Dissertation on
CLINICAL STUDY ON PROFILE AND SPECTRUM OF BACTERIAL AND
FUNGAL CORNEAL ULCERS IN A TERTIARY CARE HOSPITAL IN
CHENNAI
M. S. OPHTHALMOLOGY
BRANCH III
Of
REGIONAL INSTITUTE OF OPHTHALMOLOGY
MADRAS MEDICAL COLLEGE
CHENNAI – 600 003
THE TAMILNADU DR.M.G.R. MEDICAL UNIVERSITY
CHENNAI-600 003
MAY - 2019
CERTIFICATE
This is to certify that this dissertation entitled
“CLINICAL STUDY ON
PROFILE AND SPECTRUM OF BACTERIAL AND FUNGAL CORNEAL
ULCERS IN A TERTIARY CARE HOSPITAL IN CHENNAI”
is a bonafide
record of the research work done by
Dr. NATHIYA S
, Post graduate in Regional
Institute of Ophthalmology, Madras Medical College and Research Institute,
Government General Hospital,Chennai-08, in partial fulfillment of the regulations laid
down by The Tamil Nadu Dr.M.G.R. Medical University for the award of
M.S.Ophthalmology Branch III, under my guidance and supervision during the
academic years 2016-2019.
Prof.Dr. M.ANANDA BABU, M.S. D.O.,
Chief , Department of Cornea,
Director and Superintendent,
Regional Institute of Ophthalmology
Madras Medical College & Research
Institute,
Govt. General Hospital,
Chennai – 600 008
Prof.Dr. M.ANANDA BABU, M.S. D.O.,
Director and Superintendent,
Regional Institute of Ophthalmology
Madras Medical College & Research
Institute,
Govt. General Hospital,
Chennai – 600 008
Government General Hospital & Research Institute,
Chennai-600003
ACKNOWLEDGEMENT
I would like to express my sincere thanks and gratitude to
PROF.DR.R.JAYANTHI.,M.D.,FRCP(Glas)
Dean, Madras Medical College and
Government General Hospital for
giving me permission to conduct the study in this
Institution.
I have great pleasure in thanking
PROF. DR.M. ANANDA BABU, M.S.D.O.,
Director and Superintendent, RIOGOH,
Madras Medical College, my unit Chief and
my guide for his valuable advice in preparing this dissertation. I express my profound
gratitude to
PROF. DR.A.YOGESWARI M.S.DO.,
my unit chief for her valuable
guidance and
constant support for of this study.
I am grateful to
DR.V.SHARMILA DEVI M.S., AND DR.B.MEENAKSHI
M.S.,
my Assistant Professors, my Co Guides for their ideas, support and constant
guidance at every stage of this study.
My sincere thanks to my unit Assistant Professors
DR. M.SIVAKAMI M.S.,
and
DR. J.JAYALATHA DO.,M.S.,
for timely help and guidance in conducting
this study.
I wish to express my sincere thanks to my family, friends and all my colleagues
who helped me in bringing out this study.
Last but not the least, my heartful gratitude and sincere thanks to all my patients
DECLARATION BY THE CANDIDATE
I hereby declare that this dissertation entitled,
“CLINICAL STUDY ON
PROFILE AND SPECTRUM OF BACTERIAL AND FUNGAL CORNEAL
ULCERS IN A TERTIARY CARE HOSPITAL IN CHENNAI ”
is a bonafide and
genuine research work conducted by me under the guidance of
Prof Dr.M.ANANDA
BABU , M.S., D.O.,
Director and superintendent,
Head of Department of Cornea,
Regional institute of ophthalmology & Government Ophthalmic Hospital.
Chennai-600008.
Dr. NATHIYA S
Place: Chennai
CERTIFICATE
This is to certify that this dissertation work titled
“CLINICAL STUDY ON
PROFILE AND SPECTRUM OF BACTERIAL AND FUNGAL CORNEAL
ULCERS IN A TERTIARY CARE HOSPITAL IN CHENNAI
”
of the candidate
DR. NATHIYA S
with registration number
221613005
for the award of MS in the
branch of OPHTHALMOLOGY.
I personally verified the urkund.com website for the purpose of plagiarism
Check. I found that the uploaded thesis file contains from introduction to conclusion
pages and result shows 1 % percentage of plagiarism in the dissertation.
CONTENTS
SERIAL NO
TITLE
PAGE NO
PART I
1
INTRODUCTION
1
2
ANATOMY
4
3
EMBRYOLOGY
14
4
PHYSIOLOGY
15
5
CORNEAL ULCER
17
6
BACTERIAL CORNEAL ULCER
18
7
FUNGAL CORNEAL ULCER
43
8
NON HEALING ULCERS
52
9
COMPLICATIONS
54
PART 2
10
AIM
56
11
MATERIALS AND METHODS
57
12
RESULTS AND ANALYSIS
72
13
DISCUSSION
74
14
CONCLUSION
76
15
BIBLIOGRAPHY
i
16
PROFORMA
vi
17
KEY TO MASTER CHART
vi
18
MASTER CHART
vii
INTRODUCTION
Corneal ulcer is defined as disruption of epithelium with infiltration in surrounding and underlying stroma. In many of the developing countries in the world, corneal ulcer plays a major role in monoocular blindness and visual disability. It affects all age groups , both men and women worldwide.
Corneal ulcer is more commonly, a seriously infective condition which needs immediate and timely medical attention , to avoid visual disability in future.
Thus proper knowledge about the causative agents and various susceptible factors will be very much useful in appropriate management of the patients with corneal ulcer.
It can be ethier infective or non infective . Infective corneal ulcers are more prevalent than non infective causes.
Infective causes may be bacterial, viral, fungal, parasitic. Non infective causes may be traumatic, due to exposure , due to decreased corneal sensation.
Patient usually presents with sudden onset of pain,, redness, watering , and defective vision . Usually patients have history of trauma, fall of dust , or eye rubbing. If the ulcer is small and immune status of patient is good, ulcer heals fast , if associated with systemic illness or old age, with immuno compromised state, it usually progresses.
REVIEW OF LITRATURE
A Study conducted by Bharathi et al. regarding influence of risk factors, geographical variation’s, climate on microbial keratitis, found out that among the infective etiology bacterial was 34.4 % , predominant bacteria being streptococcus pneumonia, fungus being fusarium species, agricultural workers are being at higher risk for fungal , the month between june and September has higher incidence of fungal, where bacterial is less common during this period.1
A Study conducted by Prajna et al. regarding predictors of corneal perforation and need for penetrating therapeutic keratoplasty in corneal ulcer due to fungal etiology , found that the mean age was 49, 43.3% were women, most of them were belonging to southeastern Asia. The presence of hypopyon, infiltrate in posterior one third was associated with perforation with or without in need of therapeutic keratoplasty. 2
A study conducted by lalitha et al. in south india regarding trends in bacteria and fungal keratitis found out that fungus was isolated 34.3% than bacteria , and there is increase in the prevalence of fungal is the trend. And also says that there is decrease in the prevalence of bacterial keratitis which depicts the economic development of our country and easy access to the antibiotic drugs. 3
A study conducted by gonales et al. regarding the incidence of corneal ulceration in south india, found out that annual incidence of fungal keratitis per 10000 population was about 3.4. Male : Female ratio was 1.6:1.0. 4
A study conducted by prajna et al. regarding the usage of oral voriconzole in treatment of fungal corneal ulcer found out that there is no additional benefit of adding oral voriconazole to topical antifungal agents in treatment of filamentous fungal corneal ulcer.5
ANATOMY
Cornea is a transparent avascular, structure with smooth convex outer surface and concave inner surface, which resembles a small watch glass. Its anterior surface is elliptical and posterior surface is circular. The word cornea is derived from a Latin word “corneus “which means horn. 8
Cornea is almost a sphere , the central 1/3 rd is called optical zone about 5.4 mm. Cornea contributes to 1/6 of outer fibrous coat of eyeball, that is 1.3cm square. The measurement of anterior vertical diameter is 11mm. Anterior horizontal diameter measures about 12 mm. Posterior diameter is 11.5 mm. Radius of curvature of central is about 7.8mm anteriorly and 6.5 mm posteriorly. Refractive index of cornea is 1.376. The total dioptric power of normal human eye is +58.6. out of which +43 contributed by cornea(Air tear is +43).
