Original Research Article.
Evaluation of Knowledge and Perception of Risk Factors and Screening
For Breast Cancer Among Adult Females in Tabuk City-2017
Mohammed Hamad Alrashedi
1, Waleed Essam Saleh
1, Mohammad Ahmed Alhejaili
1,
Meshari Faisal Alenezi
1, Saleh Hammad Alhawiti
1*, Hyder O Mirghani
21Sixth Year Medical Student, Faculty of Medicine, University of Tabuk, Tabuk, KSA. 2MB, Faculty of Medicine, University of Tabuk, Tabuk, KSA.
ABSTRACT
Introduction: There were 1,853 female breast cancer cases for year 2013 in Saudi Arabia. Breast cancer ranked the 1st among females accounting for 16.1%. Studies in the UK and
USA have shown that women’s perceptions of the population
risk of cancer and their personal vulnerability are at variance with medical perspectives. Before genetic risk counseling, a minority of women have an accurate view of the chances of developing breast cancer, and the majority either over- or underestimate. A number of factors have been explored for their possible association with risk perception, including demographic and psychological factors and heuristic factors. There is considerable evidence in the literature that younger women have the highest levels of perceived risk of breast cancer, despite being at the lowest actual risk. However, there is also some evidence of a curvilinear pattern of risk perception, with lowest levels of risk perception among those aged 50 to 64 years.
Methods: We have conducted a descriptive cross-sectional study in Tabuk city population, Saudi Arabia. Sampling was stratified for the different geographical areas of the city. A self-administered questionnaire, about Knowledge and perception of Breast cancer risk factors and screening, to be filled by participants and then to be returned back on the next day. Results: In this study, there was a significant relation between
age and level of knowledge (p=0.007). Older participants showed lower level of knowledge of breast cancer. 23% of participants decided not to have regular mammogram because it is likely to be painful. We reported significant relation between level of knowledge of breast cancer and level of education.
Conclusion: We need to apply more efforts to increase the knowledge of risk factors and importance and perception of screening procedures of breast cancer among females in Tabuk city.
Keywords: Breast Cancer, Risk Factors, Screening.
*Correspondence to:
Saleh Hammad,
Sixth Year Medical Student,
Faculty of Medicine, University of Tabuk, Tabuk, KSA. Article History:
Received: 28-09-2017, Revised: 21-10-2017, Accepted: 14-11-2017
Access this article online
Website:
www.ijmrp.com
Quick Response code
DOI:
10.21276/ijmrp.2017.3.6.035
INTRODUCTION
There were 1,853 female breast cancer cases for year 2013 in Saudi Arabia. Breast cancer ranked the 1st among females accounting for 16.1%.1 Identification of breast cancer predisposing
genes has created a demand for personalized risk information in families with a cancer family history.2 Studies in the UK and USA
have shown that women’s perceptions of the population risk of
cancer and their personal vulnerability are at variance with medical perspectives. Before genetic risk counseling, a minority of women have an accurate view of the chances of developing breast cancer, and the majority either over- or underestimate.3,4 A
number of factors have been explored for their possible association with risk perception, including demographic and psychological factors and heuristic factors.4-7In a study from
Scotland, older age, were found to be linked with risk overestimation before counseling, but only age was linked to any
significant degree.4 A quantitative survey of 330 women showed
that those who had lost a mother (from breast cancer) in adolescence were more likely to overestimate and to have higher levels of cancer worry.8 A study based on Behavioral Risk Factor
