Original Article
Association of TNF-α with ventricular
arrhythmias during early acute myocardial infraction
Jin Wang, Haizhou Li, Yumei Guo, Zhi Zhao, Lin Zhang, Dongwei Yang
Department of Cardiovascular Internal Medicine, Zhengzhou Central Hospital Affiliated to Zhengzhou University, Zhengzhou, Henan, China
Received December 15, 2015; Accepted February 25, 2016; Epub June 1, 2016; Published June 15, 2016
Abstract: To explore the effects of tumor necrosis factor-α (TNF-α) on ventricular arrhythmias (VAs) in rats with acute myocardial infarction (AMI). A rat model of AMI was created by ligation of the left anterior descending (LAD) coro-nary artery. ECG and spontaneous VAs were observed during the whole experiment. Monophasic action potentials (MAP) among ischemic zone, border zone and non-ischemia zone was observed and Monophasic action potential repolarization dispersion (MAPDd) were calculated. Linear correlation analysis was used to assess the relationship between TNF-α protein expression and MAPDd of the border zone. The incidence of VAs in AMI group was markedly increased at each time interval after ligation compared with Etanercept group (P<0.05). The MAPDd from the border zone of the ischemic myocardium was significantly increased at each time point after ligation compared with the ischemic zone and non-ischemic zone of the epicardium (P<0.05). Moreover, the MAPDd from the border zone of ischemic myocardium was significantly increased in the AMI group compared with the Etanercept group (P<0.05). The temporal changes of the MAPDd in the border zone coincided with the incidence of VAs in vivo during early AMI. The levels of TNF-α protein expression in the AMI group began to increase at 10 min and reached a peak at 20 min after ligation; then, they decreased. The correlation coefficient of TNF-α protein expression and MAPDd of the border zone was 0.96 (P<0.01) and showed a positive linear correlation. TNF-α could increase the MAPDd in the border zone, and promote the onset of VAs, while Etanercept could decrease the MAPDd in the border zone and lessen the incidence of VAs in rats with AMI.
Keywords: Acute myocardial infarction, ventricular arrhythmias, monophasic action potential
Introduction
Coronary heart disease (CHD) is a common car-diovascular disease. Seventy five to eighty per-cent of the world of sudden cardiac death (SCD) is the direct cause of coronary heart disease, especially the occurrence of ventricular arrhyth-mia after myocardial infarction [1]. Acute Myocardial Infarction (AMI) is one of the most common fatal cardiovascular diseases. How- ever, ventricular arrhythmia is the most serious complications of AMI [2]. More than one million people died from myocardial infarction disease every year [3]. Ventricular arrhythmia after myo-cardial infarction is one of the most common causes of SCD [4]. Therefore, it is of great sci-entific significance to study the mechanism of ventricular arrhythmia after acute myocardial infarction.
[10]. In transgenic mice, overexpression of the inflammatory cytokine TNF-α (TNF-α mice) in the heart causes mice to develop a progressive heart failure syndrome characterized by ven-tricular dilatation, decreased ejection fraction, and atrial and ventricular arrhythmias on ambu-latory telemetry monitoring [11].
AMI is currently thought to be an inflammation process [12]. TNF-α may be found augmented in the myocardium of AMI [13] and serves as one of the cytokine-mediated attractants for neutrophil migration into the ischemic region and enhances the inflammatory reaction relat-ed to progressive tissue destruction [14]. Inflammatory reaction caused by TNF-α stimu-lates paraplasm and hypertrophy of the myo-cardium and plays important roles in recovery and ventricular remodeling after AMI [15-17]. When AMI occurs, in accordance with different degrees of ischemia, myocardium could be divided into the ischemic zone, the nonisch-emic zone, and the border zone [18]. How- ever, whether TNF-α plays an important role in the occurrence of VAs remains unknown. It is reported that sudden cardiac death (SCD) causes approximately 3 million fatalities in the U.S. Annually Ventricular tachyarrhythmia aris-ing from myocardial ischemia and infarction is a leading cause [19, 20]. Recently, Shimoda et al [21] found that, in AMI patients with malig-nant ventricular arrhythmia, spontaneous and stimulated levels of TNF-α were higher than controls. However, the relationship between TNF-α and ventricular arrhythmias arising from AMI was still unknown. Therefore, this study detected expression of TNF-α in different regions of ischemic myocardium, recorded the monophasic action potentials (MAPs) and occurrence of VAs, and then explored the effect of TNF-α expression on the occurrence of VFs and the potential mechanisms.
