ANALYTICAL STUDY OF PSEUDOEXFOLIATION SYNDROME, ITS ASSOCIATION WITH GLAUCOMA
AND ITS SURGICAL COMPLICATIONS
Submitted in partial fulfillment of requirements of
M.S. OPHTHALMOLOGY
BRANCH - III
REGIONAL INSTITUTE OF OPHTHALMOLOGY
MADRAS MEDICAL COLLEGE
CHENNAI- 600 003
THE TAMILNADU
DR.M.G.R. MEDICAL UNIVERSITY
CHENNAI
This is to certify that this dissertation entitled “ANALYTICAL
STUDY OF PSEUDOEXFOLIATION SYNDROME, ITS
ASSOCIATION WITH GLAUCOMA AND ITS SURGICAL
COMPLICATIONS.” is a bonafide record of the research work done
by Dr. DIVYA SHETTY , post graduate in Regional Institute of
Ophthalmology and Government Ophthalmic Hospital, Madras Medical College and Government General Hospital, Chennai-03, in partial fulfillment of the regulations laid down by The Tamil Nadu Dr. M.G.R. Medical University for the award of M.S. Ophthalmology Branch III, under my guidance and supervision during the academic years 2012-2015.
Dr. WAHEEDA NAZIR, MS., DO.
Chief – GLAUCOMA SERVICES
RIO – GOH Egmore, Chennai – 08
Dr.K.NAMITHA BHUVANESWARI, MS., DO.
Director and Superintendent RIO – GOH
Egmore, Chennai – 08
Dr. R.VIMALA, M.D.
Dean,
Madras Medical College. and Government General Hospital
I express my sincere thanks and gratitude to Prof. Dr. R. Vimala,
M.D. Dean, Madras Medical College and Government General Hospital
for permitting me to conduct this study.
I express my sincere gratitude to Prof. Dr. K. Namitha
Bhuvaneswari, M.S., D.O., Director and Superintendent, Regional
Institute of Ophthalmology and Government Ophthalmic Hospital, Madras Medical College, Chennai for her valuable advice in preparing this dissertation.
I am extremely grateful to Prof. Dr. Waheeda Nazir, M.S.,
D.O., my Unit Chief and my guide for her valuable guidance and
constant support at every stage throughout the period of this study. I am very grateful to my Assistant Professors Dr. N. Sharmila,
M.S. and Dr. B. Kalaiselvi, M.S. for their valuable guidance and
support not only during the study but also throughout my course in all aspects.
I am grateful to my unit Assistant Professors Dr. M.S.Gokila,
M.S, D.O., and Dr R Sujatha, M. S. for rendering their constant
support during the study period.
I wish to express my sincere thanks to all the professors, assistant professors and all my colleagues who had helped me in bringing out this study.
CONTENTS
SR
NO TITLE PAGE NO
PART-1
1 INTRODUCTION 1
2 ANATOMY 3
3 REVIEW OF LITERATURE 7
PART –II
4 AIM OF THE STUDY 55
5 MATERIALS AND METHODS 56
6 OBSERVATION AND RESULTS 63
7 DISCUSSION 99
8 CONCLUSION 104
PART-III
9 BIBLIOGRAPHY 10 PROFORMA 11 MASTER CHART
INTRODUCTION
Pseudoexfoliation syndrome is an age-related disease in which abnormal fibrillar extracellular material of uncertain origin accumulates in many ocular tissues. Polymorphism of exon1 of LOXL1 gene has been found in patients with pseudoexfoliation syndrome. It is recognised as a common cause of secondary open angle glaucoma.
Deposition of amorphous grey dandruff-like material on the anterior lens surface is the most consistent and important diagnostic feature of pseudoexfoliation syndrome. Exfoliative material is also deposited on corneal endothelium, trabecular meshwork, iris, pupillary margins, zonules, ciliary processes, anterior hyaloids phase.
The presence of pseudoexfoliation is associated with increased risks of intraocular surgery, most commonly zonular dehiscence, capsular rupture, and vitreous loss during cataract extraction.
complications involved in surgical management. It shows response to argon laser trabeculoplasty, trabecular aspiration and trabeculectomy.
ANATOMY
TRABECULAR MESHWORK
It is a sieve like structure in the angle of the anterior chamber through which aqueous humour leaves the eye. It consists of the following 3 portions:
Uveal Meshwork
It is the innermost portion, which consists of cordlike meshes that extend from the root of iris to the Schwalbe‟s line. The intertrabecular spaces are relatively large and offer little resistance to the passage of aqueous.
1. Corneo-scleral meshwork
It forms the larger middle portion, which extends from the scleral spur to Schwalbe‟s line. The meshes are sheet like and inter trabecular spaces are smaller than uveal meshwork.
2. Endothelial (Juxtacanalicular) Meshwork:
Schlemm‟s canal. The juxtacanalicular meshwork is very important because it offers the major proportion of normal resistance to aqueous humour.
Gonioscopically, the trabecular meshwork has a ground glass
appearance. It consists of the following 2 parts:
1. The anterior, nonfunctional, nonpigmented part lies anterior
to the Schwalbe‟s line and has a whitish color.
2. The posterior, functional, pigmented part, which lies adjacent
to the sclera spur and has a grayish blue transparent appearance.
Trabecular pigmentation is a very rare before puberty. In senile
eyes, it involves the posterior trabeculum to a variable extent and is most marked inferiorly, Pathological trabecular hyperpigmentation is caused by the excessive shedding of pigment from the posterior layer of the iris. The main causes are pseudoexfoliation syndrome & pigment
dispersion syndrome, other causes being blunt ocular trauma, anterior
uveitis, after angle closure glaucoma, diabetes mellitus and naevus of Ota.
interlacing beams separated by intertrabecular spaces. Each trabecula has a central core of typical collagen fibrils with the usual 640 A° banding, middle basement membrane and endothelial covering. The endothelial covering consists of large flat cells containing numerous pinocytic vesicles and is the continuation of Descemet‟s endothelium. The intertrabecular spaces become progressively smaller as Schlemm‟s canal is approached. The openings of inner meshwork are 50-60µ in diameter and that of deep meshwork 1-2µ in diameter. In pseudoexfoliation syndrome, the openings of the trabecular meshwork are clogged by exfoliative material, leading to impaired aqueous outflow and thus increased intraocular pressure.
BLOOD AQUEOUS BARRIER
It is formed by the tight junctions
1. Between the endothelial cells of the iris capillaries
2. Between the non-pigmented cells of the ciliary epithelium.
The breakdown of the barrier, due to various noxious stimuli like prostaglandins in trauma leads to an increases aqueous protein concentration. In uveitis, when there is extensive breakdown of the barrier, the aqueous humour protein level can be greater than 1 g/100 ml almost similar to that in plasma. Even in pseudoexfoliation syndrome, various studies have shown impairment of blood aqueous barrier.
REVIEW OF LITERATURE
HISTORICAL ASPECT AND TERMINOLOGY
Pseudoexfoliation syndrome was first described in 1917 by LINDBERG who noted the presence of bluish grey flakes at the pupillary margin in 50% of his glaucoma patients. VOGT in 1925 thought it originated from the lens capsule and called it senile
exfoliation of the lens capsule and having established its frequent
association with open angle glaucoma, glaucoma capsulare. BUSACCA (1927), MALLING (1923) and others argued that the material was merely deposited on the normal lens capsule.
That the lens is unnecessary for the pathogenesis was finally proven by the appearance of exfoliative material many years after ICCE in aphakic eyes and on IOL implants.
lens capsule as seen in glassblowers. SUNDE (1956) 3 proposed the term
senile exfoliation syndrome which may be the most conclusive
description of the clinical, biochemical and histo-pathological findings. Considering the rarity of true exfoliation syndrome LAYDEN4 suggested the term exfoliation syndrome. Since recent ultrastructural studies indicate that the material on the lens capsule is derived, atleast in part, from the lens, it is proposed that the disorder be called exfoliation syndrome. Both terms pseudoexfoliation and exfoliation syndrome are commonly used now to describe this condition.