Surveillance showed that women residing in rural areas were less likely to receive mammograms in accordance with recommended guidelines than their urban counterparts.9 There is considerable
evidence in the literature that younger women have the highest levels of perceived risk of breast cancer, despite being at the lowest actual risk.10 However, there is also some evidence of a
curvilinear pattern of risk perception, with lowest levels of risk perception among those aged 50 to 64 years.11 It is generally
considerable evidence supporting a positive association between family history of breast cancer and increased levels of perceived risk.13 Several other factors have been found to contribute to
increased perceptions of breast cancer risk, including having had a prior benign breast symptom.14 As hypothesized by many health
behavior change models, some research supports the position that there is a positive association between risk perception and
screening behavior; that is, the greater a woman’s perceived risk,
the more likely she is to comply with screening recommendations.15 However, it has also been argued that
excessively overestimated perceptions of risk may deter some women from undergoing recommended screening.16
METHODS
We have conducted a descriptive cross-sectional study in Tabuk city population, Saudi Arabia. The study was conducted during the period from January to May 2017. The participants were female and selected by random sampling. Sampling was stratified for the different geographical areas of the city. The sample size was calculated based on the formula (n= Z1-α2 P(1-P)/d2), where n=
sample size = 384,17-18 Z = standard normal variate = 1.96 (at 5%
type I error, p= 0.05), P= expected proportion = 50%, and d= precision error = 5%. Additional 20 % was added to cover the missing data. The total sample obtained was 460. All the pupils were approached to obtain the desired sample size. A self-administered questionnaire, consisted of 20-items was developed based on an earlier studies and instruments used in other prior studies.19 The questionnaire requires information about
Knowledge and perception of Breast cancer risk factors and screening, has been filled by participants. A letter that explains the objectives of the study and asks for participants consent was sent with the questionnaire. The questionnaire requires information of Knowledge and perception about Breast cancer risk factors and screening. The questionnaire responses were analyzed using the Statistical Package for the Social Science (SPSS Inc. Chicago, IL, USA) version 20. Categorical variables were described by frequencies and percentages. Descriptive analysis involving Chi-square test was used to test significance of association between categorical variables. The level of significance was set at P< 0.05. The research was approved by the local Research Committee of the Faculty of Medicine, University of Tabuk. Pupils were asked to give their written consents before participation in the study.
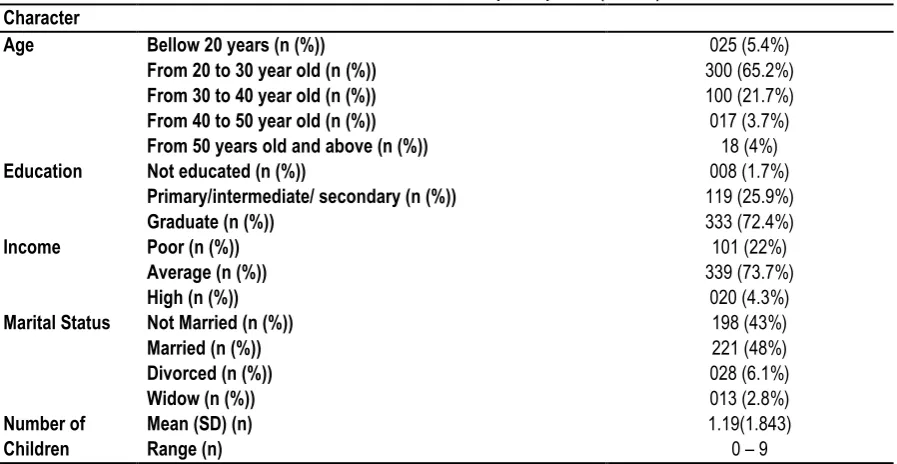
Table 1: General characteristics of participants: (n= 460) Character
Age Bellow 20 years (n (%))
From 20 to 30 year old (n (%)) From 30 to 40 year old (n (%)) From 40 to 50 year old (n (%)) From 50 years old and above (n (%))
025 (5.4%) 300 (65.2%) 100 (21.7%) 017 (3.7%) 18 (4%)
Education Not educated (n (%)) 008 (1.7%)
Primary/intermediate/ secondary (n (%)) 119 (25.9%)
Graduate (n (%)) 333 (72.4%)
Income Poor (n (%)) 101 (22%)
Average (n (%)) 339 (73.7%)
High (n (%)) 020 (4.3%)
Marital Status Not Married (n (%)) 198 (43%)
Married (n (%)) 221 (48%)
Divorced (n (%)) 028 (6.1%)
Widow (n (%)) 013 (2.8%)
Number of Children
Mean (SD) (n) 1.19(1.843)
Range (n) 0 – 9
Table 2: Frequency of level of knowledge of breast cancer:
Level of knowledge and Perception of Risk Factors Frequency Percent
Low knowledge 226 49.1
High knowledge 234 50.9
Total 460 100.0
Table 3: Relation between age and level of knowledge and perception of risk factors for breast cancer within age groups:
