R E S E A R C H A R T I C L E
Open Access
Auricular acupuncture with seed or pellet
attachments for primary insomnia: a systematic
review and meta-analysis
Ying Lan
1, Xi Wu
1, Hui-Juan Tan
1, Nan Wu
1, Jing-Jing Xing
2, Fu-Sheng Wu
1, Lei-Xiao Zhang
3and Fan-Rong Liang
1*Abstract
Background:Primary insomnia is a common health issue in the modern world. We conducted a systematic review of the auricular therapy, aiming to evaluate whether there are advantages of auricular acupuncture with seed or pellet attachments for the treatment of primary insomnia.
Methods:A search of relevant literatures was performed on major medical databases, including Medline, Embase, CENTRAL, CBM, CNKI, VIP, Wanfang Data and so on. Risk of bias evaluation, meta-analysis, sensitivity analysis and evidence rating of all extracted information were conducted also.
Results:A total of 1381 records were identified, with 15 studies deemed eligible for the present review. Meta-analyses were conducted in two comparisons separately: participants received auricular acupuncture were more likely to make an improvement in clinical effective rate (RR = 1.40, 95% CI 1.07 to 1.83), sleep duration (MD = 56.46, 95% CI 45.61 to 67.31), sleep efficiency(MD = 12.86, 95% CI 9.67 to 16.06), global score on PSQI (MD = -3.41, 95% CI -3.93 to -2.89), number of awakenings( MD = -3.27, 95% CI -6.30 to -0.25) and sleep onset latency(MD = -10.35, 95% CI -14.37 to -6.33) when compared to sham auricular acupuncture or placebo; while in auricular acupuncture VS medications comparison, a better effective rate (RR = 1.24, 95% CI 1.15 to 1.34), better sleep efficiency(MD = 21.44, 95% CI 16.30 to 26.58), lower PSQI score (MD = -3.62, 95% CI -4.59 to -2.65) and less adverse effect (RR = 0.11, 95% CI 0.04 to 0.26) can be seen also in auricular acupuncture group. Although these results suggested benefits of auricular acupuncture, the overall quality of evidence rated by the GRADE system was low.
Conclusion:Statistical analyses of the outcomes revealed a positive effect of auricular acupuncture for primary insomnia. Nonetheless, considering the poor methodological quality, insufficient sample size and possible publication bias, current evidence is not yet adequate to provide a strong support for the use of auricular acupuncture in the treatment of primary insomnia. More strictly designed clinical studies will be needed to obtain a more explicit conclusion.
Keywords:Auricular acupuncture, Insomnia, Systematic Review, GRADE
Background
Primary insomnia is a common health issue caused by multiple environmental and psychological factors. Patients suffering from insomnia may have difficulty initiating or maintaining sleep, or experience nonrestorative sleep together with functional impairment during the day-time without a clear medical or psychiatric cause [1,2].
Approximately 10-20% of the population worldwide is suffering from poor-quality sleep, among which 50% in-volve a chronic course over a month [3]. Specifically, sleep disorder persisting one month is an acute type, between one to three months is a sub-chronic type, be-yond three months could be defined as persistent in-somnia [4]. The incidence of inin-somnia increases with age and is more likely to affect women than men [5,6]. In addition, it is frequently co-morbid with growing risk of headache [7], anxiety and depression [8,9], hypertension * Correspondence:acuresearch@126.com
1Acupuncture and Tuina School/Third Teaching Hospital, Chengdu University
of Traditional Chinese Medicine, No.37, Shierqiao Road, Jin Niu District, Chengdu, Sichuan 610075, China
Full list of author information is available at the end of the article
© 2015 Lan et al.; licensee BioMed Central. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
[10,11], cardio-cerebrovascular diseases [12,13], and even suicidal thoughts or behaviours [14,15].
Current understanding of the mechanism of insomnia typically involves arousal of the central and autonomic ner-vous systems [16]. For example, sympathetic hyperarousal has been detected in insomniacs, as evidenced by increased heart rate, heart rate variability, metabolic activation, and activation of the sympathetic nervous system during sleep [17-19]. Neuroimaging studies have also revealed changes in brain activity associated with the frontal cortex, hippo-campus and anterior cingulate cortex [20,21].
There has been an adequate number of clinical studies supporting the use of cognitive behavioural therapy (CBT) and hypnotics for insomnia [4,22]. However, not all pa-tients respond well to these treatments: experiencing adverse effects from or dependency on hypnotic would all potentially diminish the impact of treatments. Besides, information regarding the long-term efficiency of hypnotic drugs is currently unavailable [23]. Although CBT has been better accepted by insomnia patients, barriers such as cost of time and limited number of trained practitioners still exist in the implementation of CBT [4,24]. Consequently, complementary and alternative medicine (CAM) has become an option that insomnia sufferers often turned to [25,26].
In ancient China, the medical classic Yellow Emperor’s Canon of Medicine first described the complicated link between ears and internal organs, and indicated that any physiological or pathological changes inside the body may reflect on the auricles. In the 1950s, Dr. Paul Nogier of France developed and refined the modern theory of auricular acupuncture, which was based on the concept of an inverted fetus map on the external ear [27], sug-gesting a reflex system useful for the diagnosis and treat-ment of diseases [28]. Clinically pellet attachtreat-ments are utilized on a large scale to provide perfect stimuli to the ears without piercing the skin. Pellets come in different materials, usually in magnetic pearls and plant seeds.
To date, many studies on auricular acupuncture for insomnia have been published worldwide. However, in-clusion of low quality of evidence and inconsistency of outcomes of the studies present challenges in drawing a firm conclusion on the benefit of this therapy [29-31]. It is therefore worthwhile to conduct a systematic review with a more rigorous inclusion criteria and evidence rating system, aiming to evaluate the advantages of auricular acupuncture with seed or pellet attachments in the treat-ment of primary insomnia in a more explicit manner.
Methods
Database
The following databases were searched: Medline (1946 to November 2013), Embase (1946 to November 2013), PsycINFO(1950 to November 2013), Cochrane Central
Register of Controlled Trials (CENTRAL, November 2013), Cochrane Methodology Register (CMR, 3rd Quarter 2013), Cochrane Database of Systematic Reviews (Cochrane DSR, 2005 to November 2013), ACP Journal Club (1991 to November 2013), Database of Abstract of Reviews of Effects (DARE, 3rd Quarter 2013), ProQuest Dissertations and Theses (PQDT, 1997 to 2013), International Clinical Trial Registry Platform (ICTRP), Centre for Clinical Trials Clinical Trials Registry (CCTCTR), and Chinese Biomedical Database (CBM, 1978 to September 2013), China National Knowledge Internet (CNKI, 1915 to September 2013), VIP Database (1989 to September 2013), Wanfang Data and Wanfang Dissertation Database (1989 to June 2013). A monthly e-mail alert was also set up at the National Center for Biotechnology Information (NCBI) from the U.S. National Library of Medicine (NLM), to obtain up-dates of new publications.
