CERTIFICATE
This is to certify that dissertation entitled ‘A PROSPECTIVE STUDY ON
LAPAROTOMY WOUND INFECTION’ is a bonafide record of work done by
Dr. JAMSHEER V. T in the Department Of General Surgery , THANJAVUR
MEDICAL COLLEGE, THANJAVUR , during his post graduate course from
2015-2018 under guidance and supervision of Prof. DR. V.KOPPERUNDEVI MS ,
DGO & PROF. DR.M. ELANGOVAN, MS ., FICS ,this is submitted in partial
fulfilment for the award of M.S. DEGREE EXAMINATION- BRANCH I
(GENERAL SURGERY) to be held in MAY 2018 under the TAMILNADU
DR. M.G.R. MEDICAL UNIVERSITY, CHENNAI.
DR.V.KOPPERUNDEVI, MS.,DGO PROF.DR. M.ELANGOVAN M.S., F.I.C.S Associate Professor & Chief, Professor and Head of Department,
Department of General Surgery, Department of General Surgery, Thanjavur Medical College, Thanjavur Medical College, Thanjavur Thanjavur
The Dean,
DECLARATION
I declare that this dissertation entitled ‘A PROSPECTIVE STUDY ON
LAPAROTOMY WOUND INFECTION’ is a record of work done by me in
Department of General Surgery , Thanjavur Medical College , Thanjavur ,
during my post graduate course from 2015-2018 under the guidance and
supervision of my unit chief DR.V. KOPPERUNDEVI, MS, DGO and
PROF AND HEAD OF DEPARTMENT, PROF .DR M. ELANGOVAN, MS.,
FICS .It is submitted in partial fulfilment for the award of MS DEGREE
EXAMINATION-BRANCH 1 (GENERAL SURGERY) to be held in may
2018 under the TAMIL NADU DR.MGR MEDICAL UNIVERSITY
,CHENNAI. This record of work has not been submitted previously by me for the
award of any degree or diploma from any other university
THANJAVUR DR.JAMSHEER V.T
ACKNOWLEDGEMENT
I express my extreme gratitude to Prof. Dr. M.ELANGOVAN M.S., F.I.C.S.,
Professor and the Head of the Department of Surgery, for his constant guidance
and suggestions throughout my study period.
I express my extreme gratitude to Dr. V. KOPPERUNDEVI, M.S.,DGO
Associate Professor and my Unit Chief, for her valuable guidance and
encouragement during my study period.
I express my profound gratitude to Asst Prof., Dr.V.PANDIYAN MS.,
Dr. THIVAGAR MS, Dr.SARAVANAN M.S for their valuable guidance and
encouragement.
I owe thanks to all ASST.PROFFESSORS OF DEPARTMENT OF
SURGERY for their valuable guidance
I thank DEAN, THANJAVUR MEDICAL COLLEGE for permitting me to
use the hospital facilities for my study .
I express my sincere thanks to all patients, who in spite of their physical and
mental sufferings have co-operated and obliged to my request for regular follow
CONTENTS
1. INTRODUCTION 1
2. AIMS AND OBJECTIVE OF STUDY 3
3. REVIEW OF LITERATURE 4
4. MATERIALS AND METHODS 28
5. OBSERVATION AND RESULTS 33
6. DISCUSSION AND CONCLUSION 55
7. BIBLIOGRAPHY
8. PROFORMA
INTRODUCTION
Laparotomy or celiotomy is a surgical procedure in which incision is put on abdominal
wall in order to approach intra-abdominal or abdominal wall pathologies. Laparotomy
etymologically originated from the Greek word LAPAROS , which means soft or
loose. Pioneer in laparotomy was Ephraim in 1809. He performed surgery without any
anaesthesia. Christian Albert Theodor Billroth(1) is known as the father of abdominal
surgery. He had done the first successful gastrectomy for pyloric cancer.
Even though laparotomy is a very common surgical procedure, we may have to
encounter many difficulties in both intraoperative and post- operative period. Surgical
site infection is one of the most common post-operative complication in laparotomy
patients. The end result of laparotomy not only depend upon the severity of underlying
illness but also depends upon abdominal incisional wound healing. Delay in wound
healing leads to increased duration of hospital stay and also the hospital expenses.
According to one study, there is an average increase of 7.3 days of hospitalisation which
is caused by surgical site infection.(2)
From patient perspective, surgical site infection cause both prolongation of ill health
and increase the mental agony about his disease. From surgeon’s perspective, even
though surgical site infection are inevitable it can be minimised to a very good extend if
SSI not only increase length of hospital stay but also contribute to morbidity and
mortality . It also causes physical and psychological trauma to the patient ; ultimately
OBJECTIVES
• To analyse incidence of wound infections
• To identify most common organisms
• To determine the relationship of post-operative wound infection with certain
predisposing factors
LITERATURE REVIEW
BASIC ANATOMY OF ANTERIAL ABDOMINAL WALL
It is bounded by superior process and costal margin posteriorly by vertebral
column and inferiorly by upper part of pelvic bone. Its layers consists of skin, superficial
fascia, muscle and their deep fascia, extra peritoneal fascia and parietal peritoniam.
