Amino Acids in Hemagglutinin Antigenic
Site B Determine Antigenic and Receptor
Binding Differences between A(H3N2)v
and Ancestral Seasonal H3N2 Influenza
Viruses
Xiaoquan Wang,aNatalia A. Ilyushina,bVladimir Y. Lugovtsev,aNicolai V. Bovin,c Laura K. Couzens,aJin Gao,a Raymond P. Donnelly,bMaryna C. Eichelberger,a Hongquan Wana
Division of Viral Products, Center for Biologics Evaluation and Research, Food and Drug Administration, Silver Spring, Maryland, USAa; Division of Biotechnology Research and Review II, Center for Drug Evaluation and Research, Food and Drug Administration, Silver Spring, Maryland, USAb; Shemyakin Institute of Bioorganic Chemistry, Moscow, Russiac
ABSTRACT Influenza A H3N2 variant [A(H3N2)v] viruses, which have caused human
infections in the United States in recent years, originated from human seasonal H3N2 viruses that were introduced into North American swine in the mid-1990s, but they are antigenically distinct from both the ancestral and current circulating H3N2 strains. A reference A(H3N2)v virus, A/Minnesota/11/2010 (MN/10), and a seasonal H3N2 strain, A/Beijing/32/1992 (BJ/92), were chosen to determine the molecular ba-sis for the antigenic difference between A(H3N2)v and the ancestral viruses. Viruses containing wild-type and mutant MN/10 or BJ/92 hemagglutinins (HAs) were con-structed and probed for reactivity with ferret antisera against MN/10 and BJ/92 in hemagglutination inhibition assays. Among the amino acids that differ between the MN/10 and BJ/92 HAs, those in antigenic site A had little impact on the antigenic phenotype. Within antigenic site B, mutations at residues 156, 158, 189, and 193 of MN/10 HA to those in BJ/92 switched the MN/10 antigenic phenotype to that of BJ/ 92. Mutations at residues 156, 157, 158, 189, and 193 of BJ/92 HA to amino acids present in MN/10 were necessary for BJ/92 to become antigenically similar to MN/ 10. The HA amino acid substitutions responsible for switching the antigenic pheno-type also impacted HA binding to sialyl receptors that are usually present in the hu-man respiratory tract. Our study demonstrates that antigenic site B residues play a critical role in determining both the unique antigenic phenotype and receptor speci-ficity of A(H3N2)v viruses, a finding that may facilitate future surveillance and risk as-sessment of novel influenza viruses.
IMPORTANCE Influenza A H3N2 variant [A(H3N2)v] viruses have caused hundreds of
human infections in multiple states in the United States since 2009. Most cases have been children who had contact with swine in agricultural fairs. These viruses origi-nated from human seasonal H3N2 viruses that were introduced into the U.S. swine population in the mid-1990s, but they are different from both these ancestral viruses and current circulating human seasonal H3N2 strains in terms of their antigenic characteristics as measured by hemagglutination inhibition (HI) assay. In this study, we identified amino acids in antigenic site B of the surface glycoprotein hemaggluti-nin (HA) that explain the antigenic difference between A(H3N2)v and the ancestral H3N2 strains. These amino acid mutations also alter binding to minor human-type glycans, suggesting that host adaptation may contribute to the selection of antigeni-cally distinct H3N2 variants which pose a threat to public health.
Received4 August 2016Accepted15 October 2016
Accepted manuscript posted online2 November 2016
CitationWang X, Ilyushina NA, Lugovtsev VY, Bovin NV, Couzens LK, Gao J, Donnelly RP, Eichelberger MC, Wan H. 2017. Amino acids in hemagglutinin antigenic site B determine antigenic and receptor binding differences between A(H3N2)v and ancestral seasonal H3N2 influenza viruses. J Virol 91:e01512-16. https:// doi.org/10.1128/JVI.01512-16.
EditorStacey Schultz-Cherry, St. Jude Children's Research Hospital
Copyright© 2017 American Society for Microbiology. All Rights Reserved.
Address correspondence to Maryna C. Eichelberger, maryna.eichelberger@fda.hhs.gov, or Hongquan Wan, hongquan.wan@fda.hhs.gov.
crossm
on November 7, 2019 by guest
http://jvi.asm.org/
KEYWORDS A(H3N2)v, influenza virus, hemagglutinin, antigenic phenotype, amino acid
S
wine serve as an important intermediate host for influenza viruses to adapt, evolve, and acquire transmissibility to humans. The H1N1 pandemic in 2009 is a reminder that swine-origin viruses represent an authentic public health threat (1). Influenza A H3N2 variant [A(H3N2)v] viruses from swine have also caused human infections in multiple states in the United States since 2009 (2–4), with more than 300 laboratory-confirmed cases in 2011 alone (5, 6). Most of the A(H3N2)v cases have been children who had contact with swine at agricultural fairs (5, 7, 8). Fortunately the symptoms of A(H3N2)v infection were generally mild, although some patients had to be hospitalized, and one case was fatal (9). It is estimated that only 1 out of approximately 200 A(H3N2)v human infections are laboratory confirmed; therefore, the number of actual human cases might be much greater than that of reported cases (10).A(H3N2)v viruses originated from human seasonal H3N2 strains that were intro-duced into North American swine in the mid-1990s (11–13). After multiple reassortment events in swine, these H3N2 viruses acquired a triple-reassortant internal gene (TRIG) cassette containing internal genes from avian, swine, and human strains (11, 14–16). Outbreaks of TRIG-H3N2 virus infections in U.S. swine were first reported in a few states in 1998 and have spread to many other states (11) and Canada (17, 18). The current circulating swine H3N2 viruses in North America, together with A(H3N2)v viruses, were termed “lineage IV” based on the phylogenetic analysis with earlier swine H3N2 isolates (13, 17–19). The majority of A(H3N2)v isolates since 2011 have acquired the matrix gene from the 2009 pandemic H1N1 virus (2, 20), which has enhanced the replication and transmission of A(H3N2)v viruses in swine (21, 22), potentially increasing the risk of human infection.
A(H3N2)v isolates are antigenically distinct from recent human seasonal H3N2 viruses as well as H3N2 viruses that circulated in humans during the period when they are thought to have been introduced into swine (2, 3, 19). Although amino acids close to the receptor binding site (RBS) in hemagglutinin (HA) are associated with antigenic evolution of human seasonal H3N2 and swine H3N2 viruses (23, 24), the specific residues that explain why swine-origin A(H3N2)v viruses are antigenically distinct from the human strains have not been identified. This information is important for our understanding of the emergence of novel antigenic influenza virus strains that pose a threat to public health. In this study, we identified amino acids in HA of A/Minnesota/ 11/2010 (MN/10), the A(H3N2)v vaccine candidate, that provide the molecular basis for the antigenic difference between A(H3N2)v and a proposed ancestral human seasonal H3N2 strain, A/Beijing/32/1992 (BJ/92). We found that substitutions of these amino acids impact receptor specificity, suggesting the antigenic differences may be the result of host adaptation in addition to immune selection.
RESULTS
Antigenic difference between A(H3N2)v MN/10 and seasonal H3N2 virus BJ/92.
To determine the molecular basis for the antigenic difference between A(H3N2)v and seasonal H3N2 viruses, an A(H3N2)v virus, MN/10, and a seasonal H3N2 virus, BJ/92, were used as prototype viruses in this study. MN/10 is a vaccine candidate for potential A(H3N2)v outbreaks. BJ/92 was selected because it is genetically closely related to the North American swine H3N2 viruses first isolated in the late 1990s (11). BJ/92 was also used as a vaccine strain during the 1993-1994 influenza season. We performed hem-agglutination inhibition (HI) assays to determine antigenic phenotype with two sets of ferret sera (each included MN/10 antiserum and BJ/92 antiserum). Since similar patterns of inhibition was observed with the two sera, only one set of data is reported. In HI assays, ferret sera against MN/10 and BJ/92 inhibited the homologous virus with HI titers of 453 and 640, respectively; however, no inhibition was observed against the
on November 7, 2019 by guest
http://jvi.asm.org/
heterologous virus (HI titers of ⬍10) (Table 1), confirming the antigenic difference between these two viruses.
