Off-Hours Admission to Pediatric Intensive Care and
Mortality
WHAT’S KNOWN ON THIS SUBJECT: Admissions to the ICU during off-hours (nights and weekends) have been variably associated with increased mortality in both adults and children. Changes in staffing patterns, patient characteristics, or other factors may have influenced this relationship over time.
WHAT THIS STUDY ADDS: This study demonstrates in a large, current, multicenter database sample that off-hours admissions to PICUs are not associated with increased risk-adjusted mortality. Admissions in the morning from 6:00AMto 10:59AMare associated with increased mortality and warrant further attention.
abstract
BACKGROUND:Critically ill patients are admitted to the pediatric ICU at all times, while staffing and other factors may vary by day of the week or time of day. The purpose of this study was to evaluate whether admission dur-ing off-hours is independently associated with mortality in PICUs.
METHODS:A retrospective cohort study of admissions of patients,18 years of age to PICUs was performed using the Virtual PICU Systems (VPS, LLC) database.“Off-hours”was defined as nighttime (7:00PMto 6:59AM) or
weekend (Saturday or Sunday any time). Mixed-effects multivariable regression was performed by using Pediatric Index of Mortality 2 (PIM2) to adjust for severity of illness. Primary outcome was death in the pediatric ICU.
RESULTS:Data from 234 192 admissions to 99 PICUs from January 2009 to September 2012 were included. When compared with regular week-day admissions, off-hours admissions were less likely to be elective, had a higher risk for mortality by PIM2, and had a higher observed ICU mortality (off-hours 2.7% vs weekdays 2.2%; P , .001). Multivariable regression revealed that, after adjustment for other significant factors, off-hours admission was associated with lower odds of mortality (odds ratio, 0.91; 95% confidence interval, 0.85–0.97;P = .004). Post hoc multivariable analysis revealed that admission during the morning period 6:00AM to 10:59 AM was independently associated with death
(odds ratio, 1.27; 95% confidence interval, 1.16–1.39;P,.0001).
CONCLUSIONS: Off-hours admission does not independently increase odds of death in the PICU. Admission from 6:00 AM to 10:59 AM is
associated with increased risk for death and warrants further investigation in the PICU population.Pediatrics2014;134:e1345–e1353 AUTHORS:Michael C. McCrory, MD, MS,aEmily W. Gower,
PhD,b,cSean L. Simpson, PhD,dThomas A. Nakagawa, MD,a
Steven S. Mou, MD,aand Peter E. Morris, MDe aDepartments of Anesthesiology, Section on Pediatric Critical
Care Medicine, bEpidemiology,cOphthalmology,eInternal
Medicine, Section on Pulmonary and Critical Care Medicine, and
dDivision of Public Health Sciences, Department of Biostatistical
Sciences, Wake Forest School of Medicine, Winston-Salem, North Carolina
KEY WORDS
pediatric critical care, mortality, patient outcomes, time factors
ABBREVIATIONS CI—confidence interval ED—emergency department OR—odds ratio
PIM2—Pediatric Index of Mortality 2 PRISM III—Pediatric Risk of Mortality III VPS—Virtual PICU Systems database
Dr McCrory designed the study, obtained the data, performed the statistical analyses, drafted the initial manuscript, prepared the tables andfigures, and revised the manuscript; Drs Gower and Simpson assisted with the statistical design and analyses (including regular meetings to discuss the statistical approach used, assisting with data cleaning and data screening, providing and reviewing code for the statistical software program, reviewing output from the statistical software program) and reviewed and revised the manuscript; Drs Nakagawa, Mou, and Morris assisted with the research design and plan for data retrieval and reviewed and revised the manuscript; and all authors approved thefinal manuscript as submitted. www.pediatrics.org/cgi/doi/10.1542/peds.2014-1071
doi:10.1542/peds.2014-1071
Accepted for publication Aug 7, 2014
Address correspondence to Michael C. McCrory, MD, MS, Department of Anesthesiology, Section on Pediatric Critical Care Medicine, Wake Forest School of Medicine, Medical Center Blvd, Winston-Salem, NC 27157-1009. E-mail: mmccrory@wakehealth. edu
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2014 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE:The authors have indicated they have nofinancial relationships relevant to this article to disclose. FUNDING:No external funding.