SUPERFICIAL FASCIA
Consist of,
• Superficial fatty layer of camper
• Deep membraneous layer of scarpa
MUSCLES OF ANTERIOLATERAL ABDOMINAL WALL
There are 5 muscles in anteriolateral group of abdominal wall. 3 flat muscles,
which includes external oblique, internal oblique and transversus abdominis. 2 vertcal
muscles near midline which are enclosed within tendinous sheat followed aponeurosis of
TECHNICAL CONSIDERATION REGARDING ABDOMINAL INCISION
VERTICAL INCISIONS
MIDLINE INCISION
It gives rapid access to and, adequate exposure of almost every region of
abdominal cavity and retroperitoneum. It is typically associated with little blood loss and
does not require transection of muscle fibre or nerves. Upper midline incision provides
adequate exposure to oesophageal hiatus, abdominal easophagus, vagus nerves, stomach,
duodenum, gall bladder, pancreas and spleen. Lower midline incision provides exposure
PARAMEDIAL INCISION
Paramedical incision are vertical incisions placed either to the right or left of the
midline on abdominal wall. During creation of paramedical incision of lower abdominal
wall, the inferior epigastric vessels may be encounters and must be ligated prior to
C
SSI (SURGICAL SITE INFECTIONS)
Surgical site infections are infections arising at the site of previous surgical procedure,
which detected before 30 days. Depending upon the depth of infection it is divided into 3
categories. Superficial incisional SSI (above facial layer) ,deep incisional SSI and organ
space infection. Deep incisional SSI and organ space infections are together called
complex surgical site infections .Stich abscess is not included under SSI. Even though
some sort of erythema is expected at the surgical site , peri-incisional pain and
tenderness, expansion of erythema, purulent discharge from surgical site should raise the
suspicion about development of surgical site infections and should be properly intervened
and treated. Most common nosocomial infection in surgical patients is SSI and each SSI
CLASSIFICATION OF WOUNDS
Depending on extend of Wound contamination, National Research Council put forward a
wound classification scheme in 1964, which includes 4 classes of wounds
CLEAN:
Uninfected surgical wound in which no inflammation is encountered,
clean wounds are closed primarily
Examples:-
• exploratory laparotomy
• non-penetrating blunt trauma
• neck surgery
• thyroidectomy
CLEAN CONTAMINATED:
Procedures involving GI or respiratory tract with no significant contamination.
Examples:-
• small bowel resection
• whipple procedure
• routine appendectomy
• cholecystectomy
CONTAMINATED:
Examples:-
• appendectomy for inflamed appendicitis
• bile spillage during cholecystectomy
• diverticulitis.
DIRTY OR INFECTED:
Acute bacterial inflammation found, pus encountered, devitalised tissue encountered.
Example:-
• incision and drainage of abscess
• peritonitis
• bowel perforation.
Wound classification has an important role in predicting risk of post op SSI. But some
studies indicates this classification alone is inaccurate.
There many better scoring system to calculate risk of SSI, commonly used are SENIC
(STUDY OF EFFICACY OF NOSOCOMIAL INFECTION CONTROL) & NNIS
(NATIONAL NOSOCOMIAL INFECTION SURVEILLANCE) Risk index
4 features are used in SENIC scoring
1. surgery more than 2 hours
2. 2 abdominal surgery
3. 3 wound class 3 /4
SENIC SCORE AND RISK OF SSI
• 0…..1%
• 1…….3-6%
• 2……9&
• 3…….17%
• 4…….27%
NNIS uses 3 instead of 4 variables which includes(3)
• ASA more than 2.
• Prolonged duration of surgery
• Wound class III/IV
SOUTHAMPTON WOUND GRADING SYSTEM FOR WOUND HEALING
0) Normal healing
1) Normal healing with mild arythema
a) Some bruising
b) Considerable bruising
c) Mild arythema
2) Erythema with other signs of inflammation
a) At one point
b) Around sutures
d. Around wound
3) Clear or hemoserous discharge
a) At one point
b) Along wound
4) Pus
a) At one point
b) Along wound
5) Deep or severe wound infection with or without wound infection, heamatoma
The ASSEPSIS wound score additional treatment
Crieteria points
Additional treatment 0
Antibiotics for wound infection 10
Drainage of pus under Anastasia 5
Debridement of wound under general Anastasia 10
Serous discharge daily 0-5
Erythema daily 0-5
Purulent exudate daily 0-10
Separation of deep tissue daily 0-10
Isolation of bacteria from wound 10
Stay as inpatient prolonged more than 2 weeks 5
ANTIBIOTICS PROPHYLAXIS
Recommended antibiotics prophylaxis (university of CINCINNATY hospital) for
colorectal surgery is cefazoline plus metronidazole and hepatobiliary surgery are
piperaziline. For maintaining adequate plasma concentration of drug we may have to
repeat the dosage especially in long duration surgical procedures
Antibiotics should be administered 30-60 min before planned incision.
Antibiotic prophylaxis is recommended in patients with class 2,3,4& in class 1 with other
RISK FACTORS FOR DEVELOPMENT OF SSI
(4)1. PATIENTS FACTORS
• Ascites (abdominal surgery
• Corticosteroid therapy(controversial)
• Obesity
• Diabetes
• Extremes of ages
• Hypocholesterolemia
• Hypoxia
• Postoperative anaemia
• Remote infection
• Under nutrition
2. ENVIRONMENTAL FACTORS
• Inadequate sterilisation
• Inadequate ventilation
• Inadequate skin antisepsis
3. TREATMENT FACTORS
• Drains
• Emergency procedure
• Hypothermia
• Oxygenation
• Prolonged operative time
• Prolonged preoperative hospitalisation
AGE
Old age patients are more prone for delayed wound healing which is due to reduced
re-epithelisation of skin, they may be having multiple comorbidities which may affect
collagen replacement after abdominal surgery.(5)
DIABETES
Diabetes associated with small vessel disease, neuropathy, altered glycaemic control(6)
all of which are predisposed to alteration in normal wound healing pathway. Common
problems seen in diabetes are increased risk of infection, delayed epithelialisation,
alteration in collagen synthesis and granulation tissue formation. In diabetes, matrix
metalloprotien function are also altered which are integral component of wound healing
IMMUNODEFICIENCY
Immunocompromised state ( old age , malnourishment, cancer, HIV) can also result in
poor wound healing.
OBESITY
Even though extensive studies carried out over this factor it has only a weak
LENGTH OF PRE-OPERATIVE HOSPITALIZATION
When the duration of preoperative hospitalisation period increases risk of SSI also
increases .It is thought to be via bacterial colonization especially with resistant organism
there evidence from 5 & 10 year studies by Cruse and Foord and the study by Mead et al
support this, but both of these studies didn’t consider comorbidities , skin flora and
organisms identified from culture. So the association between length of pre-operative
hospitalization & SSI is less significant
PRE-OPERATIVE SKIN PREPARATION
In 1971 Serropian and Reynolds studied surgical site infections in various types of skin
preparation ; which showed of 5.6% after razor shaving and 0.6% after depilator use and
0.6% after no hair removal (7) Alexander et al investigated on 1013 patients ; done an
RCT ; observations revealed that morning clipping showed lowest incidence (3.2%) and
others were significantly high (8). Mechanism of surgical site infections is because skin
aberration that may get infected by proliferative microorganisms. In contrary to our
common belief some studies even tell no need for skin preparation. If skin preparation is
indicated skin clipping is ideal
PROLONGED OPERATIVE TIME
Duration of surgery is also an independent factor which determines surgical site
infections. ( 9) especially if duration more than 2-3 hours
PERI-OPERATIVE FACTORS
Normothermia and absence of hypothermia increase tissue perfusion and helps in
TREATMENT FACTORS
Treatment with drugs such as steroids, NSAID, anti-cancer / antimitotic drugs, radiation
(RT) can also affect wound healing adversely. Ill effect of steroid on wounds planned for
secondary and tertiary wounds can be reduced by topical application of vitamin A.
antimitotic drugs and radiation therapy impedes cell cycle in rapidly dividing cells.
