T HE OPTIMUM AGE at which to begin to feed a premature baby is not yet known. Investigations designed to evaluate effectsof early or lateinitiationof feeding have so far yielded inconclusiveresults.In general, two conflicting concepts of man agement may be distinguished. On the one hand is the “¿early―regimen in which the premature infant is fed during the first 24 hours after birth, and on the other is the “¿late―regimen in which all fluids are with held until the baby is 48 to 72 hours old. In the United States the latter program has l)een more generally accepted.
Results from starvation experiments on newborn laboratory animals are species specific and cannot generally be applied to management of premature infants. The newborn full-term pig, for instance, dies if not fed within the first few hours after birth.1 In contrast, other newborn animals readily survive when feedings are withheld for 24 hours or more following birth.2'3 It is common knowledge that both full-term and premature newborn infants are able to sur vive without fluids or nutrients for more than 24 hours after birth. That physiological adjustments vary with the degree of imma turity of newborn premature babies who re ceive no fluids was demonstrated by Hansen and Smith.4 Newborn premature subjects de prived of water and nutrients during their first 3 days of life excreted small volumes of urine of high osmolarity and developed hypernatremia. On the other hand, full term babies under similar conditions of thirsting produced urines of relatively low electrolyte concentration. It was also dem onstrated that when both full-term and premature infants were fed a dextrose solu tion, body water was conserved without in
ADDRESS:3975 Broadway,New York32,New York.
creased retention of electrolytes.Smith@ recommended late feeding of premature babies because of their susceptibility to
aspiration pneumonia° and because of ap
parent absence of a detrimental effect from a reasonable period of fasting.
The ability of some newborn premature infants to withstand water and nutritional deprivationfor 3 to 4 days exemplifiestheir tolerance to physiological aberration. That such thirsting and fasting is beneficial for all premature babies, however, remains to be shown. It is rational to argue that be cause the premature baby lacks the meta bolic reserves of the full-term infant, his need for external provision of these sub stances occurs at a younger age. This is the basis for Ylppo's7 practice of early feeding of premature babies. Gleiss8 demonstrated a higher mortality rate in babies whose feedings were withheld until 36 hours as op posed to those fed between the ages of 12 and 24 hours. Burnard° recommends an early supply of calories because premature babies with respiratory distress utilize more energy as a resultof dyspnea. Administra tion of dextrose and hypotonic saline solu tion by mouth or vein within a few hours after birth has been claimed to be bene ficial to offspring of diabetic mothers.1° Such babies resemble premature infants in that they readily develop a similar respira tory distress syndrome and they also have similar biochemical and physiological dis turbances. Rudolph et al.,hm however, were unable to demonstrate that early feedings influenced the survival of such babies. Al though aspiration of milk may be a major impediment to early feeding regimens, it is unlikely that inhaled dextrose and saline solutions would have the same dire effects.
PEDIATRICS, November 1960
756
EARLY FEEDINGOF DEXTROSEAND SALINE SOLUTION TO
PREMATUREINFANTS
William Allen Bauman, M.D.
No Fluids: No administration of fluids by
any route until 36 hours of age.
Fluid Group: A sterile solution of 5% dex trose in 0.45% saline was administered through the nasogastric tube by continuous gravity drip
or infusion pump* at a rate to approximate
60 ml/kg each 24 hours; this was commenced
as soon after admission as feasible. Selection of
subjects for either the no fluid or fluid group was based upon printed instructions on cards
within sealed envelopes. The envelopes were
divided into two birth-weight categories,
1,501-1,750 grams and 1,751-2,000 grams. Each con
tained equal numbers of subjects for the fluid
or the no fluid therapy. The cards were ar
ranged in a sequence determined by a table of
random permutations. The category into which each subject would be assigned was not known until his envelope was opened. There were no defectors from the study and only one baby was not permitted by his private pediatrician to be entered. Another infant was selected to take his place. With this exception, the 50 sub jects studied represented consecutive admis sions. The protocol called for continuous ad ministration of fluid by intravenous route if
vomiting or other difficulties made nasogastric
administration inadvisable. Only one infant
received fluids in this manner.
