Research Article
Anaemia as a Risk Factor for Maternal-Perinatal Complications and Pregnancy
Outcomes in Pregnant Womens
P. V. Ingle1, S. D. Patil2, *J. M. Patel3, P. N. Dighore4, S. J. Surana3
1.Department of Pharmacy Practice, School of Pharmacy, International Medical University, Kuala Lumpur, Malaysia.
2.Department of Pharmacology, H. R. Patel Institute of Pharmaceutical Education & Research, Shirpur-425405, Dhule, Maharashtra, India.
3.Department of Clinical Pharmacy, R. C. Patel Institute of Pharmaceutical Education & Research, Shirpur-425405, Dhule, Maharashtra, India.
4.Department of Medicine, Indira Gandhi Memorial Hospital, Shirpur-425405, Dhule, Maharashtra, India. ABSTRACT
Objective: To study the prevalence and the impact of anaemia on maternal-perinatal complications and
pregnancy outcomes in pregnant women. Materials & Methods: In prospective-observational study, 450 pregnant women were grouped as anaemic and Non-anaemic based up on their third trimester hemoglobin level. Maternal perinatal complications and pregnancy outcomes were observed for both anaemic and Non-anaemic group. Anaemic women having hemoglobin value ˂ 11 g/dL while non-anaemic women having hemoglobin value ≥ 11 g/dL. Patients were asked for their diet, socioeconomic condition, medical history, obstetric history and associated diseases. Results: Pregnant women with anaemia had higher incidence of Maternal-perinatal complications compared to non-anaemic women. Anaemic women had high incidence of preterm delivery, pregnancy induced hypertension, pyrexia, low birth weight baby, meconium staining of amniotic fluid, and birth asphaxia. Majority of complications were found more in anaemic women compared to non-anaemic women. Conclusion: Maternal anaemia is associated with pregnancy complications. It is recommended that, women should be educated more about the pregnancy risk factors and encouraged to begin their antenatal clinic early in pregnancy.
Keywords: Anaemia, pregnancy, maternal-perinatal complications, pregnancy outcomes
Received 15 Aug 2015 Received in revised form 28 Aug 2015 Accepted 1 Sept 2015
*Address for correspondence: J. M. Patel,
Department of Clinical Pharmacy, R. C. Patel Institute of Pharmaceutical Education & Research, Shirpur-425405, Dhule, Maharashtra, India.
E-mail: jayshreepatel310@gmail.com
INTRODUCTION
Anaemia is a global public health problem affecting both developing and developed countries with major consequences for human health as well as social and economic development [1, 2]. Anaemia is the most frequently observed nutritional disease in the world. According to World Health Organization (WHO), anaemia during pregnancy is defined as a haemoglobin concentration ˂ 11 g/dL [3]. Prevention of anaemia during pregnancy is helpful to reduce the complications. There are several measures taken by the government to reduce the prevalence of anaemia such as National Anaemia Prophylaxis Programme (NAPP), National
in women and children, decreased capacity to learn, and reduced productivity in all individuals. The consequence of a mild form of anaemia is not yet clearly recognized. Anaemia of pregnancy is known to cause increased maternal morbidity and mortality increased foetal morbidity and mortality and, increased risk of low birth-weight [11-15].
MATERIALS & METHODS
A prospective-observational study, comparing all pregnant women with and without anaemia, attending the gynecological department of Indira Gandhi Memorial Hospital, shirpur, Maharashtra, at the time of labor from August 2010 to March 2011 were enrolled in this study. A total of 450 women were included in this study. According to WHO, maternal anaemia is defined as hemoglobin ˂ 11 g/dL during pregnancy. On the basis of hemoglobin level in third trimester performed by sahli’s method, women were categorized in two groups:
I. Anaemic: Normal hemoglobin, ˂ 11 g/dL. II. Non-anaemic: Hemoglobin, ≥ 11 g/dL Patients were recruited according to inclusion and exclusion criteria of the study. In this study only women who referred to higher centre were excluded. For the perinatal complications follow-up was taken at the seven day after delivery. Data were collected from the OPD cards of the patients, laboratory data and from verbal communication with women. The following characteristics were analyzed: maternal age, parity, gestational age at delivery, diet, socio-economic condition, medical history, associated diseases, gender of newborn and birth weight. Obstetric characteristic analyzed were: cesarean section, recurrent abortions, intra uterine growth restriction (IUGR), Placenta previa, placental abruption, pregnancy induced hypertension (PIH) [16], premature rupture of membrane (PROM), hemorrhage. The Institutional Ethics Committee of R. C. Patel Institute of Pharmaceutical Education & Research; approved the study protocol. Informed consent was taken from the patients before inclusion into the study. In this study parameter like, age, gestational age, hemoglobin (Hb), total leucocyte count,
platelet count, and blood pressure was measured. Hemoglobin was measured by sahli’s (acid hematin) method. Total leucocyte count and platelet count were performed manually. Seating blood pressure was measured on every follow-up. Statistical analysis was performed by using PRISM- 4. In order to establish the statistical significance, the data were compared by applying the student’s‘t’ test. The probability ‘p’ value less than 0.05 was considered statistically significant.