Moreover malignancy may also present with malnourishment or cancer cachexia.
Administration enteral nutritional support improves healing in malignancy
REMOTE SITE INFECTION
In 1976, study conducted by Edward (by including 1865 patients) shown a
epidemiological correlation between remote site infection and SSI. Especially in case of
UTI. But it is not recommended that the treatment of above conditions are mandatory
prior to surgery (10).
MALNOURISHMENT
In 1995 Rhodes and Alexander studied about correlation between malnourishment and
wound healing especially emphasising on hypo proteinemia, by taking serum protein less
than 6.3 as the cut off. Ehrenkrenz could not establish similar outcome as Rhode’s study,
they used patients with albumin values upto 2.8 mgs/dl, 2.8-3.4 mg/dl and more than 3.4
mg/dl.
MALIGNANCY
The presence of Malignancy and associated immunity reduction also considered to
be a risk factor for surgical site infection. Studies, however shows variable reports
444 Gastric surgery did not find any independent association between malignancy and
wound infection (11) where as Claesson and Holmlund observed a rate of 17% versus
4.5% of SSI in malignant & non malignant cases respectively.(12)
DETERMINANTS OF WOUND INFECTION
Two important predictors of SSI are:
• bacterial Contamination.
• Host resistance
A formula derived by Culberson and Altemier to predict SSI is,
This formula explains the positive correlation between risk of SSI with bacterial load and
its virulence
Dose of Bacterial Contamination x Virulence
Risk of surgical wound infection = ______________________________
Host resistance
EXOGENOUS FACTORS
Surgeons Hands
There are various types of antiseptics used for scrubbing most commonly used are
Povidone – Iodine and Chlorohexidine which are effective against both gram +ve and
gram –ve organizisms. The variation comes in the length of the scrub which might vary
GLOVE PUNCTURE
Among studies regarding glove puncture the important 2 studies are conducted by
Cruse and Foord, Whyte Et Al, both of these studies shows there is no increase of SSI
showing glove puncture and it is thought to be due to preoperative scrubbing. So glove
puncture is not considered to be a serious factor in development of SSI.
EMERGENCY PROCEDURES
An important study conducted by Garibaldy et al compared the incidence of SSI
between emergency vs elective procedures. Wound infections shows an odds ratio of 7.6(
CI 95% 3.2-18.2) for emergency vs elective surgeries. After multivariate analysis of this,
it was found to be insignificant.(14). So, Emergency operations by themselves are not
considered to be a predisposing factor to development of SSI.
PROCEDURE DURATION
As the duration of surgery increases the chance for SSI is also high. Especially if the
procedure duration is more than 2-3 hrs. there are many studies regarding this topic.
Examples, Cruse and Foord, Garibaldy and et al, Haley et al, Culver et al. among this
Haley et al studied more than 55000 and found that duration of surgery more than 2 hrs is
the 2nd greatest risk factor for development of SSI. In our study we grouped surgical
OPERATING SURGEON
In any institution surgery is commonly done by different category of doctors
ranging from intern or trainee surgeon to consultant surgeon or chief surgeon. Most of
studies shows that it is not an easy task to compare SSI rate among various group of
surgeons due to multifactorial reasons. One of the possible way to tackle these is studying
surgeon’s specific infection rate. Even though assessment is difficult, operating surgeon
WOUND CATEGORY
WOUND CATEGORY
In 1964 National Research Council proposed a wound classification system in
which all the wounds are classified from grade 1-4 depending upon the wound
contamination. For comparison purpose in our study we combined grade 3 and grade 4
together.
Table 4(A) Table on wound infection rates among various studies.
Institution Year(s)
Sample
size Class infection rate % of
(No, of patients) I (%) II III Overall Incidence Foot Hills
Hospital, Canada 1967-77 62939 1.5 7,7 15.2/40 4.7
MPLS VALC 1977-86 40915 1.4 2.8 8.4 2.5
SENIC 1975-76 59352 2.9 3.9 8.5/12.6 4.1
NAS-NRC 1964 15613 5.1 10.8 16.2/29 7.5
Category I : Clean
Category II : Clean – Contaminated
Category III : Contaminated and Dirty
Wound contamination is the single most predictor of development of SSI. So the
classification proposed by National Research Council is a very reliable tool for prediction
[image:33.612.78.530.284.615.2]SURGICAL DRAPES
Drapes are used for isolating operating area from other body part. Commonly used
surgical drapes are cotton drapes, pre-fabricated drapes and plastic drapes. The issue we
encounter with cotton drapes are bacteria can pass from unsterile area to sterile area once
the drape is wet. While using adhesive plastic drapes there is increased chance of
infection due to proliferation of bacteria by sweating beneath plastic drapes( 17).
OTHER FACTORS AFFECTING THE INCIDENCE OF WOUND INFECTIONS
Some other factors to be considered for [proper wound healing and prevention of
SSI are, achieving complete haemostasis, adequate blood supply to the wound, dead
space obliteration, tensionless suturing.
POST OP SURVIELLANCE
Wound infection, review is incomplete without proper surveillance. Proper
surveillance has shown to be an important factor reducing SSI in many studies. So many
surgical societies and disease control centers set recommendations to reduse SSI to the
MATERIALS AND METHODS
SETTING
This prospective study was conducted at TMCH ( Thanjavur Medical Collage and
Hospital ,Thanjavur) during the period of september 2016-september 2017.
SAMPLE POPULATION
Those patients underwent major laparotomy during above mentioned period are included
in this study, patients undergoing appendectomy, laparoscopic surgery, those who are not
willing for participating in study and those patients who are morbidly ill are excluded
from the study.
