Original Research Article
Vitamin D status in asthmatic children and its correlation to
asthma control
Sandeep Karanam, Soumya Reddy*, Ramesh H.
INTRODUCTION
Asthma is a common disease, affecting an estimated 330 million individuals worldwide with a reported prevalence of 5-20% in children aged between 6-15yrs.1,2 Like many
other chronic disorders, childhood asthma is likely to have an impact on the social and emotional aspects of lives of children and their families. In addition, there may be considerable financial burden on families. It also reduces the quality of life of children as it leads to growth retardation, inability to exercise and nocturnal bouts of
wheezing resulting in loss of sleep that may impair daytime concentration at school.
Bronchial Asthma is defined as a chronic inflammatory disorder of the airways associated with increased airway hyper-responsiveness, recurrent episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night/early morning.
Airway inflammation produces airflow limitation through acute bronchoconstriction, chronic mucus plug formation
ABSTRACT
Background: Asthma is a common chronic inflammatory disease of the airways, affecting around 330 million individuals worldwide. Factors like genetic predisposition, early allergen exposure, diet and vitamin D status are all proposed to influence the development and severity of asthma. Epidemiologic data suggests that low serum vitamin D (<30 ng/mL) in children with asthma is associated with more symptoms and exacerbations. The objectives of this study were to determine serum levels of vitamin D in asthmatic children (6-15 years) and to establish a relation between serum vitamin D levels and asthma control.
Methods: We conducted a cross sectional observational study. A total of 60 children with asthma were studied to know the relationship between serum vitamin D levels and asthma control, assessed according to Global Initiative for Asthma guidelines (GINA).
Results: Only 33.33% of children had sufficient vitamin D levels. Mean±SD vitamin D level of study population was 23.38±8.75. 45% children had well controlled asthma, 28.3% were partly controlled and 26.7% were uncontrolled. Significant (p <0.001) inverse association was found between level of asthma control and vitamin D status. Significant positive correlation was found between percent predicted forced expiratory volume in 1 second and forced vital capacity (P <0.01). Subjects with well controlled asthma had higher serum levels of 25 (OH) D than children with partially controlled or uncontrolled asthma.
Conclusions: Hypovitaminosis D is frequent in children with asthma and is associated with exacerbations, decreased lung functions and severe disease.
Keywords: Asthma, Asthma control, Hypovitaminosis D, Vitamin D Department ofPaediatrics, JJM Medical College, Davangere, Karnataka, India
Received: 15 December 2017
Accepted: 19 January 2018
*Correspondence:
Dr. Soumya Reddy, E-mail: sr2390@gmail.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
and airway wall oedema or remodelling. Factors such as genetic predisposition, early allergen exposure, infections, diet, tobacco smoke exposure, pollution and vitamin D status are all proposed to influence the development and severity of asthma.3-5
Over the last few decades, vitamin D deficiency and insufficiency are increasingly being recognized in the general population, and have been largely attributed to dietary, lifestyle and behavioural changes.6 The
musculoskeletal consequences of vitamin D deficiency are well established; however, a number of pulmonary disorders, including asthma, have now been linked to vitamin D status.
Vitamin D has been shown to have several effects on the innate and adaptive immune systems that might modulate the severity of asthma. Airway epithelia contain high levels of the enzyme that converts circulating 25-OH-vitamin D3 to its active form, 1,25-OH- 25-OH-vitamin D3. This active form of vitamin D has local effects in response to infections7,8 and might dampen the inflammation that is
the consequence of these infections.9
Vitamin D also has a potentially therapeutic role in reducing asthma exacerbations through its beneficial actions on TH1, TH2, and regulatory T cells.10
Epidemiologic data in most of the reported studies suggest that low serum vitamin D (defined as circulating levels of 25(OH)D of <30 ng/mL) in children with asthma is associated with more symptoms, exacerbations, reduced lung function, increased medication usage and severe disease.7,10
Aims and objectives of this study were to determine serum levels of vitamin D (25-hydroxy cholecalciferol) in asthmatic children between 6 -15 years of age, to assess level of asthma control using Global Initiative for Asthma (GINA) guidelines and to establish correlation between serumvitaminDlevelsandlevelofasthmacontrol
.
METHODS
A cross sectional observational study conducted in the Department of Paediatrics, in two hospitals attached to J.J.M Medical College, Davangere namely, Chigateri General Hospital, Davangere and Bapuji Child Health Institute and Research Centre, Davangere
All children aged between 6-15years with asthma (diagnosed as per GINA guidelines/asthma by consensus guidelines) brought to out-patient department/admitted to Chigateri and Bapuji hospitals attached to J.J.M Medical College between November 2015 to November 2016 were considered for this study.
