“A STUDY ON CLINICO-SEROLOGICAL PREVALENCE OF
SYPHILIS IN PATIENTS WITH HIV/AIDS”
Dissertation submitted in partial fulfillment of the requirements for the degree of
M.D. (DERMATOLOGY, VENEREOLOGY AND LEPROSY)
BRANCH XX
MADRAS MEDICAL COLLEGE CHENNAI.
THE TAMILNADU Dr. MGR MEDICAL UNIVERSITY CHENNAI
CERTIFICATE
Certified that this dissertation titled “CLINICO-SEROLOGICAL
PREVALENCE OF SYPHILIS IN PATIENTS WITH HIV/AIDS” is a
bonafide work done by Dr.M.MUNIRAJ Post graduate student of the
Department of Dermatology, Venereology and Leprosy, Madras Medical
College, Chennai – 3, during the academic year 2016 – 2019. This work has
not previously formed the basis for the award of any degree.
Prof. Dr. S.KALAIVANI, M.D., D.V., Prof.Dr.U.R.DHANALAKSHMI, M.D., DD.,
Director and Professor, Professor and Head,
Institute of Venereology, Department of Dermatology &
Madras Medical College, Leprosy,
Chennai – 600 003. Madras Medical College,
Chennai – 600 003.
Prof. Dr. R. JAYANTHI, M.D., FRCP (Glas).,
DEAN
Madras Medical College,
DECLARATION
The dissertation entitled “CLINICO-SEROLOGICAL
PREVALENCE OF SYPHILIS IN PATIENTS WITH HIV/AIDS” is a
bonafide work done by Dr.M.MUNIRAJ at Department of Dermatology,
Venereology and Leprosy, Madras Medical College, Chennai – 3, during the
academic year 2016 – 2019 under the guidance of Prof. Dr. S. KALAIVANI
M.D.,D.V., Director and Professor, Institute of Venereology, Madras Medical
College, Chennai -3.
This dissertation is submitted to The Tamil Nadu Dr. M.G.R. Medical
University, Chennai towards partial fulfillment of the rules and regulations for
the award of M.D Degree in Dermatology, Venereology and Leprosy
(BRANCH – XX).
Prof. Dr. S. KALAIVANI, M.D., D.V.,
Director and Professor, Institute of Venereology, Madras Medical College, Chennai- 600 003.
DECLARATION
I, Dr.M.MUNIRAJ solemnly declare that this dissertation
titled “CLINICO - SEROLOGICAL PREVALENCE OF SYPHILIS IN
PATIENTS WITH HIV/AIDS” is a bonafide work done by me at Madras Medical College during 2016-2019 under the guidance and supervision of
Prof. Dr. S.KALAIVANI, M.D., D.V., Director and Professor, Institute of
Venereology, Madras Medical College, Chennai-600 003.
This dissertation is submitted to The Tamil Nadu Dr. M.G.R. Medical
University, Chennai towards partial fulfillment of the rules and regulations for
the award of M.D Degree in Dermatology, Venereology and Leprology
(BRANCH – XX).
(DR.M.MUNIRAJ)
PLACE:
SPECIAL ACKNOWLEDGEMENT
My sincere thanks to Prof. Dr. R. JAYANTHI M.D., FRCP (Glas).,
Dean, Madras Medical College, Chennai-3 for allowing me to do this
ACKNOWLEDGEMENT
I am grateful to Prof. Dr.S.KALAIVANI, M.D., D.V., Director and Professor, Institute of Venereology., for her advice, guidance and encouragement for my study. She has been a source of constant motivation and encouragement throughout the study. I am extremely grateful to her for guiding me throughout the study.
I would like to express my sincere and heartfelt gratitude to Professor and Head of the Department of Dermatology, Prof. Dr. U.R. DHANALAKSHMI, M.D., D.D., D.N.B for her kindness and support throughout the study.
I wish to thank Dr. C. VIJAYA BASKAR, M.D., D.C.H., Associate Professor, Institute of Venereology for his guidance.
I sincerely thank Prof. Dr. S. NIRMALA M.D., Professor and HOD, Occupational and Contact Dermatitis for her valuable support.
I sincerely thank Prof. Dr. R. PRIYAVATHANI ANNIE MALATHY, M.D., D.D., D.N.B., M.N.A.M.S., Professor of dermatology for her help and support.
I thank Prof. Dr. AFTAB JAMEELA WAHAB, M.D., D.D., Professor of Dermatology for her advice and encouragement.
I thank Prof. Dr. V. SAMPATH, M.D., D.D., Professor of Dermatology for his advice and encouragement.
I am grateful to Prof. Dr. J. MANJULA, M.D., D.N.B., Professor, Department of Dermatology for her invaluable guidance, help and encouragement.
I humbly thank my Co-Guide Dr.E.BALASUBRAMANIAN, M.D.D.V.L., Assistant Professor, Institute of Venereology for his valuable guidance throughout my work. I would like to express my sincere and heartfelt gratitude for the time which he devoted for my research project.
I also thank my Assistant Professors Dr. P. PRABAHAR, M.D.D.V.L., Dr.H.DHANASELVI, M.D.D.V.L., Dr.K.GAYATHRI, M.D.D.V.L., Dr.R.SNEKAVALLI, M.D.D.V.L., Dr. T. VANATHI, M.D.D.V.L., Dr.T.VASANTHI, M.D.D.V.L., and Dr .C. DURGVATHI, M.D.D.V.L., Institute of Venereology for their able guidance.
I thank Dr. M. SUBHA, M.D (Microbiology)., DGO ., Professor of Serology and Dr.S. HEMALATHA, M.D., for her help and support.
I extend my gratitude to Dr.R.MADHU, M.D.,(DERM)., D.C.H., Dr.V.N.S.AHAMED SHARIFF, M.D.D.V.L., Dr.B.VIJAYALAKHSMI, M.D.D.V.L., Dr.R.MANIPRIYA, M.D.D.V.L., D.C.H., Dr.C.L.CHITRA, M.D.D.V.L., Dr. K.DEEPA, M.D.D.V.L., Dr.S.VENKATESAN DNB.,DD and Dr.S.THAMZIHSELVI, M.D.D.V.L., Assistant professors, Department of Dermatology for their kind support and encouragement.
CONTENTS
Sl. No. Title Page No.
1. INTRODUCTION 1
2. REVIEW OF LITERATURE 2
3. AIMS AND OBJECTIVES 37
4. MATERIALS AND METHODS 38
5. RESULTS 40
6. DISCUSSION 76
7. CONCLUSION 81
ANNEXURES
BIBLIOGRAPHY
CLINICAL IMAGES
MASTER CHART
KEY TO MASTER CHART
INFORMATION SHEET
PATIENT CONSENT FORM
PROFORMA
PLAGIARISM DIGITAL CERTIFICATE
1
INTRODUCTION
Syphilis is a infectious disease caused by Spirochaete Treponema
pallidum. The disease is transmitted mainly by sexual contact. Treponema
pallidum may infect any organ causing an infinite number of clinical
presentations. Human Immunodeficiency Virus (HIV) is the causative agent of
AIDS. HIV can infect and progressively destroy helper ”T”cells, killer ‘T’
cells and macrophages, thus altering the host immune response to other
bacteria, virus and parasites. These two sexually transmitted diseases are of
major public health concern. In this study, we made an effort to analyse
various clinical presentations of syphilis and serological prevalence of syphilis
2
REVIEW OF LITERATURE
“He who knows syphilis, knows medicine”Sir William Osler
DEFINITION (1)
Syphilis was defined by Stokes, as an infectious disease; due to
Treponema pallidum; of great chronicity; systemic from the outset; capable
of involving practically every structure of the body in its course; distinguished
by florid manifestations on the one hand and years of complete asymptomatic
latency on the other hand; able to simulate many diseases in the field of
medicine and surgery; transmissible to off-spring in man; transmissible to
certain laboratory animals and treatable to the point of presumptive cure.(1)
HISTORY OF SYPHILIS (1)
There are two theories regarding the origin of syphilis. One, the
Unitarian theory, according to which the disease originated in the tropics as a
primitive Treponemal disease and later spread to more temperate climates
affecting more advanced communities where transmission by sexual contact
became the usual mode of spread of disease.
The other theory is the Columbian theory, according to which the
disease was brought to Europe with the return of Columbus in 1493 after his
3
From Europe the disease spread to India and Far East through Portuguese
sailors.