Since the disease may occur with or without glaucoma, the term pseudo exfoliation syndrome and pseudo exfoliative glaucoma are used. EAGLE et al5 (1971) suggested that pseudoexfoliation syndrome is a basement membrane exfoliation syndrome. GARDNER AND ALEXANDE6 (1984) proposed the term oxytalanosis of aqueous based on studies of histochemical similarities of exfoliation material on zonular fibres. STREETEN7 1984 suggested the term ocular elastosis
EPIDEMIOLOGY
Prevalence
Lindberg’s first description of the pseudoexfoliation syndrome
was in a series of patients in Finland & high prevalence rates and a plethora of studies continue to be reported from the Nordic countries. It is not unique to Scandinavia, however, as the syndrome has been described to occur worldwide, virtually no area being spared. Reported prevalence rates of pseudoexfoliation vary widely in different geographic locations. Not only true difference in the prevalence rates exist, but also differences in the examination techniques among studies exist. Age of the population, racial and ethnic composition, patient selection, clinical criteria for diagnosis and thoroughness of examination and prospective versus retrospective data collection can all affect results. In fact, many cases go undetected because of failure to dilate the pupil or to examine the lens by the slit-lamp after dilatation and because of a low index of suspicion. Thus, usually, prevalence rates appear highest and most accurate in prospective studies using pupil dilatation. The prevalence of pseudoexfoliation ranges from 0% among the Eskimos to as high as
38% in Navaho Indians8. Prevalence rate in Norway is 6.3%,
England 4.7%, Germany 4%, Japan 0.2%,Indians 2% and in
rates reported were 1.88% Sood N.N.10(1965), 7.4% Lamba and
Giridhar11 (1984).The prevalence rate in south India is 3.8% Aravind
H et al12 (2003).
AGE
Age is an important determinant in the incidence of pseudoexfoliation. This syndrome is rare before the age of 50 years, but becomes increasingly common, nearby doubling in incidence every decade after the age of 50. Thus, as an overall, it is the disease of the elderly. FRAMINGHAM9 study reported a prevalence of 0.6% of people who are 52-64 years rising to 5% by 75-80 years of age.
AASVED found 0.4% rate for the ages 50-59 years and 7-9% rates for
ages 80-89. The youngest reported patients who had intra-ocular surgery in infancy was of 17 years of age.
SEX
HEREDITY
No clear hereditary pattern has yet been discerned. AASVED
suggested an autosomal dominant inheritance. A preponderance of maternal transmission include the possibility of mitochondrial inheritance.
Kelvin Y. C. Leeetal13 studied about pseudoexfoliation
syndrome and pseudoexfoliation glaucoma associations with polymorphisms of the lysyl oxidase like 1gene(LOXL1) on Chromosome15q21(1). Asian populations including Indians reported associations with LOXL1and pseudoexfoliation syndrome.
R.R.Allinghan et al14 (2001) investigated 6 islandic families
each of which had atleast 1 member affected by Pseudoexfoliation Syndrome. They concluded that Pseudoexfoliation Syndrome is an inherited condition with transmission to the 2nd generation through an affected mother.
ASYMMETRY OF INVOLVEMENT
terms unilateral and monocular are misleading. Conjuctival biopsy in fellow eyes of patients with unilateral pseudoexfoliation syndrome is invariably positive (PRINCE 15, SPEAKMAN16). Since pigment related signs of pseudoexfoliation syndrome are found in most unaffected eyes, they are actually asymmetric. Patients will exhibit these signs but who are not shown to be clinically involved by slit-lamp examination have been termed Pseudoxfoliation Suspects (PRINCE15). The terms unilateral and bilateral are used to indicate clinically detectable involvement. HENRY et al found the probability of pseudoexfoliation developing in the opposite eye as 6.8% after 5 year and 16.8 % after 10 years. Most evidence points to the facts that unilateral pseudoexfoliation is often a precursor of bilateral pseudoexfoliation.
Bilateral pseudoexfoliation syndrome and glaucoma occur at slightly older age than unilateral pseudoexfoliation and glaucoma9,17 .
CLIMATE
different climate than that found in the northern latitude.
Ultra-violet light exposure has been suggested as influencing exfoliation19. Attempts to correlate exfoliation with other signs of UV exposure, such as Pterygium, Climatic Keratopathy or Cataract have failed to reveal significant correlations18.
SYSTEMIC ASSOCIATION
No clear cut association of exfoliation with any systemic disease has been found.
CLINICAL FEATURES
Conjunctiva
Clinically the conjunctiva is normal. However, Fluorescein Angiography reveals Loss of regular limbal vascular pattern and areas of neovascularisation in advanced cases, as well as congestion of the anterior ciliary vessels. Lower scores of Schirmer testing and tear
break-up time have been found, especially if treated with beta-blockers.
Cornea
non-specific pigmentation of corneal endothelium, only occasionally having the pattern of Krukenberg spindle. More frequent several undulating pigmented lines can be observed in the peripheral cornea anterior to the Schwalbe‟s line. VANNAS et al noted a decrease in endothelial cell density, even with normal IOP, together with changes in size and shape of the cells in both affected and fellow eyes. A greater than normal frequency of cornea guttata has been suggested. NAUMANN and
SCHLOTZER suggest that a„True keratopathy’ is found in eyes with
exfoliation, predisposing them to develop early corneal endothelial decompensation after moderate rise of IOP or Cataract surgery. Spheroidal degeneration has significant association with exfoliation20.
Anterior Chamber
Rarely small pigment floaters or exfoliation material is seen floating in aqueous in the undilated eye. After mydriasis pigment dispersion is often seen reminiscent of the liberation of pigment into anterior chamber during mydriasis in pigment dispersion syndrome.
Iris
degree using high magnification and narrow slit beam. Iris in eyes with exfoliation is more rigid than in eyes without it.
Iris vascular abnormalities are the rule in pseudoexfoliation syndrome. Fluorescein Angiography studies show partial occlusion of radial iris capillaries associated with hypoperfusion, a reduced number of vessels, microneovascularisation and diffuse patchy fluorescein leakage especially in the pupillary region. Indocyanine Green Angiography
provides a better recognition of iris hypoperfusion and anastomotic vessels.
Pigment loss from the iris spincter and its deposition on anterior chamber structure is the hallmark of pseudoexfoliation syndrome. Loss of the iris pigment and its deposition in the anterior segment is reflected in the iris sphincter region transillumination, loss of the pupillary ruff, increased pigmentation and pigment deposition on the iris surface.
Generalized peripheral iris transillumination which appears as a diffuse “starry sky” appearance of the defects is associated with pseudoexfoliation.
on the anterior stroma at the sphincter. Pigment is deposited evenly over the iris surface, in contrast to its collection in the furrows in pigment dispersion syndrome.
Pseudoexfoliation suspects exhibit pigment dispersion in the absence of clinically identifiable exfoliation. Iridodonesis may be present.
Pupil
Atrophy of the sphincter pupillae gives rise to a “Moth Eaten
Appearance”. Pupillary ruff defects are the most common and most
striking in patients with unilateral involvement.
Eyes with pseudoexfoliation dilate poorly, even if miotics have never been used. They also constrict less well to topical 4% Pilocarpine.
REPO et al21 found that miosis is connected with degenerative changes
Marked IOP rises occur after pharmacological dilatation with a positive correlation between the extent of IOP rise and the pigment liberated.
Heavily pigmented synechiae may be present between the pupillary margin and anterior lens capsule.