Age Knowledge Total
Low knowledge High knowledge
Bellow 20 years (n (%)) 20 (80%) 5 (20%) 25 (100%)
From 20 to 29 year old (n (%)) 131 (43.7%) 169 (56.3%) 300 (100%)
From 30 to 39 year old (n (%)) 54 (54%) 46 (46%) 100 (100%)
From 40 to 49 year old (n (%)) 10 (58.8%) 7 (41.2%) 17 (100%)
From 50 years old and above (n (%)) 11 (61.1%) 7 (%38.9) 18 (100%)
Table 4: Relation between education and level of knowledge and perception of risk factors for breast cancer within level of education groups:
Education Knowledge Total
Low knowledge High knowledge
Not educated (n (%)) 3 (37.5%) 5 (62.5%) 8 (100%)
Primary/intermediate/ secondary (n (%)) 72 (60.5%) 47 (39.5%) 119 (100%)
Graduate (n (%)) 151 (45.3%) 182 (54.7%) 333 (100%)
Total 226 (49.1%) 234 (50.9%) 460 (100%)
Table 5: Relation between perceived barriers of screening for breast cancer and level of knowledge and Perception of risk factors for breast cancer:
Perceived barriers Knowledge P-value
Low knowledge n=226
High knowledge n=234 I do not know where a woman can go to
get a regular mammogram.
I would not have regular mammogram because it is likely to be painful.
77(34%)
40(18%)
76(32%)
54(23%)
0.002
0.000
Table 6: Relation between perception and knowledge of family history of breast cancer and level of knowledge and Perception of risk factors for breast cancer: Perception and knowledge of
family history of breast cancer
Knowledge P-value
Low knowledge n=226
High knowledge n=234 If I have a family history of male with breast cancer,
I am at increased risk to have breast cancer
52(23%) 128(54.7%) 0.000
Total 180(39.1)
RESULTS
Table 1 s shows general characteristics of the participants. Participants classified to four categories according to age: Less than 20 year (5.4%), from 20 to 29 year (65.2%), from 30 to 39 year (29.7%), from 40 to 49 year (3.7%), and 50 year or more (4%). The majority was university graduates (72.4%), and married (48%). Table 2 shows level of knowledge of participants regarding breast cancer, participants classified to two groups, high knowledge and low knowledge, they were nearly equal, high knowledge (50.9%) and low knowledge (49.1).
Table 3 shows significant relation between age and level of knowledge (p=0.007). Of total 460 participants, (5.4%) were under age 20 year, (65.2%) were 20 to 29year, (29.7%) from 30 to 39 year, (3.7%) from 40 to 49 year, and (4%) were 50 year or more. The majority of Participants who aged less than 20 year were with low knowledge of breast cancer (80%) and who were high knowledge were (20%). Among participants who aged 20 to 29 year, the level of knowledge was for high and low knowledge (56.3%) and (43.7%), respectively. Those who aged from 30 to 39, the level of knowledge were (46%) high knowledge and (54%) low knowledge. Participants aged from 40 to 49 who were with low knowledge are more than those who were with high knowledge, (58.8%) and (41.2%), respectively. the majority of participants who were 50 year or more are low knowledge (61.1%).
Table 4 shows relation between level of knowledge of breast cancer and level of education (p=0.05). (54.7%) of who were
graduated were with high knowledge. (60.5%) of whom level of education were (primary, intermediate, and secondary) are low knowledge. The majority of uneducated participants were with high knowledge (62.5%).
Table 5 shows significant relation between perceived barriers of screening for breast cancer and level of knowledge and Perception of Risk Factors for Breast Cancer. Among female with low knowledge of breast cancer (226), 34% (p=0.002) of them did not know where they can to get a regular mammogram, and 18% (p=0.000) of them decided not to have regular mammogram because it is likely to be painful. Female with high knowledge of breast cancer and its risk factors (n=234), 32% (0.002) of them did not know where they can to get a regular mammogram, and 23% (0.000) of them decided not to have regular mammogram because it is likely to be painful.