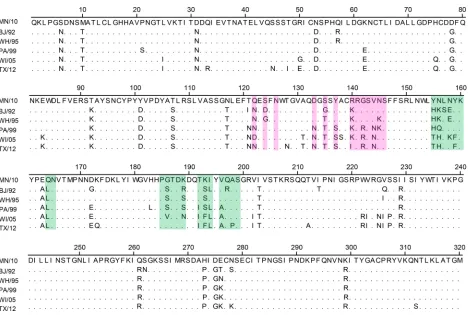
[image:3.585.42.369.84.573.2]Amino acids in antigenic site A have little impact on the antigenic phenotype of MN/10.Because HA is the target of antibodies in the HI assay, the difference of HI titers is a good indicator of amino acid variations in the HA. Indeed, there are 51 amino acid differences between the MN/10 and BJ/92 HAs, with 38 distributed throughout HA1 (Fig. 1). Many of these variations are within known antigenic domains, e.g.,
TABLE 1HI titers of ferret antisera against mutant MN/10 and BJ/92 viruses
Virus
Antigenic site(s)
HI titeraof ferret sera
MN/10 BJ/92
wt
MN/10 453 5
BJ/92 5 640
MN/10 reassortantsb
Q122N A 453 10
S124D A 453 10
S135G A 320 10
R140K A 320 5
122/124/135/140 A 320 20
Y155H B 226 5
N156K B 160 5
L157S B 320 10
N158E B 226 14
K189R B 320 5
K193S B 160 5
155/156 B 226 14
155/158 B 113 14
155/189 B 113 5
155/193 B 160 28
156/189 B 40 5
156/193 B 80 20
158/189 B 160 14
158/193 B 160 20
189/193 B 160 20
155/156/158 B 113 40
155/156/189 B 57 28
155/156/193 B 57 57
155/158/189 B 57 20
155/158/193 B 80 57
155/189/193 B 160 28
156/158/189 B 57 20
156/158/193 B 113 40
156/189/193 B 160 113
158/189/193 B 113 80
155/156/158/189 B 28 28
155/156/158/193 B 57 113
155/156/189/193 B 40 113
155/158/189/193 B 57 80
156/158/189/193 B 57 226
155/156/158/189/193 B 28 226
156/157/158/189/193 B 80 453
135/155/156/158/189/193 A and B 28 453
155/156/157/158/189/193 B 28 453
BJ/92 reassortantsc
BJ156/158/189/193 B 40 20
BJ156/157/158/189/193 B 160 40
aGeometric mean titer from two independent assays; a value of 5 was assigned to titers of⬍10 for
calculation.
bReassortant viruses possessing the HA and NA genes of MN/10 virus and the internal genes of PR8, each
containing a single residue change (e.g., Q122N) or a combination of changes (e.g., 122, 124, 135, and 140; abbreviated 122/124/135/140) to that/those present in BJ/92 HA.
cReassortant viruses containing the HA and NA genes of BJ/92 and the internal genes of PR8, with residues
at the indicated positions mutated to those in MN/10 HA.
on November 7, 2019 by guest
http://jvi.asm.org/
antigenic sites A, B, C, D, and E (18, 25–27). Among these, 4 are in antigenic site A, whereas 10 are in antigenic site B. To determine which of these amino acid variations is responsible for the observed antigenic difference, we focused on residues in anti-genic sites A and B because antibodies against these two sites are the most effective at inhibiting hemagglutination. Reassortant MN/10 and BJ/92 viruses with the A/Puerto Rico/8/1934 (PR8) internal gene constellation were generated by reverse genetics, and residues in antigenic sites A and B in the HA of reassortant MN/10 were mutated to those in BJ/92 orvice versa. The wild-type (wt) and mutant viruses were tested in HI assays to identify amino acid changes that reduced inhibition by the homologous antiserum but increased inhibition by the heterologous antiserum. Mutations that caused a ⱖ4-fold reduction in HI titers of the homologous antiserum and aⱖ4-fold increase in HI titers of the heterologous antiserum were deemed to be determinants for the antigenic phenotype.
As shown in Table 1, reassortant MN/10 viruses, each bearing one of the single-residue substitutions in antigenic site A to those present BJ/92 HA, i.e., Q122N, S124D, S135G, and R140K, were inhibited by the homologous MN/10 antiserum at an HI titer of 320 or 453, similar to that against wt MN/10 (HI titer, 453). Consistently, these viruses were not inhibited at all or only slightly inhibited by BJ/92 antiserum (HI titers ofⱕ10). A reassortant MN/10 virus possessing all 4 of these MN/10-to-BJ/92 mutations was still effectively inhibited by MN/10 antiserum (this virus is abbreviated 122/124/135/140, and other mutants with more than one residue mutation are abbreviated similarly) and was only weakly inhibited by BJ/92 antiserum, at an HI titer of 20. These data indicate that amino acid substitutions in antigenic site A do not explain the observed antigenic difference between MN/10 and BJ/92.
Amino acids in antigenic site B determine the antigenic phenotype of MN/10.
We next examined whether substitutions in antigenic site B are associated with the
FIG 1Amino acid differences between the MN/10 and BJ/92 HAs. Shown is the alignment of residues 1 to 320 of the mature HA1 sequence. Other seasonal H3N2 viruses included are A/Wuhan/359/1995 (WH/95), A/Panama/2007/1999 (PA/99), A/Wisconsin/67/2005 (WI/05), and A/Texas/50/2012 (TX/12). Dots denote residues that are identical to those in MN/10 HA. Residues in antigenic sites A and B are shaded in magenta and green, respectively.
on November 7, 2019 by guest
http://jvi.asm.org/
[image:4.585.43.511.66.381.2]antigenic phenotype of A(H3N2)v viruses. Residues 155, 156, 158, 189, and 193 in antigenic site B of MN/10 HA were examined because these residues are commonly associated with antigenic drift of human seasonal and swine influenza viruses (23, 24, 28, 29). Reassortant MN/10 viruses bearing each of the 5 single mutations from MN/10 to BJ/92, Y155H, N156K, N158E, K189R, or K193S, were inhibited by MN/10 antiserum at slightly lower HI titers (160, 226, or 320) than wt MN/10. However, none of these single mutant viruses recovered sufficient reactivity with BJ/92 antiserum; i.e., HI titers of BJ/92 antiserum were all below the detection limit, 10, except a titer of 14 against the N158E mutant virus. In contrast to these single-residue mutants, the combination of these 5 mutations in a reassortant MN/10 virus (155/156/158/189/193) restored inhibition by BJ/92 antiserum, with an HI titer of 226, which is a⬍4-fold difference from that of wt BJ/92 (640). Mutations of all 5 of these residues also resulted in a substantial loss of inhibition by MN/10 antiserum, with a⬎16-fold reduction in HI titer compared to that of the wt MN/10. These data demonstrate that amino acid mutations in antigenic site B account for the unique antigenic phenotype of MN/10 and its antigenic difference from BJ/92.
Minimal number of residues in HA that switch the MN/10 antigenic phenotype to that of BJ/92.Since our data indicated that the residue changes in antigenic site B underlie the antigenic difference between MN/10 and BJ/92, we performed HI assays to determine the minimal determinant that is associated with the antigenic difference. The reactivities of MN/10 and BJ/92 antisera were tested against reassortant MN/10 viruses containing various combinations of mutations at the 5 antigenic site B residues (155, 156, 158, 189, and 193), including almost all of the possible double, triple, and quadruple mutations. While some of the double and triple mutants, e.g., 155/156, 155/193, and 156/189/193, were inhibited at HI titers⬍4-fold different from that of wt MN/10 (i.e., HI titers of 160 and 320, versus 453 for the wt MN/10), most of the double and triple mutants had⬎4-fold decreases in HI titers; i.e., they were inhibited by MN/10 antiserum at HI titers of 57 to 113. Moreover, while some double and triple mutants, e.g., 155/189 and 156/189, gained no reactivity with BJ/92 antiserum, some other mutants, such as 156/189/193 and 158/189/193, exhibited substantially enhanced inhibition by BJ/92 antiserum (HI titers between 40 and 113, respectively). The decrease in HI titers against the homologous MN/10 antiserum was accompanied by the increase in HI titers against the heterologous BJ/92 antiserum.