The disease acquired its name from a poem “Syphilis sive morbus
gallicus” written in 1530 by an Italian Pathologist Girolamo Fracastoro about
an infected mythical shepherd named Syphilis afflicted with the French
disease as punishment for cursing the gods.
Fritz Schaudinn and Erich Hoffmann in 1905 discovered the spiral
organism in serum from a lesion of secondary syphilis. They reported that
syphilis was caused by a spirochaete which they named “Spirochaeta pallids”.
This work was quickly confirmed when Karl Landsteiner introduced the dark
field method for the detection of organism in 1906.
In 1943, Penicillin which was discovered by Sir Alexander Fleming and
developed by Florey in Oxford, was successfully used by Mahoney and his
colleague to treat syphilis. With the emergence of AIDS epidemic a time has
come, to review the earlier said quotation as ,
4
EPIDEMIOLOGY
Every cases of infectious syphilis should be considered as a potential
source of infection. Syphilis occurs all over the world without any restriction
to any social class.
The factors that operate and interact in acquisition and spread of the
disease are complex in nature. Sexual promiscuity and prostitution are the twin
menaces around which resolve other factors. The population explosion,
migration of people from rural to urban areas, disproportionate male to female
ratio in urban and pilgrim centres, the mushrooming growth of slums in the
cities and towns leading to overcrowding with lower socioeconomic status,
decline in moral values, lack of personal and sexual hygiene, all account for
the spread of disease. The social stigma attached to a sexually transmitted
disease leads to its concealment and aids its spread. The cinema, magazines,
wall posters, exhibits, advertisements, etc. also encourage promiscuity.
In India, prostitution is still an important cause for the spread of STDs.
Economic factors play a considerable role in prostitution particularly among
the underprivileged.
A country’s socioeconomic structure and its functioning determines the
prevalence of syphilis in a community. In India, as well as in other developing
countries, poor reporting systems make it difficult to obtain the exact
incidence and prevalence of syphilis. The reported incidence of early syphilis
among STD patients in India varies from 7.1 to 99.9%. Syphilis is the
5
serological surveys its prevalence ranges from 2.66 to 26.6%. Syphilis is
more common in males than in females. It has been observed that majority of
males continue to be sexually active even after acquiring the infection.(2)
PATHOGENESIS(3)
The complex host microbe interactions that characterize the varied
clinical course of syphilis are poorly understood. The outer membrane of
Treponema pallidum is a phospholipid bilayer through which only a few
antigenic proteins protrude and the major membrane immunogens are
subsurface proteolipids. These structural features, along with a slow doubling
time of 30- 33 hours, result in a delay in host immune response since the
principal immunogens are largely inaccessible as long as the spirochetes
remain intact. This feature undoubtedly plays a role in the organism’s ability to
persist despite an apparently vigorous host immune response and the
development of cross reacting non specific non treponemal antibodies. The
immune response fails to clear the infection in many instances because an
effective Th1 (cellular) response is downregulated in difference to an
ineffective Th2 (humoral) response. In immunologically dysfunctional persons
(eg. those infected with HIV) aggressive and/or persistent chronic infections
are more likely. Spirochetemia can occur throughout the course of Treponema
pallidum infection including asymptomatic stages of incubation and latent
6
CLASSIFICATION
CONGENITAL ACQUIRED
1.Early EARLY SYPHILIS (Infectious)
2.Late 1. Primary
3.Stigmata 2. Secondary
3. Early latent
4. Relapse and Reinfection
LATE SYPHILIS (Non infectious) 1.Late latent
2.Tertiary syphilis
-BENIGN TERTIARY(16%)
-CARDIOVASCULAR(10.4%)
-NEUROSYPHILIS(6.4%).
PRIMARY SYPHILIS
It is characterized by chancre which develops after an incubation
period of 9-90 days (mean 21 days) following infection and is usually
accompanied by regional lymphadenitis.
The primary chancre presents as sharply defined, usually single,
painless genital ulcer with clean surface and indurated base which express
serous exudates on manipulation and is accompanied by bilateral
7
nodes. The primary lesions will heal within three to ten weeks and may go
unnoticed by the patient.(1,4)
SECONDARY SYPHILIS(5)
The lesions of secondary syphilis usually occur six to eight
weeks after the appearance of primary lesions. The lesions are generalized,
affecting the skin and mucous membranes.
Characteristically, these eruptions are non vesicular, non pruritic,
widespread and bilaterally symmetrically distributed.
TYPES OF CUTANEOUS LESIONS IN SECONDARY SYPHILIS (6)
¾ Macular Syphilide.
¾ Papular Syphilide.
¾ Papulo squamous Syphilide.
¾ Pustular Syphilide.
¾ Annular, Corymbose, Papulosquamous, Lichenoid and Lenticular.
MACULAR SYPHILIDE
Appearing at about 8 weeks, the eruption may be pinkish, coppery red,
round or oval in shape distributed chiefly over shoulders, chest, back,
abdomen and flexor surfaces of upper arms. It disappears in few days or
8
PAPULAR SYPHILIDE
Maculopapular rash is most characteristic which appears 3 months post
infection. They present as dull red, non scaly lesion distributed over trunk,
extremities, face and genitals. Lichenoid, nodular and acneiform lesions also
occur.
CORONA VENERIS – Linear arrangement of papules along the forehead
below hairline.
BUSCHKE OLLENDORF SIGN – Deep dermal tenderness can be elicited
over the rash present over bony prominence by pressing the papule directly
with a small blunt object like pin head.
CONDYLOMA LATA
Large fleshy, grayish white, moist, flat topped and broad based
papule and plaque distributed over intertriginous areas like perianal area,
between thigh and scrotum, vulva and perineal regions. It is loaded with
9
HAIR INVOLVEMENT IN SECONDARY LESIONS MAY PRESENT
AS
1. Follicular papular lesions
2. Diffuse alopecia
3. Irregular patches of non scarring hair loss on occipital and parietal
regions of scalp (moth eaten alopecia).
NAILS
Nail involvement may lead to britttle nails, pitting, onycholysis or
shedding.
Nail fold involvement will lead to paronychia.
PAPULO SQUAMOUS SYPHILIDE:
1. Papular eruption in which scaling is prominent and papules coalesce to
form plaque.
2. Presence of scaly plaque may resemble the clinical picture of psoriasis.
LUES MALIGNA (7)
1. Malignant syphilis is an explosive form more prevalent in
immunosuppresed individuals.
2. Characterised by prodrome of fever, headache, muscular pain
10
3. The eruption soon become necrotic resulting in sharply marginated ulcer
with thick rupioid crust.
4. Mucous membrane may be involved and hepatitis may occur.
MUCOSAL PATCH - Grayish white patch in which surface gets eroded
forming a sharply defined superficial erosion surrounded by a dull red
area. Confluence of the lesions form irregular serpiginous erosions
called as ‘SNAIL TRACK ULCERS’ seen in oral and genital
mucosa.
LATENT SYPHILIS (6,8)
The latent period of syphilis follows the secondary stage. By definition
latent syphilis is that stage of syphilis where there are no clinical signs or
symptoms of the disease; the spinal fluid has been examined and its negative,
but the serological tests for syphilis are reactive. This latent period is divided
into early and late. Early means that the disease has been present for less than
two years and late for more than two years.
LATE SYPHILIS(8)
In this stage of syphilis, the following clinical features are encountered.
1. Late latent syphilis.
2. Late benign (Gumma including visceral syphilis).
11
The optic neuritis and optic atrophy are considered as special late entity.
LATE BENIGN SYPHILIS The essential lesion of late benign syphilis is
gumma. Gummas are probably the result of hypersensitivity reactions of
treponemal infection. The most common site are skin, bone and liver, but
nearly any organ may be involved.
Skin lesions may be solitary or multiple, tend to form circles or
segments of circle. They are destructive and chronic. They tend to heal
centrally and extend peripherally. Skin lesions may present as nodular
lesions, psoriasiform lesions or subcutaneous gumma. They heal with tissue
paper scarring.
Bone lesions are usually marked by periosteitis with as sociated
new bone formation, or by gummatous osteitis with bone destruction. Deep
seated boring pain at the site is the commonest symptom. The most common
sites are cranial bones, the tibia and the clavicle.
