R E S E A R C H
Open Access
Lumbar lordosis in prone position and
prone hip extension test: comparison
between subjects with and without low
back pain
Amir Massoud Arab
1*, Arash Haghighat
2, Zahra Amiri
2and Fariba Khosravi
2Abstract
Background:Prone hip extension (PHE) is a common and widely accepted test used for assessment of the lumbo-pelvic movement pattern. Considerable increased in lumbar lordosis during this test has been considered as impairment of movement patterns in lumbo-pelvic region. The purpose of this study was to investigate the change of lumbar lordosis in PHE test in subjects with and without low back pain (LBP).
Method:A two-way mixed design with repeated measurements was used to investigate the lumbar lordosis changes during PHE in two groups of subjects with and without LBP. An equal number of subjects (N= 30) were allocated to each group. A standard flexible ruler was used to measure the size of lumbar lordosis in prone-relaxed position and PHE test in each group.
Result:The result of two-way mixed-design analysis of variance revealed significant health status by position interaction effect for lumbar lordosis (P< 0.001). The main effect of test position on lumbar lordosis was statistically significant (P< 0.001). The lumbar lordosis was significantly greater in the PHE compared to prone-relaxed position in both subjects with and without LBP. The amount of difference in positions was statistically significant between two groups (P< 0.001) and greater change in lumbar lordosis was found in the healthy group compared to the subjects with LBP.
Conclusions:Greater change in lumbar lordosis during this test may be due to more stiffness in lumbopelvic muscles in the individuals with LBP.
Keywords:Low back pain, Lumbar lordosis, Movement pattern, Prone hip extension, Flexible ruler
Background
Low back pain (LBP) is a world-wide health problem and the most common and pricey musculoskeletal dis-order in the today’s societies [1, 2]. The prevalence of LBP is estimated to be between 10 and 80% depending on the population [3, 4].
During the past decades some investigators proposed the regulation of the motor system and movement pattern in evaluation and management of LBP [5, 6]. A balanced motor system is obtained from coordinated activity of synergist and antagonist muscles. Normal functioning of
the trunk depends not only on passive joint mobility, but also on normal muscular activity and central nervous system adjustment. Muscles produce and control the movement and stabilize the spine, protecting if from extreme load during functional activities [6, 7].
With regard to this point of view, repetitive move-ments and long-term incorrect postures and movemove-ments can change muscle tissue characteristics and can lead to muscle dysfunction, altered movement pattern, pain and finally movement disorders [5]. Hence, the main emphasis has been recently placed on assessment of the changed movement pattern in patients with musculo-skeletal pain and disorders such as LBP and on the im-portant of achieving normal pattern of the movement for the prevention and treatment of LBP [7–11]. * Correspondence:arabloo_masoud@hotmail.com;Amarab@uswr.ac.ir
1Department of Physical Therapy, University of Social Welfare and Rehabilitation Sciences, Evin, Koodakyar Ave, Tehran 1985713831, Iran Full list of author information is available at the end of the article
Several studies have demonstrated that LBP is associ-ated with muscle imbalance and changed activation pattern of the lumbo-pelvic muscles during different tasks [12–15].
There are some clinical tests that assess the altered movement pattern in subjects with LBP. Prone hip ex-tension (PHE) which was originally developed by Janda is a common and widely accepted test for measuring the lumbo-pelvic movement pattern [9]. The importance of PHE is that the pattern of the movement during this test has been theorized to simulate those used during func-tional movement patterns such as gait [5, 10]. In this test, a patient lies prone and lifts his leg, while keeping the knee straight. It is assumed that alterations in this pattern can decrease the stability of lumbo-pelvic region during walking and insert abnormal stress on lumbar lordosis, resulting in LBP [16]. Good reliability has been reported for PHE in detecting deviation of lumbar spine from the midline [17].
Muscle imbalance and altered activation of the lumbo-pelvic muscles has been reported during PHE test in pa-tients with chronic LBP. Coordination between muscles in the lumbo-pelvic region is thought to balance the position of the pelvis in normal posture and during the lower limb or trunk movement. It has been assumed that overactivity of the erector spinae muscles and inhib-ition or delayed activity of the gluteus maximus pro-duced anterior tilt in the pelvic and increased lumbar lordosis especially in person with lower cross syndrome. Excessive anterior pelvic tilt, lumbar rotation, lumbar hyperextension, increased lumbar lordosis and knee flexion during the PHE has been considered as abnormal movement pattern during PHE [5].