DATA RECORDING
Data recording done using proforma, a sample of which is enclosed in appendix I,
collection of date was done by M. S PG of department of surgery.
CLASSIFICATION OF CASES
Patients were grouped into 3 categories as mentioned earlier. Clean, contaminated and
PROCEDURE DONE
Laparotomy was done for various abdominal pathologies. They are categorized as
follows.
Intestinal obstruction
Hollow viscous perforation
Uppere GI surgeries )such as gastrectomy TV GJ cholecystemy)
Colorectal surgeries ( such as LAR/APR…)
Gynaecological pathology
Other procedure such as iliostomy reversal.
NATURE OF PROCEDURE
Depend on nature of procedure they are categorized into emergency or elective
procedure.
RISK FACTOR CATEGORIZATION
Depending upon the nature of risk factor, categorized into general or local risk factors.
General factors includes, presence of anemia, diabetis, TB and malignancy. Local risk
factors includes URI, LRI and UTI.
PER OPERATIVE FACTORS
DURATION OF SUREGERY
Time taken from induction of Anastasia to skin closure is considered here. We have
categorized into 3 groups. Less than 1 hr, 1 -2 hr, more than 2 hr.
PERFORMING SURGEON
In order to assess the role of performing surgeon in the incidence of SSI, we have
categorized performing surgeons into 3 groups. Chief or assistant professor or post
graduate.
ANTIBIOTICS
The role of antibiotic study in 2 different timings pre- and per operative. Pre operative
antibiotic usage could have been deliberate as in contaminate, pre- contaminate case and
incidental if patients had been known antibiotics for some other reasons such as
respiratory tract infections or UTI. Per operative antibiotics is given in patients as part of
prophylactic hygiene or if there is any gross unexpected contamination or in situations
where undue prolongation of surgery has occurred
IDENTIFICATION OF SSI (in the post operative period)
based on both clinical and microbiological findings SSI was diagnosed
CLINICAL CRITERIA
Clinical features used are progressive redness, swelling, tenderness, with or without
constitutional symptoms. Fever with more than 100 degree Fahrenheit was taken as
MICROBIOLOGICAL ANALYSIS
Serous or serosanguinous discharge were sent for microscopy, culture and sensitivity at
the time of detection. If any organism grove in the sample they were classified in infected
group. Even in the absence of other clinical signs. In the absence of above set criteria the
case were taken as not infected. If both clinical and positive culture was present then also
it was taken as infected.
ANALYSIS IN INFECTED CASES
Among infected cases day of detection, method of detection and organism grown and
outcome were studied.
DAY OF DETECTION
The day in which above said clinical characteristics present or the sample sent from a
suspected discharge which subsequently found to be positive was taken as day of
detection. If both clinical and microbiological criteria are met then whichever is earlier is
taken as day of detection
METHOD OF DETECTION
ORGANISMS GROWN
There are 6 categories in this variable.
1) No growth
2) Staphylococcus and streptococcus species
3) Klebsiella and E-coli
4) Pseudomonas
5) Citrobacter
6) Others
OUTCOME
Depend upon whether the case is resolved or not.
RESOLVED: symptoms and signs subsided following either drainage of abscess or by
proper administration of antibiotics. This group also includes infected wounds healed,
even following secondary suturing.
NOT RESOLVED: this group comprises patient went for septicaemia, fistula formation,
wound dehiscence or cutaneous gangrene.
STATISTICAL ANALYSIS
In our study we used excel software and epi info statistical package (version 6.04 ,
WHO and CDC) this factors for development of SSI were identified using Univariate
analysis. Hypothesis was tested using Chi square and Fischer’s test. Statistical
RESULTS
TABLE 6(A)
INCIDENCE OF SSI
TABLE 6(A). DISTRIBUTION OF WOUND INFECTION (n = 323)
Wound Frequency Percentage
Not Infected 286 88.6
Infected 37 11.4
Total 323 100
Total no. of patients included in the study was 323.
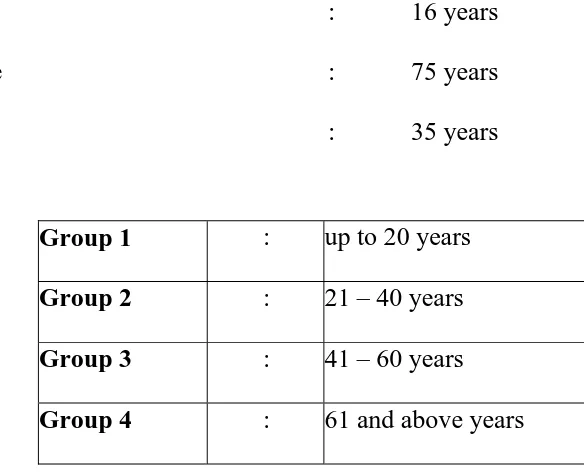
[image:40.612.196.470.238.397.2]TABLE 6(B )
DISTRIBUTION OF AGE OF PATIENTS
Our sample had a cut off of minimum age of 16 and maximum age of 75 with a median
age of 35.
Minimum Age
Maximum Age
Median
:
:
:
16 years
75 years
35 years
Group 1 : up to 20 years
Group 2 : 21 – 40 years
Group 3 : 41 – 60 years
Group 4 : 61 and above years
For analysing patients with different age groups patients
[image:41.612.150.442.198.434.2]TABLE 6(B):
FREQUENCY DISTRIBUTION AS FOLLOWS
Age Group Frequency Percentage
1 48 15.1 2 150 46.1 3 96 13.0
4 29 9.0
[image:42.612.169.467.223.472.2]6(C) DISTRIBUTION OF SEX IN PATIENTS [n = 323]
In the primary data collection. Individual Surgeries were entered. While analysing for
Frequency of distribution and Risk Association subsequently they were grouped broadly
under 6 categories
Table 6( C) Sex Distribution
Sex Frequency Percent
Male 255 78.8
Female 68 21.2
Total 323 100
6(D) TYPE OF SURGERY PERFORMED [n = 323]
Type of laparotomy were broadly categorized into 6 groups depending upon the
aetiology
Category 1 – intestinal obstruction
Category 2 – hollow viscous perforation
Category 3 – upper GI surgery ( gastrectomy, TV GJ, Cholecystectomy)
Category 4 – colorectal surgeries( LAR/APR)
Category 5 – other gynaecological process
[image:43.612.210.406.224.353.2]TABLE 6(D)
DISTRIBUTION OF SURGERY PERFORMED.
