The Natural
History
of Neonatal
Jaundice
Coleen
Kiviahan,
MD, and Elizabeth
J. P. James,
MD
From the Departments of Family and Community Medicine, Child Health, and Obstetrics, University of Missouri School of Medicine, Columbia
ABSTRACT. The relationship between infant feeding type and the occurrence and natural history of neonatal jaundice in term newborn infants has been studied. A
retrospective chart review of 124 records confirmed ear-her reports indicating that jaundice is recognized more often in breast-fed than in formula-fed infants. A
pro-spective cohort study of 140 term newborn infants was
conducted using the Minolta Air-Shields transcutaneous
jaundice meter. For 3 weeks, 115 white infants and 25
black infants were followed at predetermined intervals. The peak jaundice meter readings were higher and the elevated levels lasted longer in breast-fed than in for-mula-fed infants. Formula-fed infants’ readings returned to base-line levels in eight days whereas the readings were still elevated in breast-fed infants when the study ended on the 21st day. Black infants had higher trans-cutaneous readings than white infants due to their deeper skin pigmentation, but otherwise they followed a course identical with that of the white babies. The distribution ofjaundice in the white infants was bimodal; in approx-imately one fourth of the breast-fed infants, the jaundice meter readings reached levels corresponding to bilirubin values >13 mg/dL whereas the remaining three fourths followed a pattern similar to that of the formula-fed infants. It can be concluded that human milk feeding is associated with more prolonged hyperbilirubinemia than formula-feeding in normal term infants. Pediatrics 1984; 74:364-370; jaundice, newborn, transcutaneous jaundice, breast-feeding.
Jaundice in the newborn is a common but poorly understood problem, and it is often of uncertain clinical significance. Approximately 50% of term newborns become visibly jaundiced in the first week of life; 10% of the newborns with jaundice undergo
Received for publication Aug 1, 1983; accepted Dec 23, 1983.
This work was carried out while Dr Kivlahan was a Fellow in the Robert Wood Johnson Family Practice Academic Fellowship Program.
Reprint requests to (C.K.) Department of Family and Commu-nity Medicine, University of Missouri School of Medicine, Co-lumbia, MO 65212.
PEDIATRICS (ISSN 0031 4005). Copyright © 1984 by the American Academy of Pediatrics.
phototherapy.1’2 Early work on neonatal jaundice dealt with the importance ofconjugated and uncon-jugated bilirubin,3’4 abnormalities of bilirubin ex-cnetion,5 and Rh isoimmunization.6 Beginning in 1963, case reports79 of breast-fed infants with pro-longed jaundice began to appear, leading to general acceptance of the phenomenon of “breast milk jaundice.” These infants had more severe, longer lasting jaundice. Even in these unusual babies, del-etenious effects of the jaundice did not seem to occur, and little more was done to study the natural history of neonatal jaundice until recently.
It is generally agreed that “physiologic jaundice” peaks at 72 hours1’2’1#{176}and diminishes rapidly there-after. Only a small number of infants are found to have serum bilirubin levels >12.9 mg/dL in the first several days of life.10 However, there is a difference of opinion about the natural history of jaundice in breast-fed as compared with formula-fed in-fants.2’’12 Winfield and MacFaulT3 reported that 2.4% of breast-fed infants had persistent hypenbili-rubinemia at 3 weeks of age. Recently, Maisels and Giffond’4 carried out a prospective study on term
infants and found no difference in mean bilirubin
level on the third day of life in breast-fed and formula-fed infants. He did observe, however, that more than 80% of infants with serum bilirubin levels >12.9 mg/dL in the first four days of life were breast-fed. In another prospective study of 135
infants during the first four days of life, Kuhr and
Paneth’5 noted that breast-feeding was associated with an almost four times greater incidence of jaundice than formula-feeding. However, serum
bil-irubin levels were not measured systematically, but were measured only at the discretion of the pa-tients’ physician.
Existing studies ofthe natural history of neonatal jaundice have suffered from two major problems.