DISCUSSION
The American Cancer Society's estimates for breast cancer in the United States for 2017 are 252,710 new cases of invasive breast cancer will be diagnosed in women, about 63,410 new cases of carcinoma in situ (CIS) will be diagnosed (CIS is non-invasive and is the earliest form of breast cancer), and about 40,610 women will die from breast cancer.20 The present study findings shows
that there is deficit in knowledge of risk factors and screening procedures. In our study the majority of participants who were 50 year or more are low knowledge (61.1%). In another study there were findings similar to our results that shows lowest levels of risk perception among those aged 50 to 64 years.21 In this study there
was a significant relation between age and level of knowledge (p=0.007). Older participants showed lower level of knowledge of breast cancer. There is a considerable evidence in the literature that younger women have the highest levels of perceived risk of breast cancer, despite being at the lowest actual risk.22 This study
showed that 23% of participants decided not to have regular mammogram because it is likely to be painful, a study that done to determine the effects of patient-based mammography screening strategies reported Similar findings.23 In our study, the relation
between level of knowledge of breast cancer and the family history of male with breast cancer was significant. 39.1% of total female agreed that if they have a family history of male with breast cancer, they are at increased risk to develop breast cancer. 23% of those who were of low knowledge of breast cancer agreed that if they have a family history of male with breast cancer, they are at increased risk to develop breast cancer. At the same time, 54.7% of female who were with high knowledge agreed that that if they have a family history of male with breast cancer; they are at increased risk to develop breast cancer. In another study there were findings similar to our results that showed awareness of genetic testing for breast cancer risk assessment was found to be significantly associated with family history of breast cancer, increasing from 35% in the lowest family history risk group to 67% in the group with the strongest familial risk (p = 0.002).24 On the
other hand, another study showed that Knowledge of breast cancer and breast cancer screening among women with positive family history of breast cancer and women without family history of breast cancer did not differ significantly.25
REFERENCES
1. Kingdom of Saudi Arabia, Saudi health Council, Saudi Cancer Registry, Cancer Incidence report of (2013), retrieved from http://www.chs.gov.sa/En/HealthRecords/CancerRegistry/Pages/C ancerRegistryRecords.aspx accessed on 15 May 2017.
2. Miki Y, Swensen J, Shattuck-Eidens D, Futreal PA, Harshman K, TavtigianS, Liu QY, Cochran C, Bennett LM, Ding W, Bell R, Rosenthal J, Hussey C, Trant T, McClure M, Frye C, Hattier T, Phelps R, HaugenstranoA, Katcher H, Yakumo K, Gholami Z, Shaffer D, Stone S, Bayer S, Wray C, Bogden R, Dayananth P, Ward J, Tonin P, Narod S, Bristow PK, Norris FH, Helvering L, Morrison P, Rosteck P, Lai M, Barrett JC, Lewis C, Neuhausen S, Cannon-Albright L, Goldgar D, Wiseman R, Kamb A. Skolnick MH: A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science1994, 266:66–71.
3. Evans DGR, Burnell LD, Hopwood P, Howell A: Perception of risk in women with a family history of breast cancer. Br J Cancer 1993,67:612–614.
4. Cull A, Anderson EDC, Campbell S, Mackay J, Smyth E, Steel M: The impact of genetic counselling about breast cancer risk on
women’s risk perceptions and levels of distress. Br J Cancer 1999, 79:501–508.
5. Smith BL, Gadd MA, Lawler C, MacDonald DJ, Grudberg SC, Chi FS, Carlson K, Comegno A, Souba WW: Perception of breast cancer risk among women in breast center and primary care settings: correlation with age and family history of breast cancer. Surgery 1996, 120:297–303
6. Hopwood P, Long A, Keeling F, Poole C, Evans DGR, Howell A: Psychological support needs for women at high genetic risk of breast cancer: some preliminary indicators. Psycho-Oncology 1998, 7:402–412.
7. Shiloh L, Saxe S: Perception of risk in genetic counseling. Psychol Health 1989, 3:45–61.
8. Hopwood P, Shenton A, Lalloo F, Evans DGR, Howell A: Risk perception and cancer worry: an exploratory study of the impact of genetic risk counseling and bereavement in women with a family history of breast cancer. J Med Genet 2000:in press.
