Introduction
Until a few years ago, obesity was considered a condition associated to a high wellbeing. In fact, countries in which obesity was a relevant public health problem were the industrialized ones and in particular the United States and Europe. Unfortunately, during the last decades, data show that a rise in the prevalence of obese people has also occurred in developing countries such as Mexico, China and Thailand [1].
Today, obesity can be considered in most Organization for Economic Cooperation and Development (OECD) and European Union (EU) countries as an unprecedented public health challenge which has been underestimated, poorly assessed and not fully accepted as a strategic governmental problem with substantial economic implications [2].
Overweight affects between 30% and 80% of adults in the different countries of the World Health Organization (WHO) European Region and up to one third of children (OECD countries
show similar data). According to the WHO data [3] and to the International Obesity Task Force Organization [4], in 2005 and all around the world, more than one billion people were overweight and about three hundred million people obese; the alarming data is that, according to some assessments, 22 million young people (aged less than fifteen years) are obese, with an increasing trend.
Preventing obesity, as well as promoting health, are therefore urgent public health goals that should be dealt with through innovative environmental approaches [2]. In the light of such views, obesity cannot be considered anymore as an individual illness, but rather as the result of many environmental and socio-economic factors which highly influence dietary habits and lifestyles [1].
In view of this, the overall aim of this paper is to update the picture resulting from previous surveys, given the rapid pace at which policies are developing in the area concerned, and to expand this picture, both in terms of geographical
Review of policies adopted in 34 Countries to improve diet and physical activity
Anna Ceccarelli
Faculty of Economics, Catholic University of the Sacred Heart, Rome, Italy
Correspondence to: Anna Ceccarelli, Faculty of Economics, Catholic University of the Sacred Heart, Largo F. Vito 1, 00168 Rome, Italy. E-mail: anna.ceccarelli@rm.unicatt.it
Abstract
Background: Today, obesity can be considered in most OECD and EU countries as an unprecedented public health challenge which has been underestimated, poorly assessed and not fully accepted as a strategic governmental problem with substantial economic implications.
The aim of this paper is to provide a review of the major policy statements on diet and physical activity adopted in 34 OECD and other EU countries until 2008, and to point out similarities and differences between country approaches and factors that may explain them.
Methods: Information about policies and interventions was mainly retrieved from official sources such as the WHO Regional Office for Europe nutrition policy database, and websites of Health Ministries and national public health institutions.
Results: The review pointed out that almost all WHO and OECD Member States have government-approved policies on nutrition and food safety. Although countries have large data and documents on overweight and obesity, they do not seem to rely on them to define clear strategies and plans for action which, as a result, are often vague and unspecific.
Conclusions: In order to reverse the obesity trend down to decent levels and to reach the lower socio-economic groups, concerted, multisectorial, long-term actions are needed in combination with a much larger political determination.
coverage and analysis of cross-cutting themes. In particular, through the analysis of the major policy statements on diet and physical activity adopted in 34 OECD and other EU countries, similarities and differences between country approaches and factors that may explain them were pointed out.
First, the background to such survey and the findings of previous studies will be illustrated, thus the methods used will be described, and finally a preliminary set of findings will be presented and discussed.
Background
Obesity can be defined simply as the disease in which excess body fat has accumulated to such an extent that health may be adversely affected [5]. However, the amount of excess fat, its distribution within the body, and the associated health consequences vary considerably among obese individuals. In adults, excess body weight is defined as having a body mass index (BMI) ≥
25 kg/m2. Obesity is defined as a BMI ≥ 30 kg/m2; pre-obese is used to define adults with a BMI of 25.0–29.9 kg/m2. For children and adolescents, there are various different approaches to defining overweight and obesity [6]. This document will use the definition that corresponds to a BMI of 25 and 30 kg/m2 at age 18 years [7].
Facts and figures on obesity
Lifestyles have considerably changed in developed countries over the recent decades. Some changes have been associated with improvements in health status and life expectancy, as in the case of tobacco consumption, which has been decreasing in many countries since the 1950s. In other cases, lifestyles have become a threat to individual health. For instance, changing diets and increasingly sedentary lifestyle, particularly in the last thirty years, have contributed to a generalised increase in body weight. Spreading obesity has been associated with growing rates of chronic diseases, possibly affecting longevity [8]. In fact, excess body weight poses one of the most serious public health challenges of the 21st century at least in OECD and EU countries, where the prevalence of obesity has tripled in the last two decades and has now reached epidemic proportions, even in countries with traditionally low rates of overweight and obesity. In particular, a WHO Regional Office for Europe study [2] points out that in countries that have carried out surveys, the prevalence of overweight ranged between 32% and 79% in men, and between 28% and 78% in women. The highest prevalence of overweight was found in Albania
(in Tirana), Bosnia and Herzegovina and the United Kingdom (in Scotland). Turkmenistan and Uzbekistan had the lowest rates: the prevalence of obesity ranged from 5% to 23% among men and between 7% and 36% among women. For Italy, data retrieved by the Italian Institute of Statistics (ISTAT) in 2006 show that 35% of the population was overweight and 10,2% was obese [9]. It is worth to point out that obesity and overweight rates increase with the population age, and are particularly high in the population aged 55-74 years. Nevertheless, it is important to point out that there are major differences in the prevalence of obesity in different countries and between different socioeconomic groups within countries, and this highlights the importance of environmental and socio-cultural determinants of diet and physical activity.
If no action is taken and the prevalence of obesity continues to increase at the same rate as in the 1990s, an estimated 150 million adults and 15 million children and adolescents in these countries will be obese by 2010 [2]. In particular, the epidemic is progressing at alarming rates among children and adolescents: the annual rate of increase in the prevalence of childhood obesity has been growing steadily, and the current rate is ten times higher than it was in the 1970s. In Switzerland, for example, overweight among children increased from 4% in 1960 to 18% in 2003, and in the United Kingdom from 8% to 20% between 1974 and 2003. This trend reinforces the adult epidemic and creates a growing health challenge for the next generation.
applicable only to adults, are now being detected among children and with increasing frequency: examples include high blood pressure, early symptoms of hardening of the arteries, type 2 diabetes, non-alcoholic fatty liver disease, polycystic ovary disorder and difficulty in breathing during sleep.
Overweight also affects economic and social development through increasing health care costs and loss of productivity and income. In fact, obesity imposes an economic burden on society through increased medical costs to treat the diseases associated with it (direct), through lost productivity due to absenteeism and premature death (indirect), and through missed opportunities, psychological problems and poorer quality of life (intangible costs). Studies in the WHO European Region [5] indicate that, in general, the direct health care costs of obesity account for 2–4% of the national health expenditure, but larger estimates have been made, even up to 6%, as a study from Belgium [10] has reported. Calculations in the United States indicate that individuals with a BMI exceeding 30 kg/m2 had 36% higher annual health care costs than people with BMI 20.0–24.9 kg/ m2, and that individuals with a BMI between 25.0 and 29.9 kg/m2 had 10% higher annual health care costs than people with BMI 20.0–24.9 kg/ m2. Moreover, a study of direct cost studies worldwide reveals that health expenditure per inhabitant due to obesity ranges between US$ 13 (United Kingdom, 1998) and US$ 285 (United States, 1998) [2]. The indirect costs of obesity include obese people having a higher risk of being absent from work due to ill health or dying prematurely. However, the economic and welfare losses due to obesity depend on the labour market situation and the structure of the social security system. Recent estimates for Spain indicate that including the indirect costs due to the loss of productivity makes the total cost attributable to obesity an estimated € 2.5 billion per year. This figure corresponds to 7% of the total health budget. Including the cost of the social and psychological effects of being obese would further raise those figures. The total direct and indirect annual costs of obesity in 2002 in the 15 countries that were EU members before May 2004 were estimated to be € 32.8 billion per year [11]. Expressed as a proportion of GDP, the total cost of obesity (direct + indirect) has been estimated to be 0.2% in Germany, 0.6% in Switzerland, 1.2% in the United States and 2.1% in China, thus suggesting that the effect is more marked in developing economies [12].
