R E S E A R C H A R T I C L E
Open Access
An update of stabilisation exercises for low back
pain: a systematic review with meta-analysis
Benjamin E Smith
1*, Chris Littlewood
2and Stephen May
3Abstract
Background:
Non-specific low back pain (NSLBP) is a large and costly problem. It has a lifetime prevalence of 80%
and results in high levels of healthcare cost. It is a major cause for long term sickness amongst the workforce and is
associated with high levels of fear avoidance and kinesiophobia. Stabilisation (or
‘
core stability
’
) exercises have been
suggested to reduce symptoms of pain and disability and form an effective treatment. Despite it being the most
commonly used form of physiotherapy treatment within the UK there is a lack of positive evidence to support its
use. The aims of this systematic review update is to investigate the effectiveness of stabilisation exercises for the
treatment of NSLBP, and compare any effectiveness to other forms of exercise.
Methods:
A systematic review published in 2008 was updated with a search of PubMed, CINAHL, AMED, Pedro and
The Cochrane Library, October 2006 to October 2013. Two authors independently selected studies, and two authors
independently extracted the data. Methodological quality was evaluated using the PEDro scale. Meta-analysis was
carried out when appropriate.
Results:
29 studies were included: 22 studies (
n
= 2,258) provided post treatment effect on pain and 24 studies
(
n
= 2,359) provided post treatment effect on disability. Pain and disability scores were transformed to a 0 to 100
scale. Meta-analysis showed significant benefit for stabilisation exercises versus any alternative treatment or control
for long term pain and disability with mean difference of -6.39 (95% CI -10.14 to -2.65) and -3.92 (95% CI -7.25
to -0.59) respectively. The difference between groups was clinically insignificant. When compared with alternative
forms of exercise, there was no statistical or clinically significant difference. Mean difference for pain was -3.06
(95% CI -6.74 to 0.63) and disability -1.89 (95% CI -5.10 to 1.33).
Conclusion:
There is strong evidence stabilisation exercises are not more effective than any other form of active
exercise in the long term. The low levels of heterogeneity and large number of high methodological quality of
available studies, at long term follow-up, strengthen our current findings, and further research is unlikely to
considerably alter this conclusion.
Keywords:
Systematic review, Meta-analysis, Low back pain, Exercise therapy, Core stability, Stabilisation,
Treatment, Effectiveness
Background
Non-specific low back pain (LBP) can be described as
low back pain without underlying cause or disease, and
has a lifetime prevalence of 80% [1,2]. Point prevalence
ranges from 12% to 33%, with 90% of acute episodes
re-covering within six weeks [1,3]. However, 62% of people
experiencing their first episode of LBP will develop
chronic symptoms lasting longer than one year, with
16% of people still sick listed from work at 6 months [4].
The UK health service spends more than £1 billion on
related costs, including hospital and GP appointments
and physiotherapy treatments, with similar high costs
seen in other developed countries [5,6]. LBP is a major
cause for long term sickness amongst the workforce, and
has been estimated to cost UK employers as much as
£624 million per year, with 119 million works days lost
each year [7,8].
In the UK patients with LBP are routinely referred to
physiotherapy [6]. Treatment can involve a number of
* Correspondence:benjamin.smith3@nhs.net1
Physiotherapy Outpatients, London Road Community Hospital, Derby Hospitals NHS Foundation Trust, London Road, Derby DE1 2QY, UK Full list of author information is available at the end of the article
© 2014 Smith et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
different techniques ranging from spinal manipulations,
mobilisation, advice, general exercises and specifically
tailored exercises [9]. It has been claimed that there is a
link between dysfunction within the activation and timing
of local spinal stabilisation muscles and back pain [10-12].
Consequently a therapeutic exercise regime aimed at these
muscles was developed, designed to
‘retrain’
motor skills
and the activation dysfunction [12]. Despite doubts raised
about this link between back pain and muscle activation,
and the effectiveness of such an exercise regime (known as
stabilisation or
‘
core stability’
exercises) it has grown in
popularity and now ranks the most common form of
physiotherapy treatment in the UK for back pain [9,13-15].
[image:2.595.304.541.639.733.2]A 2008 systematic review by May and Johnson, which
included 18 trials up to 2006, concluded that specific
sta-bilisation exercises may be beneficial over no treatment,
but went on to report that it was unlikely to produce an
outcome better than any other form of exercise [13]. It
has been suggested that median duration of survival time
of a systematic review is 5.5 years, with 23% of systematic
reviews being out of date within two years of publication
[16]. Since 2006 there has been considerable growth in the
evidence base, with a large number of new trials being
published. In total there have been seven systematic
re-views that have looked at stabilisation exercises [13,17-22],
with the previous three performing a meta-analysis
[17,21,22]. Macedo et al [17] included studies published
up to June 2008 and concluded that stabilisation exercises
were no better than general exercise. In 2012 Wang et al
[21] carried out a systematic review and also concluded
there was no significant difference between
‘core stability’
and general exercises [21]. However, Wang et al’s narrow
definition of
‘
core stability’
exercises was
“exercises
per-formed on unstable surfaces”, rather than a broader
defin-ition based upon specific muscle activation. Furthermore,
they only included randomised controlled trials (RCT)
that specifically compared intervention versus general
exercise, rather than any other alternative treatment, and
only included people suffering back pain for more than
three months. Consequently only five articles fulfilled their
inclusion criteria [21]. Our systematic review uses a more
broader definition and comparison, similar to May and
Johnson [13], and found 19 further articles to add to the
original 18 [13]. In contract to these results more recently
Byström et al [22] reported that stabilisation exercises
were more favourable than general exercises. They
searched the literature up to October 2011, but did not
limit their participants to non specific back pain and had
far stricter inclusion criteria. Our review included a further
15 articles to Byström et al thus providing the justification
for a more up to date review.
This systemic review and meta-analysis was conducted
to update the 2008 data by May and Johnson [13]. The
primary aim of this analysis is to systematically review
the most current up to date literature to determine
whether stabilisation (or
‘core stability’) exercises are an
effective therapeutic treatment compared to an alternative
treatment for people with non-specific low back pain. The
secondary aim is to determine if stabilisation exercises are
as effective as other forms of exercise, and to evaluate
findings by meta-analysis if appropriate. This systematic
review update followed the recommendations of the
PRISMA statement [23].
Methods
Search strategy
An electronic database search of title and abstract was
conducted October 2006 to October 2013 on the
follow-ing databases: (1) PubMed, (2) the Cumulative Index to
Nursing and Allied Health Literature (CINAHL), (3) The
Allied and Complimentary Medicine Database (AMED),
(4) Physiotherapy Evidence Database (Pedro), (5) The
Cochrane Library. Specific search strategies depended
on the particular database being searched. For the
keywords and the PubMed search strategy used see
Table 1. Hand searches of the reference list of included
articles were also performed.
Study selection
For inclusion the studies had to meet the following
criteria.
Participants
Adults recruited from the general population with
non-specific low back pain of any length of time. Low back
pain defined as, but not restrictive to, pain and/or stiffness
between the lower rib and buttock crease with or without
leg pain. Studies with specific pathology, such as systemic
inflammatory diseases, prolapsed disc, spondylolisthesis,
pregnancy related, fractures, tumours, infections or
osteo-porosis were excluded.
Interventions
Primary intervention arm of stabilisation, or
‘core
stabil-ity’, exercises defined as: facilitation of deep muscles of
the spine (primarily transversus abdominis or multifidus)
at low level, integrated into exercise, progressing into
functional activity, according to Richardson et al [12],
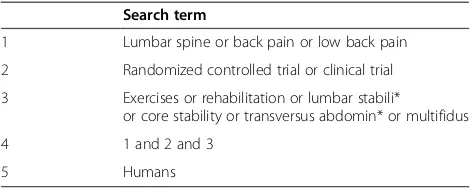
Table 1 PubMed search strategy
Search term
1 Lumbar spine or back pain or low back pain
2 Randomized controlled trial or clinical trial
3 Exercises or rehabilitation or lumbar stabili*
or core stability or transversus abdomin* or multifidus
4 1 and 2 and 3
5 Humans
Norris et al [24] or O’Sullivan et al [25]. Comparison
group of any other intervention, placebo or control were
considered appropriate.
Outcomes
Included studies were required to report an outcome
measure of pain and/or functional disability.
Study design
Studies had to be full randomised controlled trials
(RCTs), published in English, in a peer reviewed journal.
Studies that were not randomised or quasi-random were
excluded.
Study selection
One reviewer (BS) conducted the electronic database
searches and screened the title and abstracts. Full copies
of potential eligible paper were retrieved and
independ-ently screened by two reviewers (BS and CL). Initial
per-centage agreement was 68%, and using Cohen
’
s statistic
method kappa agreement was
k
= 0.29, which is
consid-ered poor to fair agreement [26-28]. Disagreements were
resolved by consensus without the need for a third
reviewer (SM), who was available. Initial disagreements
were due to; intervention criteria [29-33], study
popula-tion [34,35], study design [36-39] and duplicapopula-tion of
results from another publication being missed [40,41].
Our review excluded participants with specific pathology,
so all three reviewers (BS, CL and SM) verified any
exclu-sion of studies from the 2008 review [13].