LAYERS OF CORNEA:
There are six layers in cornea . They are 1. Epithelium,
2. Bowmans layer, 3. Stroma,
4. Predescemets layer of Dua, 5. Descemets layer ,
6. Endothelium.
1.Epithelium:
Epithelium is stratified squamous type .
Microvilli of epithelium helps in tear film stability
Epithelium is replaced once a week by itself.
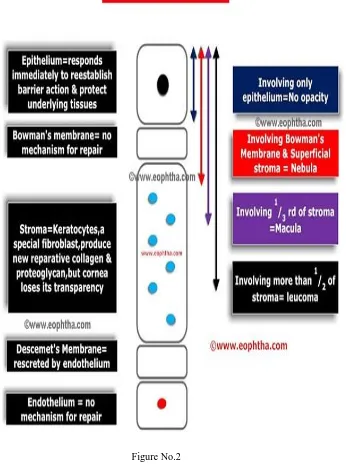
Figure No.1 – Layers of Cornea 2. Bowman’s layer:
Once destroyed , it cannot regenerate and it leaves a superficial corneal scar.
3.Stroma (substantia propria):
It contributes about 90 percent of total thickness of cornea.
It is composed of collagen fibres .
The lattice arrangement of collagen fibrils embedded in extracellular Matrix is partly responsible for corneal transparency.
Type I and type V fibrillation collagen are interwined with filaments of type VI collagen.
Keratocyte cells of corneal stroma produce ground substance and collagen fibrils during embryogenesis.
4.Predescemets membrane of Dua:
It is also called as dua's layer
It is discovered in 2003 by Harminder Dua. 5. Descemet membrane:
It is the basement membrane of corneal endothelium.
It maintains the integrity of eye ball.
It is about 15 micrometer thick , acellular.
It is very strong and impervious to air.
Descements layer once destroyed, it regenerates.
It’s prominent peripheral end forms schwalbe's line.
6.Endothelium:
It is the inner most layer of cornea.
Made up of closely interdigitated cells arranged in a mosaic pattern of mostly hexagonal cells.
It is the metabolically active layer of cornea. And corneal hydration is mainly controlled by the endothelial pump Na+ K+ ATPase pump.
Normal endothelial cell density is between 2000 and 3000 cells/mm 2
TOPOGRAPHY OF CORNEA:
Shape of the cornea is important for fitting the contact lens.
It flattens on convergence
Curvature varies from Apex to limbus, greater flattening in nasal and superior
Small spherical zone of anterior curvature is decentered up and outwards with visual axis, but correctly centered for pupillary aperture is termed as corneal Apex or cap
It is flatter in men than women.7
COMPOSITION OF HUMAN CORNEA :
Water – 78 %
Collagen Type I – 50-55 % Type III – 1 % Type IV – 8-10 % Type VI – 25–30 %
Keratan sulphate – 0.7 %
Chondroitin sulphate – 0.3 %
Salt 1 %
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
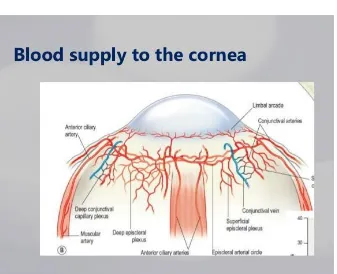
BLOOD SUPPLY OF CORNEA:
The cornea is an avascular structure
Small loops derived from the anterior ciliary vessels derived from Anterior ciliary artery and forms perilimbal plexuses of blood vessels and invade its periphery for about 1 mm
[image:21.612.74.411.336.610.2] Actually , these loops are not in cornea but in the subconjunctival tissue which overlaps the cornea.9
NERVE SUPPLY OF CONREA :
Cornea is rich in sensory nerve supply derived from ophthalmic division of trigeminal nerve via long and short ciliary nerves.
They form a pericorneal plexus just outside the limbus and then pass onto cornea as 60- 70 trunks.
These nerves loose their myelin sheath and reach cornea.
[image:22.612.52.474.123.633.2] Cornea does not have proprioceptive sensation.10
Figure No.4 - Nerve supply to the Cornea
BIOMECHANICS OF THE CORNEA:
Cornea provides a stiff , strong outer coating of eye.
Bowman’s layer and the corneal stroma are key factors contributing to cornea's biomechanical properties .
Failure of biomechanical properties of cornea leads to corneal ectasia, where the shape of the cornea is distorted, causing irregular astigmatism and vision loss.7
EMBRYOLOGY
The formation of cornea is induced by the lens and optic cup by 7 weeks of intrauterine life.
Epithelium- Surface Ectoderm
Bowman’s membrane – Mesenchyme
Stroma – Mesenchyme and Neuralcrest
[image:24.612.60.426.238.657.2] Descemets membrane -Synthesized by endothelium Endothelium- Neural crest 7
Figure No.5 – Development of Eye
PHYSIOLOGY
To meet the functional demands of cornea , It must be having the following features:
It must be transparent
It must be Refractive to light
Contain intraocular pressure
Provides protective interface
FACTORS MAINTAINING CORNEAL TRANSPARENCY
:1.Anatomical factors:
Avascularity of cornea
Demyelinated nerves
Lattice arrangement of collagen fibrils in corneal stroma
Regular arrangement of epithelial and endothelial cells
Non keratinized surface epithelium
Presence of tear film
Absence of corneal pigmentation
Paucity of cells in corneal stroma
2. Relative dehydration of stroma
- Endothelial Na- K ATP ase pump
- Special intercellular junction in endothelium
- Epithelium is largely impermeable to water
3. Intra ocular pressure
Any acute raise in intraocular pressure will cause corneal edema.7
Formatted: Bulleted + Level: 1 + Aligned at: 1" + Indent at: 1.25"
CORNEAL ULCER
:It is defined as loss of corneal epithelium with infiltration into the surrounding and underlying stroma. 10
It can be infectious and non infectious.
INFECTIOUS NON INFECTIOUS
Bacterial
Viral
Fungal
Parasitic
Acanthamoeba
Peripheral ulcerativve keratitis
Moorens ulcer
Neurotrophic keratopathy
Exposure keratopathy
Drug iduced keratopathy Normal commensals of ocular surface:
1.Staphylococcus epidermidis
2.Diphtheroids
3.Propionibacterium acne
4.Staphylococcus aureus
5.Streptococcus viridans
Formatted: Bulleted + Level: 1 + Aligned at: 1" + Indent at: 1.25"
Formatted: Bulleted + Level: 1 + Aligned at: 1" + Indent at: 1.25"
6.Streptococcus pneumonia 9
BACTERIAL CORNEAL ULCER:
It develops when,
Either the Local ocular defence mechanism is jeopardized or
Causative organism is very virulent
Figure No.6 The predisposing factors are
Corneal abrasion
Trauma
Foreign body
Inappropriate Usage of steroid drops
Contact lens Usage- particularly in extended lens users.
Exposure or neurotrophic keratitis
OCULAR SURFACE DISORDERS AND CORNEAL ULCERS:
Herpetic keratitis
Bullous keratopathy
Dry eye
Chronic blepharitis
Trichiasis
Entropion
Ectropion
Exposure Keratitis
Severe allergic eye disease
Corneal anaesthesia due to neurotrophic keratitis.
Formatted: Bulleted + Level: 1 + Aligned at: 1.04" + Indent at: 1.29"
Examination of ocular surface in keratitis
Eyelid magins Meibomian gland dysfunction Margin ulceration
Eyelash abnormalities Punctal abnormalities
Tear film Dry eye
Conjunctiva Discharge Inflammation
Structural alterations like follicles, papillae Cicatrization. Keratinization
Membrane, Foreign body.