RESULTS
Total of 450 patients were selected in the study (Table 1). Among them 19.11% (n=86) had hemoglobin above 11g/dL, 67.03% (n=244) had mild anaemia, 24.66% (n=111) had moderate anaemia, and 2% (n=9) had severe anaemia. The overall prevalence of anaemia in this study was 81%.
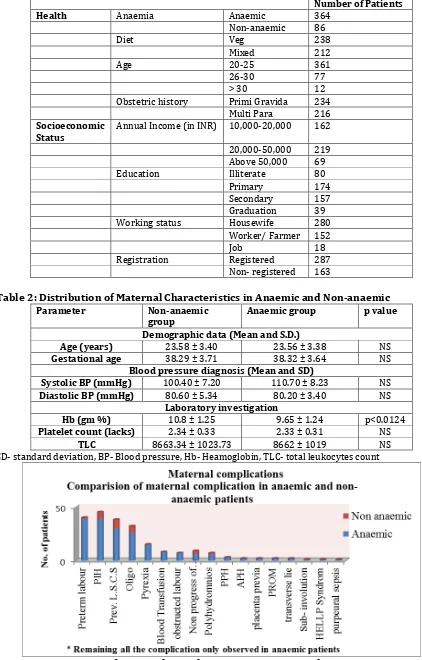
The mean ± standard deviation for age, gestational age, total leucocyte count, platelet count, Blood pressure (B.P.) of both the group is shown in (Table 2). The mean gestational age in anaemic and non-anaemic was found to be 38.32 ± 3.64 and 38.29 ± 3.71, respectively. The mean systolic blood pressure in anaemic and non-anaemic was found to be 110.70 ± 8.23 and 100.40 ± 7.20, respectively. No stastically significant difference was found between two groups. To assess the impact of anaemia on complication, the Comparision of complication was done in both anaemic and non-anaemic patients. In the present study all the complications were found in both group but the proportion of complication is more in anaemic patient (87%) as compare to non-anaemic patients. There are some complications that are only found in anaemic patients such as, pyrexia, blood transfusion, postpartum hemorrhage, Antepartum hemorrhage, PROM, Placenta previa, sub-involution, transverse lie, HELLP syndrome, and puerperal sepsis (Figure 1 & Table 2).
Table 1: Total Number of Cases Collected
Number of Patients
Health Anaemia Anaemic 364
Non-anaemic 86
Diet Veg 238
Mixed 212
Age 20-25 361
26-30 77
> 30 12
Obstetric history Primi Gravida 234 Multi Para 216 Socioeconomic
Status Annual Income (in INR) 10,000-20,000 162
20,000-50,000 219 Above 50,000 69
Education Illiterate 80
Primary 174
Secondary 157 Graduation 39 Working status Housewife 280
Worker/ Farmer 152
Job 18
Registration Registered 287 Non- registered 163
Table 2: Distribution of Maternal Characteristics in Anaemic and Non-anaemic
Parameter Non-anaemic
group Anaemic group p value
Demographic data (Mean and S.D.)