The MN/10 antiserum had ⱖ8-fold-lower HI titers against all of the quadruple mutants, demonstrating that these mutants were antigenically different from the wt MN/10 virus. The impact of quadruple mutations was also evident in the reactivity pattern of BJ/92 antiserum: all of the quadruple mutants except 155/156/158/189 became susceptible to inhibition by BJ/92 antiserum, with HI titers ofⱖ80. One of the quadruple mutants, 156/158/189/193, was antigenically similar to wt BJ/92, with a ⬍4-fold HI titer difference from wt BJ/92 virus (HI titers of 226 and 640, respectively, with BJ/92 antiserum) (Table 1 and Fig. 2). Thus, a minimum of 4 amino acid substitu-tions at posisubstitu-tions 156, 158, 189, and 193 in antigenic site B switched the antigenic phenotype of MN/10 to that of BJ/92.
Amino acid 157 plays a role in determining the antigenic difference between MN/10 and BJ/92. Our results showed that mutants 156/158/189/193 and 155/156/ 189/193 were antigenically similar to BJ/92; however, the HI titers of BJ/92 antiserum against both mutants were still⬎2-fold-lower than that against the wt BJ/92 virus (226 versus 640). Therefore, we next tested whether additional mutations, including those single mutations that did not have a profound impact on the antigenic phenotype, could enhance the inhibition by BJ/92 antiserum. The L157S mutation was examined in particular because of its structural proximity to residues 156, 158, 189, and 193 (Fig. 3). While the L157S mutation alone did not alter the antigenic phenotype of MN/10, introduction of this change into mutants 156/158/189/193 and 155/156/158/189/193 enhanced inhibition by BJ/92 antiserum, reaching HI titers very similar to that against the wt BJ/92 virus (453 versus 640) (Table 1 and Fig. 2). The addition of S135G to the 155/156/158/189/193 virus also enhanced the inhibition by BJ/92 antiserum (Table 1).
on November 7, 2019 by guest
http://jvi.asm.org/
These findings indicate that additional substitutions in the HA can enhance binding of polyclonal antibodies and thereby contribute to the antigenic difference between A(H3N2)v and seasonal H3N2 viruses.
To confirm the importance of residues 156, 158, 189, and 193 within antigenic site B for inhibition by BJ/92 antiserum, we rescued a reassortant BJ/92 virus that carries the HA and neuraminidase (NA) genes of BJ/92 and the internal genes of PR8, with HA residues 156, 158, 189, and 193 mutated to those present in MN/10 HA. This mutant BJ/92 reassortant virus, abbreviated BJ156/158/189/193, had dramatically reduced sensitivity to BJ/92 antiserum, with an HI titer of 20 compared to 640 for wt BJ/92, confirming the key role of these amino acids in recognition of BJ/92-specific antibodies; however, this virus was only weakly inhibited by MN/10 antiserum, with an HI titer of 40. Interestingly, when S157 in this reassortant BJ/92 virus was mutated to L, which is present in MN/10 HA, the HI titer of MN/10 antiserum against the reassortant increased, resulting in a⬍4-fold difference from that for wt MN/10 (Table 1 and Fig. 2), thereby switching the BJ/92 antigenic phenotype to that of MN/10. These results further highlight the critical role of amino acids in antigenic site B, including residue 157, in defining the antigenic difference between MN/10 and BJ/92 viruses.
HA amino acid substitutions responsible for switching the antigenic pheno-type affect receptor specificity.Since antigenic site B is in close proximity to the RBS, we investigated the effect on virus receptor specificity of HA amino acid substitutions at positions 156, 157, 158, 189, and 193 that are responsible for switching the antigenic phenotype of the virus. We measured the affinities of MN/10, BJ/92, and five mutants, 156/158/189/193, 155/156/158/189/193, 156/157/158/189/193, BJ156/158/189/193, and BJ156/157/158/189/193, for synthetic Neu5Ac␣2,6-glycopolymers (Table 2). The pattern of binding to the major analogs of human receptors 6=SL, 6=SLN, and sulfated 6-Su-6=SLN and the surrogate of human receptors Neu5AcBn (30) was identical among all viruses tested (Table 2 shows the structures and abbreviations of sialylglycopoly-mers). The binding of MN/10 and BJ/92 to 9NAc-6=SLN and 6=SLN(Gc), glycans that are represented only in swine respiratory epithelial cells (30–32), was significantly distinct and independent of amino acids 156, 157, 158, 189, and 193, because viruses with mutations at these sites retained the parental HA binding pattern. Despite the fact that the glycan SiaTn is rarely found in the human respiratory tract (33), MN/10 and BJ/92 both bound this glycan with high affinity, although binding of the MN/10 virus was significantly greater (dissociation constant [Kd] of⬍0.1M Neu5Ac, compared to BJ/92
with aKdof 1.5⫾0.4M Neu5Ac [P⬍0.05]) (Table 2).
FIG 2Minimum amino acid changes in HA that switched the antigenic phenotypes of MN/10 and BJ/92. Reassortant MN/10 virus with residues at positions 156, 158, 189, and 193 mutated to those present in BJ/92 (156/158/189/193) has an antigenic phenotype typical of wt BJ/92, while reassortant BJ/92 virus with residues 156, 157, 158, 189, and 193 mutated to those in MN/10 (BJ156/157/189/193) exhibited an antigenic phenotype similar to that of wt MN/10 virus. Each bar represents the average of the log2values of HI titers obtained from two independent assays. The dashed line indicates the detection limit.
on November 7, 2019 by guest
http://jvi.asm.org/
[image:6.585.109.302.68.247.2]Interestingly, the mutations at amino acids that we identified as determinants of the antigenic phenotype contributed to the switch in binding affinity. Binding of MN/10 toward SiaTn and Neu5Ac6Gal was significantly reduced when residues 156, 158, 189, and 193 were mutated to those in BJ/92 (P ⬍ 0.05). The binding affinity of BJ/92 significantly increased when these 4 residues were replaced with amino acids from MN/10. A similar switch in binding affinity was observed for glycans YDS, 6-SiaTF, and swine-specific receptor Neu5Gc-Tn (32) in wt MN/10 and MN/10-like mutants. However, unlike binding to the previously mentioned glycans, the amino acid at position 157 of HA had a substantial impact on the affinity of the BJ/92 virus. For example, introduction of the S157L mutation into mutant BJ156/158/189/193 resulted in acquisition of moderate binding to Neu5Gc-Tn and 6-SiaTF receptors (i.e., the increase in receptor binding affinity was dependent on amino acid 157; P⬍0.05) (Table 2). In addition, there was a significant positive correlation between HI titers of MN/10 antiserum and binding to 2 similar sialylglycopolymers, SiaTn and 6-SiaTF, which are rarely found in humans (33, 34). Spearman correlation coefficients were 0.78 (P⫽0.049) and 0.80 (P⫽ 0.048), respectively (Fig. 4). Our data demonstrated that amino acids which are critical antigenic determinants impact the affinity of A(H3N2)v viruses for some minor human glycans.
HA amino acid substitutions responsible for switching the antigenic pheno-type have a profound impact on antibody binding.Finally we investigated whether differences in HI titer were due to a direct effect of antibody binding. We selected 8 mouse monoclonal antibodies (MAbs) against the MN/10 HA and measured their FIG 3Locations of HA amino acids that define the antigenic difference between A(H3N2)v and the ancestral seasonal H3N2 viruses. The monomers in the HA trimer of A/Hong Kong/1/1968 (PDB accession no. 4FNK) are shown in light gray, cyan, and dark gray. The 5 key residues that define the antigenic difference between MN/10 and BJ/92 are highlighted in green. Antigenic site B residue 155 is labeled blue, and the 4 antigenic site A residues tested are in magenta. Residues Y98, S136, W153, T155, H183, G186, D190, L194, L226, and S228 are colored yellow to depict the location of the RBS. The image was generated with PyMOL software (Delano Scientific).