Inclusion criteria
All children aged between 6-15 years diagnosed with bronchial asthma.
Exclusion criteria
• Children on vitamin D supplements
• Children on drugs which might affect vitamin D levels for the past one year
• Children with renal, liver and endocrine diseases
Sample design and size
Sample size was calculated using appropriate formula taking 5% level of significance and was estimated to be 60.
Method of examination
After taking informed consent, a pre-structured questionnaire was used to record the relevant information from individual cases selected for study, detailed clinical examination was conducted and level of asthma control over a period of 4 weeks was assessed as per GINA guidelines. All selected cases were subjected to spirometry as per ATS (American Thoracic Society) guidelines.
Under aseptic precautions blood was drawn for estimation of serum 25, OH-D levels and analyzed using fully automated chemiluminescent immunoassay using Siemens ADVIA Centaur, standardized against ID-LC/MS/MS, as per vitamin D standardization program.
RESULTS
Descriptive and inferential statistical analysis was carried out in the present study. Significance was assessed at 5% level of significance. Chi-square/Fisher exact test was used to find the significance of study parameters on categorical scale between two or more groups.
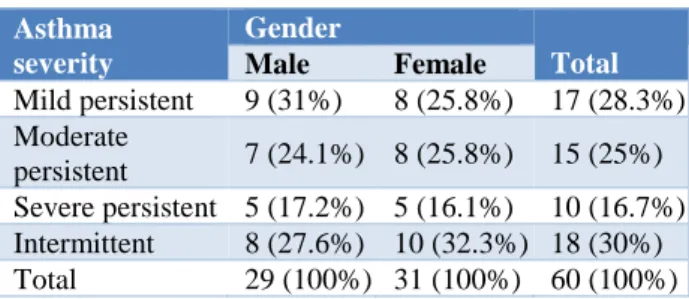
Table 1: Severity of asthma.
Asthma severity
Gender
Total Male Female
Mild persistent 9 (31%) 8 (25.8%) 17 (28.3%) Moderate
persistent 7 (24.1%) 8 (25.8%) 15 (25%) Severe persistent 5 (17.2%) 5 (16.1%) 10 (16.7%) Intermittent 8 (27.6%) 10 (32.3%) 18 (30%) Total 29 (100%) 31 (100%) 60 (100%)
Significant diurnal variation was observed in study subjects with most of them (70%) experiencing symptoms during night time, followed by early morning hours. Mild persistent asthma was found in 17 cases (28.3%), moderate persistent in 15 (25%), severe persistent asthma in 10 (16.7%) and intermittent asthma in 18 (30%) (Table 1).
Level of asthma control was assessed based on GINA guidelines. 45% of the study population were found to have well controlled asthma, 28.3% were partly controlled and 26.7% had uncontrolled asthma (Table 2).
Table 2: Level of asthma control.
Asthma control Gender Total
Male Female
Well controlled 11 (37.9%) 16 (51.6%) 27 (45%) Partly controlled 9 (31%) 8 (25.8%) 17 (8.3%) Poorly controlled 9 (31%) 7 (22.6%) 16 (26.7%) Total 29 (100%) 31 (100%) 60 (100%)
Based on vitamin D levels, study population was divided into three groups: deficient (serum 25-OH Vitamin D levels <20 ng/ml), insufficient (serum 25-OH Vitamin D levels between 20- 30ng/ml) and sufficient (serum 25-OH Vitamin D levels >30ng/ml). 40% of study subjects were deficient, 26.3% were insufficient and 33.3% had sufficient vitamin D levels (Table 3).
Table 3: Vitamin D status.
Vitamin D status
Gender
Total Male Female
Deficient 12 (41.4%) 12 (38.7%) 24 (40%) Insufficient 7 (24.1%) 9 (29%) 16 (26.7%) Sufficient 10 (34.5%) 10 (32.3%) 20 (33.3%) Total 29 (100%) 31 (100%) 60 (100%)
Mean age of onset of asthma in years±SD was 7.75±3.2, 6.7±2.7, 6.8±2.4 in deficient, insufficient and sufficient groups respectively.
We found a significant inverse correlation between level of asthma control and vitamin D levels. 75% of children with sufficient vitamin D levels had well controlled asthma, conversely 66.7% of children with vitamin D deficiency had uncontrolled asthma (Table 4).