Rationale for government intervention
The imbalance between energy intake and expenditure is the outcome of contemporary social trends. In fact, at least two thirds of the adults in the EU, as well as in the OECD countries, are insufficiently physically active for optimal health. Moreover, a large proportion of the population also consumes too many energy-dense and low nutrient foods and drinks and not enough fruit and vegetables. In fact, understanding why people might consume excess energy and why people might not expend enough energy to prevent weight gain, requires examining the determinants of health, and in particular factors which can influence the dietary intake and the physical activity behaviour of individuals.
Understanding interactions between individual health-related behaviours and the range of determinants that contribute to shaping such behaviours is a fundamental step in the design of effective interventions [13]. In particular, in a policy perspective, evidence of causality is required before interventions on specific determinants can be taken into consideration. Environmental factors such as food production technologies, restaurant density, the price of restaurant meals, and the density of urban developments have a causal influence on obesity [14-16].
If lifestyles are viewed as independent from other determinants, and purely the result of free choice, the case for collective intervention is weakened. This is consistent with an individualised approach for preventing disease, not dissimilar to the traditional (personal) health care approach. If, on the other hand, lifestyles are viewed as individual responses to environmental influences, the focus of policy will shift towards the environmental factors that determine individual behaviours.
A number of government policies may have unintended adverse consequences for the health of a population, possibly by providing incentives to individuals, or even forcing them, to make certain lifestyle choices. For instance, agricultural policies adopted in most developed countries, which are mostly based on taxes and subsidies, may raise the relative prices of healthy foods, such as fruits and vegetables, and may lower the relative price of unhealthy foods, such as fats and sugar. Town planning and traffic regulation may discourage active transport (such as walking and cycling) in favour of inactive (vehicular) transport.
health, partly through their effects on lifestyle choices. To the extent that these associations are causal, the question can be posed as to whether governments are fully taking such effects into account in the budgets they set for publicly-financed or publicly-provided education [13].
The determinants of chronic diseases are the result of market-based interactions or, in the case of government policies with unintended health consequences, they are the result of political processes pursuing legitimate public interests. Those interactions and policies are generally based on the expectation that welfare gains would be attained as a result.
Market and rationality failures may potentially affect the efficient working of the markets in which lifestyle choices are made and of those associated with other health determinants. Such failures may prevent markets from ensuring efficient and equitable outcomes, providing a justification for preventive interventions aimed at improving health, welfare and their distribution. The main potential sources of market failure include the following: spill-over effects on individuals other than those who make the lifestyle choices concerned; lack of information or communication of information; failures in the supply of lifestyle and other commodities. Failures of rationality, particularly those affecting consumers of lifestyle commodities, may add to the effects of classical market failures. The former include inconsistencies in time preferences, leading to poor self-control in health-related consumption, and limitations of rationality such as biased risk perception and common cognitive errors. Existing government policies may also produce unintended health consequences which prevent the maximisation of individual and social welfare, or an equitable distribution of health.
Market and rationality failures, as well as government policies with unintended health consequences, may be addressed directly with actions aimed at correcting failures, or indirectly with actions aimed at compensating their effects [13]. The latter may be an option when direct interventions are not possible or effective. The targeting of specific market failures in the design of prevention policies should be based on two main factors: whether these market failures have a sufficiently large impact to warrant government intervention; and whether the same market failures are liable to correction through appropriate, efficient and equitable policies. If individuals were able to make lifestyle choices, e.g. choose which foods to consume or what physical activities to undertake, through efficient
market transactions, they would likely maximise their own welfare by making tradeoffs among different forms of consumption which would be fairly priced on the basis of their production costs. In the absence of significant spill-over effects, societal welfare would also be maximised, at least as an aggregation of individual welfare.
Governments often intervene to correct market failures when these cause substantial damage to consumers and society and when interventions have the prospect of either increasing or improving the distribution of welfare.
Findings from previous international reviews of policies
Tackling unhealthy diets and sedentary lifestyles has become an increasingly important area of public health policy in recent years. Particularly as a result of an impressive growth of overweight and obesity rates, most countries in the OECD and EU areas have adopted policies and implemented interventions to improve diets and promote physical activity. Policy developments in these two domains have been reviewed in at least three international surveys undertaken since 2006.
Health, food and physical activity: Nordic Plan of Action on better health and quality of life through diet and physical activity [17]
stakeholders, local and state authorities, as well as action at the international level. The Nordic Council of Ministers defined a number of common short and long-term goals on diet, physical activity, and overweight to be met by the Nordic countries: a common policy agenda was established in order to reach those goals, although individual countries have adopted, and will continue to adopt, partly different sets of actions within the designated areas of common priority. In fact, variety is viewed as an asset as it allows for informative comparisons and exchange of knowledge. In their efforts to create a supportive environment for healthy individual lifestyle choices, the Nordic countries will pay particular attention to certain population groups, particularly children, socially vulnerable individuals and ethnic minorities, who have the most difficulties in making healthy choices. Finally, a general policy aim in the Nordic countries is to develop and strengthen public/ private partnerships, as an important element in the effort to promote a healthy diet and physical activity, and to prevent overweight and obesity.
Nutrition, physical activity and prevention of obesity: recent policy developments in the WHO European Region [18]
This report was prepared for the WHO European Ministerial Conference on Counteracting Obesity, held in Istanbul, Turkey on 15–17 November 2006. Its aims was to highlight recent policy developments in the area of nutrition, physical activity and prevention of obesity in the Member States of the WHO European Region. Most countries have developed policy documents dealing with obesity risk factors and in particular with food and nutrition, with only a few relating to physical activity. Besides making a statement of general objectives, many countries set specific dietary goals, although few countries have defined quantifiable goals for overweight and obesity and physical activity. Country policies recognize the need to act at the national, regional, community and individual levels, and the need to involve stakeholders in implementing policy. In particular, most strategies identify stakeholders, and measures to involve them include creating partnerships or platforms or achieving commitment through signed agreements. All policy strategies identify target groups relating to the life-course approach. In a very few cases, particular groups are targeted including individuals with low socioeconomic status, distressed people, the chronically ill and disabled, ethnic minorities, immigrants and those with limited education. Specific policy actions have been implemented in multiple settings,
and in particular in schools, workplaces, and health care services. Schools are the settings where most interventions take place, with the common goal of changing the school environment by providing a good framework for physical activity and strengthened health education. Actions undertaken to promote healthy food are mainly aimed at revising food product design and changing food labeling in order to promote better information to consumers. Marketing of food and beverages to children is a major issue in Europe and actions carried out by European countries vary from statutory regulations that ban this form of advertising to non-statutory guidelines that impose some limitations. Other countries simply rely on self regulation by the advertising and media industries. In order to promote physical activity, most countries focus on active transport, such as constructing safe walking and cycling paths.