Lens
Deposits of white material in the anterior lens surface is the most
consistent and diagnostic feature of pseudoexfoliation syndrome. The
classic pattern consists of three distinct zones that become fully visible in a fully dilated pupil.
1. Transclucent Central Zone
2. Intermediate clear zone
This zone surrounds the central disc in a concentric ring. It is thought that this clear zone is caused by the movement of the iris and pupillary border in eyes not on miotic therapy and thus, rubbing the exfoliative materials off the lens.
3. Peripheral granular zone
This zone surrounds the intermediate zone. It is always present. It may be granular in the periphery and frost white centrally and radial striations are often seen.
Development of pseudoexfoliation is described in various stages. In precapsular stage, a homogeneous "groundglass" or "matte"
appearance of the lens surface is noted. Ultrastructurally, the pre-capsular layer consists of micro-fibrils, but not mature exfoliation fibrils. Slightly later in pre-granular stage, a faint radiant non-granular striae is noticed on middle one third of the anterior capsule behind the iris.
away and eventually the clear zone is formed. With time, these clefts increase in size and become confluent and only small bridges may remain which indicates the previous layer of exfoliation material. The central disk may become thick in some patients and peel away in sheets from the lens, giving rise to appearance of True Exfoliation Syndrome.
Clinical classification of pseudoexfoliation syndrome based on morphologic alterations of the anterior lens capsule.
Preclinical stage (Electron Microscopy): Clinically invisible Suspected Pseudoexfoliation Syndrome: Precapsular layer. Mini-Pseudoexfoliation Syndrome: Focal defects in pre-capsular layer especially supero-nasally.
Classic Pseudoexfoliation Syndrome: Late stage.
Subluxation or dislocation of crystalline lens is a rare but definite complication of pseudoexfoliation syndrome. This is due to weakening of zonular attachment to ciliary body perhaps by the deposition of exfoliation material at the site of insertion of zonular fibres.
more likely the phacodonesis. Association with cataract formation is not clear. A study by SELAND22 (1982) revealed that Nuclear Cataract is more commonly associated than cortical cataract. A higher rate of sub capsular cataract has also been reported.
Zonules and Ciliary Body
Zonular exfoliation material may predate development of peripheral granular zone. Whether the zonules are just coated with exfoliation material or replaced by it, they are often frayed and broken. SCHLOTZER23 (1994) showed typical alterations occurred at three sites.
1. At their origin and anchorage in ciliary body, the zonular bundles were separated from the disputed basement membrane of the non pigmented epithelium by the intercalating exfoliation fibres
2. In the pars plicata of ciliary body, the material infiltrates the zonular bundles passing along the ciliary processes leading to rupture.
3. At their attachment to anterior lens capsule, zonular fibres were focally lifted and subsequently ruptured by exfoliation masses erupting the capsular mass.
revealed accumulation of exfoliative material in all eyes in which it is present on the anterior lens surface and in fellow eyes of unilateral cases24.
Anterior Chamber Angle
Increased trabecular pigmentation is a prominent sign in pseudoexfoliation syndrome especially in the posterior portion and may be an early diagnostic finding before deposits in the pupil or anterior lens capsule (SPAETH et al25 1985).
Many patients have open angle glaucoma. Recent studies by GROSS (1996) have shown that significant number of eyes have occludable angles.
Since iris is rigid, aqueous presence in posterior chamber causes it to bulge at the iris route which is the weakest point. Thereby, the localized iris bombe near the iris route narrows the angle, giving a pseudo-plateau iris configuration and leads to chronic angle closure glaucoma
Vitreous and Retina
After cataract extraction, exfoliative material may be found on the vitreous face, on vitreous strands when face is ruptured. KOZOBOLIS et al found a correlation between pseudoexfoliation and macular degeneration attributing this to the fact that both disorders increase with age and altitude. One study reported abnormalities of pattern ERG findings and and oscillatory potentials in eyes with exfoliation.
Optic Disc
Intraocular pressure
Mean IOP in normotensive eyes with pseudoexfoliation are usually higher than in those without pseudoexfoliation. Glaucomatous optic nerve head and visual field damage also tend to be greater in patients with pseudoexfoliation glaucoma. This reflects the effects of higher IOP on the optic nerve. Surgical treatment for glaucoma is often necessary in pseudoexfoliative glaucoma.
GLAUCOMA
About 50% of patients with exfoliation syndrome are ultimately diagnosed with glaucoma, whether found at the time of initial examination or at a later date. Figures vary from 20-85%. Pseudoexfoliation syndrome accounts for 15-20% of open angle glaucoma cases.
Pseudoexfoliation Syndrome, than in those with POAG. Glaucomatous damage of optic nerve at the time of diagnosis is more severe and progression is also more rapid in eyes with Pseudoexfoliative glaucoma.
Risk of glaucoma with time
In patients with pseudoexfoliation, the risk of developing glaucoma is cumulative over time. HENRY et al found 5 and 10 year cumulative probabilities of initially non-glaucomatous eyes with exfoliation developing glaucoma to be 5.3% and 15.4% respectively. Thus pseudoexfoliation should be a warning sign that glaucoma can develop. Patient should be followed at regular intervals and an accurate observation of the disc should be made at each examination.
OPEN ANGLE GLAUCOMA
Mechanism of glaucoma
Glaucoma‟s in eyes with pseudoexfoliation syndrome may be the result of
1. Blockage of trabecular meshwork by exfoliation material or pigment liberated from the iris.
2. Dysfunction of trabecular endothelial cells or
Secondary glaucoma due to exfoliation v/s POAG
Most researchers believe that glaucoma in pseudoexfoliation is a secondary process, distinct from primary open angle glaucoma.
Several clinical observations support this idea. First, pseudoexfoliation glaucoma has a more aggressive clinical course, with higher intraocular pressure and a poorer response to medication. Second, steroid challenge tests looking for intraocular pressure elevation after topical steroid treatment, revealed no increased incidence of higher responders as evidenced by a study by POHJOLO26 and associates. Finally elevated IOP occurs much more commonly in patients with pseudoexfoliation syndrome than in an otherwise method control population.
extracellular matrix components and further decrease the porosity of this critical portion of the aqueous outflow channels.
The second difference is the occurrence of plaques of material seen in primary glaucoma27. These plaques are actually fibrillar tendons with their surrounding collagen sheaths, running through juxtacanalicular tissue. When histological sections are cut in the usual radial orientation (sagittal sections), the tendon and sheaths appear as discontinuous plaques, whereas in tangential section they appear as tendons. The tendon sheaths become thicker with age and are especially thick in primary glaucoma, appearing as an increase in plaque material when viewed with the standard sagittal histologic sections. Pseudoexfoliation glaucoma eyes do not have this excess tendon sheath or plaque material but rather have amounts similar to control eyes26. This indicates a fundamental difference in the nature of pseudoexfoliative glaucoma and of primary glaucoma.
In patients with unilateral exfoliation and open angles, glaucoma may also occur in the uninvolved fellow eye, suggesting an underlying defect in the aqueous dynamics28. This concept is also consistent with the finding of greater pigmentation in the affected eye. It is possible that in eyes with normal aqueous dynamics, glaucoma will result.
Pigment may be a contributing factor in the pathogenesis of pseudoexfoliative glaucoma. Histologically, pigment is present within trabecular cells and occasionally within the intertrabecular spaces, although the outflow spaces do not appear narrowed enough because of this to produce elevated pressure29.
Unilateral exfoliation with bilateral glaucoma
The observation that some patients with unilateral exfoliation have bilateral glaucoma counters the idea of a simple obstruction. The recent finding that exfoliation material may be found in the conjunctiva in eyes with increased pigmentation of the trabecular meshwork in absence of clinically visible exfoliation of lens underscores the importance of further elucidation of its role in the development of glaucoma30.