Search strategy
1. auricular acupuncture, ear acupuncture or acupuncture ear in full text;
2. auricular therapy, auriculotherapy, auricular needle, auricular acupressure, otopoint$, otoneedle, auriculoacupuncture$ or otopuncture$ in title and abstract;
3. 1 or 2
4. sleep or insomnia in full text;
5. sleep$, insomnia$ ,wakeful$ , somnambul$ or somnipathy$ in title and abstract;
6. 4 or 5 7. 3 and 6
(Additional file 1-Search Strategy) was supple-mented by hand searching the reference lists from iden-tified reviews and original articles in the full text.
Inclusion criteria
1. Design: randomized controlled trials only.
2. Participants: age between 18 ~ 80 with dissatisfaction
about sleep quality of longer than one month’s
duration [32-34].
3. Intervention: plant seeds, metal pellets, or magnets attached on the auricles was suppose to be the single intervention in treatment groups; while sham auricular acupuncture, placebo, no treatment, or drug therapy could be adopted in the control arms. 4. Primary outcome
Effective rate, defined as the proportion of
effectiveness and ought to be reported by participants themselves.
5. Secondary outcomes
Sleep parameters, measured by either subjective
or objective approaches, e.g., sleep diary, actigraphy, electroencephalogram (EEG) or polysomnogram (PSG);
Sleep efficiency, the ratio of total sleep time to
time in bed, could be derived from either subjective or objective ways as well;
Scales or index for sleep quality evaluation, e.g.,
the Pittsburgh Sleep Quality Index(PSQI), Insomnia Severity Index (ISI), Athens Insomnia Scale (ASI) et al.;
Adverse effect, reported in the articles or
measured by validated scales, e.g., Health Survey Questionnaire, Treatment Emergent Symptom Scale (TESS) et al.
6. Language restriction: English and Chinese records only.
Exclusion criteria
Studies that compared different auricular point prescrip-tions or stimulaprescrip-tions in parallel groups were excluded. Studies without mention about randomization were ex-cluded. Redundant publications were exex-cluded.
Data collection and analysis
Two review authors were independently responsible for article screening and data extraction; the third one veri-fied all information. Disagreements were resolved by con-sensus. The data extraction form was designed previously meeting the Cochrane standard [35]. The authors attempted to contact the original authors of all included articles for further information by email or telephone.
The formulae fromCochrane Handbook for Systematic Reviews of Interventions (Handbook) Chapter 7.7.3.8 were adopted to combine data from two subgroups into one, if more than two parallel groups appeared.
Assessment of risk bias was in accordance with Hand-book, in which a domain-based evaluation method was highly recommended. We designated the following seven domains for each study: random sequence generation, allo-cation concealment [36], blinding personnel and partici-pants, blinding assessor, incomplete data outcome, selective reporting, and other bias.
Summary statistics
We chose risk radio (RR) for dichotomous data and mean difference (MD) for continuous data, with 95% confidence intervals (CI) in the meta-analysis. For heterogeneity evaluation, we employed the Q (χ2
) test and I2statistics. Fixed effect model was used to calculate summary sta-tistics in the absence of substantial heterogeneity (I2<
40%). Conversely, random effect model was chosen when I2> 40%. All meta-analyses results were presented accord-ing to different control methods separately. If possible, we planned to conduct subgroup analyses or sensitivity ana-lyses for different diagnostic criteria, age groups, course of disease to assess robustness of all the outcomes.
We planned to generate funnel plots for publication bias assessing when more than ten studies reported the same outcome and use the GRADE system for evidence rating [37]. Quality of evidence for each outcome was ranked at one of four levels, namely high, moderate, low or very low level based on five downgrading factors [38-42] and three upgrading factors [43].
Review Manager 5.2.5 was utilized for statistical analysis, GRADEprofiler 3.6 for evidence profile making. We pre-sented this review under the guidance of Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [44,45].
Results
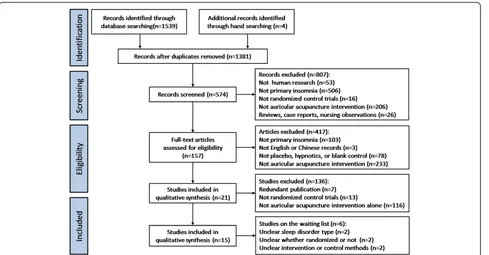
Finally, 15 out of 1381 records were identified. They were performed in mainland China [46-56], Hong Kong [57], Taiwan [58,59], and the US [60], from 1993 to 2013 (Figure 1).
All together 1429 participants were included, aged from18 to 78, 510 male, with insomnia duration from one month to more than ten years. Of these participants, 737 received auricular acupuncture and 664 received control method. Sample sizes ranged from 21 to 300, yet calcula-tion methods weren’t revealed in any of these articles.
Diagnosis of insomnia was made using the following criteria: International Classification of Disease, 10th Version(ICD-10) [60], Chinese Classification of Mental Disorders(CCMD) [46-49,51,52,55,59], Clinical Research Guidelines of New Chinese Herbal Medicine [55,56,59], Chinese Medicine Clinical Syndrome Diagnostic Criteria [54,59], sleep efficiency [55,57-60], Pittsburgh Sleep Quality Index (PSQI) [47,48,50-52,58] and self-report of enduring poor sleep [53].
In the treatment groups, seven studies [46-48,51-53,59] picked Semen Vaccariae for auricular attachment, six [49,50,54,56,58,60] chose magnetic pearls, one [57] study used seeds in one group and magnetic pearls in a second group, and only one study [55] did not report the type of material for attachment. While in the control groups, two studies [48,52] chose sham auris-points method, two used [50,59] pseudo plasters, three studies [57,58,60] treated participants with no pressure or additional force on the pellets or seeds; four utilized [49,51,55,56] estazolam, and four adopted [46,47,53,54] diazepam control. Eight studies [46-48,51,54,57,58,60] took a standard points protocol and the rest seven took individual prescriptions according to syndrome differentiation instead.
Six studies [46,47,49,55,56,59] assessed effects with Guiding Principle of Clinical Study on New Drug of Traditional Chinese Medicine, one study [54] adopted Criteria of Diagnosis and Therapeutic Effect of Interna1 Diseases and Syndromes in Traditional Chinese medicine, six studies [47,48,50-52,59] took the change value of sleep quality assessment scale, and only one [53] took self-made standard. Four studies [49,53,55,56] reported adverse events and two [57,60] reported follow up duration.
Risk of bias
Of the fifteen included studies, six described the details of random sequence generation by computer software [50,52,60] or random number table [48,56,58], and merely one [60] conducted proper allocation concealment. Seven studies [48,50,52,57-60] used sham auricular acupunc-ture or placebo control to blind the participants. Three [48,57,60] out of fifteen studies reported drop-outs and two [57,60] with reasons, and one [48] carried out the intention-to-treat analysis. In addition, six studies [46,47,53,54,58,59] declared no drop-outs in their pro-gram. In selective reporting, two studies [51,59] failed to report all parameters from PSQI scale, while three studies [50,54,57] lacked between-group baseline com-parison (Table 1).
