MANAGEMENT OF GINGIVAL HYPERPIGMENTATION
USING DIODE LASER AND CO2 LASER THERAPY:
A COMPARATIVE STUDY
Dissertation submitted to
THE TAMIL NADU DR. M.G.R. MEDICAL UNIVERSITY
In partial fulfillment for the Degree of
MASTER OF DENTAL SURGERY
BRANCH III
ORAL AND MAXILLOFACIAL SURGERY
viii
ABSTRACT
DISSERTATION TITLE: Management of Gingival hyperpigmentation using Diode laser and CO2 laser therapy: A comparative study.
BACKROUND:
A smile expresses a feeling of joy, success, sensuality, affection, and courtesy and can
reflect self-confidence and kindness. The aesthetic needs of the patients are increasing day by
day. Each and every patient wants a beautiful smile.The pigmentation of the gingiva, when it is
not related to the skin complexion, is a dampening factor in an otherwise acceptable smile
window. In recent years, the use of laser photoablation has been recognized as one of the most
effective, pleasant, and reliable techniques for treatment of gingival hyperpigmentation.
Different lasers have been used for gingival depigmentation, including carbon dioxide (CO2)
(10,600 nm), diode (820 nm), neodymium-doped:yttrium, aluminium, and garnet (Nd:YAG)
(1,064 nm), erbium (Er-doped:YAG) (2,940 nm), and erbium- and chromium-doped:yttrium,
scandium, gallium, garnet (Er,Cr:YSGG) (2,780 nm) lasers. This study compares the efficiency
of carbon dioxide (CO2) and diode laser techniques to change the colour of the gingiva in the
treatment of gingival hyperpigmentation by assessing the colour of the gingiva, gingival
bleeding, operator’s difficulty, post operative wound healing, pain and esthetic perception by the
patient at 1 week,2 week,3 week and 4 week post-operatively.
MATERIALS AND METHODS:
This double-blinded study was conducted at Department of oral and maxillofacial
surgery, Rajas dental college and hospital, Tirunelveli from February 2013 to November 2015.
ix
TheRajas dental college.The patient was blinded about the type of laser used for depigmentation
of his/her gingiva. Gingival depigmentation was done from canine to canine in the upper anterior
region.A total of 20 anterior segments were treated: 10 randomly to Carbon dioxide & Diode
Laser group using Flip coin method. Pre-operative photographs & Post operative radiographs
were obtained with a digital camera with standardized settings for grey, white, black and a cm
scale with standard lighting and backdrop. Macroscopic distribution and colour of the
pigmentation of all surfaces were recorded in detail. A single surgeon performed the procedure
in each segment using diode or CO2 laser as allocated by the co-investigator. The primary
investigator who was blinded about the allocation of segment evaluated the primary or secondary
parameters like colour of the gingival, bleeding, difficulties of the operator, pain perception of
patient and post-operative wound healing. The parameters were evaluated intra- operatively and
post-operatively till 4th week of follow-up.
DATA ANALYSIS:
The collected patient data were tabulated and statistical analysis were performed.
Microsoft Excel 2010 software to derive the mean and standard deviation and SPSS software
version 21 was used for statistical analysis. Charts and graphic representations were obtained
with the results. Descriptive statistics done by Measures of central tendency E.g. Mean and
Measures of Dispersion E.g. Standard deviation was calculated for all the parameters. Inferential
Statistics was done by unpaired student ‘t’ test to compare the mean difference between the two
groups for difference in the colour of the gingival, bleeding, difficulties of the operator, pain
perception of patient and post-operative wound healing.P value of 5% was considered
x
RESULTS AND STATISTICS:
A total of 10 patients were selected for treatment of gingival hyperpigmentation. Out of
10 patients in the study group 6 were males and 4 were females. Pre-operatively,in both the study
group, the colour of the gingiva was heavy. The results of this study shows that the degree of
pigmentationat the end of 4thweek wasless in diode group with 20% of the patient showing no pigmentation compared to CO2group (10%). Unpaired student‘t’ test was done to assess the
difference in colour of gingiva pre and post-operatively.There was slight statistical significance
between the two groups in the colour of the gingival (p value=0.047*).Regarding difficulty of the
operator and pain and wound healing, there was no statistical significant difference between the
diode and CO2group (p value=1,000NS).In case of bleeding, there was marginally significant
difference between the diode and CO2group (p value=0.0632+) in the immediate post-operative
period. With regards to esthetic perception by the patient, there was marginally significant
difference between the diode and CO2group (p value=0.0632+) at the end of 4th week. Regarding
the aesthetic consideration diode laser group scored more satisfaction than CO2 laser study
group.
SUMMARY AND CONCLUSION:
Growing aesthetic need requires the removal of hyperpigmented areas to create pleasant
and confident smile which altogether alter personality of an individual. From our study we come
to the conclusion that on comparing both the group diode laser study group had better outcome
than CO2 laser study group.
xii
ABBREVATIONS
Bd
-
Bleeding
CO
2-
Carbon dioxide
COG
-
Colour of gingival
DO
-
Difficulty of the operator
Imm-post-op -
Immediate post operatively
Intra-op
-
Intra operatively
OE
-
Overall esthetics
Post-op
-
Post operatively
PP
-
Pain perception
Pre-op
-
Preoperatively
VAS
-
Visual analog scale
xiii
CONTENTS
S.NO
TOPIC
PAGE
NO.
1
INTRODUCTION
1-11
2
AIM
12
3
OBJECTIVE
13
4
REVIEW OFLITERATURE
14-26
5
MATERIALS ANDMETHODS
27-37
6
SURGICAL
PICTURESANDASSESSMENTS
38-47
7
RESULTS ANDSTATISTICS
48-68
8
TABLES
1-16
9
FIGURES
1-18
10
CHARTS
I-XVII
11
DISCUSSION
69-75
12
SUMMARY ANDCONCLUSION
76-78
13
BIBILIOGRAPHY
79-86
[image:12.612.81.522.133.663.2]INTRODUCTION
1
INTRODUCTION
Esthetic dentistry targeted at designing the perfect smile is delivered only by harmonious blend of the soft and hard tissues of the oral cavity. Very often deft clinical efforts at managing esthetic discrepancies of teeth are hampered by not so satisfactory soft tissue profiles. One of the deciding factors of the soft tissue profile is the colour of the gingiva. The color of the gingiva varies among different individuals, and depends on the vascular supply of the gingiva, epithelial thickness, degree of keratinisation of the epithelium and the presence of pigmented cells38.
Oral pigmentation is the discoloration of the mucosa or gingiva. It can be either due to physiological or pathological conditions. Gingiva is the most common site of pigmentation in the oral cavity. Gingival hyperpigmentation is seen as a genetic variation in some populations independent of their age and sex and termed as physiological or racial gingival pigmentation. Melanosis of the gingiva is frequently present in dark-skinned ethnic groups as well as in different medical conditions. Although pigmentation of the gingiva is a completely benign condition it is an esthetic problem in many individuals.
INTRODUCTION
2
The colour of the attached and marginal gingiva is generally described as coral pink29. The pigmentation of the gingiva, when it is not related to the skin complexion, is a dampening factor in an otherwise acceptable smile window43 Although melanin pigmentation of the gingiva is completely benign and does not present a medical problem, complaints of black gums are common particularly in patients who have a very high smile line (gummy smile)45, 10
Causes for Pathologic Oral Pigmentation10, 56
Endogenous Factors 1. Diseases that increase melanin pigmentation:
Addison’s disease, Peutz-Jeghers syndrome, Albright’s syndrome, Von Reckling Hausen disease.