Ulceration Scarring- Thinning Nodule
Cornea Location
Density
Size, shape, satellite lesions Character of infiltrate margin Status of endothelium
Lacrimal apparatus Regurgitation of purulent material on pressing on lacrimal area.
SYSTEMIC ASSOCIATIONS AND CORNEAL ULCER
oDiabetes
oHypovitaminosis A
oMalnutrition
oImmunosuppression
oChronic alcoholism8
CONTACT LENS USERS AND CORNEAL ULCER:
Particularly with extended lens users
Because of hypoxia, corneal epithelium compromise occurs, so even minor trauma can cause defect.
Soft contact lens users are more at risk than rigid contact lens wearer.
Infection occurs mainly due to poor lens 22iphthe.
Virulent organism which can penetrate intact healthy corneal epithelium are 1. Neisseria
2. Cornybacterium 22iphtheria 3. Hemophilus influenza 4. Listeria monocytogenes
Common bacteria causing keratitis in India :
Gram positive cocci staphylococcus aureus
Staphylococcus epidermidis
Streptococcus pneumonia
Formatted: Bulleted + Level: 1 + Aligned at: 1" + Indent at: 1.25"
Gram positive bacilli
corynebacterium diphtheroids
C. xerosis
Gram Negative Bacilli pseudomonas aeruginosa
Acinetobactor species
Enterobacteriaceae- klebsiella
Serratia
Proteus
Escherichia coli
Gram negative diplobacillus Moraxella lacunata
Gram negative coccobacillus Hemophilus influenza
Hemophilus aegyptius
Gram positive filaments Nocardia asteroids
Nocardia brasiliensis
Non tuberculous mycobacterium Mycobacterium fortuitum
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Mycobacterium chelonae
Acid fast organism Nocardia STAGES OF CORNEAL ULCER:
I . Stage of infiltration 2. Stage of active ulceration 3. Stage of regression 4. Stage of cicatrisation
:
Figure No. 7 - Corneal Ulcer Stages 1.Stage of infiltration
Infiltration of polymorphonuclear cells with or without lymphocytes occur into the epithelium
Further course of the ulcer will depend on the dynamic balance between hosts defence mechanism and virulence of invading organism.6
2.Stage of active ulceration:
1. At this stage, necrosis and sloughing of epithelium, Bowman’s and stroma
occurs
2. Active hyperemia, exudation over ulcer bed, hypopyon occurs.
3. If the virulence of organism is more, or in absence of antimicrobial agents, it spreads in deeper tissues
4. Walls project above normal surface
5. Grey zone of infiltration present.
6. Hypopyon
7. Progress laterally or deeper
3.The stage of regression :
a line of demarcation occurs
digestion of necrotic material
Vascularization
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5", Tab stops: Not at
begin to heal
Occurs when body’s defence mechanism takes upper hand over invading organism
Clinically associated with rounding of edges of ulcer and regular orientation of infiltrates
4.Stage of cicatrisation:
If the involvement is epithelium only there is no scar.
progressive re epithelization along with scar formation due to laydown of collagen fibrils by activated fibroblasts
opacity which formed can be Nebula, or Macula or leucoma based on the location of involvement.9
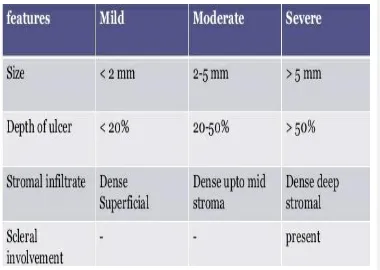
GRADING OF ULCERS:
Figure No. 8 – Grading of Ulcer
Factors determining bacterial virulence: 1. Bacterial adherence –
Biological slime produced by bacteria not only helps in adhesion to host but also helps to resist phagocytosis
2. Bacterial invasion-
Bacterial capsule and other surface components are important in bacterial invasion- subcapsular constituents of bacteria are major mediators of corneal inflammation. Protease released from bacteria also facilitates bacterial invasion.
3. Corneal inflammatory response-
Recruitment of acute inflammatory cells occurs within few hours of bacterial inoculation,. Vasodilation , increased vascular permeability results in inflammatory exudation, hypopyon formation. Uncontrolled infective and inflammatory response may lead to corneal perforation.8
Symptoms of bacterial corneal ulcer
Toxic looking patients
Symptoms more than signs
There will be lot of conjunctival congestion,discharge and chemosis
Pain, redness,watering,
Blurring of Vision
Mucopurulent discharge 6
Signs of bacterial corneal ulcer:
Lid edema
Circumcorneal congestion
Epithelial defect with surrounding stromal infiltrate
Stromal edema
Well defined ulcer, with clear base without any necrotic tissue
Single ulcer
Sterile , hypopyon, which changes the shape with change in head posture.
Decematocele, impending ulceration
Scleritis can oEndophthalmitis7
Figure No. 9 – Images belonging to Patients who presented to our Clinic with Corneal Ulcers
Formatted: Centered, Space After: 0 pt, Line spacing: 1.5 lines
Characteristics of specific bacterial ulcers:
Staphylococcus aureus It is a gram positive cocci
Coagulase positive organism
Normal commensal of nares, conjunctiva, skin
Classically presents with focal well defined infiltrates.
Sevaral smaller infiltrates in a patient with marked blepharitis is typical of staphylococcus.
Commonly seen in compromised cornea’s such as bullous keratopathy, chronic herpetic keratitis, dry eyes, ocular rosacea.
May present with marked suppuration, deep stromal abscess
Staphylococcus epidermidis Indolent course
May cause stromal abscess
Streptococcus pneumonia It is gram positive bacteria ,
Commensal of upper respiratory tract
associated with chronic dacryocystitis,
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Bulleted + Level: 1 + Aligned at: 0.5" + Indent at: 0.75"
ulcers are characteristically well defined , localised round or oval shaped with distinct borders.
seen in immunocompromised patient with deep stromal infiltrate and dense hypopyon.
Infection are usually aggressive
Presents with deep,oval, central stromal ulceration, with progressive edge.
Posterior corneal abscess and hypopyon are usually due to exotoxins released by the pathogens
Pneumococcus is called as ulcus Serpens. It forms a serpiginous ulcer
Pseudomonas aeruginosa It is a gram negative bacilli ,
commensal of GIT ,
Causes fulminant, aggressive infection,
rapidly progressing, with lot of suppuration, greenish discharge with hypopyon and
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
produce hour glass appearance even within 48 hours.
most commonly seen in Soft contact lens users, associated with paracentral corneal infiltrate with surrounding corneal edema and hypopyon.
It is a gram negative bacilli ,
commensal of GIT ,
Causes fulminant, aggressive infection,
produce hour glass appearance even within 48 hours.
Marked stromal melt
Ring infiltrate
Decematocele formation and perforation
Surrounding stroma shows ground glass appearance with diffuse greying of epithelium
Mucopurulent discharge
Proteus Features similar to pseudomonas
Associated with chronic epithelial disease
Formatted: Bulleted + Level: 1 + Aligned at: 0.5" + Indent at: 0.75"
Klebsiella
Moraxella Keratitis after trauma in debilitated, alcoholic, malnourished or diabetic patients
Indolent ulcer with moderate anterior chamber reaction
Neisseria gonorrhoea Rapidly progressive, hyperpurulent
conjunctivitis, with marked chemosis and stromal infiltration
Nocardia Indolent ulcer after minor trauma,especially with contaminated soil.
Characteristically raised, superficial,pin head like infiltrates in a wreath like configuration, brush fire like border with multifocal lesions
Infiltrates have indistinct fluffy or feather like appearance like cracked windshield or snow flake appearance.
Non tuberculous
Slowly progressive keratitis
Usually by contaminated sharp instruments like
Formatted: Bulleted + Level: 1 + Aligned at: 0.5" + Indent at: 0.75"
Formatted: Bulleted + Level: 1 + Aligned at: 0.5" + Indent at: 0.75"
Formatted: Bulleted + Level: 1 + Aligned at: 0.5" + Indent at: 0.75"
mycobacterium knife, blade, sutures.