There was also a significant relation noted between vitamin D levels and severity of asthma. 70% of children with sufficient vitamin D levels had intermittent asthma as compared to 41.7% and 50% of children with severe persistent asthma and moderate persistent asthma respectively. We noticed that number of hospitalizations/emergency visits per year were higher in vitamin D deficient group than insufficient/sufficient group (p = 0.03, moderately significant).
Table 4: Level of asthma control and association with Vitamin D status.
Level of control Vitamin D status
Total Deficient Insufficient Sufficient
Well controlled 2 (8.3%) 10 (62.5%) 15 (75%) 27 (45%)
Partly controlled 6 (25%) 6 (37.5%) 5 (25%) 17 (28.3%)
Uncontrolled 16 (66.7%) 0 (0%) 0 (0%) 16 (26.7%)
Total 24 (100%) 16 (100%) 20 (100%) 60 (100%)
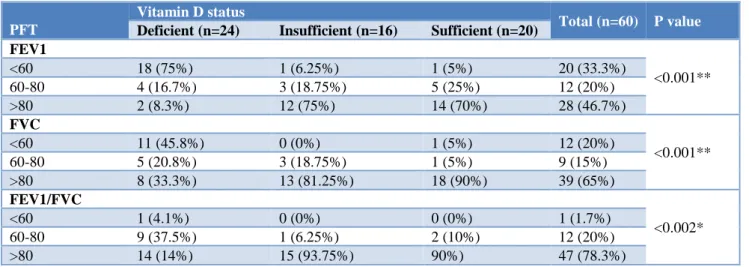
Table 1: Association of pulmonary function tests with vitamin D status.
PFT
Vitamin D status
Total (n=60) P value Deficient (n=24) Insufficient (n=16) Sufficient (n=20)
FEV1
<0.001**
<60 18 (75%) 1 (6.25%) 1 (5%) 20 (33.3%)
60-80 4 (16.7%) 3 (18.75%) 5 (25%) 12 (20%)
>80 2 (8.3%) 12 (75%) 14 (70%) 28 (46.7%)
FVC
<0.001**
<60 11 (45.8%) 0 (0%) 1 (5%) 12 (20%)
60-80 5 (20.8%) 3 (18.75%) 1 (5%) 9 (15%)
>80 8 (33.3%) 13 (81.25%) 18 (90%) 39 (65%)
FEV1/FVC
<0.002*
<60 1 (4.1%) 0 (0%) 0 (0%) 1 (1.7%)
60-80 9 (37.5%) 1 (6.25%) 2 (10%) 12 (20%)
>80 14 (14%) 15 (93.75%) 90%) 47 (78.3%)
Significant correlation was observed between percent predicted FEV1, FVC and FEV1/FVC. Higher levels of percent predicted FEV1, FVC and FEV1/FVC were found in children with sufficient vitamin D levels than insufficient and deficient group (Table 5).
DISCUSSION
As bronchial asthma is still the most common disease of childhood and one of the leading causes of morbidity in children worldwide, the number of studies concerning the association between vitamin D deficiency and asthma and allergies has significantly increased in recent years. Epidemiologic data in most of the reported studies suggest that low vitamin D levels (defined as serum 25-OH vitamin D level <20ng/ml) in children with asthma is associated with more symptoms, exacerbations, decreased lung function, increased medication use and severe disease.7
This study was intended to know the relation between vitamin D status and level of asthma control in known asthmatic children. Level of asthma control was classified based on GINA guidelines.11
In this study 66.6% of patients were vitamin D deficient/insufficient (40% were deficient with vitamin D levels <20 ng/ml and 26.7% were in insufficient range with levels between 20-30 ng/ml) which is similar to prevalence of vitamin D deficiency in general population.12 Prevalence of vitamin D deficiency in a
study done at Thailand by Krobtrakulchai et al is similar to that of the present study (64% were vitamin D deficient/insufficient).13 High prevalence rates of vitamin
D deficiency/insufficiency are reported in otherwise healthy infants, children and adolescents and also from diverse countries around the world including India.14-16
This may be due to behavioural factors, such as sunscreen use, decreased time spent outdoors and lower vitamin D intake in diet.
However, in this study we could not predict vitamin D status using questionnaires about sun exposure or vitamin D enriched food intake. A well-designed questionnaire with a larger sample size will be needed to find the correlation between vitamin D levels and sun exposure/vitamin D enriched food intake.