Group Frequency Percentage
1 95 29.4 2 123 38.0 3 46 14.3 4 29 9.0 5 9 2.9 6 21 6.5
[image:44.612.214.452.197.478.2]TABLE 6(E) TYPE OF SURGERY [n = 323]
TABLE 6(E) DISTRIBUTION OF SURGERY BASED ON WOUND CLASS
Type Frequency Percent
Clean 193 59.6
Clean
Contaminated 79 24.5
Contaminated 51 15.9
[image:45.612.197.466.223.471.2]TABLE 6(F)
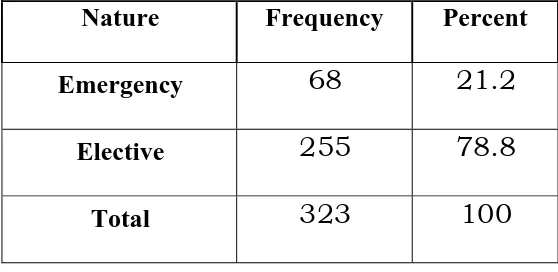
NATURE OF SURGERY [n = 323]
TABLE 6(F) – DISTRIBUTION OF EMERGENCY & ELECTIVE SURGERY
Nature Frequency Percent
Emergency 68 21.2
Elective 255 78.8
Total 323 100
The frequency of Emergency procedures as shown in Table 6(F) were 21.2% and that of
[image:47.612.193.472.196.332.2]TABLE 6(G)
RISK FACTORS
They were categorized into 2 groups – General and Local / Specific.
6(G).1 DISTRIBUTION OF GENERAL RISK FACTORS [n = 323]
TABLE 6(G)1 DISTRIBUTION OF GENERAL RISK FACTORS
Present Absent
Risk Factor Frequency Frequency
(%) (%)
Anemia 42 (13.1) 281 (86.9)
Diabetes 16 (4.9) 307 (95.1)
Tuberculosis 4 (1.2) 319 (98.8)
Malignancy 21 (6.5) 302 (93.5)
As shown in table 6(G)1 most prevalent risk factor were anaemia followed by malignancy
and diabetes mellitus. Other factors tuberculosis was very low in incidence. Hence it was
[image:48.612.89.503.283.530.2]TABLE 6(G)2
DISTRIBUTION OF LOCAL / SPECIFIC RISK FACTORS
[n = 323]
6.(G)2 – DISTRIBUTION OF SPECIFIC / LOCAL RISK FACTORS
Present Absent
Risk Factor Frequency Frequency
(%) (%)
UTI 20 (6.1) 303 (93.9)
URI 0(0) 323 (100)
LRI 21(6.5) 302 (93.5)
Table 6.(G)2indicates UTI and LRI were the most important risk factors followed by,
[image:49.612.191.492.224.454.2]TABLE 6(H).
ADMINISTRATION OF PRE-OP ANTIBIOTICS [n = 323]
TABLE 6( H) FREQUENCY OF ADMINISTRATION OF PRE-OP
ANTIBIOTICS.
Pre-Op.
Antibiotics
Frequency Present
Not Given 195 60.4
Given 128 39.6
Total 323 100
Table 6(H) shows that 128 cases were given pre op antibiotics for the indications
[image:50.612.194.484.194.449.2]6.(I) DURATION OF SURGERY [n = 323]
TABLE 6.(I)
DISTRIBUTION OF DURATION OF SURGERY
Duration Frequency Percent
< 1 hour 83 25.7
1 – 2 hours 144 44.5
>2 hours 96 29.8
As shown in Table 6(I) operations performed between 1-2 hrs were more. Comprises
[image:51.612.206.448.195.384.2]6.(J). OPERATING SURGEON[n = 323]
TABLE 6.(J) :
CASE DISTRIBUTION BASED ON OPERATING SURGEON
Done by Frequency Percent
Chiefs 54 16.7
Assistant Professor 169 52.2
PG 100 31.2
Table 6.(J) shows that 169 cases ( 61 %) of the cases were performed by assistant
professors, trainees performed 100 cases and chiefs performed 54 cases (16.3) . Most of
the cases performed by chief were ASA category 3, contaminated and those patients with
[image:52.612.144.470.195.348.2]6.(K) UNIVARIATE ANALYSIS FOR RISK FACTORS FOR SSI
TABLE 6(K) : RISK FACTORS FOR SSI
Sample Incidence
S.No Risk Factor Size Wound P value
Infection(%)
1. Sex 0.977
male 323 29/253(11.5)
Female 8/68(11.5)
2. Age 0.010*
Up to 20 0/48(0)
21-40 13/148(8.8)
41-60 323 17/96(17.8)
60 and above 7/29(22.7)
3. Surgical procedure 0.000*
1 8/94(8.3)
2 9/122(7.5)
3 323 10/46(22.9)
[image:53.612.73.541.160.713.2]5 0/9(0)
6 9/21(43.8)
4.
Type of
surgery
0.052
Clean 25/191(13.0)
Clean 323
Contaminated 3/79(3.3)
Contaminated 9/51(17.9)
5.
Nature 0.312
Emergency 11/68(15.4)
Elective 323 26/254(10.4)
6.
Anemia
0.424
Present 7/42(15.6)
Absent 30/279(10.8)
7.
Diabetes
0.633
Yes 3/16(16.7)
No 323 34/305(11.2)
Yes 0/4(0)
No 323 37/317(11.6)
9.
Malignancy
0.024*
Yes 7/21(31.3)
No 323 30/300(10.0)
10. UTI 0.018*
Yes
323 7/20(33.3)
No 30/301(10.0)
11.
