Published online 2017 July 15 . Research Article
Prevalence of musculoskeletal disorders among Iranian dentists
Samir Zahedpasha
1, Sediqe Ebrahimipour
2, Gholamreza Sharifzadeh
3, Anousheh
Rashed-Mohassel
4,Amin Mortaheb5 1
Department of Oral and Maxillofacial Medicine and Diagnostic Sciences, Case Western Reserve University, Faculty of Dental Medicine, Ohio, USA
2
Dental Research Center, Birjand University of Medical Sciences, Birjand, IR Iran
3
Social Determinants of Health Research Center, Birjand University of Medical Sciences, Birjand, Iran
4
Pedodontist, Private practice, Mashad, Iran
5
Department of Endodontics, School of Dentistry, Islamic Azad University of Khorasgan, Isfahan, Iran
*Corresponding author: Sediqe Ebrahimipour, Assistant Professor, Department of Endodontics, Faculty of Dentistry, Dental Research Center, Birjand University of Medical Sciences, Birjand, IR Iran. Tel:05632381700, Fax: 05632237553, Email: Sdent22@gmail.com
Received 2017 February 2; Revised 2017 May 2; Accepted 2017 July 2
1. Introduction
WMSDs (work related musculoskeletal disorders) are a group of non-traumatic musculoskeletal pain resulting from overuse and develop over time interfering with activities, and perceived as related to work. These injuries have involved many professions and is highly prevalent and also imposes heavy treatment costs (1, 2).
According to the American Federation of Labor and Congress of Industrial Organizations (AFL-CIO), MSDs
accounted for 29-35% of all occupational injuries and illnesses involving early retirement in private industries (3).
MSDs are also increasing among dentists due to occupational practices. Prolonged static postures, Repetitive movements and non-normative stressful working conditions are the main causes (4-6). Dentists' health is the most important component in providing successful dental services. Keeping the correct body posture and equipment layout is necessary for this purpose (7). However, few dentists consider their job among high-risk professions.
Abstract
Background: Work related musculoskeletal disorders (WMSDs) among dentists that caused due to physical conditions during dental procedures have become a serious health threat and impose many complications and heavy costs to the dentist and thus the community. In order to avoid these complications it is necessary the causative and predisposing factors to be known and be tackled.
Objective: This study deals with the prevalence of musculoskeletal disorders (MSDs) and related factors among dentists Methods: In this cross - sectional study, 116 dentists who were attended in a national continuing education program were participated. The data gathered trough a questionnaire and then were entered into SPSS 18 software and were analyzed using descriptive statistics and Mann-Whitney and Kruskal-Wallis tests at 0.05 significant levels.
Results: 116 Dentist with an average working experiences of 11.7±7.2 years participated in the study. 50% were male and the others were female.87 dentists (75%) had MSDs. The highest affected body part were in order the neck (56.9%) shoulders (43.1%), back (43.1%)hand/wrist (28.4%) and hand/ fingers (26.7%). The average number of MSDs in each dentist was 2.71±2.1. 34.5% were currently under treatment. Data analysis revealed no significant differences in MSDs based on gender, work experience; work hours per day, using the dental assistant and the exercise.
Conclusions: Considering the high prevalence of MSDs among dental practitioners and lack of knowledge with ergonomic principles, it seems that more attention should be done in college educations and holding retraining courses for dentists to adopt with ergonomics and getting familiar with the new materials and modern equipment.
Keywords: Ergonomics; Occupational health; Dentists; MSDs
Many studies have shown the relationship between improper postures during clinical practice and the rise of pain in different part of the body in dentists, and the results have shown that the back, neck, shoulders and hands are the most common affected body parts (8, 9).
Physiological changes that occur due to prolonged static postures such as increases disk pressures and spinal hypo mobility, may lead to degenerative changes within the lumbar spine and low back pain or injury (10).
Prolonged, static muscle contractions caused muscle ischemia or necrosis. Muscles lengthening or shortening to accommodate these postures, result muscle imbalance leading to structural damage and pain and finally lead to poor operator posture (10).
Recently several studies have been conducted examining the prevalence of MSDs among Iranian dentists
(11-13).
The aim of this study thus was to investigate the prevalence of MSDs and related factors among dentists.