Critically ill patients may be admitted to the ICU at any time, but care provided may vary by day of the week or time of day. Decreased staff numbers and ex-perience level, as well as human factors such as fatigue1and circadian rhythm
disruption2have been hypothesized to
adversely affect outcomes of patients admitted during off-hours.3 A
meta-analysis and a large national registry study of adult ICU admissions, each evaluating .130 000 admissions, dem-onstrated increased odds of death as-sociated with weekend admission.4,5In
the largest study in the pediatric ICU setting to date, which included .20 000 admissions to 15 PICUs from 1995 to 2001, nighttime admis-sion was associated with increased odds of death.6Several smaller studies
in PICUs found no difference in risk-adjusted mortality for patients admitted during off-hours when compared with weekdays,7–9and 1 study found lower
risk-adjusted mortality for admissions during off-hours.10
Reasons for the varied results in studies evaluating off-hours admission and mortality in the pediatric ICU population may include type II error related to smaller numbers of admissions and lower mortality rates compared with adult studies, heterogeneous samples, or changes in care over time (such as increased prevalence of 24-hour in-house attending intensivist coverage). Our objective in this study was to in-vestigate the possible association be-tween off-hours admission and mortality in a large, current sample of pediatric ICU patients. We hypothesized that mortality would be higher for off-hours admissions when compared with regular weekday admissions, even when adjusted for other signif-icant factors. Additionally, we hypoth-esized that risk-adjusted mortality would be higher for the subsets of (1) weekend versus weekday and (2) night versus daytime admissions.
METHODS
Study Population
De-identified admission data were ob-tained from the Virtual PICU Systems (VPS, LLC) database for all admissions ,18 years of age to a participating pediatric ICU in the United States from January 1, 2009 through September 29, 2012. This represented the most recent period for which data were available in thefields of interest at the time of data retrieval. The VPS data-base is a multicenter datadata-base of PICUs, defined as a physical space dedicated exclusively to the care of critically ill children, and is used primarily for benchmarking and quality assess-ments.11 VPS data were provided by
the VPS, LLC. No endorsement or edito-rial restriction of the interpretation of these data or opinions of the authors has been implied or stated.
Data collected from the VPS database included academic center designation, 24-hour every day in-house (24/7) at-tending intensivist presence, demo-graphics, admission diagnosis, origin of admission, trauma status, day and time of admission, severity of illness scoring, and ICU mortality. All variables were specific to each admission (eg, 24-hour, in-house intensivist designation for that center at the time of admission). The 8 most frequent primary diagnostic categories were retained for descriptive statistics (respiratory, cardiovascular, neurologic, injury/poisoning/adverse ef-fects, hematology/oncology, orthopedic, infectious, and gastrointestinal), with the remainder being consolidated into 1 category,“other”(see Appendix). Admis-sions designated as post-cardiac bypass were excluded owing to concern for in-ability to adequately control for severity of illness.12Origin of admission was
grouped as emergency department (ED), inpatient (including ward and step-down), operating room, post-anesthesia care unit, another ICU from the same hospital (neonatal ICU, delivery room, or
adult ICU), outside hospital ICU, outside hospital ED, and“other”(see Appendix).
Study Design
This was a retrospective cohort study. The primary outcome was ICU mortality. The exposure was off-hours admission, defined as admission occurring during nighttime (between 7:00PMand 6:59AM
the next day, regardless of day of week) or weekends (12:00 AM Saturday until
11:59 PM Sunday). Regular weekdays
were defined as Monday through Friday 7:00AMto 6:59PMfor comparison with
off-hours. For secondary analyses the fol-lowing comparisons were made: (1) admissions on weekends (12:00AM
Sat-urday until 11:59PMSunday) were
com-pared with weekdays (12:00AMMonday
until 11:59PMFriday) and (2) admissions
during nighttime (7:00 PM until 6:59 AM
every day) were compared with daytime (7:00AMuntil 6:59PMevery day).
Severity of illness adjustment was per-formed by using Pediatric Index of Mortality 2 (PIM2),13as this is a required
datafield in the database. PIM2 risk of mortality values were multiplied by 100 (converted to a percent value) for the purposes of scale. Pediatric Risk of Mortality III (PRISM III)14data were also
obtained when available and the pri-mary analysis was again performed by using this adjustment for comparison. Evaluation of high-risk subgroups pre-viously identified to have increased risk for death with nighttime admission6
in-cluded patients who had cardiac arrest before admission identified from the PIM2 high-risk diagnosisfield, patients who had congenital cardiovascular disease identified from the VPS primary diagnosis subcategoryfield (excluding those immediately post-cardiac bypass as noted previously), and patients who had shock identified from ICD-9-CM codes (see Appendix).
ensure data quality and inter-rater re-liability. All variables in the primary analysis were required for VPS partic-ipants during the study period, thus there were 0% missing data for these fields. PRISM III was not a requiredfield in the VPS database, however 91% of admissions had PRISM III data available.