Occurs after corneal trauma, or surgery like LASIK
Multifocal infiltrates with spoke like margins.
Heal very slowly
Bacillus cereus Typical stromal rig infiltrate remote from site of injury, with rapid progression to stromal abscess.
DIAGRAMMATIC REPRESENTATION OF CORNEAL PATHOLOGY IN CLINICAL PRACTICE
black colour is used to depict foreign bodies ,contact lenses
Blue colour used to represent edema ,epithelialsand stromal edema
brown colour used to represent Iris and Iris pigmentation
red colour represent blood vessels
green colour fluorescein staining of epithelial defect, corneal ulcer.
Yellow – stromal infiltrates. 9
Formatted: Bulleted + Level: 1 + Aligned at: 0.5" + Indent at: 0.75"
Formatted: Bulleted + Level: 1 + Aligned at: 0.5" + Indent at: 0.75"
Signs OF HEALING CORNEAL ULCER:
o Decrease in the density of stromal infiltrates
o decrease in stromal edema
o decrease in endothelial plaque
o decrease in the anterior chamber reaction
o reduction in the size of hypopyon
o Re epithelialization
o Cessation of corneal thinning
INVESTIGATIONS:
Corneal smear and from the edges and moraxella are recovered from the base of the ulcer. calcium alginate swab is used for better results. culture plates are streaked with C shaped design.
Stains commonly used are 1. Gram stain
2. Acidine orange 3. Calcoflour white 4. Giemsa
Formatted: Bulleted + Level: 2 + Aligned at: 0.75" + Indent at: 1"
Procedure of gram staining:
fix the slide in methyl alcohol
flood slide with Crystal gentian Violet for one minute
Rinse the slide with grams iron for one minute
Decolorize with acid alcohol for 20 seconds
Counterstain with dilute carbolfuschin or safranin for one minute 8
PRINCIPLE OF GRAM STAINING:
Thicker peptidoglycan layer in the cell wall of Gram Positive organism makes it more permeable to primary stain , so it retains the gentian violet - iodine Complex and appear purple. where as Gram Negative bacteria loses the primary stain that is gentian violet iodine Complex with discoloration step and appear pink when counterstained with saffranin.
Various culture medias used in ulcers :
o Blood agar – aerobic bacteria and facultative Saprophytic fungi
Anaerobic bacteria like P.aeruginosa, s. Aureus S.Pneumonia
o Chocolate agar – aerobic and facultative, anaerobic bacteria like Hemophilus , Neisseria and bartonella, moraxella
o Brain heart infusion – Bacteria, fungi
o Sabouraud’s dextrose agar - fungi
o Enriched thioglycollate broth – aerobic and anaerobic bacteria
o Lowenstein Jenson agar – Non tuberculous mycobacteria
o E coli plated non nutrient agar – Acanthamoeba 5
[image:49.612.49.592.101.765.2]Staphylococcus aureus- pearly white colonies in C shaped steaks on a blood agar plate . Diminishing number of colonies are noted in consecutive C Streaks , indicating bonafide infection rather than contamination of plate.
Figure No. 10
DIFFERENTIAL DIAGNOSIS:
Formatted: Bulleted + Level: 2 + Aligned at: 0.75" + Indent at: 1"
o Keratitis due to other organisms like fungal, acanthamoeba, stromal herpes simplex keratitis, mycobacterium
o Marginal keratitis
o Sterile inflammatory corneal infiltrates associated with contact lens Usage
o Peripheral ulcerative keratitis
o Toxic keratitis 8
TREATMENT
Aims of treatment:
o Eliminate viable bacteria from the cornea
o Suppression of inflammatory response Principle :
o Symptomatic relief
o Control of infection
o Prevention of complications like perforation
Always start with cycloplegics to relieve ciliary spasm.
Monotheraphy with moxifloxacin can be started at every half an hour intervals, in the mean time to get microbiology reports.
Formatted: Bulleted + Level: 2 + Aligned at: 0.75" + Indent at: 1"
Formatted: Bulleted + Level: 2 + Aligned at: 0.75" + Indent at: 1"
Then depending on the microbiology report , antimicrobial therapy has to be started.9
Agents against gram positive organisms are:
Fortified cefazolin
0.5 Percent moxifloxacin
Vancomycin
Chloramphenicol
Agents against gram negative bacteria are
Amikacin
Gentamycin
Ceftazidime
Ciprofloxacin
Ofloxacin
Levofloxacin
PREPARATION OF FORTIFIED ANTIBIOTICS:
1. CEFAZOLIN – Add 10 ml of distilled water to 500 mg vial of cefazolin to obtain 5 % solution
2. Amikacin - Add 10 ml of distilled water to 100 mg of amikacin to get 1% percent solution
3. Gentamycin – Add 2 ml of injectable gentamycin to 5 ml of commercial topical preparation.
5 ml has 15 mg
added drug 2 ml has 80 mg total in 7 ml , there is 95 mg so one ml contains 13.5 mg
4. vancomycin – Add 10 ml of distilled water to 500 mg vial of vancomycin to obtain 5% solution
5. Ceftazidime – Add 9.2 ml of artificial tears to a vial of ceftazidime 1g powder for injection
Dissolve and take 5 ml of this solution and add it to 5 ml artificial tears. Refrigirate and shake well before use.
6. Tobramycin –
Add 2 ml to tobramycin ophthalmic solution to give 14 mg/ml solution Refrigerate and shake well before use.
INDICATIONS TO START ON SYSTEMIC ANTIBIOTICS:
Impending perforation
Peripheral ulcer with scleral infiltrations
Infection with Neisseria, pseudomonas, Hemophilus( Ciprofloxacin with polymyxin)9
Indications for therapeutic keratoplasty
Decematocele formation
Impending perforation
FUNGAL CORNEAL ULCERS
Typically patients will have history of injury with vegetative matter, animal tail. History of injury in agricultural fields ,
. Most commonly occurs in farmers.
Also seen in immunocompromised patients , patients on long term steroid therapy, patients with dry eye. 6
FUNGUS RESPONSIBLE FOR CORNEAL ULCERS: 1.FILAMENTOUS
A.Septated 1.Non pigmented
Fusarium solani, oxysporum, moniliforme,
Aspergillus
Fumigatous flavus
Cephalosporin (Acremonium)
Paecilomyces
2. Pigmented
curvularia
Alternaria
cladasporium
Senegelensis
Verruculosa , pallescenes
Lasiodiplodia
Theobromac
Celletotrichum
Drechslera ( Helminthosporium) B. Nonseptated
Rhizopus
(mucormycosis
Absida
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Formatted: Bulleted + Level: 1 + Aligned at: 0.29" + Indent at: 0.54"
II . Yeast
Candida
Cryptoccus neoformans
Rhinosporidium
Albicans, parapsilosis
Krusei, tropicalis III. Dimorphic fungi
Histoplasmosis
Most common fungus seen in north India is aspergillus 5 Most common fungi seen in south India is fusarium. 5
Characteristics of typical fungal corneal ulcer
Symptoms are always inappropriate with signs
Dry looking
Greyish white
Feathery margins
Indistinct borders
With necrotic base
Satellite lesions
Formatted: Bulleted + Level: 1 + Aligned at: 0.29" + Indent at: 0.54"
Multiple ulcers with single large ulcer in the middle
Endothelial plaques
Hypopyon- typically non sterile, fixed, convex upper border, cheesy hypopyon with fungal hyphae
Gritty texture while scraping
INVESTIGATIONS
Scraping
. Scraping samples to be sent for 10 Percent KOH mount used for detection of fungal hyphae.
KOH will stain fungal filaments( due to its chitin content) and Acanthamoeba cysts.