2. Methods
This descriptive, cross-sectional study was performed on dentists who participated in an international scientific conference in 2014 that be held in Esfahan. Data were collected using modified Nordic Questionnaire (14). This study was reviewed and approved by the ethics committee of Birjand University of medical sciences.
The questions of mentioned form were consisted of three parts demographic data, characteristics and professional history and the presence or absence of pain in different body parts. The validity of the questionnaire was confirmed using content validity method and test retest (one week later) was performed to confirm the reliability. (r=0.85)
Verbal consent was obtained from each participant. Collected data were analyzed using descriptive statistics, Mann-Whitney and Kruskal-Wallis tests and analysis of variance at 0.05 of confidence by SPSS18.
3. Results
116 dentists were participated in this study, with the average age was 37.8± 8.3 years, the Minimum age of 24 and the maximum age of 58 years, 58 were males and the rest were females.
The frequency distribution of demographic data of studied dentists is presented in Table 1.
87 dentists (75%) had MSDs, and only 29 dentists (25%) reported no pain. The highest incidence of MSDs in order related to the neck (56.9%) shoulders (43.1%), back (43.1%) hand/wrist (28.4%) and hand/ fingers (26.7%). The frequency of affected body parts are listed in Table 2.
41 dentist (35.3%) had to go to the doctor because of pain and 40 (34.5%) were currently under treatment. 78 (2/67%) Dentists announced that they need to train ergonomic principles. 70 (3/60%) were devoted time to exercise in a week and 44 (9/37%) dentists were doing stretching movements at the time of rest between patients. The Average of working hours per day was 6.1±2.1 with a minimum of 1 and a maximum of 12 hours.
Table 1: distribution of demographic data of studied dentists
Variable Frequency (%)
Duration of professional work:
Ten years or less 58 (50)
10- 20 years 39 (33.6)
Over 20 years 19 (16.4)
Working location:
private 57 (49.1)
Hospital and governmental 25 (21.6)
Others 8 (6.9)
Private and governmental 26 (22.4) Number of work shift per day:
One shift 53 (45.7)
Two shift 59 (50.9)
Three shift 4 (3.4)
Using dental assistant:
Yes 96 (82.8)
No 20 (17.2)
Positioning:
right hand, using right handed unit 99 (85.3) Left hand, using right handed unit 11 (9.5) Left hand, using left handed unit 6 (5.2) Work hours per day:
Less than 6 hours 48 (41.4)
6 hours 22 (19)
7-8 hours 33 (28.4)
More than 8 hours 13 (11.2) Working break:
Always 6 (5.3)
Often 20 (17.2)
Sometimes 80 (69)
Never 10 (8.6)
Working status
Standing 5 (4.3)
Sitting 90 (77.6)
Standing and sitting 21 (18.1)
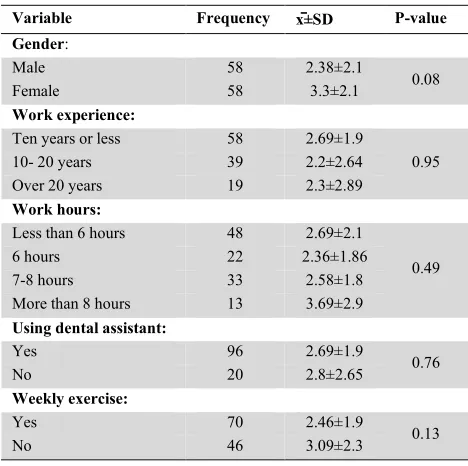
In this study the presence of MSDs in eleven parts of the body were studied, that the average number of MSDs in each dentist were 2.71± 2.1. Based on the data in Table 3 no significant differences were observed in dentists between the number of MSDs and the gender, work experience, work hours per day, using the assistant and doing weekly exercise.
4. Discussion
In the present study, we studied the prevalence of MSDs in different parts of the body of dental practitioners and its relationship with some indexes such as gender, work experience, work hours per day, using of dental assistant and exercise. The study results show that a high percentage
of dentists (75%), suffered from musculoskeletal pain and the number of MSDs in each dentist was 2.71±2.1. Pain in female was higher than in male, although the difference was not significant. The highest incidence of pain was related to the neck and shoulders. According to the Occupational Safety and Health Administration (OSHA) neck injury also had more incidence than other injuries among dentists and the reason was noted changing in working status from standing to sitting position because till then low back pain had a higher prevalence. The prevalence of neck and shoulder pain among dentists was reported high in different studies (8,9) and Iranian dentists have also not been spared
(11-13).
