality was related to percent TBSAB. Thirteen out of 18 patients who had TBSAB more than 60% died as compared to 5 out of 31 with TBSAB less than 40%. Staphylococcus aureus, Pseudomonas aeruginosa and
hemolytic streptococci (BHS) were the most frequent organisms causing hospital acquired infection. Except for BHS all other organisms were highly drug resistant. Better compliance with hand washing and barrier nursing techniques, stricter control over disinfection and sterilization practices and usage of broad spectrum antibiotics, and reduction of the environmental contamination with S. aureus are required to reduce the HAI rates.13
16 intravenous or bladder catheter, and were more often bedridden. Logistic regression demonstrated presence of an intravenous catheter (odds ratio [OR] 7.5, 95% confidence interval [CI] 2.5–22.9) and being bedridden (OR 2.9, 95% CI 1.6–5.3) as independent risk factors for BSI. In univariate analysis nosocomial BSI was associated with increased mortality (22.0% vs. 11.0%; P=0.029). After adjustment for confounding covariates, however, nosocomial BSI was not associated with mortality (hazard ratio 1.3, 95% CI 0.6–2.6). Being bedridden and increasing age were independent risk factors for death. They concluded that the Intravenous catheters and being bedridden are the main risk factors for nosocomial BSI. Although associated with higher mortality, this infectious complication seems not to be an independent risk factor for death in geriatric patients.14
17 sp. was the fourth isolated organism. A high resistance to third-generation cephalosporins was recorded in K pneumoniae and E coli isolates. They concluded that the burden of NI, and identifies the major focus for future NI control and prevention programs. Except for pBSI, BW had a poor performance as a variable for risk-stratified NI rate reporting.15
Jung et al., conducted a retrospective, observational study of 527 patients with HCAP or CAP who were hospitalized at Severance Hospital in South Korea between January and December 2008 to determine the differences between HCAP and CAP in terms of clinical features, pathogens, and outcomes, and to clarify approaches for initial antibiotic management. Of these patients, 231 (43.8%) had HCAP, and 296 (56.2%) had CAP. Potentially drug-resistant (PDR) bacteria were more frequently isolated in HCAP than CAP (12.6% vs. 4.7%; P = 0.001), especially in the low-risk group of the PSI classes (41.2% vs. 13.9%; P = 0.027). In-hospital mortality was higher for HCAP than CAP patients (28.1% vs. 10.8%, P < 0.001), especially in the low-risk group of PSI classes (16.4% vs. 3.1%; P = 0.001). Moreover, tube feeding and prior hospitalization with antibiotic treatment within 90 days of pneumonia onset were significant risk factors for PDR pathogens, with odds ratios of 14.94 (95% CI 4.62-48.31; P < 0.001) and 2.68 (95% CI 1.32-5.46; P = 0.007), respectively. They concluded that the HCAP patients with different backgrounds, various pathogens and antibiotic resistance of should be considered, and careful selection of patients requiring broad-spectrum antibiotics is important when physicians start initial antibiotic treatments.16
Oteo et al., reported the antibiotic susceptibility results of invasive
18 Surveillance System (EARSS) during the period of 2000-2002. The increasing prevalence of antibiotic resistance was a cause of serious concern, requiring an international approach to its management. In Europe, antimicrobial resistance of invasive pathogens has been monitored since 1998 by the European Antimicrobial Resistance Surveillance System (EARSS). The purpose of EARSS is to document variations in antimicrobial resistance over time and space to provide the basis for, and assess the effectiveness of, prevention programmes and policy decisions. They concluded that antibiotic multiresistance S. aureus was frequent in invasive S. aureus
in Spain, with phenotypes changing over time. However, resistance was not uniform and varied according to several parameters, such as hospital size, patient age and hospital department. Therefore, properly designed and conducted surveillance systems will continue to be essential in providing safe and effective empirical therapies. Moreover, results obtained from these surveillance systems must be used to implement prevention programmes and policy decisions to prevent emergence and spread of antimicrobial resistance.17
Rahbar et al., discussed the rate of nosocomial infection and the organisms involved as well as the antibiotic resistance in patients with bacteraemia. This study was helpful to track nosocomial bloodstream infections and emerging trends in antibiotic resistance. Study also reviewed that gram-positive cocci, including coagulase-negative staphylococci, Staphylococcus aureus, Streptococcus pneumonia
were the most common causes of nosocomial bacteraemia and accounted for 42.3% of isolates. Gram-negative bacilli were responsible for another 42.3% of isolates;
19
Mizuta et al., evaluated the utility of a novel combination antibiogram to determine the optimal combination of antimicrobial agents for empirical therapy of