ANGLE CLOSURE GLAUCOMA
occludable angles to be present in significant number of patients with exfoliation syndrome and they even go to the extent of suggesting that exfoliation syndrome may represent a high risk population for the development of angle closure glaucoma. However, these studies are in contrast to the studies of BARTHOLOMEW AND FORSUS et al18.
Another factor that may play role in the development of secondary glaucoma is the possible relationship of phakodonesis as a sign of zonular weakness or the complication of central anterior lens capsule adhesions to iris pigmentation. Both could cause increased pupillary block.
Factors favouring development of glaucoma
A vexing question still remains: Why do only some eyes with
pseudoexfoliation develop glaucoma? One factor may be simple the
composition and porosity of this region are determined in part by trabecular cells and thus may also vary between eyes. Exfoliation material probably passes through this tissue more easily in some eyes than others. With time, the cellular and extracellular capacities of almost any eye to deal with chronic, repetitive or large amounts of exfoliative material may become inadequate causing obstruction of aqueous channels and glaucoma.
BLOOD AQUEOUS BARRIER
Alterations of the integrity of blood aqueous barrier in pseudoexfoliation syndrome are frequent findings. KUCHLE et al
(1995) found that aqueous protein concentration in pseudoexfoliation
syndrome was significantly higher than normal and POAG patients. He also, quantified flare using Laser Flare Cell Meter (LFCM) and found it to be significantly increased in pseudoexfoliation syndrome patients.
Inflammation after cataract extraction is more common and a transient fibrinoid reaction is attributed to breakdown of Blood-aqueous barrier.
SOURCE OF EXFOLIATION MATERIAL
iris, ciliary processes and zonules.
INTRAOCULAR SITES
Lens
BUSACCA found minute vacuoles in the deep and superficial layers of the lens capsule with exfoliation material appearing to flake off the capsular surface. However, debate continues as to whether there is primary involvement of the capsule and epithelial cells of the lens or whether it is a secondary deposit.
Ciliary Processes
Iris
Exfoliation material has been found on the iris pigment epithelium, blood vessel wall and on the anterior stroma. Accumulation of material is seen on the pigment epithelium layer, both posteriorly and at the pupillary margin. Microscopically, exfoliative material is intermixed with a duplicated and disorganized basement membrane of iris pigment epithelial cells, which also have degenerative and disruptive changes. Iris vasculature may contain subendothelial accumulation of the material often in conjunction with disrupted basement membrane. These changes may occlude the lumen in some areas and may explain the clinical observation of drop out and leakage of iris vessels and occasional areas of vaso proliferation seen with fluorescein angiography.
Trabecular Meshwork
cells. Some studies have described exfoliation material to be present in sub cellular regions of trabecular lamellae and also within trabecular cell vacuoles, suggesting local production, whereas others have reported that these structures are normal29. Pseudoexfoliation syndrome is also associated with increased pigmentation of the meshwork. The pigment is undoubtedly washed in from the aqueous and appears as granules within trabecular cells as well as in the intertrabecular spaces.
HARNISCH described both intercellular and intracellular
pigment granules in trabecular cells. This is an indication that endothelial cells of trabecular beams are not as seriously involved as in pigmentary dispersion syndrome29.
Zonules
Although exfoliation material frequently coats the zonular fibres and has structural and histochemical similarity with them, the zonular fibres themselves are usually intact and unaffected.
EXTRA-OCULAR SITES
Conjunctiva
sclera channels, its presence on the palpebral conjunctiva makes this less likely. STREETEN7 and associates commented on the association of exfoliation fibrils with elastic fibrils and suggested pseudoexfoliation syndrome may be a type of elastosis resulting from an abnormal aggregation of components related to elastic microfibrils. They, also, found that conjuctival exfoliation material can be present in the absence of ocular exfoliation signs except for iris pigmentary dispersion and especially in patients with glaucoma.
Skin
Although an early study by RINGVOLD (1973) did not find exfoliation material on eyelid skin or oral mucosa, a study by
STREETEN33 (1990) found it in several skin sites distant from the eye.
Areas with exfoliation fibrils were retroauricular skin, buttock skin and eyelid skin. The exfoliation material was found primarily along elastic fibrils and appeared to be influenced by an accompanying dermal elastoses32.
EXFOLIATION SYNDROME - A SYSTEMIC DISORDER
STREETEN34 & SCHLOTZER35 found similar fibrils in a
connective tissue portions or septa. The presence of exfoliative fibrils in sites like skin and visceral organs remote from the eye points to the possibility of pseudoexfoliation syndrome being local manifestation of a systemic disorder closely related o elastosis. Lectin electron microscopical histochemistry of exfoliation material in skin by AMARI
et al (1994) revealed that both intraocular and extraocular materials were
of same nature. This study, the first documentation of lectin binding sites on extraocular exfoliation material, also, supported the hypothesis of pseudoexfoliation syndrome as a systemic disorder. Thus, exfoliation syndrome is now recognized as a systemic disorder. Association of pseudoexfoliation syndrome with aneurysm of abdominal aorta is being extensively studied.
NATURE OF EXFOLIATIVE MATERIAL
Despite pseudoexfoliation syndrome have been a recognized entity for over 80 years, the essential nature of exfoliation in the anterior segment of the eye is still obscure. It was hoped that the application of electron microscopy would supplement the limited information obtained from light microscopy and it has done so but, still, without resolving the essential nature of exfoliation material.
PAS positive staining substance under light microscopy2,31. Periodic Acid Schiff staining indicates a material rich in polysaccharides. Transmission electron microscopy shows exfoliation material to be randomly arranged tangle of filaments embedded in an amorphous ground substance. The filaments are small, thread-like rods, about 10nm in diameter, whereas the larger fibrils have a diameter of about 50nm. The fibrils show a characteristic banding31. The amorphous ground substance is thought to consist of glycosaminoglycans, consistent with Periodic Acid Schiff staining, where as filaments and fibrils are protein.
Scanning electron microscopy demonstrated exfoliation material
to be a roughly appearing coating, that under high power, is a fine net of fibrillar material and bushlike excrescences of coarser fibres. The distribution and appearances vary, resembling a precipitate in some areas of the lens and or more homogenous matted group of fibres in other areas.
A variety of enzymatic, histochemical and immunological tests have been performed on exfoliation material. These tests indicate that fibrils and filaments consist of noncollagenous protein, because they are insoluble in enzymes and do not contain hydroxyproline. Amino acid
1. Microfibrils of elastin 2. Basement membrane 3. Amyloid
Elastin
Elastic tissue, basically, consists of 2 major components: elastin, an amorphous appearing, insoluble protein and elastic filaments of which there are several varieties including oxytalan. The elastic filaments themselves consist of glycoproteins. Ultrastructural, histochemical and antigenic similarities exist between elastic filaments and exfoliation material37. Oxytalan is the essential protein component of zonular fibres. It is present in body in areas of mechanical stress. GARDNER &
ALEXANDER (1984) suggested that it can also be the product of either
lens or ciliary processes epithelium, these also being subject to variable mechanical stresses in accordance with demands of accommodation. It is in this context that they proposed the term oxytalanosis of the aqueous
for this condition.
NETEN (1995) did an electron microscopic study of optic nerve
pseudoexfoliation syndrome with glaucoma, suggesting an abnormal regulation of elastin synthesis or degradation on optic nerve head of patients with pseudoexfoliation syndrome.
Basement Membrane
Numerous studies have described exfoliation material in association with basement membrane, which often appear duplicated,
disrupted or degenerated. These changes are present in the lens capsule
and have also been noted in the iris, ciliary processes and conjunctiva. Basement membrane is a conglomeration of material by the epithelial cells and is present in structure throughout the age. It consists of collagen filaments intermixed with glycoprotein (laminin and fibronectin) and proteoglycans. The diffuse locations of exfoliative material in accompaniment with abnormally appearing basement membrane has led
EAGLE et al5 to call the condition basement membrane exfoliation
syndrome. Whether basement membranes throughout the body are
affected is unclear, because reports are contradictory with regard to the presence of material in the skin in sites distant to the eye.