Addition of 10 Percent glycerol with KOH will act as mordant and keep the smear for 6 months
Figure No. 11 – Fungal Hyphae
Culture media used for fungal cultures are
in sabouraud’s dextrose agar
Potato dextrose agar
Brain heart infusion
Blood agar
Most of the fungi causing causing keratitis are evident within 2-3 days of culture. Typical colony formation takes 1-2 weeks. Hence , culture must be continued for atleast 2 weeks before it is declared negative.6
Figure No. 13 – Various Culture Media Formatted: Centered
Formatted: Font: (Default) Times New Roman, 13 pt
Figure No. 14 – Various Culture Media
TREATMENT:
Always start with cycloplegics to relieve ciliary spasm and pain.
Based on clinical diagnosis , antifungal therapy( Natamycin) should be started without delay.
Most of the commonly used antifungal drugs penetrate the cornea poorly. So necrotic debris over the ulcer bed should be scrapped to make those drugs
Formatted: Font: (Default) Times New Roman, 13 pt
Under topical anesthesia, daily under slit lamp, with the help of blunt end Bard Parker no 11 Blade necrotic tissues are scrapped. 6
ANTIFUNGAL AGENTS: I . POLYENES :
Large molecular weights- Amphotericin B, Nystatin
Smallar molecular weight - natamycin 2.IMIDAZOLES
Ketoconazole
Clotrimoxazole
Econazole
Miconazole
Thiabendazole
Newer imidazole derived from fluconazole _ voriconazole. It is a newer azole derived from fluconazole. It is active against aspergillus, Fusaruim, Candida. It exhibits cytochrome p450 dependent 14 sterol demethylase, an enzyme responsible for conversion of lanosterol to 14 demethylase lanosterol.
ANTIMETABOLITES
1.flucytosine
Formatted: Bulleted + Level: 1 + Aligned at: 0.74" + Indent at: 0.99"
Formatted: Bulleted + Level: 1 + Aligned at: 0.69" + Indent at: 0.94"
Natamycin is the drug of choice for filamentous fungi especially Fusarium
AMPHOTERICIN B for non filamentous fungi, especially Aspergillus 5
Voriconazole for deep stromal involvement, along with systemic ketoconazole
Amphotericin B as topical preparation will act better against Candida
Natamycin has got better penetration power than Amphotericin B5 Indications for oral antifungal:
Deeper ulcers , not responding to topical medications
Ulcer involving the limbus and extending to sclera
In such cases oral ketoconazole tablets 200 mg BD can be used after assessing liver function test.
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5"
Figure No. 15 – Treatment Algorithm for Managing Fungal Corneal Ulcers Formatted: Font: 13 pt, Not Bold
Formatted: Centered
Formatted: Font: 13 pt, Not Bold
NON HEALING CORNEAL ULCERS
:
Causes:
1. Patient factor 2. Organism factor 3. Adnexal pathology PATIENT FACTOR:
Non compliant patient
Not applying the drops as prescribed by the doctor. ORGANISM FACTOR:
If the organism is so virulent
Or identified organism may be wrong, so reculture the organism. ADNEXAL PATHOLOGY:
Rule out any blepharitis ,entropion ,ectropion, blepharitis, dacryocystitis and all adnexal pathologies as mentioned earlier.
TREATMENT OF NON HEALING CORNEAL ULCERS:
1. Treatment differs to each case .
1. Re culture to confirm the initial organism
2. Re check the adnexal structures especially for dacrocystitis
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5", Tab stops: Not at 0.5"
3. intrastromal injection of voriconazole.
4. Removal of hidden/ impacted foreign body
5. Secondary glaucoma should be treated with oral acetazolamide along with topical antiglaucoma drugs.
6. Tarsorrhaphy
7. At last resort for recalcitrant cases Therapeutic penetrating keratoplasty
PRINCIPLES OF DOING THERAPEUTIC KERATOPLASTY IN CORNEAL ULCER
aims to control and eliminate the infection
Done along with peripheral iridectomy
1 mm of uninvolved corneal tissue is removed along with the infective issue is removed.
INDICATIONS FOR DOING KERATOPLASTY IN CASES OF CORNEAL ULCER
perforated corneal ulcer
impending corneal ulcer
COMPLICATIONS OF CORNEAL ULCERS
Subdivided into
1. Before perforation
2. Perforation
3. After perforation Before perforation;
1. Corneal opacity can be nebula, Macula, Leucoma
2. Iritis/ iridocyclitis- as a result of diffused toxins in Anterior chamber
3. Decematocele- in impending perforation stage, descemet membrane will bulge out as a transparent bulging structure called decematocele
4. Complicated cataract
Perforation :
In a progressive case, decematocele ruptures due to sudden strains, with lowering of intar ocular pressure.
1. Rupture
2. PAS
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5", Tab stops: Not at
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5", Tab stops: Not at
3. Very shallow AC
4. Hypotonic eyeball
5. Iris prolapse- perforated ulcer may have inflammatory exudates and iris plugging at the perforated site
After perforation
1. Iris tissue prolapse
2. Adherent Leucoma/ scarring- it becomes the most common cause for vision loss following healed corneal ulcer.
3. Pseudocornea
4. PAS
5. Endophthalmitis
6. Panophthalmitus
7. In case of large perforation, iris prolapse through perforation. Grey yellow exudates deposits over iris. The exudate organise and forms thin layer of connective tissue. The iris and newly formed cicatricial tissue are too week to withstand the intra ocular pressure and bulges. The ectatic cicatrix in which iris is incarcerated is called as anterior staphyloma
8. Phthisis bulbi – intra ocular pressure falls, the eye may shrink. Its shape becomes quadrilateral due to pressure by text muscles on hypotonous eye. Degenerative changes occur which leads to no perception of light.
9. Secondary glaucoma – dense exudates blocking the trabecular meshwork will cause raise in IOP
10. Decematocele
TITLE
:“CLINICAL STUDY ON PROFILE AND SPECTRUM OF BACTERIAL
AND FUNGAL CORNEAL ULCERS IN A TERTIARY CARE HOSPITAL IN CHENNAI.
AIM:
1. To study the demography of various corneal ulcers.
2. To study the aetiology, risk factors and clinical presentation of various Corneal ulcers
OBJECTIVES:
1. To study the incidence, predisposing factors and epidemiological characteristics of corneal ulcers
2. To study the various modes of presentation of corneal ulcers.
INTRODUCTION:
Infectious keratitis is a serious concern for ocular morbidity in a developing country like ours. It can lead to a variety of ocular complications a major proportion of
Formatted: Bulleted + Level: 1 + Aligned at: 0.25" + Indent at: 0.5", Tab stops: Not at
which is preventable, if intervened early. Though a variety of technological advancements have revolutionised ophthalmology, managing corneal ulcers is still a difficult. As the treatment requires usage of topical medications for prolonged periods, the cost factor and socioeconomic status of the patient plays a huge role in the management and recovery.
In this study, we analyse the incidence, etiological and epidemiological factors, clinical and microbiological profile of the patients in a large tertiary eye center over a period of one year.
STUDY DESIGN
:
Prospective observational study
DURATION OF THE STUDY
–1 year 2017 – 2018.
METHODOLOGY (MATERIALS AND METHODS):
Subject selection:
100 patients who presented with various forms of infectious corneal ulcers to the Cornea services of Regional Institute of Ophthalmology and Government Ophthalmic Hospital were included in the study.
Inclusion criteria: All Infectious corneal ulcers (bacterial/ viral/ fungal/ protozoal)
2. Perforated corneal ulcers when scraping is not possible 3. Peripheral ulcerative keratitis
4. Sterile neurotrophic ulcers and
5. Other ulcers associated with autoimmune conditions. 6. Pre existing corneal disorders.
SAMPLE SIZE:
100 patientsMETHODS:
From all patients detailed history was recorded. Everyone was subjected to detailed anterior segment examination with slit lamp biomicroscopy and findings were documented with colour coded diagrams. Corneal scraping was done and sent for gram staining and KOH mount. Patients’ stay in the hospital was documented and the complications/ recovery were monitored.