Pseudomonas aeruginosa infection. Infections due to antibiotic-resistant bacteria are associated with increased morbidity and mortality. Administration of inadequate empirical antibiotic therapy has been frequently associated with increased mortality. A common cause of inadequate therapy is infection with an antibiotic-resistant pathogen. One potential option is to use empirical dual antimicrobial therapy, with the hope that at least one of the selected agents will be active against the infecting pathogen. Dual therapy is commonly used when infection due to Pseudomonas aeruginosa is suspected. In the current best-case scenario, one would consult the local antibiogram to determine the two agents to which P. aeruginosa is most often susceptible. They also suggested that the combination antibiogram allowed modest fine-tuning of choices for dual antibiotic therapy, selections based on the two antibiograms did not differ substantively. Drug combinations with the broadest coverage were consistently composed of an amino glycoside and a ß-lactam.19
20 and thus for the development of a strategy to confront this major public health problem.20
Smith et al., investigated the patients with infections due to Staphylococcus aureus, with intermediate glycopeptides resistance. Staphylococcus aureus was one of the most common causes of nosocomial and community- acquired infection. Since the emergence of Methicillin-resistant S. aureus, the glycopeptide Vancomycin has been the only uniformly effective treatment for staphylococcal infections. After performing the study, they concluded that the emergence of S. aureus with intermediate glycopeptide resistance threatens to return us to the era before the development of antibiotics. To prevent further emergence of S. aureus strains with intermediate glycopeptide resistance and the emergence of S. aureus with full Vancomycin resistance, the use of Vancomycin must be optimized, laboratory methods for the detection of resistant pathogens must be enhanced, and infection-control precautions must be strictly followed for infected or colonized patients.21
21 Fluoroquinolones (Ciprofloxacin and Levofloxacin) remained stable. Isolates of P. aeruginosa with multidrug resistance phenotypes were slowly becoming increasingly prevalent at the expense of a decrease in the prevalence of isolates with single-drug resistance phenotypes. New antimicrobial agents with activity against P. aeruginosa
will not be available in the near future, ongoing surveillance of the activities of currently available agents were critical.22
Klevens et al., presented the incidence rates and estimated number of invasive
MRSA infections and in-hospital deaths among patients with MRSA in the United
States in 2005. The standardized incidence rate of invasive MRSA was 31.8%.
Incidence rates were highest among persons 65 years and older, blacks and males.
There were 1598 in-hospital deaths among patients with MRSA infection during the
surveillance period. In 2005, the standardized mortality rate was 6.3%. They also
concluded that invasive MRSA infection affects certain populations
disproportionately. It was a major public health problem primarily related to health
care but no longer confined to intensive care units, acute care hospitals, or any health
care institution.23
Troillet et al.,evaluated potential risk factor for the detection of Imipenem-resistant Pseudomonas aeruginosa in clinical specimens from hospitalized patients. Imipenem, a broad-spectrum ß-lactam antibiotic and the first Carbapenem approved for clinical use, in an important drug for treatment of Pseudomonas aeruginosa
22 hospitalized patients. No other risk factor related to the hospital environment was identified. The use of other ß-lactam antibiotics, including third-generation Cephalosporins, did not predict resistance to Imipenem, even though Imipenem-resistant P. aeruginosa isolates were more likely to be resistant to other common antipseudomonal drugs than were Imipenem-susceptible isolates.24
Obritsch et al.,demonstrated the significant increases in resistance to single antipseudomonal agents, multidrug resistance, and dual resistance to commonly prescribed combination therapies among P. aeruginosa isolates during the 10-year period from 1993 to 2002 by using the intensive care unit surveillance study database. Nosocomial infections caused by Pseudomonas aeruginosa in critically ill patients were often difficult to treat due to resistance to multiple antimicrobials. The selection of appropriate antimicrobial therapy requires active surveillance of emerging resistance trends and continuing education among the health care providers and institution involved. They also suggested that susceptibility of antipseudomonal agents against ICU isolates decreased while multidrug resistance and dual resistance rates increased from 1993 to 2002. Significant reduction in susceptibilities of P. aeruginosa
isolates may compromise the ability to choose efficacious empirical regimens for treatment of this formidable pathogen in critically ill patients. This study also provided valuable information related to emerging trends in resistance, and dual resistance rates which were vital to clinicians in the selection of reliable empirical therapy for P. aeruginosa infections in ICU.25
Aubert et al., analyzed the effect of reducing prescription of fluoroquinolones in an intensive care unit (ICU) upon bacterial resistance, particularly as regards
23 minimum. There was a 75.8% restriction in prescriptions of fluoroquinolones. There was no significant change in bacterial ecology between the periods preceding (12 months) and following (12 months) restriction. There was a significant recovery of sensitivity of P. aeruginosa to ciprofloxacin with a decrease in resistant strains from 71.3% in the prerestriction period to 52.4% in the post-restriction period. Regarding clinical data, no significant differences were noted between the pre-restriction and the post-restriction periods, except for the number of cases of ventilator associated pneumonia with P. aeruginosa resistant to ciprofloxacin. This study also demonstrated the possibility of introducing rotation of antibiotics in an ICU.26