Amyloid
stains suggestive of amyloid: congo red, thioflavin T and thioflavin S. Both amyloid and exfoliation material also stain with ruthenium red and react positively for tyrosine and tryptophan on histochemical tests36, 31. Several patients with amyloidosis have been reported to have deposits on the equator of the lens capsule and on the surface of iris, reminiscent of exfoliative deposits38. Although these cross reactivities and similarities are alluring, they are not pathognomonic. Amyloid is usually thought to consist of immunoglobulin light chains and exfoliative material. In addition, other studies have failed to find pseudoexfoliation to stain with congo red and also comment on the nonspecificity of the thioflavin reaction36, 31.
DIAGNOSIS
Koeppe gonioscopy appears to be more revealing than with gonioscopy with Zeiss or Goldmann lenses. When one sweeps across the iris to the angle, small deposits in the pupillary border can be highlighted. Cystoscopy may also be helpful in making a diagnosis. However the identification of small amount of pigment on endothelium of cornea, elevated IOP, characteristic pigmentation on gonioscopy and deposits on the anterior surface of pupil and lens are generally sufficient.
DIFFERENTIAL DIAGNOSIS
The most important entity in the differential diagnosis of pseudoexfoliation syndrome is pigment dispersion syndrome.
Pigment dispersion syndrome
discontinuous, segmented, pattern. Transillumination defects in a pigmentary glaucoma are midstromal and slit like but in pseudoexfoliation syndrome are at pupillary ruff and margin.
True exfoliation
True exfoliation of the lens capsule should also be differentiated. It is seen in those with exposure to high temperature, such as glass blowers, is associated with cataract and rarely associated with glaucoma. The deposit from the heat induced cataract is rolled up in a characteristic thin sheet as a clear diaphanous membrane with a free edge floating in the aqueous, in contrast to the frosty appearance of pseudoexfoliation syndrome.
Iritis with pigment dispersion on the meshwork and adhesions of
pupillary marginto the anterior lens capsule can be differentiated by the absence of exfoliation material on the anterior lens capsule.
Toxic exfoliation from iridocyclitis or foreign bodies such as
Other conditions characterized by pigment changes such as
Fuch’s Heterochromic Iridocyclitis, pigmentation of anterior chamber
angle with ageing or after surgery and pigmentation secondary to intraocular tumours can usually be readily distinguished.
MANAGEMENT
Glaucoma
The frequent association of glaucoma in pseudoexfoliation syndrome and its aggressive nature requires the clinician to be wary of the condition. Regular periodic examinations should be performed with initial baseline optic disc drawings or photographs. Tonography may give an indication of function of outflow channels, with borderline or abnormal values indicating more frequent follow up.
Medical
Laser
Argon laser trabeculoplasty is especially successful in pseudoexfoliation syndrome. Studies report average initial success rate upto 80%39. The increased success rate is thought to be due to the higher starting IOPs and the generally increased trabecular pigmentation40. As in POAG, success rates decrease with time, averaging 50% or less in 5 years39.
In narrow angle glaucoma in pseudoexfoliation, laser iridotomy should be preceded by peripheral iridoplasty to widen the distance between iris and trabecular meshwork41.
Surgery
Trabeculectomy in pseudoexfoliation syndrome has success rate similar to that in POAG. According to Törnqvist & Drolsum42 (1991), 77%, 64% and 48% of patients with pseudoexfoliation glaucoma did not require any glaucoma therapy after 2,5 and 10 years of observation.
JACOBIE et al43 (1995) have reported success with Trabecular
Aspiration, a technique designed to remove pseudoexfoliation material
Non penetrating filtering surgery is another treatment option in pseudoexfoliation glaucoma. Studies by Drolsum44 2006 found similar success rates following deep sclerectomy in pseudoexfoliation glaucoma and POAG after follow up of 3.5 years. Since anterior chamber is not entered in non penetrating surgeries it is of benefit in pseudoexfoliation syndrome where there is abnormal blood aqueous barrier. However, the trabeculo-Descemets membrane is more fragile in eyes with pseudoexfoliation so the surgery becomes difficult.
CATARACT SURGERY IN PSEUDOEXFOLIATION
Patients with Pseudoexfoliation Syndrome are prone to have more complications during cataract surgery. Due to poor pupillary dilatation in eyes with pseudoexfoliation syndrome they have greater incidence of capsular rupture, zonular dehiscence and vitreous loss. Pupillary diameter and zonular fragility are the most important risk factors for capsular rupture and vitreous loss.
Posterior capsular opacification is more common. Zonular weakness may lead to late post-operative decentration of intra-ocular lens. Also exaggeration of Capsular contraction syndrome can lead to intra-ocular lens dislocation. Aggravation blood-aqueous barrier breakdown can lead to secondary cataract.
Skuta G.L., Parrish R.K.et al45 (1987) showed an increased
incidence of zonular dialysis during cataract surgery in patients with Pseudoexfoliation Syndrome. It was stated by them that pre-operative phacodonesis, excessive lens movement during anterior capsulotomy and anterior chamber depth asymmetry should alert to the presence of zonular dialysis.
Naumann G.O., Kuchle M. Schonherr U46 (1989) noted a
seven fold increase in vitreous loss during cataract surgery in 72patients with Pseudoexfoliation Syndrome undergoing surgery.
Wang L., Yamasita R.et al47 (1999) studied 26eyes with
Pseudoexfoliation Syndrome and an inverse correlation was shown with the flare.
Lumme P. Lattikaanen L48 (1993) performed a prospective
study of 351 patients undergoing cataract surgery. The prevalence of Pseudoexfoliation Syndrome was more in patients greater than 70years in their study. The risk of intra-operative complications in Pseudoexfoliation Syndrome is increased either directly (due to rupture of zonules) or through poor dilation of pupil (rupture of posterior capsule). There was four fold occurrence of vitreous loss and there was tenfold need to use anterior chamber intra-ocular lens was in these patients.
Moreno et al49 (2000) suggested poor dilatation,
Freyler H. Radax U50 (1994) compared ECCE with
phacoemulsification in 311 and 68patients respectively. Poor pupillary dilatation and phacodonesis were reported as the primary risk factors for cataract surgery in Pseudoexfoliation Syndrome. Compared with ECCE, phacoemulsification had significantly fewer complications with regard to poor pupillary dilatation but not phacodonesis. They advised applying a small iris retractor to reduce the complications arising from poor dilatation.
Kuchle et al51 (2000) suggested that a shallow anterior chamber
depth of less than 2.5mm pre-operatively indicates zonular instability and should alert the surgeon of intra-operative complications.
Bayram laret al52 (2007), conducted a retrospective study in 225
Albert Galand M D, Michael Kuchle M D, Etienne Thchet
MD53(2004) during a symposium held in the 21st congress of the ESCRS reviewed the patho-physiological alterations associated with pseudoexfoliation, the complications of cataract surgery, and the considerations for surgical modifications and IOL selection. They stressed on poor dilatation, and its management by injection of high viscosity visco elastic agent. They also advocated use of iris hooks, either plastic or metallic as necessary. Dr.Hachet cautioned against performing sphincterotomy, because it resulted in persistent dilatation and poor postoperative cosmosis. He advocated the use of capsular tension rings. Foldable IOL‟s is desirable to minimize the induction of blood-aqueous barrier breakdown. Also hydrophobic acrylic and silicone are associated with a low rate of PCO, but hydrophobic acrylic has an additional advantage as it causes the least amount of capsular contraction. For haptics, open loop haptics are probably preferred. Dr
Kuchleal so discouraged the use of plate haptic design or
accommodative IOL‟s in patients with pseudoexfoliation.