The parameters for measurement of the ef fects of early feeding consisted of the incidence of respiratory distress and mortality. It was ex pected that useful information could be ob
tained after 40 to 50 subjects had been treated.
RESULTS
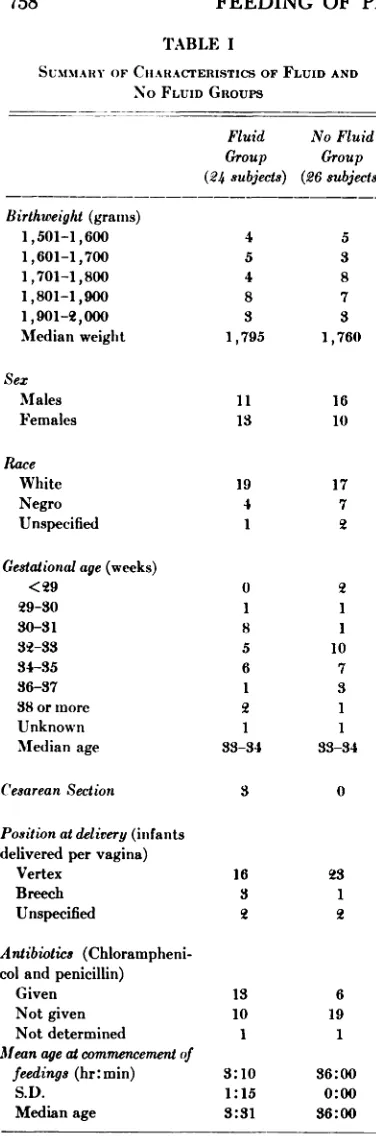
The study was commenced in Septem ber, 1958, and completed in October, 1959, after 50 subjects had been treated. There were 24 babies who received fluid and 26 who received none. The median age of the subjects upon admission to the Premature
Nursery of Babies Hospital was 55 minutes
(range 20 minutes to 4 hours). Numerous characteristics of the two groups are sum marized in Table I. The median birth weight of the fluid treated group was 1,795 grams and that of the other group was 1,760 grams. The distribution of sex and race in the two groups was similar. There was no significant difference in the median gesta
0 Manufactured by the Harvard Apparatus Co.,
Dover, Mass.
Because of these conflicting findings and opinions, a clinical trial was undertaken to test the hypotheses that early feeding of dextrose and hypotonic saline solution to premature babies would decrease the mor tality and diminish the incidence of respi ratory distress. Previous experience12 at the Premature Nursery of Babies Hospital showed that the incidence of respiratory distress in infants of birth weights between
1,501 and 2,000 grams was 25% at age 6 hours and decreased to 11% by age 24 hours. About 10% of all infants in this
weight category died before 8 days of age.
SUBJECTS AND METHODS
A protocol designed to minimize the role
of bias utilized a number of predetermined
criteria for admission to the study and for sub
sequent treatment. Only premature infants
born in the Sloane Hospital for Women, Ob
stetrical Service of the Columbia-Presbyterian
Medical Center, were accepted. Their birth
weights ranged between 1,501 and 2,000 grams. All infants were weighed and examined. A polyethylene nasogastric catheter was in serted and its proximal end was taped onto the subject's face. The incubator temperature was
controlled so as to maintain axillary tempera
tures between 96 and 98°F (35.5 to 37.1°C). Relative humidity was kept between 80 and 90%. Oxygen was administered only as indicated by the presence of cyanosis. Chioramphenicol. 15 mg/kg/day, and penicillin, 100,000 units twice a day, were injected by the intramuscular route only to those subjects whose mothers had infection or had premature rupture of membranes. An oral preparation containing
vitamin K analogue, 1 mg, vitamin E, 25 mg,
and vitamin C, 50 mg/dose, was given daily
commencing at age 12 hours. All babies were
placed in the supine position with the neck
extended by means of a rolled towel under the
upper back. Measurement of vital signs, in cluding temperature, respiratory rate and re traction score,12 was performed at age 6 hours and every 6 hours thereafter until 5 days of age. This information was obtained by a meth od which required the nurse to evaluate each in fant at each scoring period without knowledge of the previous score.12 All babies were weighed at 36 hours and again at 72 hours.