Dossier: Prevention for Health: Nutrition and Physical Activity – a Key to Healthy Living [19]
a decisive target group, and health promotion in schools is one of the most prominent approaches for interventions in all member countries.
Methods
This research is part of the OECD project on “Economics of Prevention” which is being managed by the Health Division in the Directorate for Employment, Labour and Social Affairs. It also entails collaboration with other OECD Directorates, notably the Trade and Agriculture and the Education Directorates, and with other international organizations working on similar issues, in particular the European Commission and the World Health Organization.
The research considered policy documents related to the promotion of healthy diets and of physical activity adopted until 2008 by 34 OECD and other EU countries (namely: Australia, Austria, Belgium, Canada, Cyprus, Denmark, Estonia, Finland, France, Germany, Hungary, Italy, Ireland, Iceland, Japan, Korea, Latvia, Lithuania, Luxembourg, Malta, Mexico, Netherlands, New Zealand, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and United Kingdom). Information about policies and interventions was mainly retrieved from official sources such as the WHO Regional Office for Europe nutrition policy database [22], and websites of Health Ministries and national public health institutions. It should be noted that only policy documents in English, French, Italian, Spanish and Portuguese languages, available in electronic format through the Internet, were considered in the analysis. For these reasons, it is possible that a small number of policy statements on diet and physical activity (in particular those coming from: Cyprus, Germany, Latvia, Lithuania, Malta, Poland, Romania, Slovakia and Turkey) may not have been taken into account, mainly due to language barriers.
For each country, documents retrieved were divided into qualitative and quantitative ones.
The first group is made of policy statements and/or white papers. However, the scope of such documents may vary substantially; therefore, a distinction was made between documents containing an identification of the problem or a conceptual framework, and those spelling out agendas for action. These were analysed along five key issues which were chosen in order to reflect as much as possible the main content and purpose of the documents: i) In what terms is the obesity problem identified? ii) Are the determinants of the obesity problem identified? iii) What objectives have been set to address the
obesity problem? iv) Who are the main actors involved in addressing the obesity problem? v) Is there a rationale for government intervention?
The second group, quantitative documents, mostly includes analyses of policy issues associated with nutrition, physical activity and obesity based on national data from routine surveys or ad hoc investigations. In a few of the latter documents, projections of future trends in obesity or costs related to non communicable diseases were also considered as a means of determining the magnitude of the issues policy makers are faced with.
Results
Most OECD and EU countries, in the last ten years, have produced a large amount of qualitative and quantitative documents dealing with problems of unhealthy diets and sedentary lifestyles, particularly in relation to the emerging obesity epidemic.
Analysis of qualitative documents
Most countries use data and trends on overweight and obesity as a background to justify actions and policies proposed to counteract the problem. Some countries (Australia, Denmark, Estonia, Finland, Iceland, Norway, Slovenia, and Switzerland, for example) also provide a deep analysis of eating and physical activity habits of their population, and in some cases present a comparison with the standards fixed by international recommendations (Denmark, Netherlands, Norway and Switzerland for example).
Although all OECD and EU member countries are concerned by the levels of obesity and by the growth of the problem over time, only a few make comparisons with data of other countries or with EU levels of obesity. The problem of obesity is considered in relative terms only by few countries: Canada makes comparisons of obesity rates with the United States, and of the directs costs of obesity with New Zealand, Australia, France, Netherlands and United States. The United Kingdom compares its rates of obesity with the ones found in the United States, in Australia and in Europe (to be more precise: in Finland, in Norway and in Sweden). Others countries such as Norway, Portugal, Slovenia, Spain and Switzerland use the European levels of obesity as a means of comparison.
All OECD and EU member countries are concerned about the distribution of obesity across population groups, with a particular emphasis on children, which represent the most targeted group. Moreover there is a general agreement between countries that obesity rates are unfairly distributed between population with different socio-economic status (SES): people with a lower SES are often the ones with highest obesity rates. Some countries also point out the problem (and therefore have targeted interventions in their policy statements) in specific population groups: Australia analyses data concerning obesity for its indigenous populations, Canada for its aboriginal population and New Zealand for its Maori and Pacific people. Other countries make distinctions between obesity rates among men and women (Estonia, Netherlands, Iceland for children, Ireland, Spain and Sweden). Only Spain and Italy take into account the problem of obesity in terms of geographic distribution of the population.
All OECD and EU member countries are concerned about the burden associated with obesity, although most of these rely on the WHO data and “call for action”. Australia and Estonia have implemented a specific strategy for prevention of chronic and cardiovascular diseases, respectively. The Australian National
Chronic Disease Strategy [24] provides an overarching framework of national direction for improving chronic disease prevention and care across Australia. It is a nationally agreed agenda to encourage coordinated action in response to the growing impact of chronic disease on the health of Australians and the health care system. The Estonian National Strategy for Prevention of Cardiovascular Diseases 2005-2020 [25] is particularly focused on five strategic areas (physical activity; nutrition; smoking; health care; dissemination of information and securing local capacity) pertaining to the main cardiovascular diseases (CVD) factors and, within these, it plans out activities which are evidence-based and likely to bring about changes in attitudes, health behaviour, and in the environment, and thus, in the long run, in morbidity and mortality.
Many OECD and EU countries are also concerned about the health expenditure associated with obesity. Nevertheless, some countries, such as Australia, France, Netherlands, New Zealand, Sweden and Switzerland (for example), refer to “the costs attributable to obesity” without specifying what these include. Australia calculates direct health-care costs attributable to diet, while Ireland considers the costs associated to deaths caused by chronic diseases. Only Canada and the United Kingdom have calculated both direct and indirect costs of weight-related chronic diseases, and costs for the health care system which are related to physical inactivity. In the United Kingdom, for example, direct costs are estimated to be £ 4.2 billion and Foresight [8] forecasts these will more than double by 2050. Foresight [8] also estimates that weight problems already cost the wider economy in the region of £ 16 billion, and that this will rise to £ 50 billion per year by 2050, if left unchecked. As the indirect costs, such as the loss of productivity, produced by obesity and overweight are more difficult to estimate, there is no reference of these in most of policy documents analysed.