Materials and methods
Animal care
All experimental procedures were approved by the Institutional Authority for Laboratory Animal Care and conformed to the Guide for the Care and Use of Laboratory Animals published by the National Institutes of Health (NIH publication No. 85e23, revised 1985).
AMI rat model
Myocardial infarction (MI) was induced in 8-week-old male Sprague-Dawley rats weighing
250-300 g through ligation of the left anter- ior descending coronary artery as previously described [22]. Briefly, All male SD rats were anesthetized with pentobarbital sodium (30∼ 35 mL/kg) by intraperitoneal injection. Under controlled ventilation, a thoracotomy through a left parasternal 3, 4 intercostal spaces was performed, the pericardium was incised, and the anterior wall of the left ventricle was exposed. Left anterior descending coronary artery (LAD) proximal end was ligated with 6-0 line at the junction of the pulmonary cones and the left atrial appendage, which could induce extensive infarction of left ventricular anterior wall. When the ventricular anterior wall turned to be pale or cyanosed and ECG showed ST-segment elevated, myocardial infarction model succeeded.
Experimental groups
Ninety SD rats were randomized into AMI group (n = 30), sham operation group (n = 30), and Etanercept group (n = 30). Anterior wall myocar-dial infarction was produced in AMI group by ligating the left anterior descending coronary artery (LAD); there was no ligation but opera-tion in sham-operaopera-tion group. Etanercept group was treated with recombinant human tumor necrosis factor receptor: Fc fusion protein (rhT-NFR: Fc) (10 mg/kg), a TNF-α antagonist, 24 hours before LAD ligation. ECG and spontane-ous VAs were observed during the whole experi-ment. Monophasic action potentials (MAPs) among the ischemic zone, the border zone, and the non-ischemia zone were observed at base-line, 10 min, 20 min, 30 min, 60 min, 3 h, 6 h, and 12 h after ligation, and monophasic action potential duration disperses (MAPDds) were calculated, while VFs were induced by S1S2 programmed electrical stimulation and re- corded.
Recording of MAP and calculation of mono-phasic action potential repolarization disper-sion (MAPDd)
after ligation. After measuring MAPD90 of five points of each zone.
MAPDd MAPD90 _X 590
_ x
MAPD
1 2
5 2
=^ - h +f+^ - h
Western blotting of TNF-α protein
Total cell plasma protein of myocardium of rats in AMI group, sham operation group, and Etaner- cept group, respectively, were extracted by 50
[image:3.612.93.363.73.518.2]microwave for 10 min, incubated with BSA at 37°C for 40 min, with a 1:200 dilution of goat anti-rat TNF-α/TNFSF1A antibody (R&D Sys- tems, USA) TNF-α antibody at 4°C overnight, with a 1:100 dilution of biotinylated rabbit anti-goat secondary antibody (Boshide, China) at 37°C for 40 min, with avidin-biotin-horseradish peroxidase complexes at 37°C for 60 min, then colored with diaminobenzidine, stained with
Figure 1. Ventricular Arrhythmias in AMI Rat Models. A. Recording of PVCs in ECG in AMI Rat Models. B. Recording of VT/VF in ECG in AMI Rat Models. C. The incidence of PVCs at different time intervals of post-ligation. D. The incidence of VT/VF at different time intervals of post-ligation. #versus sham group; *versus AMI group. #P<0.01, *P<0.01. 3.2 The MAPDds in the Border Zone before and after ligation.