on November 7, 2019 by guest
http://jvi.asm.org/
[image:7.585.122.288.73.380.2]TABLE 2 Effect of H3 HA amino acid substitutions responsible for switching the antigenic phenotype on receptor specificity a Biotinylated sialylglycopolymer (abbreviation) K d ( M Neu5Ac) a with virus: wt MN/10 wt BJ/92 156/158/189/193 155/156/158/189/193 156/157/158/189/193 BJ156/158/189/193 BJ156/157/158/189/193 Binding similar to that of wt virus Neu5Ac ␣ 2-OCH 2C 6H 4 (Neu5AcBn) 0.1 ⫾ 0.1 0.2 ⫾ 0.1 0.2 ⫾ 0.1 0.2 ⫾ 0.1 0.2 ⫾ 0.1 0.2 ⫾ 0.1 0.2 ⫾ 0.1 Neu5Ac ␣ 2-6Gal  1-4Glc (6 = SL) 0.5 ⫾ 0.1 1.1 ⫾ 0.3 1.0 ⫾ 0.3 0.8 ⫾ 0.3 0.9 ⫾ 0.3 0.7 ⫾ 0.2 0.6 ⫾ 0.2 Neu5Ac ␣ 2-6Gal  1-4GlcNAc (6 = SLN) 0.7 ⫾ 0.3 1.2 ⫾ 0.5 1.5 ⫾ 0.6 0.7 ⫾ 0.3 1.2 ⫾ 0.4 1.6 ⫾ 0.7 1.2 ⫾ 0.4 Neu5Ac ␣ 2-6Gal  1-4(6-O-Su)GlcNAc (6-Su-6 = SLN) 0.5 ⫾ 0.1 0.7 ⫾ 0.1 0.7 ⫾ 0.2 0.5 ⫾ 0.1 0.7 ⫾ 0.3 0.9 ⫾ 0.3 0.8 ⫾ 0.2 9-(AcN)-Neu5Ac ␣ 2-6Gal  1-4GlcNAc (9NAc-6 = SLN) 1.3 ⫾ 0.5° ⬎ 50 * 1.0 ⫾ 0.3° 0.5 ⫾ 0.2° 1.0 ⫾ 0.4° ⬎ 50 * ⬎ 50 * Neu5Gc ␣ 2-6Gal  1-4GlcNAc [6 = SLN(Gc)] 15.0 ⫾ 4.1° ⬎ 50 * 22.3 ⫾ 10.8° 13.2 ⫾ 6.1° 25.6 ⫾ 7.0° ⬎ 50 * ⬎ 50 * Binding different from that of wt virus Neu5Ac ␣ 2-6GalNAc ␣ (SiaTn) ⬍ 0.1° 1.5 ⫾ 0.4 * 1.0 ⫾ 0.4 * 0.9 ⫾ 0.3 * 0.9 ⫾ 0.3 * 0.4 ⫾ 0.1° 0.4 ⫾ 0.1° Neu5Ac ␣ 2-6Gal  (Neu5Ac6Gal) 0.9 ⫾ 0.4° 4.5 ⫾ 0.8 * 4.7 ⫾ 0.7 * 3.9 ⫾ 0.6 * 4.9 ⫾ 0.3 * 1.8 ⫾ 0.4° 1.3 ⫾ 0.3° Neu5Ac ␣ 2-6Gal  1-4GlcNAc-Man-GlcNAc-GlcNAcNeu5Ac ␣ 2-6Gal  1-4GlcNAc-Man (YDS) 0.6 ⫾ 0.2° 3.6 ⫾ 0.5 * 3.0 ⫾ 0.9 * 2.2 ⫾ 0.4 * 2.8 ⫾ 0.4 * 4.2 ⫾ 1.1 * 2.9 ⫾ 0.7 * Neu5Gc ␣ 2-6GalNAc ␣ (Neu5Gc-Tn) 0.6 ⫾ 0.3° ⬎ 50 * 11.3 ⫾ 4.0 *, ° 10.6 ⫾ 2.5 *, ° 16.5 ⫾ 5.2 *, ° ⬎ 50 * 15.0 ⫾ 2.9 *, ° Neu5Ac ␣ 2-6(Galb1-3)GalNAc ␣ (6-SiaTF) 5.0 ⫾ 2.2° ⬎ 50 * ⬎ 50 * ⬎ 50 * ⬎ 50 * ⬎ 50 * 19.5 ⫾ 1.9 *, ° Neu5Ac ␣ 2-6(Neu5Aca2-3)GalNAc ␣ (3,6-SiaTn) ⬎ 50 ⬎ 50 ⬎ 50 ⬎ 50 ⬎ 50 6.3 ⫾ 3.7 *, ° 3.3 ⫾ 2.0 *, ° a The dissociation constants ( K d) of virus complexes with synthetic sialylglycopolymers are shown. Lower K d values indicate stronger binding. The values represent the mean ⫾ standard deviation (SD) from at least 4 independent experiments. °, P ⬍ 0.05 compared to the values for wt BJ/92 virus by one-way ANOVA; * , P ⬍ 0.05 compared to the values for wt MN/10 virus by one-way ANOVA.
on November 7, 2019 by guest
http://jvi.asm.org/
[image:8.585.102.305.75.733.2]binding to some of the MN/10 and BJ/92 mutants by enzyme-linked immunosorbent assay (ELISA). Six of these MAbs inhibited MN/10 virus in the HI assay (Table 3). This observation and the sequencing data for the escape mutants indicate that they target epitopes in antigenic sites A and B in the globular head of the HA. The remaining 2 antibodies (HA13 and HA59) do not inhibit hemagglutination, implying that they bind antigenic sites C, D, or E or the stalk of HA. MAb binding to wt MN/10, wt BJ/92, and 5 mutants that exhibited substantial antigenic change (156/158/189/193, 155/156/158/ 189/193, 156/157/158/189/193, BJ156/158/189/193, and BJ156/157/158/189/193) was tested in the ELISA (Fig. 5). MN/10 with a single mutation at residue 157 to that in BJ/92 (L157S) was also included. All of the 8 MAbs reacted well with wt MN/10, with optical densities at 490 nm (OD490) between 1.9 and 2.5, versus⬍0.1 for the negative control
[image:9.585.82.329.69.186.2](data not shown). The mutations that changed the antigenic phenotype of MN/10 to that of BJ/92 caused dramatic loss of binding by some of the MAbs that possess HI activity. For example, relative to wt MN/10, the 156/158/189/193 virus had significantly lower levels of binding by MAbs HA20, HA25, and HE42 and completely lost binding by MAb HB27; mutant 155/156/158/189/193 was not bound by antibodies HA20, HA25, HB27, and HE42 and had reduced binding by MAb HB1. Antibody HB67 targets antigenic site A (Table 3); therefore, its reactivity with MN/10 virus was not significantly changed by the tested mutations, which are all within antigenic site B. Weak binding of HB67 to BJ/92 was observed, suggesting some level of conservation in antigenic site A of MN/10 and BJ/92. Only MAbs HA13 and HA59 bound all MN/10 mutants (only the HA13 data are shown in Fig. 5). While none of the MAbs reacted strongly with wt BJ/92, binding by most of these antibodies was observed when BJ/92 HA residues were FIG 4Correlation between HI titers of ferret MN/10 antiserum and binding to SiaTn (A) and 6-SiaTF (B) sialylglycopolymers. Data are plotted as HI titers of ferret antiserum raised against MN/10 virus versus receptor binding affinity (1/Kd, 1/M of Neu5Ac) of wt MN/10, wt BJ/92 and 5 mutants, 156/158/189/193, 155/156/158/189/193, 156/157/158/189/193, BJ156/158/189/193, and BJ156/157/158/189/193. Means are represented as circles, and linear regression is represented by dashed lines.
TABLE 3Mouse MAbs used for antibody binding assay
MAb Isotype HI titera
Mutation in HA of escape mutants
HA13 IgG1 ⬍10 NDb
HA20 IgG1 10,240 K160T or N165Kc
HA25 IgG1 5,120 Y159D
HA59 IgG1 ⬍10 ND
HB1 IgG2a 5,120 155YN- -YK160d
HB27 IgG2a 10,240 Y159D or 155YN- -YK160
HB67 IgG2a 320 G142R or S143L
HE42 IgG1 2,560 N145K or N158D
Mouse serum 640 ND
aMeasured with 1 mg/ml of each MAb. MN/10 antiserum collected from the mouse used for generation of
the HA-specific MAbs was used as a positive control.
bND, not done.
cThese mutations are present in different mutants selected by the same MAb.
dThe mutant possesses a deletion of 2 amino acids, either 156NL157 or 157LN158, from the wt sequence
155YNLNYK160.
on November 7, 2019 by guest
http://jvi.asm.org/
[image:9.585.42.372.575.685.2]mutated to those in MN/10 (Fig. 5). These data indicate that the amino acid mutations introduced into the HAs of MN/10 and BJ/92 directly impact antibody binding to HA, which is likely the major reason for the observed antigenic switch.