Data extraction
We extracted the following data from the included articles:
study design, participant information, interventions and
setting, follow-up period and outcome data [42]. These
data were then compiled into a standard table by one
reviewer (BS) and then independently checked and verified
by a second reviewer (SM). Disagreements were resolved
through consensus. A third reviewer (CL) was available in
the event of an agreement not being reached, but was not
required. Of the included articles three had inconsistencies
within their text, figures or tables with regards to their
re-sults [33,43,44]. All were contacted by e-mail, and all gave
clarification. One study published median outcome scores,
and the authors were contacted and provided mean
out-come data [45]. Effectiveness was judged for short term
(≤3 months from randomisation), medium term (>3 and
<12 months) and long term (≥12 months), as
recom-mended by the 2009 Updated Method Guidelines for
Sys-tematic Reviews in the Cochrane Back Review Group and
in keeping with the original 2008 systematic review [13,46].
Data from the 2008 review was taken directly from the
published review [13].
Quality assessment
Studies meeting the inclusion criteria were assessed for
methodological quality and risk of bias using the PEDro
scale [47]. The 11 item PEDro scale was developed by
Verhagen et al using the Delphi consensus technique to
develop a list of criteria thought by experts in the field
to measure methodological quality [48]. The PEDro scale
consists of the following items: (1) Was eligibility criteria
specified? (2) Were all subjects randomly allocated? (3)
Were allocations concealed? (4) Were the groups similar
at baseline? (5) Was there blinding of all subjects? (6)
Was there blinding of all therapists? (7) Was there
blinding of all assessors? (8) Was there measures of at
least one key outcome for more than 85% of the subjects
initially allocated to groups? (9) Did all subjects for
whom outcome measures were available receive the
treatment or control condition as allocated or, where
this was not the case, data for at least one key outcome
was analysed by
“intention to treat”? (10) Were the
re-sults of between group statistical comparisons reported
for at least one key outcome? (11) Did the study have
both point measures and measures of variability for at
least one key outcome? [47]. Items 2
–
9 refer to the
internal validity of a paper, and items 10 and 11 refer to
the statistical analysis, ensuring sufficient data to enable
appropriate interpretation of the results. Item 1 is
re-lated to the external validity and therefore not included
in the total PEDro score [49].
All included articles were already scored within the
PEDro database, and these data were extracted from the
PEDro website [50]. Based upon the original 2008 paper
and precedent within the literature, studies scoring
≥6
out of 10 were considered to be high quality [13,51].
Statistical analysis
Pain and disability mean scores, along with their measure
of range (standard deviation/95% confidence interval)
were transformed to a score ranging from 0 to 100 [52].
All data analyses were performed using the
OpenMetaA-nalyst software [53]. Statistical between study
heterogen-eity was assessed with the
I
2statistic, and this review
considered 25% low, 50% moderate and 75% high [54]. If
trials were considered sufficiently homogenous then
out-come data was pooled according to outout-come (pain or
dis-ability), methodological quality (PEDro scores <6, or
≥6)
and follow-up period. Due to the inherent heterogeneity
in low back pain within the literature, the DerSimonian
and Laird random effects model was used [55].
Sensitivity analysis
The robustness of our results was tested through a
sensi-tivity analysis. We assessed the impact of using solely high
quality studies with using studies of low, medium and high
quality combined.
Smithet al. BMC Musculoskeletal Disorders2014,15:416 Page 3 of 21
Results
Study identification
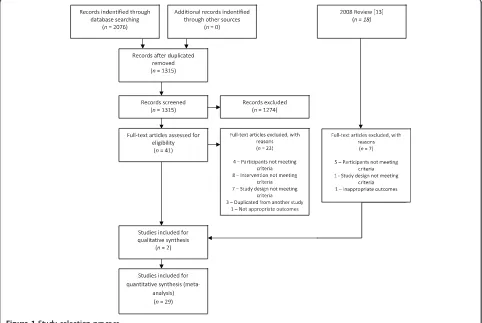
The initial database search produced 2,076 citations, of
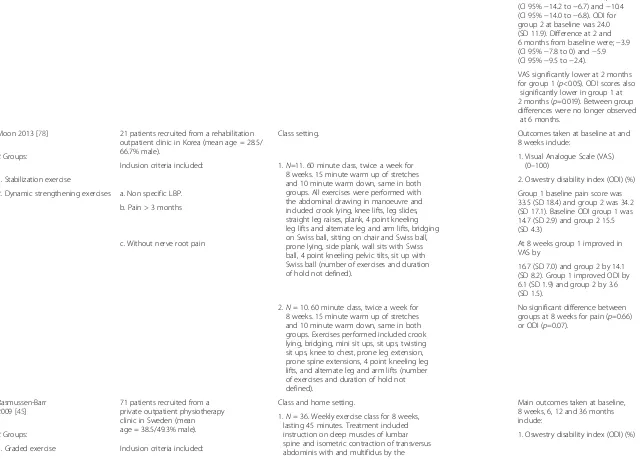
which 41 were appropriate for full text review, see
Figure 1 for study selection process.
After full text review 23 articles were excluded. Reasons
being: participants not meeting criteria [34,35,56,57],
intervention not meeting criteria [29,31,32,58-61], study
design not meeting criteria [36-39,62-64], duplications of
results from other included studies [40,41,65] and no
appropriate outcome measures [66]. That left a total 18
studies for inclusion [33,43-45,67-80]. Of the 18, two were
separate publications of different treatment groups of the
same larger study [71,72]. Of note is that Franca et al [71]
did not perform an intention to treat analysis, and so has
a lower PEDro score than Franca at al [72]. However, as
both had a PEDro score
≥
6 this does not affect the
pool-ing of both comparisons within the data synthesis.
There-fore, a total of 17 separate trials were included.
From the 18 included studies from the 2008 review,
seven were rejected for this review, five due to this
re-view only including patients with non specific back pain
[25,81-84], one because it was a pilot study [85] and one
due to inappropriate outcomes [86]. That resulted in 12
studies being drawn from the 2008 review (one from
two publications) [87-99], with 29 studies in total
in-cluded for this updated review.
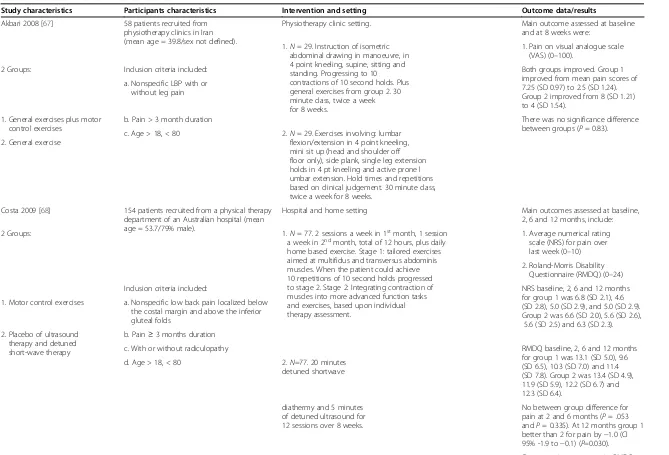
Characteristics of included studies
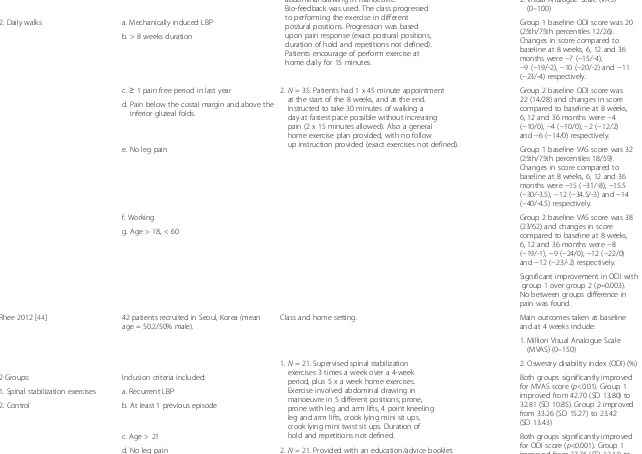
A summary of the characteristics of the included studies
along with the main results is shown in Table 2. There
were heterogeneous populations within the studies, with
regard to duration of symptoms and presence of leg
symptoms. Ten of the studies specified participants having
back pain lasting more than three months [43,67,69,
71-73,76-78], with two studies specifying pain lasting three
or more months [68,70], two specifying more than two
months [33,45], one specified any length of time [75], and
two studies did not detail their criteria [44,74]. Four
stud-ies included participants with or without leg pain [67-70],
eight excluded participants with leg pain [33,44,45,
71-73,77,78] and six were not clear on their inclusion
criteria with regards to leg pain [43,74-76,79,80].
[image:4.595.57.539.400.723.2]Stabilisation exercises were the sole intervention for
the majority of the studies, with five being individually
treated [68,70-72,75,79] and nine being in a class
set-ting [33,44,45,64,73,76-78,80]. Three studies combined
stabilisation exercises with other forms of treatment,
such as general exercises [43,67], and electrotherapy
treatment [74].
Figure 1Study selection process.