Vickie Lee and Anthony Maloof 54(2002) stated that a CTR by
Howard Fine55 (2008) suggested that CTR will convert a high
risk case with compromised zonular integrity into a routine case. CTR work because the ring diameter is larger than that of the capsule diameter so that there is centrifugal force on the capsular fornix. Any focal force on the capsule cannot be transmitted only to the adjacent zonules, the CTR.
It makes that focal force distributed circumferentially to the entire zonular apparatus. In cases of advanced zonulopathy with subluxation of the capsular bag, the capsular tension segments (CTS) can be used. The CTS is a 120˚ partial CTR that features an islet positioned within the capsulorrhexis to receive an iris hook for support. Two CTS can be used to support a very lose bag. The CTS can also be used in eyes with anterior or posterior capsular tears. The CTS are also designed for suture sclera fixation, also for long term capsular bag centration.
TRABECULECTOMY AND COMBINED SURGERY IN
PSEUDOEXFOLIATION
case of loose zonules and anterior movement of lens, vitreous may obliterate trabeculectomy opening. The risk of fibrinous reaction in the early post op period is increased in pseudoexfoliation.
Combined cataract and glaucoma surgery is an option in pseudoexfoliation eyes with cataract and glaucoma. Studies have reported results similar to that in eyes with POAG.
MANAGEMENT OF CATARACT SURGERY IN
PSEUDOEXFOLIATION SYNDROME56, 57, 58, 59, 60
These are several important points to remember during cataract surgery in eyes with Pseudoexfoliation syndrome.
1. Making the diagnosis
Limited pharmacological mydriasis adversely affects the ability to make the diagnosis. Flaky deposits on the corneal endothelium can be differentiated from true keratic precipitate by their bright white color and fluffy appearance. When differentiation is difficult, a one to two week course of topical steroids can help in diagnosis, as keratic precipitates change in appearance or disappear with topical steroid use but there is no effect on exfoliation material.
instability indicates Pseudoexfoliation especially if it is asymmetrical. Even though a patient's symptomatic complaints and cataract are monocular, the contra-lateral eye may have subtle findings of pseudoexfoliation.
Even if Pseudoexfoliation material is not clinically visible on the endothelium, the endothelial cell count may be significantly reduced and the remaining cells may not function well, hence additional endothelial protection including a viscoelastic such as healon is advised.
2. Maximal dilatation of pupil during surgery.
cause posterior pressure on the lens and further damage the weakened zonules.
3. Ensuring adequate capsulorrhexis/capsulotomy.
4. Attention to phacodonesis while performing capsulorrhexis /
capsulotomy.
Weak zonules is one of the most notorious and significant problem faced by cataract surgeon in Pseudoexfoliation syndrome. Dislocation of the nucleus into the vitreous cavity may occur during routine hydrodissection. During capsulorrhexis or capsulotomy creation, if diffuse zonular weakness or laxity is sensed, then use of flexible "iris" retractors can engage the capsulorrhexis margin and stabilize the loosened capsular bag61.
5. Management of zonular dialysis.
6. Choice of intraocularlens.
Capsular contraction is more likely as there is reduced zonular counter- traction against the centripetal forces of the lens epithelial cells. Capsulorrhexis of 5mm or greater, and use of a CTR is advisable to reduce risk of this complication. As capsular contraction is more common with silicone intraocular lens, another material is recommended. An intraocular lens with a sharp posterior edge is recommended to reduce lens epithelial cell migration and subsequent posterior capsular opacification.
AIM OF THE STUDY
To clinically analyze cases of pseudoexfoliation syndrome
1. To determine the association of glaucoma in pseudoexfoliation syndrome with respect to
a. Type
b. Presentation of glaucoma
MATERIALS AND METHODS
100 patients with pseudoexfoliation syndrome who attended the Regional Institute of Ophthalmology and Government Ophthalmic Hospital between November 2012 and September 2014 were included in the study.
SELECTION CRITERIA:
Presence of exfoliation material on the pupillary margin and/or lens.
EXCLUSION CRITERIA:
Patients with
1. Previous history of trauma 2. Anterior uveitis
3. Secondary cataract
4. primary open and closed angle glaucoma 5. Other secondary glaucoma
METHOD:
All the patients were subjected to a detailed slit lamp examination and following signs were looked for
Conjunctiva-congestion
Cornea-edema, pigmentation, exfoliation material
Anterior chamber depth-flare, cells, depth, exfoliation material, pigment dispersion
Iris-pattern, transillumination defects, iridodonesis
Pupil-size, reaction to light, exfoliation material, dilatation with mydriatics
Lens-exfoliation material, cataractous or not, phacodonesis, subluxation or dislocation of lens
Pupil was dilated as a routine in most of the cases to note the three zones of exfoliation material on the lens capsule.
Glaucoma workup was done for all patients, which included Gonioscopy with Goldmann single mirror lens, Tonometry using Goldmann applanation tonometer, automated perimetry with octopus 301 in selected cases. During gonioscopy the presence of exfoliation material and increased trabecular pigmentation were also noted.
In patients undergoing cataract or combined surgery, A scan, K reading were noted and IOL power was calculated by SRK 2 formula.
Routine investigations like blood sugar, urine albumin sugar and blood pressure measurement were done.
Pre operative preparation for cataract or combined surgery
The patients undergoing cataract surgery or combined surgery were given topical antibiotic eyedrops 6 times/ day on pre operative day.
On the day of surgery pupils dilated adequately with 0.8% tropicamide and 5% phenylephrine eye drops every 15 minute, 1 hr before surgery.
Steps of manual SICS:
xylocaine mixed with 1500 U of hyaluronidase. Universal eye speculum was applied. Superior rectus suture applied to fix the eye in downward gaze. Conjunctival peritomy done and sclera was exposed. Hemostasis was achieved using adequate cautery. A self sealing sclero corneal tunnel incision made. Anterior capsulotomy was done by continuous curvilinear capsulorrhexis or can opener technique as per surgeon‟s preference. Hydrodissection was done. Depending on degree of mydriasis pupil was stretched mechanically or sphincterotomies were done. Nucleus delivered and cortical matter removed by irrigation and aspiration. In case of posterior capsular tear, integrity of capsular bag was assessed to place IOL. In case of vitreous loss, manual anterior vitrectomy was done. If there was no complication posterior chamber intraocular lens was placed in capsular bag. Visco elastic cleared from anterior chamber. Subconjunctival Gentamicin with Dexamethasone 0.5cc given at end of procedure. Pad and bandage applied.
Steps of Combined Surgery:
Postoperatively all patients received topical antibiotic steroid eye drops 6 times a day initially which was tapered every week .Systemic antibiotics given for 3 post operative days.
Follow up:
Patient undergoing cataract and combined surgery were under follow up for 6 weeks post operatively- initially weekly for 2 weeks, every 2 weeks for one month. At each visit, visual acuity measurement, anterior segment examination, intraocular pressure measurement and fundus examination were done.