Age (years) 23.58 ± 3.40 23.56 ± 3.38 NS
Gestational age 38.29 ± 3.71 38.32 ± 3.64 NS
Blood pressure diagnosis (Mean and SD)
Systolic BP (mmHg) 100.40 ± 7.20 110.70 ± 8.23 NS
Diastolic BP (mmHg) 80.60 ± 5.34 80.20 ± 3.40 NS
Laboratory investigation
Hb (gm %) 10.8 ± 1.25 9.65 ± 1.24 p<0.0124
Platelet count (lacks) 2.34 ± 0.33 2.33 ± 0.31 NS
TLC 8663.34 ± 1023.73 8662 ± 1019 NS
SD- standard deviation, BP- Blood pressure, Hb- Heamoglobin, TLC- total leukocytes count
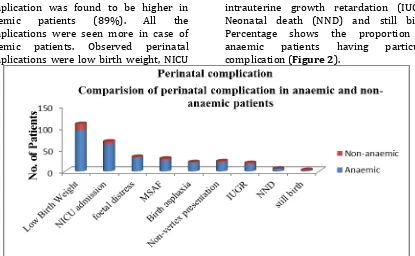
In the study, among 450 patients 202 patients (45%) having perinatal complication. Among this the proportion of complication was found to be higher in anaemic patients (89%). All the complications were seen more in case of anaemic patients. Observed perinatal complications were low birth weight, NICU
admission, foetal distress, Meconium stained amniotic fluid (MSAF), birth asphaxia, non-vertex presentation, intrauterine growth retardation (IUGR), Neonatal death (NND) and still birth. Percentage shows the proportion of anaemic patients having particular complication (Figure 2).
Figure 2: Comparison of Perinatal Complications in Anaemic and Non-anaemic Patients Here, we divided all the patients in four
different groups as per the severity of anaemia: Mild, Moderate, Severe, and Control. Study data shows that the proportion of complication was increases as the severity of anaemia is increases. Although the most of the patients having the mild forms of anaemia only 49%
patients have complications, where as in severe form of anaemia 89% patients having these complications. Highest proportion of complication was found in patients having the severe forms of anaemia. In control group (Non-anaemic), 32% patients having complications.
Figure 3: Comparision of Proportion of Complications in Varying Degree of Anaemia The diet of women during pregnancy
generally affects their hemoglobin count. It is a normal notion that the non-vegetarians
to be having pure vegetarian and 212 (47.11%) patients were found to be mixed type of diet. Patients who take non-vegetarian diet two or more times in a week were grouped in mixed diet category. The majority of patients in this study were vegetarian.
However, data indicates the proportion of anaemic women was more in the vegetarian group (212 patients, 89.07%) as compare to patients having the mixed type (152 patients, 71.69%) of diet.
Also, in this study mothers were grouped in three categories: Poor, Middle, and Rich, according to their socioeconomic conditions. These categories were based on their income per annum. A woman having their income per annum in between Rs.10, 000-20,000 comes in poor category, like wise women having income per annum in between Rs.20, 000 - 50,000 and who have income above Rs.50, 000 comes in the middleclass and Rich category respectively. The data collected reveled that, maximum percentage (49%) of women comes from the middle class, whereas the highest percentage (91.35%) of the anaemic women was found to be in poor category, and the proportion of the anaemic women decreases as the socio-economic condition increases.
We also study the correlation between anaemia and parity and we found that among 450 patients, 234 (52%) patients were primipara and 216 (48%) patients were multipara. In present study, data revealed shows that percentage of anaemic patients in primipara and multipara were 80% and 81%, respectively. No significant statistically difference was found between primipara and multipara.
DISCUSSION
The prevalence of anaemia in rural area near to shirpur was found to be high (81%) in pregnant women. In the study parameters like age, gestational age, blood pressure, platelet count, and total leucocyte count but no statistically significant results were found between two groups. This indicates that these factors not responsible for the anaemia during pregnancy.
In this study to assess the effect of anaemia on pregnancy complication comparision
anaemic patients. We found that the rate of complication was higher in case of anaemic women as compare to non-anaemic women. Statistically significant results (p ˂ 0.005) were found between anaemic and non-anaemic women indicates that anaemia during pregnancy is responsible for pregnancy complications.
In this study; we tried to correlate the risk factor for the anaemia during pregnancy. For that we studied the diet habits of women, socioeconomic condition, parity and education. Statistically significant differences between anaemic and non-anaemic women for the diet, socioeconomic condition, and education indicates that these factors are related to anaemia while parity does not show any significant difference between two groups.
CONCLUSION
It was concluded from the study that the prevalence of anaemia among the pregnant women in the rural area near to shirpur was relatively high. Study also suggests that, the moderate and severe type of anaemia during pregnancy significantly associated with the pregnancy complications. Mild type of anaemia was not directly associated with pregnancy complications. Study also suggest that there is a need of some anaemia prevention programme particularly in rural area where the people does not know what is anaemia and its impact on pregnancy.