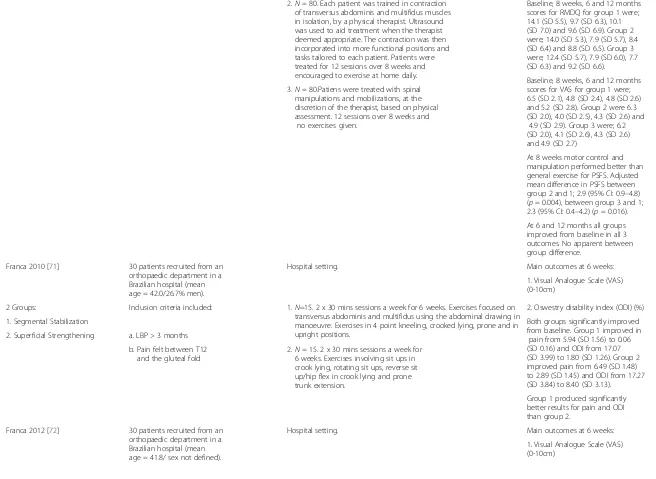
Table 2 Characteristics of included studies
Study characteristics Participants characteristics Intervention and setting Outcome data/results
Akbari 2008 [67] 58 patients recruited from physiotherapy clinics in Iran (mean age = 39.8/sex not defined).
Physiotherapy clinic setting. Main outcome assessed at baseline and at 8 weeks were:
1.N= 29. Instruction of isometric abdominal drawing in manoeuvre, in 4 point kneeling, supine, sitting and standing. Progressing to 10 contractions of 10 second holds. Plus general exercises from group 2. 30 minute class, twice a week for 8 weeks.
1. Pain on visual analogue scale (VAS) (0–100).
2 Groups: Both groups improved. Group 1
improved from mean pain scores of 7.25 (SD 0.97) to 2.5 (SD 1.24). Group 2 improved from 8 (SD 1.21) to 4 (SD 1.54).
Inclusion criteria included:
a. Nonspecific LBP with or without leg pain
1. General exercises plus motor control exercises
b. Pain > 3 month duration There was no significance difference
between groups (P= 0.83). c. Age > 18, < 80 2.N= 29. Exercises involving: lumbar
flexion/extension in 4 point kneeling, mini sit up (head and shoulder off floor only), side plank, single leg extension holds in 4 pt kneeling and active prone l umbar extension. Hold times and repetitions based on clinical judgement. 30 minute class, twice a week for 8 weeks.
2. General exercise
Costa 2009 [68] 154 patients recruited from a physical therapy department of an Australian hospital (mean age = 53.7/79% male).
Hospital and home setting Main outcomes assessed at baseline, 2, 6 and 12 months, include:
1. Average numerical rating scale (NRS) for pain over last week (0–10)
2 Groups: 1.N= 77. 2 sessions a week in 1stmonth, 1 session
a week in 2ndmonth, total of 12 hours, plus daily home based exercise. Stage 1: tailored exercises aimed at multifidus and transversus abdominis muscles. When the patient could achieve 10 repetitions of 10 second holds progressed to stage 2. Stage 2: Integrating contraction of muscles into more advanced function tasks and exercises, based upon individual therapy assessment.
2. Roland-Morris Disability Questionnaire (RMDQ) (0–24)
Inclusion criteria included: NRS baseline, 2, 6 and 12 months
for group 1 was 6.8 (SD 2.1), 4.6 (SD 2.8), 5.0 (SD 2.9), and 5.0 (SD 2.9). Group 2 was 6.6 (SD 2.0), 5.6 (SD 2.6),
5.6 (SD 2.5) and 6.3 (SD 2.3). a. Nonspecific low back pain localized below
the costal margin and above the inferior gluteal folds
1. Motor control exercises
2. Placebo of ultrasound therapy and detuned short-wave therapy
b. Pain≥3 months duration
c. With or without radiculopathy RMDQ baseline, 2, 6 and 12 months
for group 1 was 13.1 (SD 5.0), 9.6 (SD 6.5), 10.3 (SD 7.0) and 11.4 (SD 7.8). Group 2 was 13.4 (SD 4.9), 11.9 (SD 5.9), 12.2 (SD 6.7) and 12.3 (SD 6.4).
d. Age > 18, < 80 2.N=77. 20 minutes detuned shortwave
diathermy and 5 minutes of detuned ultrasound for 12 sessions over 8 weeks.
No between group difference for pain at 2 and 6 months (P= .053 andP= 0.335). At 12 months group 1 better than 2 for pain by−1.0 (CI 95% -1.9 to−0.1) (P=0.030). Short term improvement in RMDQ at 2 and 6 months for group 1
Smith
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
5
o
f
2
1
http://ww
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
compared to 2, (P= 0.003 and
P= 0.014). But no difference at 12 months (P= 0.271). Critchley 2007 [69] 212 patients recruited from primary or
secondary care in a UK hospital (mean age = 44.3/36% male).
Hospital and home setting. Main outcomes at 6, 12 and
18 months include:
1. Roland-Morris Disability Questionnaire (RMDQ) (0–24)
3 Groups: Inclusion criteria included: 1.N=71. Assessed and treated according to assessment findings. Treatments include combinations of joint mobilizations, manipulations, massage and exercise. Exercises included specific trunk muscle retraining, stretches, and general spinal mobility. Up to 12 sessions of around 30 minutes.
2. Pain on numerical analogue scale (0–100)
1. Usual physiotherapy At 18 months RMDQ score improved
from 11.1 (95% CI 9.6–12.6) to 6.9 (95% CI 5.3–8.4) with group 1, 12.8 (95% CI 11.4-14.2) to 6.8
(95% CI 4.9–8.6) with group 2, and 11.5 (95% CI 9.8–13.1) to 6.5 (95% CI 4.5–8.6) for group 2. 2. Spinal stabilization classes a. Low back pain of more than 12 weeks
duration
3. Pain management classes b. With or without leg pain
c. Age > 18
2.N= 72. Tailored to assessment findings and progressed within participants’ability, working on transversus abdominis and lumbar multifidus muscle training followed by group exercises that challenged spinal stability. Maximum of 8 sessions of 90 minutes supervised exercise.
At 18 months pain improved from 60 (95% CI 54–66) to 39 (95% CI 31–46) for group 1, 67 (95% CI 61–73) to 32 (95% CI 24–40) for group 2 and 59 (95% CI 52–65) to 38 (95% CI 29–47) for group 3.
3.N= 69. A combination of structured back pain education with group general strengthening, stretching, and light aerobic exercises. A maximum of 8 sessions of 90 minutes.
No between group differences were found for RMDQ (P=0.46) or pain.
Ferreira 2007 [70] 240 patients recruited from a physical therapy department from hospitals in Australia (mean age = 53.6/31% male).
Hospital and home setting. Outcomes at 8 weeks, 6 and
12 months, include:
1. Patient-Specific Functional Scale (PSFS) (3–30)
3 Groups: Inclusion criteria included: 1.N= 80. Modelled on the‘Back to Fitness’program by Klaber
2. Roland-Morris Disability Questionnaire (RMDQ) (0–24)
1. General exercise Moffet and Frost. 1 hour exercise group,
12 sessions over 8 weeks. Starts with 1 minute warm up followed by stretches and 10 exercises performed for 1 min each. Intensity dictated by patients’response to exercise. Exercises include: walking/running on spot, sideways trunk curls, side steps/star jumps, press ups, side lying leg raises, prone leg raises, trunk curls, sit to stand, arm circling in 90° of abduction and bridging. Participants also encouraged to exercise at home at least once a day.
3. Average VAS (0–10) for pain over last week
2. Motor control exercise
a. Nonspecific low back pain with or without leg pain
Baseline, 8 weeks, 6 and 12 months scores for PSFS for group 1 were; 10.1 (SD 4.2), 14.4 (SD 6.6), 15.0 (SD 7.4) and 13.9 (SD 7.2). Group 2 were; 10.7 (SD 4.0), 17.7 (SD 6.2), 16.4 (SD 6.6) and 15.7). Group 3 were; 11.2 (SD 4.6), 17.5 (SD 6.8), 17.3 (SD 7.0) and 15.2 (SD 6.8). 3. Spinal manipulation b. Pain≥3 months duration
c. Age > 18, < 80
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
6
o
f
2
1
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
2.N= 80. Each patient was trained in contraction of transversus abdominis and multifidus muscles in isolation, by a physical therapist. Ultrasound was used to aid treatment when the therapist deemed appropriate. The contraction was then incorporated into more functional positions and tasks tailored to each patient. Patients were treated for 12 sessions over 8 weeks and encouraged to exercise at home daily.
Baseline, 8 weeks, 6 and 12 months scores for RMDQ for group 1 were; 14.1 (SD 5.5), 9.7 (SD 6.3), 10.1 (SD 7.0) and 9.6 (SD 6.9). Group 2 were; 14.0 (SD 5.3), 7.9 (SD 5.7), 8.4 (SD 6.4) and 8.8 (SD 6.5). Group 3 were; 12.4 (SD 5.7), 7.9 (SD 6.0), 7.7 (SD 6.3) and 9.2 (SD 6.6).
Baseline, 8 weeks, 6 and 12 months scores for VAS for group 1 were; 6.5 (SD 2.1), 4.8 (SD 2.4), 4.8 (SD 2.6) and 5.2 (SD 2.8). Group 2 were 6.3 (SD 2.0), 4.0 (SD 2.5), 4.3 (SD 2.6) and
4.9 (SD 2.9). Group 3 were; 6.2 (SD 2.0), 4.1 (SD 2.6), 4.3 (SD 2.6) and 4.9 (SD 2.7)
3.N= 80.Patiens were treated with spinal manipulations and mobilizations, at the discretion of the therapist, based on physical assessment. 12 sessions over 8 weeks and
no exercises given.