Analyses
Continuous descriptive data were compared by using Student’s t test for parametric data or Mann-Whitney
Utest for non-parametric data, where appropriate. Categorical data were compared using Pearson’sx2test.
Factors selected a priori to be evaluated in the analysis included off-hours ad-mission, PIM2 risk of mortality, age category, gender, origin of admission,15
trauma status, and 24/7 in-house int-ensivist presence. Components of each severity of illness scoring tool were not used individually in the regression model, because the PIM2 risk of mor-tality entered in the model had been calculated using these elements. Pri-mary diagnosis categories were also not used individually in the model be-cause PIM2 risk of mortality entered in the model includesfields for high- and low-risk diagnoses. Mixed effects multi-variable logistic regression with cluster-ing at the hospital level was performed using all variables. Evaluation of condi-tion index and variance inflation factor was performed to exclude collinearity. For secondary outcomes, a similar mixed-effects multivariable logistic re-gression was performed substituting nighttime or weekend admission, re-spectively, for off-hours admission. An additional analysis was performed us-ing PRISM III score to adjust for severity of illness instead of PIM2 score for those centers reporting PRISM III data. Ob-served versus expected graphical anal-ysis was performed by calculating actual mortality for patients admitted during each day of the week or hour of the day, and comparing with expected mortality
by mean PIM2 score for all patients ad-mitted during that day or hour, as appro-priate. Graphical review of admissions by day of week and time of day was performed for each center to ensure that all units admitted patients during nights and weekends. Post hoc analysis was performed using admission during the hours of 6:00 AMto 10:59AMon all
days of the week as an independent variable (versus all other times of ad-mission).
Data were analyzed by using SAS soft-ware version 9.2 (SAS Institute Inc, Cary, NC). The Institutional Review Board of Wake Forest University Baptist Hospital approved this study.
RESULTS
Retrospective data meeting inclusion criteria from 243 292 admissions to 99 centers were obtained from the VPS, LLC database. One admission was ex-cluded owing to a negative entry for age, and 9099 were excluded owing to being designated as post-cardiac by-pass, leaving 234 192 admissions in the final analysis. The median number of admissions per center was 2093 (inter-quartile range, 821–3486; range, 67–7984), and 66% were classified as academic centers. Centers ranged in capacity from categories of 0–7 to$30 beds; median category was 18 to 20 beds, and 70% of centers were designated as having 15 beds or more. In-house, 24/7 staffing by a pediatric intensive care attending was present in 55/99 (56%) centers for at least part of the study period (45% for the entire period).
Patient ages ranged from newborn through 17 years. Patient characteristics are summarized in Table 1. Overall ICU mortality was 2.4% for the sample. Mortality by day of admission is shown in Fig 1; weekend admissions had a higher observed mortality (3.1%) com-pared with weekday admissions (2.3%). Mortality by hour of admission is shown in Fig 2; nighttime admissions
had a higher observed mortality (2.5%) than daytime admissions (2.4%).
Primary admission diagnoses are sum-marized in Table 2. For all time periods, respiratory causes were the most com-mon reason for admission. Admissions classified as trauma were predominantly in the Injury/Poisoning/Adverse Effects category for primary diagnosis (81%), with some in the Neurologic category (11%), and the remainder divided across other categories.