The original intent of the PHE as taught by Janda was as a screen of lumbar stability in order to observe the timing, overactivity and delayed response of the lumbo-pelvic muscles and also the timing of the lumbar spine movement with concomitant anterior pelvic tilting dur-ing PHE test. However, with regard to the altered activity of the lumbo-pelvic muscles in subjects with chronic LBP, increased lumbar lordosis during PHE test might be expected in these subjects. Oh et al. stated that pa-tients with LBP performing these exercises are often seen doing both hip and excessive lumbar spine move-ments, inducing unwanted anterior pelvic tilt and lumbar lordosis [18]. They believed that hip extension exercise may lead to a hyperlordotic lumbar angle and excessive pelvic tilt, because of instability in the lumbar and pelvis and imbalances in surrounding muscles, ac-cordingly suggested lumbar stability exercises to pre-vent unwanted lumbar spine hyperlordosis and pelvic movement substitution [18]. Arab et al. found, although not statistically significant, greater change in lumbar lordosis during prone knee flexion test (another
accepted clinical test for assessment of the lumbo-pelvic movement patterns) in subjects with LBP com-pared to those without LBP [19].
However, to our knowledge, no study has investigated the change in lumbar lordosis during PHE in patients with chronic LBP. The purpose of this study was to in-vestigate the change in the size of lumbar lordosis dur-ing PHE in subjects with and without chronic LBP.
Methods Subjects
A two-way mixed design was used to investigate the lumbar lordosis changes during PHE in two groups of men: men with chronic non-specific LBP (N= 30, age age: 33.6 (SD = 7.27); range: 22-47 years old, aver-age height: 163.1 (SD = 8.25) cm, averaver-age weight: 59.5 (SD = 10.34) kg) and men with no history of LBP (N= 30, average age: 22.33 (SD = 1.93); range: 19-27 years old years old, average height: 177.42 (SD = 5.54) cm, average weight: 71.9 (SD = 8.98) kg).
The subject population in this study was a sample of convenience. The LBP patients were referred by physio-therapy clinics and orthopedic specialist. The patients were included if they had a history of non-specific LBP for more than six weeks’duration before the study date, or had intermittent (on and off ) LBP with at least three previous episodes each lasting more than one week, during the year before the study [20]. The control group were evaluated and found to have no complaint of any pain in their pelvis, low back, thoracic and lower extremities.
The exclusion criteria in both groups were history of dyspnea, history of hip pain, dislocation or fracture, history of lumbar spine surgeries, history of anterior knee ligament injury or rupture, history of anterior knee pain, recent episodes of ankle sprain, leg length difference of more than 1 cm, inability to perform ac-tive PHE without pain, history of lower extremity injury in the past 3 months, shortness of hip flexors, positive neurological symptoms and cardiopulmonary disorders. Each eligible subject was enrolled after signing an in-formed consent form approved by the human subjects committee at the University of Social Welfare and Re-habilitation Sciences. Ethical approval for this study was granted from the internal ethics committee at the University of Social Welfare and Rehabilitation Sciences.
Procedures
Measuring lumbar lordosis
A standard flexible ruler was used to measure the size of lumbar lordosis in prone position before and after PHE. For this purpose, the position of subject was prone lying on a treatment table with the arms along the sides. The spinous process of L1 and base of sacrum was located by palpation and marked with removable stickers. A stand-ard flexible ruler was fitted in subject’s lumbar curve, over the lumbar spinous processes of L1–S1. The curve of the flexible ruler, resembling the degree of subject’s lumbar curvature, was graphed on a paper, noting where the two reference points for L1 and S1 were located. The method explained by others [20–24] was used to quantify the size of lumbar lordosis (Ɵ). Two points on the curve, depicting L1 and S1, were connected by a line (L). A vertical line (H), representing the height of the lumbar curve, bisected line L. The length of each line was computed in millimeters, and the values were used in the following formula to calculate the degree of lumbar lordosis
θ ¼ 4 Arctan 2H½ ð =LÞ
A very high correlation (r= 0.92) has been found be-tween size of lumbar lordosis measured by a flexible ruler and from lumbar X-rays [20–24]. In the past, the reliability of flexible curve for measurement of lumbar lordosis has been established [20].
Ethical approval
This research was reviewed and was approved by the Human Subject Committee at University of Social Welfare and Rehabilitation Sciences.