mmol/L Tris eHCl (pH 7.4). Samples containing 30 mg of total protein were electropho-resed on 15% polyacrylamide gels (Bio-Rad, Hercules, CA) for 1 h (4C, constant current for 80 mA). Separated pro-teins were electrophoretically transferred onto a nitrocellu-lose membrane (Invitrogen, Carlsbad, CA). Negative (no protein added) controls were used at the same time. Transfer time was 28 min. Blocking with 5% nonfat milk was done for 2 h at 37°C. TNF-α protein expression was detected by a 1:500 dilution of goat anti-rat TNF-α poly-clonal antibody (Santa Cruz Biotechnology, Santa Cruz, CA) as the first antibody, respectively. A 1:5000 dilu-tion of horseradish peroxi-dase-conjugated rabbit anti-goat (Santa Cruz Biotech- nology) was used as the sec-ond antibody and then devel-oped with the enhanced che-miluminescence Western blo- tting detection system (Pier- ce Biotechnology, Rockford, IL).
Immunohistochemistry for TNF-α
haematoxylin, and, finally, observed. Selecting five sights at each slice, TNF-α expression in every section was measured and analyzed by HMIAS Series Color Medical Image Analyze System (Champion Image Ltd., China).
both in the induced and raw state. The occur-rence of VAs was showed in Figure 1.
[image:4.612.92.372.69.553.2]To explore the relation between MAPDd of the border zone (BZ) and the incidence of VAs at
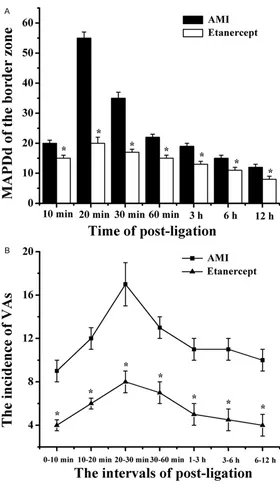
Figure 2. The MAPDd of the border zone (BZ) and the incidence of VAs at different time point. A. The MAPDd of the border zone at different time point. B. The incidence of VAs at different time point. Compared with AMI group, the MAPDd of the border zone significantly decreases at different point in early AMI in Etanercept group. The change of MAPDd of the border zone with time is in accordance with change of the incidence of VAs in early AMI. n=10, *versus AMI group, *P<0.05.
Statistical analysis
All values are expressed as mean ± SD. Results were ana-lyzed by using Student’s t-te- st and analysis of variance (ANOVA) for multiple compari-sons followed by a two-si- ded Dunnett’s test or Stud- ent Newman-Keuls test when appropriate. Linear correla-tion analysis was used for the relationship between TNF-α and ventricular arrhythmias. Statistical significance was assumed at P<0.05.
Results
Ventricular arrhythmias in AMI rat models
Figure 3. The expression of TNF-α protein in different group and the correla-tion between TNF-α expression and MAPDd of the border zone. A. The ex-pression of TNF-α protein at different time point of border zone in AMI group. B. The expression of TNF-α protein at different time point of border zone in Etanercept group. C. The expression of TNF-α protein in different groups. Western blot showed different expressions of TNF-α at different time among
groups. Compared with sham group, the expression of TNF-α protein significantly increases at different time point in both AMI group and Etanercept group. Compared with AMI group, the expression of TNF-α protein sig-nificantly decreases at different time point in Etanercept group. #versus sham group; *versus AMI group. #P<0.05, *P<0.05. D. The correlation between TNF-α expression and MAPDds of the border zone. The positive corre-lation coefficient between TNF-α expression and MAPDds of the border zone is 0.9837 (P<0.01) in AMI group.
different time point, MAP was recorded in the ischemic zone, the border zone (BZ), and the non-ischemia zone with electrode. The MAPDds in the border zone significant-ly increased after LAD liga-tion, reached a peak time at 20 min, and recovered gradu-ally then. At the same time point, MAPDds of AMI group were significantly greater than Etanercept group, P<0.05 (Figure 2A). The time window of the changes of MAPDds in the border zone was in accor-dance with the occurrence of VAs in acute ischemic myocar-dium. This shows that the MAPDd of the border zone promotes the occurrence of Vas (Figure 2).
