Executive Summary of the Workshop on the Border of Viability
Rosemary D. Higgins, MD*; Maria Delivoria-Papadopoulos, MD‡; and Tonse N.K. Raju, MD*
ABSTRACT. One of the most complex areas in perina-tal-neonatal medicine remains the care of the mother delivering a newborn infant at the border of viability, referred to as “periviable” gestation. To address the knowledge gaps that preclude optimal, evidence-based care in this critical field of perinatal medicine, the Na-tional Institute of Child Health and Human Develop-ment organized a workshop in March 2004. This article provides a summary of the discussions, focusing on ma-jor knowledge gaps and prioritized suggestions for stud-ies in this area. Pediatrics 2005;115:1392–1396; prematu-rity, fetal death, cerebral palsy, neonatal resuscitation, intensive care, ethics.
T
he care of women with pregnancy complica-tions at gestacomplica-tions considered near the “border of viability” involves a complex set of medical, emotional, and social challenges for health care pro-fessionals and for the concerned families of patients.1Because there is no uniformly accepted definition for the term “border of viability,” we use the term “periviable” to refer to the fetus at 20 to 26 weeks of gestational age, when brief pregnancy prolongation can alter dramatically the potential for survival and long-term complications. Care practices have varied widely in this critical area of perinatal-neonatal med-icine. Few randomized, controlled trials have been conducted to identify optimal approaches to the care of women and infants at periviable gestations, and no guidelines help clinicians formulate uniform treatment plans.
To address these issues, the Pregnancy and Peri-natology Branch of the National Institute of Child Health and Human Development sponsored a work-shop titled “Border of Viability” in March 2004. The participating expert panel reviewed the existing lit-erature and discussed challenges facing the health care team in providing prenatal, perinatal, and neo-natal management for infants born at the threshold of viability, in light of the current statistics on
short-term survival rates and long-short-term sequelae. The panel reviewed gaps in knowledge and variations in current management practice and formulated re-search priorities to rectify the gaps and to facilitate development of uniform practice guidelines in the future. This article provides a summary of those discussions.
OBSTETRIC CARE AT PERIVIABLE GESTATIONS When the need for periviable delivery is consid-ered, obstetric care requires a critical evaluation of the medical conditions of both the mother and the fetus. Under certain circumstances (eg, clinically ev-ident intrauterine infection), delivery is necessary to reduce both maternal and fetal/neonatal morbidity. In other circumstances, the need for expeditious de-livery may be less clear or the needs of the mother and fetus may conflict. In the absence of an acute indication for delivery, estimates of maternal, fetal, and neonatal risks with efforts to conserve the preg-nancy must be weighed against the risks of perinatal death and long-term sequelae with expeditious de-livery. Efforts to continue the pregnancy to allow additional fetal growth and maturation may occur in a potentially “hostile” intrauterine environment. A crucial step in estimating newborn risk in the perivi-able period is accurate assessment of gestational age and fetal growth. Regarding maternal and fetal risks of continued pregnancy, there is a need to under-stand the impact of the maternal or fetal condition necessitating consideration of delivery and the con-sequences of continued pregnancy in such a circum-stance.
The dilemma for obstetricians can be seen in the following example. For a pregnant woman present-ing at a reported gestation of 23 weeks with signs of hypertension, a 2-week prolongation of pregnancy may benefit her fetus, because survival rates after periviable birth improve from 20% to 35% at 23 weeks to 50% to 70% at 25 weeks.2If the gestational
age assignment is inaccurate and the pregnancy is only 21 weeks at presentation, then pregnancy pro-longation of 2 weeks can increase potential survival rates from 0% to 20% to 35%, with a significant risk of serious long-term morbidity among survivors. A 25-week gestation with a growth-restricted, 23-week-sized fetus may also demonstrate significantly im-proved survival rates with a 2-week delay in deliv-ery, but with increased potential for fetal loss. If the mother has mild chronic hypertension, then conser-vative management is often well tolerated. For a mother with new-onset acute hypertension associ-ated with severe preeclampsia, however, attempts to From the *Pregnancy and Perinatology Branch, Center for Developmental
Biology and Perinatal Medicine, National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland; and ‡Department of Pediatrics, St Christopher’s Hospital for Children, Drexel University College of Medicine, Philadelphia, Pennsylvania. Accepted for publication Sep 13, 2004.
doi:10.1542/peds.2004-1989 No conflict of interest declared.