Data analysis
Statistical analysis was performed using SPSS version 16.00. We tested the difference in lumbar lordosis be-tween positions and groups by using two-way mixed-design ANOVA, accounting for position (prone-relaxed vs. PHE), health status (LBP vs. no LBP) and interaction of position and health status effects. Independent t-test was used to compare the amount of change in lumbar lordosis between positions (PHE minus prone-relaxed) across subjects with and without LBP. Statistical signifi-cant was attributed to P value less than 0.05.
Results
The demographic data for the subjects is showed in Table 1. Statistical analysis showed no significant differ-ence in subjects’age (P= 0.15), height (P= 0.28), weight (P= 0.56) and BMI (P= 0.26) among the two groups.
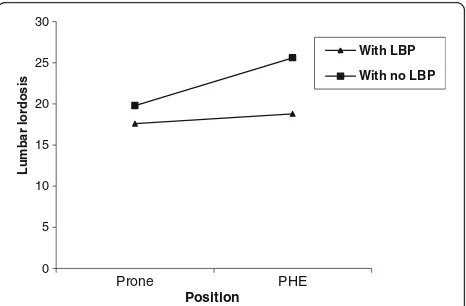
Figure 1 depicts the average measurement scores for lumbar lordosis in each position for two groups. Detailed descriptive statistics (Mean SD) are presented in Table 2.
The result of two-way mixed-design analysis of variance revealed significant health status by position interaction effect for lumbar lordosis at α= 0.05 (F = 27.41, P< 0.001). The main effect of test position on lumbar lor-dosis was statistically significant (F = 63.47, P< 0.001). Overall, the lumbar lordosis was significantly greater in the PHE compared to prone-relaxed position in both subjects with and without LBP (Table 2). The health status had significant effect of on lumbar lordosis (F = 25.30,P< 0.001). The mean difference in lumbar lordo-sis as measured by flexible curve between positions was 1.2 and 5.8 for subjects with LBP compared to those without LBP respectively. The amount of difference in positions was statistically significant between two groups (P< 0.001).
Discussion
The current study compared the change in lumbar lor-dosis during PHE test between subjects with and with-out LBP. The results of this study indicate an increase in the size of lumbar lordosis during PHE compared to prone-relaxed position regardless of health status. How-ever, greater change in lumbar lordosis was found in the healthy group compared to the subjects with LBP.
In this study, none of the subjects reported that pain was a limiting factor to perform PHE test, so, direct ef-fects of pain can be minimized. However, nociception can influence the lumbar movement.
Table 1Demographic data of the subjects in each group (Mean ± SD)
Variables With no LBP (n= 30) With LBP (n= 30)
Age (years) 22.33 ± 1.93 33.6 ± 7.27
Weight (kg) 75.23 ± 22.91 59.5 ± 10.34
Height (cm) 177.00 ± 5.54 163.1 ± 8.25
BMI (kg/m2) 21.05 ± 2.26 22.31 ± 3.31
BMIBody Mass Index
0 5 10 15 20 25 30
Prone PHE
Lum
b
ar
l
o
rdosis
Position
With LBP
With no LBP
Lumbar extension and anterior rotation of the pelvis are often observed during hip extension motion. In-crease in the size of lumbar lordosis during PHE found in both groups can be attributed to the accompanied lumbar extension during extension of hip. In theory, it is proposed that excessive anterior pelvic tilt, lumbar hyperextension and increased lumbar lordosis during the PHE are commonly seen as abnormal movement patterns in patients with chronic LBP. Investigators at-tributed these to muscle imbalance and changed activa-tion of the lumbo-pelvic muscles [5]. They attributed excessive lumbar extension and hyperlordosis during PHE to deficit in controlling anterior pelvic rotation during hip extension because of muscular dysfunction in the lumbo-pelvic region [5, 18].
Sahrmann [5] proposed the concept of "relative flexi-bility or stiffness" that has been linked to uncontrolled movement, pain and pathology by causing direction re-lated stress and strain during different functional move-ments in the patients with LBP. She suggested that increased stiffness of the anterior supporting structures of the thigh, hip and lumbar spine can result in compen-satory exaggerated anterior pelvic tilt with lumbar exten-sion motion during knee flexion or prone hip extenexten-sion. In this study, stiffness in thigh and anterior supporting structures of the lumbar spine was not measured and just change in lumbar lordosis during PHE was measured.