CARDIOVASCULAR SYPHILIS(8)
Cardiovascular syphilis is usually caused by medial necrosis of
aorta, with aortic dilatation which may extend into valve commissures. The
clinical signs of cardiovascular syphilis are those of aortic insufficiency or
saccular aneurysm of the thoracic aorta. When fully developed, these
12
hypertension, arteriosclerosis and previous rheumatic heart disease is
essential.
Saccular aneurysm of the thoracic aorta is primafacie evidence
of cardiovascular syphilis. Aortic insufficiency with no other valvular lesions
in a person of middle age, with a reactive serological test should be
considered cardiovascular syphilis, until proven otherwise. VDRL titre are
usually low in cardiovascular syphilis.
CENTRAL NERVOUS SYSTEM SYPHILIS(1, 9, 10)
The treponemes usually invade CNS within 3-18months of inoculation
with the organism. Syphilitic invasion of the CNS may be asymptomatically
present throughout the entire course of infection and may present as clinical
neurosyphilis at any point in the natural history of infection beyond the
primary stage. The initial event in the neurosyhilitic infection is a meningitis,
which occurs in 25 percent of all cases of syphilis. Usually, the meningitis is
asymptomatic and can be discovered only by lumbar puncture. This meningitis
may persist in an asymptomatic stage or ultimately after a period of years
leads to either General paresis of insane due to parenchymal involvement of
brain or Tabes doralis due to parenchymatous involvement of spinal cord. In
some cases, however there may be a natural subsidence of the meningitis-
spontaneous regressions. Asymptomatic neurosyphilis can be recognized
13
Examination Of The Cerebrospinal Fluid In Neurosyphilis (11, 12)
The CSF is a sensitive indicator of presence of active neurosyphilitic
infection. The CSF abnormalities consists of
1. Cell count : More than 5 lymphocytes is abnormal.
2. Total proteins : A total protein of more than 40mgs% is usually
abnormal.
3. CSF VDRL : A reactive CSF VDRL is practically always an
indication of central nervous system syphilis, but
not necessarily of its activity. False positive
reactions in the spinal fluid are rare.
4. Increase in gammaglobulin(IgG) - Usually with oligoclonal banding.
The glucose content is usually normal. In general, the cell count may
be expected to return first to normal followed by the protein and finally the
serological test. Early forms of neurosyphilis (meningeal and meningo
vascular) and ocular syphilis (uveitis) were more common in patients who
were inadequately treated for early syphilis than in untreated patients. Partial
therapy cleared most treponemes from the peripheral sites of infection,
organisms remaining in the eye and the central nervous system after
inadequate therapy were then able to multiply unhampered by the immune
14
DIAGNOSIS:
BEDSIDE INVESTIGATIONS(13)
DARK FIELD MICROSCOPY
In a dark field microscope only light rays hitting the organism or
particles at an oblique angle, enter the microscope objective and so the
organism appears bright object which exhibits cork screw movement on a
dark background. The main component of a dark field microscope is the dark
field condenser.
SPECIMEN COLLECTION
ULCER
1. With gloved hands clean the ulcer using a gauze piece soaked in normal
saline. Let the ulcer dry. Hold the ulcer between thumb and index finger.
Allow serous fluid to come out from the ulcer. Transfer the serous fluid
to clean sterile glass slide. Put the cover slip and add drop of oil on the
condenser of dark field microscope and examine the slide immediately.
LYMPH NODE
Lymph nodes commonly affected are inguinal, axillary, cervical,
15
In cases without genital ulcer, lymph node is injected with 0.2
ml of sterile normal saline, then aspiration should be done and aspirated fluid is
examined under dark field microscope for motile treponemes.
GRAM STAIN - To look for gram negative organisms.
TZANCK SMEAR - To look for herpes virus.
TISSUE SMEAR - To look for donovanosis.
SEROLOGICAL TESTS FOR SYPHILIS(14)
NON TREPONEMAL TESTS TREPONEMAL TESTS
Complement fixation
tests(Wasserman reaction)
Flocculation test
-Rapid plasma regain(RPR)
-Venereal Disease Research
Laboratory(VDRL)
-Toluidine Red Unheated Serum
Test(TRUST)
Treponema pallidum immobilization
assay(TPI)
Fluorecent treponemal antibody
absorption(FTA-AbS) test.
Treponema pallidum haemagglutination
assay(TPHA)
Treponema pallidum passive particle
agglutination assay(TPPA)
Enzyme immune assay(EIA)
Western Blot(WB) and Pseudoblots
Automated Chemiluminescence platforms
Chromatographic point of care (POC)tests
16
RAPID PLASMA (15)
The rapid plasma reagin refers to a type of rapid diagnostic test
that looks for non specific antibodies in the blood of patients. The term reagin
means that the test does not look for antibodies against the actual bacterium
but for antibodies against substances released by cells when they are damaged
by Treponema pallidum.
VDRL
Slide Flocculation tests
REQUIREMENTS
1. VDRL antigen (Cardiolipin antigen is an alcoholic solution composed of
0.03% cardiolipin, 0.21% lecithin, 0.9% cholesterol), 0.9% normal
saline, VDRL slide, micropipette.
READING
No Clumps - Non reactive.
Small Clumps - Weakly Reactive.
Medium and large clumps - Strongly reactive.
17
TREPONEMA PALLIDUM HAEMAGGLUTINATION ASSAY (TPHA):
Patient’s Serum + Sheep erythrocytes*
(*Coated with sonically treated T.Pallidum)
Incubate
Agglutination No agglutination
(antibody in serum of patients with syphilis) (no antibody)
Irregular deposition of RBCs in the form of a smooth matt, Clear button type
covering the well. deposit of RBCs.
18
FLUORESCENT TREPONEMAL ANTIBODY ABSORPTION
(FTA-Abs) TEST:
Patient’s serum + sorbent (autoclaved culture of Reiter’s treponeme)
Group reactive antibodies removed
Slide with acetone fixed killed Treponema pallidum
Incubate fluorescein conjugated anti human globulin serum
Dark ground condenser with UV microscope
Antibody to T.pallidum present No antibody to T.pallidum
Fluorescent treponemes No Fluorescent treponemes
19
TREATMENT OF PRIMARY, SECONDARY AND EARLY LATENT
SYPHILIS (15, 16)
RECOMMENDED REGIMEN
- Inj. Benzathine penicillin G 2.4million units intramuscular single dose (1.2
million units deep IM in each buttock) given after testing intradermal
sensitivity for penicillin (or)
Inj.Procaine benzyl penicillin 1.2 million IU daily I.M for 10 days.
All the patients who have syphilis should be tested for HIV infection. If
it is negative, a repeat test should be done after 3 months, especially in areas
where the HIV prevalence is high. Patients with early syphilis who have
features suggestive of meningitis or uveitis should be evaluated for
neurosyphilis.
ALTERNATIVE REGIMEN FOR PENICILLIN ALLERGIC PATIENTS
- Cap. Doxycycline 100mg BD orally for 2weeks (or)
- Tab. Erythromycin 500mg QID orally for 2weeks.
The efficiency of these regimens is not well documented. Hence
frequent follow up of the patients receiving these therapies is essential. The
effectiveness of these therapies in HIV infected patients has not been studied.
Although limited clinical studies suggest that azithromycin and ceftriaxone are
effective in the treatment of syphilis, their use in the clinical practice is yet to
20
FOLLOW UP
EVERY MONTH - FIRST 3 MONTHS.
EVERY 3 MONTH - NEXT 9 MONTHS.
EVERY 6 MONTHS - NEXT 1 YEAR.
There should be fourfold decrease in the non treponemal (VDRL) titre
within 6 months. Patients who have persistent symptoms or recurrence, or who
have four fold increase in the VDRL titre or failure of titre to decline four
fold within 6 months should be re-evaluated for reinfection, treatment failure,
HIV infection or unrecognized CNS infection. All such patients should
undergo a thorough neurological evaluation including CSF analysis and HIV
testing. When they are retreated, they should preferably be given 3 weekly
doses of Inj. Benzathine penicillin G 2.4million units, unless CSF examination
indicates that neurosyphilis is present.
TREATMENT OF LATE LATENT SYPHILIS
All the patients who have latent syphilis should be evaluated for tertiary
syphilis. CSF analysis is clearly indicated if any one of the following criteria is
present.
- CNS or eye changes.
- Evidence of active tertiary syphilis.