Address correspondence to Rosemary D. Higgins, MD, Pregnancy and Perinatology Branch, Center for Developmental Biology and Perinatal Med-icine, National Institute of Child Health and Human Development, Na-tional Institutes of Health, 6100 Executive Blvd, Room 4B03B, MSC 7510, Bethesda, MD 20892. E-mail: higginsr@mail.nih.gov
prolong the pregnancy place the mother at increased risk of complications, including acute hypertensive crisis, stroke and myocardial ischemia, eclampsia and hemolysis/elevated liver enzymes/low platelets syndrome, and renal failure, among other serious complications. In this situation, therefore, accurate assessments of the gestational age and fetal growth, techniques to predict fetal reserve serially and accu-rately, a better understanding of the effects of pro-longed exposure to uteroplacental dysfunction in the periviable period, and markers to better distinguish those who can be successfully treated conservatively for extended periods from those who cannot, in the setting of hypertension, are needed.
ACCURACY OF GESTATIONAL AGE ASSESSMENTS Unfortunately, even after decades of significant advances in obstetrics, the accuracy of estimating gestational age in mid-pregnancy remains far from satisfactory. Although there are established criteria for gestational age assessments based on the date of the last menstrual period and ultrasound studies, the margins of error for these methods remain relatively large, because of random errors in the range of the windows of fertility and conception and variations in fetal growth in the second and third trimesters. Even an apparently small margin of error of 1 to 2 weeks in estimated gestational age at mid-gestation can affect therapeutic decisions dramatically, in opposite directions, because survival rates improve tremen-dously with each advancing week of gestation be-yond 23 weeks. In addition to the gestational age assessment, another knowledge gap is in the ability to determine why some infants appear to be physi-ologically more mature than others at identical ges-tational ages, as exemplified by female infants, whose lung function is superior, on average, to that of male infants of the same gestational age.
PERINATAL COUNSELING AND THERAPY Because of the lack of randomized controlled trials, most obstetric decisions involving the care of women with pregnancy complications in the late second tri-mester and early third tritri-mester have been empirical, based on small case series, expert opinion, and prac-tice experiences. Such experiences and opinions of-ten cannot be generalized. Although the “best avail-able” information should be offered to patients with these complications, an appraisal of the limitations of the available information is appropriate. Health care professionals planning to counsel such women in labor should also have accurate current information regarding infant survival rates and long-term se-quelae after periviable birth, with evidence-based data. The information provided should include na-tional statistics, integrated with local experience re-garding outcomes related to specific disorders (eg, outcomes of pregnancies complicated by fetal ab-dominal wall defects and surgery to treat such de-fects), where possible.
It is well established that therapies such as prena-tal corticosteroid therapy for feprena-tal lung maturation3
among women with preterm labor and antibiotic treatment for pregnancy prolongation with
prema-ture rupprema-ture of the membranes4are beneficial when
used for pregnancies with preterm delivery. How-ever, the value of these therapies has not been fully studied among women at risk for delivery between 20 and 24 weeks of gestation. Furthermore, the opti-mal mode of delivery (vaginal versus cesarean) for the fetus and the mother in the periviable period is not known. Scientists planning future randomized, controlled trials in these areas might wish to consider the baseline data from early observational trials de-scribing such interventions and outcomes. Other spe-cific aspects of knowledge gaps regarding the care of fetus and newborn at periviable gestations are listed in Table 1.
NEONATAL RESUSCITATION AND CARDIOPULMONARY MANAGEMENT There is little specific information to guide resus-citation of a periviable infant in the delivery room.