FOLLOW UP:
Using Statistical package
[image:73.612.61.433.281.684.2]OBSERVATION AND RESULTS:
TABLE 1: AGE-WISE DISTRIBUTION
AGE GROUP NUMBER
20-30 1
31-40 5
41-50 32
51-60 23
61-70 30
71-80 9
GRAPH 1: AGE-WISE DISTRIBUTION
AGE
TABLE 2 : SEX DISTRIBUTION
MALE 71
FEMALE 25
GRAPH 2 : SEX DISTRIBUTION
SEX
MALE FEMALE
TABLE 3 : LITERACY LEVEL
LITERATE 7
ILLITERATE 93
TABLE 4: OCCUPATION
LABOURER 35
DRIVER 6
FARMER 22
MECHANIC 6
OTHERS 31
LITERACY LEVEL
LITERATE ILLITERATE
GRAPH 4: OCCUPATION
TABLE 5 : DEMOGRAPHIC NUMBERS OF RURAL/URBAN POPULATION
RURAL 61
URBAN 39
OCCUPATION
GRAPH 5 : DEMOGRAPHIC NUMBERS OF RURAL/URBAN POPULATION
TABLE 6 : PRESENCE OF HYPOPYON
NUMBER
YES 77
NO 23
GRAPH : PRESENCE OF HYPOPYON
HYPOPYON
TABLE 7 : DURATION OF SYMPTOMS
3 DAYS 36
1 WEEK 26
2 WEEKS 23
1 MONTH 15
GRAPH 7 : DURATION OF SYMPTOMS AND PRESENTATION
0 5 10 15 20 25 30 35 40
3 DAYS 1 WEEK 2 WEEK 1 MONTH
DURATION PRESENTATION
DURATION
36
TABLE 8: LOCATION OF ULCER
CENTRAL 42
PERIPHERAL 28
PARACENTRAL 30
GRAPH 8: LOCATION OF ULCER
0 10 20 30 40 50
CENTRAL PARACENTRAL PERIPHERAL
LOCATION OF ULCER
LOCATION OF ULCER
42 30
TABLE 9: TRAUMATIC AGENT
ANIMAL MATTER** 15
PLANT MATTER 37
METAL FB 21
UNKNOWN** 17
FINGERNAIL 10
GRAPH 9: TRAUMATIC AGENT
TRAUMATIC AGENT
ANIMAL PLANT METAL FB UNKNOWN FINGERNAIL
37 15
21 17
ANIMAL MATER** : INSECT,COW TAIL, etc UKNOWN** : SOMETHING FALLEN INTO EYE
TABLE 10: CULTURE RESULTS
POSITIVE 50
NEGATIVE 50
GRAPH 10 : CULTURE RESULTS
CULTURE
POSITIVE NEGATIVE
Formatted: Space Before: 12 pt
Formatted: Space Before: 12 pt
TABLE 11: CULTURE POSTIVITY SUBGROUP ANALYSIS
PURE BACTERIAL 7
PURE FUNGAL 13
MIXED 25
OTHERS** 5
OTHERS** : ACANTHAMOEBA
TABLE 12: TREATMENT RESPONSE
ULCER HEALED 53
REQUIRED TKP 47
GRAPH 13: TREATMENT RESPONSE
CULTURE POSITIVE
PURE BACTERIAL PURE FUNGAL OTHERS MIXED
25
7
13
TABLE 13: HISTORY OF DIABETES
WITH HISTORY OF DIABETES 67 WITHOUT DIABETES 33
RESPONSE
HEALED ULCER REQUIRED TKP
GRAPH 13: HISTORY OF DIABETES
RESULTS
DIABETES
YES NO
A total of 100 patients who presented to the cornea clinic, Regional Institute of Ophthalmology, Chennai were included in this study. 71 patients were males and 29 were females. The major presentation age group is between 41-50 years.
Majority of them (35/100) were labourer and farmers(22/100) by occupation. Study showed that illiterate (93/100) were more commonly associated with corneal ulcer. People coming from rural areas (61/100) was commonly associated. One of the predisposing factors, Diabetes mellitus was studied in all patients. A majority of them (67/100) were diabetic.
We studied the duration of symptoms and the time taken for presentation to the hospital. 15 patients presented 1 month after the onset of symptoms. Most of them who presented late took treatment outside, and presented in later stages of ulcer. But majority of them (36/100) presented within 3 days of symptom onset. During presentation (77/100) many patients had hypopyon.
83 patients gave a definite source of traumatic agent, with plant material being the most common offending agent (37/100). 17 patients did not know the offending agent.
Dacryocystitis of the culture positive cases, (n=50), bacterial colonies could be recovered in 32 patients. 25 were gram positive 7 were gram negative. Fungal colonies were grown in 13 patients, who were KOH positive in staining. Mixed bacterial and fungal colonies were found in 25 patients. Pure bacterial colonies were isolated in 7 patients. The remaining 5 patients had acanthamoebal growth in staining and culture methods. None of them were contact lens users.
With successful medical management, 63 patients responded well , some of them needed intrastromal voriconazole injections. 47 patients progressed to perforation/ impending perforation, inspite of all modalities of medical management, required Therapeutic keratoplasty. 15 of these patients required regraft due to multiple reinfection. This was found to be significantly higher in those patients who presented late and had mixed organisms in microbiological analysis.
Trauma is one of the important causes for corneal blindness, thus its spectrum covers all age groups, with greatest impact on the younger age group. Infectious keratitis presents early in the course of the disease since it causes painful defective vision. If appropriately managed, vision threatening complications can be limited to a great extent.
In our study, we found the men in the 40-50 year age group to be commonly affected by infectious keratitis. This could be explained by the fact that this group contributes significantly to the work force in the society. Majority of them were illiterates and labourers by occupation. This compounded by the easy availability of over –the-counter steroid eye drops and use of Tradional Eye Medications(TEM) like mothers milk, castor oil can lead to late presentation in the clinic, with serious complications. We documented 5 cases of usage of TEM where 5 of them used castor oil.
Among the bacterial isolates, Gram-positive cocci were the predominant isolates, with Streptococcus pneumoniae being most common and Pseudomonas spp. was the predominant bacterial isolate among Gram-negative bacilli. Mixed bacterial and fungal colonies predominated our series. But Upadhaya et al have reported more bacterial isolates from corneal ulcers. Also Deshpande and Koppikar, found Pseudomonas aeruginosa as the most common bacterial isolate in their study.
significant role in the common fungal species grown in culture as they are present as saprophytes in the environment.
About half of the isolates did not grow any organism. This has been reported in many other studies. Usage of topical medications before the hospital visit can lead to a poor yield in corneal scraping. This was the hypothesis proposed by Deorukhkar et al in their study. We did not withhold any topical medication before gram staining/culture.
Sengupta et al12, analysed the changing patterns of infectious keratitis over a 7 year period in South India and found increasing incidence of fungal keratitis with a declining trend in bacterial keratitis. Lalitha et al3 proposed changing economic developments and increased access to antibiotics as one of the reasons for declining trend in smear positive bacterial culture yield. In our study, we isolated mixed bacterial and fungal colonies in half of the culture positive patients.
One major obstacle in the management of corneal ulcer is the proper usage of eye drops. Using these eye drops on hourly basis, ensuring adequate interval between each eye drop, ensuring proper storage and refilling the eye drop once bottle gets over are some of the areas where the treating physician has to spend time with the patient to ensure compliance and adherence. Underlying systemic illness has to addressed as well. In our series, about 67 patients had Diabetes mellitus among them Uncontrolled diabetes mellitus is commonly associated with ulcer.
Corneal ulceration due to trauma is a common problem, associated with male preponderance , mixed ulcers are being the commonest infection. The Study emphasises the need for microbiological diagnosis for treatment. Early presentation and the nature of organism plays a major role in healing of ulcer. Our results highlight the importance of microbiologic diagnosis for infectious keratitis. The vast majority of corneal ulcers seen clinically have mixed bacterial and fungal etiology. Empirical treatment based on clinical examination alone will not be sufficient.
