Behavior and Quality of Life at 6 Years
for Children With Hypoplastic Left
Heart Syndrome
Caren S. Goldberg, MD,aChenwei Hu, MS,bCheryl Brosig, PhD,cJ. William Gaynor, MD,dWilliam T. Mahle, MD,e Thomas Miller, DO,fKathleen A. Mussatto, PhD,cRenee Sananes, PhD,gKaren Uzark, PhD,aFelicia Trachtenberg, PhD,b Christian Pizarro, MD,hVictoria L. Pemberton, MS,iAlan B. Lewis, MD,jJennifer S. Li, MD,k,l,mJeffrey P. Jacobs, MD,n James Cnota, MD,oAndrew M. Atz, MD,pWyman W. Lai, MD,sDavid Bellinger, PhD,q,rJane W. Newburger, MD,rPHN INVESTIGATORS
abstract
OBJECTIVES:We measured behavioral, quality of life (QoL), and functional status outcomes for6-year-old children with hypoplastic left heart syndrome enrolled in the Single Ventricle Reconstruction Trial. We sought to compare these outcomes with those in the normative population and to analyze risk factors for worse outcomes within the single-ventricle group.
METHODS:Parent-response instruments included the Vineland Adaptive Behavior Scales, Second
Edition (Vineland-II) (primary outcome), Behavior Assessment System for Children 2, Pediatric Quality of Life Inventory 4.0, and other measures of QoL and functional status. We compared subjects with those in the normative sample using 1-sample Wilcoxon rank tests and assessed outcome predictors using multivariable regression.
RESULTS:Of 325 eligible patients, 250 (77%) participated. Compared with population norms,
participants had lower scores on the Vineland-II motor skills domain (90617 vs 100615;
P,.001), with 11% scoring.2 SDs below the normative mean. On nearly all major domains, more study subjects (3.3%–19.7%) scored outside the normal range than anticipated for the general population. Independent risk factors for lower Vineland-II scores included
perioperative extracorporeal membrane oxygenation, male sex, use of regional cerebral perfusion, catheterization after stage 2 operation, visual problems, seizure history, and more complications after 2 years (R2= 0.32). Independent predictors of worse Behavior Assessment System for Children 2 (R2 = 0.07–0.20) and Pediatric Quality of Life Inventory 4.0 (R2 = 0.17–0.25) domain scores also included sociodemographic factors and measures of morbidity and/or greater course complexity.
CONCLUSIONS:At 6 years, children with hypoplastic left heart syndrome had difficulty in areas of adaptive behavior, behavioral symptoms, QoL, and functional status. Principal risks for adverse outcomes include sociodemographic factors and measures of greater course complexity. However, models reveal less than one-third of outcome variance.
WHAT’S KNOWN ON THIS SUBJECT:Children with hypoplastic left heart syndrome and other related single-ventricle anomalies have been shown to be at increased risk for neurocognitive and behavioral impairments.
WHAT THIS STUDY ADDS:This study includes a large cohort of children with hypoplastic left heart syndrome and related anomalies whose clinical course has been prospectively characterized since birth and provides an exceptional opportunity to identify risks for adverse behavioral, quality of life, and functional status outcomes.