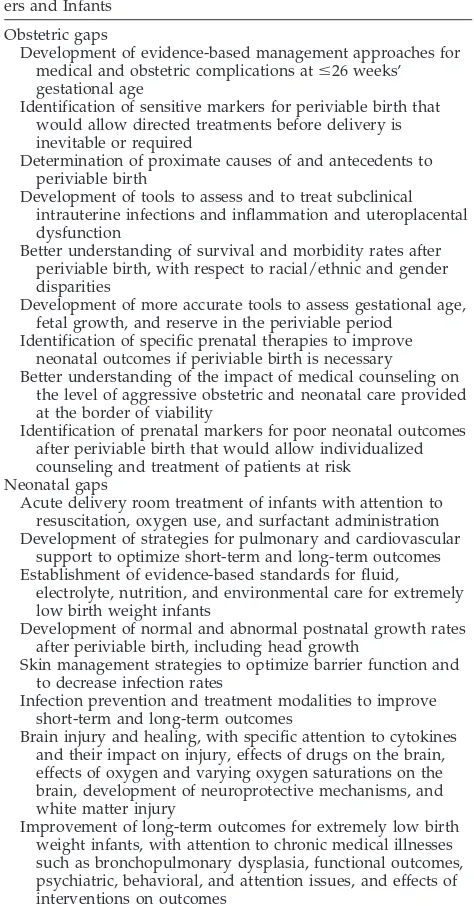
TABLE 1. Prioritized List of Gaps in Knowledge That Need to Be Rectified for the Assessment and Treatment of Periviable Moth-ers and Infants
Obstetric gaps
Development of evidence-based management approaches for medical and obstetric complications atⱕ26 weeks’ gestational age
Identification of sensitive markers for periviable birth that would allow directed treatments before delivery is inevitable or required
Determination of proximate causes of and antecedents to periviable birth
Development of tools to assess and to treat subclinical intrauterine infections and inflammation and uteroplacental dysfunction
Better understanding of survival and morbidity rates after periviable birth, with respect to racial/ethnic and gender disparities
Development of more accurate tools to assess gestational age, fetal growth, and reserve in the periviable period
Identification of specific prenatal therapies to improve neonatal outcomes if periviable birth is necessary Better understanding of the impact of medical counseling on
the level of aggressive obstetric and neonatal care provided at the border of viability
Identification of prenatal markers for poor neonatal outcomes after periviable birth that would allow individualized counseling and treatment of patients at risk
Neonatal gaps
Acute delivery room treatment of infants with attention to resuscitation, oxygen use, and surfactant administration Development of strategies for pulmonary and cardiovascular
support to optimize short-term and long-term outcomes Establishment of evidence-based standards for fluid,
electrolyte, nutrition, and environmental care for extremely low birth weight infants
Development of normal and abnormal postnatal growth rates after periviable birth, including head growth
Skin management strategies to optimize barrier function and to decrease infection rates
Infection prevention and treatment modalities to improve short-term and long-term outcomes
Brain injury and healing, with specific attention to cytokines and their impact on injury, effects of drugs on the brain, effects of oxygen and varying oxygen saturations on the brain, development of neuroprotective mechanisms, and white matter injury
For instance, we do not know what concentration of oxygen is optimal. Nor do we know what means of mechanical intervention provides optimal lung ex-pansion and transpulmonary gas exchange while minimizing the risk of chronic lung disease. In this regard, the value of continuous positive airway pres-sure begun in the delivery room has yet to be stud-ied. Furthermore, management strategies for perivi-able infants in the intensive care nursery remain empirical, especially with regard to the dose and appropriate frequency of exogenous surfactant ther-apy and the methods of ideal ventilatory support (eg, high frequency, conventional, assist control, or vol-ume guarantee). Studies are needed to establish the optimal range for the safe effective use of supple-mental oxygen with assisted ventilation. This is crit-ically needed, because too-low concentrations might lead to hypoxic injury and too-high concentrations to retinopathy of prematurity and chronic lung disease. Periviable infants are often cared for with equipment designed for larger infants. It may be that optimal treatment requires specific equipment of appropriate size and design to accommodate the specific needs of this population.
The impact of preterm birth on the cardiovascular system is not well studied. The status of the ductus arteriosus and changes in pulmonary blood flow may affect both the cardiac and pulmonary systems. Routine use of prophylactic or therapeutic indometh-acin treatment for early patent ductus arteriosus clo-sure remains controversial. Similarly, myocardial function among periviable infants has not been well studied. Studies are needed urgently to define nor-mal boundaries of systemic blood pressure, mecha-nisms that control changes in blood pressure, and effects on cerebral blood flow. Effects of medications on the cardiopulmonary system are not well delin-eated. The short-term and long-term effects of apnea are unclear. Long-term cardiopulmonary outcomes in early childhood and adulthood for the tiniest sur-vivors remain a significant issue.
FLUID, NUTRITION, AND MEDICATION SUPPORT Fluid management of periviable infants remains a major challenge. Extreme skin immaturity, high rates of insensible water loss, and cardiovascular instabil-ity all add to the complexinstabil-ity of fluid management among periviable infants. Therefore, optimal fluid and electrolyte management remains unclear. Some issues include high versus low fluid intake (200 –300 vs 60 –90 mL/kg per day), time and mode of treat-ment of patent ductus arteriosus, fluid managetreat-ment in relation to patent ductus arteriosus, regulation of the enzyme Na⫹/K⫹-ATPase, effects of electrolyte abnormalities (hyponatremia and calcium abnormal-ities) and glucose abnormalities on neurodevelop-mental outcomes, and optimization of parenteral nu-trition, with supplementation of trace elements, micronutrients, and vitamins. The best strategy for providing environmental support, including optimal temperature and humidity, has not been well estab-lished for this population.
