Differentiation between postoperative scar and recurrent disk herniation: prospective comparison of MR, CT, and contrast enhanced CT
Full text
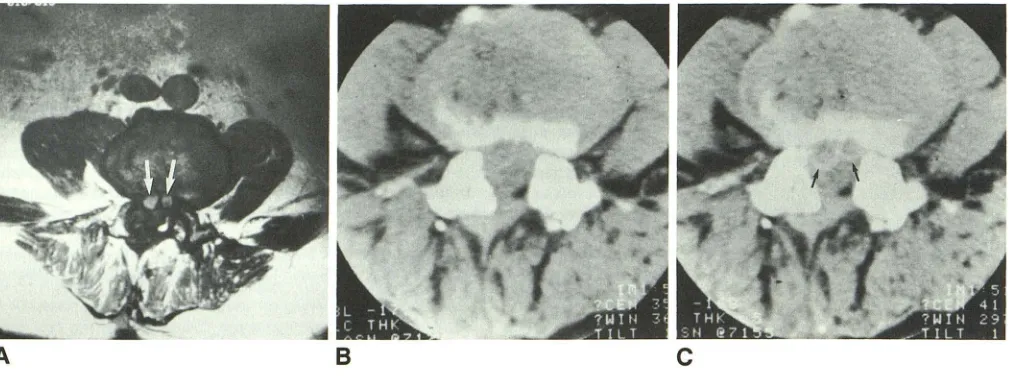
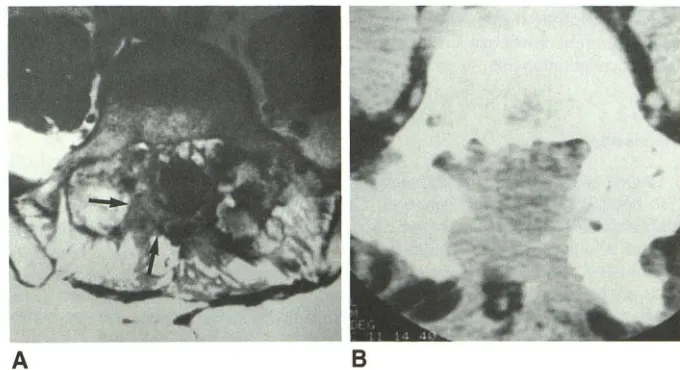
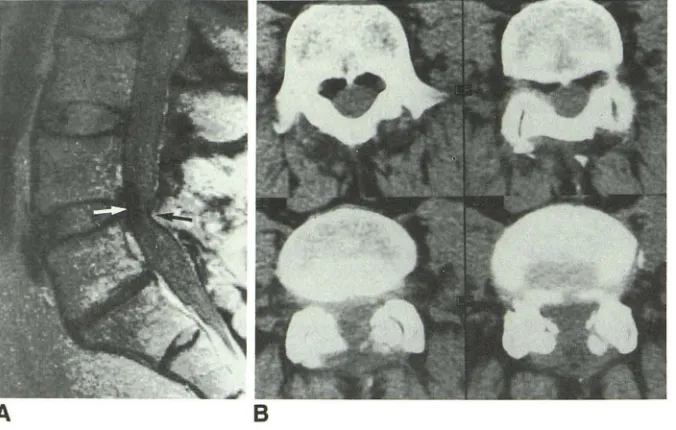
Figure
Related documents
[11] Many liquid chromatographic methods have been applied for quantification of SN- 38 in human plasma, [12] simultaneous determination of lactone and carboxylate forms in
Further, we observed that miR-21-5p mimic transfection decreased the LCRG1 pro- tein in human laryngeal carcinoma Hep2 cells as indicated by Western blotting analysis, and promoted
Conclusion: Antiphospholipid antibodies high correlated with increased Anti Rubella antibodies in pregnant women but low relation.. between of apL with abortion in
The XRD analysis of the different Ni nanoparticles showed the formation of Ni/NiO nanoparticles with face centered cubic structure and average particle size was
Each mouse was subjected to the motor function score (MFS) test on 14 day. Data were represented as mean of MFS+ SEM for 5 mice in each group. 5) Effect of I 1 antagonist
MiR-181d functions as a potential tumor suppressor in oral squamous cell carcinoma by targeting K-ras.. Yuyuan Shi 1 , Ying Li 2 , Wei Wu 1 , Bing Xu 1 , Jing
Our results suggested that miR- 200a regulated cell viability and invasion of ESCC cells in vitro via regulating its target ge- ne RKIP expression. This regulatory effect was
DHQ reduced inflammatory responses from APAP-induced acute liver injury in mice through the detection of the levels of TNF-α (A) and IL-6 (B) in liver tissue by an ELISA and