Hanberger et al., evaluated the incidence of decreased antibiotic susceptibility among aerobic gram-negative bacilli isolated from patients in ICUs in 5 European countries (Belgium, France, Portugal, Spain, and Sweden) by using determination of minimum inhibitory concentration. More than 20% of patients admitted to European intensive care unit (ICUs) develop an ICU acquired infection. The results showed that the most frequently isolated organisms were Enterobacteriaceae, followed by
24 suggested that hospitals should have an active program for online antibiotic resistance surveillance of common drugs, using quantitatively accurate minimum inhibitory concentration methods, to constantly evaluate antibiotic administration and pharmacy formulary options.27
Bantar et al., presented that laboratory-based data underestimate the frequency of several major resistant organisms in patients with hospital-acquired infection. Increasing bacterial resistance was a worrisome problem, especially in the nosocomial setting. Variation in the frequency of these resistant bacteria was monitored by several surveillance systems worldwide. These systems make use of a network of laboratory-generated antibiograms that were constructed on the basis of the cumulative antimicrobial susceptibility data from each hospital. Antibiograms were currently used to estimate the impact of changes in antibiotic usage and to determine infection control strategies and antibiotic usage policies. Furthermore, within the nosocomial setting, antibiograms were often taken into account to define a rational selection of the empirical antimicrobial therapy for treating patients with hospital-acquired infections. Clinical validation of the individual susceptibility reports, performed by a multidisciplinary team prior to data entering, seems to be a suitable strategy to get more reliable data to guide the rational selection of antimicrobial empirical therapy in patients with hospital-acquired infections.28
Carmeli et al., analysed relative risks for emergence of resistant
25 showed a particular propensity for the development of resistance. The emergence of resistance in P.aeruginosa also limits future therapeutic choices and is associated with increased rates of mortality and morbidity and higher costs. Knowledge about the relative risks of emergence of resistance with different antibiotics could be useful in helping to guide therapeutic choices. Result showed that out of 271 patients, resistance emerged in 28 patients. There were evident differences among antibiotics in the likelihood that their use would allow emergence of resistance in P.aeruginosa. Ceftazidime was associated with the lowest risk, and Imipenem had the highest risk.29
Lautenbach et al., illustrated risk factors for infection with Imipenem-resistant Pseudomonas aeruginosa and also determined the impact of Imipenem resistance on clinical and economic outcomes among patients infected with P. aeruginosa. Imipenem remains among the most reliable agents for treating P.
26
Melinda et al., assessed national rates of antimicrobial resistance among gram negative aerobic isolates recovered from ICU patients and compare these rates to antimicrobial use. Susceptibility data derived from national surveillance can be a barometer of emerging resistance problems. The results showed that high incidence of reduced antibiotic susceptibility among gram-negative bacteria. They also documented the increasing incidence of Ciprofloxacin resistance among gram-negative bacilli that has occurred coincident with increased use of fluoroquinolones. Fluoroquinolones that are not affected by currently circulating resistance mechanisms need to be developed to conserve this class of agents. In the meantime, ongoing surveillance and more judicious use of Fluoroquinolone antibiotics will be necessary to limit this downward trend in susceptibility.31
Gasink et al., evaluated risk factors for infection or colonization with Aztreonam-resistant Pseudomonas aeruginosa and examined the impact of this organism on mortality. They concluded that Aztreonam resistance in P. aeruginosa
was an important problem that has been largely ignored. Infection with an Aztreonam-resistant strain of P. aeruginosa did not appear to have a significant impact on mortality, the loss of effective therapeutic agents to treat P. aeruginosa was of great concern, and increases in the prevalence of Aztreonam-resistant P. aeruginosa further limit the available antipseudomonal armamentarium. Efforts should be made to preserve the utility of Aztreonam by curbing unwarranted use of Fluoroquinolones and agents active against anaerobes. Their study also provided additional evidence that restriction of Fluoroquinolone use was critically important in the fight against the emergence of antimicrobial resistance.32
27 In this study they found the hazard of death from the date of receipt of the antibiogram to day thirty was higher for both inadequate empirical therapy and adequate empirical monotherapy than for adequate empirical combination therapy. Compared to adequate definitive combination therapy, the risk of death at thirty days was also higher with inadequate definitive therapy but not with adequate definitive monotherapy. They concluded that clinicians who expect Pseudomonas aeruginosa bacteremia initiate empirical therapy with two antipseudomonal agents. In the case of confirmed
28
AIM AND OBJECTIVES
AIM
The primary aim of the study is to evaluate the resistance patterns of microorganisms to various antibiotics in Nosocomial infections undertaking a surveillance study by using antibiogram reports.