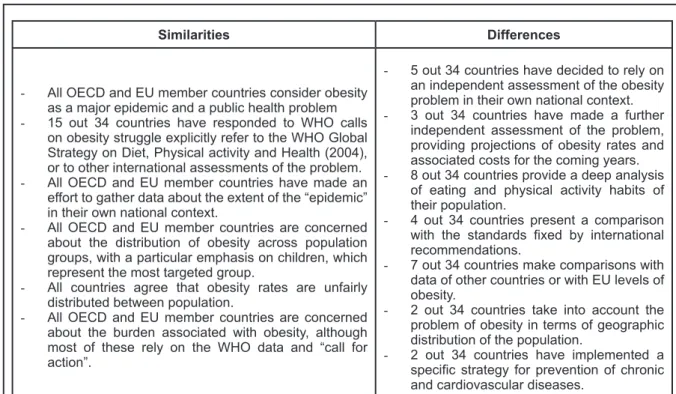
Table 1 summarizes similarities and differences between countries with respect to the key issue “In what terms is the obesity problem identified?”.
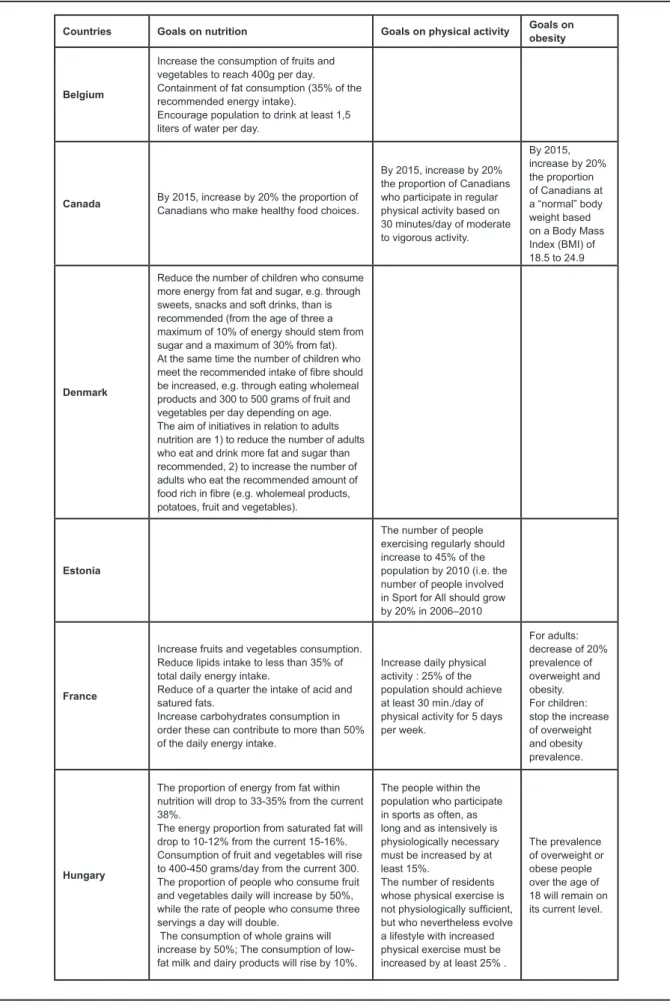
and quantifiable objectives have been set in policies related to healthy nutrition and physical activity promotion. Many OECD and EU member countries have mainly set goals for nutrition. Nutrition-related goals refer mainly to total or specific fat intake. Only in a few cases (for example, Belgium, Denmark, Iceland, Norway, Sweden and the United Kingdom) is there a reference to the most appropriate intake of carbohydrate, sugar, salt, dietary fibre and fruit and vegetables. In these cases, the benchmark is defined by the WHO recommendations. Some countries (Canada, Estonia, France, Hungary, Iceland, Ireland, Korea, Netherlands, Slovenia, Sweden, Switzerland, and United Kingdom) have also set specific goals for obesity or physical activity. In these cases, the objective is to increase the number of adults engaging in at least 30 minutes (or 60 minutes for children) of physical activity per day. Nevertheless, in none of the policy documents analysed are measurable and quantifiable objectives supported by specific related interventions: the measures proposed in the field of nutrition and physical activity are strictly linked to the targets which in some cases even refer to the intake of fruits and vegetables per day. Finally, the time perspective to reach objectives vary from a minimum of 4 years (Estonia, Netherlands, Switzerland) to a maximum of up to 10 years (Canada, Finland, United Kingdom), although the most common time perspective
chosen is ten years (Hungary, Iceland, Austria, Australia, Portugal). Some countries (Italy, Japan, Spain, Sweden) do not specify in their policy documents the lapse of time required to reach the fixed targets. The time perspective of the goals is irrespective of their nature (unspecific vs measurable) and of their area (nutrition vs physical activity vs obesity rates).
As mentioned previously, obesity is now seen as a major public health problem in all OECD and EU member countries. Probably this is why many of the policy documents concerning obesity have been produced by the Ministry of Health. Only in some cases (for example, Australia, Canada, Denmark, Ireland and Norway) documents which provide a background for the final policy statement have been prepared by a national coordination institute. The role of this body is to advise the government on developing, implementing, monitoring and evaluating nutrition policies, guidelines and action plans. On the contrary, policy documents which propose a very specific strategy – for example concerning only physical activity or only eating habits – have been prepared by the Ministries of Education or Culture (Estonia and Finland) and by the Ministry of Agriculture, Forestry and Fisheries (Japan) respectively.
Although there still isn’t a common point of view on who is responsible for the health of individuals and for their choices on lifestyles, all
Similarities Differences
- All OECD and EU member countries consider obesity
as a major epidemic and a public health problem
- 15 out 34 countries have responded to WHO calls on obesity struggle explicitly refer to the WHO Global Strategy on Diet, Physical activity and Health (2004), or to other international assessments of the problem.
- All OECD and EU member countries have made an
effort to gather data about the extent of the “epidemic” in their own national context.
- All OECD and EU member countries are concerned
about the distribution of obesity across population groups, with a particular emphasis on children, which represent the most targeted group.
- All countries agree that obesity rates are unfairly distributed between population.
- All OECD and EU member countries are concerned
about the burden associated with obesity, although most of these rely on the WHO data and “call for action”.
- 5 out 34 countries have decided to rely on
an independent assessment of the obesity problem in their own national context.
- 3 out 34 countries have made a further independent assessment of the problem, providing projections of obesity rates and associated costs for the coming years.
- 8 out 34 countries provide a deep analysis
of eating and physical activity habits of their population.
- 4 out 34 countries present a comparison
with the standards fixed by international
recommendations.
- 7 out 34 countries make comparisons with
data of other countries or with EU levels of obesity.
- 2 out 34 countries take into account the problem of obesity in terms of geographic distribution of the population.
- 2 out 34 countries have implemented a
specific strategy for prevention of chronic
and cardiovascular diseases.
Countries Goals on nutrition Goals on physical activity Goals on obesity
Belgium
Increase the consumption of fruits and vegetables to reach 400g per day. Containment of fat consumption (35% of the recommended energy intake).
Encourage population to drink at least 1,5 liters of water per day.
Canada By 2015, increase by 20% the proportion of Canadians who make healthy food choices.
By 2015, increase by 20% the proportion of Canadians who participate in regular physical activity based on 30 minutes/day of moderate to vigorous activity.