The worst posture was noted during the surgery, pediatric dentistry and that root canal therapy that may indicate the effect of work stress and duration of procedure on the physical condition of the dentist (15). In this study, there was no relationship between work experience and presence MSDs. A study performed by Saad and Kawai on dental students also showed that over 93 percent of dental students showed symptoms of MSDs (16). This could reflect the impact of stress on physical conditions of dentists, so that less experienced dentists had more stress than experienced dentists. On the other hand experienced dentists can better adjust their time and working hours based on body condition. Several studies showed that the prevalence of musculoskeletal pain increases with age, (17, 18) in the present study, even though the prevalence of pain was more in dentists with work experience of over 20 years, but this difference was not significant.
Most of dentists had not regularly rested between the patients (77.6%) and most of them (58.6%) worked over 6 hours per day; these two factors could explain the high levels of pain and numerous of MSDs among dentists. Forwarded and rotated posture of the neck for prolonged time in static position compared to non-working condition considerably keeps pathophysiological mechanisms occurring at the motor unit, (10) also duration, frequency and force used during a specific dental task were suggestive high risk factors that can be added to the above-mentioned. Over 34% of dentists were currently under treatment This amount is similar to Australian and Saudi Arabian dentists, where over one-third had sought medical attention.(6, 19).
60.3% of dentists were allocated time per week to exercise, while 75% had painful disorders. It could mean that the exercise alone could not be deterrent to pain. But Table 2: The frequency of MSDs based on the location
No Frequency (%) Yes Frequency (%) Pain 50 (41.3) 66 (56.9) Neck 66 (56.7) 50 (43.1) Shoulders 66 (56.9) 50 (43.1) Low Back 80 (69) 36 (31) Backbone 83 (71.6) 33 (28.4) Wrist 85 (73.3) 31 (26.7) Fingers 100 (86.2) 16 (13.8) Hip 103 (88.8) 13 (11.2) Arms 103 (88.8) 13 (11.2) Knees 112 (96.6) 4 (3.4) Ankles 114(98.3) 2 (1.7) Leg
Table3: Comparison of MSDs number based on demographic variables
Variable Frequency x̄±SD P-value Gender:
Male 58 2.38±2.1
0.08
Female 58 3.3±2.1
Work experience:
Ten years or less 58 2.69±1.9
0.95
10- 20 years 39 2.2±2.64
Over 20 years 19 2.3±2.89 Work hours:
Less than 6 hours 48 2.69±2.1
0.49
6 hours 22 2.36±1.86
7-8 hours 33 2.58±1.8
More than 8 hours 13 3.69±2.9 Using dental assistant:
Yes 96 2.69±1.9
0.76
No 20 2.8±2.65
Weekly exercise:
Yes 70 2.46±1.9
0.13
No 46 3.09±2.3
also continuous and prolonged work despite fatigue, inadequate rest and severe fatigue at the end of the day are the main causes of pain and its complications especially in the neck and back (12) that must be treated with preventive measures, physical therapy and ergonomic advices. Most of the dentists (67.2%) expressed they need to train ergonomics. Ergonomics is essentially fitting the workplace to the worker. Learn the science of modification and optimization the working environment and dental equipment so that is proportional to the limitations and capabilities of individuals should be started from college and the necessary trainings such as standard clock method, use the dental mirror, do work in both sitting and standing positions and diversification of work be included in the curriculum.
There is a significant relationship between the compliance with ergonomic recommendations and reducing MSDs, so that 72% of surveyed dentists reported that their pain has improved or declined with respect these recommendations (20, 21).
Retraining courses for ergonomic and education of exclusive stretching exercise for different part of the body as well as using new materials and modern equipment should be held. Four-handed dentistry that means the presence of an experienced full-time assistant besides the dentist to reduce the time and stress of the work to the dentist also is highly effective and emphasized.
Future studies should be focus on the effects of this preventive and curative methods on dentists who is suffering from MSDs.