At 8 weeks motor control and manipulation performed better than general exercise for PSFS. Adjusted mean difference in PSFS between group 2 and 1; 2.9 (95% CI: 0.9–4.8) (p= 0.004), between group 3 and 1; 2.3 (95% CI: 0.4–4.2) (p= 0.016). At 6 and 12 months all groups improved from baseline in all 3 outcomes. No apparent between group difference.
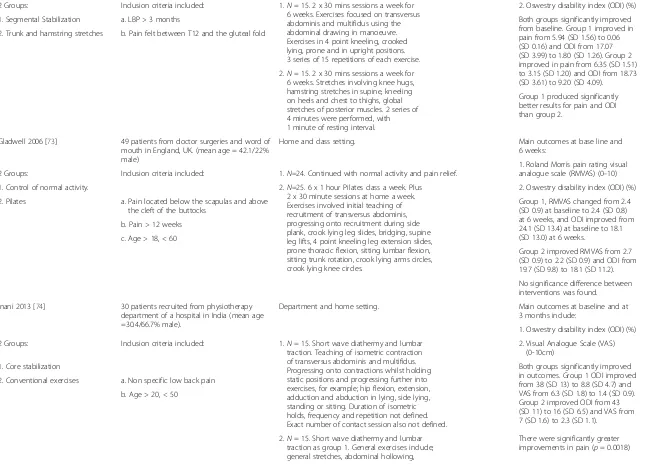
Franca 2010 [71] 30 patients recruited from an orthopaedic department in a Brazilian hospital (mean age = 42.0/26.7% men).
Hospital setting. Main outcomes at 6 weeks:
1. Visual Analogue Scale (VAS) (0-10cm)
2 Groups: Inclusion criteria included: 1.N=15. 2 x 30 mins sessions a week for 6 weeks. Exercises focused on transversus abdominis and multifidus using the abdominal drawing in manoeuvre. Exercises in 4 point kneeling, crooked lying, prone and in upright positions.
2. Oswestry disability index (ODI) (%)
1. Segmental Stabilization Both groups significantly improved
from baseline. Group 1 improved in pain from 5.94 (SD 1.56) to 0.06 (SD 0.16) and ODI from 17.07 (SD 3.99) to 1.80 (SD 1.26). Group 2 improved pain from 6.49 (SD 1.48) to 2.89 (SD 1.45) and ODI from 17.27 (SD 3.84) to 8.40 (SD 3.13).
2. Superficial Strengthening a. LBP > 3 months
b. Pain felt between T12 and the gluteal fold
2.N= 15. 2 x 30 mins sessions a week for 6 weeks. Exercises involving sit ups in crook lying, rotating sit ups, reverse sit up/hip flex in crook lying and prone trunk extension.
Group 1 produced significantly better results for pain and ODI than group 2.
Franca 2012 [72] 30 patients recruited from an orthopaedic department in a Brazilian hospital (mean age = 41.8/ sex not defined).
Hospital setting. Main outcomes at 6 weeks:
1. Visual Analogue Scale (VAS) (0-10cm)
Smith
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
7
o
f
2
1
http://ww
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
2 Groups: Inclusion criteria included: 1.N= 15. 2 x 30 mins sessions a week for 6 weeks. Exercises focused on transversus abdominis and multifidus using the abdominal drawing in manoeuvre. Exercises in 4 point kneeling, crooked lying, prone and in upright positions. 3 series of 15 repetitions of each exercise.
2. Oswestry disability index (ODI) (%)
1. Segmental Stabilization Both groups significantly improved
from baseline. Group 1 improved in pain from 5.94 (SD 1.56) to 0.06 (SD 0.16) and ODI from 17.07 (SD 3.99) to 1.80 (SD 1.26). Group 2 improved in pain from 6.35 (SD 1.51) to 3.15 (SD 1.20) and ODI from 18.73 (SD 3.61) to 9.20 (SD 4.09).
a. LBP > 3 months
2. Trunk and hamstring stretches b. Pain felt between T12 and the gluteal fold
2.N= 15. 2 x 30 mins sessions a week for 6 weeks. Stretches involving knee hugs, hamstring stretches in supine, kneeling on heels and chest to thighs, global stretches of posterior muscles. 2 series of 4 minutes were performed, with 1 minute of resting interval.
Group 1 produced significantly better results for pain and ODI than group 2.
Gladwell 2006 [73] 49 patients from doctor surgeries and word of mouth in England, UK. (mean age = 42.1/22% male)
Home and class setting. Main outcomes at base line and
6 weeks:
1. Roland Morris pain rating visual analogue scale (RMVAS) (0–10) 2 Groups: Inclusion criteria included: 1.N=24. Continued with normal activity and pain relief.
1. Control of normal activity. 2.N=25. 6 x 1 hour Pilates class a week. Plus 2 x 30 minute sessions at home a week. Exercises involved initial teaching of recruitment of transversus abdominis, progressing onto recruitment during side plank, crook lying leg slides, bridging, supine leg lifts, 4 point kneeling leg extension slides, prone thoracic flexion, sitting lumbar flexion, sitting trunk rotation, crook lying arms circles, crook lying knee circles.
2. Oswestry disability index (ODI) (%)
2. Pilates a. Pain located below the scapulas and above the cleft of the buttocks
Group 1, RMVAS changed from 2.4 (SD 0.9) at baseline to 2.4 (SD 0.8) at 6 weeks, and ODI improved from 24.1 (SD 13.4) at baseline to 18.1 (SD 13.0) at 6 weeks.
b. Pain > 12 weeks
c. Age > 18, < 60
Group 2 improved RMVAS from 2.7 (SD 0.9) to 2.2 (SD 0.9) and ODI from 19.7 (SD 9.8) to 18.1 (SD 11.2).
No significance difference between interventions was found.
Inani 2013 [74] 30 patients recruited from physiotherapy department of a hospital in India (mean age =30.4/66.7% male).
Department and home setting. Main outcomes at baseline and at 3 months include:
1. Oswestry disability index (ODI) (%)
2 Groups: Inclusion criteria included: 1.N= 15. Short wave diathermy and lumbar traction. Teaching of isometric contraction of transversus abdominis and multifidus. Progressing onto contractions whilst holding static positions and progressing further into exercises, for example; hip flexion, extension, adduction and abduction in lying, side lying, standing or sitting. Duration of isometric holds, frequency and repetition not defined. Exact number of contact session also not defined.
2. Visual Analogue Scale (VAS) (0-10cm)
1. Core stabilization Both groups significantly improved
in outcomes. Group 1 ODI improved from 38 (SD 13) to 8.8 (SD 4.7) and VAS from 6.3 (SD 1.8) to 1.4 (SD 0.9). Group 2 improved ODI from 43 (SD 11) to 16 (SD 6.5) and VAS from 7 (SD 1.6) to 2.3 (SD 1.1).
2. Conventional exercises a. Non specific low back pain
b. Age > 20, < 50
2.N= 15. Short wave diathermy and lumbar traction as group 1. General exercises include; general stretches, abdominal hollowing,
There were significantly greater improvements in pain (p= 0.0018)
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
8
o
f
2
1
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
isometric lumbar extension, bridges, graded flexion and extension exercises. Duration of holds, frequency and repetition not defined. Exact number of contact session also not defined.
and disability (p= 0.0309) for group 1 over 2
Javadian 2012 [43] 30 patients recruited in Iran, location not defined (age and sex not defined)
Class setting. Main outcomes at baseline and
at 3 months include:
2 Groups: Inclusion criteria included: 1. N = 15. 15 minute warm up of cycling and general stretches of hip musculature, hamstring and calf. Stabilization exercises included isometric
contraction of deep muscles of the lumbar spine in supine, bridging, kneeling, sitting and standing. Progressed onto Swiss ball and wobble board. Duration of isometric holds, frequency and repetition not defined. Routine exercises included single and double knee to chest, bridging, lower limb raises, supine cycling, heel slides, leg slides and crunches. Repetitions not defined.
1. Visual Analogue Scale (VAS) (0-100mm)
1. Stabilization exercises plus routine exercises
2. Oswestry disability index (ODI) (%)
a. LBP > 3 months Both groups
significantly improved
in outcomes. Group 1 improved in VAS from 45.06 (SD 4.15) to 18.41 (SD 2.15) and ODI from 43.84 (SD 5.55) to 16.83 (3.45). Group 2 improved in VAS from 47.73 (SD 3.82) to 9.58 (SD 1.56) and ODI from 45.80 (SD 6.64) to 5.16 (SD 2.16). 2. Routine exercises b. Age > 18, < 45
c. At
least 1 positive from the following:
1. Painful arc during flexion and return from flexion
2. Gower’s sign
3. Instability Catch The control group improved more
than the intervention group, but not significantly.
d. Negative straight leg raise 2. N = 15. 15 minutes warm up as group 1, and routine exercises as group 1. c. Positive prone instability test
Total number of classes over the 3 months not defined.