OBJECTIVES
To conduct a surveillance study on antibiotic resistance in patients with Nosocomial infections using antibiogram reports.
To determine the sensitivity patterns of microorganisms to the antibiotics prescribed during the study period.
To determine the resistance patterns of microorganisms to the antibiotics prescribed during the study period.
To monitor the extent of compliance of antibiotics prescribed with the results of antibiograms.
To understand the present prescribing patterns of antibiotics in
nosocomial infections in the hospital.
To aid in optimum drug therapy by promoting rational use of
29
PLAN OF STUDY
PHASES STEPS ACTIVITY TIME PERIOD
PHASE I
STEP I
Identification of target areas for possible study
July ’11
STEP II Literature survey July’11
STEP III Define criteria and
standards Aug ’11
STEP IV Designing of data
entry form Aug ’11
PHASE II STEP V
Collection of patient’s lists with antibiogram report
Sep ’11 - Jan ’12
PHASE III STEP VI
Collection of prospective data from patients
Sep ’11 - Jan ’12
30
METHODOLOGY
The study was conducted in Kovai Medical Center and Hospital; a modernized 657 bedded multidisciplinary advanced super specialty hospital at Coimbatore. It is one of the largest hospitals in Coimbatore which excels in diverse specialized fields like Nephrology, Neurology, Cardiology, Pulmonology, Orthopedics, Oncology, Dermatology, Gynecology, Endocrinology, Pediatrics, General medicine, General surgery, ENT, Dentistry, Gastroenterology and Physical medicine and rehabilitation.
Study Design:
The study was designed to determine the susceptibility of isolates of microorganisms to antibiotics. The details of the bacterial strains isolated from any specimens of patients suffering from nosocomial infections were collected and studied. The study is a Prospective observational study.
Study Site:
The study was conducted at the Department of Microbiology in Kovai Medical Center and Hospital, a super specialty hospital in Coimbatore.
Study Period:
The study was conducted over a period of seven months from July 2011 to January 2012.
Study Population:
31
Study Criteria:
Inclusion Criteria
Patients with positive cultures after 48 hours of hospitalization.
Patients for whom antibiotic sensitivity testing was performed.
Exclusion Criteria
Out patients
Patients receiving antibiotics without obtaining antibiogram report.
Patients who present with positive culture at the time of
hospitalization.
Study Protocol:
Topic Selection
32 Literature Review
An extensive literature survey was done on, antimicrobial usage, antimicrobial resistance, challenges of antimicrobial resistance, strategies to minimize the spread of antimicrobial resistance, importance of antibiogram surveillance method etc. The literatures supporting the study were gathered from various journals like Clinical Infectious Diseases, British medical journal, Journal of antimicrobial chemotherapy etc. The articles from the journals were mainly collected with the help of SCIENCE DIRECT, IOWA DRUG INFORMATION SYSTEMS (IDIS), MEDLINE and from other Internet sources. Informations were also gathered from documents published by WHO.
Development of patient data entry form
A well-designed data entry form was used for collecting data for this study. Data collected included patient details, antibiotics prescribed and other drugs prescribed. For every subject in this study patient name, inpatient number, date of admission, age, sex, ward of admission and length of stay in the hospital were recorded. Details of antibiotic therapy such as name of the antibiotics, dose, route of administration, frequency of administration and duration of therapy and antibiogram report were recorded.