5. Conclusion
Considering the high prevalence of MSDs among dental practitioners and lack of knowledge with ergonomic principles, it seems that more attention should be done in college educations and holding retraining courses for dentists to adopt with ergonomics and getting familiar with the new materials and modern equipment.
Conflict of interest
The authors declare no conflict of interest
6. Acknowledgements
This article was extracted from the research project approve and supported by research deputy of Birjand university of medical sciences.
References
1. Bhattacharya A. Costs of occupational musculoskeletal disorders (MSDs) in the United States. International Journal of Industrial Ergonomics. 2014;44(3):448-54.
2. Veisi H, Choobineh A, Ghaem H. Musculoskeletal Problems in Iranian Hand-Woven Shoe-Sole Making Operation and Developing Guidelines for Workstation Design. The international journal of occupational and environmental medicine. 2016;7(2 April):725-87-97.
3. Safety A, editor. Health Department Death on the Job: The Toll of Neglect. 2002: Washington, DC: American Federation of Labor-Congress of Industrial Organizations.
4. Rabiei M, Shakiba M, DEHGAN-SHAHREZA H, Talebzadeh M. Musculoskeletal disorders in dentists. International journal of occupational hygiene. 2015;4(1):36-40.
5. Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2010;35(4):419-29.
6. Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders and symptom severity among Australian dental hygienists. BMC research notes. 2013;6(1):250.
7. Mandel ID. Occupational risks in dentistry: comforts and concerns. The Journal of the American Dental Association. 1993;124(10):40-9.
8. Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: a review. Industrial health. 2007;45(5):611-21.
9. Roquelaure Y, Ha C, Leclerc A, Touranchet A, Sauteron M, Melchior M, et al. Epidemiologic surveillance of upper‐extremity musculoskeletal disorders in the working population. Arthritis Care & Research. 2006;55(5):765-78.
10. Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. The Journal of the American Dental Association. 2003;134(10):1344-50.
11. Chamani G, Zarei MR, Momenzadeh A, Safizadeh H, Rad M, Alahyari A. Prevalence of musculoskeletal disorders among dentists in Kerman, Iran. Journal of Musculoskeletal Pain. 2012;20(3):202-7.
12. Memarpour M, Badakhsh S, Khosroshahi SS, Vossoughi M. Work-related musculoskeletal disorders among Iranian dentists. Work. 2013;45(4):465-74.
13. Rahmani N, Amiri M, Ali Mohseni-Bandpei M, Mohsenifar H, Pourahmadi MR. Work related neck pain in Iranian dentists: An epidemiological study. Journal of back and musculoskeletal rehabilitation. 2013;26(1):9-15.
14. Palmer K, Smith G, Kellingray S, Cooper C. Repeatability and validity of an upper limb and neck discomfort questionnaire: the utility of the standardized Nordic questionnaire. Occupational medicine. 1999;49(3):171-5.
15. Yaghobee S, Esmaeili V. Evaluation of the effect of the ergonomic principles’ instructions on the dental students’ postures an ergonomic assessment. Journal of Dental Medicine. 2010;23(2):121-7.
16. Khan SA, Chew KY. Effect of working characteristics and taught ergonomics on the prevalence of musculoskeletal disorders amongst dental students. BMC musculoskeletal disorders. 2013;14(1):118.
17. Meenakshi S, Raghunath N, Nandlal NVM. Work Related Musculoskeletal Disorders among General Dental Practitioners of Mysore District, Karnataka-A Questionnaire Survey. International Journal of Health Sciences and Research (IJHSR). 2014;4(10):131-41.
18. Rayyan MR, Hetou SC, Al Salem RF, Tokhtah HA, Alrajhi AD, Mohamed LH, et al. Work-related Musculoskeletal Disorders among Dental Students of Different Academic Levels. Journal of International Oral Health. 2016;8(4):471.
19. Al Wassan K, Almas K, Al Shethri S, Al Qahtani M. Back & neck problems among dentists and dental auxiliaries. J Contemp Dent Pract. 2001;2(3):017-30.
20. Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. Journal of the California Dental Association. 2002;30(2):139-48.
21. Warren N. Work stress and musculoskeletal disorder etiology: The relative roles of psychosocial and physical risk factors. Work. 2001;17(3):221-34.