and without chronic lung disease. Pediatrics 1991;88:527—
532; preterm infant, rehospitalization, respiratory illness.
ABBREVIATIONS.BPD, bronchopulmonarydysplasia;NICU,
neonatal intensive care unit; RSV, respiratory syncytial virus; VLBW, very low birth weight.
It is known that preterm infants are at increased risk for rehospitalization after nursery discharge'3 and that respiratory illness is the most common reason for admission.' More than 40% of infants with bronchopulmonary dysplasia (BPD) will re quire rehospitalization during the first year of life because of acute viral respiratory tract infec tions46; however, the incidence of serious illness in preterm infants with little or no lung disease in the neonatal period has not been studied extensively. Furthermore, the impacts of the season of neonatal intensive care unit (NICU) discharge and the age ofthe infant during the first respiratory viral season on the risk of rehospitalization are not known.
We prospectively studied rehospitalization for respiratory illness among a cohort of preterm in fants and a socioeconomically matched full-term group. We compared the incidence of hospitaliza tion for preterm infants with and without BPD and
examinedneonataland environmentalfactorsthat
predispose preterm infants to serious respiratory illness.ABSTRACT.All 133survivinginfantsof gestationalage
s32 weeks born July 1, 1985, to June 30, 1986, as well as a socioeconomically matched full-term control group were
observed prospectively for 2 years to determine the mci
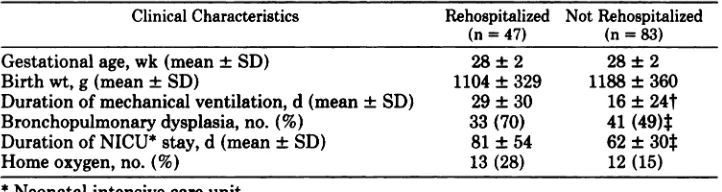
dence of rehospitalization for respiratory illness. Pen natal and seasonal factors associated with increased risk for such hospitalizations were also examined. Forty-seven (36%) preterm infants were rehospitalized compared with 3 (2.5%) of 121 term infants (P < .001). Pneterm infants with and without rehospitalization were similar for mean
birth weight (1104±329 g and 1188±360 g, respectively) and gestational age (28 ±2 weeks for both groups); however, infants who were subsequently rehospitalized
had required more days of mechanical ventilation, supple mental oxygen therapy, and neonatal intensive care. While a history of bronchopulmonany dysplasia was a risk factor for rehospitalization (45% compared with 25% of those without bronchopulmonary dysplasia, P < .05), preterm infants with no history of bronchopulmonary dysplasia still showed a 10-fold increase compared with
control infants. Among the 43 infants who required no
mechanical ventilation beyond the day of birth, 10 (23%) required rehospitalization. More than 80% of rehospital
ized infants required their first admission within 4
months of discharge from the neonatal intensive cane unit. Consequently, initial hospital discharge between September and December (the months immediately pre ceding peak respiratory viral season) resulted in an al most 3-fold increased risk of rehospitalization compared with discharge between May and August (P < .05). At 6 months of age, infants rehospitalized prior to that time had more than twice the incidence of neurologic abnor malities (12/23 [36%] vs 9/83 [11%], P < .01) than did infants who were never rehospitalized. The former group also had significantly lower motor scores on the Bayley Scales of Infant Development (89 ±18 vs 97 ±14, P < .05). These differences were not apparent at 15 and 24 months of age. Respiratory illness contributes signifi cantly to postdischarge morbidity in preterm infants with
Received for publication Jul 5, 1990; accepted Oct 12, 1990. Reprint requests to (C.K.C.) Dept of Pediatrics, SUNY Health Science Center, 750 E Adams St, Syracuse, NY 13210. PEDIATRICS (ISSN 0031 4005). Copyright ©1991 by the American Academy of Pediatrics.