FluidNo
FluidGroupGroup(24
subjects)(26subjects)
SUMMARY OF CIIARAc-FERISTIcS OF FLUID AND
Birthweight (grains)
1,501—1,600
1,601—1,700
1,701—1,800 1,801—1,900 1,901—2,000 Median weight
Sex
Males
Females Race
White
Negro Unspecified
Gestational age (weeks)
<29
29—30
30—31 32—33 34—35
36—37
38 or more Unknown Median age
Cesarean Section
Position at delivery (infants
delivered per vagina) Vertex
Breech
Unspecified
Antibiotics (Chlorampheni coland penicillin)
Given
Not given Not determined
Mean age at commencement of feedings (hr:min)
S.D.
Median age
0
1
8
5
6
2
1
33—34 3
tionalages nor in the position
TABLE Iantibiotics than in the untreated group,
this difference was no greater than would
No FLUID GROUPS be expected to occur as a result of chance
alone. Half of the treated subjects were started on the solution by the age 3% hours, and in all but one it was commenced be
______ ___________ fore the first scoring period at 6 hours of
age. This one subject was started at age 6
4 5 hours, 18 minutes.
Respiratory performance, as measured by
8 the retraction score,'2 disclosed increased
3 incidence of dyspnea in the subjectsof the 1,795 1,760 fluid treated group. At age 6 hours, nine babies in the treated group and three babies in the untreated group had respiratory dis tress.At 12 hours, 18 hours and 24 hours of age, there were appproximately three to four times as many subjects in the fluid 19 17 treated group with significantdyspnea as
4 7 in the group who received no fluids (Table
1 2 II).
The mortality at 56 and 168 hours of age was not significantly greater in the subjects 1 who received earlyfluidsthan in those who
1 were not fed until age 36 hours (Table III).
10 Weight loss at 36 hours of age was con
sistent in all the non-fluid treated subjects whereas about half of their fluid treated
1 cohorts had no loss (Table IV).
33-34 Necropsies were performed on all seven
subjects who died. The principal anatomi
0 cal findings are listed in Table V. Pulmo
nary hyaline membranes were present in
three of the five treated babies but were
16 23 absent in the two untreated infants.All had 3 1 edema of the extremities or manifested
2 2. congestion and edema of the viscera.
DISCUSSION
13 6 Cursory examination of the resultssug
10 19 gests that early administration of a solution
1 1 of hypotonic sodium chloride and 5% dex
trose to one group of premature infants
3:10 36:00 .
1:15 0:00 durmg their first36 hours was associated 3:31 36:00 with increased dyspnea, whereas there was
Age (hours)FluidsNo
Fluids
3,@
Distress No
DistressDistress No Distress6
12 18 249(38)a
15
10(44)'@ 13
8(37)c 14
6(29)d 153(12)
23
2( 8) 24
3(12) 23
2( 8) 243.3
<0.1 7.1 <0.01 2.9 <0.1 6.2 <0.02
FluidsNo Fluidsx', pDied
Before 168 hours
Before 56 hours5
(18%)
4 (20%)2
(7.5%) 1(4%).25
>0.5 1 .08 >0.3Survived1924
TABLE II
RESPIRATORY PERFORMANCE
(Figures in Parentheses Represent Per Cent Retracting)
(a) 99% binomial confidence limits are 15—65% (b) 99% binomial confidence limits are 18—71%
(c) 99% binomial confidence limits are 16-66%
(d) 99% binomial confidence limits are 8—59%
Binomial confidence limits from Tablesfor use vyithBinomial Samples by Mainland, D., Herrera, L. and Sut
cliffe,M.: Department ofMedicalStatistics,New York UniversityCollegeof Medicine,New York 16,New York,
1956.
the result of chance distribution. Although 23 of the treated subjects had received some fluids before age 6:01 hours, the max imum quantity administered was 21 ml and the mean volume was 11.5 ml. It is unlikely that such a small amount could influence respiratory performance this rapidly, even when the factors of regurgitation and aspi ration are considered. Although precautions had been taken to obtain two comparable groups of babies, those destined to receive fluid therapy had a higher incidence of dyspnea early in the course of treatment by age 6 hours (Table II). Despite the probability that such a difference between the two groups could occur as a result of chance only 1 in 10 times, it is unlikely that
any factor, other than chance, exerted this
influence.