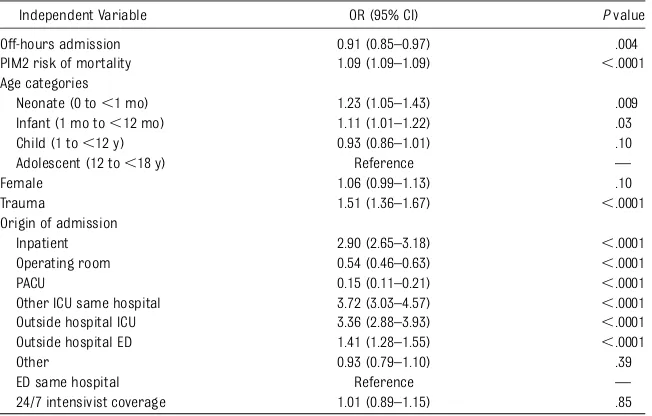
Associations with ICU mortality on multivariable analysis are displayed in Table 3. Use of PRISM III rather than PIM2 risk of mortality in the multivari-able model yielded a similar odds ratio estimate for off-hours admission (odds ratio [OR], 0.90; 95% confidence in-terval [CI], 0.83–0.97; P = .005). Sec-ondary analysis of weekend (Saturday 12:00 AM to Sunday 11:59 PM) versus
weekday (Monday 12:00 AM to Friday
11:59 PM) admissions yielded no
sig-nificant difference in odds of mortality (OR, 1.01; 95% CI, 0.94–1.09; P= .79). Nighttime admissions (7:00 PM until
6:59AMevery day) were associated with
significantly lower odds of mortality versus daytime (7:00AMuntil 06:59PM
every day) (OR, 0.86; 95% CI, 0.81–0.92;
P, .0001). Off-hours admission was not significantly associated with mor-tality when the multivariable model was applied to the subgroups of patients admitted with cardiac arrest (n= 4420; OR for off-hours admission 1.05; 95% CI, 0.89–1.23; P = .59), congential cardio-vascular disease (n= 5962; OR, 1.04; 95% CI, 0.73–1.49;P= .81), or shock (n= 3475; OR, 0.78; 95% CI, 0.59–1.03;P= .08).
A post hoc analysis was performed to evaluate the morning hours of admis-sion between 6:00AMand10:59AM, which
a more extended period from 7:00AM
to 2:59 PM during which admissions
were associated with higher mortality (Fig 2). Admissions during the 7:00AM
hour were associated with the highest unadjusted ICU mortality on weekdays
(3.5%), whereas mortality was highest for admissions during the 9:00AMhour
on weekends (4.4%). A multivariable regression analysis across the entire sample for admission during the pe-riod of 6:00 AMto 10:59AM, compared
with all other hours, revealed an OR for ICU mortality of 1.27 (95% CI, 1.26– 1.39;P,.0001).
A review of admission trends revealed that the morning period of 6:00 AMto
10:59 AM accounted for only 24 715
(10.6%) admissions (if all hours had equal admission density, a 5-hour pe-riod would be expected to contain ∼20% of admissions), with the lowest percentage of admissions during the day occurring during the 07:00AMhour
(Fig 3). During the period from 6:00AM
to 10:59 AM, admissions from the
in-patientfloor accounted for a signif-icantly larger proportion of total admissions (morning, 24.4% of admis-sions versus all other times: 12.9%;P,
.0001) and deaths (morning, 27.2% of patients who died were admitted from inpatient floor versus all other times: 16.7% of patients who died were ad-mitted from inpatientfloor;P,.0001). A post hoc evaluation of morning admissions who died versus survived revealed no significant differences as-sociated with minimum nighttime ICU coverage models (nighttime attending intensivist model in place for 58% of morning admissions who died versus 58% who survived,P= .64; fellow, 25% vs 24%,P= .43; resident, 9.3% vs 10.5%,
P= .30; hospitalist, 0.6% vs 1.2%,P= .18; attending from home only, 6.5% vs 6.8%,P= .78).
DISCUSSION
This study reports on the largest cohort to date on this topic and demonstrates that admission to the pediatric ICU during off-hours is independently as-sociated with decreased risk of mor-tality. Thesefindings are contrary to the original hypothesis for the study, and discordant with the increased risk for death for nighttime admissions found in the largest previous multicenter study in the pediatric ICU population.6 Our
study demonstrated a decreased risk for death specifically for nighttime
FIGURE 1
Mortality by day of admission. Observed, unadjusted mortality compared with expected (by mean PIM2 risk of mortality) for admissions to the pediatric ICU for each day of the week. Observed, unadjusted mortality by admission day was as follows: Monday, 2.1%; Tuesday, 2.0%; Wednesday, 2.2%; Thursday, 2.4%; Friday, 2.5%; Saturday, 3.1%; and Sunday, 3.1%.