Consent from Ethics Committee:
33 from the Chairman and approved by Ethics committee Kovai Medical Center and Hospital, Coimbatore on 17th September 2011.
Prospective Study
34
RESULTS AND DISCUSSION
The study was carried out at Kovai Medical Center and Hospital over a period of seven months from July 2011 to January 2012. A prospective observational study in which data pertaining to the time period between July 2011 to January 2012 were collected.
During the entire study period, a total of 69 patients antibiogram report were collected. Of these, 25 patients were identified as Nosocomial infections. The data of 25 patients were collected as part of the prospective study. The results of the study are as follows:
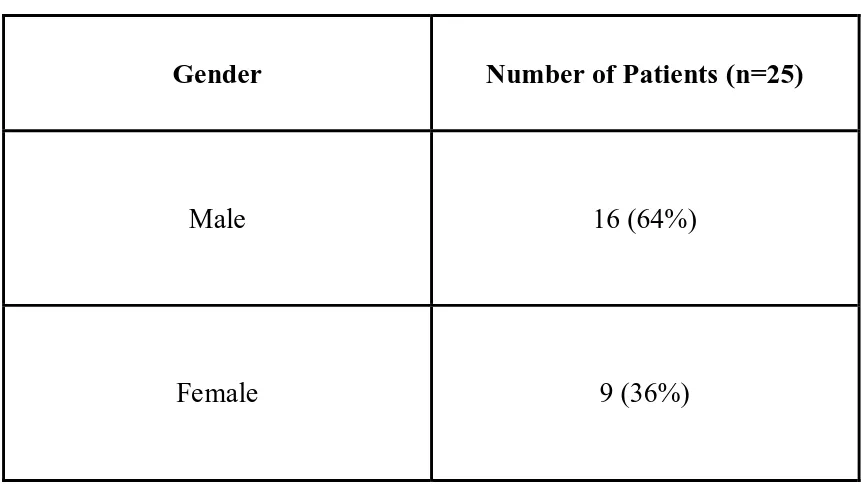
Evaluation of the demographic data of the subjects revealed that among the 25 patients included in this study, 64% (n=16) were male while 36% (n=9) were female. Nosocomial infections was more common among men than among women.34 This gender disparity in Nosocomial infections could be also due to patients those who were admitted in ICUs, mainly from road-traffic accidents and men were more prone to this. [Tab 1, Fig 1]
Age group analysis of the patients showed that, the most prominent age group were ‘61-70’ years and ’31-40’ years each comprising of 32% (n=8) and 20% (n=5) respectively. Our data showed that majority of Nosocomial infection cases were among patients over 60 years old. This might be due to decrease in the immunity in this age group.35 [Tab 2, Fig 2]
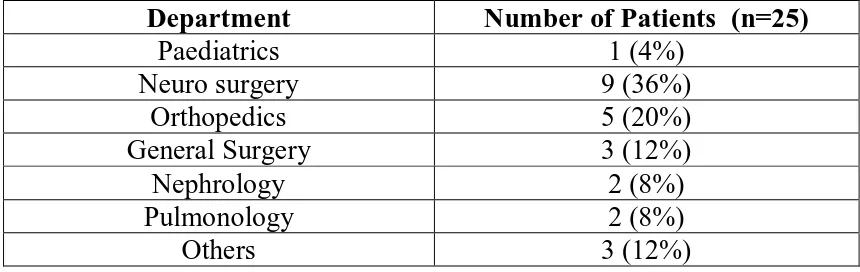
35 (n=9) followed by Orthopedics 20% (n=5). Among these departments, most of the patients were admitted in ICUs only, and those who were critically ill or immunocompromised requiring mechanical support and indwelling devices.35[Tab 3, Fig3]
Nosocomial infections contribute to extra hospital days and causing extra charges per hospitalization.36 Our study also showed that from a total of 25 cases, most of the patients 24% (n=6) were admitted for more than 30 days followed by 16% (n=4) were 6-10 days. So these longer hospital stay could be a major reason for the emergence of organisms resistant to the antibiotic therapy. [Tab 4, Fig 4]
The monitoring of the antibiotic therapy among the patients those who were admitted during the entire study period showed that most of the patients received one antibiotic as per their treatment schedule i.e 52% (n=13) followed by 40% (n=10) patients were on more than one antibiotics. The usage of multiple antibiotics in the hospital settings could thus be a major reason for the increase in antibiotic resistance. [Tab 5, Fig 5]
The most commonly prescribed antibiotics during the entire study period were Amoxicillin/ Clavulanic acid which was accounted by 21.88% prescriptions, followed by Cefoperazone/ Sulbactam (15.63%), Colistinmethate sodium (15.63%) and Amikacin (12.5%) etc. [Tab 6, Fig 6]
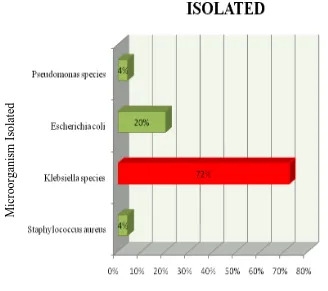
36 the microorganisms isolated from each specimen. This data indicated the prevalence of Klebsiella species and Escherichia coli to be the highest over all other organisms during the entire study period. Isolates of Klebsiella species were found to be 72% (n=18) of all specimens while Escherichia coli isolates were found to be 20% (n=5) specimens. Followed by Staphylococcus and Pseudomonas species accounted by 4% (n=1) each. [Tab 7, Fig 7]