PEDIATRICSVol. 88 No. 3 September1991
527
Rehospitalizationfor RespiratoryIllness in
Infants of Less Than 32 Weeks' Gestation
Coleen K. Cunningham, MD; Julia A. McMiIIan, MD;
and Steven J.Gross, MD
Fromthe Departmentof Pediatrics,StateUniversityof New York HealthScienceCenterat Syracuse
MATERIALSAND METHODS
The study population included all 133 survivors
from the 156 infants of gestational age less than 32
weeks cared for in the NICU at Crouse Irving
at Viet Nam:AAP Sponsored on September 1, 2020
www.aappublications.org/news
Memorial Hospital between July 1, 1985, and June 30, 1986. This is the sole tertiary care facility serv ing an 18-county region in central New York State. Gestational age for these infants was determined from maternal dates of the last menstrual period. Gestational age was substantiated by early second trimester ultrasonographic examination in 85% of the cases. Gestational age of all infants of >28 weeks' gestation was confirmed by Dubowitz ex
amination.7 Twenty-one infants were transported
from outlying hospitals and 112 were inborn. Forty seven (36%) of the infants were of @27weeks gestational age and 48 (37%) had birth weights
@1ooo
g.Duringtheneonatalperiod,datacollected
prospectively included durations of mechanical ventilation, supplemental oxygen therapy, and in tensive care as well as month of hospital discharge. Bronchopulmonary dysplasia was defined as an oxygen requirement greater than room air at 28 days of life.A control group consisted of 121 healthy, appro
priately grown, term infants matched to the pre
term infants for sex, race, and maternal age (by groups 17, 18 through 34, or 35 years), education (less than high school or completion ofhigh school), and marital status. These infants were born in the same hospital (Crouse Irving Memorial Hospital) that houses the NICU and over the same time period as were the preterm infants.
All preterm and term infants were seen for fol
low-up visits at 6, 15, and 24 months of age (using
age corrected for prematurity). At each visit infor
mation was obtained regarding all interval hospi
talizations. Charts for all rehospitalizations were
reviewedby one of us (C.K.C.). For eachhospital
admission, the infant's age, month of the year, diagnosis, treatment, and duration were recorded. All hospital admissions for respiratory illness (tachypnea, retractions, cyanosis) were included in the
analyses. Infants with uncomplicated otitis media or apnea were not included in this category. Infants with chronic lung disease who experienced wors ening respiratory symptoms leading to rehospitali
zation wereincluded.
To determinethe association
betweenrehospi
talization and neurodevelopmental outcome, at
eachfollow-up visit physical,neuromotor,8and de
velopmental examinations were performed. A child was considered to have abnormal neurologic ex amination results if there was evidence of moderate to severe alteration in muscle tone or hydrocephalus requiring shunt placement. Growth measurements were plotted on standard growth charts.9 Develop mental evaluations were made using the Bayley Scales of Infant Development.'0 This study was approved by the Hospital's Human Research Review Committee. Parental consent was obtained for each patient.
STATISTICS
Term and preterm infants were compared for rate of hospital admission. Preterm infants with and without rehospitalization were compared to
determine perinatal and demographic factors asso
ciatedwith hospitalreadmission.
Analysesof con
tinuous data were done using Student's t test and
categorical
datawereanalyzedusingx2andFisher's
exact probability tests where appropriate. All values are expressed as mean ±SD unless otherwise noted. A P value of less than .05 was considered signifi cant.RESULTS
Of the 133 preterm infants discharged from the nursery, 3 subsequently died of nonrespiratory causes (biliary atresia, sudden infant death syn
drome, and gastroenteritis) and were excluded from
further analysis. Four additional children died of respiratory illness during the study (data included in analysis). All 126 surviving infants returned for follow-up examination at 6 months. Two infants
did not return for follow-upat 15 months;these
two and one additional child did not return at 24 months.The parents of the 3 infants not returning for follow-up were contacted by telephone and in cidences of hospitalization were obtained. Among the full-term control infants, 118 (98%) of 121 were seen for all three follow-up visits.
Rehospitalization for any cause was required for 68 (52%) of the 130 preterm infants. Two thirds of rehospitalized infants required one or more admis sions for respiratory illness. The rate of rehospital ization for respiratory illness for preterm infants (47/130, 36%) was significantly greater than that for the term infants studied (3/121, 2.5%) (P < .001). Approximately half the admissions were to the Pediatric Service of SUNY Health Science Cen ter at Syracuse; the remaining admissions were to
regionalhospitalsthroughoutupstateNewYork.
Characteristics
of PretermInfantsWhoRequired
Rehospitalization
The 47 preterm infants who required readmission for respiratory illness were similar with regard to gestationalageandbirth weightto the 83 who never required rehospitalization (Table 1). Maternal so
Clinical CharacteristicsRehospitalized
(n=47)Not
Rehospitalized (n=83)Gestational
age, wk (mean ±SD)28 ±228 ±
2Birth
wt, g (mean ±SD)1104 ±3291188 ±
360Duration
of mechanical ventilation, d (mean ±SD)29 ±3016 ± 24tBronchopulmonary
dysplasia, no. (%)33 (70)41 (49)1Duration
of NICU* stay, d (mean ±SD)81 ±5462 ±
30@Home
oxygen, no. (%)13 (28)12 (15)
TABLE 1. Perinata.lCharacteristicsof PretermInfantsStudied
* Neonatal intensive care unit. tP< .01.