LRI 0.004*
Yes 323 8/21(50)
6.(L).1 ANALYSIS OF INFECTED CASES [n = 28] DAY OF DETECTION OF WOUND INFECTION
TABLE 6.(L)1
DISTRIBUTION OF DAY OF DETECTION OF WOUND INFECTION
Day of Detection Frequency Percent
2 4 10.7
3 7 17.9
4 10 28.6
5 8 21.4
6 5 14.3
7 1 3.6
8 1 3.6
Total 36 100
As shown in Table 6.(K)1 POD 4 was the day in which highest no. of wound infections
[image:56.612.169.466.222.553.2]6.(L)2 METHOD OF DETECTION
TABLE 6.(L)2 : DISTRIBUTION OF METHOD OF DETECTION
Method Frequency Percent
Clinical 9 25
Clinical and Microbiological 27 75
Microbiological 0 0
Total 36 100
Table 6.(L)2 shows that clinical and microbiological detection combinely showed a
frequency of about 75% combining with clinical alone ( 25%) there was no case detected
[image:58.612.181.496.165.390.2]6.(L)C. ORGANISM CULTURED FROM WOUND (n = 21)
TABLE 6.(L)C : DISTRIBUTION OF ORGANISMS ISOLATED
Organism Frequency Percent
No Growth 1 3.5
Staph & Strep species 8
28.6
Klebsiella &
Escherichia
9 32.1
Pseudomonas 4 14.3
Citrobacter Spp. 3 10.7
Others
3 10.7
Total 28 100
As Table 6(L)3shows Escherichia & Klebsiella spp. Show a high frequency distribution.
[image:59.612.145.519.164.552.2]14.3 10.7 10.7 ORGANI 3.5 32.1 7
ISM ISOLAATED
28.6 N S K E P C O
No Growth taph & Strep s Klebsiella &
scherichia Pseudomonas Citrobacter Spp Others
species
6.(L)D OUTCOME OF WOUND INFECTION [n = 28]
6.(L) D: DISTRIBUTION OF OUTCOME OF WOUND INFECTION
As shown in Table 6(L)D around 93% of SSI cases resolved without any
sequel, whereas 2 cases went for other complications.
Outcome Frequency Percent
Resolved 34 92.9
Not-Resolved 2 7.1
DISCUSSION
7(A) INCIDENCE OF SSI (SURGICAL SITE INFECTION)
7.(A).1 Overall Incidence of SSI
The incidence of SSI in the present study is 11.4% which is
High as compared to other studies.
Table 7(A) : Comparison of Incidence of wound infection
CLASS INFECTION
STUDY OVERALL RATE (%)
I II III
MPLS – VAMC 2.5 1.4 2.8 8.4
Foothills Hospital 4.7 1.5 7.7 15.2/40
NAS – NRC 7.5 5.1 10.8 16.2/29
SENIC 4.1 2.9 3.9 8.5/12.6
[image:62.612.102.498.319.594.2]COMPARISION OF OVERALL INCIDENCE OF SSI
2.5
4.7
7.5
4.1
11.4
0 2 4 6 8 10 12
INCIDENCE- CATEGORY WISE
1.4 1.5
5.1
2.9
13
0 2 4 6 8 10 12 14
MPLS – VAMC Foothills Hospital NAS – NRC SENIC PRESENT
0 2 4 6 8 10 12 2.8
MPLS – VAAMC Footh
7.7
hills Hospital
clean
10.8
NAS – NR
n
contam
0 2 4 6 8 10 12 14 16 18 20 8.4
MPLS – VAMC
1
C Foothill
15.2
s Hospital
Con
16.2
NAS – NRC
7(A)2 INCIDENCE OF WOUND INFECTION CATEGORY WISE
• The Incidence among clean contaminated group(3.3%) and contaminated
group(17.9%) categories compares similar to other studies ; but Incidence of clean
case group were (13.0%) is very high which may be the reason for high overall
incidence (11.0%).
• The reason behind this issue may be due to observer bias , Intern &Trainee were
first to examine the wound, they might have over diagnosed rate of SSI. Especially
in clean cases where pre or intra opetrative antibiotics were not given
7(B) RISK FACTORS FOR WOUND INFECTION
7.(B)1. AGE AND SEX:
In our study the incidence among both male and female were almost similar.(11.4 % vs
11.5%) hence it is well proved that sex does not appear to be a risk factor for
development for SSI. As other studies age has a strong positive correlation with
less than 20 years vs patients more than 6 years with a p value of 0.01. which is
statistically significant.
7.(B)2. SURGICAL PROCEDURE:
Surgical procedure were arranged into 6 groups based on the aetiological factor behind
laparotomy. These surgical procedure categories had a strong correlation with
development of SSI with a p value of 0.000. among the 6 categories ileostomy or
colostomy reversal had a high incidence of SSI. The underlying factor may be faecal
contamination, malignancy and malnourishment following incomplete absorption of food.
In category 3( upper GI surgeries, gastrectomy TV GJ, ) wound infection rate were high
since many of the cases were having malignancy. There are very few SSI in
gynaecological related laparotomy may be due to sterile nature of ovarian or uterine
pathology.
7.(B) 3 TYPE OF PROCEDURE (BASED ON WOUND CLASS)
In our study wound category based on wound contamination is both an important risk
0.0152, it is not statistically significant risk factor, which might be due to discrepancy in
incidence among clean cases compared with other studies.
7.(B)4 NATURE OF SURGICAL PROCEDURE
Emergency surgery shows higher rate(15.4%) of SSI as compared with elective
procedure(10.4%). The results are expected since many of the emergency cases are
having clean contaminated class and also have pre existing illness such as LRI or UTI. As
Garibaldi et al. the emergency procedures by themselves do not function as a risk factor.
Our studies also shows parallel results in this regard.(19)
7(B).5 ANALYSIS OF ANEMIA, DIABETES MELLITUS, TUBERCULOSIS
AND MALIGNANCY AS RISK FACTORS.
Among the variables mentioned Malignanc is havinh striong association as a risk factor
7.(B).6 ANALYSIS OF UTI, LRI, FOCUS OF INFECTION AS RISK FACTOR.
Among UTI incidence wer (33.3 %), LRI (37.5%) with p value of 0.018, 0.004
respectively showed a strong association for development of SSI which is statistically
very significant
7.(B)7 DURATION OF SURGERY
In many studies SSI is directly proportional to rate of duration of surgical procedure . In
our study higher incidence is seen in surgeries performed between 1-2 hr than in other
categories. It would be better to remember that in our study duration was set arbitrarily,
which was not on the lines of recommended in recent literature. The observations not
fully support above said statement as there is less no.of cases done in more than 2 hrs.