The antibiotic therapy given to each individual was reviewed against the corresponding antibiogram report and the following observations were made. Of the 25 cases, 24% (n=6) of subjects the antibiotics given empirically were found to be sensitive to the microorganism according to the antibiogram. In 48% (n=12) of the patients, the antibiotics given empirically were changed according to the antibiogram report. In 28% (n=7) of the patients, the antibiogram reports did not translate into any changes in the choice of antibiotics given. These inadequate administration of antimicrobial treatment may contribute antimicrobial resistance which would be an important determinant of patient outcome.37[Tab 8, Fig 8]
Antibiotic susceptibility testing was done on these isolates to determine the susceptibility of the isolate to an array of antibiotics which would determine the extent of resistance or sensitivity of the organism to each antibiotic. The following antibiotics were included the study for susceptibility testing according to the antibiogram reports.
37 Of the 18 isolates of Klebsiella species, 100% (n=18) resistance were found in Amoxicillin/Clavulanic acid, Ceftriaxone, Cefotaxime, Cefepime, Ciprofloxacin, Ofloxacin, Levofloxacin, Moxifloxacin, Doxycycline while 94.12% (n=16) in Cefoperazone/Sulbactum, 93.75% (n=15) in Piperacillin/Tazobactum, 72.22% (n=13) in Amikacin, Ertapenem, Meropenem. Similarly 100% sensitivity were found in Colistinmethate sodium and Tigecycline followed by 33.33% (n=6) in Imipenem, followed by 27.78 (n=5) in Meropenem and Ertapenem each.[Tab 9, Fig 9: A-B]
A study by Anastasia et al. concluded that the existence and prolonged or inadequate use in the critically ill patients with multi drug resistant gram negative pathogens may lead to the emergence of colistimethate sodium resistance. The latter events urge for the development of new antimicrobials against multi resistant gram negative pathogens, the prudent use of colistimthate sodium and the strict implementation of hand hygene rules.40
All the 5 isolates of Escherichia coli, 100% (n=5) resistant to Amoxicillin/Clavulanic acid, Ceftriaxone, Cefotaxime, Ciprofloxacin, Ofloxacin, Levofloxacin, Moxifloxacin, Doxycycline, Vancomycin, Linezolid while 80% (n=4) resistant to Piperaciline/Tazobactum, Cefoperazone, Cefepime, Amikacin, Ertapenem and Meropenem, 60% (n=3) for Imipenem. At the same time 100% sensitivity were found in Colistinmethate sodium and Tigecycline followed by 40% (n=2) in Imipenem. [Tab 9, Fig 9: C-D]
38 A total of 25 patients, 4% (n=1) were identified as the isolates of
Staphylococcus aureus. Of these, 100% resistance was found in
Amoxicillin/Clavulanic acid, Piperacillin/Tazobactum, Cefoperazone/Sulbactum, Ceftriaxone, Cefotaxime and Cefepime. Similarly 100% of sensitivity was also found in Tigecycline, Doxycycline, Vancomycin. These observed results of Vancomycin also similar in the study carried out by Oteo et al.17 [Tab 9, Fig 9: E]
A total of 25 patients, 4% (n=1) were identified as the isolates of
Pseudomonas species. Among this 100% were found to be resistant to Amoxicillin/ Clavulanic acid, Piperacillin/Tazobactum, Cefoperazone, Ceftriaxone, Cefotaxime, Cefepime, Ciprofloxacine, Ofloxacin, Moxifloxacin and Doxycycline. At the same time 100% of sensitivity was also found in Colistinmethate sodium, Amikacin, Imipenem, Meropenem. The observed sensitivity to Imipenem is in contrast to the results given by Hanberger et al.27[Tab 9, Fig 9: F-G]