First, the duration of follow-up has generally been
levels have generally been determined at the discre-tion of the physician based on clinical assessment of skin color. Variability in the clinical expression of jaundice on closer surveillance of breast-fed
in-fants for jaundice, therefore, could create bias in
the detection of hypenbilirubinemia.
In the present study, jaundice levels were mea-sured at regular, predetermined intervals in term breast-fed and formula-fed infants during the first 21 days of life. Because it was both impractical and painful to perform repeated heelstick punctures for serum bilirubin values on otherwise healthy infants, we used a Minolta Air-Shields transcutaneous jaun-dice meter’9 to approximate serum bilirubin levels. The goal of the study was to define the natural course of neonatal jaundice oven the first 3 weeks of life and to detect any differences in the
course of neonatal jaundice associated with type of
infant feeding.
The study is in three parts: (1) an initial
netno-spective study was conducted by chart reviews to
estimate the frequency of jaundice in breast-fed and formula-fed infants in our patient population; (2) the jaundice meter was calibrated with serum bilirubin levels in our laboratory to evaluate its accuracy and limitations; (3) a cohort of infants was followed from birth to 21 days of age with periodic measurement of jaundice.
METHODS
Retrospective Study
The records of 161 newborn infants bonn in 1980 at the University of Missouri Health Sciences Cen-ten were reviewed retrospectively to determine the frequency ofjaundice in breast-fed and formula-fed infants in the first 6 weeks of life. Thirty-seven infants were excluded because of inadequate birth information or the presence of secondary forms of hyperbilirubinemia (hemolysis, sepsis, hypoxia, on cephalhematoma). Of the remaining 124 infants, all were >37 and <42 weeks of gestation as mea-sured by Dubowitz examination, had Apgar scores >6, peripheral hematocnit values between 50% to 70% and negative findings on Coombs’ test.
All infants were hospitalized in the same nursery. Weights were recorded daily. Serum bilirubin levels were drawn by physicians only when there was clinical suspicion ofjaundice. Type of feeding, din-icaljaundice, frequency and level of serum bilirubin determinations, weight loss, and the number of return visits during the first 6 weeks of life were recorded for each study infant. Return visits were measured because breast-fed infants would have more opportunities to be noted to be clinically jaundiced if for some reason they had more
outpa-tient visits in the first few weeks of life.
x2
tests and analysis of covariance were used to test for differences. A P value < .05 was considered signifi-cant.Prospective Study
This project was approved by the Human Studies Committee of the University of Missouri School of Medicine, and individual informed consent was ob-tamed from a parent of each infant studied. After completion of the retrospective study, a prospective cohort study was carried out to determine the nat-ural history ofjaundice in newborns during the first 21 days of life. The Minolta transcutaneous jaun-dice meter was chosen as a practical alternative to repeated serum measures for use in this study.
The jaundice meter was standardized on 32 white infants in the intensive care nursery chosen because they were having frequent bilirubin levels per-formed. Sixty concurrent readings were collected. The concurrent reading was defined as a tnanscu-taneous jaundice measurement from the infant’s forehead taken within one hour of a measurement of serum bilirubin level. Infants receiving photo-therapy were excluded. Total serum bilirubin
con-centrations were measured by the Neonatal
Labo-ratory using the DuPont automatic clinical analyzer (ACA III Instruction Manual, DuPont Co, Clinical Systems Division, Wilmington, DE, 1980). A linear regression equation and correlation coefficient (Pearson’s r) were calculated from the data. Be-cause the mean gestational age of the babies studied was 34 weeks, the bilirubin levels that correspond to specific meter readings may differ slightly from those of term babies.
Following meter standardization, the cohort study was performed on healthy term newborns from the University of Missouri Health Sciences
Center well baby nursery from July 1982 to June 1983. There were 115 white and 25 black infants in the cohort study. Sample size necessary to detect a 40% difference between breast-fed and formula-fed newborns with a type I error of 0.5 and a type II
error of 0.1 was calculated prior to beginning the
study to be 114 for each racial cohort.2#{176}Thus, only the group of white infants was large enough to meet these standards. Infants with hypoxia, acidosis, Ap-gan scone <6, sepsis, Coombs’ positive hemolytic anemia, polycythemia, or cephalhematoma were ex-eluded to reduce the likelihood of contamination of the study by infants with secondary
hypenbilirubi-nemia. Fifteen infants with racial backgrounds
other than white on black were excluded because of small sample size or racial heterogeneity.