It should be noted that the incidence of breathing difficulty in the treated subjects
TABLE III
MORTALITY
remained high and did not decrease signifi cantly at subsequent scoring periods. Thus, dyspnea persisted in spite of administration of the dextrose and saline solution. The lack of influence on frequency and diffi culty of respirations supports the findings of Rudolph et at.―Before final conclusions can be drawn the roles of dextrose, sodium chloride, water and other nutrients in vari ous concentrations and combinations re quire testing. Moreover, it would be ad vantageous to apply additional criteria such as electrolyte changes, measurement of heart size, hypoglycemia, etc., beside the development of respiratory difficulty in as sessment of morbidity in prematurity.
The difference in mortality in the two groups parallels the difference in incidence of respiratory distress. In the study of in fants of diabetic mothers1' a similar rela tionship was noted. That neonatal dyspnea and increased mortality of premature ba bies are associated has also been previously
demonstrated'2
FluidsNo FluidsX@,)1Loss
No LossLoss No
LossAt36hours
At 72 hours10
11
17 126
0
25 014.3
<0.01
.032 >0.8
FluidsNo FluidsAge
at Death6 hrMassive hr12 hr18 hr34 hr78 hr51 hr106
aspiration of amniotic fluid contents
EmphysemaAtelectasis
Ilyaline mem braneMassive
aspira tion of amniotic fluid contents
AtelectasisPleural
effu sion
Pulmonary congestionMassive
aspira tion of amniotic fluid contents
AtelectasisAtelectasis Pulmonary edemaMassive
aspira tion of amniotic fluid contents
Omphalitisllyaline
membrane
Pulmonary edema
Pneumonia
Intraventricular hemorrhage
Subeapsular
hematoma of liverVi@ral congestion
Edema of limbsIlyaline
mem brane
Edema of limbs
Subcapsular hematoma of liverDilation
of heart
AscitesEmphysemaPulmonary edema
Visceral congestion
()mphalitisIntracere
bralhemor
rhageSepsis
hemorrhagic pneumonia
Dilatation of heart
Congestion of visceraDilated
ductus arteriosusI)ilated
ductus arteriosus
TABLE IV
WEIGHT CHANGE IN SURVIVING SUBJECTS
early feedings. A salutary effect from such conservation of body water during the first days of life has not been proven. In another study,4 even when dextrose water alone was given, there was conservation of body fluids. The mechanism by which this occurs, al though poorly understood, perhaps leads to enhancement of anabolism. McCance and Widdowson― suggest that in newborn babies most substances which decrease cel lular catabolism promote growth through conservation of minerals and fluids. It is in teresting that although the 11 subjects who did not lose weight commenced taking a milk formula at age 36 hours, all but one weighed less at 72 hours than at 36 hours. One possible explanation is that the osmolar load of the formula necessitated excretion of body water.
Numerous theories relative to the patho
genesis of pulmonary hyaline membrane production have been formulated.14 Cor relations among the various pulmonary findings in necropsies of newborn infants have been reported.'5 In this study all seven subjects who died had anatomical evidence of excessive body fluid or of con gestion of blood vessels. There were no significant differences in the presence of these or other abnormalities between the treated and untreated babies (Table V). However, it was observed that hyaline membranes occurred only in the babies who received fluid. If more extensive stud ies show this relationship to be significant, the etiologic roles of overhydration or as piration of gastric contents must be seri ously reconsidered. It should be remem bered, however, that hyaline membranes also develop in premature newborn babies
TABLE V
ARTICLES 761
who have not been fed. That there are nu merous factors, each of which may lead to the clinical phenomenon of dyspnea and may culminate with the pathologic finding of hyaline membrane, is a possibility which still exists.
SUMMARY AND CONCLUSIONS
Conflicting opinions concerning the op timum age at which to commence feeding premature infants have resulted in either early or late regimens. In order to test the hypothesis that the early administration of fluids to premature babies was bene ficial, a controlled study of 50 newborn pre mature subjects was undertaken. Fluids consisting of 5% dextrose in 0.45% saline were started before the age of 6 hours by constant drip through a nasogastric plastic catheter in 24 subjects selected by a pre designed method using a table of random permutations. The average intake during the test period was 54.5 ml/kg/24 hours. The other 26 control subjects received no fluids until age 36 hours, when both groups were started on formula.