BIBLIOGRAPHY
1.
MICROBIAL KERATITIS IN SOUTH INDIA: INFLUENCE OF RISK
FACTORS, CLIMATE, AND GEOGRAPHICAL VARIATION.
BHARATHI
MJ
1, RAMAKRISHNAN
R, MEENAKSHI
R, PADMAVATHY
S, SHIVAKUMAR C, SRINIVASAN M.
2.
PREDICTORS OF CORNEAL PERFORATION
OR
NEED
FOR
THERAPEUTIC KERATOPLASTY IN SEVERE FUNGALKERATITIS: A
SECONDARY ANALYSIS OF THE MYCOTIC ULCER TREATMENT
TRIAL II.
PRAJNA
NV
1, KRISHNAN
T
1, RAJARAMAN
R
1, PATEL
S
2, SHAH
R
3, SRINIVASAN
M
1, DAS
M
1, RAY
KJ
4, OLDENBURG
CE
4, MCLEOD
SD
4,5, ZEGANS
ME
6, ACHARYA
NR
4,5,7, LIETMAN
TM
4,5,7,
ROSE-NUSSBAUMER J
4,5; MYCOTIC ULCER TREATMENT TRIAL GROUP.
3.
TRENDS
IN
BACTERIAL
AND
FUNGAL
KERATITIS
IN
SOUTH INDIA, 2002-2012.
LALITHA
P
1, PRAJNA
NV
2, MANOHARAN
G
1, SRINIVASAN
4.
INCIDENCE OF CORNEAL ULCERATION IN MADURAI DISTRICT,
SOUTH INDIA.
GONZALES CA
1, SRINIVASAN M, WHITCHER JP, SMOLIN G.
5.
EFFECT OF ORAL VORICONAZOLE ON FUNGAL KERATITIS IN
THE MYCOTIC ULCER TREATMENT TRIAL II (MUTT II): A
RANDOMIZED CLINICAL TRIAL.
PRAJNA NV
1, KRISHNAN T
1, RAJARAMAN R
1, PATEL S
2, SRINIVASAN
M
1, DAS
M
1, RAY
KJ
3, O'BRIEN
KS
3, OLDENBURG
CE
3, MCLEOD
SD
3,4, ZEGANS ME
5, PORCO TC
3,4,6, ACHARYA NR
3,4, LIETMAN TM
3,4,6,
ROSE-NUSSBAUMER J
3,4; MYCOTIC ULCER TREATMENT TRIAL II GROUP.
6.
KANSKI'S CLINICAL OPHTHALMOLOGY
A SYSTEMATIC APPROACH AUTHORS:
BRAD BOWLING
7.
KHURANA A K
ANATOMY AND PHYSIOLOGY OF EYE
8.
CORNEA COLOR ATLAS
KRACHMER
,J.H/PALAY,D
9.
CORNEAL
ULCERS
DIAGNOSIS
AND
MANAGEMENT
WITH
10.
CORNEAL ULCERS DIAGNOSIS AND MANAGEMENT BY
NAMRATA
SHARMA RASIK B VAJPAYEE
11.
A
CLINICAL
MICROBIOLOGICAL
STUDY
OF CORNEAL
ULCER PATIENTS AT WESTERN GUJARAT, INDIA.
SOMABHAI KATARA R, DHANJIBHAI PATEL N, SINHA M.
12.
CHANGING
REFERRAL
PATTERNS
OF
INFECTIOUS
CORNEAL ULCERS TO A TERTIARY CARE FACILITY IN
SOUTH INDIA - 7-YEAR ANALYSIS.
SENGUPTA
S,
THIRUVENGADAKRISHNAN
K,
RAVINDRAN
RD,
VAITILINGAM MC.
13.
SPECTRUM OF BACTERIAL KERATITIS AT A TERTIARY EYE
CARE CENTRE IN INDIA.
KALIAMURTHY J, KALAVATHY CM, PARMAR P, NELSON JESUDASAN CA,
THOMAS PA.
14.
DEMOGRAPHIC PROFILE, CLINICAL FEATURES AND OUTCOME
OF PERIPHERAL ULCERATIVE KERATITIS: A PROSPECTIVE STUDY.
SHARMA N, SINHA G, SHEKHAR H, TITIYAL JS, AGARWAL T, CHAWLA B,
15. CORNEAL ULCERATION IN THE ELDERLY IN HYDERABAD,
SOUTH INDIA.
PROFORMA
1.
Name: Date:
2.
Age /Sex : Male/Female
3.
OP/IP No: Occupation:
4.
Affected eye:
5.
H/o of injury, if any:
6.
Any predisposing factors:
7.
Previous treatments: Antibiotics/ native medicines/ steroids/ nil
8.
Vision:
9.
Ulcer location: Central/ paracentral/ midperipheral/ marginal
10.
Ulcer size: Small/ medium/ larges
11.
Outcome of keratitis: Healed with scarring/ Progressed with need for
keratoplasty
12.
Corneal scraping : Gram + / - Cocci / Bacilli
13.
KOH: + / -
Mixed: Negative: Cyst:
KEY TO MASTER CHART
M – Male
F – Female
FB – Foreign body
TKP – Therapeutic penetrating keratoplasty
RURAL/URBAN :
RURAL-1
URBAN- 2
TRAUMATIC AGENT:
UKNOWN- SOMETHING FALLEN INTO EYE
OTHERS :
YES- ACANTHAMOEBA
CONTROL:
1-
CONTROLLED DIABETES MELLITUS
2-
UNCONTROLLED DIABETES MELLITUS
HYPOPYON:
NO AGE SEX OCCUPATION RURAL/URBAN LITERACY DIABETES CONTROL DURATION LOCATION OF ULCER HYPOPYON DUCT TRAUMATIC AGENT CULTURE PURE BACTERIAL FUNGAL OTHERS MIXED ULCER HEALED TKP
1 25 M FARMER 1 2 NO 1 3 DAYS CENTRAL YES 1 PLANT POSITIVE YES - - - YES
-2 60 F OTHERS 1 2 YES 1 1 MONTH CENTRAL YES 1 UNKNOWN POSITIVE - - YES NO YES
3 50 F OTHERS 1 2 YES 1 2 WEEKS PARACENTRAL YES 1 UNKNOWN POSITIVE - YES - - NO YES
4 45 M LABOURER 1 2 NO 1 1 WEEK PARACENTRAL YES 1 FINGERNAIL POSITIVE - - YES - NO YES
5 34 M LABOURER 1 2 NO 1 2 WEEKS PARACENTRAL YES 1 PLANT NEGATIVE - - - - NO YES
6 49 M DRIVER 1 1 YES 1 3 DAYS PARACENTRAL YES 1 METAL FB POSITIVE - - - YES YES
-7 56 M LABOURER 1 2 YES 1 1 MONTH CENTRAL YES 1 METAL FB NEGATIVE - - - - NO YES
8 67 M LABOURER 1 2 YES 1 1 MONTH CENTRAL YES 1 METAL FB NEGATIVE - - - - YES NO
9 70 M LABOURER 1 2 YES 1 1 MONTH CENTRAL YES 1 METAL FB NEGATIVE - - - - YES NO
10 80 M LABOURER 1 2 YES 1 1 MONTH CENTRAL YES 1 METAL FB NEGATIVE - - - - YES NO
11 76 M LABOURER 1 2 YES 1 3 DAYS CENTRAL YES 1 METAL FB NEGATIVE - - - - YES NO
12 56 M OTHERS 1 2 NO 1 3 DAYS CENTRAL YES 1 UNKNOWN NEGATIVE - - - - YES NO
13 45 M OTHERS 1 2 NO 1 3 DAYS CENTRAL YES 2 UNKNOWN NEGATIVE - - - - YES NO
14 44 M OTHERS 1 2 NO 1 3 DAYS CENTRAL NO 1 UNKNOWN NEGATIVE - - - - YES NO