- HIV infection.
-Treatment failure.
21
If the CSF analysis shows features of neurosyphilis then the patient
should be treated for the same.
Late latent syphilis should be treated with 3 weekly doses of Inj.
Benzathine Penicillin G 2.4 million units IM after test dose or Inj. Procaine
benzyl penicillin G 1.2 million units IM daily for 20 days.(16)
DOSES IN CHILDREN
Three weekly injection of Benzathine Penicillin G at a dose of 50,000
units per kg body weight upto an adult dose of 2.4million units IM.
FOLLOW-UP
EVERY MONTH - FIRST 3 MONTHS.
EVERY 3 MONTH - NEXT 9 MONTHS.
EVERY 6 MONTHS - NEXT 1 YEAR.
EVERY YEAR - NEXT 3 YEARS.
After treatment, the patient should be re-evaluated for neurosyphilis if
any of the following criteria is present.
- Fourfold increase in the titre of VDRL.
- An initially high VDRL titre(>1.32) failing to decline at least fourfold
within 12-24 months of therapy.
22
ALTERNATIVE REGIMENS FOR PENICILLIN ALLERGIC
PATIENTS
- Cap.Doxycycline 100mg orally BD for 30days or
- Tab. Erythromycin 500mg orally QID for 30days
TREATMENT OF TERTIARY SYPHILIS (GUMMA AND
CARDIOVASCULAR SYPHILIS)
Three weekly doses of Inj. Benzathine Penicillin G 2.4 million units
deep i.m after test dose.
TREATMENT OF NEUROSYPHILIS
Patients with neurosyphilis or syphilitic eye disease in the form of
neuroretinitis, optic neuritis, uveitis or any other cranial nerve palsies should
have CSF examination and be treated with Aqueous crystalline penicillin G
18-24 million units per day administered as 3-4million units IV every 4hours or
continuous infusion for 10to 14 days.
Benzathine penicillin G has no role in the treatment of neurosyphilis as
it does not cross the blood barrier in sufficient quantity.
FOLLOW UP
CSF should be re-examined every 6 months until it becomes normal.
CSF cell count should become normal by 6 months and CSF VDRL and
23
MANAGEMENT OF SEX PARTNERS
The sex partners should be evaluated clinically and serologically and
treated according to the following recommendations.
1. Persons who are exposed within the 90 days preceding the diagnosis of
primary, secondary or early latent syphilis in a sex partner might be
infected even if seronegative; therefore such persons should be treated
with epidose of Inj. Benzathine penicillin 2.4 million units deep i.m
after test dose (single dose).
2. Persons who were exposed >90 days before the diagnosis of primary,
secondary or early latent syphilis in a sex partner should be treated
presumptively if serologic test results are not available immediately and
the opportunity for follow up is uncertain.
3. For purpose of partner notification and presumptive treatment of
exposed sex partners, patients with syphilis of unknown duration who
have high non treponemal serological test titre(>1.32) can be assumed
to have early syphilis. However serologic titre should not be used to
differentiate early from late latent syphilis for the purpose of
determining treatment.
4. Long term sex partners of patients who have latent syphilis should be
evaluated clinically and serologically for syphilis and treated on the
24
ACQUIRED IMMUNE DEFICIENCY SYNDROME
Human immunodeficiency virus (HIV) the aetiological agent
of AIDS belongs to lentivirus, subgroup of the family retroviridae. AIDS was
first reported in the year 1981, a case report of rare disease, pneumocystis
carnii pneumonia and other unusual infections among young homosexual
men. In 1980 Robert Gallo and his colleagues reported the isolation of first
human retro virus which they named Human T cell lymphotropic virus(17)
In 2017, HIV prevalence in India was 0.2 % . Between 2010
and 2017 new infections declined by 27% and AIDS – related deaths more than
halved, falling by 56%. (17)
The three states with the highest HIV prevalence in India are
Manipur, Mizoram and Nagaland. High prevalence districts in Tamil nadu are
Madurai, Chennai, Thiruvallur, Trichy, Tirunelveli, Salem, Coimbatore and
Namakkal. (17)
In 1985, the first commercial ELISA test for the detection of
HIV was developed. In 1986, the first case was detected in Madras Medical
College, Chennai, South India. In 1987, the first drug active against HIV-
Zidovudine was introduced.
HIV 1 is related to virus found in chimpanzee. HIV 2 virus is
25
HIV 1 is divided into 3 groups.
M Group (major) - Most common worldwide.
Subtypes are A, B, C, D, F, G, H, J, K. Different subtypes can combine genetic
material to form a hybrid virus known as circulating recombinant
forms(CRF). Around 89 CRF exist.
N Group (non-M, non-O ) - 20 Group N infections have been recorded.
O Group (Outlier group) - Not usually seen outside of west central
Africa.
WHO CLINICAL DEFINITION
In Africa, AIDS cases reporting is largely based on the WHO clinical
BANGUI definition. Using this definition AIDS in an adult is defined by the
existence of atleast 2 of the major signs associated with atleast 1 minor sign, in
the absence of major causes of immune suppression such as cancer or severe
malnutrition or recognized aetiologies.
MAJOR SIGNS
a. Weight loss >10% of body weight.
b. Chronic diarrhoea >1 month.
26
MINOR SIGNS
a. Persistent cough for more than one month.
b. Generalized pruritic dermatitis.
c. Recurrent Herpes zoster.
d. Oropharyngeal candidiasis.
e. Chronic progressive and disseminated Herpes simplex infection.
f. Generalized lymphadenopathy.
WHO CLINICAL STAGING
PRIMARY HIV INFECTION
Asymptomatic
Acute retroviral syndrome
STAGE 1
Asymptomatic
Persistent generalized lymphadenopathy
STAGE 2
Unexplained weight loss( less than 10% presumed body weight).
Recurrent respiratory tract infection
27
Herpes zoster
Recurrent oral ulceration
Papular pruritic eruptions
Seborrheic dermatitis
STAGE 3
Unexplained weight loss( greater than 10%)
Chronic diarrhoea > 1 month
Unexplained fever > 1 month
Persistant oral candidiasis
Oral hairy leukoplakia
Pulmonray Tuberculosis( CURRENT)
Unexplained anaemia, neutropenia, thrombocytopenia
STAGE 4
HIV wasting syndrome
Pneumocystic Carinii Pneumonia
Severe bacterial pneumonia
Chronic herpes infection
Oesophageal candidiasis
Kaposi sarcoma
CMV infection
28
Disseminated mycosis
HIV encephalopathy.
DIAGNOSIS OF HIV
Direct predictors of HIV
1.Antibody detection.
2.Antigen detection :p24 antigen.
3. Detection of viral nucleic acid.
4.Virus isolation.
Indirect predictors of HIV
1.Total and differential leukocyte count
2. T- lymphocyte subset assays.
3. Platelet count.
4. IgG and IgA levels.
5.Skin test for CMI.
SCREENING TEST
ELISA AND RAPID TEST
ENZYME LINKED IMMUNOSORBENT ASSAY (ELISA) (18)
It detects IgG and uses indirect, sandwich, or competitive
methodologies. Serological test for the detection of HIV are classified as first
to fourth generation test based on the type of antigens used and the principle of
29
GENERATION ANTIGENS COMMENTS
FIRST Antigens from HIV lysates. Lack of sensitivity and
specificity.
SECOND Recombinant proteins and or
synthetic peptides.
Improved sensitivity.
THIRD Recombinant proteins and or
synthetic peptides in an antigen
sandwich configuration.
Very high
sensitivity;reduces window
period;detects HIV 1 and
HIV 2 separately.
FOURTH Detection of both HIV antigens
and antibodies .
Further reducing the
window periods.
FALSE POSITIVE
Autoimmune diseases
Alcoholic hepatitis
Primary biliary cirrhosis
Leprosy
30
FALSE NEGATIVE
Technical error.
Window period
RAPID TEST
NACO recommends the use of rapid test kits which detects >99.5% of
all HIV infected individuals and have false positive results < 2% of all
those who are tested.
TYPES
Immunoconcentration (Vertical flow).
Agglutination assay.
Immunochromatographic assay.
Dipstick comb assay on Enzyme immune assay.