9. Stearns SC, Bernard SL, Fasick SB, Schwartz R, Konrad TR, Ory MG, DeFriese GH. The Economic Implications of Self-Care: The Effect of Lifestyle, Functional Adaptations, and Medical Self-Care Among a National Sample of Medicare Beneficiaries. Am J Public Health. 2000 Oct; 90(10):1608-12.
10. Alexander, N.E., Ross, J., Sumner, W., Nease, R.F. Jr., Littenberg, B. The effect of an educational intervention on the perceived risk of breast cancer. Journal of General Internal Medicine. 1996;11:92–97.
11.Polednak, A.P., Lane, D.S., Burg, M.A. Risk perception, family history and use of breast cancer screening tests. Cancer Detection and Prevention. 1991;15:257–263.
12. Pearlman, D., Clark, M., Rakowski, W., Ehrich, B. Screening for breast and cervical cancers: The importance of knowledge and perceived cancer survivability. Women & Health. 1999;28:93–112. 13. Lipkus, I.M., Biradavolu, M., Fenn, K., Keller, P., Rimer, B.K. Informing women about their breast cancer risks: truth and consequences. Health Communications. 2001;13:205–226. 14. Facione, N.C. Perceived risk of breast cancer. Influence of heuristic thinking. Cancer Practice. 2002;10:256–262.
15. Champion, V.L. Revised susceptibility, benefits and barriers scale for mammography screening. Research in Nursing and Health. 1999;22:341–348.
16. Calvocoressi, L., Kasi, S.V., Lee, C.H., Stolar, M., Claus, E.B., Jones, B.A. A prospective study of perceived susceptibility to breast cancer and nonadherence to mammography screening guidelines in African American and white women aged 40 to 79 years. Cancer Epidemiology, Biomarkers, & Prevention. 2004;13:2096–2105
17. www.surveymonkey.com/mp/sample-size-calculator accessed on 10 May 2017.
18. Kingdom of Saudi Arabia. 2012. census 2010 https://www.stats.gov.sa/sites/default/files/en-census2010-dtl-result_2_1.pdf [Accessed on 10 May 2017]
19. Amin, T. T., Al Mulhim, A. R., & Al Meqihwi, A. (2009). Breast cancer knowledge, risk factors and screening among adult Saudi women in a primary health care setting. Asian Pac J Cancer Prev, 10(1), 133-8.
21. Polednak, A.P., Lane, D.S., Burg, M.A. Risk perception, family history and use of breast cancer screening tests. Cancer Detection and Prevention. 1991;15:257–263
22. Alexander, N.E., Ross, J., Sumner, W., Nease, R.F. Jr., Littenberg, B. The effect of an educational intervention on the perceived risk of breast cancer. Journal of General Internal Medicine. 1996;11:92–97
23. Robin Yabroff, Jeanne Mandelblatt: Interventions targeted toward patients to increase mammography use. Cancer Epidemiology Biomarkers & Prevention. 1999, 8: 749-757 24. Mouchawar J, Byers T, Cutter G, Dignan M, Michael S. A study of the relationship between family history of breast cancer and knowledge of breast cancer genetic testing prerequisites. Cancer Detect Prev. 1999;23(1):22-30.
25. Yelena Bird, Matthew P. Banegas, John Moraros, Sasha King, Surasri Prapasiri, and Beti Thompson. The Impact of Family History of Breast Cancer on Knowledge, Attitudes, and Early Detection Practices of Mexican Women Along the Mexico-US Border. J Immigr Minor Health. 2011 Oct; 13(5): 867–875.
Source of Support: Nil. Conflict of Interest: None Declared.
Copyright: © the author(s) and publisher. IJMRP is an official publication of Ibn Sina Academy of Medieval Medicine & Sciences, registered in 2001 under Indian Trusts Act, 1882. This is an open access article distributed under the terms of the Creative Commons Attribution Non-commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article as: Mohammed Hamad Alrashedi, Waleed Essam Saleh, Mohammad Ahmed Alhejaili, Meshari Faisal Alenezi, Saleh Hammad Alhawiti, Hyder O Mirghani. Evaluation of Knowledge and Perception of Risk Factors and Screening For Breast Cancer Among Adult Females in Tabuk City-2017. Int J Med Res Prof. 2017 Nov; 3(6):177-81.