Photocopying permittedbylicenseonly the Harwood Academic Publishers imprint, part of The Gordon and BreachPublishingGroup. Printed in Malaysia.
Percutaneous
Transluminal
Angioscopy during
Coronary
Intervention
KYOICHI MIZUNO*, SHUNNTA SAKAI, SHINNYA YOKOYAMA, TAKAYOSHI OHBA,
RYUTAUEMURA,YASUTSUGU SEIMIYA,MASAMITSU TAKANO,JUN TANABE,
MASATO TOMIMURA,TAKAHIRO IMAIZUMI, SHUMEI MA, SHIGENOBU INAMI,
KENTAROUOKAMATSU andNORITAKE HATA
CardiovascularCenterand.DepartmentofInternal Medicine, ChibaHokusoh Hospital, Nippon Medical School, 1715 Kamagari, Inba, Chiba, 270-1694,Japan
(Received2May2000," Revised 13June2000,"Infinalform19June2000)
To investigate the feasibility of angioscopic-guided percutaneous transluminalcoronary
angioplasty and to elucidate the mechanism ofefficacy of coronary stenting for acute
myocardial infarction,weperformedcoronary angioscopyin102 patientswithstableangina
oracute myocardialinfarction. Thrombiand intimalflapswereobserved inmost patients
after coronary angioplasty.Largeintimalsplitswereseen in one thirdof patients.Stents
wereinserted in10 patientswho were revealedtohave alargeflaporprotruding split tothe inner lumen. Thrombolytic agents were administered in 2 patients with large thrombi. Additionaltreatmentswererequiredin32% of patients.Noacute myocardialinfarction or unstableangina occurredinpatients during hospitalization.Thus,angioscopy ofthe
coron-ary lumen enables cliniciansto determine themost appropriate and least riskycoronary
intervention strategy. In patients with acute myocardial infarction, angioscopyrevealed occlusiveorprotrudingthrombiin34 of 35 patients.Theprotrudingthrombidisappeared
after stenting.Thefrequency of largeintimal flapsincreased afterpredilatationwith
bal-loon,but thesedisappeared after stenting. Thepresentangioscopic studydemonstrates that
thecoronary stent compressesthe occlusive orprotrudingthrombiand covers theruptured
thrombogenicplaque. Consequently, smooth-surfacedand wide vessel lumen are obtained.
Keywords: PTCA, Acutemyocardialinfarction,Stableangina,Coronarystent
INTRODUCTION
Percutaneous transluminalcoronaryangioscopyis
a new diagnostic tool that permits non-operative
imaging of intravascular structures. It provides a
precise, full-color, three-dimensional perspective
of the interior surface of coronary arteries [1,2].
Thehighresolution of imagescandisclose luminal
changes in minute plaque rupture, ulceration,
intimal flap or torn tissue strands not typically
appreciated by coronary arteriography [3,4].
Color discrimination makes it relatively easy to
distinguish betweenathrombus andaplaque [5,6]. Therefore, angioscopy facilitates not only in the
correlation of anatomical and pathological
fea-turesbut alsoin the monitoring of coronary
inter-ventions. Recently, the coronary stent has been
widely used for the management of abrupt or
threaded occlusionduring percutaneous
translum-inal coronary angioplasty
(PTCA)
(bailout) andfor the management ofacutemyocardialinfarction
[7]. However,
why stenting is efficacious againstacute myocardial infarction remains unclear. The
purposeof this studyis toinvestigate the feasibility
ofangioscopic-guided PTCA and to elucidate the
mechanism of efficacy of coronary stenting for
acute myocardialinfarction.
CORONARY ANGIOSCOPY
Coronary angioscopy was performed using of a
4.5F monorail typed rapid exchange angioscope.
Before coronary angioscopy, thewhitebalancewas
adjustedforcolorcorrection.The coronarylumen
could been observed in 5cm long segments by
inflating the occlusion cuff on the outer catheter
and by moving the optic bundle.Warmsaline
(0.6-0.8
ml/sec)
wasinjectedintothe coronary lumentoobtain aclear view. Light power was adjusted to
avoid refractionandto obtainadequatecolor. The
images were displayed on the monitor and
recor-dedonS-VHS.Angioscopic findingscanbe
classi-fied into the following 7 categories: thrombus,
hemorrhage, dissection, intimal flap, intimal split,
ulceration and stable atheroma, according to
color,mobility, irregularity ofintraluminalsurface,
shape and protrusioninto theinnerlumen.