Interestingly, while the L157S mutation alone did not impact the binding by the tested MAbs, the addition of L157S in mutant 156/158/189/193 decreased the binding of antibody HB1 to the resultant virus, 156/157/158/189/193 (Fig. 5). More interestingly, while BJ156/158/189/193 was not recognized by HB1 in our ELISA, BJ156/157/158/189/ 193, with S157 mutated to L in MN/10, reacted with HB1 as effectively as wt MN/10 virus. This finding is consistent with the observation that the MN/10 antiserum has a 4-fold-higher HI titer with BJ156/157/158/189/193 than with BJ156/158/189/193 (Table 1) and implies that residue 157, together with other residues (e.g., 156, 158, 189, and 193), is a critical determinant of the antigenic phenotype.
DISCUSSION
H3N2 influenza A viruses are endemic in the U.S. swine population. Some of these swine H3N2 viruses, e.g., the H3N2 variants that have been transmitted to humans in the past years, pose a potential threat, particularly to children. Serological studies with human serum samples demonstrate that while a significant proportion of adolescents and young adults have cross-reactive antibodies against A(H3N2)v viruses, young children lack such preexisting immunity (35, 36). Investigations in the ferret model suggest that vaccination with seasonal trivalent inactivated influenza vaccines does not provide protection against transmission of A(H3N2)v virus (37, 38). These findings highlight the antigenic difference between circulating H3N2 and the swine-origin viruses and the need to evaluate and approve A(H3N2)v vaccines. In this study, we identified amino acids in the HA of MN/10, the A(H3N2)v vaccine candidate, that explain why this virus is antigenically distinct from an ancestral human seasonal H3N2 strain, BJ/92. In addition, we demonstrated that the amino acid substitutions that confer the antigenic phenotype impact both receptor specificity and antibody binding. Our findings provide additional evidence that residues near the HA RBS, especially those in antigenic site B, play significant role in the antigenic evolution of H3N2 viruses (23, 24).
FIG 5Binding of MN/10 and BJ/92 viruses by a panel of HA-specific MAbs. The binding was measured by ELISA with plates coated with the indicated wt and mutant viruses and was detected by each MAb (1g/ml) and peroxidase-conjugated anti-mouse IgG. Serum from the mouse immunized for MAb generation, which has an HI titer of 640 against wt MN/10, was included as a positive control. The OD490 values generated with mutant viruses and wt BJ/92 were normalized to those of wt MN/10 virus. Shown are the averages from 2 independent assays run in duplicate wells, and standard deviations are indicated by error bars.
on November 7, 2019 by guest
http://jvi.asm.org/
[image:10.585.49.473.73.306.2]Seasonal H3N2 viruses experience antigenic drift, which necessitates frequent up-dates of H3N2 candidate viruses for seasonal influenza vaccines (24, 29). Antigenic drift of H3N2 viruses is often due to single- or double-amino-acid mutations at several positions in the HA, e.g., 145, 155, 156, 158, 189, and 193 (24). A similar antigenic drift mechanism was also observed in H1N1 and H5N1 viruses (39, 40). However, evolution over longer periods of time may result in a larger number of amino acid changes in antigenic sites. For example, 5 amino acid substitutions are responsible for the anti-genic divergence from the 1968 to 2002 H3N2 viruses (A/Hong Kong/1/1968 to A/Fujian/411/2002) (24). Consistent with this observation, our data from this study indicate that at least 4 or 5 amino acid mutations are needed to switch the antigenic phenotypes between A(H3N2)v and the ancestral seasonal H3N2 viruses. This may be due to multiple reasons. First, it has been⬃20 years since the introduction of human H3N2 viruses into the U.S. swine population. Multiple antigenic drifts could have occurred during the evolution in such a long period. Furthermore, swine represent a very different evolutionary host from humans in terms of physiology, life span, vacci-nation regime, etc. Some of the residues that are associated with the antigenic difference might also be the result of host adaptation. Indeed, the residues critical for the antigenic difference between MN/10 and BJ/92 are also associated with the receptor binding property of the viruses. Taken together, both the long term antigenic evolution and host adaptation might have determined the molecular basis for the observed antigenic difference between A(H3N2)v and seasonal H3N2 viruses. These changes are not as simple as the antigenic drift seen in human seasonal influenza viruses, which is often caused by a single amino acid mutation in the HA.
The amino acid residues identified in the present study as critical for the antigenic difference between A(H3N2)v and seasonal H3N2 viruses are all located near the RBS in HA, which is in agreement with the observations in other studies that examined H3N2 antigenic evolution (19, 23, 24). Our study indicated that the amino acid mutations which switched the antigenic phenotype of MN/10 and BJ/92 influenced receptor binding. Moreover, these mutations have a profound direct impact on binding of the HA by mouse MAbs. Consistent with this finding, mutations at these residues have also been found to impact the binding by human MAbs (41). Taken together, the antigenic difference between MN/10 and BJ/92 is likely the result of changes in receptor binding avidity as well as antibody selection. Interestingly, all of the identified critical residues are located within antigenic site B, adding evidence that residue substitutions in antigenic site B more frequently impact antibody recognition than those in antigenic site A. It was somewhat surprising that antigenic site B is the primary target of both MN/10 and BJ/92 ferret antisera, since there are a number of additional amino acid differences between these HAs. The fact that antigenic site A of A(H3N2)v viruses also included residue substitutions suggests that selective pressure is present on this antigenic site during the evolution of H3N2 in swine. A very recent study reported the isolation of human antibody H3v-41, which binds antigenic site A (41), demonstrating that immunity against antigenic site A was induced in humans vaccinated against A(H3N2)v. In our study, one of the escape mutants selected by mouse MAb HE42 bears an N-to-K mutation at residue 145, suggesting that antigenic site A is also targeted by the mouse immune response. The reason why ferret antisera identify residues within antigenic site B as the major determinants for the antigenic difference between MN/10 and BJ/92 viruses deserves further investigation.
Ferret antisera are routinely used in HI assays to characterize the antigenic pheno-type of influenza viruses. Since these sera are collected from ferrets recovering from primary influenza virus infection, it is likely that the specificity and avidity of antibodies may differ from those of human antisera. For instance, serological assays with human antiserum samples can discriminate between K166 and Q166 in the HA of H1N1 viruses; this difference was not detected by ferret antisera (42). The K166Q mutation has been proposed to be one of the reasons for the increased morbidity and mortality caused by influenza among middle-aged people during the 2013-2014 influenza season (42). In light of this observation, a comprehensive analysis of data generated with both ferret
on November 7, 2019 by guest
http://jvi.asm.org/
and human antisera might facilitate a better understanding of influenza virus evolution as well as decisions to update influenza vaccines.
Our results show that residue 157, which is not often reported to be involved in antigenic evolution, also played a role in determining the antigenic difference between A(H3N2)v and seasonal H3N2 viruses. Our ELISA data demonstrated that residue 157, in combination with the neighboring and adjacent residues, e.g., 156, 158, 189, and 193, has a direct impact on the binding of antibodies such as HB1 to HA. This residue was also observed to influence the receptor binding avidity of the BJ/92 mutant to certain glycans (e.g., Neu5Gc-Tn and 6-SiaTF). Residue 157 is within the 150-loop that consti-tutes the RBS, and is in close proximity to other residues (e.g., those in 190-helix) that are critical for the antigenic phenotype, so it is not surprising that it may also interact with antibodies and contribute to the avidity of HA when binding to some glycans. Regardless of the reasons why particular amino acid changes were selected during the evolution of MN/10, our results show that residues in antigenic site B, especially those at positions 156, 157, 158, 189 and 193, deserve close monitoring in surveillance and risk assessment of emerging H3N2 viruses.
Previous studies have shown that HA mutations can decrease HI antibody activity by increasing the viral HA binding avidity to cell surface glycan receptors (43, 44). Our data identified MN/10 and BJ/92 mutants that switched both their antigenic and receptor binding phenotypes to those of the heterologous virus, suggesting that a change in receptor binding affinity can impact antigenicity. Similarly, Hensley et al. (45) demon-strated a positive correlation between receptor binding avidity and escape from polyclonal antibodies by H1 influenza viruses, indicating that variations in receptor binding support the emergence of antibody-selected mutants. Interestingly, our data indicate a significant positive correlation between HI titers of MN/10 antiserum and binding to SiaTn and 6-SiaTF sialylglycopolymers. These results suggest that changes in receptor binding properties correlate with antigenic structure (35), and therefore both host adaptation and immune selection are likely to contribute to the antigenic differ-ences between A(H3N2)v and seasonal H3N2 viruses.