By 2015, increase by 20% the proportion of Canadians at a “normal” body weight based on a Body Mass Index (BMI) of 18.5 to 24.9
Denmark
Reduce the number of children who consume more energy from fat and sugar, e.g. through sweets, snacks and soft drinks, than is recommended (from the age of three a maximum of 10% of energy should stem from sugar and a maximum of 30% from fat). At the same time the number of children who meet the recommended intake of fibre should be increased, e.g. through eating wholemeal products and 300 to 500 grams of fruit and vegetables per day depending on age. The aim of initiatives in relation to adults nutrition are 1) to reduce the number of adults who eat and drink more fat and sugar than recommended, 2) to increase the number of adults who eat the recommended amount of food rich in fibre (e.g. wholemeal products, potatoes, fruit and vegetables).
Estonia
The number of people exercising regularly should increase to 45% of the population by 2010 (i.e. the number of people involved in Sport for All should grow by 20% in 2006–2010
France
Increase fruits and vegetables consumption. Reduce lipids intake to less than 35% of total daily energy intake.
Reduce of a quarter the intake of acid and satured fats.
Increase carbohydrates consumption in order these can contribute to more than 50% of the daily energy intake.
Increase daily physical activity : 25% of the population should achieve at least 30 min./day of physical activity for 5 days per week.
For adults: decrease of 20% prevalence of overweight and obesity. For children: stop the increase of overweight and obesity prevalence.
Hungary
The proportion of energy from fat within nutrition will drop to 33-35% from the current 38%.
The energy proportion from saturated fat will drop to 10-12% from the current 15-16%. Consumption of fruit and vegetables will rise to 400-450 grams/day from the current 300. The proportion of people who consume fruit and vegetables daily will increase by 50%, while the rate of people who consume three servings a day will double.
The consumption of whole grains will increase by 50%; The consumption of low-fat milk and dairy products will rise by 10%.
The people within the population who participate in sports as often, as long and as intensively is physiologically necessary must be increased by at least 15%. The number of residents whose physical exercise is not physiologically sufficient, but who nevertheless evolve a lifestyle with increased physical exercise must be increased by at least 25% .
The prevalence of overweight or obese people over the age of 18 will remain on its current level.
countries agree that different stakeholders should share this responsibility. In fact, communities can and should influence individual choices by providing information, dispensing knowledge and shaping attitudes.
In this sense, all documents pointed out that the causes underlying obesity are so complex that the health care sector alone cannot solve the problem of obesity and achieve the goals set to address it. Coordination and collaboration is required across different sectors; involving various stakeholders at
some point and taking an intersectoral approach at the national, local and community levels are necessary. In fact, most policy documents identify a wide range of stakeholders. First, most countries mention various government institutions and ministries as stakeholders, with a leading role for the Health Ministry. Other common ministries involved are Ministry of Sport, Ministry of Education, Ministry of Communication, Ministry of Agriculture, Ministry of Transportation and Ministry of Social Affairs.
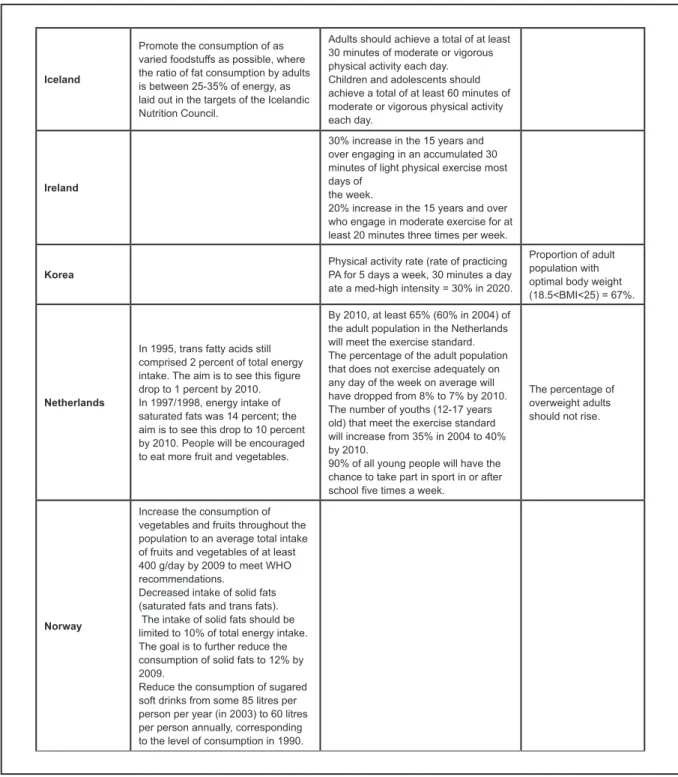
Iceland
Promote the consumption of as varied foodstuffs as possible, where the ratio of fat consumption by adults is between 25-35% of energy, as laid out in the targets of the Icelandic Nutrition Council.
Adults should achieve a total of at least 30 minutes of moderate or vigorous physical activity each day. Children and adolescents should achieve a total of at least 60 minutes of moderate or vigorous physical activity each day.
Ireland
30% increase in the 15 years and over engaging in an accumulated 30 minutes of light physical exercise most days of
the week. 20% increase in the 15 years and over who engage in moderate exercise for at least 20 minutes three times per week.
Korea Physical activity rate (rate of practicing PA for 5 days a week, 30 minutes a day ate a med-high intensity = 30% in 2020.
Proportion of adult population with optimal body weight (18.5<BMI<25) = 67%.
Netherlands
In 1995, trans fatty acids still comprised 2 percent of total energy intake. The aim is to see this figure drop to 1 percent by 2010. In 1997/1998, energy intake of saturated fats was 14 percent; the aim is to see this drop to 10 percent by 2010. People will be encouraged to eat more fruit and vegetables.
By 2010, at least 65% (60% in 2004) of the adult population in the Netherlands will meet the exercise standard. The percentage of the adult population that does not exercise adequately on any day of the week on average will have dropped from 8% to 7% by 2010. The number of youths (12-17 years old) that meet the exercise standard will increase from 35% in 2004 to 40% by 2010.
90% of all young people will have the chance to take part in sport in or after school five times a week.
The percentage of overweight adults should not rise.
Norway
Increase the consumption of vegetables and fruits throughout the population to an average total intake of fruits and vegetables of at least 400 g/day by 2009 to meet WHO recommendations.
Decreased intake of solid fats (saturated fats and trans fats). The intake of solid fats should be limited to 10% of total energy intake. The goal is to further reduce the consumption of solid fats to 12% by 2009.
Reduce the consumption of sugared soft drinks from some 85 litres per person per year (in 2003) to 60 litres per person annually, corresponding to the level of consumption in 1990.