2. Bile pigments can stain skin and mucous membranes
3. The deposition of iron in hemochromatosis that can stain oral mucous membranes
4. Polycythemia, Cyanotic conditions
Exogenous factors
1. Atmospheric irritants(coal and metal dust) Colouring agents in food or lozenges
2. Metallic pigmentation: heavy metals (bismuth, lead, arsenic mercury and silver)
INTRODUCTION
3
4. Amalgam tattoo
5. Anti-malarial drugs
Melanin, carotene, reduced hemoglobin and oxy hemoglobin are main pigments which contribute to the normal color of gingiva. Gingival hyperpigmentation is a condition in which there will be an increased pigmentation beyond the normally expected degree of the oral mucosa6. Gingival pigmentation may appear as early as 3 hours after birth.55 Gingival pigmentation is considered to be multifactorial.6.The most common cause for gingival hyperpigmentation is due to excessive melanin deposition by melanocytes, which in turn depends on the activity of enzyme tyrosinase. Melanin pigmentation of the gingiva is completely benign and does not presents a medical problem49
Pathogenesis of hyperpigmentation
Melanin is derived from the Greek word ‘‘melas,’’ which means black25. It is an endogenous pigment produced by the melanocytes which are cells of neural crest origin present in the basal and suprabasal layers of the epithelium3, 44
Melanocytes are round nucleus with a double nuclear membrane, and a clear cytoplasm, lacking desmosomes or attachment plates. It contains few intracellular
filaments, but an abundance of mitochondria which sometimes fill the cytoplasm. Biochemically, polypeptides are synthesized in ribonucleoprotein granules,
INTRODUCTION
4
capable of melanogenesis. Tyrosinase activity is present in premelanosomes and melanosomes, but absent in melanin granules.55
Active melanocytes synthesize tyrosinase enzyme, which accumulates in the vesicles of the Golgi apparatus, leading to formation of premelanosomes. Tyrosinase enzyme leads to oxidation of tyrosine via a number of intermediate products, including dihydroxyphenylalanine (DOPA), resulting in the formation of a dense pigment melanin, which forms homogeneous, opaque melanosomes. Premelanosomes are transferred by melanocytes to the adjacent keratinocytes by cytocrine ability. This process is known as inoculation, where in keratinocytes play an active phagocytic role. This structural and functional relationship gives rise to the concept of the epithelial–melanin unit. Individuals, regardless of race, have approximately the same number of melanocytes in any given region. A ratio of 1:15 (Melanocyte / Basal keratinocyte) has been found in the human gingival epithelium.55
Epidemiology of hyperpigmentation
Gingival hyperpigmentation is seen as a genetic trait in some population and is more appropriately termed as physiological or racial gingival pigmentation. Physiologic pigmentation is probably genetically determined, but as Dummett suggested, the degree of pigmentation is partially related to mechanical, chemical and physical stimulation. There were no significant difference in oral pigmentation between males and females.56 Fair-skinned individuals are very likely to have non-pigmented gingiva, but in darker Fair-skinned persons, the chance of having pigmented gingiva is extremely high.
INTRODUCTION
5
different areas of the same mouth.56 The distribution of oral pigmentation in black individuals is as follows: gingiva = 60%; hard palate = 61%; mucous membrane = 22%; and tongue = 15%. The highest rate of gingival pigmentation has been observed in the area of incisors. The rate decreases considerably in the posterior region.3
The prevalence of melanin in different population has been reported to vary between 0% to 89% with regard to ethnic factors and smoking habit. Complaints of 'black gums' are common among the patients having a very high smile line (gummy smile) and hyperpigmented gingival tissue often forces patients to seek cosmetic treatment. Although melanin pigmentation of the gingiva is completely benign, cosmetic concerns are common, particularly in patients having a very high smile line (gummy smile).
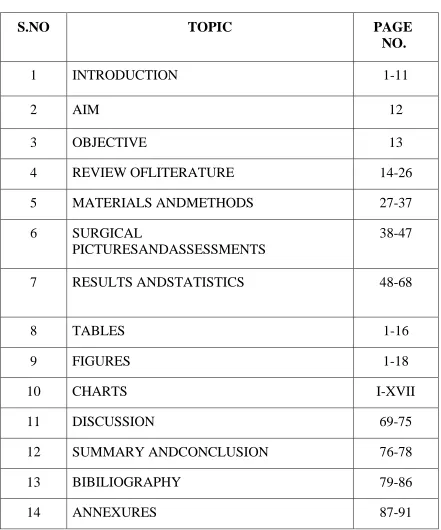
Oral pigmentation index (DOPI):35
This index of oral pigmentation is the commonly used index due to its simplicity and ease of use.
The scores are as follows:
– 0= No Clinical Pigmentation (Pink tissue)
– 1= Mild (Light brown tissue)
– 2= Moderate (Brown tissue)
– 3= Heavy (Deep brown or Black tissue) Gingival pigmentation index: 35
• Score 0: Absence of pigmentation
• Score 1: Spots of brown to black color or pigments.
• Score 2: Brown to black patches but not diffuse pigmentation
INTRODUCTION
6
Methods of depigmentation
In 1951 an attempt was made to burn out the pigmented gingiva by using phenol and alcohol. But the attempt was futile in completely eliminating the pigments and the gingival repigmentation and the depth was difficult to control1
Different Technique Employed56
Methods aimed at removing the pigment layer
. Surgical methods of depigmentation
Scalpel surgical technique
a. Slicing, or partial thickness flap technique b. Bone denudation
c. Abrasion d. Scraping e. Gingivectomy
Cryosurgery
Electrosurgery
Laser surgery like Nd:YAG, Er:YAG, CO2 lasers
Chemical method of depigmentation using caustic chemicals. Eg. 90% phenol
Methods aimed at masking the pigmented gingiva with grafts from less pigmented areas.
Free gingival grafts (FGG)
INTRODUCTION
7
Of all these techniques the laser have proved to be very effective in the management of gingival hyperpigmentation and it provides less morbidity.
Lasers in dentistry
LASER- Light Amplification by Stimulated Emission of Radiation. It’s an Electromagnetic wave with Monocromatic – Coherent - Collimated6
Lasers were first introduced in 1960 by Maiman and were brought into general practice by Dr William and Terry Myers.31 Lasers have been used in dentistry since the beginning of the 1980s.23 Over the last decade there has been a progressive increase in research concerning application of lasers to various clinical problems and a refinement of the concepts of laser/ soft tissue interactions.2 In recent years, the use of laser photoablation has been recognized as one of the most effective, pleasant, and reliable techniques for this purpose23
Laser production needs
o A source of Energy ( Electrical or another light source)
o Laser medium ( Solid, liquid, gaseous)
Each laser has a particular wavelength. When laser is directed at a tissue component called Chromosherepes each tissue has inherent absorption capacity for a particular wavelength. Different lasers have been used for gingival depigmentation, including carbon dioxide (CO2) (10,600 nm), diode (820 nm), neodymium-doped:yttrium, aluminium, and
garnet (Nd:YAG) (1,064 nm), erbium (Er)-doped:YAG (2,940 nm), and erbium- and
INTRODUCTION
8
CO2 laser
CO2 laser introduced in 1965 by Polanyi & associates, CO2 laser wavelength is
absorbed by water based tissues resulting in vaporization of intra and extra cellular fluid & disintegration of cells. Collateral thermal damage is less.
In a Carbon Dioxide Laser, an electrical current is passed through a mixture of several gases, including Carbon Dioxide. The current oscillates very quickly from positive to negative, and excites the Carbon Dioxide molecules, causing them to shed the extra energy as a photon of light. This light, which is infrared light, can then be focused into a beam and used for multiple applications. High energy Carbon Dioxide Lasers are often used in manufacturing and industrial applications and low energy lasers are used for surgical procedures
Carbon Dioxide Lasers work very well for soft tissue surgical procedures because the specific type (wavelength) of the infrared light produced by the laser is absorbed very well by the water in the tissue (soft tissue is mostly water). During surgery, the target tissue is vaporized very efficiently by the laser beam. The energy absorption of the tissue is so efficient that the energy only penetrates about 0.1 mm into the adjacent tissue, regardless of the depth of the cut. CO2 laser causes minimal damage to the periosteum and underlying
bone and it has unique characteristics of being able to remove a thin layer of epithelium cleanly.9 CO2 laser can damage tooth surface and the delivery system is very cumbersome.