In conclusion, the results we present in this report confirm that A(H3N2)v viruses are antigenically distinct from the ancestral seasonal H3N2 strains that circulated in the early 1990s and identify multiple amino acids in antigenic site B of HA that are critical for this antigenic difference. This is in agreement with previous observations that substitutions near the HA RBS determine antigenic changes during influenza virus evolution. Our findings define the molecular basis for the unique antigenic phenotype of A(H3N2)v viruses and may facilitate future surveillance and risk assessment of novel influenza viruses.
MATERIALS AND METHODS
wt viruses and ferret sera.A(H3N2)v virus A/Minnesota/11/2010 (MN/10) and seasonal H3N2 virus A/Beijing/32/1992 (BJ/92) were grown in 11-day-old embryonated specific-pathogen-free (SPF) chicken eggs and stored at⫺70°C until use. Ferret sera against MN/10 and BJ/92 were generated by intranasal infection of ferrets with MN/10 or BJ/92 virus following protocols approved by the Center for Biologics Evaluation and Research (CBER) Animal Care and Use Committee. Briefly, ferrets were anesthetized with a mixture of ketamine and xylazine intramuscularly and inoculated intranasally with 107median tissue culture infectious doses (TCID50) of MN/10 or BJ/92 virus diluted in 1 ml phosphate-buffered saline (PBS) (0.5 ml/nostril). Ferrets were bled 3 weeks after the infection, and the sera were stored at⫺30°C. Sera collected from 4 ferrets, 2 for MN/10 antiserum and 2 for BJ/92 antiserum, were used in the studies.
Site-directed mutagenesis.Nucleotide changes corresponding to single or multiple amino acid mutations were introduced into the HA gene in plasmid pHW2000 with the QuikChange multi site-directed mutagenesis kit (Stratagene, La Jolla, CA). The resulting plasmids were sequenced to verify the presence of introduced mutations and the absence of additional, unwanted mutations.
Reverse genetics.Reassortant MN/10 and BJ/92 viruses that bear the wt or mutant HA and NA genes of MN/10 or BJ/92 and the internal genes of the H1N1 virus PR8 were generated as previously reported (46, 47). Briefly, plasmids (1g each) containing each of the 8 virus genes were transfected into a mixture of 293T human embryonic kidney cells and Madin-Darby canine kidney (MDCK) cells. The transfection mixture was replaced with Opti-MEM I medium (Invitrogen, Grand Island, NY) after 6 h of incubation at 37°C. Opti-MEM I medium supplemented with 1g/ml trypsin was added 24 h later. At 48 to 72 h posttransfection, the culture supernatant was collected and propagated in 11-day-old embryonated SPF chicken eggs.
on November 7, 2019 by guest
http://jvi.asm.org/
HI assay.The antigenic phenotypes of wt and reassortant viruses were determined by performing HI assays. Briefly, ferret sera were treated overnight at 37°C with receptor-destroying enzyme fromVibrio cholerae
(Denka Seiken, Tokyo, Japan) and then heat inactivated at 56°C for 30 min. After dilution with PBS to 1:10, the sera were absorbed with packed turkey red blood cells to remove nonspecific inhibitors and then serially diluted before mixing with 4 hemagglutination units of virus and 0.5% turkey red blood cells. Two indepen-dent HI assays were performed for each virus, and the geometric mean titers were calculated.
Receptor binding assay.The affinity of each virus for biotinylated 6=-sialylglycopolymers was measured in a direct binding assay as described previously (48). Briefly, plates were coated with 4 to 8 hemagglutination units of each virus at 4°C for 16 h, followed by washing with 0.05% Tween 20 in phosphate-buffered saline (PBS-T). After the addition of biotinylated sialylglycopolymer in PBS supple-mented with 0.02% Tween 20, 0.02% bovine serum albumin (BSA), and 3M oseltamivir carboxylate, plates were incubated at 4°C for 1 h. Plates were then washed with cold PBS-T and incubated with streptavidin-peroxidase (Sigma-Aldrich, St. Louis, MO) at 4°C for 1 h. After washing, tetramethylbenzidine (TMB) substrate solution (KPL, Gaithersburg, MD) was added, and the reaction was stopped with TMB stop solution (KPL, Gaithersburg, MD). Optical density was determined at 450 nm with a Synergy 2 multimode microplate reader (BioTek Instruments, Winooski, VT). The dissociation constants (Kds) were determined by Scatchard plot analysis;Kdwas defined as the sialic acid concentration (M Neu5Ac) at 1/2 theAmax, whereAmaxrepresents maximum absorbance. The reported data represent the mean of at least four individual experiments for each virus.
Generation of MAbs against the HA of MN/10 virus.A panel of HA-specific mouse MAbs was used in the analysis of antibody binding to viruses. Hybridomas that secrete MAbs were generated through immunizing BALB/c mice (The Jackson Laboratory, Bar Harbor, ME) with inactivated MN/10 virus and fusing splenocytes from an immunized mouse with Sp2/0 cells. The HA specificity of MAbs was confirmed by ELISA using 293T cells transfected with an HA-expressing plasmid (pCAGGS-MN/10 HA) as the antigen (49). Selected hybridomas were cultured in a CELLine device (BD Biosciences, San Jose, CA) and the MAbs purified using protein G columns (GE Healthcare, Uppsala, Sweden). The key residues in HA for antibody binding were identified by sequencing the HA genes of escape mutants of MN/10 virus, which were selected in 11-day-old embryonated SPF chicken eggs in the presence of MAb (49).
Antibody binding assay.The binding of viruses by MAbs was measured by ELISA. Briefly, purified wt and mutant viruses were applied to Immulon 2HB microtiter plates (Thermo Scientific, Rochester, NY) at 1g/well. The virus-coated plates were blocked with 1% BSA in PBS and then incubated with each MAb (1 g/ml) in 1% BSA–PBS-T. After an additional incubation with peroxidase-conjugated goat anti-mouse IgG (Sigma-Aldrich, St. Louis, MO), the signal was developed usingo-phenylenediamine dihydrochloride (OPD) as the substrate. The reaction was stopped with 1N H2SO4, and OD490values were read. The OD490values of mutant viruses and wt BJ/92 were normalized to those of wt MN/10. Two independent assays were performed, and each was run in duplicate wells.
Gene sequencing and alignment. The HA gene of each virus was sequenced to confirm the expected mutations. Viral RNA was extracted from infectious allantoic fluid with an RNeasy minikit (Qiagen, Valencia, CA). cDNA synthesis and PCR were performed as previously described (50) to amplify the HA gene. PCR products were sequenced at the Facility for Biotechnology Resources, CBER, FDA. DNA and amino acid sequences were analyzed with DNAStar Lasergene software version 13 (DNAStar, Inc., Madison, WI).
Statistical analysis.TheKdvalues were compared by analysis of variance (ANOVA). Probability values ofⱕ0.05 indicate statistically significant differences. Associations between HI titers and receptor binding affinity were evaluated using the Spearman correlation test.
ACKNOWLEDGMENTS
We thank Robert G. Webster (St. Jude Children’s Research Hospital, Memphis, TN) for providing plasmids used to generate influenza viruses by reverse genetics. We are indebted to staff of the Division of Veterinary Services, CBER, FDA, for excellent animal care and the Facility for Biotechnology Resources, CBER, FDA, for sequence analyses.
This study was supported by intramural FDA funds and by RAS Presidium Grant Molecular and Cell Biology to N.V.B.
REFERENCES
1. Neumann G, Noda T, Kawaoka Y. 2009. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 459:931–939. https://doi.org/10.1038/nature08157.
2. Lindstrom S, Garten R, Balish A, Shu B, Emery S, Berman L, Barnes N, Sleeman K, Gubareva L, Villanueva J, Klimov A. 2012. Human infections with novel reassortant influenza A(H3N2)v viruses, United States, 2011. Emerg Infect Dis 18:834 – 837. https://doi.org/10.3201/eid1805.111922. 3. Shu B, Garten R, Emery S, Balish A, Cooper L, Sessions W, Deyde V, Smith
C, Berman L, Klimov A, Lindstrom S, Xu X. 2012. Genetic analysis and antigenic characterization of swine origin influenza viruses isolated from humans in the United States, 1990-2010. Virology 422:151–160. https:// doi.org/10.1016/j.virol.2011.10.016.