Trans-cutaneous jaundice levels and weights were
mea-100 (81%) 19 (15%) 5 (4%) 57 (46%)
67 (54%) 78 (63%) 40 (32%) 6 (5%)
35/78 (45%) 4/40 (10%)
29/78 (37%) 4/40 (10%)
29/78 (37%) 4/40 (10%) surements were made by one of the authors or a research assistant during the first few days in the hospital and at subsequent home visits after hos-pital discharge. Serum bilirubin levels were deter-mined only at the discretion of the patients’ mdi-vidual physicians. The number of serum bilirubin levels measured was recorded. Eight infants under-went phototherapy while enrolled in the study, all for less than two days. The transcutaneous jaundice readings were not omitted because of phototherapy; either the days the infants were receiving photo-therapy did not correspond to the predetermined study days or the index was measured under a forehead patch that excluded the light from this area.
Feeding choice was determined by the mother. There were no attempts to interfere with this de-cision, but a request was made to use only one type of milk for the first 21 days of life. Infants were followed as either breast- or formula-fed.
RESULTS
Retrospective Study
The results are summarized in Table 1. Sixty-three percent of the 124 newborns were breast-fed, 32% were formula-fed, and 5% received both breast milk and formula in the first 6 weeks of life.
This compares with 58% of infants breast-fed at birth in the United States in 1981.21 Examination of the medical records completed by nurses and physicians showed that breast-fed infants were noted clinically to be jaundiced significantly more often than formula-fed infants (45% v 10%, P <
.05). Infants fed human milk were also three times more likely to have serum bilirubin measured than
TABLE 1. Retrospective Study Findings (N = 124) Race
White Black Other Sex
Male Female Feeding preference
Breast Formula Both
Clinical jaundice noted Breast
Formula
Had at least 1 bilirubin drawn Breast
Formula
Serum bilirubin >10 mg/dL Breast
Formula
formula-fed infants. Almost four times as many breast-fed infants as formula-fed infants had a se-rum bilirubin value >10 mg/dL (37% v 10%, P <
.05).
Prospective Study
The regression line calculated from the concur-rent readings of the transcutaneous jaundice index and the serum bilirubin values is shown in Fig 1. The Pearson correlation coefficient was .89, show-ing excellent agreement. Two reading levels will be referred to frequently in the text: a jaundice meter index of 17, which corresponds to a serum bilirubin value of 9 to 10 mg/dL and an index of 20, which corresponds to a serum bilirubin value of approxi-mately 12 to 13 mg/dL. An index of 20 on a serum bilirubin value of 12.9 mg/dL has been used by other authors2’19’22 to define “hypenbilirubinemia,” jaundice in the range of clinical concern.
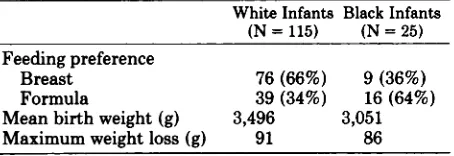
Although we standardized the meter only on white infants, we noted and others18’19’22 have noted that the meter readings vary with skin pigmenta-tion. There have been no large studies reporting standardization of the meter on black infants. For these reasons, as well as because of the different sizes of the two groups, data from white and black infants will be presented separately. The predomi-nance of white infants in the study closely approx-imates the racial distribution in our community as a whole. The distribution of feeding preference closely matches that of the retrospective study and of national figures for the immediate neonatal pe-nod.2’ The characteristics of the infants in the prospective study are shown in Table 2.