ANGIOSCOPIC-GUIDED PTCA
Patients
Forty
patients diagnosedwithstable anginaor oldmyocardial infarction underwent coronary
angio-scopy immediately after PTCA. PTCA was
successfullyin all patients by angiographiccriteria
(residualminimumlumen diameter
<=
50%).
Results
Immediately following coronary intervention, the
angioscopic visualization of 40 lesions of the 40
patients were reviewed in the cardiac
catheteliza-tion room.Angioscopy could notbe reviewedin 3
patients because of delivery failure of the
angio-scope
(2
patients) and inadequatevisualization(1
patient). Therefore, 37 patients comprised the
study population. Thebaseline clinical and
angio-graphic characteristics of these 37 patients are
showninTableI. Thrembi wereobservedin most
patients after angioplasty despite the use of
anti-coagulant and antiplatelet agents before and the
duringprocedure.Intimalflapswerealso observed
in mostpatients.
Large
intimal splits were seen inone third of patients
(Table
II).
AngiographyTABLE Angioscopic findings immediately after
PTCAin 37patients
Thrombus 35(96 %)
Hemorrhage 3(80%)
Intimalflap 34(92%)
Intimalsplit 12(32%)
TABLE II Baseline characteristics of patients with stable
angina(n 37)who underwentangioscopic-guidedPTCA
Age (mean+SD) 61+9 Men 27(73%) Hypertension 23(62%) Diabetes millitus 9(24%) Hyperlipidemia 21 (57%) Smoker 14(37%) PreviousMI 11 (30%) Targetvessel LAD 21 (57%) RCA 12(32%) Lcx 4(11%)
No.ofdiseasedvessels
vessel 21 (57%)
2vessels 8(22%)
3vessels 8(22%)
MI: Myocardial infarction, LAD: Left anterior descending,
no acute or subacute coronary occlusions
occur-red. Tissue plasminogen activator was
adminis-tered intracoronary using the guide catheter in
2 patients with large thrombi. Thrombi were
partially dissolved. Additional treatment during
coronary intervention was provided in 12 of 37
patients
(32.4%)
(Fig.2).
No acute myocardialinfarction or unstable angina was observed in
patients during hospitalization, nor at 6-month
postoperative follow-up.
THE MECHANISM OF EFFICACY OF STENT AGAINST ACUTE
MYOCARDIALINFARCTION
FIGURE Angioscopic-guidedPTCA.Afterballoon angio-plasty (POBA), large protruding disruption was observed
byangioscopy (rightupper),but coronaryarteriographyfailed
to disclose disruption (left upper). After stenting, disruption
wassealed with stent(rightlower). Largecoronary lumenwas
obtained(left lower).
Angioscopic findings after PTCA and subsequent management n=3"
Largeflap Largethrombus Smallflap surface protruding disruption n=2 disruption, small thrombus
n=10 n=25
therapy Stent placement Thrombolytic therapy
Noadditional intervention required
FIGURE 2 Changes in management due to angioscopy
during PTCA. Angioscopyinfluencedclinical management in 12 of 37(32.4%)patients.
revealed intimal flaps in only 2 patients and
thrombi in patient.
A
stent was inserted in l0patientswho hadalarge flaporprotruding splitto
theinner lumen in orderto prevent abrupt
occlu-sion of thecoronary artery. After the insertion of
the stent, largeintimal flaps orprotruding
disrup-tions were sealed withthe stent (Fig.
1).
Only tinyflaps were revealedby angioscopy. After stenting,
Patients
Primary stenting was performed in 65 patients
diagnosed with acute myocardial infarction.
Thirty-five of these patients had undergone
suc-cessful coronary angioscopy before coronary
intervention by predilatation with a balloon and
stenting. Baseline clinical and angiographic
char-acteristics of thepatients are shown inTableIII.
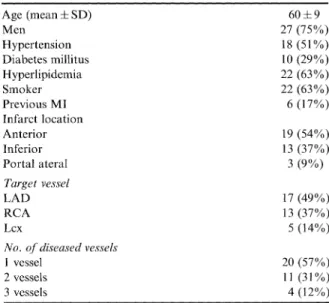
TABLE III Baseline characteristics ofprimary stenting in
patientswith acute myocardial infarction(n 35)
Age (mean+SD) 60+/-9 Men 27(75%) Hypertension 18(51%) Diabetesmillitus 10(29%) Hyperlipidemia 22(63 %) Smoker 22(63%) PreviousMI 6(17%) Infarct location Anterior 19(54%) Inferior 13(37%) Portal ateral 3(9%) Targetvessel LAD 17(49%) RCA 13(37%) Lcx 5(14%)
No. ofdiseasedvessels
vessel 20(57%)
2vessels 11 (31%)
3vessels 4(12%)
MI: Myocardial infarction, LAD: Left anterior descending, RCA: Rightcoronaryartery, Lcx:Left circumflex,No.:Number.