TABLE 1 Patient Characteristics
Regular Weekdays (Mon to Fri 7:00AMto 6:59PM)
N= 108 291 Admissions
Off-Hours (All Other Times)
N= 125 901 Admissions
Pvalue
Age, y, median (IQR) 4.4 (1.1–11.8) 4.8 (1.2–12.2) ,.0001 Age categories, %
Neonate (0 to,1 mo) 3.4 3.9 ,.0001
Infant (1 mo to,12 mo) 20.8 18.7 ,.0001
Child (1 to,12 y) 51.6 51.7 .45
Adolescent (12 to,18 y) 24.2 25.7 ,.0001
Female, % 44.8 43.4 ,.0001
PIM2 risk of mortality, mean % 2.4 3.1 ,.0001
Elective admission, %a 34.4 6.1 ,.0001
Recovery from surgery, %a 36.9 8.9 ,.0001
Mechanical ventilation on admission, %a 23.5 25.3 ,.0001 Cardiac arrest before admission, %a 1.6 2.2 ,.0001
Trauma, % 4.5 12.7 ,.0001
Origin of admission, %
Inpatient 13.3 14.8 ,.0001
Operating room 22.5 5.7 ,.0001
PACU 18.4 5.0 ,.0001
Other ICU same hospital 1.3 0.6 ,.0001
Outside hospital ICU 1.8 1.7 .01
Outside hospital ED 12.0 24.7 ,.0001
Other 10.2 4.2 ,.0001
ED same hospital 20.5 43.3 ,.0001
24-h intensivist present 57.0 58.4 ,.0001
ICU LOS, d, median (IQR) 1.4 (1.0–3.3) 1.7 (0.8–3.6) ,.0001
Death in ICU ,% 2.2 2.7 ,.0001
ICU LOS before death, d, median (IQR) 3.9 (1.3–12.1) 3.1 (1.1–8.3) ,.0001 LOS, length of stay; PACU, post-anesthesia care unit.
admissions compared with daytime, whereas weekend admissions were no different from weekdays on multi-variable analysis. Thisfinding is simi-lar to a report from a single pediatric ICU in Australia, in which admissions
during off-hours had an OR for mor-tality of 0.71 (95% CI, 0.52–0.98).10
Ourfinding of decreased odds of death for nighttime admissions may simply reflect that the highest risk period for our cohort was actually 6:00AMto
10:59AM, resulting in the majority of the
higher-risk period being in the daytime cohort. Only 10.7% of admissions oc-curred during this 5-hour morning period, demonstrating that high vol-ume of admissions did not contribute to thefinding, but raising the concern that the results may be skewed owing to the relatively small sample during those hours.
Alternatively, there may be variations in care contributing to decreased risk for death for nighttime admissions and increased risk for morning admissions. The increased proportion of transfers from the inpatient floor during the morning period of 6:00AMto 10:59 (and
deaths among these patients) raises
FIGURE 2
Mortality by hour of admission. Observed, unadjusted mortality compared with expected (by mean PIM2 risk of mortality) for admissions to the pediatric ICU for each hour. For the total sample (all days), the hours of 6:00AMthrough 10:59AMhad observed mortality percentages of 2.9% to 3.8%, each higher than any other
hour-long period and exceeding expected mortality.
TABLE 2 Primary Admission Diagnosis
Primary Admission Diagnosis (%) Regular Weekdays (Mon to Fri 7:00AMto 6:59PM)
N= 108 291 admissions
Off-Hours (All Other Times)
N= 125 901 admissions
Pvalue
Respiratory 28.3 29.5 ,.0001
Neurologic 16.6 15.7 ,.0001
Cardiovascular 9.2 5.1 ,.0001
Hematology/oncology 7.0 4.6 ,.0001
Injury/poisoning/adverse effects 7.0 17.9 ,.0001
Orthopedic 6.0 1.2 ,.0001
Infectious 3.7 5.3 ,.0001
Gastrointestinal 3.7 3.7 .71
the concern for clinical deterioration overnight that was under-recognized, leading to delayed transfer to the ICU until the morning and increased mor-tality. Nighttime caregivers on the in-patient floors (such as nurses and resident physicians) may be less ex-perienced and have increased work-load, leading to delayed recognition of need for transfer to the ICU. This could be particularly problematic in patients having progression of their original disease process and/or responding poorly to clinical interventions during their inpatient stay.15The extent of
ill-ness of such patients may not be com-pletely captured using PIM2 or other scoring systems. Furthermore, the later hour associated with peak mortality for weekend admissions (peak mortality for admissions at 9:00AMon weekends
versus 7:00AMon weekdays) could be
attributable to later arrival of daytime caregivers to assess patients on the inpatientfloors. A similar phenomenon could also delay patient presentation to the ER overnight (with subsequent delay of ICU transfer), as caregivers may be sleeping or otherwise less disposed to bring their child to medical atten-tion late at night. Informaatten-tion about
nighttime hospital floor coverage, rapid response team activation, or ER admission patterns was not available for our sample, but may warrant fur-ther evaluation in future studies on this topic.