Effect estimates
According to various control methods tested in the tri-als, we conducted meta-analyses in two comparisons re-spectively: auricular acupuncture VS sham or placebo
method, andauricular acupuncture VS medications. Since outcome measurements varied in studies, effect estimates on outcome measurements were different, and then not all fifteen studies appeared in each meta-analyses.
Effective rate
This is a dichotomous outcome and a subjective assess-ment of overall effectiveness, defined as the proportion of participants who had improved obviously in sleep quality.
Auricular acupuncture VS sham or placebo method One study [59] reported that the auricular acupuncture group had better effective rate compared to the sham acupuncture (RR = 1.40, 95% CI 1.07 to 1.83, P = 0.01). (Figure 2A) But this study did not have sufficient power to prove the superiority of auricular acupuncture over sham or placebo method because the sample size was not enough.
Auricular acupuncture VS medications
Eight studies [46,47,49,51,53-56] reported the effective rate after intervention. The pooled results showed that the auricular acupuncture group was more likely to im-prove the sleep effective rate when compared to the medication (RR = 1.24, 95% CI 1.15 to 1.34). (Figure 2A) The mild heterogeneity (χ2
[image:4.595.58.547.88.343.2]= 7.64, P = 0.37, I2= 8%) might be because of different evaluation criteria for the effective rate. Therefore, we carried out a sensitivity ana-lysis without those referring to other criteria to confirm whether the heterogeneity was due to different criteria,
Table 1 Characteristics of Included studies
Study Sample Size* Randomized Method Treatment Control Course Outcome Measurements Follow-Up Safety Assessment
(Male/Female) of Bias**
Chen 2012 [46] 16/20 14/22 NR SV Diazepam 30 Days Effective rate NR NR ?,?,-,?,+,?,?
Chyi Lo 2013 [58] 0/14 0/13 Random Number Table MP Sham AA >21 Days PSG, PSQI NR NR
+,?,+,-,+,+,-Hisghman 2006 [60] 1/10 1/9 Computer Software MP Stainless Steel Pellet 17 Days PSQI Sleep Diary, ISI, MOS SF-12, TEQ 12 Days NR
+,+,+,?,+,+,-Hu 2010 [47] 22/10 18/13 NR SV Diazepam 28 Days Effective rate, PQSI, AIS NR NR
+,-,-,-,+,-,-Jiang 2010 [48] 14/49 10/52 Random Number Table SV Sham AA 20-25 Days PSQI NR NR
+,-,+,-,+,+,-Jin 2012 [49] 13/27 15/25 NR MP Estazolam 7-14 Days Effective rate, TESS NR Reported +,-,-,?,?,?,?
Lin 2007 [59] 16/14 17/13 NR SV Sham AA 51 Days Effective rate, EEG, PQSI NR NR
?,?,+,?,+,-,-Liu 2008 [50] 26/74 37/63 Computer Software MP Sham AA 30 Days PSQI NR NR
+,?,+,?,-,-,-Luo 2010 [51] 11/10 9/12 NR SV Estazolam 30 Days Effective rate, PQSI NR NR ?,?,,?,,,
-Pi 2012 [52] 71/79 75/75 Computer Software SV Sham AA 8 Weeks PSQI NR NR
+,-,+,-,-,-,-Suen 2002 [57] 10/110*** NR MP/SV Junci Medulla Attachment 21 Days Sleep Diary, Actigraphy 0.5-1 Year NR
?,?,+,+,+,-,-Wang 1993 [53] 10/20 12/18 NR SV Diazepam 20 Days Effective rate, SCL-90 NR Reported
?,?,-,?,+,-,-Wang 2002 [54] 17/13 14/16 NR MP Diazepam 3-10 Days Effective rate NR NR
?,?,-,?,+,-,-Wei 2010 [55] 22/14 21/15 NR NR Estazolam 28 Days Effective rate, Sleep Efficiency NR Reported
?,?,-,?,?,?,-Zhang 2008 [56] 10/58 8/50 Random Number Table MP Estazolam 18 Days Effective rate NR Reported
?,?,-,?,?,?,-Abbreviations: NRNot Reported,SVSemen Vaccariae Attachment,MPMagnetic Pearls Attachment,AAAuricular Acupuncture,PGSPolysomnography,PSQIPittsburgh Sleep Quality Index,MOS SF-12Medical Outcomes Study Short Form-12,TEQTreatment Expectancy Questionnaire,AISAthens Insomnia Scale,TESSTreatment Emergent Symptom Scale,EEGelectroencephalogram,SCL-90Symptom CheckList-90. *Sample Size:sample size of treatment groups are on the left column, control groups on the right. **Assessment of Bias: the seven domains were random sequence generation, allocation concealment, blinding personnel and participants, blinding assessor, incomplete data outcome, selective reporting, and other forms of bias from left to right. +: low risk, - : high risk, ?: *** In study Suen 2002, the male to female ratio was not reported after grouping.
Lan
et
al.
BMC
Comple
mentary
and
Alterna
tive
Medicine
(2015) 15:103
Page
5
of
and remaining five studies [46,47,49,55,56] all used Chinese Classification of Mental Disorders(CCMD) [61] for effective rate evaluation. The pooled result of these five still confirmed an advantage of auricular acupuncture over medications (RR = 1.27, 95% CI 1.16 to 1. 40), indicating the outcome of original meta-analysis was stable and dif-ferent criteria had few effects on it.
Total sleep time(minutes)
Total sleep time is time in bed minus sleep onset latency and minus waking time after sleep onset. This is continu-ous data, better indicated by higher values. Longer than six hours is defined as one of the treatment goals [62].
Auricular acupuncture VS sham or placebo method Four studies reported the outcome measured by self-reported sleep diary [60], wrist actigraphy [57], EEG [59] and PSG [58]. Statistics showed that auricular acupunc-ture intervention was more likely to prolong total sleep time compared to the control group (MD = 56.46, 95% CI 45.61 to 67.31), with no heterogeneity (χ2
= 1.72, P = 0.63, I2= 0%). (Figure 2B) In all treatment groups of these four studies, the total sleep time extended longer
than six hours after intervention, indicating benefit from auricular acupuncture was clinically relevant.
Auricular acupuncture VS medications
No studies in this comparison reported this outcome.
Sleep efficiency(%)
Sleep efficiency, the percent of time asleep while in bed, is also continuous data and higher values indicate better sleep efficiency. Higher than 80% to 85% is defined as normal [62].
Auricular acupuncture VS sham or placebo method Due to the high heterogeneity of included studies MD = 12.86, 95% CI 9.67 to 16.06, χ2 = 10.30, P = 0.02, I2 = 71%, we introduced subgroups according to age. As we can see in the old age subgroup [57,58,60], sleep efficiency was comparatively higher in auricular acupuncture inter-vention (MD = 9.14, 95% CI 5.14 to 13.14), with no het-erogeneity (χ2
[image:6.595.59.539.91.403.2]= 1.08, P = 0.58, I2= 0%). Also, there was a better improvement in the middle age group [59] (MD = 19.46, 95% CI 14.13 to 24.79) and the sleep efficiency was higher than 80% after treatment. These results indicated some benefit from auricular acupuncture, and it was more
significant in the middle-aged than that in the old (Figure 3A).