39
TABLE: 1
GENDER DISTRIBUTION
Gender
Number of Patients (n=25)
Male
16 (64%)
Female
9 (36%)
[image:59.595.99.530.122.364.2]40
TABLE: 2
AGE DISTRIBUTION
Age in Years
Number of Patients (n=25)
<1
1 (4%)
1-10
0 (0%)
11-20
0 (0%)
21-30
2 (8%)
31-40
5 (20%)
41-50
3 (12%)
51-60
2 (8%)
61-70
8 (32%)
71-80
3 (12%)
81-90
1 (4%)
[image:60.595.117.507.474.750.2]91-100
0 (0%)
41
TABLE: 3
DISTRIBUTION OF PATIENTS WITH DEPARTMENTS
Department
Number of Patients (n=25)
Paediatrics
1 (4%)
Neuro surgery
9 (36%)
Orthopedics
5 (20%)
General Surgery
3 (12%)
Nephrology
2 (8%)
Pulmonology
2 (8%)
[image:61.595.104.531.365.675.2]Others
3 (12%)
42
TABLE: 4
DURATION OF STAY IN HOSPITAL
Duration of Stay in Hospital
Number of Patients (n=25)
1-5
4 (16%)
6-10
4 (16%)
11-15
3 (12%)
16-20
3 (12%)
21-25
3 (12%)
26-30
2 (8%)
>31
6 (24%)
[image:62.595.108.518.335.641.2]43
TABLE: 5
NUMBER OF ANTIBIOTICS PRESCRIBED PER PATIENT
Number of Antibiotics
Number of Patients (n=25)
One
13 (52%)
Two
6 (24%)
Three
4 (16%)
Greater than Three
2 (8%)
[image:63.595.108.528.417.645.2]44
TABLE: 6
COMMONLY USED ANTIBIOTICS
Commonly Used Antibiotics
Number of Patients (n=25)
Amoxicillin/Clavulanic acid
7 (21.85%)
Cefoperazone/Sulbactum
5 (15.63%)
Amikacin
4 (12.5%)
Linezolid
2 (6.25%)
Moxifloxacin
2 (6.25%)
Tigecycline
1 (3.13%)
Colistimethate sodium
5 (15.63%)
Cefepime/Tazobactum
2 (6.25%)
Imipenem
2 (6.25%)
Piperacillin/Tazobactum
2 (6.25%)
[image:64.595.105.502.396.682.2]45
TABLE: 7
[image:65.595.90.418.414.705.2]DISTRIBUTION OF MICROORGANISM
Microorganism Isolated
Number of Patients (n=25)
Escherichia coli
5 (20%)
Klebsiella species
18 (72%)
Staphylococcus aureus
1 (4%)
Pseudomonas species
1 (4%)
FIGURE: 7
M
icr
oor
ga
nis
m
Is
olate
d
46
TABLE: 8
MODE OF TREATMENT BASED ON ANTIBIOGRAM REPORT
Mode of Treatment
Number of Patients (%) (n=25)
Patients Empirically Started on
Sensitive Antibiotics
6 (24%)
Antibiotics Changed According to
Antibiogram
12 (48%)
Antibiotics Not Changed According
[image:66.595.101.508.418.707.2]to Antibiogram
7 (28%)
FIGURE: 8
Mode of Treatment
N
um
be
r
of
P
at
ie
nt
s
(%
47
TABLE: 9
SENSITIVITY PATTERN OF INDIVIDUAL ANTIBIOTIC TO VARIOUS MICROORGANISMS
Antibiotics Klebsiella species (n=18) Escherichia coli (n=5) Staphylococcus aureus (n=1) Pseudomonas species (n=1)
S R S R S R S R
Colistimethate sodium 15 (100%) - 3 (100%) - - - 1 (100%) - Tigecycline 14 (100%) - 3 (100%) - 1 (100%) - - - Amoxicillin/ Clavulanic acid - 18 (100) - 5 (100%) - 1 (100%) - 1 (100%) Piperacillin/ Tazobactum 1 (6.25%) 15 (93.75%) 1 (20%) 4 (80%) - 1 (100%) - 1 (100%) Cefoprazone/ Sulbactum 1 (5.88%) 16 (94.12) 1 (20%) 4 (80%) - 1 (100%) - 1 (100%)
Ceftriaxone -
48 Antibiotics Klebsiella species (n=18) Escherichia coli (n=5) Staphylococcus aureus (n=1) Pseudomonas species (n=1)
S R S R S R S R
Cefotaxime -
18 (100%) - 5 (100%) - 1 (100%) - 1 (100%)
Cefepime -
18 (100%) 1 (20%) 4 (80%) - 1 (100%) - 1 (100%)
Ciprofloxacin -
18 (100%) - 5 (100%) - - - 1 (100%)
Ofloxacin -
18 (100%) - 5 (100%) - - - 1 (100%)
Levofloxacin -
18 (100%) - 5 (100%) - - - -
Moxifloxacin -
49 Antibiotics Klebsiella species (n=18) Escherichia coli (n=5) Staphylococcus aureus (n=1) Pseudomonas species (n=1)
S R S R S R S R