Variations in care within the ICU, such as transitions of care and dilution of caregiver attention, could also contrib-ute to the decreased odds of death for nighttime admissions with increased risk for morning admissions. Hand-offs between physicians, nurses, and other care providers often occur during the 7:00AMhour, which was associated with
peak mortality (3.8%) for the overall sample. However, no such increase in mortality was observed around the 7:00
PM hour when similar transitions may
occur on weekdays; there was a small increase at 7:00PMnoted on weekends.
At night, there are fewer admissions overall and reduced activities such as rounds, conferences, or transports out of the unit for diagnostic or therapeutic procedures, which could compete for the attention of daytime caregivers. The period from 6:00AMto 10:59AMincludes
a time period when morning rounds are conducted in most ICUs. In a study of medical and surgical admissions to
4 adult ICUs, Afessa et al16reported that
admission during the rounding time from 8:00 AM to 10:59 AM was
inde-pendently associated with increased risk for hospital death, with an OR of 1.32 (95% CI, 1.18–1.48). Similarly, de Souza et al17 evaluated medical and
surgical admissions to 5 adult ICUs and found that admission between 8:00 AM
and 11:59AM was associated with
creased severity of illness and in-creased odds of ICU mortality (OR, 1.19; 95% CI, 1.03–1.38). Several other studies have shown peak mortality for adult ICU patients admitted in the morn-ing,5,18,19however, no studies in the
pe-diatric ICU population to date have reported a similar finding. The ob-served difference in time associated with peak mortality on weekends (9:00 AM) versus weekdays (7:00 AM)
could relate to later rounding time in the ICU on weekends. Future studies are warranted to determine whether an as-sociation with increased mortality with morning admissions persists across other samples and what factors may be contributory.
Factors independently associated with increased risk for mortality in our study included neonatal and infant age groups, certain origins of ad-mission (particularly inpatient loca-tions or other ICUs), and being a trauma admission. Age has not uniformly been associated with mortality pre-viously,6,13 however, neonatal and
infant age groups appear to often be at higher risk when age is stratified into these groups.9,20,21Increased risk for
death for ICU admissions from in-patient locations has been previously described,6,15 and may represent
ad-ditional patient decompensation de-spite interventions over time, which is not fully captured by severity of illness scoring.
Mortality is relatively rare in the pedi-atric ICU and is influenced by a myriad of factors that may or may not be related
TABLE 3 Associations With Pediatric ICU Mortality by Multivariable Analysis
Independent Variable OR (95% CI) Pvalue
Off-hours admission 0.91 (0.85–0.97) .004
PIM2 risk of mortality 1.09 (1.09–1.09) ,.0001 Age categories
Neonate (0 to,1 mo) 1.23 (1.05–1.43) .009
Infant (1 mo to,12 mo) 1.11 (1.01–1.22) .03
Child (1 to,12 y) 0.93 (0.86–1.01) .10
Adolescent (12 to,18 y) Reference —
Female 1.06 (0.99–1.13) .10
Trauma 1.51 (1.36–1.67) ,.0001
Origin of admission
Inpatient 2.90 (2.65–3.18) ,.0001
Operating room 0.54 (0.46–0.63) ,.0001
PACU 0.15 (0.11–0.21) ,.0001
Other ICU same hospital 3.72 (3.03–4.57) ,.0001 Outside hospital ICU 3.36 (2.88–3.93) ,.0001
Outside hospital ED 1.41 (1.28–1.55) ,.0001
Other 0.93 (0.79–1.10) .39
ED same hospital Reference —
to factors at the time of admission. Among those who died, median length of stay until death was 3.9 days for regular weekday admissions and 3.1 days for off-hours admissions. It is unclear over what time period any variation in care at the time of ad-mission is likely to influence mortality, and likely varies widely among patients and diagnoses. Our study did not evaluate other clinically important outcomes other than mortality, or aspects of off-hours care at later times during the ICU stay. Cardiac arrests occurring in the ICU dur-ing nights and weekends have been
associated with decreased survival in both adults and children.22,23
Med-ication errors24 and complications
during intubation25 in pediatric
in-patients have also been reported to be more common during off-hours. Although 24/7 in-house intensivist coverage at the time of off-hours ad-mission did not affect mortality in our study, transition to 24/7 in-house intensivist staffing has been associ-ated with decreased duration of me-chanical ventilation and ICU length of stay at a large tertiary care PICU,26
im-plying that improved care during off-hours could affect ventilator weaning
and other factors over the course of a patient’s stay.
A major strength of our study is the large number of admissions included across 99 PICUs, including both academic and non-academic centers and many centers with 24-hour, in-house intensivist staff-ing. The PICUs in the United States in-cluded in this study represent 29% of the ∼337 PICUs in the United States.27
An-other strength of our study is the data quality; only 1 admission was excluded owing to an erroneous value for age, and complete data were available for every independent variable included in the primary analysis.