INTRODUCTION
9
Diode Laser
Diode laser was introduced in 1995. The diode laser is a solid-state semiconductor laser that typically uses a combination of Gallium (Ga), Arsenide (Ar), and other elements, such as Aluminum (Al) and Indium (In), to change electrical energy into light energy.6 The semiconductor diode laser is emitted in continuous-wave or gated-pulsed modes, and is usually operated in a contact method using a flexible fibre optic delivery system22, 6
The 810-nm diode laser has energy and wavelength characteristics that specially target the soft tissues. It has an affinity for hemoglobin and melanin, therefore it is more efficient and better equipped to address deeper soft tissue problems.20
Diode lasers usage is similar to electrocauterization. Semi conductor diode laser has been used for gingivectomy, frenectomy, incisional and excisional biopsy, soft tissue tuberosity reduction, operculectomy, coagulation of donor site, and exposure of soft tissue covering osseointegrated implants14 and for numerous “fixed” soft tissue procedures including gingival hyperplasia, crown lengthening and hyperpigmentation.20
INTRODUCTION
10
Advantage of laser
The advantages of diode lasers are the smaller size of the units as well as the financial costs.6 The diode laser causes minimal damage to the periosteum and bone under the gingiva being treated. It has the unique property of being able to remove a thin layer of epithelium cleanly.22
There are many advantages of laser over surgical procedure. These include:
1. Dry and bloodless surgery,
2. Instant sterilization of surgical site,
3. Reduced bacteremia,
4. Reduced mechanical trauma,
5. Minimal post operative scaring and swelling,
6. Minimal post-operative pain. 11, 6
Pain reduction after using lasers may be due to the protein coagulum formed on the wound surface that seals off sensory nerve endings and it also acts as a biologic dressing. The rapid wound healing after using lasers may be related to the photobiomodulation (PBM). PBM accelerates lymphatic and blood flow resulting in reduction in toxins and contributes to a larger expression of collagen and elastic fibers during the early phases of the wound-healing process. This helps to reduce pain, enhance repair, and induce regeneration thus promoting faster healing and return to the normal.11
INTRODUCTION
11
needs expensive and sophisticated equipment that is not available commonly at all places and makes the treatment very expensive.54 The advantages of diode lasers are the smaller size of the units as well as the lower financial costs. Diode laser did not produce any deleterious effect on the root surface54, 22
Laser safety
AIM OF STUDY
12
AIM OF STUDY:
TO COMPARE THE CLINICAL EFFICIENCY OF CO2 AND DIODE
OBJECTIVE OF STUDY
13
OBJECTIVES:
PRIMARY:
To compare the efficiency of carbon dioxide (CO2) and diode laser techniques to change
the colour of the gingiva in the treatment of gingival hyperpigmentation.
SECONDARY:
REVIEW OF LITERATURE
14
Hans-Henning Horch et al (23) (1986) gained experience in the treatment of patients
with oral dysplastic precancerous lesions with CO2 laser. Besides 7 lichens planus, 50
leukoplakias of all grades of dysplasia, and carcinoma in situ and one lentigo maligna were
removed superficially with a defocused laser. Within the average follow-up period of 37 months,
22% local recurrences were observed. In comparison with conservative drug therapy,
conventional surgical procedures, and cryosurgical therapy, the CO2 laser treatment of
multicentric premalignant diseases of the oral mucosa 'can be recommended as an alternative
therapy.
Phimon Atsawasuwan et al (34) (2000) presented a case report of four cases that used
Nd:YAG laser for gingival depigmentation. The Nd: YAG laser was set at 6 watts,60 millijoules
per pulse, and 100 pulses per second. The procedure was performed with contact mode in all
pigmented areas by using a handpiece with a 320 micrometer diameter fibre optic. Three to four
weeks after the procedure the hyperpigmented gingiva appeared healthy, pink, and firm. No
recurrence of hyperpigmentation was found in 11 to 13 months of follow-up.
Mattias Kreisler et al (32) (2001) evaluated the effects of diode laser treatment of root
surface specimens on the attachment of periodontal ligament cells in vitro. He observed that
there was no significant positive effect on the new attachment of PDL cells on the tooth
REVIEW OF LITERATURE
15
Atif Kazmi et al (7) (2002) conducted a retrospective study examined hair removal using
Lightsheer Diode Laser System among 1000 women, and demonstrated that the Light Sheer
Diode Laser System provides both safe and effective removal of unwanted hair in patients
Esen E et al (18) (2004) evaluated the use of the flexible fiber CO2 surgical laser for
treating Gingival Melanin Pigmentation. Not only was the ablation of the pigmented gingiva
achieved without any bleeding, there was also no charring or carbonization during any of the
procedures. None of the patients required repetition in the early postoperative period, and healing
was completed in just 2 weeks, without any scar formation. There were no infections or
significant postoperative complications. The study concluded that using the CO2 laser in Super
Pulse mode is an effective and safe method for the elimination of Gingival Melanin
Pigmentation.
A. Chandu et al (12) (2004) presented a clinical paper regarding the use of CO2 laser in
the treatment of oral white patches. Forty-three patients with 73 primary oral leukoplakia were
assessed for outcome and factors affecting survival. The mean observation time was 47.2 _ 28.2
months (range 2–102 months). Disease-free survival was 55.4% at 3 years that dropped to 33.9%
after 5 years. The malignant transformation rate was 7.3%.The results demonstrated that there is
no significant prognostic factors were found on univariate analysis but alcohol consumption (P =
0.034) and previous malignancy (P = 0.018) were found to be significant prognostic indicators
using multivariate analysis. Continuation to smoke approached significance (P = 0.061)
G.Berk et al (9) (2005) presented two cases regarding gingival depigmentation using an
Er,Cr:YSGG laser, and a short follow-up period(6 months) for repigmentation results. There was
no intra-operative or post operative pain or discomfort. After 24hours the laser gingiva was
REVIEW OF LITERATURE
16
The ablated wound healed almost completely in 1 week. The results pointed out that YSGG
laser is a good and safe choice for removal of pigmented gingiva without local anesthesia. The
postoperative period is comfortable for the patient and healing is fast and good. No
repigmentation occurred in either patient after 6 months.
Carlo Maiorana et al( 11) (2006) used superpulsed diode laser for different surgical
procedures like to uncover impacted teeth, remove epulis, and treat intraoral hemangioma. The
use of a superpulsed diode laser allowed the surgeon to operate using high energy and very short
pulse duration.This allow the best control of insicion depth and reduced the thermal damage to
the target tissue.
Sameer A. Mokeem et al (41) ( 2006) reported three cases of gingival depigmentation
using surgical ablation. He observed that the technique was relatively simple and versatile and
requires minimum time and effort. If repigmentation occurs, the procedure can be done
repeatedly in the same area without limitation or causing any permanent damage. After eighteen
months follow up, none of the cases showed any recurrence of the pigmentation.
Daniel Simo˜es et al (14) ( 2007) conducted a study that reported removal of gingival
melanin pigmentation using an Er:YAG laser in a short-term clinical observation. His
observations were Er:YAG laser effectively ablated the epithelial tissue containing melanin
pigmentation. At 1 week, gingiva showed fast epithelization with a healthy appearance in all
cases. At 2 weeks, gingiva showed satisfactory healing with significant improvement in color
and recovery of the tissue thickness. At 1 month, complete healing was observed; after the
3-month evaluation, no gingival deformity or recession was observed. However, there was a slight
REVIEW OF LITERATURE
17
Manal M. Azzeh et al (29) in 2007 conducted a study in which sixty patients were
included.They used Erbium-Doped: Yttrium Aluminium and Garnet laser for treatment of
gingival depigmentation for esthetic purpose. In all patients, no discomfort, pain, or bleeding
complications were found intraoperatively or 4 days postoperatively. Ablated wounds healed
almost completely within 4 days. No recurrence of gingival hyperpigmentation was found during
the follow-up periods. They concluded that that the depigmentation of melanin hyperpigmented
gingiva by the Er:YAG laser is a reliable and satisfactory procedure.