Also evaluates 0.342 . anyhow increase in incidence among less than 1 hr group to 1-2 hr
group from 9.6 to 14.7% shows that duration of surgery is significant risk factor for
7.(B)8 OPERATING SURGEON
Our study shows higher incidence of SSI in surgeries perfiormed by chiefs as compared
to other groups with a p value of 0.487. it is both statistically insignificant and most of the
surgeries done by chiefs are coming under high risk surgeries like patients with
pre-existing illness, ASA categpory 3, malignancy, grossly contraminated cases, etc. the
surgeries done by trainees shows least incidence( 8.1%) maybe due to uncomplicated
cases they are doing.
7.2.9 ANTIBIOTICS:
According to our study preoperative antibiotic exposure group showed a strong
association with development of SSI(p value 0.015) the reason is supposed to be due to
antimicrobial resistance to antibiotics or also due to inadequate infection control
7.(C)ANALYSIS OF INFECTED CASES:
Which include day of detection, method of detections, organisms isolated and outcome of
7.(C).1 DAY OF SSI DETECTION
Around half of the cases are diagnosed on day 4. 26.6% and day 5 . most of the cases are
detected in first week of surgery. The most delayed SSI ditection was on POD 8
7(C).2 METHOD OF DETECTION
In our study we have used 3 ways for diagnosing SSI as in table 6(L)2 there is no clinical
case categorized under microbiological means alone. Clinical diagnosis was upto 25% of
the cases. There is also an expected inter observer bias in clinical detection of SSI s we
have explained earlier.
7(C).3 ORGANISMS ISOLATED
27 out of 36 case were found to have positivity to micro organisms. The result showed
following observations. Klebsiella, e-coli species were positive about 1/3rd cases and
staph and strep comprised about 28.6%. combining all these 4 organisms comes about
7.(C)4 OUTCOME OF SSI
In our study 34 out of 36 cases resolved without any sequele. In other 2 cases one
got septicaemia and another got enterocutaneous fistula. Limiting factor in our study is
diagnosis and observations made by a group of people. Diagnosing a wound infection
may have high interobeserver bias which may leads to statistical variations. Which is
more pronounced while diagnosing SSI in clean cases, even before diagnostic criteria
written earlier developed fully, we are forced to start antibiotics to treat development of
infection. This overdiagnosis purely on clinical grounds maybe the cause of certain
results in our study, such as increase incidence among week cases, advancement in day of
SUMMARY AND CONCLUSION
• Our study on post laparotomy wound infection was carried out for a span of one
year duration on a sample size of 323 patients an overall incidence of 11.4 % (36
out of 323) had SSI classwise categorization were bbased on National Reasearch
Council Adhoc Committee showed 13% clean, 3.3 % clean contaminated and
17.9% in contaminated cases.
• Factors which influence wound infection shows the following observations in our
study.
• The factors considered are age , sex ,co morbidities , type of surgery, nature of
surgery, duration of surgery, aetiology for laparotomy and performing surgeon.
• Sex was not having a difference in incidence rate in development of SSI.(incidence
• Increasing age showed a strong association for the development of SSI. Under age
20 the development of SSI was 0% whereas age over 61 has an incidence of 22.7%
with a p value of 0.01, which is statistically significant.
• 2 categories of pre-existing illness we have studied which includes general and
local/specific factors. Anaemia, TB ,malignancy and diabetes were the general
factors we analysed.
• Malignancy showed a high incidence of SSI.(31.3%) as compared with other
group (10%) with a p value of 0.024. which is statistically significant. Diabetes,
TB , anaemia did not show any statistically significant association for development
of SSI.
• UTI and LRI were categorized under local/ specific factors, analysed as a risk
factor for development of SSI. They showed a p value of 0.018, 0.004
• Various aetiological factors which result in laparotomy were having a p value of
0.000 showed that it is/ statistically significant risk factor for development of SSI.
Highest incidence is seen in category with ileostomy / colostomy reversal group
which maybe due to malnouriushment by underlying malignancy or reduced food
absorption due to inadequate length of bowel and fecal cointamination. Category
3( upper GI surgeries, gastrectomy TV GJ, ) wound infection rate were high since
many of the cases were having malignancy.
• There are very few SSI in gynaecological related laparotomy may be due to sterile
nature of ovarian or uterine pathology.
• When we are comparing emergency surgery vs elective surgery incidence of
wound infection were 15.4 vs 10.4. the analysis had a p value of 0.312 which was
• Regarding duration of surgery and performing surgeon did not show any positive
correlation with development of wound infection because their p value were 0.342
and 0.487 respectively.
• We found incidence of SSI in clean ,clean contaminated and contaminated were
13%,3.3%, 17.09% respectively. Bias in overdiagnosing wound infection is
supposed to be the reason for this variation.
• Antibiotic resistance and inadequate control of previous infections such as LRI and
UTI maybe the reason why the patient with preoperative and perioperative cases
had a strong association with SSI (p value of 0.015 which is statistically
significant).
• Out of 36 infected cases 34 had complete resolution with pour treatment . POD 4
was the day on which most of the infections were diagnosed, diagnosis were made
common organisms identified as aetiological agents in development of SSI were e
CONCLUSION
• Our study shows a group wise incidence ratio of SSI were 13.0%, 3.3%, 17.9% in
category 1 (clean) , category 2( clean-contaminated) and category 3 (contaminated
& dirty cases respectively). And combined incidence ratio is 11.4%
• Variables like sex , wound category, nature of surgery (emergency / elective) ,
surgery duration, TB (pulmonary tuberculosis) , Diabetes Mellitus or Anaemia did
not associate strongly with wound infection.
• The variables which showed a strong correlation with SSI are increasing age, type
of surgery, associated malignancy ,UTI(urinary tract infection) & LRI (lower
respiratory tract infection)
• Out of Infected group [N = 36]
• 92.9% had complete resolution, 7.1% had post SSI sequele
• Post operative day -4 recorded maximum SSI
• Similar to literature common bacterial agents are Staphylococcus and
BIBLIOGRAPHY
1.Maingot’s abdominal operations 12th edition, Page No. 3
2.Mangram AJ, Horan TC, Perlson ML, Guidelines for prevention of SSI, 1999
3.Gayness RP, Culver DH, Horan TC Et Al, SSI rates in US 1992-1998
4.Sabiston Textbook of Surgery The Biological Basis of Modern Surgical Practice,
20th Edition
5.Frantz MG, Robston MC, Steed DL Guidelines to Aid Healing of Acute Wound by
Decreasing Impediments of Healing. Wound Rep Reg 2008.