TNF-α protein expression by Western blot
signifi-cantly decreases at different time point in Etanercept group (Figure 3C). Linear correla-tion analysis of the relacorrela-tionships between detected expression of TNF-α and the MAPDds in the border zone was performed both in AMI group and Etanercept group. The correlation coefficient of AMI group was 0.9837, <0.01, and showed positive linear correlation (Figure 3D).
TNF-α expression detected by immunohisto-chemistry
TNF-α in acute ischemic myocardium began to increase at 10 min after infarction, reached a
climax at 20-30 min, and recovered gradually then. At the same time point, TNF-α in the isch-emic zone was higher than the others, and the second was in the border zone. Compared to the AMI group, TNF-α detected by immunohis-tochemistry in Etanercept group was signifi-cantly less than the AMI group (P<0.05), and the expression of TNF-α in the sham group was extremely low (Figure 4B).
Discussion
It is known that TNF-α is an acute phase reac-tive protein and a basic media of
[image:6.612.92.524.79.540.2]cal regulation. It serves as a critical role in the inflammatory reaction. AMI is thought to be an inflammation process [12]. Moreover, TNF-α participates in cardiac remodeling and in final rehabilitation after AMI [15-17, 23]. Ventricular arrhythmia followed by AMI is one of the most severe complications of AMI. However, the rela-tionship between TNF-α and ventricular arrhyth-mias arising from AMI was unknown. Therefore, we performed this study. In this study, we dupli-cated AMI rat models. Ventricular arrhythmias happened in the early period after ligation in AMI rats, including PVC, VT. Meanwhile, protein level of TNF-α began to increase at 10 min after ligation and reached a peak time at 20-30 min, then decreased (Figures 3 and 4). The time-dependent manner coincided with the previous report [24]. Protein expression levels of TNF-α were higher in AMI group than in Etanercept group (P<0.05). In AMI group, the occurrence time of ventricular arrhythmias coincided with the secretion of TNF-α. These results indicated that the considerable secretion of TNFa may be related to ventricular arrhythmias arising from AMI. Immunohistochemical staining showed TNF-α expression predominated in surviving cardiomyocytes of the infarct zone and cardio-myocytes in non-infarct zone. Thus, we could conclude that TNF-α may autocrine from car-diocyte in the rats of AMI.
The occurrence of VAs after ligation happened most frequently in 10 to 30 min and gradually decreased in rat AMI model, which coincided with the previous report [25]. After peak time, the decreasing occurrence of VAs may be relat-ed to coronary collateral circulation formation, water and salt electrolyte disorder, energy metabolism. But the mechanism of the occur-rence of VAs after AMI is not clear yet [26]. Compared to the AMI group, the occurrence of Vas (PVCs and VT/VF) in Etanercept group sig-nificantly decreased in every time point (Figure 1C and 1D). These results provide direct evi-dence that TNF-α plays an important role in the occurrence of VAs in early AMI. Yalta et al [27] also found that the block of TNF-α during AMI could reduce the occurrence of arrhythmias, which coincided with our study.
Monophasic action potential (MAP) is the aver-age extracellular potential of contacted local myocardial cells recorded by electrode. During AMI, myocardial tissue develops into three dis-tinct zones, which is the ischemic zone, the
bor-der zone, and the non-ischemia zone. Zaitsev considered that the ischemic zone and the bor-der zone play reverse role in the occurrence of ventricular arrhythmias. The border zone was regarded as the principal factor in the develop-ing of ventricular arrhythmias while the isch-emic zone could lessen the occurrence of ven-tricular arrhythmias by stabilizing the wave of depolarization [27]. We found that the MAPDds in the border zone significantly increased after LAD ligation, reached climax at 20 min, and recovered gradually then. The time window of the TNF-α expression was similar to that of MAPDds in the border zone, which showed that MAPDds in the border zone were related to the expression of TNF-α. With rhTNFR: Fc, MAPDds in the border zone of Etanercept group still increased, but the extent of increase sharply reduced. Meanwhile, the appearance of VAs significantly decreased as well, which suggest-ed that TNF-α promotes the occurrence of acute ischemic VAs by enlarging MAPDds in the border zone, and rhTNFR: Fc decreases the occurrence of VAs by inhibiting the biological effects of TNF-α. The time window of the chang-es of MAPDds in the border zone was in accor-dance with the occurrence of VAs in acute isch-emic myocardium. This shows that the MAPDd of the border zone promotes the occurrence of Vas (Figure 2).