White Infants
The natural history of jaundice in white infants is shown in Fig 2. The peak jaundice level as mea-sured by the meter in the breast-fed infants was 15.2 (approximately 7.5 mg/dL); in formula-fed in-fants it was 14.6 (approximately 7 mg/dL), not a statistically significant difference. However, as shown in Fig 2, jaundice lasted longer in breast-fed infants with statistically significant differences at days 6, 8, 14, and 21. In addition, the meter readings still were abnormal at day 21 in the breast-fed infants whereas they had returned to base line at day 8 in the formula-fed infants.
0
00 0
0
cx:, o
00
0
R 0.89 0 SE : 1.77 R2 0.79 Y s 8.3 . 0.9 (X)
00 0 00
15
13
11#{149}
9.
7.
0 0 0 0 0 0
0
2:0 4.0 6:0 8:0 10.0 ‘ 12.0 14.0
Serum
BilIrubIn
(mg/dI)
16.0 18.0 20.0
27
‘C
25
C
23
221 V
C
20
. 19
3
0
C
3 U
C
I-2
Fig 1. Linear regression scattergram.
TABLE 2. Characteristics of Infants in Prospective Study
White Infants Black Infants
(N
=
115) (N=
25)Feeding preference
Breast 76 (66%) 9 (36%)
Formula 39 (34%) 16 (64%)
Mean birth weight (g) 3,496 3,051
Maximum weight loss (g) 91 86
similar to those of formula-fed infants. A histogram of the readings from breast-fed infants at day 8 showed a bimodal distribution. The mean jaundice index of the two groups of breast-fed infants was significantly different (18 v 10, P < .05).
Weight loss and dehydration have been proposed as possible explanations for the increased jaundice in breast-fed infants. In this study, weight loss was measured as the difference between the birth weight and the lowest weight recorded in the first 21 days of life. Infants with the greatest weight losses were no more likely to be breast-fed than formula-fed, nor were they more likely to be jaundiced. Approx-imately 16% of each feeding group lost more than 170 g (5% of birth weight) through the observation period.
As indicated earlier, serum bilirubin levels were not measured as part of the study. Thus, the fre-quency with which physicians ordered determina-tion of serum bilirubin levels became a measurable outcome of clinically apparent jaundice. Though not statistically significant, a single serum bilirubin level was drawn more frequently in breast-fed as compared with formula-fed infants (23.6% v 15.3%, P = .15). The mean serum bilirubin level of
for-mula-fed infants was 8.8 mg/dL with a range of 5.5 to 10.7 mg/dL whereas the mean serum bilirubin of breast-fed infants was 11.3 mg/dL with a range of 6.5 to 17 mg/dL.
Eight infants underwent phototherapy; all were breast-fed. There were seven white infants in this group; one infant was black.
Black Infants
Eighteen percent (25/140) of our sample was black, a figure that closely parallels the distribution of blacks in our hospital deliveries and in our corn-munity. The natural history ofjaundice in the black infants closely paralleled that in the white infants, with statistically significant differences found at days 6, 8, 14, and 21. The average skin reflectance readings were higher in black than in white infants because of the increased skin pigmentation in the black infants (Fig 4). Like white babies, black breast-fed infants were found to have a greater duration of jaundice than formula-fed infants (Fig 5). In this instance, statistically significant differ-ences were found every time readings were made throughout the study.
DISCUSSION
16#{149}
15#{149}
S Formula Fed (n 39)
#{174}Breast Fed (n = 76)
8
7- * p‘ .05
-a;
;
l 4 ‘ l’o 1’l 12 13 16 17 18 19 20 21Days
Fig 2. Natural history ofjaundice in white breast-fed and formula-fed infants.
#{174}Breast Fed, Peak2O (n=16)
0 Breast Fed, Peak20 (n=60) S Formula Fed, Peak20 (n=39)
No Formula Fed, Peak 20
21
20
19
18
17
16
15
14
13
12
11
10 9
8
12345678
T I I I I I I I I I I
9 101112131415161718192021
Days
Fig 3. Natural history of white infants with peak jaundice indices >20 and <20 (12.9 mg/dL).
‘C 9 .5 C
9
U 14
.5
g
9
-, 12 9
3
0 ii.