Supaporn Suthprasertporn et al(48) (2007) presented a case report of two cases in the
treatment of gingival melanin hyperpigmentation by Er,Cr:YSGG laser device which was set at
1.0-1.75 watt,7% water and 11% air for gingival ablation, and then 0.5 watt,0%water and 11%
air for biological bandage. He observed that removal of melanin pigment was seen immediately
after treatment. Healing was good within a week. No post operative complication such as
infection, pain or bleeding was encountered. The final outcome was satisfactory for all patients.
Slight repigmentation was found in one patient in the eleventh month of observation.
Sushma Lagdive et al(49) (2009) describes two simple and effective surgical
depigmentation techniques scalpel blade surgery and semiconductor diode laser surgery -for
gingival depigmentation. Better results were achieved with semiconductor diode laser than
conventional scalpel blade surgery.
Ameet mani et al(2) (2009) presented a case report that described three different surgical
depigmentation techniques scalpel blade surgery, abrasion with diamond bur, and semiconductor
diode laser for gingival depigmentation. Better results were achieved with semiconductor diode
REVIEW OF LITERATURE
18
Hyuk-Jin Ko et al(24) ( 2010) evaluated the clinical effectiveness of and patient’s
satisfaction with treatment of gingival melanin hyperpigmentation with a Nd:YAG laser and a
high speed rotary instrument. In all cases, both anterior gingival areas were depigmented with
satisfaction and the patients did not complain of severe pain or discomfort. At the 1st week of
healing, the gingiva showed moderate to fast epithelization. Two weeks after the procedure,
clinically, the gingiva showed almost complete healing. Four weeks after the procedure, there
was significant improvement in gingival melanin hyperpigmentation. He concluded that the
Nd:YAG laser and the high speed rotary instruments seem to be effective for the esthetic
treatment of gingival melanin hyperpigmentation.
A pilot study conducted by Valerie G.A.Suter et al(51) (2010) evaluated the
histopathological characteristics and suitability of CO2 and diode laser for performing excisional
biopsies of similar lesions of the oral mucosa. His observations were the thermal damage zone of
the excised specimens created by the CO2 laser was significantly less pronounced than with the
diode laser. He also observed that the CO2 laser was more appropriate than the diode laser for
intraoral excision of premalignant or malignant lesion where the margins of the removed
specimens must be histopathologically evaluated.
Dosumu Oluwole O et al(17) (2010) determined the predominant gingival tissue color in
Nigerian environment. They assessed the association of gingival tissue color with gender and
facial skin color. They found that there is no significant association between gingival color and
gender. The study supported that there is strong relationship exist between facial skin color and
gingival tissue pigmentation.
Kumara Ajeya E G et al(27) ( 2011) presented a case report in which he compared the
REVIEW OF LITERATURE
19
healing responses and patient satisfaction. Maxillary anterior region was the area of concern for
the patient, where at the right side scalpel technique and at the left side. Both the treatment
modalities showed comparative results in terms of patient acceptance. Scalpel depigmentation
resulted in uneventful healing of the treated site. Laser depigmentation resulted in absolute
bloodless field which healed uneventfully. Patient discomfort was more in laser treated areas
during the initial healing period.
Goksel Simsek Kaya et al(20) ( 2011) compared the use of diode and Er:YAG laser in
treating gingival melanin pigmentation in terms of gingival depigmentation local anaesthesia
requirements, post operative pain/discomfort, depigmentation effectiveness, and total treatment
duration. Procedures were carried out without the need for any topical or local anesthetic, and no
unpleasant events occurred during the actual procedure or the healing period. The total length of
treatment was significantly shorter with the diode laser than with the Er:YAG laser. No melanin
recurrence was detected during any follow-up session.
Geeti Gupta et al(19) ( 2011) presented a case report that described simple and effective
depigmentation technique using semiconductor diode laser surgery – for gingival
depigmentation. A 23-year-old male patient complaining of heavily
pigmented gums visited department of Periodontics was considered for study. Healing was good
at 1 month with pink color comparable to nearby non-treated area, resulting in a significant
improvement in aesthetic appearance. No infection or significant postoperative complications
such as pain or bleeding were encountered. Fifteen months follow-up showed no signs of
recurrence of pigmentaion. The method used here produced desired results and above all, the
patient was satisfied with the outcome, which is the ultimate goal of any therapy that is carried
REVIEW OF LITERATURE
20
Maryam Talebi et al(31) (2012) presented a case report regarding the effects of
cryotherapy on physiologic pigmentations of oral mucosa in a 9-year-old boy . Cryotherapy is a
method of tissue destruction by rapid freezing. It is an atraumatic, cost-effective and simple
method for treating oral pig-mentation. This report concluded that the cryotherapy as an
atraumatic, cost-effective and simple method for treating oral pigmentation without recurrent
lesions after 12 months.
Zingade AN et al(56) ( 2012) presented a case report in a 20 years old male patient
reported to the university periodontology clinic with the complaints of darkly pigmented gums
and irregularly placed teeth. It was planned to carry out depigmentaion procedure using different
technique like a scalpel, bur abrasion, cryotherapy and lase for the four different quadrant under
local anesthesia. All the three different techniques followed for depigmentation in this case
provided similar comparable outcomes at 3 months follow-up. There was no evidence of
repigmentation.
Sanjeevini H et al(42) ( 2012) reported two cases of gingival pigmentation treated by
simple surgical technique of de-epithelialization. The procedure adopted was quite simple, cost
effective and less painful with minimal tissue loss and hence can be repeated without
complication keeping in mind the fact that repigmentation is a possibility in most cases. The
above mentioned procedure can also be performed by general dental practitioners to reduce and
lighten the pigmentation and thereby improve the gingival appearance
Sujal Shah et al(47) in (2012) describes two distinct surgical depigmentation procedures:
scalpel blade surgery and semiconductor diode laser for complete removal of gingival
pigmentation, tissue healing following the surgery and fulfillment of patient centered outcomes
REVIEW OF LITERATURE
21
semiconductor laser that combines Gallium (Ga), Arsenide (Ar) and other elements like
aluminum (Al) and Indium (In), converting electric energy into light energy. In this report both
the surgical techniques have shown excellent results, however scalpel blade surgery showed
marginally better results in terms of tissue healing and esthetics.
Walter Duki et al(54) ( 2012) evaluated the effect of a 980-nm diode laser as an adjunct
to scaling and root planing (SRP) treatment. The present results indicated that non-surgical
periodontal therapy using hand instruments and a sonic device alone or in combination with a
diode laser provide significant improvements in clinical parameters like bleeding on probing
(BOP), probing depth (PD), and clinical attachment level (CAL) for both moderate and deep
pockets at 6 and 18 weeks after treatment. In the present study, the use of a 980-nm diode laser
with a power of 2 W as an adjunctive to SRP significantly reduced gingival inflammation during
the observation period, although these results were not superior to the use of SRP alone.
Vishal Singh et al(52) ( 2012) compared and evaluated the gingival depigmentation by
diode laser and cryosurgery using tetrafluoroethane. Both procedures were equally effective in
depigmentation. At the 18-month follow-up, spotted repigmentation was found in one case in
each group. Although there was initial healing discomfort and mild pain with cryosurgery, all the
patients were satisfied with the esthetic outcomes. During the 18-month follow-up, the
depigmentation achieved using both the techniques was found equivalent and satisfactory.
M.Bhanu moorthy et al(10) 2012 reported case series in which she described three
different surgical depigmentation techniques: scalpel surgery, abrasion with rotary abrasive, and
a diode laser. She observed that better results of depigmentation were achieved with diode laser
REVIEW OF LITERATURE
22
that lasers were an effective and a safe means to removal of hyperpigmentation from the gingiva.
Healing was uneventful and no repigmentation occurred.