Auricular acupuncture VS medications
One study [55] reported that auricular acupuncture was superior to estazolam in sleep efficiency (MD = 21.44, 95% CI 16.30 to 26.58, P < 0.00001). (Figure 3A) This study however, was poor in methodological quality and failed to provide useful information about details, so this result needs further consideration.
Global score on PSQI(points)
PSQI is a numeric rating scale range from 0 to 21. Its seven components yield one global score [63]. Higher score indi-cates worse sleep quality. Clinically important effects were defined as a decrease by at least 1.93 for a beneficial effect and an increase of at least 2.9 for a negative effect [64].
Auricular acupuncture VS sham or placebo method Five out of the fifteen studies [48,50,52,58,59] revealed the global score on PSQI, and pooled results were in favour
of auricular acupuncture (MD = -3.41, 95% CI -3.93 to -2.89). The heterogeneity assessment result was also accept-able (χ2
= 6.11, P = 0.19, I2= 35%). (Figure 3B) More import-antly, the global score before and after intervention from all these treatment groups dropped more than 1.93, according to reported data, indicating the benefit of auricular acupunc-ture in sleep quality improvement was clinically relevant.
Auricular acupuncture VS medications
Only one study [47] was eligible for the meta-analysis and revealed lower PSQI score after auricular therapy compared to diazepam (MD = -3.62, 95% CI -4.59 to -2.65, P < 0.00001). (Figure 3B) This study was also poor in quality and inadequate to support the outcome.
Mean number of awakenings(No.)
[image:7.595.58.537.354.686.2]Average number of mid-sleep awakenings is continuous data. The more frequent awakenings occurred, the poorer sleep could be.
Figure 3The pooled outcomes of sleep efficiency and global score on PSQI revealed a better therapeutic effect of auricular acupuncture, statistically. A. Forest plot of sleep efficiency; Percent of time asleep while in bed, higher values indicate better sleep efficiency, and higher than 80% to 85% is defined as normal.B. Forest plot of global score on PSQI; Range 0-21, clinically important effects were defined as a minimum decrease by at least 1.93 for a beneficial effect and an increase of at least 2.9 for a negative effect.
Auricular acupuncture VS sham or placebo method Three studies reported the number of awakenings as assessed by sleep diary [60], EEG [59] or wrist actigraphiy [57]. Since the substantial heterogeneity among studies (χ2
= 11.27, P = 0.004, I2= 82%) cannot be resolved by subgroup analyses, pooled results were calculated with random model (MD = -3.27, 95% CI -6.30 to -0.25). (Figure 4A) Decreased frequency of awakenings reflected a better sleep quality after auricular acupuncture. The large heterogeneity might be caused by the difference in outcome measures used.
Auricular acupuncture VS medications
No studies in this comparison reported this outcome.
Sleep onset latency(minutes)
Sleep onset latency, the time in bed until falling asleep, is continuous data. Less than 30 minutes is defined as normal [62].
Auricular acupuncture VS sham or placebo method PSG [58], EEG [59], and wrist actigraphy [57] were adopted in three studies respectively and the pooled results showed sleep onset latency was shortened in the auricular acupunc-ture group compared to the control group (MD = -10.35, 95% CI -14.37 to -6.33). However, the difference of just ten minutes was not clinically relevant. The slight heterogeneity
might be explained by the different age of participants included in studies (χ2
= 2.63, P < 0.00001, I2= 24%) (Figure 4B).
Auricular acupuncture VS medications
No studies in this comparison reported this outcome.
Adverse effect
Auricular acupuncture VS sham or placebo method
No studies in this comparison reported this outcome.
Auricular acupuncture VS medications
[image:8.595.55.540.430.684.2]Four studies, taking estazolam or diazepam as the control, reported adverse events during intervention. Wei [55] re-ported two cases of auricle pain in treatment group, while the control group had two cases of headache, three of dizziness, one of thirst, and two of fatigue. Five cases of symptoms of a hangover, four of weakness, and one of poor coordination were reported in the control group from Wang’s study [53]. In Zhang’s study [56], five cases in the control group had daytime sleepiness. Jin [49] re-ported two cases using magnetic pearls experienced red-ness at the attached points and withdrew after treatment, as well as twenty-five cases experiencing drug dependence in the control group. In meta-analysis, RR was 0.11, 95% CI ranged from 0.04 to 0.26, and heterogeneity assessment turned out to be χ2= 2.58, P < 0.00001, I2= 0%, signalling
a reliable outcome in favour of the intervention group. Results demonstrated that auricular acupuncture caused less frequent and less severe adverse events compared with conventional hypnotics (Figure 4C).
Publication bias
As less than ten studies were included in a single out-come, the funnel plot would have no valuable reference.
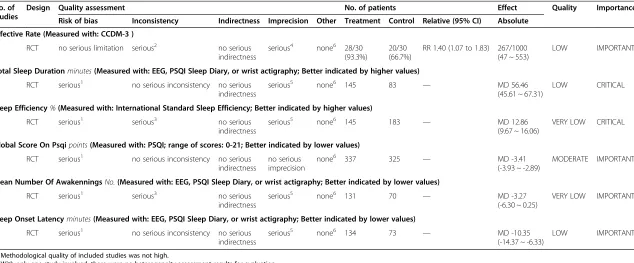
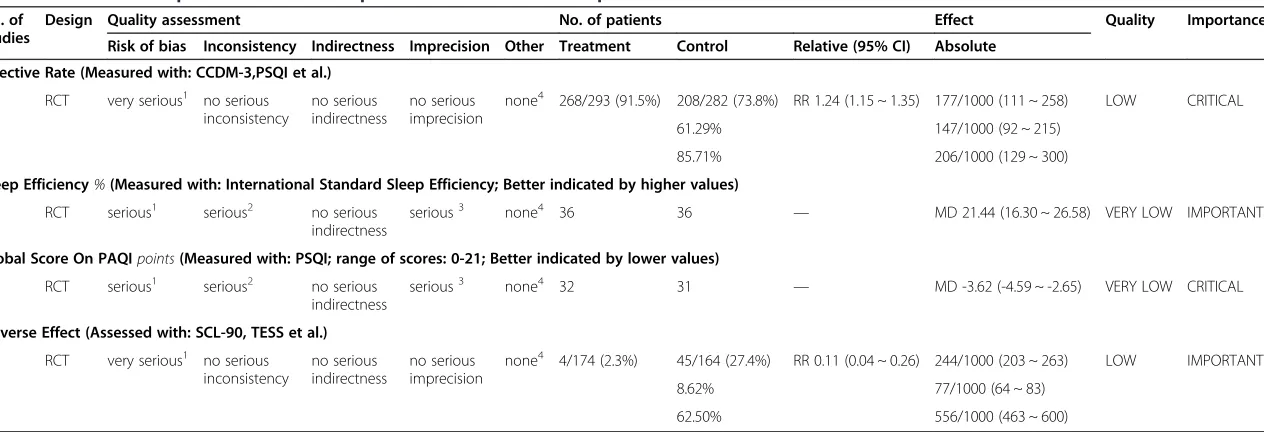
Evidence rating
Evidence rating would provide a transparent, concise illustration of decision making process in form of the GRADE evidence profile. Ten outcomes from meta-analyses were presented in two tables (Tables 2 and 3).