9
C
0 10
3
U 0
C
9 I-.
C
9 9
‘C .5
C
.
U
0
C 3
9
-)
0 3 0 S
C
S
3 U
S
C
S
C
S
S
population, suffer from the same design problems as did the earlier studies. The prospective study resolves these difficulties. We found no difference in the peak jaundice level at day 4 in breast- and formula-fed infants, a finding that is in agreement with the two recent prospective studies14”5 of in-fants through the fourth day of life. However, after day 4, two important differences were noted. First, breast-fed infants had jaundice levels that stayed elevated from day 4 through day 21 compared with formula-fed infants. In fact, the breast-fed infants’ readings did not return to their base-line day 1 levels by day 21, the final day ofthe study. Formula-fed infants’ readings fell below the day 1 measure-ment by day 8. This supports the clinical suspicion that breast-fed infants are jaundiced beyond the
.-. White infants (n 1 15) .-. Black Infants (n =25)
* p < .05
1 23 456 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
Days
Fig 4. Natural history of jaundice in white infants compared with black infants.
21
20 -#{174} Breast Fed (n =
9)
19 .- -S Formula
Fed (n
16)
18
17
16
15
14
13
12
11
* p<.05
*
I 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
Days
Fig 5. Natural history ofjaundice in black infants.
18 K
e
. 17
16
.5
C 15
3 S
2 14
S 13 S
I 1E
‘C S
V C
S
U V
C 3
S
-,
S 30
S C S
3 U S C S
I-more closely approximated those of formula-fed infants.
It is not known what features these more jaun-diced infants had in common, but the present find-ings add to the growing awareness of the need for a redefinition of physiologic jaundice. None of the
infants in this study required subsequent admission
for phototherapy on for evaluation of secondary hyperbilirubinemia. It is doubtful that such levels of jaundice indicate serious illness. This is impor-tant in light of the recent attention given the din-ical practice of phototherapy for elevated serum bilirubin levels in otherwise healthy newborns.23’24 Watchko and Oski23 questioned the rationale
un-derlying the use of photothenapy as standard clini-cal practice in this population. Although we did not
address this issue in our study, if the greater
mci-dence of jaundice in breast-fed infants is physio-logic and the biliruhin concentrations seldom reach “dangerous” levels, then perhaps serial observa-tions of the newborn should replace therapeutic interventions. Further, the increased family anxiety and separation, cost, and occasional cessation of breast-feeding that results from hospitalization for phototherapy make it important that this practice be investigated in term, otherwise healthy infants.
the outpatient setting because it is convenient,
painless, and less expensive than serum bilirubin
determinations. It is also well accepted by families. The jaundice meter was quite useful for following a newborn with serial measurements from birth through the first 1 to 2 weeks of life. The meter must be calibrated in each individual nursery, and certainly for each racial group. It might be most appropriate to correlate a transcutaneous reading with a serum bilirubin level in each newborn when the skin index begins to increase. The meter read-ings could then be followed until they reached a predetermined level above which serum bilirubin would be measured, remembering that the range of bilirubin values corresponding to a single reading on the jaundice meter is rather wide. Maisels and Conrad’7 recently calculated the negative predictive value of normal meter readings, the probability that a negative test predicts the absence of hyperbiliru-binemia, to be 100%. Our study also indicates that the jaundice meter has an acceptably low false-negative rate. We found it especially useful in the outpatient evaluation of neonatal jaundice.
SUMMARY
To determine the natural history of jaundice in healthy, full-term infants, 1 15 white and 25 black infants were followed during the first 3 weeks of life. Breast-feeding was associated with neonatal jaundice that lasted longer and reached higher peak levels. We believe that this is not only a statistically but also a clinically significant finding. Breast-fed
infants tended to have more frequent serum
bili-rubin levels measured and underwent phototherapy more often than formula-fed infants. This is im-portant in light of the renewed interest in
breast-feeding among the medical profession and society
as a whole. Further research should focus on appro-pniate therapeutic practices for this group of in-fants.