F. Agha-Hosseini et al(1) 2012 did a comparative evaluation of low-level laser and CO2
laser therapies for the treatment of oral lichen planus. The clinical trial was conducted with 28
patients. One group received CO2 laser therapy, the other received low-level laser therapy
(LLLT) for 5 sessions every other day. Improvements in size of lesions, in pain and clinical
response scores were achieved in both groups. The present study showed that LLLT displayed
better results than CO2 laser therapy as alternative or additional therapy, but further
investigations in comparison with standard treatment modalities with a prolonged follow-up
period will be necessary to confirm the efficacy of laser therapy in the treatment of OLP.
Gurumoorthy Kaarthikeyan et al (22)( 2012) evaluated intra-operative and
postoperative pain levels by a Visual Analog Scale (VAS) during gingival depigmentation
procedures using scalpel surgery and lasers. He also determined whether the pain responses were
influenced by the age and gender of the patient. This study concludes that laser procedures for
gingival depigmentation produce less pain and discomfort during surgery compared to scalpel
procedures. However there was no difference in the levels of pain 24 hours postoperatively and 1
week postoperatively between the two procedures.
Rashmi Hegde et al (40)(2012) compared the various techniques for gingival
depigmentation like surgical stripping, Erbium-Doped:Yttrium, Aluminium, and Garnet laser;
and carbon dioxide laser. The study also evaluated their effect on histological changes in
melanocyte activity and clinical repigmentation. They concluded that surgical stripping for
gingival depigmentation remained the gold standard. Er:YAG laser and CO2 laser can be
REVIEW OF LITERATURE
23
A comparative study done by Desai Urmi et al (16)(2013) regarding patient perception on
gingival depigmentation using scalpel and diode laser. VAS score was used for pain perception
after surgery .Pain perception was less when diode laser was used and regarding the esthetic
change, patient expectation and retreatment of the two surgical procedures were at par with one
and another.
A randomized split-mouth clinical trial conducted by Marco Giannelli et al (30) (2013)
compared the clinical efficacy of two different photoablative dental lasers erbium:
yttrium-aluminium–garnet and diode, for the treatment of gingival hyperpigmentation. In the study they
observed that both diode and Er:YAG laser gave excellent results in gingival hyperpigmentation.
Er:YAG laser induced deeper gingival tissue injury than diode laser, as judged by bleeding at
surgery, delayed healing and histopathological analysis. Diode laser caused less postoperative
discomfort and pain.
Santhosh Kumar et al (44) (2013) done a comparative evaluation of the gingival
depigmentation by using Tetrafluoroethane cryosurgery and the gingival abrasion technique – 2
years of follow up. The study group was 10 healthy patients. Tetrafluoroethane was used for the
cryosurgical depigmentation and the gingival abrasion technique used a coarse flame shaped bur.
The statistical analysis which was done after 90th, 180th days and 2 years. The p-value which
was obtained (p<.001) showed the superiority of cryosurgery over the gingival abrasion. During
the follow up period, no side effects were seen for both the techniques and the improved
aesthetics was maintained upto 2 years.
Rajiv saini et al(39) 2013 presented a case report that describes the application of semi
conductor diode laser procedure for gingival depigmentation. In a 25 year old patient the
REVIEW OF LITERATURE
24
980 nm was selected for the procedure. No postoperative pain, hemorrhage, infection or scarring
occurred in first and subsequent visits. Healing was uneventful. Patient s acceptance of the
procedure was good and results were excellent as perceived by the patient.
Sharmila verma et al(45) 2013 presented a case report in which gingival depigmentation
was done with scraping technique in a 26 old male patient. The healing process was preceded
normally and patient did not report any discomfort. At the end of one month re-epithelialization
was complete and healing was found to be satisfactory. Patient had no complaints of
postoperative pain or sensitivity. At the end of six months the gingiva appeared healthy and no
further repigmentation was seen.
Javier D. Sanz-Moliner et al (26) (2013) compared the tissue response and postoperative
pain after the use of a diode laser (810 nm) (DL) as an adjunct to modified Widman flap (MWF)
surgery to that of MWF alone. Thirteen patients with generalized severe chronic periodontitis
completed the study. Pain scale assessment (PS), pain medication consumption (PM), tissue
edema (TE), and tissue color (TC) were evaluated 1 week after surgery. The results were
statistically significant and he concluded that the use of an 810-nm diode laser provided
additional benefits to MWF surgery in terms of less edema and postoperative pain.
A cross sectional study conducted by Deepa Ponnaiyan et al (15) (2014) correlated the
skin color with gingival pigmentation patterns in South India. She observed that the highest rate
of gingival pigmentation was observed in the area of incisiors. Incidence of pigmentation did not
differ between the sexes.
Basser Ali Abdullah et al (8) (2014) compared the effectiveness of Er Cr YSGG & Diode
laser on de pigmentation of gingival melanin pigmentation & compared their possible
REVIEW OF LITERATURE
25
simple & accepted by the patients .,both waterlase & diode laser are effective in oral melanin
depigmentation. The use of diode laser is associated with pain &delayed healing compared with
waterlase. According to result of this study we found that waterlase is better than diode laser in
melanin depigmentation.
Amit Bhardwaj et al(3) 2014 undertook a study to to evaluate patient response and
recurrence of pigmentation following gingival depigmentation carried out with a surgical blade
and diode laser. Patients were evaluated for pain (1 day, 1 week), wound healing and melanin
repigmentation (Melanin Pigmentation Index) immediately and at 1 week, 1 month and 3
months, respectively. Comparative pain assessment (P = 0.148) and repigmentation scores (P =
0.288) at various time intervals between the two groups did not show any statistical significance.
Both the procedures did not result in any post-operative complications and the gingiva healed
uneventfully. When compared, both the techniques were found to be equally efficacious.
Shirin Amini Sedeh et al (46)(2014) conducted a study that aimed to compare the
recurrence rate of gingival pigmentation after treatment by liquid nitrogen swap and a cryoprob
in 18 months. A total of 26 patients with physiologic gingival pigmentation were selected. The
anterior sextant was divided into left and right segments; each segment was treated randomly by
swap technique or cryoprob. Standard photos were evaluated with photoshop software (Red,
Green, Blue, Cyan, Magenta, Yellow, Black [RGB, CMYK]) before and at 2 week, 1, 3, 6, 9, 12,
15, 18 months after the treatment. The results were both methods of cryosurgery are appropriate
in treatment of gingival depigmentation because no significant recurrence was observed during
18 months follow-up.
Semih Ozbayrak et al(32) 2014 conducted a study regarding the treatment of melanin
REVIEW OF LITERATURE
26
procedure well. Clinical keratinization was completed in 3-5 wks after the treatment, and the
treated areas were similar in color to that of the normal mucosa. Clinical repigmentation also did
not occurred in the follow up period of 18 months.
Recent study conducted by Shilpi et al(33) 2014 regarding the surgical esthetic correction
for gingival pigmentation by scalpel technique .Either slicing or scraping of the epithelium was
done using the scalpel. She observed that no complication was encounted and recurrence of
MATERIALS & METHODS
27
MATERIALS & METHODS
• The Patients were selected from the outpatient Department of Oral and maxillofacial
surgery, RDC, Kavalkinaru, Tirunelveli.
• A signed informed consent was obtained from all patients willing to participate in this
study.
• A total of 20 anterior segments were treated: 10 randomly to Carbon dioxide & Diode
Laser group by split mouth technique.
• Assignment was performed according to flip-coin method by co-investigator.
• Patients underwent periodontal therapy consisting of oral hygiene instructions and full
mouth oral prophylaxis.
• Gingival depigmentation was planned from canine to canine in the upper anterior region.
• All patients were evaluated by Primary investigator.
• Pre-operative photographs & Post operative radiographs were obtained with a digital
camera with standardized settings for grey, white, black and a cm scale with standard
lighting and backdrop. Macroscopic distribution and colour of the pigmentation of all
surfaces were recorded in detail.