Enzyme linked immunosorbent assay
MOLECULAR ANALYSIS (18)
Nucleic acid amplification test (NAAT) includes test for the
qualitative detection of HIV 1 DNA or RNA as well as quantitative detection
of HIV 1 RNA through various assays. Though positive NAAT result confirm
HIV diagnosis, the NAAT result may turn out negative if tested within 7 to 10
days of exposure. NACO does not recommend the use of NAAT during acute
31
QUALITATIVE PCR FOR HIV DNA
In infants the sensitivity for detection of HIV DNA is 100 % at
4 to 6 weeks of age.
QUALITATIVE TRANSCRIPTION MEDIATED AMPLIFICATION
FOR HIV-1 RNA
Sensitivity is 100% at 6 to 12 weeks of age.
p24 Antigen(16,18)
The HIV p24 antigen is present as either an immune complex,
with anti p24 antibodies or as free p24 antigen in the blood of infected
individuals. The positive p24 test confirms diagnosis of HIV infection. p24
antigen increases to detectable levels between 1 and 3 weeks after HIV
infection. However negative test does not rules out HIV infection. This test is
based on ELISA.
SYPHILIS AND HIV CO-INFECTION
The interaction between syphilis and HIV co infection is complex and
remained incompletely understood despite there being more than 2 decades of
clinical experience with co-infected patients. The increase in the rate of
syphilis and other sexually transmitted diseases among MSM represent a
32
PATHOGENESIS
Effect of syphilis over HIV(19)
1. Syphilitic genital ulcers are cofactors for the bidirectional transmission of
HIV.
2. Virulent Treponema pallidum and /or its abundant membrane lipoproteins
(NTP 47) induce HIV-1 gene expression and production in chronically
infected macrophages via NF-kB activation, leading to the progression of HIV
infection.
3. Syphilis causes transient increase in viral load and decrease in CD4 cell
count but that recedes after infection is treated. The transient increase in viral
load constitute to the increased rise of HIV transmission among patients with
concordant HIV infection and syphilis.
EFFECT OF HIV OVER SYPHILIS.(19)
1. HIV infection reduces the immunologic responses to treponemal infection,
both cell-mediated and humoral immunity, which impairs the host defence
against syphilis and facilitate its progression.
2.Transient immunosuppression during the early stage of syphilis has a
similar effect on host defences against HIV, leading to a synergistic
immunosuppressive state as manifested by a decrease invitro lymphocyte
33
CLINICAL PRESENTATIONS
1. Despite minor difference, syphilis presents similarly in HIV infected and
HIV uninfected patients.
2. In primary syphilis, HIV infected patients may present with multiple
chancre and with larger and deeper lesions.
3. Rapid progression from primary to secondary stage of syphilis.
Approximately one fourth of HIV infected patients presents with concomitant
lesions of both primary and secondary stage of syphilis at time of diagnosis.
4. In secondary stage papular or nodular eruptions, nodulo ulcerative lesions
with necrotic centre(LUES MALIGNA). These skin lesions have been
characterized as more aggressive forms of secondary syphilis in HIV infected
persons.
5. NEUROSYPHILIS IN HIV (20)
Approximately 35% of persons with secondary syphilis have
asymptomatic CNS involvement. Most cases of symptomatic neurosyphilis
reported among HIV infected persons are acute syphilitic meningitis and
meningovascular neurosyphilis.
A case report of medial medullary syndrome with neurovascular
34
reported in a HIV infected workers who had been exposed 7years earlier.
Other cases of syphilitic meningomyelitic with sporadic parapareisis,
syphilitic poyradiculopathy with progressive leg pain and weakness are also
reported.
Ocular and otolgic complications have been reported widely. The most
common ocular finding in patients with concurrent HIV infection is retinitis
followed by uveitis, chorioretinitis, retro bulbar neuritis, papillitis and optic
neuronitis.
Otolgic syphilis- sensorineural hearing loss, tinnitus, imbalance.
The diagnosis of syphilis may be more complicated in HIV infected
patients because of false positive and false negative serological results for
Treponema pallidum and atypical clinical presentation in HIV.
CSF WBC may be elevated due to opportunistic infection or unknown
cause. CSF WBC>20 is sensitive and specific criteria for neurosyphilis in such
situations. Currently CDC does not recommend CSF examination in early
syphilis who have no CNS symptoms.
TREATMENT OF SYPHILIS AND HIV CO- INFECTION
Primary, secondary, Early latent syphilis
35
FOLLOW UP
Clinical and serological follow up are done at 3, 6, 12, 24 months. CSF
examination and retreatment with 3 weekly doses of Inj. Benzathine penicillin
G are recommended in patients whose non treponemal titre do not fall
fourfold within 6-12 months of therapy.
LATE LATENT SYPHILIS
Patients with late latent syphilis or syphilis of unknown duration should
undergo CSF examination. If it is normal then 3 weekly doses of Inj.
Benzathine penicillin G 2.4 million units is given. If there are CSF
abnormalities then they are treated as neurosyphilis.(16)
FOLLOW UP
Clinical and serological examination are repeated at 6, 12, 18, 24
36
TREATMENT OF NEUROSYPHILIS (16)
Intravenous administration of Aqueous crystalline penicillin G at a
dose of 18 – 24 million units daily for 14 days. Alternatively procaine
penicillin G is given at a dose of 2.4 million units IM daily for 14 days along
with probenecid 500 mg QID for 14 days.(16)
FOLLOW UP
CSF examination should be done at 6 month interval until CSF is
normal and reassessment of CSF should be undertaken when neurosyphilis is
37
AIMS AND OBJECTIVES
1. To study the socio demographic patterns and the risk factors involved in
transmission of syphilis.
2. To analyse the clinical presentations of syphilis in presence of
HIV/AIDS .
3. To analyse the serological variations of syphilis in presence of
38
MATERIALS AND METHODS
STUDY DESIGN
Prospective study
STUDY PERIOD
One year ( June 2017 – May 2018).
SAMPLE
Patients attending for self screening and high risk groups in Out Patient
Department, Institute of Venereology, Madras Medical College/RGGGH,
Chennai – 600003.
INCLUSION CRITERIA.
1. Those who are willing to participate in the study.
2. Age >12 years and <60 years.
3. High Risk groups like Homosexuals, IV drug abuse, recepients of blood
and blood products.
EXCLUSION CRITERIA
1. Patients who refuse to participate in the study.
39
METHODOLOGY (MATERIALS AND METHODS)
Detailed clinical history including presenting complaints, sexual
history, past history of Ano-genital disease and any treatment taken would be
elicited. All the participants should undergo complete genital and physical
examination.
In both male and patients presenting with genital ulcer, microscopic
examination of smear from ulcers will be done with dark field microscopy,
gram staining and leishman stains, Tzanck and Tissue smear. In case of
genital discharge, in male patients – gram stain smear for gonococci, normal
saline and potassium hydroxide wet mount would done. In females,
endocervical swab for gonococcus culture and endocervical smear for gram
stain will be done. Smears from vagina for gram staining, normal saline and
potassium hydroxide wet mount will be taken.
Routine Laboratory tests and serological investigations will be done for
all participants. Screening test for syphilis will be done by VDRL and
confirmed by Treponema pallidum hemagglutination assay (TPHA). ELISA
for HIV-1 and 2 ANTIBODY ASSAY will be done after informed consent and
40
[image:48.595.109.557.454.751.2]RESULTS
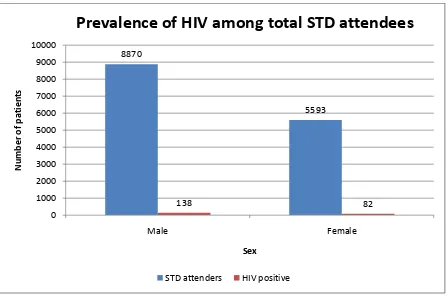
Table 1: PREVALENCE OF HIV POSITIVE AMONG STD
ATTENDEES DURING STUDY PERIOD
SEX
STD ATTENDEES
(NUMBERS)
HIV POSITIVE (NUMBERS)
PREVALENCE (%)
MALE 8870 138 1.6 %
FEMALE 5593 82 1.5 %
TOTAL 14463 220 1.5 %
Prevalence of HIV positive among STD attendees during study period was
estimated at 1.5 %.