ACKNOWLEDGMENTS
The authors thank Jeffrey Johnson for his help as research assistant and Cindy Cordes and Betty Kinder for secretarial assistance. We are indebted to Dr Gerald Perkoff for his direction and editorial assistance.
REFERENCES
1. Lawrence RA: Breast Feeding: A Guide for the Medical Profession. St Louis, CV Mosby Co, 1979, pp 206-220 2. Maisels MJ: Jaundice in the newborn. Pediatr Rev
1982;3:305-319
3. Billing BH, Cole PG, Lathe GH: The excretion of bilirubin as a diglucuronide giving the direct van den Bergh reaction. Biochem J 1957;65:774-784
4. Schmid R: The identification of “direct-reacting” bilir.ubin as bilirubin glucuronide. J Biol Chem 1957;229:881-888
5. Arias IM, Johnson L, Wolfson S: Biliary excretion of in-jected conjugated and unconjugated bilirubin by normal and
Gunn rats. Am J Physiol 1961;200:1091-1094
6. Allen FH Jr, Diamond LK: Erythroblastosis Fetalis. Boston,
Little, Brown and Co, 1957
7. Newman AJ, Gross S: Hyperbilirubinemia in breast-fed
infants. Pediatrics 1963;32:995-1001
8. Stiehm ER, Ryan J: Breast milk jaundice. Am J Dis Child
1965;109:212-216
9. Arias IM, Gartner LM, Seifter S, et al: Prolonged neonatal unconjugated hyperbilirubinemia associated with breast feeding and a steroid, pregnane-3 (alpha), 20 (beta)-diol, in maternal milk that inhibits glucuronide formation in vitro. J Clin Invest 1964;43:2037-2047
10. Hardy JB, Drage JS, Jackson EC: The first year of life, in:
The Collaborative Peririatal Project of the National Institute
of Neurological and Communicative Disorders and Stroke.
Baltimore, Johns Hopkins University Press, 1979, p 104 11. Dahms BB, Krauss AN, Gartner LM, et al: Breast feeding
and serum bilirubin values during the first four days of life. J Pediatr 1973;83:1049-1054
12. DeAngelis C, Sargent J, Chun MK: Breast milk jaundice.
Wis Med J 1980;7940-42
13. Winfield CR, MacFaul, R: Clinical study of prolonged jaun-dice in breast- and bottle-fed babies. Arch Dis Child
1978;53:506-507
14. Maisels MJ, Gifford K: Neonatal jaundice in full-term in-fants. Am J Dis Child 1983;137:561-562
15. Kuhr M, Paneth N: Feeding practices and early neonatal jaundice. J Pediatr Gastroenterol Nutr 1982;1:485-488 16. Minolta Air-Shields Jaundice Meter 101: Operator’s Manual.
Narco Scientific/Air-Shields Division, Hatboro, PA, 1981 17. Maisels MJ, Conrad S: Transcutaneous bilirubin
measure-ments in full-term infants. Pediatrics 1982;70:464-467 18. Hegyi T, Hiatt IM, Indyk L: Transcutaneous
bilirubinome-try: I. Correlations in term infants. J Pediatr 1981;98:454-457
19. Yamanouchi I, Yamanouchi Y, Igarashi I: Transcutaneous bilirubinometry: Preliminary studies of noninvasive trans-cutaneous bilirubin meter in the Okayama National Hospi-tal. Pediatrics 1980;65:195-202
20. Feinstein AR: Clinical biostatistics: XXXIV. The other side of ‘statistical significance’: Alpha, beta, delta, and the cal-culation of sample size. Clin Pharrnacol Ther
1975;18:491-505
21. Martinez GA, Dodd DA: 1981 milk feeding patterns in the United States during the first 12 months of life. Pediatrics
1983;71:166-170
22. Goldman SL, Penalver A, Penaranda R: Jaundice meter: Evaluation of new guidelines. J Pediatr 1982;101:253-256 23. Watchko JF, Oski FA: Bilirubin 20 mg/dl
=
vigintiphobia.Pediatrics1983;71:660-663
24. Lucey JF: Bilirubin and brain damage: A real mess.