FIGURE 3
Admission density by hour. Percentage of admissions to the pediatric ICU by hour of the day. For the total sample (all days), lowest admission volume was 7:00AM
Limitations of our study are primarily related to the confines of using a large multicenter dataset. We did not have information about deaths after ICU discharge (such as on the hospital ward, at home, or in hospice care). In-formation about limitations in care at the time of admission were not avail-able. Protocols that may have been present at certain centers such as caps on nighttime admissions, separate admitting teams, or extra physician
staffing for admissions during rounds or other times, were not available. Details of nurse and advance practice provider staffing were not available. Increased nurse staffing has been as-sociated with improved outcomes in the ICU setting, including reduced mortal-ity,28,29so it is possible that an
associ-ation between off-hours admissions and mortality could exist in a subset of centers with decreased nurse staffing during these time periods.
CONCLUSIONS
Our study provides evidence in a large, current sample of PICUs that off-hours admission is independently associated with decreased mortality. Future studies are warranted to evaluate admissions during the morning time period of 6:00
AMto 10:59AM, which were associated
with peak mortality in our study, as well as other clinically important outcomes that could be associated with variations in care during off-hours.
REFERENCES
1. Chung MH, Kuo TB, Hsu N, Chuo KR, Chu H, Yang CC. Comparison of sleep-related car-diac autonomic function between rotating-shift and permanent night-rotating-shift workers. Ind Health. 2011;49(5):589–596
2. Kuhn G. Circadian rhythm, shift work, and emergency medicine. Ann Emerg Med. 2001;37(1):88–98
3. Montgomery VL. Effect of fatigue, workload, and environment on patient safety in the pediatric intensive care unit. Pediatr Crit Care Med. 2007;8(2 suppl):S11–S16
4. Cavallazzi R, Marik PE, Hirani A, Pachin-buravan M, Vasu TS, Leiby BE. Association between time of admission to the ICU and mortality: a systematic review and meta-analysis.Chest. 2010;138(1):68–75
5. Kuijsten HA, Brinkman S, Meynaar IA, et al. Hospital mortality is associated with ICU admission time.Intensive Care Med. 2010; 36(10):1765–1771
6. Arias Y, Taylor DS, Marcin JP. Association between evening admissions and higher mortality rates in the pediatric intensive care unit.Pediatrics. 2004;113(6). Available at: www. pediatrics.org/cgi/content/full/113/6/e530
7. Peeters B, Jansen NJ, Bollen CW, van Vught AJ, van der Heide D, Albers MJ. Off-hours admission and mortality in two pediatric in-tensive care units without 24-h in-house se-nior staff attendance. Intensive Care Med. 2010;36(11):1923–1927
8. Arslankoylu AE, Bayrakci B, Oymak Y. Ad-mission time and mortality rates.Indian J Pediatr. 2008;75(7):691–694
9. Hixson ED, Davis S, Morris S, Harrison AM. Do weekends or evenings matter in a pe-diatric intensive care unit? Pediatr Crit Care Med. 2005;6(5):523–530
10. Numa A, Williams G, Awad J, Duffy B. After-hours admissions are not associated with increased risk-adjusted mortality in
pedi-atric intensive care. Intensive Care Med. 2008;34(1):148–151
11. Wetzel RC, Sachedeva R, Rice TB. Are all ICUs the same?Paediatr Anaesth. 2011;21(7):787–793
12. Czaja AS, Scanlon MC, Kuhn EM, Jeffries HE. Performance of the Pediatric Index of Mor-tality 2 for pediatric cardiac surgery patients. Pediatr Crit Care Med. 2011;12(2):184–189
13. Slater A, Shann F, Pearson G; Paediatric Index of Mortality (PIM) Study Group. PIM2: a re-vised version of the Paediatric Index of Mor-tality.Intensive Care Med. 2003;29(2):278–285
14. Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated Pediatric Risk of Mortality score.Crit Care Med. 1996;24(5):743–752
15. Odetola FO, Rosenberg AL, Davis MM, Clark SJ, Dechert RE, Shanley TP. Do outcomes vary according to the source of admission to the pediatric intensive care unit?Pediatr Crit Care Med. 2008;9(1):20–25
16. Afessa B, Gajic O, Morales IJ, Keegan MT, Peters SG, Hubmayr RD. Association between ICU admission during morning rounds and mortality.Chest. 2009;136(6):1489–1495