8870 5593 138 82 0 1000 2000 3000 4000 5000 6000 7000 8000 9000 10000 Male Female Number of patients Sex
Prevalence
of
HIV
among
total
STD
attendees
41 14463 187 0 2000 4000 6000 8000 10000 12000 14000 16000 Prevalence Number of patients
Prevalence
of
syphilis
among
STD
attendees
[image:49.595.114.556.346.736.2]STD attenders Syphilis postive
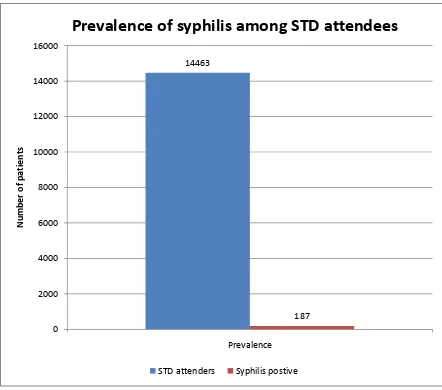
Table 2: PREVALENCE OF SYPHILIS AMONG GENERAL STD
ATTENDEES
STD ATTENDEES (NUMBERS)
SYPHILIS ALONE POSITIVE
PREVALENCE OF SYPHILIS (%)
14463 187 1.29%
The prevalence of syphilis among STD attendees during the study period was
42
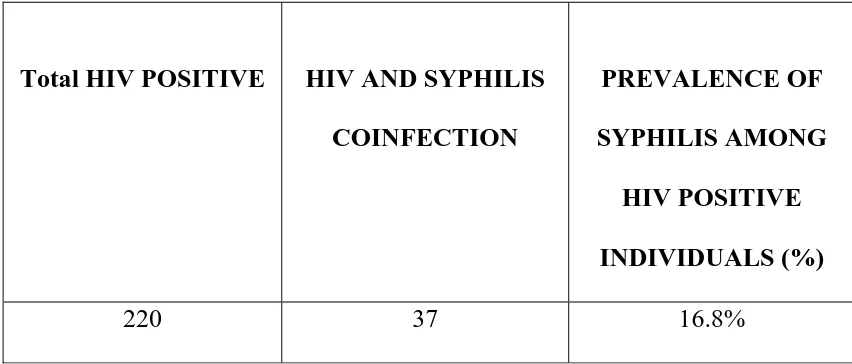
Table 3: PREVALENCE OF SYPHILIS AMONG HIV POSITIVE
INDIVIDUALS
Total HIV POSITIVE HIV AND SYPHILIS
COINFECTION
PREVALENCE OF
SYPHILIS AMONG
HIV POSITIVE
INDIVIDUALS (%)
220 37 16.8%
The prevalence of syphilis among HIV infected individuals during the
43 220
37
0 50 100 150 200 250
Prevalence
Number
of
patients
Prevalence
of
HIV
and
syphilis
coinfection
among
STD
attendees
44
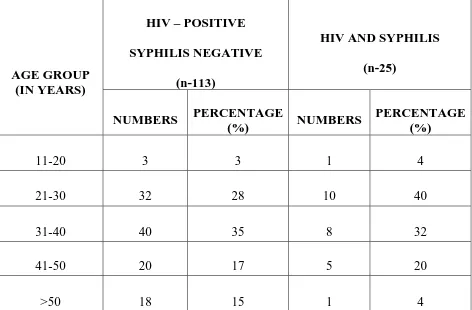
Table 4(a): AGE WISE DISTRIBUTION OF HIV POSITIVE
PATIENTS VS HIV AND SYPHILIS COINFECTED PATIENTS
(MALES INCLUDING TRANSGENDER).
AGE GROUP (IN YEARS)
HIV – POSITIVE
SYPHILIS NEGATIVE
(n-113)
HIV AND SYPHILIS
(n-25)
NUMBERS PERCENTAGE
(%) NUMBERS
PERCENTAGE (%)
11-20 3 3 1 4
21-30 32 28 10 40
31-40 40 35 8 32
41-50 20 17 5 20
>50 18 15 1 4
The prevalence of HIV infection and HIV and syphilis coinfection
[image:52.595.81.553.167.477.2]45 3 32 40 20 18 1 10 8 5 1 0 5 10 15 20 25 30 35 40 45
11‐20 21‐30 31‐40 41‐50 >50
Number of male patients
Age group
Age
distribution(Males)
46
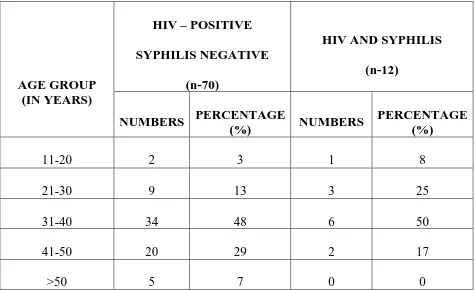
Table 4(b): AGE WISE DISTRIBUTION OF HIV POSITIVE
PATIENTS VS HIV AND SYPHILIS COINFECTED PATIENTS
(FEMALES).
AGE GROUP (IN YEARS)
HIV – POSITIVE
SYPHILIS NEGATIVE
(n-70)
HIV AND SYPHILIS
(n-12)
NUMBERS PERCENTAGE
(%) NUMBERS
PERCENTAGE (%)
11-20 2 3 1 8
21-30 9 13 3 25
31-40 34 48 6 50
41-50 20 29 2 17
>50 5 7 0 0
The prevalence of HIV infection and HIV and syphilis coinfection
[image:54.595.79.554.165.455.2]47 2 9 34 20 5 1 3 6 2 0 0 5 10 15 20 25 30 35 40
11‐20 21‐30 31‐40 41‐50 >50
Number of female patients
Age group
Age
distribution(Females)
48
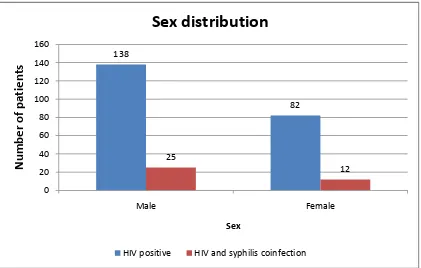
Table 5: PREVALENCE OF SYPHILIS AMONG HIV POSITIVE
INDIVIDUALS
Analysis of sex distribution revealed that males have higher prevalence
(18.11%) of HIV and syphilis coinfection.
138 82 25 12 0 20 40 60 80 100 120 140 160 Male Female Number of pa tien ts Sex
Sex
distribution
HIV positive HIV and syphilis coinfection
SEX TOTAL HIV POSITIVE (NUMBERS)
HIV AND SYPHILIS COINFECTION (NUMBERS) PREVALENCE OF SYPHILIS AND HIV COINFECTION (%)
MALE 138 25 18.11%
FEMALE 82 12 14.63%
49
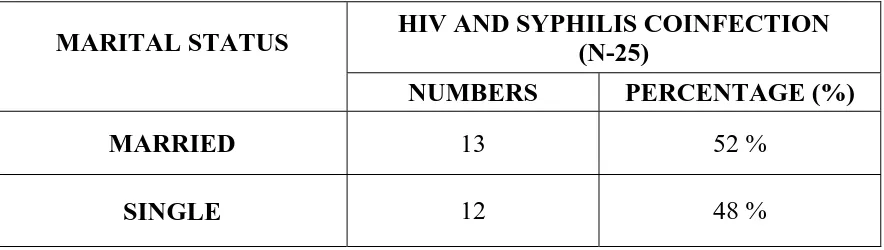
Table 6(a): MARITAL STATUS OF HIV AND SYPHILIS
COINFECTED MALE PATIENTS
MARITAL STATUS HIV AND SYPHILIS COINFECTION (N-25)
NUMBERS PERCENTAGE (%)
MARRIED 13 52 %
SINGLE 12 48 %
Majority of males with HIV and syphilis coinfection were
[image:57.595.96.538.161.286.2]50 13
12
11.4 11.6 11.8 12 12.2 12.4 12.6 12.8 13 13.2
Married Single
Number
of
male
patients
Marital history
51
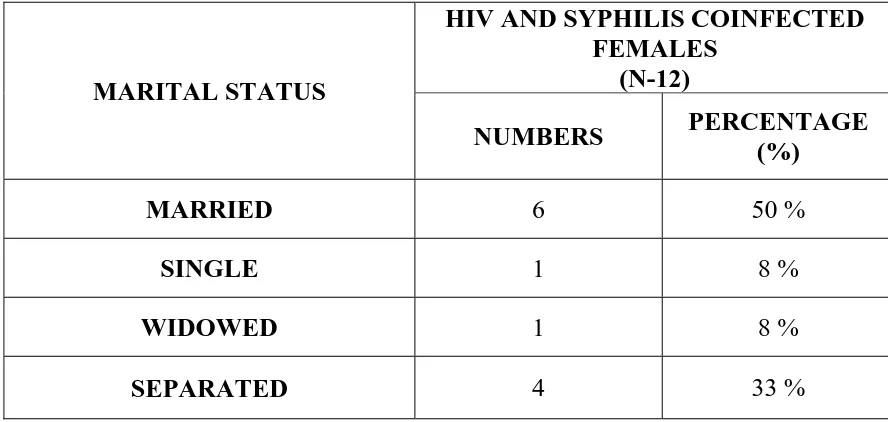
Table 6(b): MARITAL STATUS OF HIV AND SYPHILIS
COINFECTED FEMALE PATIENTS.