Breakdown of skin integrity and infection continue be vexing problems among periviable infants,
partic-ularly during the first and second weeks of life and among infants supported with high environmental humidity. However, the best methods to prevent the loss of skin integrity, especially with its roles in heat loss, fluid loss, and prevention of infection, remain undetermined. Although the skin is the largest organ in the body, its function in the neonatal period has not been well studied. Studies are needed to under-stand the developmental maturation of the skin, with respect to gestational age, in relation to fluid and electrolyte exchange functions, the maintenance of skin integrity and immunologic functions, and the best measures to support proper skin growth.
Providing appropriate nutritional support for periviable infants remains a major challenge. Scien-tific evidence is lacking to guide optimal parenteral and enteral administration of protein, fat, and carbo-hydrates and the appropriate caloric balance in the early neonatal period for infants born at periviable gestations. Enteral feeding strategies for this group have not been well evaluated. The effects of reflux and antireflux medications on short- and long-term outcomes among periviable infants are unknown.
The maturation of the gastrointestinal tract and its role in immunity are emerging areas of research. Necrotizing enterocolitis continues to be a significant problem in the NICU. The definition of ideal growth for periviable infants remains unclear. How fast should an infant grow? Should treatment aim to achieve maintenance of intrauterine growth rates? What are the long-term effects of variations in growth and growth rates? What is the impact of growth on brain growth? These questions must be addressed. Similarly, the composition of breast milk from mothers who deliver periviable infants and breast milk’s role in improving outcomes remain to be elucidated. At the present time, we use normative information for growth parameters such as length, weight, and head circumference based on data for full-term infants; for assessment of growth, however, we need data for extremely low birth weight infants. It is unclear whether information from intrauterine fetal growth or infants born at periviable gestations should be used. The effects of early and late inter-ventions to promote optimal growth and their long-term outcomes need to be studied.
The study of drugs and the effects of maternal drugs on periviable infants is a large scientific gap. Similarly, data are not available on the pharmacoki-netic features, doses, and metabolism of common drugs used for newborn infants, such as antibiotics, inotropic agents, and analgesics.
NEONATAL INFECTIONS
out-comes than are those without such diagnoses. De-spite the widespread use of antibiotics in the treat-ment of proven or presumed sepsis, there is a paucity of information about the short-term and long-term safety of antibiotic therapy for periviable infants. It is unclear to what extent the illness or the treatments lead to adverse outcomes.
Other concurrent conditions and treatments may alter the course of neonatal sepsis or may themselves be altered by sepsis. Some of these conditions in-clude respiratory distress syndrome, intraventricular hemorrhage, periventricular leukomalacia, chronic lung disease, and corticosteroid treatment. Similarly, the effects of nutrition and growth on immune func-tion and the development of sepsis, possible racial and ethnic differences in responses to infections, and the overall relationships of these factors to anteced-ent chorioamnionitis remain to be studied.
NEUROLOGIC ISSUES
The high frequency of severe long-term neurologic sequelae after periviable birth remains an important challenge. More studies are needed to understand the biological basis for injury to the developing brain and mitigators of such damage. In this regard, elu-cidation of the role of cytokines as inflammatory mediators and neuroprotective factors may provide insights.
The effects of oxygenation (both hypoxia and hy-peroxia and relative amounts of oxygen tation), iron treatment (transfusions and supplemen-tation), and carbon dioxide levels on the brain, optimization of oxygen levels, and the effects of bil-irubin on periviable brain development need to be studied. Although indomethacin prophylaxis has been shown to be effective in reducing grades III and IV intraventricular hemorrhage,5 there is no
long-term benefit from such therapy.6The specific value
of indomethacin among periviable infants is unclear. The effects of maternal thyroid status and the en-docrinologic effects of early placental withdrawal on the periviable fetus are unknown. Influences of the micro- and macroenvironment on the brain and the developing nervous system before delivery and in the NICU are not well studied. The factors that might affect optimal growth and development of the brain in the ex utero environment, compared with the in utero environment, have yet to be elucidated.