Previous studies have demonstrated that patients with chronic or recurrent LBP use different strategies which are different from common one´s [25]. Scholtes et al. [25] found that during prone hip lateral rotation, sub-jects with LBP demonstrated a greater maximal lumbar-pelvic rotation angle compared to those without LBP, as the lumbar-pelvic region may move more frequently during the early ranges of lower limb movement in daily activities.
In this study, lumbar lordosis was significantly higher during PHE compared to prone relaxed position in jects with or without LBP. However, we found that sub-jects with LBP, although not statistically significant, have a lower degree of lumbar lordosis change compared with those without LBP. The reason for this may be due to the increased hamstring stiffness and tightness in indi-viduals with LBP. Previous studies have supported the change in mechanical behavior, extensibility and stiffness
of hamstring muscles in subjects with LBP [20, 26–28]. Van Wingerden et al. considered hamstring muscle stiff-ness in patients with LBP as a compensatory mechanism to reduce pelvic instability and gluteal muscle weakness [29]. Investigators have attributed the increased activity of trunk muscles found in patients with LBP to func-tional adaptations following reduced lumbo-pelvic stabil-ity. Arab et al. [30] showed an increased EMG activity of the hamstring muscles during PHE in subjects with LBP compared to those without LBP. Because the hamstring muscle attaches to the ischial tuberosity, it is hypothe-sized that tightness and stiffness of these muscles may induce posterior pelvic tilt. However, in this study we did not measure the hamstring stiffness during PHE.
Some studies have found that patients with LBP have measurably greater stiffness than when they have no pain [31]. Others found that chronic LBP limits the maximal range of lumbar extension more than acute LBP [32]. The fact that change in lumbar lordosis during hip extension was smaller in patients with LBP com-pared to those without LBP may be due to the greater stiffness in subjects with chronic LBP.
Another area of concern in this topic may be fear-avoidance belief and pain fear-avoidance in LBP. Fear may protect the individual from impending danger as it insti-gates defensive behavior. A large body of research re-vealed that LBP patients with pain-related fear report increased disability [33]. According to the fear-avoidance model of LBP, chronic LBP patients typically show sub-maximal performance and limited range of motion dur-ing physical activities such as straight leg raise, hip extension, trunk extension/flexion, and etc [11, 34, 35]. These findings suggest that performance during lumbo-pelvic extension, as measured by lumbar and hip excur-sions, may be influenced by individual differences in pain-related fear. Fritz and colleagues [35] have previ-ously reported significant correlations between mea-sures of fear avoidance behavior and some physical impairment that included lumbar range of motion (flexion, extension, average side bending, and average straight leg raise).
Lesser change in lumbar lordosis during PHE move-ment pattern in patients with LBP; found in this study, might be due to more limited hip and lumbar extension in these subjects as a results of fear-avoidance.
Table 2The (Mean ± SD) scores of lumbar lordosis in each position for subjects with and without LBP
Variable Group Position Difference
between positions p -value
Prone PHE
Lumbar lordosis (degree) With LBP (N = 30) 17.6 ± 2.07 18.8 ± 2.05 1.2 0.000
With no LBP (N= 30) 19.8 ± 4.02 25.6 ± 5.9 5.8 0.000
p-value 0.23 0.000 0.000
PHEProne hip extension
Some investigators proposed “guarding mechanism” during movement and activities in patients with LBP and stated that LBP patients show "guarded" movements during functional activities) [36]. This guarded move-ment during PHE may decrease lumbar lordosis changes in subjected with LBP [37].
Limitations
We acknowledge some limitations. In this study the pa-tients with chronic non-specific LBP were examined and other LBP patients (specific or acute LBP) were not ex-amined. One other limitation of this study was this issue that LBP subjects were not categorized based on move-ment system impairmove-ment-based classified for LBP as de-scribed by Sahrmann [5]. It is suggested to investigate the lumbar lordosis change in LBP patients with different movement system impairment-based categories.
Another limitation of the study is that the original in-tent of the PHE as taught by Janda was as a screen of lumbar stability in order to observe the timing, over-activity and delayed response of the lumbo-pelvic mus-cles and also the timing of the lumbar spine movement with concomitant anterior pelvic tilting during PHE test. In this study we did not measure the electromyography (EMG) activity of the stabilizing and prime mover mus-cles during PHE to find the pattern of musmus-cles recruit-ment. Another area of concern is that in this study, we did not measure lumbar -pelvic kinematics during PHE. Another issue is that the subjects with LBP were sub-stantially older on average than those without LBP. This should be considered as the limitation in this study.