6.Pomposelli JJ, Baxter JK, 3rd, Babineau TJ, et al: Early postoperative glucose
control predicts nosocomial infectionrate in diabetic patients.
7.Ameracan Journal of Surgery, 1971- ;121, Seropian R, Reynolds BM Wound
Infection after preoperative depilator versus razor preparation.
8.Alexander JW. Fischer JE, Boyalian M. The influence of hair removal methods on
wound infection. Arch Surg 1983 ; 118 : 347.
9.Cruse PGE Foord F The Epidemiology of Wound Infection: A 10 year prospective
study of 6-9 Wounds
10. Edwards LD, The epidemiologist of 2056 remote site infections and 1966
surgical wound infection occurring in 1865 patients. A four year study of 40,923
operations at Rush-prebysterin – St.Lukes Hospital Chicag. Ann Surg, 1976 ; 184 :
11. Lewis RT. Wound infection after gastroduodenal operations, A 10 year review.
Can J surg, 1977;20 : 435.
12. Claesson BEB, Holmlund DEW. Predictons of intra operative bacterial
comtamination and post operative infection in elective colorectal surgery. J
Hosp.Infect 1988 ; 11: 227.
13. Dineen P, An evaluation of duration of the surgical scrub. Surg Gynecol Obstet
1969;129:1181
14. Garibaldi RA, cushing D, Lorer T. Risk factors for Post operative infection.
Am J Med 1991 ; 91 (Suppl 3B) : 1585.
15. Culver Dh, Horen TC, Gaynes RP. Surgical wound infection rates by wound
class, operative procedure, and patient risk indes. Am J Med, 1991; 91 (Suppl
3B) : 152 S.
16. Page CP, et al. Antimicrobial Probphylaxis for surgical wounds: guidelines for
clinical care. Arch Surg 1993 ; 79 : 128.
17. Paskin DL, Lerner HJ. A prospective study of wound infections. Ann Surg
1969;35;627.
18. Cruse P JE, Foord R The Eipdemiologyb of Wound Infection a 10 year
prospective study of 62939 wounds surg clin noth Am 1980
19. Garibaldi RA , Cushing D, Lawrel D, risk factors for post operative infection.
BOOK REFERENCES
1. Maingot’s Abdominal Operations 12th Editions
2. The Washington Manual of Surgery 7th Edition
3. Bailey and Love’s Short Practice of Surgery
4. Sabiston Textbook of Surgery 20th Edition
5. Schwartz’s Principles of Surgery
6. Fischer’s Mastery of Surgery
7. Trauma By Kenneth L Mattox 7th edition
APPENDIX
PROFORMA : WOUND – INFECTION
INFECTED / NOT INFCTED
AGE : NAME :
SEX :
ADDRESS : OCCUPATION :
HOSPITAL NO : SOCIO-ECONOMIC
STATUS :
CLINICAL SUMMARY AND DIAGNOSIS :
INVESTIGATIONS :
Hob% : Blood Sugar :
Urine – Others :
RISK FACTORS :
GENERAL YES NO
ANEMIA ( ) ( )
DIABETES ( ) ( )
TUBERCULOSIS ( ) ( )
MALIGNANCY ( ) ( )
SPECIFIC / LOCAL YES NO
UTI ( ) ( )
URI ( ) ( )
SURGERY PROPOSED
SURGERY PERFORMED
TYPE OF SURGERY:
CLEAN ( )
CLEAN-CONTAMINATED ( )
CONTAMINATED/DIRTY ( )
NATURE OF SURGERY:
ELECTIVE ( )
EMERGENCY ( )
PRE-OPERATIVE ANTIBIOTICS:
GIVEN ( )
NOT GIVEN ( )
PER-OPERATIVE
DURATION OF SURGERY:
<1 Hrs. ( )
1-2 Hrs. ( )
>2 Hrs. ( )
PERFORMED BY:
CHIEFS ( )
ASST. PROFS. ( )
TRAINEES ( )
ANTIBIOTICS:
USED ( )
NOT USED ( )
POST OPERATIVE:
INFECTED ( )
FOR “INFECTED” CASES ONLY
DAY OF DETECTION:
METHOD OF DETECTION:
CLINICAL ( )
MICROBIOLOGICAL ( )
BOTH ( )
ORGANISMS GROWN IN CULTURES:
SENSITIVITY PATTERN TO
ANTIBIOTICS:
OUTCOME:
RESOLVED ( )
NOT RESOLVED ( )
ANTIBOITICS
USED
1
NOT-USED
0
POST-OPERATIVE
METHOD OF DETECTION
CLINICAL
1
MICROBIOLOGICAL
2
CLINICAL & MICROBIOLOGICAL
OUTCOME
RESOLVED
1
NOT-RESOVED
0
ORGANISM GROWN IN CULTURE
NO GROWTH
0
STAPHLOCOCCUS AND STREPTOCOCCUS SPECIES 1
ESCHERICHIA AND KLEBSIELLA SPECIES 2
PSEUDOMONAS AEURIGINOSA
3
CITROBACTER DIVERSIS
4
OTHERS
*CODING
NAME
CODE
WOUND
INFECTED
1
NOTINFECTED
0
SEX
MALE
1
FEMALE
SURGERY DONE
TYPE OF SURGERY
CLEAN
1
CLEAN-CONTAMINATED
2
CONTAMINATED
NATURE OF SURGERY
EMERGENCY
1
ELECTIVE
2
RISK FACTORS
PRESENT
1
NOT-PRESENT
0
PRE-OPERATIVE ANTIBIOTICS
USED
1
NOT-USED
0
DURATION
<1 HOUR
1-2 HOURS
2
>2 HOURS
ABBREVIATIONS USED
SSI Surgical Site Infection
NNIS National Nosocomial Infection Control
S.AUREUS Staphylococcus aureus
E COLI Escherichia coli
CT Computerised Tomography
LRI Lower Respiratory Tract Infection
URI Upper Respiratory Tract Infection
UTI Urinary Tract Infection
DM Diabetes Mellitus