MARITAL STATUS
HIV AND SYPHILIS COINFECTED FEMALES
(N-12)
NUMBERS PERCENTAGE (%)
MARRIED 6 50 %
SINGLE 1 8 %
WIDOWED 1 8 %
SEPARATED 4 33 %
Majority of HIV positive females were married(50%), though a
significant number were either separated from their husband (33%) or
[image:59.595.106.550.147.358.2]52 6
1 1
4
0 1 2 3 4 5 6 7
Married Single Widowed Separated
Number
of
female
patients
Marital history
53
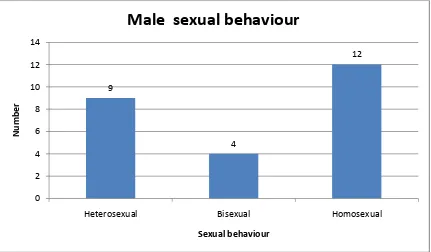
Table 7(a): SEXUAL BEHAVIOUR OF HIV AND SYPHILIS
COINFECTED MALE PATIENTS
SEXUAL BEHAVIOR HIV AND SYPHILIS
COINFECTED MALE PATIENTS NUMBERS PERCENTAGE
(%)
HETEROSEXUAL 9 36
BISEXUAL 4 16
HOMOSEXUAL 12 48
Majority of males were promiscuous and failed to use condoms. Most
of them were homosexual (48%).
9
4
12
0 2 4 6 8 10 12 14
Heterosexual Bisexual Homosexual
Number
[image:61.595.112.543.462.714.2]54
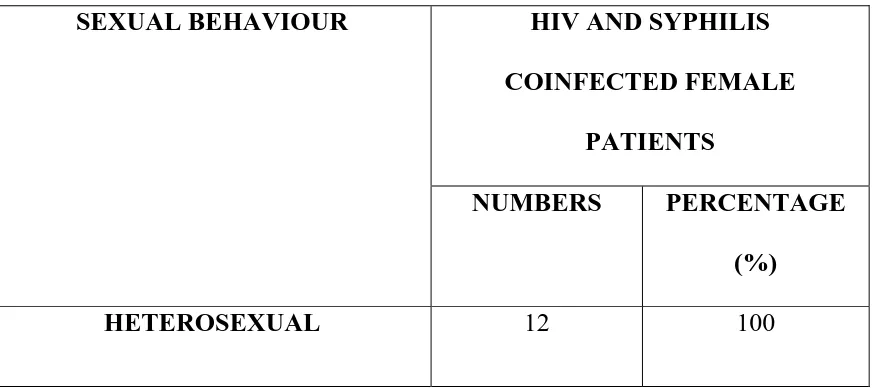
Table 7(b): SEXUAL BEHAVIOUR OF HIV AND SYPHILIS
COINFECTED FEMALE PATIENTS
SEXUAL BEHAVIOUR HIV AND SYPHILIS
COINFECTED FEMALE
PATIENTS
NUMBERS PERCENTAGE
(%)
[image:62.595.100.538.159.354.2]55
Table 8(a): DOMICILE OF HIV POSITIVE VS HIV AND SYPHILIS
COINFECTED MALE PATIENTS
48 65 9 16 0 10 20 30 40 50 60 70 Rural Urban Number of male patients Domicile
Domicile
vs
Infection
HIV positive HIV and syphilis coinfection
DOMICILE HIV-POSITIVE
(N-113)
HIV AND SYPHILIS
COINFECTION (N-25) NUMBERS PERCENTAGE (%) NUMBERS PERCENTAGE (%)
RURAL 48 42 9 36
[image:63.595.92.544.150.386.2]56
Table 8(b): DOMICILE OF HIV POSITIVE VS HIV AND SYPHILIS
COINFECTED FEMALE PATIENTS.
65% of both HIV positive Vs HIV and syphilis coinfected males and
females hailed from urban areas.
25 45 4 8 0 5 10 15 20 25 30 35 40 45 50 Rural Urban Number of female patients Domicile
Domicile
vs
Infection
HIV positive HIV and syphilis coinfection
DOMICILE HIV-POSITIVE
(N-70)
HIV AND SYPHILIS
COINFECTION (N-12) NUMBERS PERCENTAGE (%) NUMBERS PERCENTAGE (%)
RURAL 25 36 4 33
[image:64.595.110.538.501.770.2]57
Table 9(a): OCCUPATION OF HIV AND SYPHILIS COINFECTED
MALE PATIENTS.
OCCUPATION HIV AND SYPHILIS
COINFECTED MALE
PATIENTS
(N-25)
NUMBERS PERCENTAGE
(%)
Agriculture 2 8
Coolie 5 20
Private company
(Graduates- B.A, B.Com, B.Sc)
9 36
Electrician 3 12
Barber 2 8
Driver 2 8
MSM sex worker 1 4
Painter 1 4
A significant number of HIV and syphilis coinfected males were
working in private company (36%), remaining patients (Agriculture, coolie,
[image:65.595.92.542.160.642.2]58 2
5
9
3
2 2
1 1
0 1 2 3 4 5 6 7 8 9 10
Number
of
male
patients
Occupation
59
Table 9(b): OCCUPATION OF HIV AND SYPHILIS COINFECTED
FEMALE PATIENTS
OCCUPATION HIV AND SYPHILIS
COINFECTED FEMALE
PATIENTS
(N-12)
NUMBERS PERCENTAGE
(%)
Agriculture 2 17
Coolie 2 17
Private company
(Graduates -B.A, B.Com, B.Sc)
4 33
House wife 2 17
House keeping 1 8
Commercial Sex Worker(CSW) 1 8
A significant number of HIV and syphilis coinfected females were
working in private company(33%), remaining patients (Agriculture, coolie)
[image:67.595.97.538.159.572.2]60 2 2 4 2 1 1 0 0.5 1 1.5 2 2.5 3 3.5 4 4.5
Agriculture Coolie Private
company
Housewife House
keeping CSW Number of female patients Occupation
61
Table 10(a): PRESENTING COMPLAINTS OF HIV AND SYPHILIS
COINFECTED MALE PATIENTS.
COMPLAINTS HIV AND SYPHILIS
COINFECTED MALE
PATIENTS
(N-25)
NUMBERS PERCENTAGE
(%)
Self screening 8 32
Urethral Discharge 1 4
Genital ulcer 4 16
Genital wart 2 8
Skin rash 5 20
Constitutional symptoms like Fever,Cough
Loss of weight and appetite –private
referral
4 16
Genital itching 1 4
A significant number of HIV and syphilis coinfected positive males
(32%) had come for self screening. Among symptomatic, significant number
[image:69.595.99.534.159.642.2]62 8
1
4
2
1
5
4
0 1 2 3 4 5 6 7 8 9
Number
of
male
patients
Presenting complaints
63
Table 10(b): PRESENTING COMPLAINTS OF HIV AND SYPHILIS
COINFECTED FEMALE PATIENTS.
COMPLAINTS HIV AND SYPHILIS
COINFECTED FEMALE
PATIENTS
(N-12)
NUMBERS PERCENTAGE
(%)
Self screening 5 42
Genital Discharge 2 17
Genital ulcer 1 8
Skin rash 1 8
Constitutional symptoms like Fever,Cough
Loss of weight and appetite –private
referral
3 25
A significant number of HIV and syphilis coinfected positive females
(42%) had come for routine screening. Among symptomatic, significant
[image:71.595.102.534.160.574.2]64 5
2
1 1
3
0 1 2 3 4 5 6
Self checkup Discharge Genital ulcer Skin rash Constitutional
symptoms
Number
of
female
patients
Presenting complaints
65
Table 11(a): ASSOCIATED DISEASES OF HIV AND SYPHILIS
COINFECTED MALE PATIENTS.