Kumar 2010 [75] 141 patients recruited from a rehabilitation department of an India hospital (mean age = 35.1/64.5% male)
Rehabilitation department setting. Main outcomes at baseline and 6 months.
1. Visual Analogue Scale (VAS) (0-10cm)
1.N= 69. Ultrasound 5 minutes, Short wave diathermy 15 minutes, plus lumbar strengthening exercises. These included 10 repetitions of; prone lying leg elevation, prone lying chest elevation and supine bridging. 20 sessions lasting approximately 40 minutes.
2. Quality of life health survey (SF-36) (36–151)
2 Groups: Inclusion criteria included: Group 1 improved in pain by 2.87
(SD 0.15) and group 2 improved by 3.95 (SD 0.26).
1. Conventional treatment
a. LBP of any duration Group 1 improved in SF-36 by 10.70
(SD 5.9) and group 2 improved by 24.6 (SD 7.6).
2. Dynamic muscular stabilization techniques
b. Age > 20, < 40 2.N= 72. 20 sessions of one on one dynamic muscular stabilization exercise. Isometric abdominal drawing in manoeuvre in crook lying, progressing onto contraction holds with leg lifts. Progressing onto positions of sitting, 4 point kneeling, standing, supine and kneeling. Progressing onto functional high speed exercises, at the discretion of the therapist.
Smith
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
9
o
f
2
1
http://ww
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
Patients were not allowed to have pain r elief during the study period.
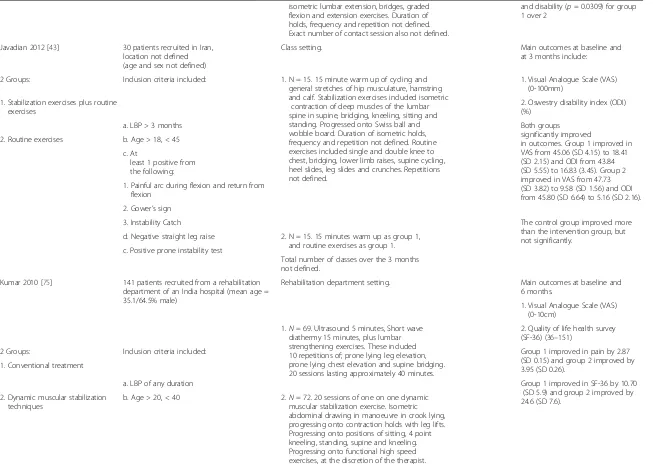
Macedo 2012 [76] 172 patients were recruited by general practitioners or from a physical therapy department waiting list in Australia (mean age = 49.1/48.8% male).
Class and home setting. Outcome taken at baseline,
2 months, 6 months and 12 months include:
1.N= 86. 2 sessions a week in 1stmonth, 1 session a week in 2ndmonth, total of 12 hours, plus daily home based exercise. Plus 2 booster sessions at 4 and 10 months. Stage 1: tailored exercises aimed at multifidus and transversus abdominis muscles. When the patient could achieve 10 repetitions of 10 second holds progressed to stage 2. Stage 2: Integrating contraction of muscles
into more advanced function tasks and exercises, based upon individual therapy assessment. Patients advised to do 30 minutes per week in 1stmonth, and 60 minutes a week in 2ndmonth.
1. Average numerical rating scale (NRS) for pain over last week (0–10)
2 Groups:
2. Roland-Morris Disability Questionnaire (RMDQ) (0–24)
1. Motor control exercises Group 1 pain scores at baseline, 2,
6 and 12 months were 6.1 (SD 1.9), 4.1 (SD 2.5), 4.1 (SD 2.5) and 3.7 (SD 2.7).
Inclusion criteria included:
Group 2 pain scores were; 6.1 (SD 2.1), 4.1 (SD 2.5), 4.1 (SD 2.7) and 3.7 (SD 2.6).
2. Graded activity a. Chronic nonspecific low back pain
b. duration > 3 months Group 1 RMDQ at baseline, 2, 6 and 1
2 months were; 11.4 (SD 4.8), 7.5 (SD 6.4), 8.0 (SD 7.1) and 7.4 (SD 6.7). Group 2 RMDQ were; 11.2 (SD 5.3), 8.0 (SD 6.5), 8.6 (SD 6.8) and 8.0 (SD 6.9).
c. age > 18, < 80 2.N= 86. Same class duration, frequency and home exercises as group 1. The programme
included individualized and submaximal exercises working on generalized (whole body) exercises without consideration of specific muscle activity. It was aimed at ignoring illness behaviours
and reinforcing wellness behaviours. Cognitive behavioural principles were used to help the participants overcome the natural anxiety associated with pain and activities.
There were no significant differences between treatment groups at any of the time points.
Marshall 2013 [77] 64 patients were recruited via community advertising in Australia (mean age = 36.2/ 62.5% male).
Exercise class setting. Outcomes taken at baseline,
2 months and 6 months include:
1. Visual Analogue Scale (VAS) (0-10cm)
2 Groups: 1.N= 32. 50–60 minutes, 3 x a week for
8 weeks. The teaching of the isometric abdominal drawing in manoeuvre, with biofeedback pressure transducer under lumbar spine. Working in side lying, prone lying positions with upper and lower limb exercises. Including warm and cool down with whole body stretches.
2. Oswestry disability index (ODI) (%)
VAS for group 1 at baseline was 3.6 (SD 2.1). Difference at 2 and 6 months from baseline were;−1.9 (CI 95%−2.6 to−1.2) and−1.6 (CI 95% -14.2 to−6.7). VAS for group 2 at baseline was 4.5 (SD 2.5). Difference at 2 and 6 months from baseline were;−0.8 (CI 95%−1.5 to−0.1) and−1.2 (CI 95%−1.9 to−0.6).
1. Specific trunk exercises Inclusion criteria included:
2. Stationary cycling a. Pain between the costal margins and inferior gluteal folds
b. Age > 18, < 50 2.N= 32. 50–60 minutes, 3 x a week for 8 weeks. Stationary bike, with variation in seated/standing positions, resistance and cadence with warm up and down and whole-body stretching.
ODI for group 1 at baseline was 25.4 (SD 11.2). Difference at 2 and 6 c. Duration > 3 months
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
10
of
21
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
months from baseline were;−10.4 (CI 95%−14.2 to−6.7) and−10.4 (CI 95%−14.0 to−6.8). ODI for group 2 at baseline was 24.0 (SD 11.9). Difference at 2 and 6 months from baseline were;−3.9 (CI 95%−7.8 to 0) and−5.9 (CI 95%−9.5 to−2.4).
VAS significantly lower at 2 months for group 1 (p<0.05). ODI scores also
significantly lower in group 1 at 2 months (p=0.019). Between group differences were no longer observed
at 6 months.
Moon 2013 [78] 21 patients recruited from a rehabilitation outpatient clinic in Korea (mean age = 28.5/ 66.7% male).
Class setting. Outcomes taken at baseline at and
8 weeks include:
2 Groups: 1. Visual Analogue Scale (VAS)
(0–100) Inclusion criteria included: 1.N=11. 60 minute class, twice a week for
8 weeks. 15 minute warm up of stretches and 10 minute warm down, same in both groups. All exercises were performed with the abdominal drawing in manoeuvre and included crook lying, knee lifts, leg slides, straight leg raises, plank, 4 point kneeling leg lifts and alternate leg and arm lifts, bridging on Swiss ball, sitting on chair and Swiss ball, prone lying, side plank, wall sits with Swiss ball, 4 point kneeling pelvic tilts, sit up with Swiss ball (number of exercises and duration of hold not defined).
2. Oswestry disability index (ODI) (%) 1. Stabilization exercise
Group 1 baseline pain score was 33.5 (SD 18.4) and group 2 was 34.2 (SD 17.1). Baseline ODI group 1 was 14.7 (SD 2.9) and group 2 15.5 (SD 4.3)
2. Dynamic strengthening exercises a. Non specific LBP.
b. Pain > 3 months
c. Without nerve root pain At 8 weeks group 1 improved in
VAS by
16.7 (SD 7.0) and group 2 by 14.1 (SD 8.2). Group 1 improved ODI by 6.1 (SD 1.9) and group 2 by 3.6 (SD 1.5).
2.N= 10. 60 minute class, twice a week for 8 weeks. 15 minute warm up of stretches and 10 minute warm down, same in both groups. Exercises performed included crook lying, bridging, mini sit ups, sit ups, twisting sit ups, knee to chest, prone leg extension, prone spine extensions, 4 point kneeling leg lifts, and alternate leg and arm lifts (number of exercises and duration of hold not defined).
No significant difference between groups at 8 weeks for pain (p=0.66) or ODI (p=0.07).
Rasmussen-Barr 2009 [45]
71 patients recruited from a private outpatient physiotherapy clinic in Sweden (mean age = 38.5/49.3% male).
Class and home setting. Main outcomes taken at baseline,
8 weeks, 6, 12 and 36 months include:
1.N= 36. Weekly exercise class for 8 weeks, lasting 45 minutes. Treatment included instruction on deep muscles of lumbar spine and isometric contraction of transversus abdominis with and multifidus by the
2 Groups: 1. Oswestry disability index (ODI) (%)
Inclusion criteria included: 1. Graded exercise
Smith
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
11
of
21
http://ww
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
abdominal drawing in manoeuvre. Bio-feedback was used. The class progressed to performing the exercise in different postural positions. Progression was based upon pain response (exact postural positions, duration of hold and repetitions not defined). Patients encourage of perform exercise at home daily for 15 minutes.