60 asthmatic children aged between 6-15 years were included in this study. Mean age in years ±SD in this study group is 11.0±2.8. 31 of 60 (51.7%) were males and 29 of 60 (48.3%) were females. This is similar to the study done by Krobtrakulchai, et al.13 Mean±SD vitamin
D level in the study population was 23.38±8.76. There was no significant difference in vitamin D levels in both sexes (Mean±SD vitamin D level in males was 23.68±7.17 and in females was 23.06±10.16), which was in accordance with the study done by Krobtrakulchai et al13
Based on Vitamin D levels, present study population was divided into 3 groups: Vitamin D deficient (vitamin D levels <20ng/ml), Vitamin D insufficient (vitamin D levels between 20-30 ng/ml) and Vitamin D sufficient (vitamin D levels >30ng/ml), similar to the studies done by Chinellato et al, Krobtrakulchai et al and Brehm, et al.17,13,18 Mean±SD vitamin D levels in deficient,
insufficient and sufficient group were 14.38±3.8, 25.2±2.6, 32.53±4.02 respectively. In the present study there was no significant difference in mean age of onset of asthma in deficient, insufficient and sufficient group (Mean age in years ±SD 7.75±3.2, 6.7±2.7, 6.8±2.4 in deficient, insufficient and sufficient groups respectively). But there was significant inverse relation (p=0.01) between duration of symptoms and vitamin D status.
In this study it was noticed that number of hospitalizations/emergency visits per year were higher in vitamin D deficient group than insufficient/sufficient group (p = 0.03, moderately significant), suggesting lesser number/ milder exacerbations and consequently decreased hospitalizations/ emergency visits in those with sufficient vitamin D levels. Higher vitamin D levels are likely associated with decreased risk of severe exacerbations through multiple mechanisms. One mechanism might be through improved response to respiratory tract infections because vitamin D has been shown to induce the production of antimicrobial proteins (AMPs), such as cathelicidin (which has both antimicrobial and antiviral properties) and defensins.19
Induction of AMPs has been shown to occur at the airway epithelium. In addition to the induction of AMPs, vitamin D might modulate the inflammatory response to viral infections. Airway epithelial cells exposed to vitamin D produce less inflammatory cytokines (without adversely affecting viral clearance) than cells not exposed to vitamin D when infected with viruses. These findings suggest that although higher vitamin D levels might not prevent the occurrence of infections, higher levels might allow improved handling of these infections and decreased inflammatory responses, resulting in less severe disease and sequelae of these viral infections. This is supported by our data.
A significant inverse association was observed between vitamin D levels and severity of asthma (p <0.001). 70% of cases with intermittent asthma had sufficient vitamin D levels as compared to 91.6% cases with moderate/severe persistent asthma with vitamin D deficiency. This is in accordance with studies done by Chinellato et al and Gupta, et al (p=0.01).17,20 It was suggested that vitamin D
deficiency or insufficiency due to down regulation of glucocorticoid pathways leads to the need for increased steroid doses and this may itself increase asthma severity.21
In this study significantly higher levels of FEV1 (p <0.01), FVC (p <0.01) and FEV1/FVC (p = 0.02) percent predicted were found in vitamin D Sufficient children as compared to vitamin D insufficient and deficient children. Levels of asthma control in this study were assessed over a period of 4 weeks, and were classified as well controlled, partly controlled and uncontrolled as per GINA guidelines. The proportion of patients with different levels of asthma control were 45% well controlled, 28.3% partly controlled and 26.7% were uncontrolled. Mean±SD vitamin D levels in well controlled, partly controlled and uncontrolled were respectively, 29.08±6.3, 23.24±7.2, 13.9±4.64. Significant (p <0.01) inverse correlation was found between vitamin D levels and level of control of asthma. (75% of children with sufficient levels of vitamin D were associated with good asthma control). These findings are in accordance with that of other studies done by Chinellato, et al(p = 0.011), Gupta, et al (p <0.001), Huria MA et al (p=<0.0001).17,20,23 This indicates that
higher levels of vitamin D correspond to better perception of disease control by the patients and their parents.
CONCLUSION
Vitamin D deficiency is highly prevalent throughout the world including India. Both males and females are equally prone for vitamin D deficiency.
Hypovitaminosis D is frequent in children with asthma. In this study 66.6% of patients were vitamin D deficient/insufficient. This study concludes that sufficient vitamin D levels were associated with better asthma control. Furthermore, low vitamin D levels are associated with more symptoms, exacerbations, decreased lung functions and severe disease.