4. Wong KK, Greenbaum A, Moll ME, Lando J, Moore EL, Ganatra R, Big-gerstaff M, Lam E, Smith EE, Storms AD, Miller JR, Dato V, Nalluswami K, Nambiar A, Silvestri SA, Lute JR, Ostroff S, Hancock K, Branch A, Trock SC, Klimov A, Shu B, Brammer L, Epperson S, Finelli L, Jhung MA. 2012. Outbreak of influenza A (H3N2) variant virus infection among attendees of an agricultural fair, Pennsylvania, USA, 2011. Emerg Infect Dis 18: 1937–1944. https://doi.org/10.3201/eid1812.121097.
5. CDC. 2012. Update: influenza activity—United States and worldwide, May 20-September 22, 2012. MMWR Morb Mortal Wkly Rep 61:785–789. 6. Johnson C, Hohenboken M, Poling T, Jaehnig P, Kanesa-Thasan N. 2015. Safety and immunogenicity of cell culture-derived A/H3N2 variant influenza vaccines: a phase I randomized, observer-blind,
on November 7, 2019 by guest
http://jvi.asm.org/
dose-ranging study. J Infect Dis 212:72– 80. https://doi.org/10.1093/ infdis/jiu826.
7. CDC. 2011. Limited human-to-human transmission of novel influenza A (H3N2) virus—Iowa, November 2011. MMWR Morb Mortal Wkly Rep 60:1615–1617.
8. Greenbaum A, Quinn C, Bailer J, Su S, Havers F, Durand LO, Jiang V, Page S, Budd J, Shaw M, Biggerstaff M, de Fijter S, Smith K, Reed C, Epperson S, Brammer L, Feltz D, Sohner K, Ford J, Jain S, Gargiullo P, Weiss E, Burg P, DiOrio M, Fowler B, Finelli L, Jhung MA. 2015. Investigation of an outbreak of variant influenza A(H3N2) virus infection associated with an agricultural fair—Ohio, August 2012. J Infect Dis 212:1592–1599. https:// doi.org/10.1093/infdis/jiv269.
9. CDC. 2012. Influenza A (H3N2) variant virus-related hospitalizations: Ohio, 2012. MMWR Morb Mortal Wkly Rep 61:764 –767.
10. Biggerstaff M, Reed C, Epperson S, Jhung MA, Gambhir M, Bresee JS, Jernigan DB, Swerdlow DL, Finelli L. 2013. Estimates of the number of human infections with influenza A(H3N2) variant virus, United States, August 2011-April 2012. Clin Infect Dis 57(Suppl 1):S12–S15. https:// doi.org/10.1093/cid/cit273.
11. Webby RJ, Swenson SL, Krauss SL, Gerrish PJ, Goyal SM, Webster RG. 2000. Evolution of swine H3N2 influenza viruses in the United States. J Virol 74:8243– 8251. https://doi.org/10.1128/JVI.74.18.8243-8251.2000. 12. Kitikoon P, Gauger PC, Anderson TK, Culhane MR, Swenson S, Loving CL,
Perez DR, Vincent AL. 2013. Swine influenza virus vaccine serologic cross-reactivity to contemporary US swine H3N2 and efficacy in pigs infected with an H3N2 similar to 2011-2012 H3N2v. Influenza Other Respir Viruses 7(Suppl 4):S32–S41.
13. Kitikoon P, Vincent AL, Gauger PC, Schlink SN, Bayles DO, Gramer MR, Darnell D, Webby RJ, Lager KM, Swenson SL, Klimov A. 2012. Pathoge-nicity and transmission in pigs of the novel A(H3N2)v influenza virus isolated from humans and characterization of swine H3N2 viruses iso-lated in 2010-2011. J Virol 86:6804 – 6814. https://doi.org/10.1128/ JVI.00197-12.
14. Zhou NN, Senne DA, Landgraf JS, Swenson SL, Erickson G, Rossow K, Liu L, Yoon K, Krauss S, Webster RG. 1999. Genetic reassortment of avian, swine, and human influenza A viruses in American pigs. J Virol 73: 8851– 8856.
15. Lina B, Bouscambert M, Enouf V, Rousset D, Valette M, van der Werf S. 2011. S-OtrH3N2 viruses: use of sequence data for description of the molecular characteristics of the viruses and their relatedness to previ-ously circulating H3N2 human viruses. Euro Surveill 16(50):pii⫽20039. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId⫽20039. 16. Lorusso A, Vincent AL, Gramer ME, Lager KM, Ciacci-Zanella JR. 2013.
Contemporary epidemiology of North American lineage triple reas-sortant influenza A viruses in pigs. Curr Top Microbiol Immunol 370: 113–132.
17. Olsen CW, Karasin AI, Carman S, Li Y, Bastien N, Ojkic D, Alves D, Charbonneau G, Henning BM, Low DE, Burton L, Broukhanski G. 2006. Triple reassortant H3N2 influenza A viruses, Canada, 2005. Emerg Infect Dis 12:1132–1135. https://doi.org/10.3201/eid1207.060268.
18. Grgic H, Costa M, Friendship RM, Carman S, Nagy E, Wideman G, Weese S, Poljak Z. 2014. Molecular characterization of H3N2 influenza A viruses isolated from Ontario swine in 2011 and 2012. Virol J 11:194. https:// doi.org/10.1186/s12985-014-0194-z.
19. Lewis NS, Anderson TK, Kitikoon P, Skepner E, Burke DF, Vincent AL. 2014. Substitutions near the hemagglutinin receptor-binding site deter-mine the antigenic evolution of influenza A H3N2 viruses in U.S. swine. J Virol 88:4752– 4763. https://doi.org/10.1128/JVI.03805-13.
20. Finelli L, Swerdlow DL. 2013. The emergence of influenza A (H3N2)v virus: what we learned from the first wave. Clin Infect Dis 57(Suppl 1):S1–S3. https://doi.org/10.1093/cid/cit324.
21. Ma J, Shen H, Liu Q, Bawa B, Qi W, Duff M, Lang Y, Lee J, Yu H, Bai J, Tong G, Hesse RA, Richt JA, Ma W. 2015. Pathogenicity and transmissibility of novel reassortant H3N2 influenza viruses with 2009 pandemic H1N1 genes in pigs. J Virol 89:2831–2841. https://doi.org/10.1128/JVI.03355-14. 22. Chou YY, Albrecht RA, Pica N, Lowen AC, Richt JA, Garcia-Sastre A, Palese
P, Hai R. 2011. The M segment of the 2009 new pandemic H1N1 influenza virus is critical for its high transmission efficiency in the guinea pig model. J Virol 85:11235–11241. https://doi.org/10.1128/JVI.05794-11. 23. Abente EJ, Santos J, Lewis NS, Gauger PC, Stratton J, Skepner E, Ander-son TK, Rajao DS, Perez DR, Vincent AL. 2016. The molecular determi-nants of antibody recognition and antigenic drift in the H3 hemagglu-tinin of swine influenza A virus. J Virol 90:8266 – 8280. https://doi.org/ 10.1128/JVI.01002-16.
24. Koel BF, Burke DF, Bestebroer TM, van der Vliet S, Zondag GC, Vervaet G, Skepner E, Lewis NS, Spronken MI, Russell CA, Eropkin MY, Hurt AC, Barr IG, de Jong JC, Rimmelzwaan GF, Osterhaus AD, Fouchier RA, Smith DJ. 2013. Substitutions near the receptor binding site determine major antigenic change during influenza virus evolution. Science 342:976 –979. https://doi.org/10.1126/science.1244730.
25. Smith DJ, Lapedes AS, de Jong JC, Bestebroer TM, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2004. Mapping the antigenic and genetic evolution of influenza virus. Science 305:371–376. https://doi.org/ 10.1126/science.1097211.
26. Tewawong N, Prachayangprecha S, Vichiwattana P, Korkong S, Klinfueng S, Vongpunsawad S, Thongmee T, Theamboonlers A, Poovorawan Y. 2015. Assessing antigenic drift of seasonal influenza A(H3N2) and A(H1N1)pdm09 viruses. PLoS One 10:e0139958. https://doi.org/10.1371/ journal.pone.0139958.