Discussion
Summary of main outcomes
We found auricular acupuncture showed benefit in all meta-analyses with significant differences between treat-ment groups and control groups. It improved the clinical effective rate, total sleep time, sleep efficiency, and lowered PSQI score, shortened sleep onset latency, and reduced number of awakenings when compared to sham auricular acupuncture or placebo. Also, it improved effective rate and sleep efficiency, lowered PSQI score, reduced the inci-dence of adverse effects when compared to conventional medications. But some of these statistical differences were not clinically relevant.
It is worth noting that, all included studies took either magnetic pearls or Semen Vaccariae for auricular pressing, the top two in clinical use. Some ear acupuncturists be-lieve that it is not just choices of the modality of stimu-lation that matter but also the choice of material [65]. Magnetic pearls will place a magnetic field over bio-logical tissues, when ions in the blood flow through mag-netic lines, the electromagmag-netic interaction will happen, thus improving the circulation of blood. This idea was confirmed by previous studies that using magnetic pearls for insomnia [57,66]. For the purpose of this review, our primary concern is whether the therapeutic effect of auricular acupuncture stands out, instead of the material being use. So we didn’t plan subgroup analyses for mag-netic pearls or Semen Vaccariae.
Although meta-analyses emphasised the positive aspect, the evidence rating was quite different. We evaluated ten outcomes through the GRADE system and presented results in two evidence profiles: inauricular acupuncture
VS sham or placebo method comparison, one ranked
moderate, three ranked low and two ranked very low; in auricular acupuncture VS medications comparison, two ranked low and two ranked very low. The most common reasons for downgrade lay in risk of bias and impreci-sion, for the majority of included studies were poorly designed or reported. They neglected crucial details for
methodological evaluation [40], and their cumulative sam-ple size failed to reach an appropriate level [41].
Comparison with other reviews
Previous systematic reviews on auricular acupuncture for insomnia [29,67] all reported that evidence was inadequate to make a firm conclusion. One more recent review [68] utilizing auricular acupuncture as an adjuvant method concluded that body and auricular acupuncture combined was superior to body acupuncture alone. Moreover, sys-tematic reviews [31,69-71] on a broader range taking all acupuncture modalities into account were conservative about the clinical relevance of auricular acupuncture. These inconsistencies were apparently owing to poor quality of methodology, weakness of data, high levels of heterogeneity and publication bias.
In comparison, our work narrowed the inclusion criteria to studies in which auricular acupuncture was the sole intervention. Then, we chose primary insomnia sufferers with at least one month of sleep problem as target population. Because secondary insomnia patients varied in physical conditions, symptoms and might result in substantial clinical heterogeneity in meta-analyses. Add-itionally, outcomes selected in the meta-analyses were of credible reliability and validity: five from the auricular
acupuncture VS sham or placebo method comparison
were all continuous variable, measured by PSG, EEG, actigraphic monitoring, PSQI, or Sleep Diary. These are internationally accepted indexes of sleep evaluation [72-74] and particularly the former three are objective sleep parameters; the adverse effects from the auricular acu-puncture VS medicationscomparison have complemented the assessment from another point of view. Likewise, the GRADE system would help to evaluate each outcome not only statistically but also methodologically by revealing and detailing all defects, which will definitely facilitate a better understanding and improvement for further research.
Implication of findings
With many countries reporting a high incidence of sleep disturbance in children and adolescents [75,76], insomnia appears to be a significant public health issue requiring accurate diagnosis and proper management. Our findings suggest auricular acupuncture is beneficial to primary in-somnia sufferers in respect of sleep quality and quantity.
Modern studies on the mechanism of the interaction of seed or pellet attachment on the ear proved the under-lying principles. Since the ear is richly innervated, the afferent projections from the auricular branch of the vagus nerve to the solitary tract nucleus formed the ana-tomical basis for the neuroregulation of auricular acu-puncture [77]. On applying pressure, a nerve impulse could be received by both autonomic nervous system
Table 2 Grade evidence profile of auricular acupuncture vs sham or placebo method comparison
No. of studies
Design Quality assessment No. of patients Effect Quality Importance
Risk of bias Inconsistency Indirectness Imprecision Other Treatment Control Relative (95% CI) Absolute Effective Rate (Measured with: CCDM-3 )
1 RCT no serious limitation serious2 no serious indirectness
serious4 none6 28/30 (93.3%)
20/30 (66.7%)
RR 1.40 (1.07 to 1.83) 267/1000 (47 ~ 553)
LOW IMPORTANT
Total Sleep Durationminutes(Measured with: EEG, PSQI Sleep Diary, or wrist actigraphy; Better indicated by higher values)
4 RCT serious1 no serious inconsistency no serious indirectness
serious5 none6 145 83 — MD 56.46
(45.61 ~ 67.31)
LOW CRITICAL
Sleep Efficiency%(Measured with: International Standard Sleep Efficiency; Better indicated by higher values)
4 RCT serious1 serious3 no serious indirectness
serious5 none6 145 183 — MD 12.86
(9.67 ~ 16.06)
VERY LOW CRITICAL
Global Score On Psqipoints(Measured with: PSQI; range of scores: 0-21; Better indicated by lower values)
5 RCT serious1 no serious inconsistency no serious indirectness
no serious imprecision
none6 337 325 — MD -3.41
(-3.93 ~ -2.89)
MODERATE IMPORTANT
Mean Number Of AwakenningsNo.(Measured with: EEG, PSQI Sleep Diary, or wrist actigraphy; Better indicated by lower values)
3 RCT serious1 serious3 no serious indirectness
serious5 none6 131 70 — MD -3.27
(-6.30 ~ 0.25)
VERY LOW IMPORTANT
Sleep Onset Latencyminutes(Measured with: EEG, PSQI Sleep Diary, or wrist actigraphy; Better indicated by lower values)
3 RCT serious1 no serious inconsistency no serious indirectness
serious5 none6 134 73
— MD -10.35
(-14.37 ~ -6.33)
LOW IMPORTANT
1. Methodological quality of included studies was not high.
2. With only one study involved, there were no heterogeneity assessment results for evaluation. 3. The pooled outcome revealed high heterogeneity.