To cite:Goldberg CS, Hu C, Brosig C, et al. Behavior and Quality of Life at 6 Years for Children With Hypoplastic Left Heart Syndrome.Pediatrics. 2019;144(5):e20191010
a
Department of Pediatrics, Medical School, University of Michigan and Michigan Medicine, Ann Arbor, Michigan;
bNew England Research Institutes, Watertown, Massachusetts;cDepartment of Pediatrics, Medical College of
Wisconsin and Children’s Hospital of Wisconsin, Milwaukee, Wisconsin;dPediatric Cardiothoracic Surgery, School of Medicine, University of Pennsylvania and Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania;
eDepartment of Pediatrics, Emory University and Children’s Healthcare of Atlanta, Atlanta, Georgia;fDepartment of
Pediatrics, and The University of Utah and Primary Children’s Hospital, Salt Lake City, Utah;gLabatt Family Heart
Center, Hospital for Sick Children, Toronto, Canada;hDepartment of Surgery, Nemours Cardiac Center, Nemours/
Alfred I. duPont Hospital for Children, Wilmington, Delaware;iNational Heart, Lung, and Blood Institute, National
Institutes of Health, Bethesda, Maryland;jDepartment of Pediatrics, Children’s Hospital Los Angeles, Los Angeles,
California;kDepartment of Pediatrics, Duke University, Durham, North Carolina;lDepartment of Pediatrics, East Carolina University, Greenville, North Carolina;mDepartment of Pediatrics, Wake Forest University, Winston-Salem,
Among congenital heart defects, hypoplastic left heart syndrome (HLHS) carries the greatest risk of neurodevelopmental impairment.1 Many factors contribute to adverse neurodevelopment in children with HLHS and other single right ventricular anomalies, including patient characteristics,2genetic factors, operative and perioperative events during admission for the Norwood procedure, the need for unexpected operations, and general cardiac morbidities, such as cyanosis and congestive heart failure.3–5 Previous studies of
neurodevelopmental outcome in patients with HLHS at early school age have been handicapped by relatively small sample sizes, cross-sectional design, and limited power for multivariable analysis.
From 2005 to 2008, children with HLHS and other related single right ventricle anomalies were enrolled prospectively from 15 North American centers in the Pediatric Heart Network’s Single Ventricle Reconstruction Trial (SVR) and randomly assigned either to a modified Blalock-Taussig shunt (MBTS) or a right ventricle to pulmonary artery shunt (RVPAS) at the time of the neonatal Norwood operation.6,7We have previously published the developmental and behavioral outcomes measured at the 1-year4,8and 3-year follow-up.5We report here thefindings related to adaptive behavior, behavioral symptoms, quality of life (QoL), and functional status measured for the SVR cohort at age 6 years and the risk factors for adverse outcomes.
METHODS
Subjects
In the SVR, 549 neonates with HLHS and other related single right ventricle malformations from 15 centers were randomly assigned either to the MBTS or the RVPAS and underwent the Norwood operation.6
Transplant-free survivors from this trial were eligible to participate in the neurodevelopmental aim of the SVR Extension Study,9which included parent completion of multiple measures focused on development, adaptive behavior, behavioral symptoms, and QoL outcomes annually from 3 to 6 years of age. We focus here on thefindings at 6 years. The study was approved by each center’s institutional review board, and written informed consent was obtained from a parent or guardian.
Data Obtained
Research coordinators reviewed the medical records and contacted parents or guardians annually to obtain the interim medical history. As previously described, we collected data related to growth, feeding modality, participation in
developmental therapies, surgical and catheterization interventions, and the incidence of major complications.9
Developmental Questionnaires
Adaptive behavior, behavioral symptoms, and QoL were measured with psychometrically valid
questionnaires, including the Vineland Adaptive Behavior Scales, Second Edition (Vineland-II), the Behavior Assessment System for Children 2 (BASC-2), the Child Health Questionnaire Parent Report Form 50 (CHQ-PF50), and the Pediatric Quality of Life Inventory 4.0 (PedsQL). The Functional Status Revised Second Edition (FSII[R]) served as an overall measure of functional status. Of note, scores on these questionnaires reflect parent ratings of their children.
The Vineland-II is a practical measure of a child’s daily functioning and therefore was the primary outcome measure for this study. It was administered by using the parent or caregiver rating form. This
instrument is used to assess 4 domains of development: (1)
FIGURE 1
communication skills, (2) skills of daily living, (3) socialization, and (4) motor skills. Information from these domains is combined to obtain the adaptive behavior composite score. The standard normative score for each domain is 100 (SD 15)10; higher scores indicate better development.