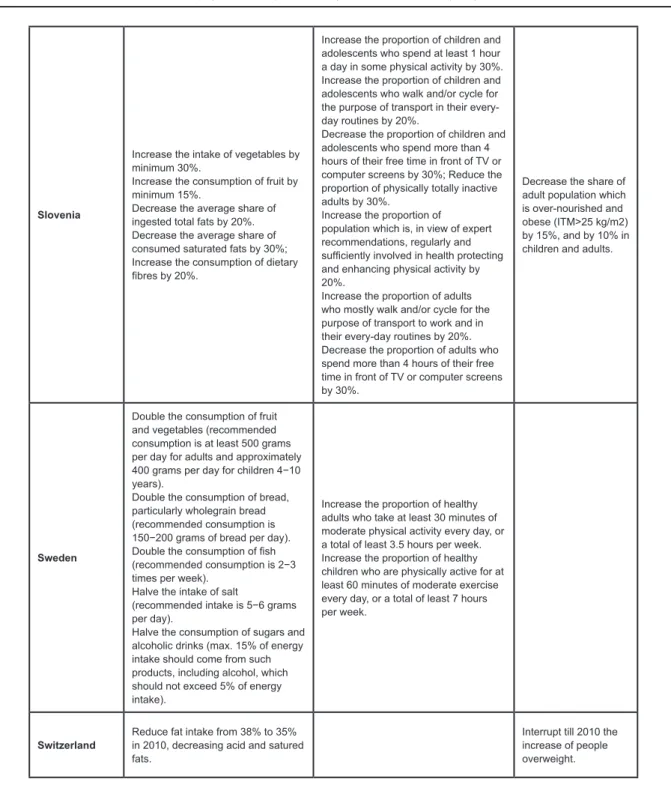
Involvement and mobilization of private industry in national nutrition policy has been an issue of debate and was stressed by the World Health Organization as a promising approach for public health; the effective intersectoral action is an overall objective for policies related to obesity. All policy statements stress the importance of the private sector, with the food industry identified as the main partner in all countries. Table 3 gives an example of the stakeholders from the private sector mentioned in some policy documents
for nutrition and physical activity. Furthermore, the pharmaceutical industry, the catering sector, distribution companies, restaurant chains, the leisure industry, transport, town planning and the mass media are identified as potential partners. In addition, all documents consider non-profit-making organizations as stakeholders, including consumer associations, employees’ unions, and patients’ and health professionals’ organizations.
In this light, most OECD and EU countries have identified different settings in which actions
Slovenia
Increase the intake of vegetables by minimum 30%.
Increase the consumption of fruit by minimum 15%.
Decrease the average share of ingested total fats by 20%. Decrease the average share of consumed saturated fats by 30%; Increase the consumption of dietary fibres by 20%.
Increase the proportion of children and adolescents who spend at least 1 hour a day in some physical activity by 30%. Increase the proportion of children and adolescents who walk and/or cycle for the purpose of transport in their every-day routines by 20%.
Decrease the proportion of children and adolescents who spend more than 4 hours of their free time in front of TV or computer screens by 30%; Reduce the proportion of physically totally inactive adults by 30%.
Increase the proportion of population which is, in view of expert recommendations, regularly and sufficiently involved in health protecting and enhancing physical activity by 20%.
Increase the proportion of adults who mostly walk and/or cycle for the purpose of transport to work and in their every-day routines by 20%. Decrease the proportion of adults who spend more than 4 hours of their free time in front of TV or computer screens by 30%.
Decrease the share of adult population which is over-nourished and obese (ITM>25 kg/m2) by 15%, and by 10% in children and adults.
Sweden
Double the consumption of fruit and vegetables (recommended consumption is at least 500 grams per day for adults and approximately 400 grams per day for children 4−10 years).
Double the consumption of bread, particularly wholegrain bread (recommended consumption is 150−200 grams of bread per day). Double the consumption of fish (recommended consumption is 2−3 times per week).
Halve the intake of salt
(recommended intake is 5−6 grams per day).
Halve the consumption of sugars and alcoholic drinks (max. 15% of energy intake should come from such products, including alcohol, which should not exceed 5% of energy intake).
Increase the proportion of healthy adults who take at least 30 minutes of moderate physical activity every day, or a total of least 3.5 hours per week. Increase the proportion of healthy children who are physically active for at least 60 minutes of moderate exercise every day, or a total of least 7 hours per week.
Switzerland Reduce fat intake from 38% to 35% in 2010, decreasing acid and satured fats.
Interrupt till 2010 the increase of people overweight.
to counteract obesity should take place. The most common settings identified are community and physical environment, workplaces, schools, home and family environment. Starting from this point, each actor entitled to address the obesity problem is called to contribute through its own activities and role in society to achieving the government targets on overweight. Most of the plans analyzed, however, do not elaborate on the specific role and strategies that will be used to mobilize the stakeholders; very little information
seems to be available on how different actors contributed to the development of the plan. It seems that stakeholder mobilization is largely restricted to the implementation phase and the lack of documentation of the planning phase support the hypothesis that in most cases a top-down approach is used. Some examples on how collaboration with the private sector can take place are given by Denmark (flexible partnerships), Netherlands (self-regulation model) and Sweden, France, and the United Kingdom
UK
Increase average consumption of a variety of fruit and vegetables to at least 5 portions per day (currently 2.8 portions per day).
increase the average intake of dietary fibre to 18 grams per day (currently 13.8 grams per day); reduce average intake of salt to 6 grams per day (currently 9.5 grams per day).
reduce average intake of saturated fat to 11% of food energy (currently at 13.3%).
maintain the current trends in reducing average intake of total fat to 35% of food energy (currently at 35.3%).
Reduce the average intake of added sugar to 11% of food energy (currently 12.7%).
Increase levels of participation in physical activity and sport of 70% of individuals undertaking 30 minutes of physical activity five days a week by 2020. Increase the number of people >16 years old who participate in active sports, at least 12 times a year by 3%, and increasing the number who engage in at least 30 minutes of moderate-intensity-level sport, at least three times a week by 3%. The percentage of school children in England who spend a minimum of two hours each week on high-quality Physical Education and school sport within and beyond the curriculum increases from 25% in 2002 to 75% by 2006 and 85% by 2008 in England, and to at least 75% in each school sport partnership by 2008.
Halt the year-on-year increase in obesity among children under 11 by 2010. By 2020 reduction of the proportion of overweight and obese children to 2000 levels.
Table 2. Quantifiable goals on nutrition, physical activity and obesity reported in different policy documents.
Denmark Finland Sweden France NetherlandsThe KingdomUnited
Food industry √ √ √ √ √ √
Retailers √ √ √ √
Catering
companies √ √ √ √ √ √
Sport goods
manufacturers √ √ √
Advertising and recreation
businesses √ √ √
Insurance and
banking groups √ √
Pharmaceutical
companies √ √
Media √ √ √
(dialogue with the food industry). The Danish plan proposes flexible partnerships to implement the program and lists for each objective how the different stakeholders can contribute. The Dutch plan promotes a self-regulation mechanism and encourages the entire commercial sector to participate in the activities; the food industry is particularly stimulated to lower the fat content and improve the fatty acid composition of their products. In these cases, the government would only intervene with appropriate measures when self-regulation fails. One of the central aims of the Swedish plan is to promote dialogue with the food industry. In this context, the French plan incorporates specific activities to inform the food industry on how their commercial message ought to comply with national guidelines, whereas in the UK, specific structures have been put in place to ensure the dialogue with the food industry.
Last but not least, the documental analysis points out that many OECD and EU countries (14 out 34) clearly consider the government intervention as a duty in a policy aimed at counteracting obesity. In fact, although each country has its own reasons for justifying government intervention in this area, there are at least three main points which are common to all countries.