Amikacin 5 (27.78%) 13 (72.22%) 1 (20%) 4 (80%) - - 1 (100%) -
Doxycyclin -
18 (100%) - 5 (100%) 1 (100%) - - 1 (100%) Imipenem 6 (33.33%) 12 (66.67%) 2 (40%) 3 (60%) - - 1 (100%) - Ertapenem 5 (27.78%) 13 (72.22%) 1 (20%) 4 (80%) - - - - Meropenem 5 (27.78%) 13 (72.22%) 1 (20%) 4 (80%) - - 1 (100%) -
Vancomycin - - -
5 (100%)
1 (100%)
- - -
Linezolid - - -
5
(100%)
50
FIGURE: 9-A
FIGURE: 9-B
[image:70.595.105.542.128.765.2]51
FIGURE: 9-C
FIGURE: 9-D
[image:71.595.107.517.91.748.2]52
FIGURE: 9-E
FIGURE: 9-F
Antibiotics
[image:72.595.113.509.96.755.2] [image:72.595.119.505.357.686.2]53
FIGURE: 9-G
[image:73.595.103.511.156.456.2]54
SUMMARY AND CONCLUSION
A total of 25 in-patients, included in the study between July 2011 to January 2012 and for whom antibiotic sensitivity testing was performed against various microorganisms isolated from their specimens mainly urine and blood, were reviewed during the entire study period. Nosocomial was more common among men than among women in this study. A high percentage of patients aged between ‘61-70’ in this study population showed that patients over 60 years old are more prone to nosocomial infections.
The culture reports revealed that gram-negative organisms like Klebsiella species, eshcerichia coli, pseudomonas species were the predominant organisms causing HAI followed by staphylococcus aureus, a gram-positive organism. A total of 25 specimens containing 4 various microorganisms, underwent susceptibility testing against various antibiotics, among this 19 antimicrobials were included in this study.
Combination of β-lactam antibiotics with β-lactamase inhibitors are now very commonly used in the treatment of various infections. It is usual for the physicians to use these combinations as empirical therapy. Among this group, Piperacillin/ Tazobactum and Cefoperazone/ Sulbactum were showed higher sensitivity than Amoxicillin/ Clavulanic acid against various microorganisms in this study. The result also showed that Piperacillin/ Tazobactum and Cefperazone/Sulbactum had essential sensitivity towards Klebsiella species and
55 During the entire study, Polymyxin antibiotics showed sensitivity to all microorganisms. Cephalosporins showed low sensitivity towards gram negative microorganisms. But Flouroquinolones showed fully resistant patterns in
Klebsiella species,E.coli,S.aureus and Pseudomonas.
Amino glycoside (Amikacin) and Tetracyclin antibiotics are shown fairly good sensitivity towards all the gram-positive and gram-negative organisms involved in this study. Carbapenems like Imipenem and Ertapenem showed appreciable activity against gram-negative organisms in the entire study. Glycopeptide antibiotics such as Vancomycin and Teicoplanin showed appreciable sensitivity towards gram-positive organisms. However, since the sample size was inadequate, so the result could not be consider as accurate.
Furthermore, our data suggest that the most effective antimicrobials remain for gram-positive organism such as Staphylococcus aureus in this study is Doxycyclin followed by Vancomycin and for gram-negative species such as
Klebsiella species, Escherichia coli, Pseudomonas aeruginosa is Carbapenams followed by Piperacillin/Tazobactum.
56 knowledge of the most likely causative organisms and their expected resistance patterns can increase the probability of selecting an effectiv