Our findings first suggested that TNF-α pro-motes acute ischemic VAs through enlarging MAPDds of the border zone. The underlying mechanisms need to be further studied. Besides, whether there are some other path-ways in the process that TNF-α causes VAs remains unknown.
The expression of TNF-α increased greatly after acute myocardial infarction. TNF-α could enlarge the MADds in the border zone and pro-mote the onset of VAs while rhTNFR: Fc could diminish the MADds in the border zone and lessen the onset of VAs in AMI rats. Our results demonstrated that TNF-α expressed by isch-emic myocardium may play an important role in the occurrence of VAs in AMI rats.
Acknowledgements
Disclosure of conflict of interest
None.
Address correspondence to: Dr. Yuma Goo, Depart- ment of Cardiovascular Internal Medicine, Zheng- zhou Central Hospital Affiliated to Zhengzhou Uni- versity, 195 Tonga Road, Zhengzhou 450007, He- nan, China. E-mail: yesorno_yy@tom.com
References
[1] Subbiah R, Gula LJ, Klein GJ, Skanes AC, White J, Yee R, Krahn AD. Workup of the cardiac ar-rest survivor: for the symposium on sudden cardiac death for progress in cardiovascular diseases. Prog Cardiovasc Dis 2008; 51: 195-203.
[2] Franz MR. Method and theory of monophasic action potential recording. Prog Cardiovasc Dis 1991; 33: 347-368.
[3] Nattel S, Maguy A, Le Bouter S, Yeh YH. Arrhythmogenic ion-channel remodeling in the heart: heart failure, myocardial infarction, and atrial fibrillation. Physiol Rev 2007; 87: 425-456.
[4] Huikuri HV, Castellanos A, Myerburg RJ. Medical progress: Sudden death due to cardi-ac arrhythmias. New England Journal of Medicine 2001; 345: 1473-1482.
[5] Sun M, Dawood F, Wen WH, Chen M, Dixon I, Kirshenbaum LA, Liu PP. Excessive tumor ne-crosis factor activation after infarction contrib-utes to susceptibility of myocardial rupture and left ventricular dysfunction. Circulation 2004; 110: 3221-3228.
[6] Valgimigli M, Ceconi C, Malagutti P, et al. Tumor necrosis factor-αlpha receptor 1 is a major pre-dictor of mortality and new-onset heart failure in patients with acute myocardial infarction: the Cytokine-Activation and Long-Term Pro- gnosis in Myocardial Infarction (C-ALPHA) study. Circulation 2005; 111: 863-870. [7] Hirono S, Islam M O, Nakazawa M, Yoshida Y,
Kodama M, Shibata A, Izumi T, Imai S. Expression of inducible nitric oxide synthase in rat experimental autoimmune myocarditis with special reference to changes in cardiac hemo-dynamics. Circ Res 1997; 80: 11-20.
[8] Mann DL, McMurray JJ, Packer M, Swedberg K, Borer JS, Colucci WS, Djian J, Drexler H, Feldman A, Kober L, Krum H, Liu P, Nieminen M, Tavazzi L, van Veldhuisen DJ, Waldenstrom A, Warren M, Westheim A, Zannad F, Fleming T. Targeted anticytokine therapy in patients with chronic heart failure: results of the Randomized Etanercept Worldwide Evaluation (RENEWAL). Circulation 2004; 109: 1594-1602.
[9] Saba S,Janczewski AM, Baker LC, Shusterman V, Gursoy EC, Feldman AM, Salama G, McTiernan CF, London B. Atrial contractile dys-function, fibrosis, and arrhythmias in a mouse model of cardiomyopathy secondary to cardi-ac-specific overexpression of tumor necrosis factor-{alpha}. Am J Physiol Heart Circ Physiol 2005; 289: H1456-H1467.