There was no alteration of symptoms of respiratory distress in the group receiving early feedings. One-half of these subjects did not lose weight while being fed the dextrose and saline solution. They promptly lost weight, however, when regu lar milk feedings were commenced.
The seven infants who died had similar pathologic findings. It was noted that three of the five in the fluid treated group also had pulmonary hyaline membranes. There were no hyaline membranes in the lungs of the two subjects deprived of water.
From this study neither beneficial nor detrimental effects of early feeding could be demonstrated by use of the criteria of dyspnea or mortality. The question of when to start to feed premature babies is still unanswered. There is need for further feeding trials, in which associations among age of commencement, nature of sub stances fed and the consequent physiologic responses, can be observed.
REFERENCES
1. Graham, R., Sampson, J., and Hester, H.
R.: I.Acute hypoglycemia in newly-born
pigs (so-called baby pig disease). Proc. Soc. Exp. Biol. & Med., 47:338, 1941. 2. Sampson, J., Taylor, R. B., and Smith, J.:
Hypoglycemic coma and convulsions in fasting baby lambs. Cornell Vet., 45:10, 1955.
3. Goodwin, R. F. W.: The concentration of blood sugar during starvation in the newborn calf and foal. J. Comp. Path.
& Therap., 67:289, 1957.
4. Hansen, J. D. L., and Smith, C. A.: Effects of withholding fluid in the immediate postnatal period. PEDIATIuc5, 12:99, 1953.
5. Smith, C. A.: Reasons for delaying feeding of premature infants. Ann. paediat. Fen niae, 3:261, 1957.
6. Rhaney, K., and MacGregor, A.: Pneu monia in newborn resulting from inhala tion of gastric contents. Arch. Dis. Child hood, 23:254, 1948.
7. Ylppo, A.: Premature children; should they fast or be fed the first days of life. Ann. paediat. Fenniae, 1:99, 1954.
8. Gleiss, J.: Ztschr. Kinderh., 76:261, 1955. (As quoted by Smith, C. A.: Reasons for delaying feeding of premature in fants. Ann. paediat. Fenniae, 3:261,
1957.)
9. Burnard, E. D.: Changes in heart sizein the dyspnoeic newborn baby. Brit. M.J., 1:1495, 1959.
10. Reardon, H. S., Field, S., Vega, L., Car rington, E., Arey, J., and Baumann, M.D.: Treatment of acute respiratory distress in newborn infants of diabetic and “¿prediabetic―mothers. (Abst.) A.M.A.J. Dis. Child., 94:558, 1957.
11. Rudolph, A. J., Hubbell, J. P., Jr., Dror
baugh, J. E., Cherry, R. B., Auld, P. A. M., and Smith, C. A.: Early versus late feedingof infantsof diabeticmothers:a controlled study. (Abst.) A.M.A.J. Dis.
Child., 98:496, 1959.
12. Bauman, W. A.: The respiratory distress
syndrome and its significance in prema
ture infants. PEDIATRICS,24:194, 1959. 13. McCance, R. A., and Widdowson, E. M.:
Physiology of the newborn animal. Lan cet, 2:585, 1957.
14. Curtis, P.: Hyaline membrane disease. J. Pediat., 51:726, 1957.
15. Landing, B. H.: Pulmonary lesions of new
born infants; a statistical study. PEDIAT
1960;26;756
Pediatrics
William Allen Bauman
INFANTS
EARLY FEEDING OF DEXTROSE AND SALINE SOLUTION TO PREMATURE
Services
Updated Information &
http://pediatrics.aappublications.org/content/26/5/756 including high resolution figures, can be found at:
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or in its
Reprints
1960;26;756
Pediatrics
William Allen Bauman
INFANTS
EARLY FEEDING OF DEXTROSE AND SALINE SOLUTION TO PREMATURE
http://pediatrics.aappublications.org/content/26/5/756
the World Wide Web at:
The online version of this article, along with updated information and services, is located on
American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.