ACKNOWLEDGEMENTS
Authors would like to place on record their deepest gratitude to Dr. C. R. Banapurmath, President IAP- IYCF chapter 2017-18, Professor and Former Director, Bapuji Child Health Institute and Research Centre for his constant support and guidance. Authors express humble thanks to Dr. A. C. Basavaraj, Professor and Head, Department of Paediatrics, JJM Medical College, Davangere for his encouragement and support in conducting this study
Funding: No funding sources Conflict of interest: None declared
Ethical approval: The study was approved by the Institutional Ethics Committee
REFERENCES
1. Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, et al. National surveillance for asthma: United States, 1980-2004. MMWR Surveill Summ. 2007;56:1-54.
2. Ait-Khaled N, Pearce N, Anderson HR. Global map of the prevalence of symptoms of rhinoconjunctivitis in children: The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three. Allergy. 2009;64:123-48. 3. Eder W, Ege MJ, von Mutius E. The asthma
epidemic. N Engl J Med. 2006;355:2226-35. 4. Saglani S, Bush A. The early-life origins of asthma.
Curr Opin Allergy Clin Immunol. 2007;7:83-90. 5. Litonjua AA, Weiss ST. Is vitamin D deficiency to
blame for the asthma epidemic? J Allergy Clin Immunol. 2007;120:1031-5.
6. Holick MF. Vitamin D deficiency. N Engl J Med. 2007; 357:266-81.
7. Kunisaki KM, Niewoehner DE, Connett JE. COPD Clinical Research Network. Vitamin D levels and risk of acute exacerbations of chronic obstructive pulmonary disease: a prospective cohort study. Am J Respir Crit Care Med. 2012;185(3):286-90. 8. Hansdottir S, Monick MM, Hinde SL, Lovan N,
Look DC, Hunninghake GW. Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense. J Immunol. 2008;181:7090.
9. Hansdottir S, Monick MM, Lovan N, Powers L, Gerke A, Hunninghake GW. Vitamin D decreases respiratory syncytial virus induction of NF-kappa Blinked chemokines and cytokines in airway epithelium while maintaining the antiviral state. J Immunol. 2010;184:965-74
10. Litonjua AA. Childhood asthma may be a consequence of vitamin D deficiency. Curr Opin Allergy Clin Immunol. 2009;9:202-7.
11. GINA. Global initiative for asthma. A pocket guide for Health profesionals. 2015:9-10.
12. Kumar J, Muntner P, Kaskei FJ. Prevalence and association of 25-hydroxyvitamin D deficiency in US children: NHANES 2001-2004. Pediatrics 2009;124(3):e362-70.
13. Krobtrakulchai W, Praikanahok J, Visitsunthorn N, Vichyanond P. The effect of Vitamin D status on pediatric asthma at a university hospital, Thailand. Allergy Asthma Immunol Res. 2013;5(5):289-94. 14. Holick MF. The vitamin D deficiency pandemic and
consequences for nonskeletal health: mechanisms of action. Mol Aspects Med. 2008;29:361-8.
15. Huh SY, Gordon CM. Vitamin D deficiency in children and adolescents: Epidemiology, impact and treatment. Rev Endocr Metab Disord. 2008;9:161-70
16. Marwaha RK, Tandon N, Agrawal N, Puri S, Agrawal R, Singh S, et al. Impact of two regimens of vitamin D supplementation on calcium-vitamin DPTH axis of school girls of Delhi. Indian Pediatr. 2010;47:761-9.
18. Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol. 2010;126(1):52-8.
19. Adorini L, Penna G, Giarratana N. Dendritic cells as key targets for immunomodulation by vitamin D receptor ligands. J Steroid Biochem Mol Biol. 2004;89:437-41.
20. Gupta A, Sjoukes A, Richards D, Banya W, Hawrylowicz C. Relationship between serum Vitamin D, disease severity, and airway remodelling in children with asthma. Am J Respir Crit Care Med. 2011;184(12):1342-9.
21. Searing DA, Zhang Y, Murphy JR. Decreased serum vitamin D levels in children with asthma are
associated with increased corticosteroid use. J Allergy Clin Immunol.2010;125(5):995-1000. 22. Burns JS, Dockery DW, Neas LM. Low dietary
nutrient intake and respiratory health in adolescents. Chest. 2007;132:238-45.
23. Aldubi HM, Alissa EM, Kamfar HZ, Gaber O, Marzouki ZM. Bronchial asthma and hypovitaminosis D in Saudi children. Asia Pac Allergy. 2015;5:103-13.