The BASC-2 parent report was used to measure adaptive and abnormal behaviors present in both the home and school. The report includes 14 subscales that compose 4 composite scores: internalizing problems, externalizing problems, behavioral symptoms index, and adaptive skills. The BASC-2 was completed at 3, 4, 5, and 6 years of age. Scores on each composite are compared with the standard population mean score of 50 points (SD 10). For the adaptive scales, higher scores indicate better performance; scores are considered at risk or clinically significant if they are between 31 and 40 or,31, respectively. For scales used to
measure behavioral problems, higher scores indicate worse performance; scores are considered at risk or clinically significant if they are between 60 and 69 or.69, respectively.11
QoL measurement was performed at 6 years with both the PedsQL and the CHQ-PF50. The PedsQL instrument is used to address physical, emotional, social, and school functioning. The PedsQL cardiac disease–specific module was used to assess issues of QoL specific to children with cardiac disease.12For each of these modules, higher scores represent better health-related QoL.13The CHQ-PF50 includes 50 items to assess 14 concepts (physical functioning, physical role or social limitations, general health, bodily discomfort, parental impact, emotional role or social limitations, self-esteem, mental health, general behavior, family, and change in health); higher scores represent better QoL.14
Functional status was assessed at 6 years with the FSII(R). The FSII(R) is used to assess the degree of daily age-appropriate function and provide a total score with common elements across all ages. Greater scores reflect better functional status.15
Statistical Methods
All analyses were conducted by using SAS version 9.4 (SAS Institute, Inc, Cary, NC), and statistical significance was tested at a level of 0.05 unless otherwise noted. Characteristics of subjects who did and did not complete the Vineland-II at age 6 years were compared by using
ttests,x2tests, and Fisher’s exact tests. The percentage outside the normal range was calculated for each major index. The study cohort was compared with the normative population for each scale by using 1-sample Wilcoxon rank tests. Although Wilcoxon rank tests were used because of nonnormal distribution, means and SDs are reported to be
TABLE 1SVR Cohort Main Outcomes at 6 Years Compared With Normative Sample
Instrument and Domain SVR Cohort Mean (SD) Abnormal (.1 SD) From Normative Mean (%)a
Abnormal (.2 SD) From Normative Mean (%)b
Normative Sample Mean (SD)
Pc
Vineland-II
Communication 104.3 (18.6) 24/222 (10.8) 10/222 (4.5) 100 (15) ,.001 Daily living skills 102.3 (21.8) 17/215 (7.9) 15/215 (7.0) 100 (15) .035
Socialization 104.6 (19.5) 17/182 (9.3) 6/182 (3.3) 100 (15) ,.001
Motor skills 90.3 (17.8) 49/215 (22.8) 24/215 (11.2) 100 (15) ,.001 Adaptive behavior composite 101.1 (19.9) 26/171 (15.2) 10/171 (5.8) 100 (15) .218 BASC-2
Internalizing behavior 48.2 (9.9) 11/245 (4.5) 8/245 (3.3) 50 (10) ,.001 Externalizing behavior 49.4 (10.1) 18/244 (7.4) 10/244 (4.1) 50 (10) .040 Behavior symptoms index 50 (10) 24/244 (9.8) 10/244 (4.1) 50 (10) .318 Adaptive skills composite 47.3 (11.8) 54/244 (22.1) 16/244 (6.6) 50 (10) .001 PedsQL generic module
Physical function 70.6 (23.2) 55/248 (22.2) 26/248 (10.5) 80.4 (20.8) ,.001 Emotional function 77.0 (18.2) 33/248 (13.3) 19/248 (7.7) 80.1 (15.9) .007 Social function 76.1 (19.0) 62/248 (25.0) 5/248 (2.0) 80.6 (20.4) ,.001 School function 70.1 (20.1) 57/247 (23.1) 12/247 (4.9) 77.4 (19.5) ,.001 Psychosocial health 74.4 (15.6) 59/248 (23.8) 12/248 (4.8) 79.4 (15.3) ,.001 Total score 73.1 (16.7) 57/248 (23.0) 19/248 (7.7) 79.7 (15.9) ,.001 CHQ-PF50
Physical summary T-score 43.1 (12.3) 53/248 (21.4) 38/248 (15.3) 53.1 (10.4) ,.001 Psychosocial summary
T-score
51.7 (8.7) 38/248 (15.3) 16/248 (6.5) 52.5 (7.6) .156 FSII(R)
Total score 92.4 (9.4) 30/249 (12.0) 49/249 (19.7) 97.7 (4.5) ,.001
aFor the normative sample, 15.9% would be expected to score 1 SD below the mean. bFor the normative sample, 2.3% would be expected to score 2 SD below the mean.