2. Visual Analogue Scale (VAS) (0–100)
Group 1 baseline ODI score was 20 (25th/75th percentiles 12/26). Changes in score compared to baseline at 8 weeks, 6, 12 and 36 months were−7 (−15/-4),
−9 (−19/-2),−10 (−20/-2) and−11 (−23/-4) respectively.
2. Daily walks a. Mechanically induced LBP
b. > 8 weeks duration
Group 2 baseline ODI score was 22 (14/28) and changes in score compared to baseline at 8 weeks, 6, 12 and 36 months were−4 (−10/0),−4 (−10/0),−2 (−12/2) and−6 (−14/0) respectively. c.≥1 pain free period in last year 2.N= 35. Patients had 1 x 45 minute appointment
at the start of the 8 weeks, and at the end. Instructed to take 30 minutes of walking a day at fastest pace possible without increasing pain (2 x 15 minutes allowed). Also a general home exercise plan provided, with no follow up instruction provided (exact exercises not defined). d. Pain below the costal margin and above the
inferior gluteal folds.
Group 1 baseline VAS score was 32 (25th/75th percentiles 18/59). Changes in score compared to baseline at 8 weeks, 6, 12 and 36 months were−15 (−31/-8),−15.5 (−30/-3.5),−12 (−34.5/-3) and−14 (−40/-4.5) respectively.
e. No leg pain
f. Working Group 2 baseline VAS score was 38
(23/62) and changes in score compared to baseline at 8 weeks, 6, 12 and 36 months were−8 (−19/-1),−9 (−24/0),−12 (−22/0) and−12 (−23/-2) respectively. g. Age > 18, < 60
Significant improvement in ODI with group 1 over group 2 (p=0.003). No between groups difference in pain was found.
Rhee 2012 [44] 42 patients recruited in Seoul, Korea (mean age = 50.2/50% male).
Class and home setting. Main outcomes taken at baseline
and at 4 weeks include:
1. Million Visual Analogue Scale (MVAS) (0–150)
1.N= 21. Supervised spinal stabilization exercises 3 times a week over a 4-week period, plus 5 x a week home exercises. Exercise involved abdominal drawing in manoeuvre in 5 different positions; prone, prone with leg and arm lifts, 4 point kneeling leg and arm lifts, crook lying mini sit ups, crook lying mini twist sit ups. Duration of hold and repetitions not defined.
2. Oswestry disability index (ODI) (%)
2 Groups: Inclusion criteria included: Both groups significantly improved
for MVAS score (p<0.01). Group 1 improved from 42.70 (SD 13.80) to 32.81 (SD 10.85). Group 2 improved from 33.26 (SD 15.27) to 23.42 (SD 13.43)
1. Spinal stabilization exercises a. Recurrent LBP
2. Control b. At least 1 previous episode
Both groups significantly improved for ODI score (p<0.001). Group 1 improved from 27.76 (SD 12.11) to c. Age > 21
d. No leg pain 2.N= 21. Provided with an education/advice booklet.
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
12
of
21
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
25.29 (SD 12.59) and group 2 improved from 17.29 (SD 9.15) to 12.52 (SD 8.50).
Sung 2013 [33] 46 patients recruited in Cleveland, Ohio (mean age 50.4/47.8% male).
Class and home setting. Main outcomes taken as baseline
and at 4 weeks include:
1. Oswestry disability index (ODI) (%)
2 Groups: 1.N= 21. Class setting for 20 minutes, 1 x a week
for 4 weeks. Plus at home daily for 20 minutes. Exercise involved abdominal drawing in manoeuvre in 5 different positions; prone, prone with leg and arm lifts, 4 point kneeling leg and arm lifts, crook lying mini sit ups,
crook lying mini twist sit ups. 5 second holds 2 x 15 reps.
Group 1 significantly improved from 24.89 (SD 11.89) to 17.73 (SD 11.75) (p= 0.03). Group 2 improved from 26.69 (SD 8.65) to 24.46 (SD 8.87) (p= 0.40).
Inclusion criteria included:
1. Core stabilization exercise a. LBP > 2 months
2. Spinal flexibility exercise b. Age > 21
No statistically significant difference between groups.
c. No leg pain 2.N= 25. Class setting for 20 minutes, 1 x a week for 4 weeks. Plus at home daily for 20 minutes. Exercise involved; single and double knee to chest in supine, 4 point kneeling flexion stretch, sitting flexion stretch and standing side flexion stretch. 5 second holds 2 x 15 reps.
Unsgaard-Tondel 2010 [79] 109 patients recruited from general practitioners, physical therapist and advertisements at a hospital in Norway (mean age = 40.0/30.3% male).
Local fitness centre, physical therapy department of hospital and home setting.
Main outcomes taken at baseline, 8 weeks and 1 year include:
3 Groups: 1. Numerical rating scale (NRS) for
current pain (0–10)
2. Oswestry disability index (ODI) (%)
1.N=36. 1 x 40 minutes one on one treatment at physical therapy department for 8 weeks. Teaching of isometric contraction of transversus abdominis with the use of ultrasound machine for feedback, initially in crook lying. Progression of exercises were individualized, but incorporated the isometric contraction of the local muscles. Participants were encouraged to perform the exercises at home, 10 contractions of 10 second holds 2–3 x a day.
NRS for group 1 at baseline, 8 weeks and 1 year was; 3.31 (SD 1.42), 1.76 (SD 1.54) and 2.01 (SD 1.94). Group 2 ; 3.61 (SD 1.75), 2.34 (SD 2.26) and 2.70 (SD 2.22). Group 3; 3.30 (SD 1.74), 2.73 (SD 2.32) and 2.66 (SD 2.03).
1. Motor control exercises Inclusion criteria included:
2. Sling exercises a. LBP > 3 months
3. General exercises b. Age > 19, < 60
c. Pain > 2, < 10 Numeric Pain Rating Scale (NPRS) (0–10
ODI for group 1 at baseline, 8 weeks was; 19.44 (SD 8.38) and 12.78 (SD 7.62). Group 2; 22.28 (SD 11.22) and 16.18 (SD 10.88). Group 3; 20.84 (SD 9.43) and 17.75 (SD 9.63). 2.N=36. 1 x 40 minutes one on one treatment at
physical therapy department for 8 weeks. Unloading elastic bands were attached to the pelvis to help participants maintain the neutral spine position through a range of leg and arm positions and movements. Progression of exercises were individualized, but generally was achieved through reducing the elastic band support.
The number of repetitions and sets was individualized.
No between group difference for pain 8 weeks (p=0.19) or 1 year p = 0.42) and no between group difference for ODI at 8 week (p= 0.21)
3.N=37. Local fitness centre classes of 2–8 patients for 1 hour, 1 x a week for 8 weeks. General trunk strengthening and stretching exercises.
Smith
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
13
of
21
http://ww
w.biomedce
ntral.com/1
Table 2 Characteristics of included studies
(Continued)
For example resisted trunk flexion, extension and rotation. 10 repetitions, in 3 sets.
Wang 2012 [80] 60 patients recruited from an outpatient rehabilitation department in a Chinese hospital (mean age = 38.6/58.3% male).
Class setting in rehabilitation centre. Main outcomes taken at baseline and at 12 weeks include:
1. Visual Analogue Scale (VAS) (0–10)
2 Groups: 1.N= 32. 40 minutes, 3 x a week for 12 weeks.
5 minute warm up. 30 minutes of exercises including; control of neutral spine alignment in sitting, prone, bridging, leg lifts, double knee flexion and reverse bridge. 5 minute warm down. Increasing difficulty as appropriate (exact details of exercises and progression not defined).
1. Core stability exercises Inclusion criteria included: 2. Oswestry disability index (ODI) (%)
2. Control of conventional exercise VAS improved in group 1 from 5.52
(SD 3.46) to 2.15 (SD 1.58) and in group 2 from 5.11 (SD 2.78) to 2.92 (2.13).
a. LBP > 3 months
b. Age > 19, < 60
c. Pain reproduced by movement ODI improved in group 1 from 33.11
(SD 5.73) to 15.34 (SD 7.65), and in group 2 from 30.42 (SD 7.44) to 19.18 (SD 10.21).
2.N= 28. 40 minutes, 3 x a week for 12 weeks. 5 minute warm up. 30 minutes of exercises including; sit ups, straight leg raises, bilateral straight leg raises, prone trunk extension. Then 5 minute warm down. Gradually increasing difficulty over 12 weeks (exact details of exercises and progression not defined).
Significant difference in favour of group 1 for VAS (p= 0.036) and ODI
(p= 0.027) at 8 weeks.
et
al.
BMC
Musculosk
eletal
Disorders
2014,
15
:416
Page
14
of
21
w.biomedce
ntral.com/1
Thirteen studies used a visual analogue scale to measure
pain [43-45,67,70-75,77,78,80], whilst four used an ordinal
numerical rating scale [62,63,70,73]. Four studies used the
Roland-Morris disability Questionnaire (RMDQ) to
meas-ure disability [62,63,70,73], whilst 12 measmeas-ured disability
using the Oswestry Disability Index (ODI) [33,43-45,64,
71-74,77-80]. Two studies also included the
Fear-Avoidance Beliefs Questionnaire (FABQ) as an outcome
measure [77,79].