4. The pooled (cumulative) sample size was lower than the optimal information size (OIS) and/or the total enrollment was less than 400 (continuous data). 5. The pooled (cumulative) sample size was lower than the optimal information size (OIS) and/or the total enrollment was less than 300 (dichotomous data). 6. The number of included studies is not enough to estimate publication bias temporarily.
Abbreviations:
95% CI: 95% Confidence Interval.
CCMD-3: Chinese Classification of Mental Disorders, 3rd
version; MD: Mean Difference
EEG: Electroencephalogram. PSQI: Pittsburgh Sleep Quality Index. RR: Risk Radio.
Comple
mentary
and
Alterna
tive
Medicine
(2015) 15:103
Page
10
of
Table 3 Grade evidence profile of auricular acupuncture vs medications comparison
No. of studies
Design Quality assessment No. of patients Effect Quality Importance
Risk of bias Inconsistency Indirectness Imprecision Other Treatment Control Relative (95% CI) Absolute Effective Rate (Measured with: CCDM-3,PSQI et al.)
8 RCT very serious1 no serious inconsistency
no serious indirectness
no serious imprecision
none4 268/293 (91.5%) 208/282 (73.8%) RR 1.24 (1.15 ~ 1.35) 177/1000 (111 ~ 258) LOW CRITICAL
61.29% 147/1000 (92 ~ 215)
85.71% 206/1000 (129 ~ 300)
Sleep Efficiency%(Measured with: International Standard Sleep Efficiency; Better indicated by higher values)
1 RCT serious1 serious2 no serious indirectness
serious3 none4 36 36 — MD 21.44 (16.30 ~ 26.58) VERY LOW IMPORTANT
Global Score On PAQIpoints(Measured with: PSQI; range of scores: 0-21; Better indicated by lower values)
1 RCT serious1 serious2 no serious indirectness
serious3 none4 32 31 — MD -3.62 (-4.59 ~ -2.65) VERY LOW CRITICAL
Adverse Effect (Assessed with: SCL-90, TESS et al.)
4 RCT very serious1 no serious inconsistency
no serious indirectness
no serious imprecision
none4 4/174 (2.3%) 45/164 (27.4%) RR 0.11 (0.04 ~ 0.26) 244/1000 (203 ~ 263) LOW IMPORTANT
8.62% 77/1000 (64 ~ 83)
62.50% 556/1000 (463 ~ 600)
1. Methodological quality of included studies was not high.
2. With only one study involved, there were no heterogeneity assessment results for evaluation.
3. The pooled (cumulative) sample size was lower than the optimal information size (OIS) and/or the total enrollment was less than 400 (continuous data). 4. The number of included studies is not enough to estimate publication bias temporarily.
Abbreviations:
95% CI: 95% Confidence Interval.
CCMD-3: Chinese Classification of Mental Disorders, 3rd version. MD: Mean Difference.
PSQI: Pittsburgh Sleep Quality Index. SCL-90: Symptom Check List-90. TESS: Treatment Emergent Symptom Scale. RR: Risk Radio.
Lan
et
al.
BMC
Comple
mentary
and
Alterna
tive
Medicine
(2015) 15:103
Page
11
of
and central nervous system. At the same time, magnetic fields were added if magnetic pearls were attached. In traditional Chinese medicine theory this effect might promote the circulation of Qi and blood, therefore im-proving the physiological condition of the body.
The results of these studies explained the overall im-provement of sleep parameters after intervention: longer total sleep time, higher sleep efficiency and clinical effect-ive rate, lower PQSI score, shorter sleep onset latency, less awakening times and adverse events. However, methodo-logical assessments indicated a lack of sufficient evidence to support a strong recommendation. More strictly de-signed clinical trials are required in order to facilitate an explicit conclusion on the benefits of auricular acupunc-ture for primary insomnia.
Limitation
Several limitations in this review should be noted. First, only four of the included studies [53,57,58,60] referred standard ear maps. Currently, it is a major problem in research of auricular therapy both in western and eastern medical systems [27,78,79]. Diversity in point location may lead to different clinical outcomes, misunderstanding in medical research and academic communication, as well as ambiguous conclusions in a systematic review. Second, RCTs with sham auricular acupuncture, placebo or blank control were inadequate in quantity. As a compromise, we extended the inclusion criteria for trials taking medica-tions as control and presented results according to sep-arate control methods [80]. Third, we pooled data from Semen Vaccariae or magnetic pearls groups together in meta-analyses because studies with same material were limited. However, we believe it will be more rigorous to perform subgroup analyses or sensitivity analyses if data permitted. Additionally, we only conducted a search for Chinese and English articles so that inclusion bias was unavoidable.
Conclusions
Auricular acupuncture has been extensively adopted in Asian countries. With minimal consumption of medical resources, auricular acupuncture could be integrated into routine care for insomnia without difficulty in a wide range of clinical settings. In this review, meta-analyses of all included studies revealed a positive effect of aur-icular acupuncture for primary insomnia, however the poor methodological quality, insufficient sample size and possible publication bias of these studies mean that the evidence is not yet adequate to provide a strong support for the therapy in primary insomnia management. Future experimental designs and publications need to be more specific in details [81], such as implementation, point selection and location, extension and time of stimula-tion. We hope this review will raise attention to this
cost-effective, safe therapy and produce more scientific evidence to support its clinical application.
Additional file
Additional file 1:Search Strategy for Medline, Embase and CBM.
Competing interests
The authors declare that they have no competing interest.
Authors’contributions
Study concept and design: LF, WX, LY. Acquisition of data: LY, TH, WF. Analysis and interpretation of data: LY, WX. Drafting of the manuscript: LY, TH, WN. Modification of the manuscript: LY, WX, TH, WN, ZL. All authors have approved the final version of the manuscript.
Acknowledgements
The authors thank the following Professor and students for their help in literature search: Mr. Lixuan Zheng, Brandeis University, USA., Mr. Rui Liu, Shanghai Jiao Tong University, Mr. Xiaoguang Hu, University of Bristol, UK and Prof. Byung-Cheul Shin from Pusan National University, South Korea. We thank Lei Lan, PhD., Chengdu University of TCM , for her advice in protocol creation, and thank Prof. Chieh-Mei Wang from Sichuan University and Mr. Robert Crane from Chengdu University of TCM, for their effort in the manuscript amendment.
Sincere thanks to the authors of included studies for providing additional information: Hisghman IV, Ph.D., University of Virginia , USA. Weihong Liu, Associate Research Fellow, Beijing Institute of Traditional Chinese Medicine. Bin Jiang, Associate Chief Physician, General Hospital of Peoples Liberation Army. Yanling Pi, Attending Doctor, Lianyang Community Health Service Center of Pudong New District. Xiaolin Luo, Chief Physician, Second People’s Hospital of Hubei Province. Wei Hu, Attending Doctor, Hunan Provincial Work Injury Rehabilitation Center.