17. de Souza IA, Karvellas CJ, Gibney RN, Bag-shaw SM. Impact of intensive care unit admission during morning bedside rounds and mortality: a multi-center retrospective cohort study.Crit Care. 2012;16(3):R72
18. Bhonagiri D, Pilcher DV, Bailey MJ. Increased mortality associated with after-hours and weekend admission to the intensive care unit: a retrospective analysis.Med J Aust. 2011;194(6):287–292
19. Laupland KB, Misset B, Souweine B, et al. Mortality associated with timing of admission to and discharge from ICU: a retrospective cohort study.BMC Health Serv Res. 2011;11:321
20. Epstein D, Wong CF, Khemani RG, et al. Race/ Ethnicity is not associated with mortality in the PICU.Pediatrics. 2011;127(3). Available at: www. pediatrics.org/cgi/content/full/127/3/e588
21. Slonim AD, Khandelwal S, He J, et al. Char-acteristics associated with pediatric inpatient death.Pediatrics. 2010;125(6):1208–1216
22. Peberdy MA, Ornato JP, Larkin GL, et al; National Registry of Cardiopulmonary Re-suscitation Investigators. Survival from in-hospital cardiac arrest during nights and weekends.JAMA. 2008;299(7):785–792
23. Gaies MG, Clarke NS, Donohue JE, Gurney JG, Charpie JR, Hirsch JC. Personnel and unit factors impacting outcome after car-diac arrest in a dedicated pediatric carcar-diac intensive care unit.Pediatr Crit Care Med. 2012;13(5):583–588
24. Miller AD, Piro CC, Rudisill CN, Bookstaver PB, Bair JD, Bennett CL. Nighttime and weekend medication error rates in an inpatient pedi-atric population.Ann Pharmacother. 2010;44 (11):1739–1746
25. Carroll CL, Spinella PC, Corsi JM, Stoltz P, Zucker AR. Emergent endotracheal intuba-tions in children: be careful if it’s late when you intubate. Pediatr Crit Care Med. 2010; 11(3):343–348
26. Nishisaki A, Pines JM, Lin R, et al. The im-pact of 24-hr, in-hospital pediatric critical care attending physician presence on pro-cess of care and patient outcomes*. Crit Care Med. 2012;40(7):2190–2195
27. Odetola FO, Clark SJ, Freed GL, Bratton SL, Davis MM. A national survey of pediatric critical care resources in the United States. Pediatrics. 2005;115(4). Available at: www. pediatrics.org/cgi/content/full/115/4/e382
28. Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: sys-tematic review and meta-analysis. Med Care. 2007;45(12):1195–1204
APPENDIX DATA GROUPINGS
Primary Diagnosis Category
“Other”category included those cat-egorized as: Dermatologic, Endocrinologic, Factors Influencing Health, Genetic, Gyne-cologic, Immunologic, Metabolic, Newborn/ Perinatal, Ophthalmologic, Psychiatric, Renal/Genitourinary, Rheumatologic, Symptoms, Transplant, and Ungroupable.
Origin of Admission
“Other” category included those cate-gorized as: outside hospital inpatient,
outside hospital stepdown, outside hos-pital operating room, outside hoshos-pital clinic, home, inpatient or outpatient pro-cedure suite, chronic care facility, physi-cal or pulmonary rehabilitation facility, psychiatric or substance abuse facility, and other.
Shock
“Shock” included ICD-9-CM codes specifying:“Anaphylactic shock,” “ Ana-phylactic shock-serum,” “Cardiogenic shock,” “Postoperative shock,” “Septic shock,” “Shock due to anesthesia,”
DOI: 10.1542/peds.2014-1071 originally published online October 6, 2014;
2014;134;e1345
Pediatrics
Steven S. Mou and Peter E. Morris
Michael C. McCrory, Emily W. Gower, Sean L. Simpson, Thomas A. Nakagawa,
Off-Hours Admission to Pediatric Intensive Care and Mortality
Services
Updated Information &
http://pediatrics.aappublications.org/content/134/5/e1345
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/134/5/e1345#BIBL
This article cites 29 articles, 4 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/safety_sub
Safety
e_management_sub
http://www.aappublications.org/cgi/collection/administration:practic
Administration/Practice Management
http://www.aappublications.org/cgi/collection/critical_care_sub
Critical Care
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2014-1071 originally published online October 6, 2014;
2014;134;e1345
Pediatrics
http://pediatrics.aappublications.org/content/134/5/e1345
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.