Sixteen studies recorded short term follow-up, with 14
measuring pain and disability [43-45,68,70-74,76-80],
one just pain [67] and one just disability [33]. Seven
studies recorded medium term follow-up, with six
re-cording outcomes for pain and disability [45,68-70,
76,77], and one just pain [75]. Six studies recorded long
term follow-up, with five recording pain and disability
[45,68-70,76], and one just pain [79]. Two further
stud-ies went on to record follow-up of disability and pain
extra long term [45,69].
For the characteristics of the 12 included studies from
the 2008 review, please refer to the original review [13].
Study quality and bias
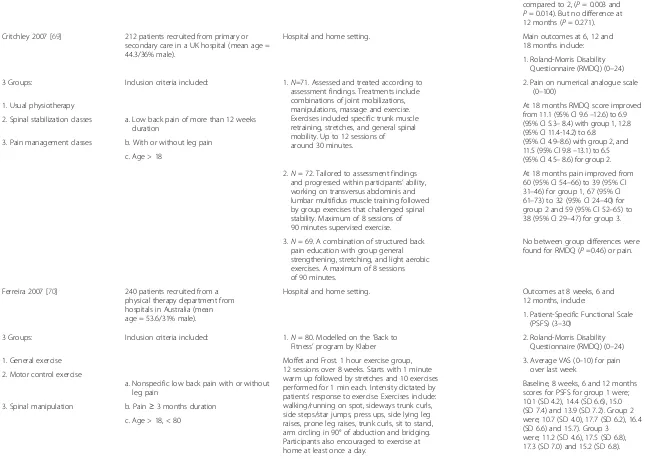
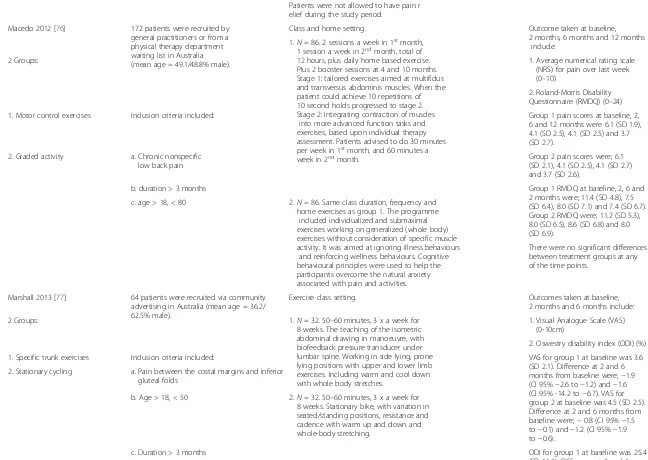
[image:15.595.68.538.89.271.2]The PEDro scores ranged from 4 to 9 [47], with mean
score of 6.6 (please refer to the PEDro website for score
breakdowns). All participants were randomly allocated
and all studies provided adequate results and analysis
(items 10 and 11). Only five studies failed to conceal
allo-cation [43,67,73,74,78] and one study assess baseline
com-parability [75]. No study blinded therapists, and only three
blinded their participants [68,75,80]. The lower scoring
studies were mainly marked down on blinding of
asses-sors, adequate follow-up, intention to treat analysis and
concealed allocation. With all studies, the greatest possible
source of bias was related to blinding. Eleven publications
scored
≥6 [33,45,68-72,76-80], along with seven from the
2008 review, totalling 18 studies of high quality [88-91,
93,95,98].
[image:15.595.67.538.556.705.2]Figure 3Forest plot of stabilisation versus other exercises: pain - long term.*Negative values favour stabilisation intervention, positive favour control.
Figure 2Forest plot of stabilisation versus alternative intervention: pain - long term.*Negative values favour stabilisation intervention, positive favour control.
Smithet al. BMC Musculoskeletal Disorders2014,15:416 Page 15 of 21
Data synthesis
Four studies from the 2008 review had insufficient data to
enable their inclusion into a meta-analysis [89,92,94,96],
one of which was a high quality paper [89]. Twenty-two
studies remained, 17 of high quality, which were
consid-ered suitably similar to warrant quantitative analysis and
synthesis. Too few studies (only two of high quality)
pro-vided data
≥18 months to warrant pooling of data results
for extra long term.
Pain
Twenty-two studies, with 2,258 participants, provided
post treatment effect on pain. Combining the results of
high quality studies demonstrated significant benefit
(mean difference) of stabilisation exercises for low back
pain short, medium and long term of -7.93 (95% CI -11.74
to -4.12), -6.10 (95% CI -10.54 to -1.65) and -6.39 (95% CI
-10.14 to -2.65) (Figure 2) respectively, when compared
with any alternative treatment or control. However, the
difference between groups was clinically insignificant with
Minimal Clinical Important Difference (MCID) for pain
being suggested as 24 to 40 [100], with between study
het-erogeneity high to moderate (
I
2= 67%, 50% and 45%
respectively).
Subgroup analysis of stabilisation exercises versus other
forms of exercise demonstrated statistical significant short
and medium term benefit, with a mean difference of -7.75
(95% CI -12.23 to -3.27) and -4.24 (95% CI -8.27 to -0.21).
Differences between groups was clinically insignificant
[100]. At long term there was no statistical or clinically
significant difference; -3.06 (95% CI -6.74 to 0.63)
(Figure 3). Between study heterogeneity was high to
negli-gible (
I
2= 66%, 0% and 0% respectively).
Combining the results of all studies for the sensitivity
analysis provided very similar results (Additional file 1).
Disability
[image:16.595.69.539.89.266.2]Twenty-four studies, with 2,359 participants, provided
post treatment effect on disability. Combining the results
of high quality studies demonstrated statistical significant
[image:16.595.68.538.572.705.2]Figure 5Forest plot of stabilisation versus other exercises: disability - long term.*Negative values favour stabilisation intervention, positive favour control.
Figure 4Forest plot of stabilisation versus alternative intervention: disability - long term.*Negative values favour stabilisation intervention, positive favour control.
benefit (mean difference) of stabilisation exercises for low
back pain short and long term of -3.61 (95% CI -6.53
to -0.70), -3.92 (95% CI -7.25 to -0.59) (Figure 4), when
compared with any alternative treatment or control.
How-ever, the difference between groups was clinically
insignifi-cant, with MCID for RMDQ 17 to 21 and 8 to 17 for ODI
(converting all to 0
–
100 scale) [100]. There was no
difference statistically or clinically medium term; -2.31
(95% CI -5.85 to 1.23). Between study heterogeneity was
high to moderate (
I
2= 83%, 65% and 56% respectively).
Subgroup analysis of stabilisation exercises versus other
forms of exercises demonstrated significant short and
medium term statistical benefit, but no significant clinical
difference, (mean difference) of -3.63 (95% CI -6.69
to -0.58) and -3.56 (95% CI -6.47 to -0.66). There was no
significant statistical or clinical long term benefit; -1.89
(95% CI -5.10 to 1.33) Figure 5. Between study
heterogen-eity was high to negligible (
I
2= 82%, 0% and 0%
respectively).
Combining the results of all studies for the sensitivity
analysis provided results that were less favourable for
stabilisation exercises for short to medium term, with
similar long term results (Additional file 1).
Two high quality studies featured FABQ as an outcome
measure. FABQ (physical activity) (0-24) and FABQ
(work) (0-42) for Marshall and Kennedy [77] at short term
follow-up had a non significant mean difference of 2.2
(95% CI
−1.3 to 5.6) and 2.3 (95% CI
−1.8 to 6.5)
respect-ively in favour of stabilisation exercises, when compared
to stationary bike exercises. There was a non significant
medium term mean difference of
−2.0 (95% CI
−5.1 to
1.0) and
−2.7 (95% CI
−7.6 to 2.1) respectively in favour of
the stationary bike. Short term mean difference for FABQ
(physical activity) for Unsgaard-Tøndel et al [79] was non
significant at -1.58 (-4.00 to 0.84) and -0.18 (-2.42 to 2.07)
in favour of sling and general exercises, respectively. Mean
difference for FABQ (work) was non significant at -0.40
(95% CI -3.81 to 3.01) in favour of slings and 0.25 (95%
CI -2.74 to 3.24) in favour of stabilisation exercises, when
compared to general exercises.
Discussion
Summary of main findings
The objective of this systematic review was to evaluate the
current evidence for the benefit of stabilisation (or
‘core
stability’) exercises for low back pain. The overall results
of the meta-analysis indicates a trend favouring core
sta-bility exercises which is not regarded as clinically
signifi-cant, when compared with any alternative treatment or
control. Minimal clinical important difference (MCID) for
pain has been suggested as 24 to 40, with 17 to 21 for
RMDQ and 8 to 17 for ODI (converting all to 0
–
100
scale) [100]. Any reduction in favour of stabilisation
exer-cises was potentially meaningless, with mean change
scores for pain (7.93, 6.10 and 6.39) and disability (3.61,
2.31 and 3.92) falling well below these MCID levels.