OBSERVATION AND RESULTS
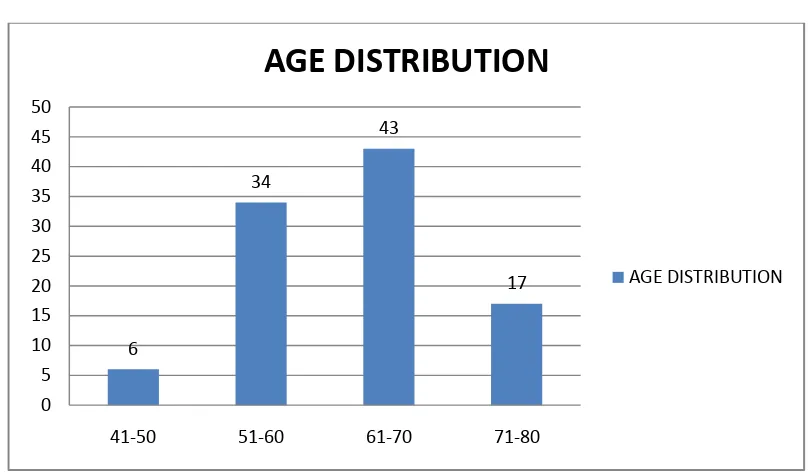
[image:71.596.102.506.349.585.2]AGE DISTRIBUTION:
Table no 1 Age Distribution
Age(years) No of cases
41-50 6
51-60 34
61-70 43
71-80 17
Chart no 1 Age Distribution
In our study, out of 100 cases, 6 cases presented between 41-50 years, 34 cases between 51-60 years, 43 cases presented between 61-70 years and 17 cases between 71-80 years. Thus the most common age group was between 61-70 years followed by 51-60 years. The mean age of the patients was 63.71 years.
6 34 43 17 0 5 10 15 20 25 30 35 40 45 50
41-50 51-60 61-70 71-80
AGE DISTRIBUTION
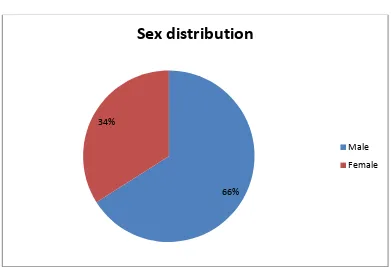
SEX DISTRIBUTION:
Table no 2 Sex distribution
Sex No of cases %
Male 66 66
Female 34 34
Chart No 2 Sex distribution
Out of the 100 cases with pseudoexfoliation, 66 (66%) were males and 34(34%) were females.
66% 34%
Sex distribution
Male
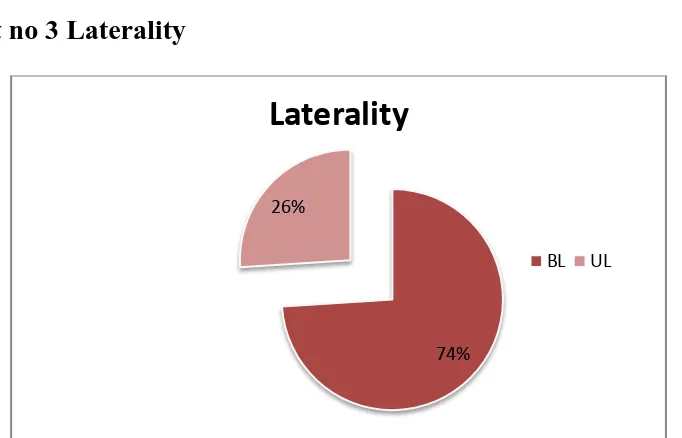
LATERALITY:
Table no 3 Laterality
No of cases % No of eyes
UL 26 26 26
BL 74 74 148
Total 100 100 174
Chart no 3 Laterality
74(74%) cases had bilateral pseudoexfoliation and 26(26%) had unilateral pseudoexfoliation. Thus, totally 174 eyes of 100 patients had pseudoexfoliation.
The higher incidence of bilateral exfoliation in this study is in accordance with various other studies (by Bartholomew 197162, Maden63 1982, Collin 64 1982).
This could be due to the possibility that the unilateral cases invariably become bilateral at a later date. The 26 patients are at risk of developing pseudoexfoliation in the other eye later. Hence they need to be followed up.
74% 26%
Laterality
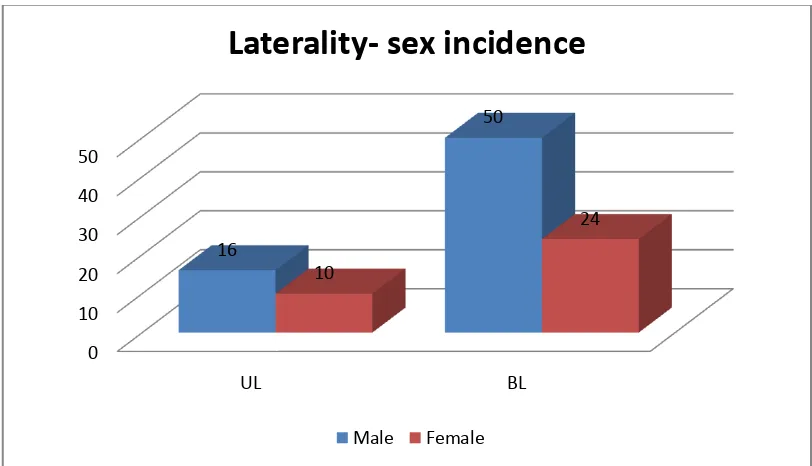
Laterality- Sex incidence
Table no 4: Laterality- sex incidence
Male Female Total
No % No % No %
UL 16 76.92 10 38.46 26 100
BL 50 67.56 24 32.43 74 100
Chart No 4: Laterality-sex incidence
There was a male preponderance in both unilateral and bilateral groups. TAYLOR65 1980 and RESNIKOFF et al66 (BJO 1991)
suggested that pseudoexfoliation syndrome could be related to environmental factor, ultraviolet light and hence the male preponderance in this study can be explained to some extent by the fact that Indian males are more likely to have outdoor activities than females.
0 10 20 30 40 50
UL BL
16
50
10
24
Laterality- sex incidence
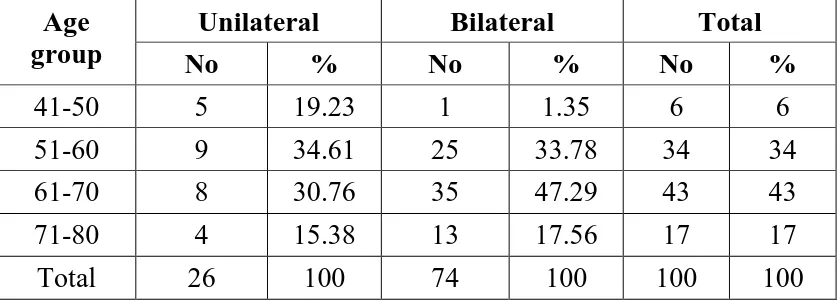
Laterality-age incidence:
Table no 5 Laterality-Age incidence
Age group
Unilateral Bilateral Total
No % No % No %
41-50 5 19.23 1 1.35 6 6
51-60 9 34.61 25 33.78 34 34
61-70 8 30.76 35 47.29 43 43
71-80 4 15.38 13 17.56 17 17
Total 26 100 74 100 100 100
Chart no 5 Laterality-Age incidence
The most common age group in bilateral cases was between 61-70 years followed by 51-60 years. In unilateral cases the most common age was between 51-60 years.
Thus, suggesting that patients with bilateral involvement were slightly older than those with unilateral involvement.
unilateral bilateral 0 5 10 15 20 25 30 35 41-50 51-60 61-70 71-80
5 9 8
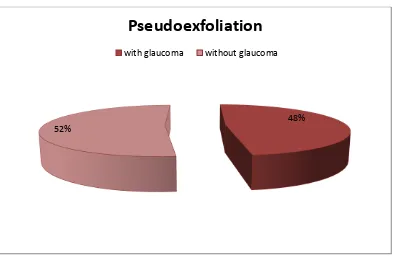
GLAUCOMA ASSOCIATION:
Table no 6 Glaucoma association
Pseudoexfoliation syndrome No of cases %
With glaucoma 48 48%
Without glaucoma 52 52%
Chart no 6 Glaucoma association
Out of the total 100 patients with pseudoexfoliation, 48(48%) patients had glaucoma while 52(52%) had no glaucoma. The incidence of glaucoma in pseudoexfoliation varies from 20-85% in the literature.