:1:P < .05.
ned), and race (80% and 90% white). The sample size may not be large enough to detect small differ ences in these socioeconomic parameters. Infants with subsequent rehospitalizations did have signif icantly greater respiratory morbidity during the newborn period, including almost twice the dura tion of mechanical ventilation and a significant increase in the incidence of BPD. More than half the infants discharged to home with oxygen (13/25, 52%) required rehospitalization (Table 1).
The 47 rehospitalized infants required 106 hos pital admissions during the first 2 years of life; 12 infants were hospitalized three or more times. The mean age of infants at the time of initial rehospi talization was 4.0 ±4.8 months. Eighty-seven per cent of initial hospitalizations occurred prior to 1 year of chronologic age. The average length of stay for each hospitalization was 10 ±14 days; the total number of days that infants remained in the hos pital over the first 2 years of life averaged 23 ±40.
Infants with BPD had a greater incidence of hospital admission than those without chronic lung disease (33/74 [45%] vs 14/56 [25%], respectively,
P < .05). Those with BPD were more likely to have
multiple readmissions (26% vs 5%, P < .01) and a prolonged cumulatjve hospital stay of 30 days
(12% vs 0%, P < .01). A previous history of BPD
did not, however, influence the level of respiratory care and mortality during rehospitalization. Infants with and without BPD were equally likely to require
supplementaloxygen (23/33 [70%] vs 12/14
[86%], respectively) and mechanical ventilation (8/ 33 [24%] vs 4/14 [29%]) during acute respiratory illness. Three infants with BPD (9%) and one in fant without BPD (7%) died during rehospitaliza tion.
Despitethe importanteffectsof BPD on subse
quent respiratory morbidity, it is important to note that the incidence of rehospitalization was signifi cantly increased as a result of prematurity per se. Twenty-five percent of preterm infants without BPD required rehospitalization—a 10-fold increase
over socioeconomically matched full-term infants.
Furthermore,of the preterminfantswhorequired
no mechanical ventilation beyond the day of birth, 10 (23%) of 43 required rehospitalization (Table 2).
SeasonalPatternof Hospitalization
In addition to the severity of lung disease, the risk of rehospitalization was correlated with season
of NICU discharge and the interval between NICU
discharge and the first winter season. Fifty-five (52%) of the 106 hospital admissions occurred dur ing the 4-month period between January and April (Fig. 1). This was the period during which respira tory syncytial virus (RSV) was prevalent in the
communities; 15 of the 19 documented RSV infec tions in our population occurred during these months (Fig. 1). Rehospitalization was also more
likely to occur shortly after NICU discharge.
Thirty-eight (81%) ofthe 47 rehospitalized children required their first hospital admission within 4 months of NICU discharge. Consequently, those infants most likely to require rehospitalization dur ing their first 4 months were those discharged be tween September and December (the months im mediately preceding their first RSV season). Sev
enteen (41%) of these 42 infants required early
rehospitalization in contrast to 6 (15%) of 39 in fants discharged from the NICU from May throughAugust (P < .05) (Fig. 2). The group discharged
January through April had an intermediate risk of rehospitalization (31%), as infants in this group who were discharged in January had a rehospitali zation rate similar to the September through De
cembergroup(42%)while infants dischargedin the
later months were less likely to require rehospitalization (27%). In addition, the infants discharged
during the summer months (May through August) who escaped early rehospitalization were thereforemore than 5 months of age during their first winter
at home. None of these infants required hospitali
zation during January through April of that first
year of life. Therefore, season of discharge and age
duringsubsequent
winterrespiratoryviral seasons
ARTICLES 529
at Viet Nam:AAP Sponsored on September 1, 2020
www.aappublications.org/news
TABLE 2. Duration of Ventilation Required for All Infants
Rehospitalizationand
Those RequiringDuration
of Mechanical VentilationTotal
No. of InfantsMean
Gesta tional Age, wk*No.
(%) of Infants With Rehospitali zation(s)@24
h 1—7d 7—28d >28 d43
21 25 4129.7
29.4 27.9 26.310
(23) 7 (33) 10(40) 20 (49)
* Mean gestational age of infants rehospitalized was not significantly different from that
of infants without rehospitalizations.