[10] Wang J, Wang H, Zhang Y, Gao H, Nattel S, Wang Z. Impairment of HERG K(+) channel function by tumor necrosis factor-αlpha: role of reactive oxygen species as a mediator. J Biol Chem 2004; 279: 13289-13292.
[11] London B, Baker LC, Lee JS, Shusterman V, Choi BR, Kubota T, McTiernan CF, Feldman AM, Salama G. Calcium-dependent arrhythmias in transgenic mice with heart failure. Am J Physiol Heart Circ Physiol 2003; 284: H431-H441. [12] Libby P. Inflammation in atherosclerosis. Na-
ture 2002; 420: 868-874.
[13] Irwin MW, Mak S, Mann DL, Qu R, Penninger JM, Yan A, Dawood F, Wen WH, Shou Z, Liu P. Tissue expression and immunolocalization of tumor necrosis factor-αlpha in postinfarction dysfunctional myocardium. Circulation 1999; 99: 1492-1498.
[14] Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarc-tion. Cardiovasc Res 2002; 53: 31-47. [15] Bozkurt B, Kribbs SB, Clubb FJ Jr, Michael LH,
Didenko VV, Hornsby PJ, Seta Y, Oral H, Spinale FG, Mann DL. Pathophysiologically relevant concentrations of tumor necrosis factor-αlpha promote progressive left ventricular dysfunc-tion and remodeling in rats. Circuladysfunc-tion 1998; 97: 1382-1391.
[16] Berthonneche C, Sulpice T, Boucher F, Gouraud L, de Leiris J, O’Connor SE, Herbert JM, Janiak P. New insights into the pathological role of TNF-alpha in early cardiac dysfunction and subsequent heart failure after infarction in rats. Am J Physiol Heart Circ Physiol 2004; 287: H340-H350.
[17] Li YY, Mctiernan CF, Feldman AM. Interplay of matrix metalloproteinases, tissue inhibitors of metalloproteinases and their regulators in car-diac matrix remodeling. Cardiovasc Res 2000; 46: 214-224.
[18] Pogwizd SM, Corr PB. Mechanism underlying ventricular tachycardia and fibrillation in the ischemic heart: relation to nonlinear dynam-ics. Ann N Y Acad Sci 1990; 591: 278-300. [19] Myerburg RJ, Mitrani R, Interian A Jr, Cas-
tellanos A. Interpretation of outcomes of anti-arrhythmic clinical trials: design features and population impact. Circulation 1998; 97: 1514-1521.
[21] Shimoda Y, Satoh M, Nakamura M, Akatsu T, Hiramori K. Activated tumour necrosis factor-αlpha shedding process is associated with in-hospital complication in patients with acute myocardial infarction. Clin Sci (Lond) 2005; 108: 339-347.
[22] Nguyen QT, Cernacek P, Calderoni A, Stewart DJ, Picard P, Sirois P, White M, Rouleau JL. Endothelin A receptor blockade causes ad-verse left ventricular remodeling but improves pulmonary artery pressure after infarction in the rat. Circulation 1998; 98: 2323-2330. [23] Spinale FG. Bioactive peptide signaling within
the myocardial interstitium and the matrix me-talloproteinases. Circ Res 2002; 91: 1082-1084.
[24] Herskowitz A, Choi S, Ansari AA, Wesselingh S. Cytokine mRNA expression in postischemic/ reperfused myocardium. Am J Pathol 1995; 146: 419-428.
[25] Curtis MJ. Characterisation, utilisation and clinical relevance of isolated perfused heart models of ischaemia-induced ventricular fibril-lation. Cardiovasc Res 1998; 39: 194-215. [26] Yalta K, Sivri N, Geyik B, Yetkin E. Tumour
ne-crosis factor-αlpha antagonism: a potential therapeutic target for prevention of arrhythmo-genesis in the setting of acute myocardial in-farction?. Heart 2014; 100: 263.