The overall results of the subgroup meta-analysis
sug-gest that stabilisation (or
‘
core stability’) exercises for
low back pain offer very minimal benefit in the short
and medium term when compared with other forms of
exercise, with mean change scores for pain (7.75 and
4.24) and disability (3.63 and 3.56) also falling well below
the clinically significant level. There was no significant
benefit in the long term, for pain or disability, when
compared with any other form of exercise. Results were
trending towards stabilisations, but results were not
sig-nificant, and any benefit would be clinically insigsig-nificant,
being largely below the MCID level.
In the subgroup analysis of long term follow-up for
stabilisations exercises versus other forms of exercises
heterogeneity was negligible (
I
2= 0%). Therefore, our
results, that stabilisation exercises offer no benefit over
alternative forms of exercises in the long term, can be
considered robust.
Whilst not statistically significant, both studies that
used FABQ as an outcome found that there was a trend
of worse scores with stabilisation exercises, compared
with stationary bikes, sling exercises and general exercises
[77,79]. The rehabilitation strategy surrounding
stabilisa-tion exercises has been challenged and has been suggested
could encourage unhealthy thoughts and beliefs on pain
and movement [101].
Limitations of included studies
For the meta-analysis of pain and disability for
stabilisa-tion versus any alternative treatment or placebo, high to
moderate heterogeneity existed.
I
2scores of pain for short,
medium and long term were 67%, 50% and 45%, and
disability, 83%, 65% and 56% respectively. The high
heterogeneity is possibly due to the different comparisons
being made between trials, and this reduces the
robust-ness of our short to medium term results. Overall, the
interventions were applied to a wide variety of patients,
including patients from low, medium or high
socio-economic groups, unemployed or employed, having had
investigations or no investigations, patients with or
with-out leg pain, patients with acute or chronic symptoms and
patients classed as
‘distressed’
or
‘distressed’
patients
excluded. Patients that have high levels of fear avoidance
scores are likely to have poor outcomes and compliance
with biomedical models of pain and treatments, such as
stabilisation exercises, and would likely do better with a
biopsychosocial approach [101]. Cairns et al. [88], for
example, excluded patients that were
‘distressed’
, which
perhaps biases results in favour of stabilisation exercises.
This compares with Ferreira et al [70], whose participants
were from low socio-economic groups, who are more
likely to develop chronic pain states with worse outcomes,
Smithet al. BMC Musculoskeletal Disorders2014,15:416 Page 17 of 21
and would perhaps bias results in favour of alternative
treatment
protocols
[102].
Furthermore,
differences
existed with how the treatments were delivered, class
set-tings only, one to one treatment only, class/one to one
treatment with home exercises or just home exercises,
plus different amount of therapist contact times.
The studies included within the main meta-analysis had
PEDro scores of
≥6, and as such were considered to have
low bias. However, the main source of bias within the
studies was blinding. No study blinded the therapist and
few studies blinded the participants. Given that the pain
and disability rating scales were patient self recorded it is
possible that this could over estimate the treatment effect
sizes. However blinding in active physiotherapy studies is
difficult to achieve.
One of the limitations with long term follow-up of RCTs,
particularly with exercise intervention, is the attrition rate.
An uneven dropout has the risk of over estimating the
ef-fect size of treatment groups. For example Ferreira et al.
[70] had an uneven dropout rate, with 9% for the general
exercise group and 19% for the stabilisation group. This
could easily bias the results in favour of the stabilisation
group.
Limitations of this review
An extensive literature search was carried out, with two
reviewers screening full texts independently for inclusion
and the data extracting independently checked. This
minimised bias within this review process, however, no
attempt was made to source unpublished studies, nor
studies published in any other language than English. It
is thought that identifying unpublished trials minimises
publication bias [103]. However, this approach has been
questioned by others, who suggest that truly unpublished
trials frequently have poor methodology, and ones with
better methodology often eventually become published
[104]. It is not possible to know if the inclusion, if available,
of any unpublished trials would considerably alter our
con-clusions, or if this truly is a weakness of this review.
Comparison with other reviews
Our main findings differ very little from the 2008 review
[13], however firmer conclusions about stabilisation
exercises can be drawn from our review. In the 2008
review the majority of the studies favouring stabilisation
exercises combined the exercises with some other form
of treatment, implying that it was the package of care
that was effective rather than stabilisation exercises
alone. In our updated review the majority of the studies
used stabilisation exercises as sole treatment, and as
such the data synthesis looks more closely at
stabilisa-tion exercises as sole treatment.
Our findings were similar to the Wang et al. [80] review,
which also concluded some short term benefit to pain and
disability for stabilisation exercises over general exercise,
with no long term benefit to pain. No comparison for long
term follow-up for disability was made, and no attempt at
analysing results against MCID was made. Of their five
in-cluded articles we inin-cluded three in our review. One was
excluded for duplicating results from another included
study, which was included in both of our and Wang et al’s
reviews. It is therefore possible that their meta-analysis
double counts these results [40,79]. The other study we
excluded during initial screening [105] looked at a
relax-ation yoga programme with meditrelax-ation, chanting and
counselling, and clearly doesn’t match our intervention
definition. It is perhaps questionable that this study was
included within Wang et al’s study [80].
Our findings differ from the Byström et al [22] review
which concluded long term benefit to disability in favour
of stabilisation exercises over general exercises and with
regards to pain at intermediate term. The differences
may be due to our inclusion of a further 15 publications;
their inclusion of studies within the analysis with high
risk of bias defined by means of a PEDro score of less
than 6; or their use of a fixed effects meta-analysis
model for pooled analysis where heterogeneity, as
mea-sured by
I
2, was less than 50%. Choosing fixed versus
random effect models solely based upon the test for
het-erogeneity is considered incorrect, and should be made
upon which model best fits the distribution of effects
sizes [106]. We used a random effects model on all
ana-lyses, since there is inherent heterogeneity in low back
pain within the literature. Using a fixed effects model
incorrectly could over estimate the pooled effect sizes
and underestimate the confidence interval width, thus
reducing reliability of results [106].
Conclusion
The results of this current systematic review suggest that
stabilisation exercises improves low back pain symptoms,
but no better than any other form of active exercise in the
long term. The low levels of heterogeneity and large
num-ber of high methodological quality of available studies, at
long term follow-up, strengthen our current findings.
There is a trend of worse fear avoidance scores.
This review cannot recommend stabilisation exercises
for low back pain in preference to other forms of general
exercise, and further research is unlikely to considerably
alter this conclusion.
Additional file
Additional file 1:Sensitivity analysis results.
Competing interests
The authors declare that they have no competing interests.
Authors’contributions
BS was responsible for conception and design, publication screening, acquisition of data, analysis and interpretation, drafting and revising the manuscript. CL was responsible for conception and design, publication screening, data interpretation, reviewing and revising the manuscript. SM was responsible for acquisition of data, data interpretation, reviewing and revising the manuscript. All authors have read and approved the final manuscript.
Source of funding
Funding for open-access publication was gained via the research support fund from the School of Health & Related Research, University of Sheffield. No other funding was obtained.
Author details
1Physiotherapy Outpatients, London Road Community Hospital, Derby
Hospitals NHS Foundation Trust, London Road, Derby DE1 2QY, UK.2School of Health & Related Research, University of Sheffield, Regent Court, 30 Regent Street, Sheffield S1 4DA, UK.3Faculty of Health & Wellbeing, Sheffield Hallam University, Sheffield S10 2BP, UK.
Received: 5 June 2014 Accepted: 1 December 2014 Published: 9 December 2014
References
1. Nachemson A, Jonsson E:Neck and Back Pain: The Scientific Evidence of Causes, Diagnosis, and Treatment.Philadelphia: Lippincott Williams and Wilkins; 2000.
2. Palmer KT, Walker-Bone K, Griffin MJ, Syddall H, Pannett B, Coggon D, Cooper C:Prevalence and occupational associations of neck pain in the British population.Scand J Work Environ Heal2001,27:49–56.
3. Walker BF:The prevalence of low back pain: a systematic review of the literature from 1966 to 1998.J Spinal Disord2000,13:205–217. 4. Hestbaek L, Leboeuf-Yde C, Manniche C:Low back pain: what is the
long-term course? A review of studies of general patient populations.
Eur Spine J2003,12:149–165.
5. Maniadakis N, Gray A:The economic burden of back pain in the UK.
Pain2000,84:95–103.
6. National Institute for Health and Care Excellence:Low Back Pain. Early Management of Persistent Non-Specific Low Back Pain [CG88].2009. 7. Pain in Europe; A 2003 Report.2003. http://www.paineurope.com. 8. Department of Health (DoH):The NHS Plan: A Plan for Investment a Plan for
Reform.2000:82.
9. Liddle SD, David Baxter G, Gracey JH:Physiotherapists’use of advice and exercise for the management of chronic low back pain: a national survey.Man Ther2009,14:189–196.
10. Hodges PW, Richardson CA:Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis.Spine (Phila Pa 1976)1996,21:2640–2650. 11. Hodges PW, Richardson CA:Altered trunk muscle recruitment in people
with low back pain with upper limb movement at different speeds.
Arch Phys Med Rehabil1999,80:1005–1012.
12. Richardson C, Jull G, Hodges P, Hides J:Therapeutic Exercise for Spinal Segmental Stabilization: In Lower Back Pain.Edinburgh: Churchill Livingstone; 1999.
13. May S, Johnson R:Stabilisation exercises for low back pain: a systematic review.Physi