[11%], P < .01) at 6 months of age. This was reflected in significantly lower motor indices on the
Bayley Scalesof Infant Development.These differ enceswere no longer apparent at subsequentages
(Table 3). Infants rehospitalized prior to 6 months
and those never rehospitalized were similar with regard to growth, neurologic abnormalities, and
performance on the Bayley Mental and Motor
scalesat both 15 and 24 months of age.
DISCUSSION
We found that the high incidence of rehospitali
zation for respiratory illness among preterm infants of <32 weeks' gestation was not limited to infants
with chronic lung disease. While 45% of infants with BPD were rehospitalized, 25% of infants with
out BPD required hospital admission. The rate for this latter group was 10-fold greater than that of a matched control group of term infants.
A high rate of rehospitalization for infants with BPD has been documented previously; however, the
percentage of patients requiring repeated hospital ization has varied greatly from study to study. Investigators have found rehospitalization rates
rangingfrom 40% to 86%.46h112These ratesare not
inconsistent with our finding of 45%. The variabil ity of findings in this regard may be attributed to
inconsistencyin studydesign,especiallyin the def
inition of BPD used by various investigators. In
addition, the duration of follow-up ranged from 4
months to 2 years. It is clear, however, that preterm infants with chronic lung disease are likely to re
quire rehospitalization early in life.
Although it has been reported that preterm in fants without residual lung disease have no greater
risk of serious respiratory illness than do term infants, those studies evaluated infants born prior to i971.@'@'@ These earlier studies evaluating mor bidity among respiratory distress syndrome survi
vorsweredoneusinga patient populationwith very low survival rates—only 18% of all preterm infants who required ventilatory support survived the mi
tial hospitalization in one series.13 Therefore, these
U ALLADMISSIONS
U RESPIRATORYSYNCYTIALVIRUSISOLATED
o@4
-J
@ @- ,_ > 0 Z
@
@ >.
@
U)
@ a. 8 0 LU (
-) w
Month
Fig 1. Numberof rehospitalizationsfor respiratoryill
ness for preterm infants by month.
50
(I) C
F
sept-doc Jan.*pr may-aug
month of NICU discharge
Fig2. Rehospitalizationfor respiratoryillnesswithin4
months of neonatal intensive care unit (NICU) discharge: relationship to month of discharge.
@ J@< .05, infants
discharged September through December were more
likely to require early readmission than those discharged May through August.
had profound impacts on incidence of rehospitali
zation.
Neurodevelopmental Follow-up
The 33 preterm infants who required rehospital ization(s) for respiratory illness prior to their first developmental follow-up assessment at 6 months
of age were compared with the 83 infants who required no such hospital admission during their first 2 years of life. The infants who required early
hospitalization had more than twice the incidence of neurologic abnormality (12/33 [36%] vs 9/83
ii
2O@
10
4O@
3O@
2O@
TABLE3. NeurodevelopmentalOutcomeof I
Never Rehospitalized*nfants
Requiring Early Rehospitalization ComparedWith InfantsEvaluation
at 6 moEvaluation at 15 moEvaluation at 24 moRehospitalizedNotRehospitalizedNotRehospitalizedNot(n
= 33)Rehospitalized (n=83)(n
= 33)Rehospitalized (n=81)(n
= 32)Rehospitalized (n=81)
10 (30)15(25)9 (18)5 (15)12 (15)7 (22)20
(27)14 (17)7 (21)15 (19)7 (22)18
(22)3
(9)7 (8)4 (12)10 (12)7 (22)15 (19)
Length <5 percentile, no. (%)
Weight <5 percentile, no. (%)
Head circumference <5 percentile,
no. (%)
Bayley MDI (mean ±SD) 97 ±21 101 ±17 99 ±21 97 ±20 92 ±23 94 ±20
Bayley PD! (mean ±SD) 89 ±18t 97 ±14t 92 ±24 99 ±20 85 ±22 89 ±16
Neurologic abnormality, no. (%) 12 (36)@ 9 (11)@ 7 (21) 9 (11) 6 (19) 6(7)
* The 10 infants first rehospitalized after 6 months of age, as well as the 4 infants who died of respiratory illness, were
not included in this comparison. MDI, Mental Developmental Index; PD!, Psychomotor Developmental Index.
t P < .05.
:I:P< .01.
infants cannot be considered to be representative
of infants who now leave the nursery alive.