DISEASE HIV AND SYPHILIS COINFECTED
MALE PATIENTS
(N-25)
NUMBERS PERCENTAGE (%)
Gonorrhoea 2 8
Genital Herpes 4 16
Genital wart 3 12
Genital scabies 1 4
Genital molluscum contagiosum 1 4
Oral candidiasis 3 12
Dermatophytosis 4 16
Tuberculosis 1 4
No other associated diseases 6 24
Genital herpes (16%) was the most common associated STD among
the HIV and syphilis coinfected male patients. Concomitant infection with
various STD’S like warts (12%), gonorrhoea(8%) and non venereal conditions
[image:73.595.94.540.160.610.2]66 2
4
3
1 1
3
4
1
6
0 1 2 3 4 5 6 7
Number
of
male
patients
Associated diseases
67
Table 11(b): ASSOCIATED DISEASES OF HIV AND SYPHILIS
COINFECTED FEMALE PATIENTS.
DISEASE
HIV AND SYPHILIS COINFECTED FEMALE PATIENTS
(N-12)
NUMBERS PERCENTAGE (%)
Bacterial vaginosis 1 8
Vulvo vaginal candidiasis 3 25
Trichomonas vaginitis 1 8
Genital wart 1 8
Dermatophytosis 2 17
Tuberculosis 1 8
No other associated diseases 3 25
Vulvo vaginal candidiasis (25%) was the most common associated STD
among the HIV and syphilis coinfected female patients. Concomitant
infection with various STD’S like Genital warts(8%), Bacterial vaginosis(8%)
and non venereal conditions like dermatophytosis, Tuberculosis were
[image:75.595.105.522.160.496.2]68
1
3
1 1
2
1
3
0 0.5 1 1.5 2 2.5 3 3.5
Number
of
female
patients
Associated diseases
69
Table 12(a): PREVALENCE - STAGE OF SYPHILIS AMONG HIV
POSITIVE MALE PATIENTS.
STAGE OF SYPHILIS
HIV AND SYPHILIS COINFECTED MALE PATIENTS
(N -25)
NUMBERS PERCENTAGE (%)
Primary syphilis 3 12
Secondary syphilis 8 32
Early latent syphilis 6 24
Late latent syphilis 7 28
Cardiovascular syphilis 1 4
Neuro syphilis 0 0
In our study, most of the HIV infected male syphilitic patients
presented with early syphilis manifestations (68%) [Primary syphilis (No 3,
12%), Secondary syphilis (No 8, 32%), Early Latent syphilis (No-6, 24%),
[image:77.595.101.531.143.429.2]70
3
8
6
7
1
0 0
1 2 3 4 5 6 7 8 9
Number
of
patients
Stages of syphilis
71
Table 12(b) : PREVALENCE - STAGE OF SYPHILIS AMONG HIV
POSITIVE FEMALE PATIENTS.
STAGE OF SYPHILIS
HIV AND SYPHILIS COINFECTED FEMALE PATIENTS
(N -12)
NUMBERS PERCENTAGE (%)
Primary syphilis 0 0
Secondary syphilis 6 50
Early latent syphilis 4 33
Late latent syphilis 2 16
Cardiovascular syphilis 0 0
Neuro syphilis 0 0
In our study, most of the HIV infected female syphilitic patients
presented with early syphilis manifestations (83%) [Primary syphilis (No 0),
Secondary syphilis (No 6, 50%), Early Latent syphilis (No-4, 33%), Late
[image:79.595.109.526.161.444.2]72 0
6
4
2
0 0
0 1 2 3 4 5 6 7
Number
of
patients
Stages of syphilis
73 420 246 512 633 589 0 100 200 300 400 500 600 700
Primary Secondary Early latent
syphilis
late latent
syphilis Cardiovascular syphilis Average CD4 count
[image:81.595.113.535.486.751.2]Stages of syphilis
CD4
count
Table 13 : AVERAGE CD4 COUNT IN HIV AND SYPHILIS
COINFECTION.
STAGE OF SYPHILIS AVERAGE CD4 COUNT
Primary syphilis 420
Secondary syphilis 246
Early latent syphilis 512
Late latent syphilis 633
Cardiovascular syphilis 589
Average CD4 count among study population was lowest
(246 cells/cumm) in patients presenting with secondary syphilis
74
Table 14: VDRL REACTIVITY IN HIV SEROPOSITIVE PATIENTS
STAGE VDRL TITRE AVERAGE
VDRL TITRE
<1:8 >1:8 to <1:64 >1:64
PRIMARY 2 1 - 9.33(N-3)
SECONDARY 1 6 7 74(N-14)
EARLY LATENT SYPHILIS
4 7 - 27.27(N-11)
LATE LATENT SYPHILIS
7 1 - 2.75(N-8)
CARDIOVASCULAR SYPHILIS
1 - - 1 (N-1)
Lowest VDRL titre =1:4
Highest VDRL titre =1:256
2 1 4 7 1 1 6 7 1 0 7 0 0 0 1 2 3 4 5 6 7 8
Primary Secondary Early latent
syphilis
late latent syphilis CardioVascular
Syphilis Number of individuals
Stages of syphilis
VDRL
reactivity
75
DISCUSSION
In India there is a strong epidemiological association between HIV
infection and syphilis. Both diseases are predominantly sexually transmitted
and syphilis patients are at increased risk for HIV infection. This study is
designed to know the prevalence of syphilis, its clinical presentations,
serological variations, therapeutic response to standard therapy in presence of
HIV infection.
The prevalence of HIV among STD attendees in this study was 1.5%
comparitevely higher than that in a study conducted by Fabiola Mesqita
callegari, Lauro Ferreira, et al., in the year 2015 where HIV prevalence among
adults in general population was 0.6%. (21)
The prevalence of syphilis infection among STD attendees in our
study was 1.29% which was somewhat lower than that observed in a study
by Signorini DJ, Monteiromc, et al., in the year 2005 was 2.7%.( 22)
In our study prevalence of syphilis in HIV infected individuals was
16.8%, whereas in a study conducted by Adolf R, Bercht F, Aronis ML, et
al., in the year 2012 the similar result (2.7% -24.4%) was obtained. (23)
Majority of patients (70%) in our study were in sexually active age
group of 20 -40 years and Mean age for Syphilis and HIV coinfected males
76
obtained in a study conducted by Joseph Forbi, et al., where the mean age of
HIV and syphilis coinfected males was 41.3 years against 30.4 years for
females. (24)
Prevalence of HIV and syphilis coinfection were higher in males
(18.11%) than females (14.63%).
It was observed that 65% of both HIV positive Vs HIV and syphilis
coinfected males and females hailed from urban areas. This indicates that
the prevalence of HIV and syphilis was higher in cities with larger floating
populations and in more developed cities. Similar results were observed in a
previous study conducted by Pan X , Zhu Y, Wang Q, et al., where 75% of
cases reported from urban areas..(25)
35% of HIV and syphilis coinfected patients hailed from rural areas.
This indicates that HIV population has also infiltrated into the rural
population.
This study found that 48 % of HIV and syphilis coinfection occurs in
patients with sexual behavior of Men sex with Men(MSM). Similar results
(54%) were obtained in a study by Wenjie Dai, Zhenzhou Luo, et al. in the year
2017. (26)
Majority of males and females with HIV and syphilis coinfection
77
from their husband (33%) or widowed (8%). This implies that the spouses of
infected persons are susceptible to acquire infection from their partners.
Majority of males were promiscus and failed to use contraceptives.
A significant number of HIV and syphilis coinfected males and females
were working in private company (35%) and Commercial sex worker(CSW)
accounts for (8%) but in a study conducted by Mwumvaneza Mutagoma,
Laetia Nyirazinyoye, et al., showed that higher prevalence among lower
socioeconomic status. (27)
Our study revealed that higher prevalence concentrated among urban
population and educated persons due to increased chance of contacts, high
risk sexual behaviours and increased Men having sex with Men. Sex
education, contraceptive methods have to be reach both urban and rural areas.
Among symptomatic males, significant number of patients account for