Funding
The study was granted by the supporting plan projects of Science and Technology Department of Sichuan Province,“Operation specification and clinical evaluation on non-drug therapy of Traditional Chinese Medicine” (No.2011SZ0302) and“Sichuan youth innovation team of Science and Technology on the Effect of acupuncture mechanism research”( No.2015TD0010). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author details
1Acupuncture and Tuina School/Third Teaching Hospital, Chengdu University
of Traditional Chinese Medicine, No.37, Shierqiao Road, Jin Niu District, Chengdu, Sichuan 610075, China.2VIP Ward of Acupuncture, First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, No.314, An Shanxi Road, Nankai District, Tianjin 300073, China.3Sichuan 2nd Hospital of Traditional Chinese Medicine, No.20, Sidao Street, Qing Yang District, Chengdu, Sichuan 610031, China.
Received: 4 April 2014 Accepted: 12 March 2015
References
1. Ohayon MM. Prevalence and correlates of nonrestorative sleep complaints. Arch Intern Med. 2005;165(1):35–41.
2. Roth T, Zammit G, Lankford A, Mayleben D, Stern T, Pitman V, et al. Nonrestorative sleep as a distinct component of insomnia. Sleep. 2010;33(4):449–58. 3. Buysse DJ. Insomnia. JAMA. 2013;309(7):706–16.
4. Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–41. 5. Yoshioka E, Saijo Y, Kita T, Satoh H, Kawaharada M, Fukui T, et al. Gender
differences in insomnia and the role of paid work and family responsibilities. Soc Psychiatry Psychiatr Epidemiol. 2012;47(4):651–62.
7. Tran DP, Spierings EL. Headache and insomnia: their relation reviewed. Cranio. 2013;31(3):165–70.
8. Staner L. Comorbidity of insomnia and depression. Sleep Med Rev. 2010;14(1):35–46.
9. Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1–3):10–9. 10. Palagini L, Bruno RM, Gemignani A, Baglioni C, Ghiadoni L, Riemann D. Sleep loss
and hypertension: a systematic review. Curr Pharm Des. 2013;19(13):2409–19. 11. Meng L, Zheng Y, Hui R. The relationship of sleep duration and insomnia to
risk of hypertension incidence: a meta-analysis of prospective cohort studies. Hypertens Res. 2013;36(11):985–95.
12. Hayes Jr D, Anstead MI, Ho J, Phillips BA. Insomnia and chronic heart failure. Heart Fail Rev. 2009;14(3):171–82.
13. Jaussent I, Empana JP, Ancelin ML, Besset A, Helmer C, Tzourio C, et al. Insomnia, daytime sleepiness and cardio-cerebrovascular diseases in the elderly: a 6-year prospective study. PLoS One. 2013;8(2):e56048. 14. Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disterbance and
suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):1160–7. 15. McCall WV, Black CG. The link between suicide and insomnia: theoretical
mechanisms. Curr Psychiatry Rep. 2013;15(9):389.
16. Huang W, Kutner N, Bliwise DL. Autonomic Activation in Insomnia: The Case for Acupuncture. J Clin Sleep Med. 2011;7(1):95–102.
17. Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14(1):9–15.
18. De Zambotti M, Covassin N, De Min TG, Sarlo M, Stegagno L. Sleep onset and cardiovascular activity in primary insomnia. J Sleep Res. 2011;20(2):318–25. 19. Covassin N, de Zambotti M, Sarlo M, De Min TG, Sarasso S, Stegagno L. Cognitive performance and cardiovascular markers of hyperarousal in primary insomnia. Int J Psychophysiol. 2011;80(1):79–86.
20. Spiegelhalder K, Regen W, Baglioni C, Riemann D, Winkelman JW. Neuroimaging studies in insomnia. Curr Psychiatry Rep. 2013;15(11):405. 21. Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M,
et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14(1):19–31.
22. Buford UJ, Nemeroff CB. Current treatment options for insomnia. Drugs Today. 2012;48(6):415–23.
23. Schwarz S, Frolich L, Deuschle M. Pharmacological interventions for insomnia in the elderly. Internist Prax. 2013;53(2):377–90.
24. Matthews EE, Arnedt JT, McCarthy MS, Cuddihy LJ, Aloia MS. Adherence to cognitive behavioral therapy for insomnia: A systematic review. Sleep Med Rev. 2013;17(6):453–64.
25. Bertisch SM, Wells RE, Smith MT, McCarthy EP. Use of relaxation techniques and complementary and alternative medicine by American adults with insomnia symptoms: results from a national survey. J Clin Sleep Med. 2012;8(6):681–91.
26. Frass M, Strassl RP, Friehs H, Mullner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: a systematic review. Ochsner J. 2012;12(1):45–56. 27. Romoli M. Ear acupuncture: historical abstract–differences of ear
cartography between the east and the west. Deutsche Zeitschrift für Akupunktur. 2010;53(4):24–33.
28. Hsu E. Innovations in acumoxa: Acupuncture analgesia, scalp and ear acupuncture in the People’s Republic of China. Soc Sci Med. 1996;42(3):421–30.
29. Lee MS, Shin BC, Suen LK, Park TY, Ernst E. Auricular acupuncture for insomnia: a systematic review. Int J Clin Pract. 2008;62(11):1744–52. 30. Sjoling M, Rolleri M, Englund E. Auricular acupuncture versus sham
acupuncture in the treatment of women who have insomnia. J Altern Complement Med. 2008;14(1):39–46.
31. Yeung WF, Chung KF, Poon MMK, Ho FYY, Zhang SP, Zhang ZJ, et al. Acupressure, reflexology, and auricular acupressure for insomnia: A systematic review of randomized controlled trials. Sleep Med. 2012;13(8):971–84. 32. Chinese Psychiatric Association. Chinese Classification of Mental Disorder(3rd
ed.) (CCMD-3). Ji Nan: Shandong science and Technology Press; 2001. 33. American Psychiatric Association. Diagnostic and statistical manual of
mental disorders(4th ed.) (DSM-IV). Washington, DC: American Psychiatric Association; 1994.
34. World Health Organization (WHO). The classification of mental and behavioral disorder diagnostic criteria for research (10th ed.)(ICD-10). Geneva, Switzerland: WHO; 1992.
35. Ping W, Huixu X, Qi Z, Naichuan S, Hongmei W, Zongdao S. How to Design the Data Collection Form in Cochrane Systematic Reviews. Chin J Evid-Based Med. 2011;11(3):341–5.
36. Taixiang W, Guanjian L. Conception, implementation and report of allocation concealment and blinding. Chin J Evid-Based Med. 2007;7(3):222–5. 37. Gordon HG, researcher GeVt, Andrew DO, Kunz R. GRADE: an emerging
consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(4):924–6.
38. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence–indirectness. J Clin Epidemiol. 2011;64(12):1303–10.
39. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence–inconsistency. J Clin Epidemiol. 2011;64(12):1294–302.
40. Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence–study limitations (risk of bias). J Clin Epidemiol. 2011;64(4):407–15.
41. Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines: 6. Rating the quality of evidence–imprecision. J Clin Epidemiol. 2011;64(12):1283–93.
42. Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence–publication bias. J Clin Epidemiol. 2011;64(12):1277–82.
43. Gordon HG, Andrew DO, Shahnaz S, Paul G. GRADE guidelines: 9. Rating up the quality of evidence. J Clin Epidemiol. 2011;64(12):1311–6.
44. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
45. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
46. Xiaoqian C. Clinical observation on treating insomnia by ear pressing. J Chin Clin Med. 2012;4(2):38–9.
47. Wei H, Ping L, Haipeng J, Qijun H. Effect of auricular point buried therapy on sleep promotion in the young and middle-aged patients with insomnia. Chin J Clin Rehabil. 2010;25(6):450–2.
48. Bin J, Zhuhong M, Fang Z. Auricular acupuncture for insomnia: a randomized controlled trial. Chin J Epidemiol. 2010;31(12):1400–2.
49. Linhong J, Yueyi L, Huali C, Shaowei H. Clinical study of severe insomnia treated with magnetic pearls attachment ear acupuncture. Shandong Journal of Traditional Chinese Medicine. 2012;31(1):36–7.
50. Weihong L, Beihai W, Jian L, Guowei W, Jie Q, Jie C, et al. Ear acupoint plaster for subhealth with sleep disturbance as main symptom: a randomized control trial. Chinese Journal of Basic Medicine in Traditional Chinese Medicine. 2008;14(3):222–3.
51. Xiaolin L, Haowen L. Observation on seed attachment ear acupuncture for 21 college students with insomnia. Guiding Journal of Traditional Chinese Medicine and Pharmacy. 2010;16(2):46–7.
52. Yanling P, Xiangyu W, Zhen Y, Miaogen C, Yongfang H, Ziling Z, et al. Clinical observation on patients with insomnia treated with ear acupuncture based on syndrome differentiation. Chinese Journal of Rehabilitation. 2012;27(1):37–8. 53. Xingming W. Seed attachment ear acupuncture and diazepam for insomnia:
a clinical research. J Clin Psychiatry. 1993;3(3):189.
54. Songtao W. Magnetic pellet attachment ear acupuncture for insomnia. Clinical Journal of Anhui Traditional Chinese Medicine. 2002;14(4):164. 55. Yan W, Jiyou K. Clinical observation on ear acupoint plaster for sleep
improvement of insomnia sufferers. China’s Naturopathy. 2010;18(4):15–6.
56. Guoxiong Z. Therapeutic effect of ear acupuncture for insomnia on college students. Chinese Journal of School Health. 2008;29(6):568.
57. Suen LK, Wong TK, Leung AW. Effectiveness of auricular therapy on sleep promotion in the elderly. Am J Chin Med. 2002;30(4):429–49.
58. Lo C, Liao WC, Liaw JJ, Hang LW, Lin JG. The stimulation effect of auricular magnetic press pellets on older female adults with sleep disturbance undergoing polysomnographic evaluation. Evid Based Complement Alternat Med. 2013;2013:530438.
59. Bolang L. Clinical study on auris-points for insomnia: a randomized control trial. Beijing: Beijing University of Chinese Medicine; 2007.
60. Hisghman IV. Effects of a standardized auricular point prescription in adults with insomnia. Virginia: University of Virginia; 2006.
61. Ministry of Health of China. Clinical Research Guidelines of New Chinese Herbal Medicine. Beijing: Ministry of Health of the People’s Republic of China; 1993.
62. Schutte-Rodin S, Broch L, Buyss D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487–504.
63. Buysse DJ, Reynolds 3rd CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
64. Yaoying L, Yan L, Jiyang P, Darong W. Research about the minimal important difference of Pittsburgh Sleep Quality Index based on clinical trials of TCM. Journal of Guangzhou University of Traditional Chinese Medicine. 2013;30(4):574–8.
65. Yang P. Clinical observation of therapeutic effect on chronic insomnia with acupuncture plus ear pressure with different materials. Nanjing: Nanjing University of Chinese medicine; 2010.
66. Wen L. Comparison between magnetic pearls or Semen Vaccariae ear pressing for 108 cases of insomnia. Chinese Acupuncture & Moxibustion. 2000;12:722–4.
67. Chen HY, Shi Y, Ng CS, Chan SM, Yung KKL, Zhang QL. Auricular acupuncture treatment for insomnia: a systematic review. J Altern Complement Med. 2007;13(6):669–76.
68. Xiaodong H, Lixin F, Sheng L, Zailing W, Ran Z. Systematic evaluation of therapeutic effect of acupuncture combined with auricular point sticking and acupuncture for treatment of insomnia in clinical study. Journal of Clinical Acupuncture and Moxibustion. 2010;26(11):56–9.
69. Cao H, Pan X, Li H, Liu J. Acupuncture for treatment of insomnia: A systematic review of randomized controlled trials. J Altern Complement Med. 2009;15(11):1171–86.
70. Huang W, Kutner N, Bliwise DL. A systematic review of the effects of acupuncture in treating insomnia. Sleep Med Rev. 2009;13(1):73–104. 71. Cheuk DK, Yeung WF, Chung KF, Wong V. Acupuncture for insomnia.
Cochrane Database Syst Rev. 2012;9, CD005472.
72. Hu J. The effect of treatment of acupuncture was evaluated by polysomnogram in patients with insomnia. Journal of modern electrophysiology. 2011;18(4):220–2. 73. Israel B, Buysse DJ, Krafty RT, Begley A, Miewald J, Hall M. Short-term stability
of sleep and heart rate variability in good sleepers and patients with insomnia: for some measures, one night is enough. Sleep. 2012;35(9):1285–91.
74. Tsai PS, Wang SY, Wang MY, Su CT, Yang TT, Huang CJ, et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual life res int j qual life asp treat care rehab. 2005;14(8):1943–52.
75. Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev. 2010;14(3):179–89. 76. Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and
problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12(2):110–8.
77. He W, Wang X, Shi H, Shang H, Li L, Jing X, et al. Auricular acupuncture and vagal regulation. Evid Based Complement Alternat Med. 2012;2012:786839. 78. Gori L, Firenzuoli F. Ear acupuncture in European traditional medicine. Evid
Based Complement Alternat Med. 2007;4 Suppl 1:13–6.
79. Hongqin L. Textual research of Chinese and foreign auricular points’ nomenclature and location based on national standard(GB/T 13734-2008) of China. Beijing: Beijing University of Chinese Medicine; 2009.
80. Nicholls SJ, Bakris GL, Kastelein JP, et al. Effect of aliskiren on progression of coronary disease in patients with prehypertension: The aquarius randomized clinical trial. JAMA. 2013;310(11):1135–44.
81. MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, et al. Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. Journal of evidence-based medicine. 2010;3(3):140–55.
Submit your next manuscript to BioMed Central and take full advantage of:
• Convenient online submission
• Thorough peer review
• No space constraints or color figure charges
• Immediate publication on acceptance
• Inclusion in PubMed, CAS, Scopus and Google Scholar
• Research which is freely available for redistribution