15 33 M OTHERS 2 2 NO 2 3 DAYS CENTRAL NO 1 UNKNOWN NEGATIVE - - - - YES NO
16 44 M OTHERS 2 2 NO 2 3 DAYS CENTRAL NO 1 UNKNOWN NEGATIVE - - - - YES NO
17 55 M OTHERS 2 2 NO 2 3 DAYS CENTRAL NO 1 UNKNOWN NEGATIVE - - - - NO YES
18 78 M LABOURER 2 2 YES 2 3 DAYS CENTRAL NO 1 PLANT NEGATIVE - - - - NO YES
19 65 M LABOURER 2 2 YES 2 3 DAYS CENTRAL NO 1 PLANT NEGATIVE - - - - YES
-20 56 M LABOURER 2 2 YES 2 3 DAYS CENTRAL NO 1 PLANT NEGATIVE - - - - YES
-21 45 M OTHERS 2 2 YES 2 3 DAYS CENTRAL NO 1 PLANT NEGATIVE - - - - YES
-22 43 M OTHERS 1 2 YES 1 3 DAYS CENTRAL NO 1 PLANT NEGATIVE - - - - YES
-23 56 M OTHERS 1 2 YES 1 3 DAYS CENTRAL NO 1 PLANT POSITIVE - - - YES YES
-24 79 F OTHERS 1 2 YES 2 1 WEEK CENTRAL NO 1 PLANT POSITIVE - - - YES YES
-25 55 F DRIVER 1 1 YES 2 1 WEEK CENTRAL NO 1 PLANT POSITIVE - - - YES YES
-26 48 F DRIVER 2 2 YES 2 1 WEEK CENTRAL NO 1 PLANT POSITIVE - - - YES YES
-27 33 F MECHANIC 2 1 YES 2 1 WEEK CENTRAL NO 1 PLANT POSITIVE YES - - - YES
-28 44 F OTHERS 2 2 YES 2 1 WEEK CENTRAL NO 1 PLANT POSITIVE YES - - - NO YES
29 66 F OTHERS 2 2 YES 2 1 WEEK CENTRAL NO 1 PLANT POSITIVE YES - - - NO YES
30 77 F OTHERS 2 2 NO 2 1 WEEK CENTRAL YES 2 PLANT POSITIVE - YES - - NO YES
31 65 F OTHERS 2 2 YES 2 1 WEEK CENTRAL YES 2 PLANT POSITIVE - YES - - NO YES
32 56 F LABOURER 2 2 YES 2 1 WEEK PERIPHERAL YES 2 ANIMAL POSITIVE - - - YES NO YES
33 40 F LABOURER 2 2 YES 2 1 WEEK PERIPHERAL YES 2 ANIMAL POSITIVE - - - YES NO YES
34 60 F LABOURER 1 2 YES 2 1 WEEK PERIPHERAL YES 2 ANIMAL POSITIVE - - - YES NO YES
35 50 F LABOURER 1 2 NO 2 1 WEEK PERIPHERAL YES 2 ANIMAL POSITIVE - - - YES NO YES
36 50 F LABOURER 1 2 YES 2 1 WEEK PERIPHERAL YES 2 ANIMAL POSITIVE - - - YES NO YES
37 50 F LABOURER 1 2 YES 2 2 WEEKS PERIPHERAL YES 1 ANIMAL POSITIVE - - - YES NO YES
38 50 F LABOURER 1 2 YES 2 2 WEEKS PERIPHERAL YES 1 ANIMAL POSITIVE - - - YES NO YES
39 46 M LABOURER 1 2 NO 2 2 WEEKS PERIPHERAL YES 1 ANIMAL POSITIVE - YES - - YES NO
40 56 M LABOURER 1 2 NO 2 2 WEEKS PERIPHERAL YES 1 ANIMAL POSITIVE - YES - - YES NO
41 58 M LABOURER 1 2 NO 2 2 WEEKS PERIPHERAL YES 1 ANIMAL POSITIVE - YES - - YES NO
42 66 M LABOURER 1 2 NO 2 2 WEEKS PERIPHERAL YES 1 FINGERNAIL POSITIVE - - YES - YES NO
43 61 M DRIVER 1 2 NO 2 2 WEEKS PERIPHERAL YES 1 FINGERNAIL POSITIVE - - YES - NO YES
44 62 M DRIVER 1 1 YES 2 2 WEEKS PERIPHERAL YES 1 FINGERNAIL POSITIVE - - YES - NO YES
45 64 M MECHANIC 1 2 NO 2 2 WEEKS PARACENTRAL YES 1 FINGERNAIL POSITIVE - - - YES NO YES
46 65 M MECHANIC 1 2 NO 2 2 WEEKS PARACENTRAL YES 1 FINGERNAIL POSITIVE - - - YES NO YES
47 67 M FARMER 1 2 NO 2 2 WEEKS PARACENTRAL YES 1 FINGERNAIL POSITIVE - - - YES NO YES
48 57 M FARMER 1 2 YES 2 2 WEEKS PARACENTRAL YES 1 FINGERNAIL POSITIVE - - - YES NO YES
49 69 M FARMER 1 2 YES 2 2 WEEKS PARACENTRAL YES 1 FINGERNAIL POSITIVE - - - YES NO YES
50 67 M FARMER 1 2 YES 2 3 DAYS PARACENTRAL YES 1 FINGERNAIL POSITIVE - - - YES NO YES
-57 67 M FARMER 2 2 YES 1 3 DAYS PERIPHERAL YES 1 PLANT NEGATIVE - - - - NO YES
58 61 M FARMER 2 2 YES 1 3 DAYS PERIPHERAL YES 2 PLANT NEGATIVE - - - - NO YES
59 43 M OTHERS 2 2 YES 1 3 DAYS PERIPHERAL YES 2 PLANT NEGATIVE - - - - YES NO
60 52 M OTHERS 2 2 YES 1 3 DAYS PERIPHERAL YES 2 PLANT NEGATIVE - - - - YES NO
61 51 M OTHERS 2 2 NO 1 3 DAYS PERIPHERAL YES 2 PLANT NEGATIVE - - - - YES NO
62 61 M OTHERS 2 2 YES 1 1 MONTH PERIPHERAL YES 2 ANIMAL NEGATIVE - - - - YES NO
63 56 M OTHERS 1 2 YES 2 1 MONTH PERIPHERAL YES 2 ANIMAL NEGATIVE - - - - YES NO
64 44 M OTHERS 1 2 YES 2 1 MONTH PERIPHERAL YES 2 ANIMAL NEGATIVE - - - - YES NO
65 31 M OTHERS 1 2 NO 2 3 DAYS PERIPHERAL YES 2 ANIMAL NEGATIVE - - - - YES NO
66 58 M OTHERS 1 2 YES 2 3 DAYS PERIPHERAL YES 2 ANIMAL NEGATIVE - - - - YES NO
67 67 M LABOURER 1 2 YES 2 3 DAYS CENTRAL YES 2 METAL FB NEGATIVE - - - - YES NO
68 66 M LABOURER 1 2 YES 2 3 DAYS CENTRAL YES 2 METAL FB NEGATIVE - - - - YES NO
69 77 M LABOURER 1 2 NO 2 3 DAYS CENTRAL YES 2 METAL FB NEGATIVE - - - - YES NO
70 60 M LABOURER 1 2 NO 2 1 MONTH CENTRAL YES 2 METAL FB NEGATIVE - - - - YES NO
71 50 M LABOURER 1 2 NO 2 1 MONTH CENTRAL YES 2 METAL FB NEGATIVE - - - - NO YES
72 49 M LABOURER 1 2 NO 2 1 MONTH CENTRAL YES 2 METAL FB NEGATIVE - - - - YES
-73 49 M LABOURER 1 2 NO 2 1 MONTH CENTRAL YES 2 METAL FB NEGATIVE - - - - YES
-74 48 M LABOURER 1 2 YES 2 1 MONTH CENTRAL YE