Results
Thrombi wereobservedin34of 35 patients
(97%).
All thrombi were occlusive or protruding before
coronary intervention. After predilatation with a
balloon, the frequency of protruding occlusive
100 9O 10 97% 51% 0%
beforeintervention afterballoon afterstentJng
ansjoplasty
FIGURE3 Changesinprotrudingthrombi before and after
stentingin patients with acutemyocardialinfarction.
100 97% 9O 80 70 6O 50 40 3O 20 10 0 31% O%
beforeintervention after balloon afterstenting an6ioplasty
FIGURE4 Changesinlarge flaps before andafterstentingin
patientswith acutemyocardialinfarction.
thrombi decreased from 97% to 51%
(16
of35).
Mural thrombi were observed in the remaining
patients. After stenting, protrudingthrombi
disap-peared in all patients (Fig.
3). Large
intimal flapswere observed in 11 of 35 patients
(31%)
beforeintervention. The frequency of large intimal flaps
increased after predilatation with a balloon from
31% to 97%.
However,
large intimal flaps weredisappeared after stentingin all patients (Fig.
4).
DISCUSSION
Angioscopic-guidedPTCA
Clinicians have conventionally used angiography
to determine the clinical outcome of coronary
intervention. Unfortunately, angiographic images
capture onlyluminal featuresand, assuch, donot
accurately assess most endovascular therapies.
Although intravascular ultrasoundography
pro-vides cross-sectional images useful in the
assess-ment and guidance of coronary interventions [8],
intravascularultrasound imagesarelimited in
spe-cificity forthrombus formation andintimal flaps.
In the present study, angioscopy indicated that
intimalflaps and thrombi wereoften present after
balloon angioplasty. Previously we reported
that the presence of a large flap, detected by
angioscopy, was associated with acute coronary
occlusion after conventional PTCA
[9].
Otherinvestigators [10,11]using angioscopyalsoshowed
that the primary cause ofpost-angioplasty
occlu-sion was intimal flap in the majority of cases, in
contrast to a thrombus in only a few cases.
Although previous angioscopic researchidentified
the cause of acute occlusion after
PTCA,
fewreports have reported the efficacy ofangioscopic
guidance in optimal coronary interventions. We
inserted the stent at the site of the large flap or
protruding disruptions which were observed by
angioscopy, and thrombolytic therapy was
pro-vided forpatients withlargethrombi afterPTCA.
No recurrent ischemia occurred during patients’
Our present results support the findings of
Teirst-ein etal.
[12]
by confirming the effectiveness ofangioscopy during coronary stenting. Clinical
decisions directly influenced by angioscopy in
Teirstein etal.’s study included the initiation of
intracoronary thrombolytic therapy for a
throm-bus visualized angioscopically, repeat angioplasty
when forming plaquewas seen to be bulging into
the lumen at the stent articulation site, and the
replacement of additional stents replaced when
angioscopy revealed significant proximalor distal
disease/or
an unsuspected gap between 2tandemstents.Angioscopy influenced the clinical
manage-ment of 18
(37.5%)
of their patients. Likewise,Mirecki etal.
[13]
reported that angioscopychan-ged clinical management in 75% of patients,
obviating the need for thrombolytic therapy and
mechanicalintervention, and alteringthe
mechan-ical intervention chosen. In the present study,
angioscopyinfluencedthe clinicalmanagement of
12 outof37
(33%)
patients. Thus, angioscopy ofthe coronary lumen enablesclinicians to determine
the most appropriate and least risky coronary
intervention strategyfor a given patient.
Further-more, angioscopywasusefulfor the prediction and
the prevention ofacute occlusion afterPTCA.
THE MECHANISMOFFEASIBILITY
OFSTENTFORACUTE MYOCARDIAL
INFARCTION
Early inthe implantationofstents,it was thought
that the use of these may be contraindicated if a
thrombus was present in the infarcted vessel
[14,15]. Recently, however, many reports have
shown that coronary stentingis feasibleafteracute
myocardial infarction and is actually associated
with excellent short-term outcomes
[7].
Interest-ingly, this may turn out to be one of the most
important applications of stenting despitetheearly
concerns about stent thrombosis. However, the
mechanism offavourable outcomes remains to be
elucidated. We used angioscopy to examine the
morphological characteristics of the
infarction-related lesion before and after stenting. Smoothly
wide lumina withoutlargeintimalflapsormultiple
lining thrombi but not occlusive or protrusive
thrombi wereobserved after stenting. The present
angioscopicstudy demonstrates that coronarystents
compress the occlusive or protruding thrombi
and cover the ruptured thrombogenic plaques.