Treatments directed against complications in a cer-tain organ system may produce adverse effects in the same or other organ systems. For instance, glucocor-ticoid therapy to facilitate the weaning of infants from mechanical ventilation can have dramatic ef-fects on the pulmonary system; however, long-term follow-up studies revealed a dose-dependent in-crease in the risk of cerebral palsy among surviving infants exposed to corticosteroid therapy postnatally, as well as acute changes in growth in this popula-tion.7
MULTIPLE GESTATIONS
Special populations of periviable infants pose unique challenges. With the advent of assisted repro-ductive technology, the rates of twin and high-order
multiple gestations have increased. These pregnan-cies are represented disproportionately among pre-term and early prepre-term births. Evidence-based man-agement guidelines with respect to prenatal, periviable, neonatal, and long-term therapies would be extremely helpful for these groups of infants.
NEONATAL FOLLOW-UP MONITORING In assessments of the long-term outcomes of periviable infants, we are confronted with such fun-damental questions as the following. What is nor-mal? What are normal development and growth? How long should an infant be given a “corrected” score (based on gestational age) on a given test? Reports of outcomes must include information re-garding birth weight, gestational age, mode of deliv-ery, prenatal glucocorticoid therapy, and population-based data with clearly defined numerators and denominators. Suggestions for realistic denomina-tors for assessment of perinatal outcomes related to periviable birth have included all women delivering periviable infants, live-born infants undergoing ag-gressive resuscitative efforts, and only infants admit-ted to the NICU. Each may be appropriate, depend-ing on the specific evaluation bedepend-ing addressed. Attrition rates in follow-up periods for population-based studies need to be minimized, so that esti-mates are accurate.
Many additional questions need to be answered. What are the correct evaluation tools for follow-up monitoring? Are we using the correct testing venues and instruments? Neonatal follow-up monitoring for children up to 3 years of age has included Bayley developmental assessments traditionally. What are the functional (as opposed to numerically scored) outcomes? Children may have problems but may be able to perform activities of daily living without much difficulty. Conversely, some children may be severely impaired, resulting in tremendous burdens for parents and caregivers. How do psychiatric, be-havioral, and attention issues affect follow-up assess-ments? These issues occur at somewhat older ages (school age). How has chronic illness affected fol-low-up assessments? Do available resources and ac-cess to care affect outcomes? Prediction of outcomes based on clinical complications and clinical courses can be performed in population-based studies, but each child may not fit the model for these types of predictions.
BRIDGING BASIC AND CLINICAL SCIENCE There are gaps in basic and translational research, including placentation and placental pathologic pro-cesses, the effects of oxygen and carbon dioxide on developing organ systems, and the effects of drugs on cells and tissues. All of these are extremely rele-vant to the care of this population. Cellular and animal studies are necessary to define normal and abnormal development more clearly.
extrapolation of information from infants born at greater gestational ages. Often clinicians are faced with very difficult medical decisions regarding esca-lation, limitation, and withdrawal of therapy. How-ever, because of the many unknown factors, offering palliative care on a routine basis is not considered appropriate. Decisions must be made on a case-by-case basis, and this is truly an art in medicine. Deci-sions must be made in consultation with parents during the crisis of a threatened or imminent perivi-able delivery; this is difficult because of gaps in knowledge. Because of these gaps, there are many approaches, none of which has been evaluated rig-orously in this population.
PREDICTION AND PREVENTION OF PERIVIABLE BIRTH
Finally, although considerable effort is needed to understand more completely and to guide optimal treatment of a mother with complications leading to periviable birth and also to maximize the infant out-come once periviable birth occurs, there is a critical need to develop predictive tools and preventative strategies for periviable birth that will allow us to avoid the end-stage clinical situation in which the mother and fetus are at direct risk and delivery may be inevitable. Because preterm birth is multifactorial in nature, because markers for preterm birth near term may not be appropriate for periviable birth, and because periviable birth is itself a relatively uncom-mon complication, affecting ⬍2% to 3% of the pop-ulation, traditional models of prediction and preven-tion may not be appropriate for periviable births. Decidual inflammation and infection play increasing roles in preterm birth with decreasing gestational age. In addition, abnormal placentation and utero-placental dysfunction may play important roles in periviable births. A better understanding of the prox-imate causes and antecedent risk factors for perivi-able birth is needed. Early pregnancy markers that are predictive of periviable birth in low- and high-risk groups must be identified. Once this is accom-plished, prospective studies evaluating focused in-terventions directed at specific groups may yield improved pregnancy outcomes. Among women at risk for periviable birth, in some cases the paradigm may need to be shifted from preterm birth preven-tion to pregnancy prolongapreven-tion and optimizapreven-tion of the timing of delivery to maximize neonatal out-comes.