• INCLUSION CRITERIA
• Patient with healthy peridontium
• Patients between 18-40 year of age
• Presence of Melanin pigmentation with score of 3 (DOPI)
• EXCLUSION CRITERIA
• Presence of systemic diseases
MATERIALS & METHODS
28 • Tobacco users
• Pregnant / Lactating patients
Selection Criteria
• The Cases are selected based on Dummett-Gupta Oral Pigmentation Index (DOPI) 1971
– 0= No Clinical Pigmentation (Pink tissue)
– 1= Mild (Light brown tissue)
– 2= Moderate (Brown tissue)
[image:45.612.128.502.289.625.2]– 3= Heavy (Deep brown or Black tissue)
MATERIALS & METHODS
29
Study Methodology-Double blinded
The study was performed as a double blinded study where both the primary investigator
whoevaluated the parameter and the patients were blinded. The co investigator and the primary
investigator were tested for normal colour vision to prevent inter examiner variability. The
co-investigator selected patient with grade 3 pigmentation according to DOPI scale.Then he
randomly allocated each patient’s right or left segment to CO2 or diode group by flip coin
method, with head being diode laser and tail being CO2 laser.All the pre-operative preparations
like photographs were taken care of by the co-investigator. The patient was blinded about the
type of laser used for depigmentation of his/her gingiva.A single surgeon performed the
procedure in each segment using diode or CO2 laser as allocated by the co-investigator. The
primary investigator who was blinded about the allocation of segment evaluated the primary or
secondary parameters like colour of the gingival, bleeding, difficulties of the operator, pain
perception of patient and post-operative wound healing.The parameters were evaluated intra-
operatively and post-operatively till 4th week of follow-up.
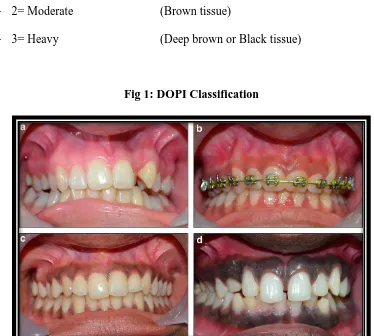
Group I: The Equipment used was AMD Diode laser Picasso, USA.Topical anesthetic gel was applied to the surgical field. Special eye glasses were worn by the patient, surgeon and
the staff to comply with the FDA laser safety rules. The properly initiated tip of the diode laser
unit (Picasso, AMD laser technologies, USA; wavelength 810 nm) angled at an external bevel of
45 degrees and at energy settings of 0.5-1.5 watts continuous wave (CW) was used with small
brush like strokes back and forth with gradual progression deeper along the same initial laser
incision to remove the tissue. A 400 μm strippable fiber was used with a power setting of 1.5
watts initially in pulsed wave mode (PW) set at 0.20 ms of pulse duration and 0.10 ms of pulse
MATERIALS & METHODS
[image:47.612.190.454.117.419.2]30
Fig 2:
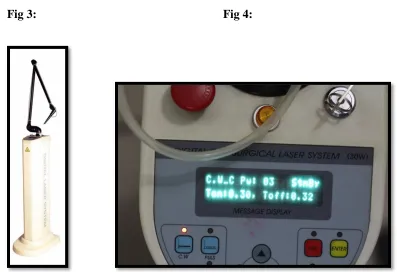
Group II: For CO2 laser Equipment used is NovaPulse LX-20 SP surgical laser
.Preoperative images are taken .The melanin pigmented gingival segment is ablated by CO2 laser
vaporization under local anesthesia. The ablation was performed by a flexible fiber Luxar
NovaPulse LX-20 SP surgical laser, the predecessor of LS-1005. The repeated A5 Super Pulse
mode was applied at 3 watts, 20 Hz, 10 milliseconds, with a 0.8 mm spot size. The remains of
the ablated tissue were removed using sterile gauze dampened with saline. This procedure was
“repeated until the desired depth of tissue removal was achieved.” To protect the adjacent teeth
from the laser beam, either an acrylic template was used to cover the labial surface of the teeth,
MATERIALS & METHODS
31
In addition, the more precise 0.4 mm laser tip was used at the gingival margins and interdental
papilla; the power setting was also reduced to 3 watts in order to achieve better control and
minimize the risk of tooth damage
Fig 3: Fig 4:
EVALUATION OF THE PRIMARY PARAMETER:
COLOUR ASSESSMENT:
To evaluate the primary parameter the colour of the gingiva, pre-operative photographs
was taken one week before the procedure and post-operative photographs were taken at first,
second, third, fourth week after the procedure of depigmentation.
The photographs were taken using the Canon EOS digital camera, standardized setting
for grey and white, centimeter scale with standard lighting with a manual shutter mode (M). All
[image:48.612.101.498.166.443.2]MATERIALS & METHODS
[image:49.612.132.477.115.382.2]32
Fig 5:
The primary investigator who was blinded about the allocation of segments either to Co2
or diode laser, evaluated the pre-operative and post-operative photographs using DOPI scale
• Dummett-Gupta Oral Pigmentation Index (DOPI):
– 0= No clinical pigmentation (Pink tissue)
– 1=Mild (Light brown tissue)
– 2= moderate ( Brown tissue)
MATERIALS & METHODS
33
EVALUATION OF THE SECONDARY PARAMETERS:
BLEEDING:
Bleeding was assessed by the primary investigator intra-operatively and immediate
post-operatively
It was evaluated as
A. None B. Slight C. Moderate D. Severe
DIFFICULTY OF THE OPERATOR:
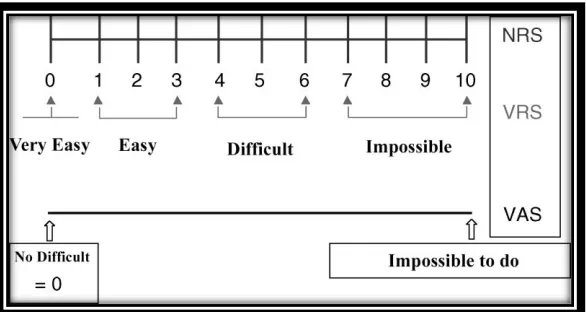
Difficulty of the operator was assessed by the primary investigator intra-operatively using
the Visual Analogue Scale
VAS Score:
MATERIALS & METHODS
[image:51.612.147.440.110.266.2]34
Fig 6:
The VAS scale was shown to the surgeon who operated. The surgeon was
asked to mark the difficulty of the procedure. The left extreme end was “Impossible”
procedure. The distance from point from the left end of the scale was recorded
intra-operatively.
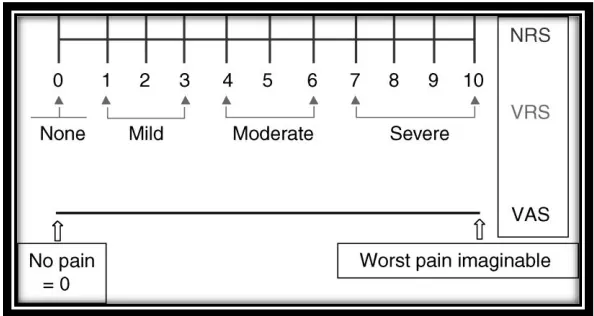
PAIN ASSESSMENT:
• Pain was assessed using Visual Analogue Scale
– VAS Score
• 0 = No pain
• 1 = Slight pain (1-3)
• 2 = Moderate pain (3.1-6)
MATERIALS & METHODS
[image:52.612.161.458.107.265.2]35
Fig 7:
• The Visual analogue scale was used to evaluate the subjective pain level experienced by
each patient. It consists of Horizontal line 100mm long starting at the left end with the
descriptor “no pain” and ending at the right side with “severe pain”. Patients were asked
to mark the severity of the pain. The distance from point from left end of the scale was
recorded intra-operatively, immediate post-op and first day post-operatively.
WOUND HEALING:
Wound healing was assessed by the primary investigator clinically on the first, second,
third, fourth week post-operatively
It was evaluated by using healing index by Landry et al.