Conclusion
This study investigated the change in lumbar lordosis during PHE test between subjects with and without LBP. The results of this study indicate an increase in the size of lumbar lordosis during PHE compared to prone-relaxed position in subjects with and without LBP. How-ever, greater change in lumbar lordosis was found in the healthy group compared to the subjects with LBP.
Abbreviations
LBP:Low back pain; PHE: Prone hip extension
Acknowledgement
The authors would like to thank Physical Therapy department at University of Social Welfare and Rehabilitation Sciences.
Funding
Not applicable
Availability of data and materials
Not applicable
Authors’contributions
AMA contributed to conception, design, analysis, interpretation of data and drafting the manuscript. AH carried out the data collection. ZA participated
in design and drafting the manuscript. FK participated in analysis and helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable
Ethics approval and consent to participate
This research was reviewed and was approved by the Human Subject Committee at University of Social Welfare and Rehabilitation Sciences.
Source of Support
Partially supported by the University of Social Welfare and Rehabilitation Sciences
Institutional review board
Human subject committee of University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author details
1Department of Physical Therapy, University of Social Welfare and Rehabilitation Sciences, Evin, Koodakyar Ave, Tehran 1985713831, Iran. 2
University of Social Welfare and Rehabilitation Sciences, Evin, Tehran, Iran.
Received: 16 March 2016 Accepted: 9 March 2017
References
1. Marras WS, Allread WG, Burr DL, Fathallah FA. Prospective validation of a low-back disorder risk model and an assessment of ergonomic interventions associated with manual materials handling tasks. Ergonomics. 2000;43:1866–86.
2. Lahiri S, Markkanen P, Levenstein C. The cost-effectiveness of occupational health interventions: preventing occupational back pain. Am J Ind Med. 2005;48(6):515–29.
3. Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998;77(3):231–9.
4. Gilgil E, Kacar C, Butun B, Tuncer T, Urhan S, Yildirim C. Prevalence of low back pain in a developing urban setting. Spine. 2005;30:1093–8. 5. Sahrmann S. Diagnosis and treatment of movement impairment syndromes.
1. Missouri: Mosby. Inc; 2002. p. 121–92.
6. Jull GA, Janda V. Muscles and motor control in low back pain:Assessment and management. In: Twomey LT, Taylor JR, editors. Physical Therapy of the Low Back. New York: Chuchill Livingstone; 1987. p. 253–78.
7. Norris CM. Spinal stabilisation 5. An exercise programme to enhance lumbar stabilisation. Physiotherapy. 1995;81(3):138–46.
8. Cholewicki J, Van Dieen JH, Arsenault AB. Muscle function and dysfunction in the spine. J Electromyoger Kinesiol. 2003;13(4):303–4.
9. Janda V. On the concept of postural muscles and posture in man. Aust J Physiother. 1983;29:83–4.
10. Janda V. Pain in the locomotor system-A broad approach. Aspects of Manipulative Therapy. Melbourne: Churchill Livingstone; 1985. p. 148–51. 11. O'Sullivan P, Phyty D, Twomey L, Allison G. Evaluation of specific stabilizing
exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22:2959–67.
12. Hodges P, Moseley G. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13:361–70. 13. Hungerford B, Gilleard W, Hodges P. Evidence of altered lumbopelvic muscle
recruitment in the presence of sacroiliac joint pain. Spine. 2003;28:1593–600. 14. Leinonen V, Kankaanpaa M, Airaksinen O, Hanninen O. Back and hip
extensor activities during trunk flexion/extension: Effects of low back pain and rehabilitation. Arch Phys Med Rehabil. 2000;81:32–7. 15. Newcomer K, Jacobson T, Gabriel D, Larson D, Brey R, An K. Muscle
16. Vogt L, Pfeifer K, Banzer W. Neuromuscular control of walking with chronic low-back pain. Man Ther. 2003;8:21–8.
17. Murphy D, Byfield D. Inter-examiner reliability of the hip extension test for suspected impaired motor control of the lumbar spine. J Manipulative Physiol Ther. 2006;29:374–77.
18. Oh JS, Cynn HS, Won JH, Kwon OY, Yi CH. Effects of performing an abdominal drwing-in maneuver during prone hip extension exercises on hip and back extensor muscle activity and amount of anterior pelvic tilt. J Orthop Sports Phys Ther. 2007;37(6):320–24.