REFERENCES
1.Adam I, Khamis AH, and Elbashir MI: Prevalence and risk factors of anaemia in pregnant women of eastern Sudan. Transactions of the Royal Society of Tropical Medicine and Hygiene 2005; 99: 739-743. 2.Gautam VP, Bansal Y, Taneja DK, Saha R:
Prevalence of anaemia amongst pregnant women and its socio-demographic associates in a rural area of Delhi. Indian Journal of Community Medicine 2002; XXVII (4): 157-160.
3.WHO global Data base on anaemia (www.who.org.)
4.Narasinga Rao BS: Prevention and Control of Anaemia in India Theory and Practice 2009; Nutrition Foundation of India. Available on http://nutritionfoundationofindia.res.in/archi ves.asp?archiveid=17 [assessed on 17th December]
5.Malagi U, Reddy M and Naik RK: Evaluation of National Nutritional Anaemia Control Programme in Dharwad. Journal of Human Ecology 2000; 20(4): 279-281.
6.Kalaivani K, Prevalence & consequences of anaemia in pregnancy. Indian journal of medical research 2009; 130: 627-633.
7.PV Ingle, AG Gandhi, PH Patil, SJ Surana. Iron Deficiency Anemia: Perspectives in Indian Pregnant Women. Research Journal of
Pharmaceutical, Biological and Chemical Sciences. 2011, July-September, 2 (3):1036-1047.
8.Malhotra M, Sharma JB, Batra S, Sharma S and Murthy NS: maternal and perinatal outcome in varying degrees of anaemia. International Journal of Gynecology and Obstetrics 2002; 79: 93–100.
9.Agarwal K, Agarwal D, Sharma A, Sharma K, Prasad K, Kalita M, Khetarpaul M, Kapoor A, Vijayalekshmi L, Govilla A, Panda S, and Kumari P: Prevalence of anaemia in pregnant & lactating women in India. Indian journal of medical research 2006; 124: 173-184.
10.Ahmad N: The prevalence of anaemia and associated factors in pregnant women in a rural Indian community. Australasian Medical Journal 2010; 1(1): 276-280.
Available on
http://www.faqs.org/periodicals/201004/2 055045581.html.
11.Levy A, Fraser D, Katz M, Mazor M and Sheiner E: Maternal anemia during pregnancy is an independent risk factor for low birth weight and preterm delivery. European Journal of Obstetrics & Gynecology and Reproductive Biology 2005; 122:182-186.
12.Fareh OI, Rizk DEE, Thomas and Berg B: Obstetric impact of anaemia in pregnant women in United Arab Emirates. Journal of Obstetrics and Gynaecology 2001; 25(5): 440-444.
13.Hamalainen H, Hakkarainen K and Heinonen S: Anaemia in the first but not in the second or third trimester is a risk factor for low birth weight. Clinical Nutrition 2003; 22(3): 271-275.
14.Malhotra M, Sharma J, Batra S, Sharma S, Murthy N, and Arora R: Maternal and perinatal outcome in varying degrees of anaemia. International Journal of Gynecology and Obstetrics 2002; 76, 93-100.
15.Patra S, Pasrija S, Trivedi SS, and Puri M.: Maternal and perinatal outcome in patients with severe anaemia in pregnancy. International Journal of Gynecology and Obstetrics 2005; 91: 64-165.
16.Pravin Ingle, Bhavin Patel, Prakash Patil. Comparative Clinical Study on Efficacy and Safety of Olmesartan Medoxomil in Combination with Hydrochlorothiazide and Amlodipine in the Treatment of Patients with Mild to Moderate Hypertension. Journal of Pharmacy Research 2010 Nov, 3(11): 2706-2708.
Oxford University press, 3rd ed, 2000. Available at www. Maternitywise.org/prof. 18.Ingle P. V., Chaudhari S. L. , Dighore P. N.,
Surana S. J. Sociocultural, Healthy Nutrition & Eating, Exercise Pattern and Use of Ayurvedic Medicines in Pregnancy. Indian Journal of Pharmacy Practice. 2012, Jul - Sep, 5(3):5-12. 19.Ingle PV, Nawal UR, Dighore PN, Surana SJ. Comparison of Serum Homocysteine and Serum Vitamin B12 Level in Adults with Pure Vegetarian and Mixed dietarian Habit. Indian Journal of Pharmacy Practice. 2011, Jul - Sep, 4(3):20-24.