1. Very poor
– Tissue colour: ≥ 50% of gingiva red, response to palpation: bleeding
– Granulation tissue: present
– Incision margin: not epithelialised, with suppuration present
2. Poor
– Tissue colour: ≥ 50% of gingiva red, response to palpation: bleeding
– Granulation tissue: present
MATERIALS & METHODS
36
3. Good
– Tissue colour: ≥ 25% and < 50% of gingiva red, response to palpation: no bleeding
4. Very good
– Tissue colour: < 25% of gingiva red ,response to palpation: no bleeding
– Granulation tissue: none ,incision margin: no connective tissue exposed
5. Excellent
Tissue colour: all tissues pink, response to palpation: no bleeding
Granulation tissue: none, incision margin: no connective tissue exposed
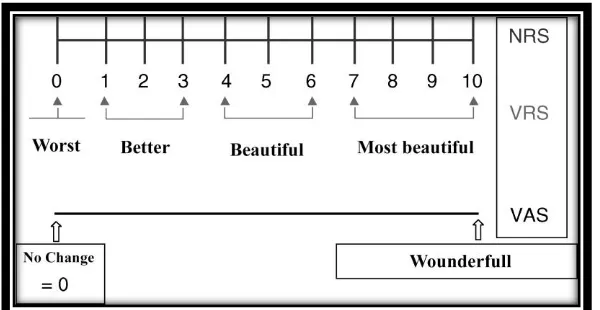
ASSESSMENT OF PATIENT OPINION ON ESTHETIC CHANGE
Esthetic change was assessed by using Visual Analogue Scale
VAS Score
– 0 = Worst
– 1 = Better (1-3)
– 2 = Beautiful (3.1-6)
[image:53.612.158.458.552.707.2]– 3 = Most Beautiful (6.1-10)
MATERIALS & METHODS
37
The VAS was used to rate the esthetic perception as denoted by the patient at the end of 4th week The most extreme left point represent the worst possible esthetic situation whereas the extreme
SURGICAL PICTURES & ASSESSEMENTS
38
CASE 1:
PRE OPERATIVE: Fig 9a PRE OPERATIVE: Fig 9b
POST OPERATIVE:
IMMEDIATE POST – OP: Fig 9c 1st DAY: Fig 9d
1st WEEK: Fig 9e 2nd WEEK: Fig 9f
SURGICAL PICTURES & ASSESSEMENTS
39
CASE 2:
PRE OPERATIVE: Fig 10a PRE OPERATIVE: Fig 10b
POST OPERATIVE:
IMMEDIATE POST – OP: Fig 10c 1st DAY: : Fig 10d
1st WEEK: : Fig 10e 2nd WEEK : : Fig 10f
SURGICAL PICTURES & ASSESSEMENTS
40
CASE 3:
PRE OPERATIVE: Fig 11a PRE OPERATIVE: Fig 11b
POST OPERATIVE:
IMMEDIATE POST – OP: Fig 11c 1st DAY: Fig 11d
1st WEEK: Fig 11e 2nd WEEK: Fig 11f
SURGICAL PICTURES & ASSESSEMENTS
41
CASE 4:
PRE OPERATIVE: Fig 12a PRE OPERATIVE: Fig 12b
POST OPERATIVE:
IMMEDIATE POST – OP: Fig 12c 1st DAY: Fig 12d
1st WEEK: Fig 12e 2nd WEEK: Fig 12f
SURGICAL PICTURES & ASSESSEMENTS
42
CASE 5:
PRE OPERATIVE: Fig 13a PRE OPERATIVE: Fig 13b
POST OPERATIVE:
IMMEDIATE POST – OP: Fig 13c 1st DAY: Fig 13d
1st WEEK: Fig 13e 2nd WEEK: Fig 13f
SURGICAL PICTURES & ASSESSEMENTS
43
CASE 6:
PRE OPERATIVE:Fig 14a PRE OPERATIVE:Fig 14b
POST OPERATIVE:
IMMEDIATE POST – OP:Fig 14c 1st DAY:Fig 14d
1st WEEK:Fig 14e 2nd WEEK:Fig 14f
SURGICAL PICTURES & ASSESSEMENTS
44
CASE 7:
PRE OPERATIVE: Fig 15a PRE OPERATIVE: Fig 15b
POST OPERATIVE:
IMMEDIATE POST – OP: Fig 15c 1st DAY: Fig 15d
1st WEEK: Fig 15e 2nd WEEK: Fig 15f
SURGICAL PICTURES & ASSESSEMENTS
45
CASE 8:
PRE OPERATIVE:Fig 16b PRE OPERATIVE:Fig 16b
POST OPERATIVE:
IMMEDIATE POST – OP:Fig 16c 1st DAY:Fig 16d
1st WEEK:Fig 16e 2nd WEEK:Fig 16f
SURGICAL PICTURES & ASSESSEMENTS
46
CASE 9:
PRE OPERATIVE:Fig 17a PRE OPERATIVE:Fig 17b
POST OPERATIVE:
IMMEDIATE POST – OP:Fig 17c 1st DAY:Fig 17d
1st WEEK:Fig 17e 2nd WEEK:Fig 17f
SURGICAL PICTURES & ASSESSEMENTS
47
CASE 10:
PRE OPERATIVE:Fig 18a PRE OPERATIVE:Fig 18b
POST OPERATIVE:
IMMEDIATE POST – OP:Fig 18c 1st DAY:Fig 18d
1st WEEK:Fig 18e 2nd WEEK:Fig 18f
RESULTS & STATISTICS
48
RESULTS AND STATISTICAL ANALYSIS
The collected patient data were tabulated and statistical analysis was performed. Microsoft Excel 2010 software to derive the mean and standard deviation and SPSS software version 21 was used for statistical analysis. Charts and graphic representations were obtained with the results.
RESULTS:
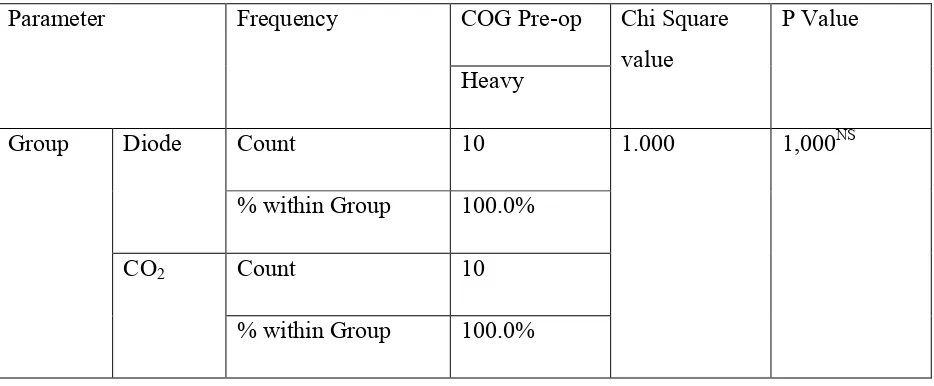
This study included 10 patients with gingival hyperpigmentation. They were aged from 18-23.Mean age of male and female patients were 19.2 yrs and 20.5 yrs respectively. Out of 10 patients in the study group 6 were males and 4 were females (Chart 1). Pre-operatively, in both the study group, the colour of the gingiva was heavy (Chart 2).
The parameters assessed were colour of the gingiva, bleeding, difficulties of the operator, pain perception of patient and post-operative wound healing.