Consequently, smooth-surfacedwidevessel lumen
areobtained.These findings reveal that the
utiliza-tion of stenting as an acute-stage intervention in
patients with acute myocardial infarction induces
morefavorableclinical outcomes.
References
[1] Mizuno,K., Arai,T., Satomura, K.etal.New
percutan-eous transluminal coronary angioscope. J. Am. Coll. Cardiol.1989; 13: 363-368.
[2] Sherman, C.T., Litvack, F. and Grundfest, W. etal.
Coronary angioscopy in patients with unstable angina
pectoris. N. Engl. J.Med. 1986;315: 913-919.
[3] Mizuno, K., Miyamoto, A., Satomura, K. etal.
Angio-scopiccoronary macromorphologyinpatientswith acute coronary disorders.Lancet 1991;337:809-812.
[4] Ramee, S.R.,White,C.J.,Collins,T.J.,etal.Percutaneous
angioscopyduring coronaryangioplastyusingasteerable microangioscope. J. Am. Coll. Cardiol.1991; 17: 100-105.
[5] Uchida, Y., Hasegawa, K., Kawamura,K. etal. Angio-scopic observation of the coronary luminal changes
induced by percutaneous transluminal coronary angio-plasty.Am.Heart 1989;117: 769-776.
[6] Mizuno, K., Satomura, K., Miyamoto, A. etal. Angio-scopic evaluation of coronary-artery thrombi in acute coronarysyndromes. N. Engl. J.Med. 1992;326:287-291.
[7] Gregg,W.S. Prospective, multicenter studyof the safety
and feasibility of primary stenting in acute myocardial
infarction:in-hospitaland30-day resultofthePAMIstent
pilottrial.J.Am. Cardiol.1998;31:23-30.
[8] Colombo,A.,Hall,P.,Nakamura, S. etal.Intracoronary
stentingwithout anticoagulationaccomplishedwith intra-vascularultrasound guidance.Circulation 1995;91: 1676.
[9] Mizuno,K.,Ohkuni,S., Takano,M. etal. Usefulness of coronaryangioscopy during coronaryintervention.J.Jpn.
Coll. Angiol. 1999;39: 33.
[10] White, C.J., Ramee, S.R., Collins, T.J. etal. Coronary
angioscopy of abrupt occlusionafterangioplasty. J. Am.
Coll. Cardiol.1995;25: 1681-1684.
[11] Waxman, S., Sassower, M.A., Mittleman, M.A. etal.
Angioscopic predictors of early adverse outcome after coronaryangioplastyinpatientswithunstable anginaand
non-Qwavemyocardioalinfarction. Circulation 1996;93:
2106-2113.
[12] Teirstein,P.S.,Schatz,R.A.,ChuiWong,S.etal.
Coron-ary stenting with angioscopic guidance. Am. J. Cardiol.
1995; 75: 34.4-347.
[13] Mirecki,F.,Sharaf,B.,Williams,D.Intracoronary
acute coronary syndromes. J. Am. Coll. Cardiol. 1994;
Abst: 170A.
[14] Monassir,J.P., Hamon,M.,Elias,J.etal. Earlyversuslate coronary stenting following acute myocardialinfarction:
Result oftheSTENTIM study(Frenchregistryof
sten-ting in acute myocardial infarction). Cathet Cardiovasc Diagn 1997;42: 243-248.
[15] Urban, P., Macaya, C., Rupprecht, H.J. etal. For
the MATTIS Investigators. Randomized evaluation
of anticoagulation versus antiplatelet therapy after coronary stent implantation in high risk patients. The Multicenter Aspirin and Ticlopidine Trial after
Intracoronary Stenting (MATTIS). Circulation 1998; 98:
Submit your manuscripts at
http://www.hindawi.com
Stem Cells International Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
MEDIATORS
INFLAMMATIONof
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Behavioural
Neurology
Endocrinology
International Journal ofHindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Disease Markers
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
BioMed
Research International
Oncology
Journal ofHindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014 Oxidative Medicine and Cellular Longevity Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
PPAR Research
The Scientific World Journal
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Immunology Research
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Journal of
Obesity
Journal ofHindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014 Computational and Mathematical Methods in Medicine
Ophthalmology
Journal ofHindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Research and Treatment
AIDS
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporation
http://www.hindawi.com Volume 2014