More recent investigators have studied infants without chronic lung disease and found readmission
for respiratory illness required for 11% to 33% of patients.―6―5 There is, however, considerable var
iability in infant selectionfor study. Factors that are likely to alter the risk of rehospitalization in dude the gestational age of infants included and the overall survival of the cohort. Additionally, if only infants with severe residual lung disease are
definedas havingBPD, then the groupwithout
BPD will include many infants with mild to mod erate symptoms, in whom respiratory morbidity is more likely to develop. Within the population in
cludedin ourstudy,thegestational
ageoftheinfant
was itself not a risk factor for readmission. It seems
likely, however,that infants of 32 to 36 weeks'
gestation and those of 36 to 40 weeks' gestation have different rates of rehospitalization than the infants studied. Results of studies that include pa
tients of more advanced gestational ages cannot be
assumed to apply to the very preterm infants. In creasing rates of rehospitalization for respiratory illnessaccompanyingincreasingsurvivalof preterm infants hasbeenshownpreviouslyby Mutch et al'6 in a study comparing very low birth weight (VLBW;
s1500 g) infants born between 1968 and 1972 with a similar cohort born between 1974 and 1978. As survival increased from 35% to 48%, rates of rehos pitalization for respiratory infections increased from 9.8% to 15.5%. In the present study, survival was 85% and rehospitalization rates for respiratory
illness showed a corresponding increase to 36%
overall.
An increased frequency of respiratory viral infec tion during the winter months is expected among pediatric patients. Full-term healthy children born
duringthe 6 monthsprior to and includingthe
month of peak RSV infection have been shown to be more likely to require hospitalization than those infants born during the remainder of the year.'7 To our knowledge, a seasonal pattern has not been shown previously among preterm infants. We have found that infants discharged shortly before the
peak respiratory viral seasonare most likely to
require early rehospitalization. It is likely that preterm infants are at greater risk soon after hospital
discharge secondary to many factors including
smallsize,residualpulmonaryabnormalities,
and
lower amounts of maternal IgG transferred trans placentally.
At the time of NICU discharge, parents are often counseled concerning the means by which the need for repeated hospitalization may be avoided. Ex
posureto tobaccosmoke,to individuals with viral
illness, and to crowds is discouraged, and breastfeedingmaybeadvocated.Unfortunately,datawere
not available regarding these and other important confounding variables including family history of allergies, exposure to day care, and presence of other children in the household. Nevertheless, theincreasedrisk for rehospitalization
amongthose
infants discharged from the NICU during the fall
months,asdemonstrated
in thisstudy,shouldbea
persuasive
argumentto emphasize
the importance
of protecting these infants in particular.
The severity of illness documented in our pa tients who were admitted demonstrates that con cern among practitioners about the potential seri ousness of respiratory illness in preterm infants is
justified.The majorityof the admissions
seenin
this study were for significant respiratory illness.
Seventy-fivepercentof all infantsrehospitalized
requiredinitiationof oxygentherapyand 26% of
those admitted required mechanical ventilation
duringoneor morehospitalizations.
ARTICLES 531
at Viet Nam:AAP Sponsored on September 1, 2020
www.aappublications.org/news
Few investigators have examined the relationship
between rehospitalization in infants and their neu
rodevelopmental outcome. McCormick et al'5 re ported that among 95 VLBW infants who were
rehospitalized
for any reasonduringthe first year
of life,53 (56%)hadmoderateto severecongenital
anomaliesor developmental
delayat 12monthsof
age. In contrast, among 164 VLBW infants born
duringthe sameyearwhodid not requirerehospi
talization,only 40 (25%) had a pooroutcome.In
that study 47% were hospitalized for respiratory
problems.Furthermore,nearly20% of the rehos
pitalizationswereas a consequence
of congenital
abnormalitiesor developmental
delay,whichcon
foundsthe relationshipwith developmental
out
come. Hack et al' found that among a cohort of 90 VLBW infants born in 1977, 30 required rehospi
talization(s) during their first year of life. Neuro
developmental outcome at 8 and 20 months of age was similar for nonhospitalized infants and thosehospitalizedfor acuteillnessincludinguncompli
catedrespiratoryinfections.Pooreroutcomewas
found only in a small subgroup of VLBW infants
rehospitalized for chronic complications of prema turity. We have demonstrated that although there
are greater numbers of neurologic abnormalities
and lower standardized test scores at 6 months
amonginfants rehospitalizedfor respiratoryillness
prior to that time, there is no measurable differencein neurodevelopmental
outcomeby 15 monthsof
age. The finding at 6 months may be a reflection of the prolonged neonatal course among infants re
quiring early rehospitalization rather than of the
readmissionitself.