27. Rajao DS, Gauger PC, Anderson TK, Lewis NS, Abente EJ, Killian ML, Perez DR, Sutton TC, Zhang J, Vincent AL. 2015. Novel reassortant human-like H3N2 and H3N1 influenza A viruses detected in pigs are virulent and antigenically distinct from swine viruses endemic to the United States. J Virol 89:11213–11222. https://doi.org/10.1128/JVI.01675-15.
28. Huang JW, Yang JM. 2011. Changed epitopes drive the antigenic drift for influenza A (H3N2) viruses. BMC Bioinformatics 12(Suppl 1):S31. https:// doi.org/10.1186/1471-2105-12-S1-S31.
29. Chambers BS, Parkhouse K, Ross TM, Alby K, Hensley SE. 2015. Identifi-cation of hemagglutinin residues responsible for H3N2 antigenic drift during the 2014-2015 influenza season. Cell Rep 12:1– 6. https://doi.org/ 10.1016/j.celrep.2015.06.005.
30. Walther T, Karamanska R, Chan RW, Chan MC, Jia N, Air G, Hopton C, Wong MP, Dell A, Malik Peiris JS, Haslam SM, Nicholls JM. 2013. Glycomic analysis of human respiratory tract tissues and correlation with influenza virus infection. PLoS Pathog 9:e1003223. https://doi.org/10.1371/ journal.ppat.1003223.
31. Burlak C, Bern M, Brito AE, Isailovic D, Wang ZY, Estrada JL, Li P, Tector AJ. 2013. N-linked glycan profiling of GGTA1/CMAH knockout pigs iden-tifies new potential carbohydrate xenoantigens. Xenotransplantation 20:277–291. https://doi.org/10.1111/xen.12047.
32. Bateman AC, Karamanska R, Busch MG, Dell A, Olsen CW, Haslam SM. 2010. Glycan analysis and influenza A virus infection of primary swine respiratory epithelial cells: the importance of NeuAc␣2-6 glycans. J Biol Chem 285:34016 –34026. https://doi.org/10.1074/jbc.M110.115998. 33. Ju T, Wang Y, Aryal RP, Lehoux SD, Ding X, Kudelka MR, Cutler C, Zeng
J, Wang J, Sun X, Heimburg-Molinaro J, Smith DF, Cummings RD. 2013. Tn and sialyl-Tn antigens, aberrant O-glycomics as human disease mark-ers. Proteomics Clin Appl 7:618 – 631. https://doi.org/10.1002/ prca.201300024.
34. Cao Y, Karsten U. 2001. Binding patterns of 51 monoclonal antibodies to peptide and carbohydrate epitopes of the epithelial mucin (MUC1) on tissue sections of adenolymphomas of the parotid (Warthin’s tumours): role of epitope masking by glycans. Histochem Cell Biol 115:349 –356. 35. Waalen K, Kilander A, Dudman SG, Ramos-Ocao R, Hungnes O. 2012.
Age-dependent prevalence of antibodies cross-reactive to the influenza A(H3N2) variant virus in sera collected in Norway in 2011. Euro Surveill 17(19):pii⫽20170. http://www.eurosurveillance.org/ViewArticle .aspx?ArticleId⫽20170.
36. CDC. 2012. Antibodies cross-reactive to influenza A (H3N2) variant virus and impact of 2010-11 seasonal influenza vaccine on cross-reactive antibodies—United States. MMWR Morb Mortal Wkly Rep 61:237–241. 37. Houser KV, Pearce MB, Katz JM, Tumpey TM. 2013. Impact of prior
seasonal H3N2 influenza vaccination or infection on protection and transmission of emerging variants of influenza A(H3N2)v virus in ferrets. J Virol 87:13480 –13489. https://doi.org/10.1128/JVI.02434-13. 38. Houser KV, Katz JM, Tumpey TM. 2013. Seasonal trivalent inactivated
influenza vaccine does not protect against newly emerging variants of influenza A (H3N2v) virus in ferrets. J Virol 87:1261–1263. https://doi.org/ 10.1128/JVI.02625-12.
39. Koel BF, van der Vliet S, Burke DF, Bestebroer TM, Bharoto EE, Yasa IW, Herliana I, Laksono BM, Xu K, Skepner E, Russell CA, Rimmelzwaan GF, Perez DR, Osterhaus AD, Smith DJ, Prajitno TY, Fouchier RA. 2014. Antigenic variation of clade 2.1 H5N1 virus is determined by a few amino acid substitutions immediately adjacent to the receptor binding site. mBio 5:e01070 –14. https://doi.org/10.1128/mBio.01070-14.
40. Koel BF, Mogling R, Chutinimitkul S, Fraaij PL, Burke DF, van der Vliet S, de Wit E, Bestebroer TM, Rimmelzwaan GF, Osterhaus AD, Smith DJ, Fouchier RA, de Graaf M. 2015. Identification of amino acid substitutions
on November 7, 2019 by guest
http://jvi.asm.org/
supporting antigenic change of influenza A(H1N1)pdm09 viruses. J Virol 89:3763–3775. https://doi.org/10.1128/JVI.02962-14.
41. Bangaru S, Nieusma T, Kose N, Thornburg NJ, Finn JA, Kaplan BS, King HG, Singh V, Lampley RM, Sapparapu G, Cisneros A 3rd, Edwards KM, Slaughter JC, Edupuganti S, Lai L, Richt JA, Webby RJ, Ward AB, Crowe JE, Jr. 2016. Recognition of influenza H3N2 variant virus by human neutralizing antibodies. JCI Insight 1:e86673.
42. Linderman SL, Chambers BS, Zost SJ, Parkhouse K, Li Y, Herrmann C, Ellebedy AH, Carter DM, Andrews SF, Zheng NY, Huang M, Huang Y, Strauss D, Shaz BH, Hodinka RL, Reyes-Teran G, Ross TM, Wilson PC, Ahmed R, Bloom JD, Hensley SE. 2014. Potential antigenic explanation for atypical H1N1 infections among middle-aged adults during the 2013-2014 influenza season. Proc Natl Acad Sci U S A 111:15798 –15803. https://doi.org/10.1073/pnas.1409171111.
43. Kaverin NV, Rudneva IA, Ilyushina NA, Lipatov AS, Krauss S, Webster RG. 2004. Structural differences among hemagglutinins of influenza A virus subtypes are reflected in their antigenic architecture: analysis of H9 escape mutants. J Virol 78:240 –249. https://doi.org/10.1128/JVI.78.1.240 -249.2004.
44. Yewdell JW, Caton AJ, Gerhard W. 1986. Selection of influenza A virus adsorptive mutants by growth in the presence of a mixture of mono-clonal antihemagglutinin antibodies. J Virol 57:623– 628.
45. Hensley SE, Das SR, Bailey AL, Schmidt LM, Hickman HD, Jayaraman A,
Viswanathan K, Raman R, Sasisekharan R, Bennink JR, Yewdell JW. 2009. Hemagglutinin receptor binding avidity drives influenza A virus anti-genic drift. Science 326:734 –736. https://doi.org/10.1126/ science.1178258.
46. Wan H, Perez DR. 2007. Amino acid 226 in the hemagglutinin of H9N2 influenza viruses determines cell tropism and replication in human airway epithelial cells. J Virol 81:5181–5191. https://doi.org/10.1128/ JVI.02827-06.
47. Neumann G, Watanabe T, Ito H, Watanabe S, Goto H, Gao P, Hughes M, Perez DR, Donis R, Hoffmann E, Hobom G, Kawaoka Y. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc Natl Acad Sci U S A 96:9345–9350. https://doi.org/10.1073/pnas.96.16.9345. 48. Gambaryan AS, Matrosovich MN. 1992. A solid-phase enzyme-linked
assay for influenza virus receptor-binding activity. J Virol Methods 39: 111–123. https://doi.org/10.1016/0166-0934(92)90130-6.
49. Wan H, Yang H, Shore DA, Garten RJ, Couzens L, Gao J, Jiang L, Carney PJ, Villanueva J, Stevens J, Eichelberger MC. 2015. Structural character-ization of a protective epitope spanning A(H1N1)pdm09 influenza virus neuraminidase monomers. Nat Commun 6:6114. https://doi.org/ 10.1038/ncomms7114.
50. Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol 146:2275–2289. https://doi.org/10.1007/s007050170002.