48% 52%
Pseudoexfoliation
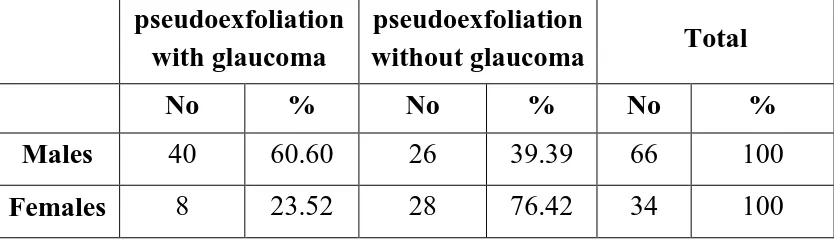
Sex incidence-glaucoma
Table no 7 Sex incidence-glaucoma
pseudoexfoliation with glaucoma
pseudoexfoliation
without glaucoma Total
No % No % No %
Males 40 60.60 26 39.39 66 100
Females 8 23.52 28 76.42 34 100
Chart no 7 Sex incidence-glaucoma%
Males showed higher predominance in pseudoexfoliation glaucoma than the females.
According to reports in literature, MADDEN et al57 in 1982, LAMBA & GIRIDHAR JIPMER 681984 reported a definite male preponderance similar to this study.
40 8 26 28 0 5 10 15 20 25 30 35 40 45 males females
Sex incidence-glaucoma
exfoliation with glaucoma
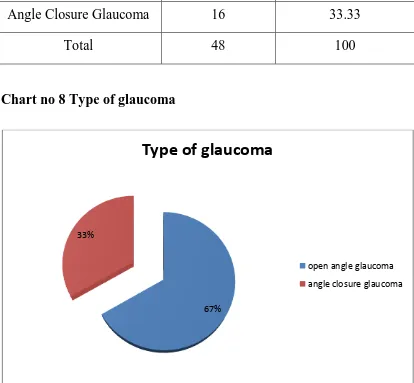
Type of glaucoma:
Table no 8 Type of glaucoma
Type of glaucoma No of patients %
Open Angle Glaucoma 32 66.66
Angle Closure Glaucoma 16 33.33
Total 48 100
Chart no 8 Type of glaucoma
Among the 48 patients with glaucoma, 32(66.66%) had open angle glaucoma and 16(33.33%) had angle closure glaucoma. Thus open angle glaucoma is more common in pseudoexfoliation syndrome.
67% 33%
Type of glaucoma
open angle glaucoma
Open angle glaucoma:
Table no 9A Open angle glaucoma Laterality
Open angle glaucoma No of cases %
Unilateral 12 37.50
Bilateral 20 62.5
Total 32 100
Table no 9B Unilateral open angle glaucoma
Unilateral open angle glaucoma No of cases
With bilateral pseudoexfoliation 4 With unilateral pseudoexfoliation 8
Total 12
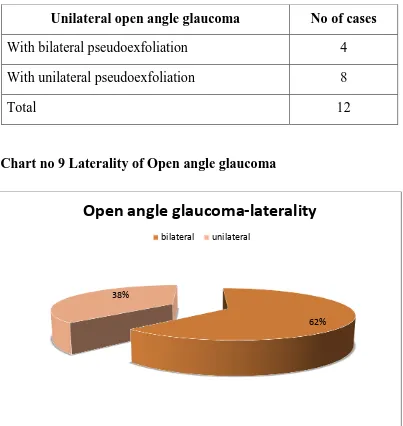
Chart no 9 Laterality of Open angle glaucoma
62% 38%
Open angle glaucoma-laterality
[image:79.596.104.507.296.722.2]Out of the 32 cases of open angle glaucoma, 20(62.50%) cases had bilateral open angle glaucoma and 12 cases (37.50%) had unilateral open angle glaucoma.
Out of the 12 cases with unilateral open angle glaucoma, 4 had pseudoexfoliation in both eyes, but glaucoma only in one eye. These patients are at high risk of developing glaucoma in the fellow eye and hence require regular follow up.
Angle closure glaucoma:
Table no 10 laterality of angle closure glaucoma
No of cases %
unilateral 7 43.75
bilateral 9 56.25
total 16 100
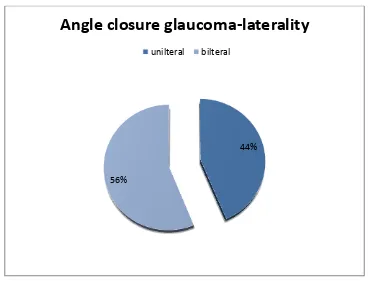
Chart no 10 Angle closure glaucoma laterality
Out of the 16 cases with angle closure glaucoma, 9 had bilateral angle closure glaucoma and 7 had unilateral angle closure glaucoma.
Among the 7 unilateral cases, 2 cases had secondary angle closure due to subluxated lens. There was no history of trauma in any case of subluxation. Thus, the subluxation evidenced by phacodonesis
44%
56%
Angle closure glaucoma-laterality
and iridodonesis is due to exfoliation material causing zonular weakness and hence pseudoexfoliation is attributed as the cause for angle closure glaucoma.
In remaining 5 cases of unilateral exfoliation and 9 cases of bilateral exfoliation and there was no secondary factor other than pseudo exfoliation. The fellow eyes also had shallow anterior chamber in unilateral cases. These patients are likely to have primary angle closure glaucoma with co existing pseudoexfoliation. Pseudoexfoliation may be the cause for aggravating angle closure glaucoma. A study by
EPSTEIN et al69 1994 has also highlighted the increased incidence of
angle closure glaucoma in pseudoexfoliation syndromes.
Apart from the 16 cases with angle closure glaucoma, occludable angles with normal IOP was noted in 5 cases. In studies of patients with Pseudoexfoliation syndrome, occludable angles were noted in 9-18% of patients (Bruce shields 1999, fourth edition).
Ritch, Schlotzer - Scherhardt (2001) noted 23% of patients with
pseudoexfoliation syndrome and glaucoma to have grade 2 or narrow angles.
Wishart et al70 (1985) noted 32% of patients in their study to
Sex incidence of glaucoma
Table no 9 Sex incidence of glaucoma
Male Female Total
Open angle glaucoma
unilteral 9 3 12
bilateral 17 3 20
Angle closure glaucoma
unilateral 6 1 7
bilateral 8 1 9
Total 40 8 48
Chart no 9 Sex incidence of glaucoma
Males had a higher preponderance in both open angle and angle closure glaucoma when compared to females.
0 2 4 6 8 10 12 14 unilateral
OAG bilateral OAG unilateral
ACG bilateral ACG
Optic Nerve damage in glaucoma
Table no 10 Optic nerve damage in glaucoma
Optic nerve head
No damage (no of eyes)
Early glaucomatou
s damage (no of eyes)
Advanced glaucomatou
s damage (no of eyes)
Total (no of eyes)
Open angle glaucoma
9 24 22 52
Angle closure glaucoma
11 7 7 25
Chart no 10 Optic Nerve damage in glaucoma
Out of the 52 eyes with open angle glaucoma, no optic nerve damage was seen in 9(17.30%) eyes, early glaucomatous damage was seen in 24(46.15%) eyes and advanced glaucomatous damage in 22(42.30%) eyes. Out of the 27 eyes with angle closure glaucoma 11(40.74%) showed no damage, 7(25.92%) eyes showed early damage and 7(25.92%) eyes showed advanced glaucomatous damage. Thus advanced glaucomatous optic nerve damage is noted more in open angle glaucoma. 0 5 10 15 20 25 Open angle glaucoma angle closure glaucoma 9 11 24 7 22 7
Optic nerve damage
no damage
early glaucomatous damage