IMPLICATIONS
Rehospitalization for respiratory illness contrib utes significantly to the morbidity and mortality associated with prematurity. As the care and sur vival of preterm infants change, the morbidity among survivors needs periodic reevaluation. It is
clear from this study that even preterm infants
without neonatal lung disease are at significant risk for serious respiratory illness requiring rehospital ization over the first 2 years of life and wouldpotentially benefit from strategiesto prevent RSV
and other respiratory infections.We thank Michele M. Choyke for secretarial assist ance.
REFERENCES
1. Hack M, DeMonterice D, Merkatz IR, Jones P, Fanaroff A. Rehospitalization ofthe very-low-birth-weight infant: a con tinuum of perinatal and environmental morbidity. AJDC. 1981;135:263—266
2. Meyers MG, McGuiness GA, Olson DB, et a!. Respiratory illnesses in survivors of infant respiratory disease syndrome. Am Rev Respir Dis. 1986;133:1011—1018
3. Outerbridge EW, Nogrady MB, Beaudry PH, Stern L. Idi opathic respiratory distress syndrome: recurrent respiratory illness in survivors. AJDC. 1972;123:99—104
4. Groothuis JR, Gutierrez KM, Lauer BA. Respiratory syn cytial virus infection in children with bronchopulmonary dysplasia. Pediatrics. 1988;82:199—203
5. Sauve RS, McMillan DD, Young L, et al. Home oxygen therapy: outcome of infants discharged from NICU on con tinuous treatment. Clin Pediatr (Phila). 1989;28:113—118 6. Sauve RS, Singhal N. Long-term morbidity of infants with
bronchopulmonary dysplasia. Pediatrics. 1985;76:725—733 7. Dubowitz LMS, Dubowitz V, Goldberg C. Clinical assess
ment of gestational age in the newborn infant. J Pediatr. 1970;77:1—10
8. Ellison PH, Horn JL, Brouning CA. Construction of an
infant neurological international battery (INFANIB) for the assessment of neurological integrity in infancy. Phys Ther. 1985;65:1326—1331
9. Growth charts 1976. Monthly Vital Statistics Report. Wash ington, DC: National Center for Health Statistics; Health Resources Administration; 1976;25(3) suppl (HRA) 75—1120 10. Bayley N. Bayley Scales of Infant Development. New York,
NY: Psychological Corp; 1969;1-78
11. Morgan MEl. Late morbidity of very low birthweight in fants.Br Med J. 1985;291:171—173
12. Yu VY, Orgill AA, Astbury J, et al. Growth and development of very low birthweight infants recovering from broncho pulmonary dysplasia. Arch Dis Child. 1983;58:791—794 13. Harrod JR, Heuruex P, Wanginsken OD, Hient CE. Long
term follow-up of severe respiratory distress syndrome treated with IPPB. J Pediatr. 1974;82:277—286
14. Lamarre A, Linsao L, Reilly BJ, Swyer PR, Levison H. Residual pulmonary abnormalities in survivors of idiopathic respiratory distress syndrome. Am Rev Respir Drs. 1973; 108:56-61
15. McCormick MC, Shapiro S, Starfield BH. Rehospitalization in the first year of life for high-risk survivors. Pediatrics. 1980;66:991-999
16. Mutch L, Newdick M, Lodwick A, Chalmers I. Secular changes in rehospitalization ofvery low birth weight infants. Pediatrics.1986;78:164—171
17. Glezen WP, Paredes A, Frank AL, et al. Risk of respiratory syncytial virus infection for infants from low-income fami lies in relationship to age, sex, ethnic group, and maternal antibody level. J Pediatr. 1981;98:708—715
1991;88;527
Pediatrics
Coleen K. Cunningham, Julia A. McMillan and Steven J. Gross
Rehospitalization for Respiratory Illness in Infants of Less Than 32 Weeks' Gestation
Services
Updated Information &
http://pediatrics.aappublications.org/content/88/3/527 including high resolution figures, can be found at:
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or in its
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml Information about ordering reprints can be found online:
at Viet Nam:AAP Sponsored on September 1, 2020
www.aappublications.org/news
1991;88;527
Pediatrics
Coleen K. Cunningham, Julia A. McMillan and Steven J. Gross
Rehospitalization for Respiratory Illness in Infants of Less Than 32 Weeks' Gestation
http://pediatrics.aappublications.org/content/88/3/527
the World Wide Web at:
The online version of this article, along with updated information and services, is located on
American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.