First, obesity is considered as a major problem of public health, with both a social and an economic incidence for the society. In fact, obesity is associated with premature death, excessive morbidity and serious psychosocial problems. The damage it causes to the welfare of citizens is extremely serious, and the downstream health care costs of doing nothing to reduce illness and premature death due to poor nutrition, physical inactivity and obesity, are unsupportable. The government is therefore responsible for creating societal conditions which ensure good health, on equal terms, for the entire population. Only the government has the tools to set a good framework for the health of individuals, families and communities and for their efforts to improve health. In particular, government can influence the preconditions for the populations’ health through the various sectors of administration. The key decisions in terms of health promotion relate to matters such as changes in the living environment, management of welfare services, targeting of taxation, improvements in education and training, job creation, ensuring product quality, social security and equality. The public sector carries this out through legislation, planning and other means and through the numerous social and health services offered by the welfare state.
Second, the government has a leading role in
ensuring that information on health and illness is disseminated, by monitoring the health of the population, by contributing to the development of new methods and by formulating collective targets and strategies for efforts to promote health and prevent disease. In fact, as there are a large amount of conflicting advice and information given to the public about food and nutrition, the government has to provide authoritative references to citizens.
Finally, the ageing population and cultural and ethnic diversification pose challenges for health policy. In fact, all population groups must be given the chance to promote their health and contribute to the workings of society. Exclusion for reasons of age or cultural differences must be avoided, not least because it has obvious effects on health. In particular, as obesity is also linked to socio-economic conditions, without a government intervention there is a clear risk of greater social and regional marginalization. In fact, before health policy can succeed, any further discrepancies between socioeconomic groups and people in different regions must be prevented towards the weakest groups in society, who need professional assistance and financial support.
As a preliminary conclusion it can be said that, on paper, countries tend to comply with overarching principles formulated by experts. For instance, all policy documents analysed point out that both a comprehensive portfolio of measures and a coordinated approach across different areas of policy activity, are needed.
Analysis of quantitative documents
the WHO. Most general health surveys target the adult population, generally starting from age 15 or 16. Infants and children are often the target of specific surveys.
In some cases, countries rely on multi-national surveys, either organised by consortia of countries, or by international organisations such as the WHO or agencies of the European Commission. These surveys tend to have smaller sample sizes for individual countries, but have the advantage of being undertaken using standard methods and data collection instruments, which make it easier to conduct comparative assessments of trends across countries. Examples of such analysis include the Finbalt Health Monitor and the Health Behaviour in School-aged Children (HBSC) surveys.
A very limited number of OECD and EU countries have also produced analyses aimed at forecasting trends in obesity and related expected costs for society and the health care system.
The Australian Burden of Disease and Injury report [27] measures mortality, disability, impairment, illness and injury arising from 176 diseases, injuries and risk factors using a common metric, the disability-adjusted life year or DALY, and methods developed by the Global Burden of Disease Study. The report provides detailed estimates of the burden of mortality and disability for each disease and injury category by sex and age. It also assesses the burden attributable to each of 14 major risk factors, and inequalities in the disease burden associated with socioeconomic disadvantage. Starting from this document, a study was undertaken drawing together epidemiological data from the Burden of Disease report, risk factor and demographic trends, and health care cost data, to model projected changes in disease prevalence and health expenditure to 2033.
The Turkish National Burden of Disease and Cost-Effectiveness Study [28] presents data on the burden of diseases and deaths by cause, age and gender, attributable to physical inactivity and insufficient fruit and vegetables-consumption.
The United Kingdom adopted a different approach. The Forecasting obesity to 2010 report [29] contains projections of obesity rates in England to 2010, based on the assumption that current trends in obesity prevalence will continue unchanged. The document is based on the results of the Health Survey for England 2003 (HSE 2003). It looks at the estimated number and proportion of adults and children who may be obese in 2010 within different socio-demographic groups.
The United Kingdom has also produced a report
[30] which considers how society might deliver a sustainable response to obesity in the UK over the next 40 years. One objective of the project was to analyse how future levels of obesity might change and to identify the most effective future responses. Looking to the future, the Foresight experts estimated that, based on current trends, levels of obesity and overweight will rise to 60 per cent in men, 50 per cent in women, and 25 per cent in children by 2050, with a further 35 per cent of adults and nearly 40 per cent of children overweight. Starting from these projections, the report presents key messages and implications for the UK. These are based on an extensive analysis of a wide range of evidence, including several commissioned evidence reviews, a systems analysis of the primary determinants of obesity, scenarios of possible futures and a quantitative model of future trends in obesity and associated diseases. Foresight commissioned a model which utilises the dataset of the Health Survey for England from 1994 to 2004 and employs extrapolation and micro simulation techniques to predict the distribution of people across various BMI categories, to 2050. The report also models current and future costs of obesity and obesity-related diseases to the health system.
Conclusions
Although almost all Member States in the European Region have government-approved policies on nutrition and food safety, the burden of disease associated with poor nutrition continues to grow both in countries of the OECD area and of the European Region, particularly as a result of the obesity epidemic.
The failure of Member States to achieve nutrition and food safety goals is due to a lack of resources, expertise, political commitment or intersectoral coordination. In addition, such plans rarely tackle the complex set of factors that affect diet, food safety and lifestyle patterns in modern society or those which are encountered at a regional level as a result of globalization and trade liberalization. Food distribution and catering in many industrialized countries is carried out by a few businessmen, who influence product supply, safety and price. The media, advertising and retail sectors, and the food industry have an influence on dietary choices, sometimes in the opposite direction from that which public health specialists recommend [42]. Urban design, too, often discourages safe, active transport, while the increasing use of television and computers encourages sedentary leisure activities, thus adding a physical inactivity component to the health challenges.
In order to reverse the obesity trend down to decent levels and to reach the lower socio-economic groups, concerted, multisectorial, long-term actions are needed in combination with a much larger political determination.
Nevertheless, a preliminary analysis of specific interventions and activities set up to improve diets and physical activity in the population, over the course of recent years, shows that that a large majority of the initiatives are aimed at improving diets, rather than physical activity, in particular through the development, diffusion and promotion of nutrition guidelines. Although these kind of actions are certainly very useful and informative, concretely they will hardly help to reduce the prevalence of overweight and obesity among population. Moreover, despite the large
number of interventions carried out by countries, only the minority are nationwide. In fact there are a lot of small and local initiatives that have been developed, but these are not coordinated at the national level.
Evidence from independent surveys across Sweden indicates that childhood obesity trends may be levelling off and possibly reversing in girls [43]. Dietary surveys and total food consumption statistics also indicate some positive changes in food habits during the same time period, which could contribute to the observed obesity trends. In particular, the consumption of soft drinks and sweets has decreased while the intake of fruit and vegetables has increased. The reasons for the observed changes in overweight and food habits are largely unknown. However, since 2003/2004 there has been an enormous media attention to overweight, healthy food habits and physical activity which have resulted in a common awareness of the problem. Local activities have started in child health care, in pre-schools, schools, and sport clubs. Sweden has a long tradition of public health activities, official nutrition recommendations and food based dietary guidelines, free child health care, free school meals and school nurses located in every school. This structure may have probably formed a solid ground for these more recent activities. However, Sweden is one of the few European countries that does not have a national action plan for healthy dietary habits and physical activity. Furthermore, no national campaigns have been launched. The positive signs are probably a result of the many regional and local actions that have taken place in many sectors and levels in the society, rather than one specific measure or national political commitment.