CONCLUSIONS
The participants recognized that there are many gaps in knowledge that need to be clarified in the care of the mother and fetus at risk for periviable birth and the newborn infant after periviable birth. Studies are needed to provide evidence-based
infor-mation that can assist clinicians regarding the com-plex biological issues, societal implications, and pa-rental expectations surrounding periviable birth. Studies should also evaluate the effects of incomplete knowledge in this area on management decisions. Attention should be devoted to determining the short-term and long-term outcomes related to perivi-able births and the benefits and burdens of such births for society. A special note was made that, although we should not hesitate to develop hospice-like care for terminally ill periviable infants, we should not forget the continued need to develop medical care and support for handicapped infants who are born at periviable gestations and survive into adulthood.
ACKNOWLEDGMENTS
The following invited scientists participated in the conference: Marilee Allen, Johns Hopkins University (Baltimore, MD); Gar-land Anderson, University of Texas (Galveston, TX); Eduardo Bancalari, University of Miami (Miami, FL); Stephen Baumgaurt, State University of New York (Stony Brook, NY); Anita Catlin, Sonoma (Napa, CA); Maureen Hack, Case Western Reserve Uni-versity (Cleveland, OH); William Hay, UniUni-versity of Colorado (Denver, CO); Brian Mercer, Case Western Reserve University (Cleveland, OH); Nigel Paneth, University of Michigan (Ann Ar-bor, MI); Jeff Perlman, Cornell University (New York, NY); Bar-bara Stoll, Emory University (Atlanta, GA) (presented by Jon Tyson, University of Texas [Houston, TX]); and Jon Tyson, versity of Texas (Houston, TX), and Katherine Wenstrom, Uni-versity of Alabama (Birmingham, AL). Moderators: Maria Delivoria-Papadopolous, Drexel University College of Medicine (Philadelphia, PA); Jerold Lucey, University of Vermont (Burling-ton, VT); Sheldon Korones, University of Tennessee (Memphis, TN); Jon Tyson, University of Texas (Houston, TX); and Betty Vohr, Brown University (Providence, RI).
REFERENCES
1. MacDonald H, American Academy of Pediatrics, Committee on the Fetus and the Newborn. Perinatal care at the threshold of viability.Pediatrics.
2002;110:1024 –1027
2. Lemons JA, Bauer CR, Oh W, et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neona-tal Research Network, January 1995 through December 1996.Pediatrics.
2001;107(1). Available at: www.pediatrics.org/cgi/content/full/107/ 1/e1
3. NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. Effects of corticosteroids for fetal maturation on perinatal outcomes.JAMA.1995;273:413– 418 4. Mercer BM, Miodovnik M, Thurnau GR, et al. Antibiotic therapy for
reduction of infant morbidity after preterm premature rupture of the membranes: National Institute of Child Health and Human Develop-ment Maternal-Fetal Medicine Units Network.JAMA.1997;278:989 –995 5. Ment LR, Oh W, Ehrenkranz RA, et al. Low dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial.Pediatrics.1994;93:543–550
6. Ment LR, Vohr B, Allan W, et al. Outcome of children in the Indometh-acin Intraventricular Hemorrhage Prevention Trial.Pediatrics.2000;105: 485– 491
DOI: 10.1542/peds.2004-1989
2005;115;1392
Pediatrics
Rosemary D. Higgins, Maria Delivoria-Papadopoulos and Tonse N.K. Raju
Executive Summary of the Workshop on the Border of Viability
Services
Updated Information &
http://pediatrics.aappublications.org/content/115/5/1392
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/115/5/1392#BIBL
This article cites 6 articles, 4 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/neonatology_sub Neonatology
sub
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_ Fetus/Newborn Infant
_management_sub
http://www.aappublications.org/cgi/collection/administration:practice Administration/Practice Management
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2004-1989
2005;115;1392
Pediatrics
Rosemary D. Higgins, Maria Delivoria-Papadopoulos and Tonse N.K. Raju
Executive Summary of the Workshop on the Border of Viability
http://pediatrics.aappublications.org/content/115/5/1392
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.