CHART I: SEX WISE DISTRIBUTION
0 2 4 6 8 10 0
6 6
0
4 4 10 10
N o o f p at ie n ts
Sexwise distribution of the study
group
RESULTS & STATISTICS
49
CHART II: COLOUR OF GINGIVA- PRE-OP
ASSESSMENT OF PRIMARY PARAMETER: COLOUR OF THE GINGIVA
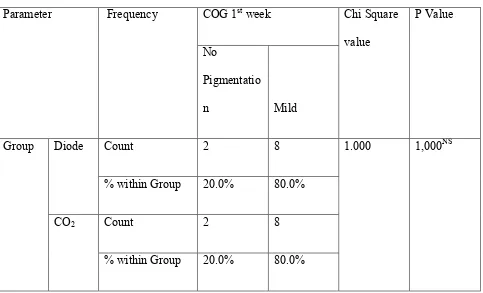
The colour of the gingiva was assessed post-operatively for both the CO2 and diode
group at first, second, third and fourth week. In both the study group at the end of 1st week the colour of the gingiva revealed no pigmentation in 2(20%) of the patients and with mild
pigmentation in 8(80%) of the patients (Chart 3). In both the study group at the end of 2nd week the colour of the gingiva revealed no pigmentation in 3(30%) of the patients and with mild pigmentation in 7(70%) of the patients (Chart 4).At the end of 3rd and 4th week, in the diode group, 2(20%) of the patients had no pigmentation, 7(70%) of the patients had mild pigmentation and 1(10%) had moderate pigmentation. In CO2 laser study group, at the end of 3rd and 4th week,
1(10%) patient had no pigmentation. 8(80%) of the patients had mild pigmentation and 1(10%) had moderate pigmentation (Chart 5).
0 2 4 6 8 10 Diode CO2 10 10
0 0
N o o f p at ie n ts
Colour of the gingiva pre-operatively
RESULTS & STATISTICS
50
Regarding the colour of the gingiva both the study group had same results at the end of 1st and 2nd week. But at the end of 3rd week and 4th week the degree of pigmentation was less in diode group than CO2 laser group.
CHART III: COLOUR OF GINGIVA – END OF FIRST WEEK
CHART IV: COLOUR OF GINGIVA – END OF 2ND WEEK
0 2 4 6 8 Diode CO2 N o o f p at ie n ts
Colour of the gingiva at the end of 1st
week
No pigmentation Mild pigmentation 0 2 4 6 8 Diode CO2 3 37 7
N o o f p at ie n ts
Colour of the gingiva at the
2nd week
RESULTS & STATISTICS
51
CHART V: COLOUR OF GINGIVA – END OF 3RD WEEK
CHART VI: COLOUR OF GINGIVA – END OF 4TH WEEK
ASSESMENTOF BLEEDING
Bleeding was assessed intra operatively and immediate post-operatively.In both the study group all the patients 10(100%) had moderate bleeding during the time of
0 2 4 6 8
No pigmentation Mild pigmentation Moderate pigmentation 2 7 1 1 8 1 N o o f p at ie n ts
Colour of the gingiva at the end of 3rd
week
Diode CO2 0 2 4 6 8No pigmentation Mild pigmentation Moderate pigmentation 2 7 1 1 8 1 N o o f p at ie n ts
Colour of the gingiva at the end of 4rd
week
RESULTS & STATISTICS
52
procedure being done (Chart 7). In diode laser study group in the immediate post operative period 2(20%) of the patients had slight bleeding and 8(80%) had moderate bleeding. In CO2
laser study group all the patients 10(100%) had moderate bleeding (Chart 8).
CHART VII: INTRA OP BLEEDING
CHART VIII: IMMEDIATE POST OP BLEEDING
0 2 4 6 8 10 Diode CO2 N o o f p at ie n ts
Intra operative bleeding
Heavy bleeding Moderate bleeding 0 2 4 6 8 10 Diode CO2 N o o f p at ie n ts
Immediate postoperative bleeding
RESULTS & STATISTICS
53
ASSESMENT OF DIFFICULTY OF OPERATOR:
The difficulty of the operator was assessed intra-operatively. The difficulty of the operator for doing the procedure was easy in all the patients 10(100%) in both the technique (Chart 9).
CHART IX: DIFFICULTY OF THE OPERATOR
ASSESSMENT OF PAIN:
Pain was assessed intra-operatively, immediate post-operatively and 1st day post-operatively.Regarding pain perception in intra-operative period both the study group 10(100%) had no pain (Chart 10). In immediate postoperative period pain perception was slight in all the patient 10(100%) during both the procedures (C1art 11).Pain perception on the 1st day was slight in all the patient 10(100%) during both the procedures (Chart 12).Both the study group
experienced no pain intra-operatively and only one patient experienced mild pain in the immediate post operative period and in the 1stpost operative period.
0 2 4 6 8 10 Diode CO2 10 10
0 0
N o o f p at ie n ts
Difficulty of the operator
RESULTS & STATISTICS
54
CHART X: PAIN PERCEPTION INTRA-OPERATIVELY
CHART XI: PAIN PERCEPTION IMMEDIATE POST OP PERIOD
0 2 4 6 8 10 Diode CO2 10 10
0 0
N o o f p at ie n ts
Pain perception intraoperatively
No pain With pain 0 2 4 6 8 10 Diode CO2 N o o f p at ie n ts
Pain perception immediate
postoperative period
RESULTS & STATISTICS
55
CHART XII: PAIN PERCEPTION – END OF 1ST DAY
ASSESMENT OF WOUND HEALING:
Wound healing was assessed on the first, second, third, fourth week post-operatively. Wound healing at the end of 1st week was good in 2(20%) of the patients and was very good in 8(80%) of the patients in diode laser study group. In CO2 laser group the wound healing was very good
in all the patients 10(100%) (Chart14). At the end of 2nd week wound healing was very good in 8(80%) of the patients and was excellent in 2(20%) of the patients in diode laser study group. In CO2 laser group the wound healing was very good in 6(60%) the patients and excellent in
4(40%) of the patients (Chart 15).All the patients in both the study group had excellent wound healing at the end of 3rdweek (Chart 16).During the 1st and 2nd week of post operative period CO2
laser had better wound healing when compared to diode laser group but at the end of 3rd week and 4th week both the study group had excellent wound healing.
0 2 4 6 8 10 Diode CO2 10 10
0 0
N o o f p at ie n ts
Pain perception at the end of 1st day
RESULTS & STATISTICS
56
CHART XIII: WOUND HEALING – END OF 1ST WEEK
CHART XIV: WOUND HEALING – END OF 2
ND WEEK 0 2 4 6 8 10 Diode CO2 2 0 8 10 N o o f p at ie n ts
Wound healing at the of 1st week
Good Very good 0 2 4 6 8 Diode CO2 8 6 2 4 N o o f p at ie n ts
Wound healing at the end of 2nd
week
RESULTS & STATISTICS
57
CHART XV: WOUND HEALING – END OF 3RD WEEK
CHART XVI: WOUND HEALING – END OF 4TH WEEK
ASSESSMENT OF ESTHETIC OPINION:
The esthetic perception was assessed at the end of 4th week. All the patients 10(100%) had beautiful aesthetics in diode laser study group. In CO2 laser study group 2(20%) had better
0 2 4 6 8 10 Diode CO2
0 0
10 10
N o o f p at ie n ts
Wound healing at the end of 3rd
week
Very good Excellent 0 2 4 6 8 10 Diode CO20 0
10 10
N o o f p at ie n ts
Wound healing at the end of 4th
week
RESULTS & STATISTICS
58
aesthetics and 8(80%) had beautiful aesthetic appearances (Chart 17).Regarding the aesthetic consideration diode laser group scored more satisfaction than CO2 laser study group.
CHART XVII: AESTHETIC OPINION OF THE PATIENT
STATISTICAL ANALYSIS
Descriptive statistics:
Measures of central tendency Eg: Mean and Measures of Dispersion Eg.
Standard deviation was calculated for all the parameters.
Inferential Statistics:
To compare the mean difference between the two groups for difference in the colour of the gingiva, bleeding, difficulties of the operator, pain perception of patient and post-operative wound healing.unpaired student ‘t’ test was used
0 2 4 6 8 10 Diode CO2 0 2 10 8 N o o f p at ie n ts
Aesthetic opinion of the patient
RESULTS & STATISTICS
59
P value of 5% was considered significant.
Significance level interpretation:
NS – Not significant