Acknowledgments
The author worked on the survey discussed in this paper while based in the OECD Health Division as an intern in 2007-08. The views expressed in this paper do not necessarily reflect those of the OECD, nor those of its Member countries.
References
1) Caballero B. The global epidemic of obesity: an overview. Epidemiologic Reviews 2007;29(1):1-5.
2) World Health Organization Regional Office for Europe. The challenge of obesity in the WHO European Region and the strategies for response. World Health Organization, 2006. 3) World Health Organization. Global Database on Body Mass Index. Available from: http://www.who.int/bmi/index.jsp
[Accessed October 20, 2008].
4) International Obesity Task Force Organization database. Available from: http://www.iotf.org/database/index.asp [Accessed October 20, 2008].
5) World Health Organization. Obesity: Preventing and managing the global epidemic. World Health Organization Technical Report Series, 2000:894.
people: a crisis in public health. Obesity Reviews 2004;5(1):4-104. 7) Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. Br Med J 2000;320:1240-3. 8) UK Government Office for Science. Tackling Obesities: Future Choices – Qualitative Modelling of Policy options. Foresight Programme, 2007.
9) ISTAT. La vita quotidiana nel 2006 – Indagine multiscopo annuale sulle famiglie “Aspetti della vita quotidiana” [Daily life in 2006 – Annual survey on families “Aspects of daily life”]. Informazioni 2007;12.
10) Institut Belge de l’Economie de la Santé. Evaluation du coût de l’obésité en Belgique [Estimation of cost of obesity in Belgium]. Institut Belge de la Santé 2000; Briefing 29. 11) Fry J, Finley W. The prevalence and costs of obesity in the EU. Proc Nutr Soc 2005;64(3):359-62.
12) Oxford Health Alliance working group. Economic consequences of chronic diseases and the economic rationale for public and private intervention. London: Oxford Health Alliance, 2005.
13) Sassi F, Hurst J. The prevention of lifestyle-related chronic diseases: an economic framework. OECD Health Working Papers 2008;32.
14) Cutler D, Glaeser E, Shapiro J. Why Have Americans Become More Obese?. J Econ Perspect 2003;17(3):93-118. 15) Plantinga AJ, Bernell S. The Association Between Urban Sprawl and Obesity: is it a Two-Way Street?. J Reg Sci 2007;47(5):857-79.
16) Rashad I. Structural Estimation of Caloric Intake, Exercise, Smoking, and Obesity. Quart Rev Econ Finance 2006;46(2):268-83.
17) The Nordic Council of Ministers for Fisheries and Aquaculture, Agriculture, Food and Forestry (MR-FJLS) and the Nordic Council of Ministers for Health and Social Affairs (MR-S). Health, food and physical activity: Nordic Plan of Action on better health and quality of life through diet and physical activity. Copenhagen: Nordic Council of Ministers, 2006. 18) World Health Organization Regional Office for Europe. Nutrition, physical activity and prevention of obesity: recent policy developments in the WHO European Region. World Health Organization, 2006.
19) German Presidency of the EU. Prevention for Health: Nutrition and Physical Activity – a Key to Healthy Living. Dossier prepared for a Conference organized by the German Presidency of the EU. Badenweiler (D), 2007;25-7.
20) Commission of the European Communities. Green paper "Promoting healthy diets and physical activity: a european dimension for the prevention of overweight, obesity and chronic diseases". European Commission, 2005.
21) European Commission, DG SANCO. White paper on a strategy for Europe on nutrition, overweight and obesity related health issues. European Commission, 2007.
22) World Health Organization Regional Office for Europe. Nutrition policy database. Available from: http://data.euro. who.int/nutrition [Accessed October 20, 2008].
23) World Health Organization. Global strategy on Diet, Physical Activity and Health. World Health Organization 2004. 24) National Health Priority Action Council. National Chronic Disease Strategy. Canberra: Australian Government Department of Health and Ageing, 2006
25) Ministry of Social Affairs. Estonian National Strategy for
Prevention of Cardiovascular Diseases 2005–2020. Tallinn: Ministry of Social Affairs, 2005.
26) Lachat C, Van Camp J, De Henauw S, Matthys C, Larondelle Y, Remaut-De Winter AM, and Kolsteren P. A concise overview of national nutritional action plans in the European Union Member States. Publ Health Nutr 2005;8:266-74.
27) Begg S, Vos T, Barker B, Stevenson C, Stanley L, Lopez AD, 2007. The burden of disease and injury in Australia 2003. Canberra: Australian Institute of Health and Welfare, 2007. 28) Turkish Ministry of Health, RSHC, The School of Public Health. Ankara: National Burden of Disease and Cost-Effectiveness Study, 2003.
29) Zaninotto P, Wardle H, Stamatakis E. Forecasting Obesity to 2010. Report prepared for UK Department of Health, 2006. 30) UK Government Office for Science. Foresight Tackling Obesities: Future Choices. Project report, 2007.
31) World Health Organization, Regional Office for Europe. The First Action Plan for Food and Nutrition Policy, WHO European Region, 2000–2005. World Health Organization, 2000 32) United Nations Economic Commission for Europe. Protocol on Water and Health to the 1992 Convention on the Protection and Use of Transboundary Watercourses and International Lakes. London, 17 June 1999
33) United Nations. Millennium Development Goals, 2000a. Available from: http://www.un.org/millenniumgoals/ [Accessed October 20, 2008].
34) World Health Organization. WHO Global Strategy for Food Safety: safer food for better health. Food Safety Programme 2002. World Health Organization, 2002a.
35) World Health Organization. Global Strategy for Infant and Young Child Feeding. World Health Organization, 2003. 36) World Health Organization Regional Office for Europe. European Strategy for Child and Adolescent Health and Development. World Health Organization, 2005.
37) Food and Agriculture Organization of the United Nations (FAO). Voluntary guidelines to support the progressive realization of the right to adequate food in the context of national food security. Food and Agriculture Organization of the United Nations (FAO), 2005.
38) World Health Organization, Regional Office for Europe. The European Strategy for the Prevention and Control of Noncommunicable Diseases. World Health Organization, 2006. 39) World Health Organization Regional Office for Europe. European Charter on Counteracting Obesity. World Health Organization, 2006.
40) World Health Organization, Regional Office for Europe. Steps to health. European framework to promote physical activity for health. World Health Organization, 2007. 41) European Commission, Directorate Public Health and Risk Assessment. EU Project on Promotion of Breastfeeding in Europe. Protection, promotion and support of breastfeeding in Europe: a blueprint for action. European Commission, 2004. 42) World Health Organization Regional Office for Europe. Proposed outline for the second action plan for food an nutrition policy; document prepared for the WHO European Ministerial Conference on Counteracting Obesity. World Health Organization, 2006.
![Table 3. Stakeholders whose involvement has been called for in policy documents from a range of countries [26].](https://thumb-us.123doks.com/thumbv2/123dok_us/8115979.2152178/12.892.106.781.168.505/table-stakeholders-involvement-called-policy-documents-range-countries.webp)