19. Arab AM, Talimkhani A, Karimi N, Ehsani F. Change in lumbar lordosis during prone lying knee flexion test in subjects with and without low back pain. Chiropr Man Therap. 2015;23:18.
20. Nourbakhsh MR, Arab AM. Relationship between mechanical factors and incidence of low back pain. J Orthop Sports Phys Ther. 2002;32:447–60. 21. Link CN, Nicholson GG, Shaddeau SA, Birch R, Gossman MR. Lumbar
curvature in standing and sitting in two types of chairs: relationship of hamstring and hip flexor muscle length. Phys Ther. 1990;70:611–8. 22. Nourbakhsh MR, Arab AM, Salavati M. The relationship between pelvic
cross syndrome and chronic low back pain. J Back Musculoskeletal Rehabil. 2006;19:119–28.
23. Youdas JW, Garrett TR, Harmsen SS. Lumbar lordosis and pelvic inclination of asymptomatic adults. PhysTher. 1996;76:1066–81.
24. Youdas JW, Garrett TR, Egan KS, Therneau TM. Lumbar lordosis and pelvic inclination in adults with chronic low back pain. Phys Ther. 2000;80:261–75. 25. Scholtes SA, Gombatto SP, Van Dillen LR. Differences in lumbopelvic motion
between people with and people without low back pain during two lower limb movement tests. Clin Biomech. 2009;24(1):7–12.
26. Arab AM, Nourbakhsh MR. Hamstring muscle length and lumbar lordosis in subjects with different lifestyle and work setting: Comparison between individuals with and without chronic low back pain. J Back Musculoskelet Rehabil. 2014;27(1):63–70.
27. Johnson EN, Thomas JS. Effect of hamstring flexibility on hip and lumbar spine joint excursions during forward-reaching tasks in participants with and without low back pain. Arch Phys Med Rehabil. 2010;91(7):1140–42. 28. Kim MH, Yoo WG, Choi BR. Differences between two subgroups of low back
pain patients in lumbopelvic rotation and symmetry in the erector spinae and hamstring muscles during trunk flexion when standing. J Electromyogr Kinesiol. 2013;23(2):387–93.
29. van Wingerden JP, Vleeming A, Kleinrensink GJ, Stoeckart R. The role of hamstring in pelvic and spinal function. In: Vleeming A, Mooney V, Dorman T, et al., editors. Movement, Stability and Low Back Pain. The Essential Role of the Pelvis. New York: Churchill Livingston; 1997. p. 207–10.
30. Arab AM, Ghamkhar L, Emami M, Nourbakhsh MR. Altered muscular activation during prone hip extension in women with and without low back pain. Chiropr Man Therap. 2011;19:18.
31. Latimer J, Lee M, Adams R, Moran CM. An investigation of the relationship between low back pain and lumbar posteroanterior stiffness. J Manipulative Physiol Ther. 1996;19:587–91.
32. Evcik D, Yucel A. Lumbar lordosis in acute and chronic low back pain patients. Rheumatol Int. 2003;23:163–5.
33. Boersma K, Linton SJ. How does persistent pain develop? An analysis of the relationship between psychological variables, pain and function across stages of chronicity. Behav Res Ther. 2005;43:1495–507.
34. Al-Obaidi SM, Nelson RM, Al-Awadhi S, Al-Shuwaie N. The role of anticipation and fear of pain in the persistence of avoidance behavior in patients with chronic low back pain. Spine. 2000;25(9):1126–31.
35. Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82(10):973–83.
36. van der Hulst M, Vollenbroek-Hutten MM, Rietman JS, Schaake L, Groothuis-Oudshoorn KG, Hermens HJ. Back muscle activation patterns in chronic low back pain during walking: a "guarding" hypothesis. Clin J Pain. 2010;26(1):30–7.
37. Brox J. Disability, pain, psychological factors and physical performance in healthy controls, patients with sub-acute and chronic low back pain: a case-control study. J Rehabil Med. 2005;37:95–9.
• We accept pre-submission inquiries
• Our selector tool helps you to find the most relevant journal • We provide round the clock customer support
• Convenient online submission • Thorough peer review
• Inclusion in PubMed and all major indexing services • Maximum visibility for your research
Submit your manuscript at www.biomedcentral.com/submit