consistent with available norms. To identify predictors of adaptive behavior, behavioral symptoms, and QoL outcomes, an extensive list of sociodemographic, surgical, and additional clinical variables was considered (Supplemental Table 7). For each outcome measure, univariate linear regression models werefitted for all candidate
predictors, including both continuous and categorical variables as well as quartiles of continuous variables. Predictors withP,.2 were candidates for entry into the
multivariable regression model. If the
Pvalues of both continuous and categorical variables for the same predictor were,.2, the more significantly associated one was selected (Supplemental Table 7). To improve thefit of the multivariable models by reducing collinearity of predictors, Pearson correlations among the candidate predictors were calculated. Pairs or groups with a correlation.0.5 or,20.5 were noted and considered to have a strong correlation, and 1 of the variables from each pair or group was then chosen for inclusion as
a candidate risk factor on the basis of consensus of clinical experts
(Supplemental Table 7). Finally, backward selection was used to build thefinal model, with a criterion of
P,.05 for entry.
RESULTS
Among the 325 transplant-free survivors from the original SVR cohort enrolled in the Extension Study, 14 had died by age 6 years, 14 underwent a cardiac transplant, 3 had undergone a biventricular repair, and 3 had withdrawn from the study before reaching the age of 6 years. Of the remaining 291 subjects, 250 (86%) completed at least 1 of the questionnaires at 6 years (Fig 1). Compared with eligible
nonparticipants, those who completed the Vineland-II had a higher socioeconomic status, were
less likely to have a genetic syndrome, and were less likely to be Hispanic (Supplemental Table 8).
Questionnaire Scores
Questionnaire scores for the study cohort and the normative scores are summarized in Table 1.
Vineland-II
Compared with the normative sample scores, Vineland-II scores for the SVR cohort were similar in all domains except the motor skills score, which was lower (worse) for the study cohort (90.3617.8 vs 100615;P, .001). Scores for the communication
FIGURE 2
SVR sample scores for the BASC-2: box and whisker plots for BASC-2 domains. A, Components of the behavioral symptoms index are on the x-axis. B, Components of the Adaptive skills composite are on the x-axis. The solid lines represent the normative sample means. The dashed lines mark the bounds of the normal range. Lower scores are better for the behavioral symptoms index and its compo-nents. Higher scores are better for the adaptive skills composite and its compocompo-nents. Higher scores indicate more concerns on the BASC-2 behavior symptoms index and its components. Lower scores indicate more concerns on the BASC-2 adaptive skills composite and its components.
TABLE 2Models for Each Outcome With R2 . 0.10: Vineland-II Adaptive Behavior Composite: Standard Score (n= 152, AdjustedR2= 0.32)
Variable Estimate P AdjustedR2
Male sex 28.5 .002 0.05
Perfusion type .04 0.03
DHCA only 2.6 — —
RCP and DHCA time#10 min 25.2 — —
RCP and DHCA with DHCA time.10 min Reference — — Need for ECMO during hospitalization 212.8 .02 0.02 Need for catheterization after stage 2 surgery 219.4 .02 0.03 Seizures reported before 6 y 211.4 .006 0.04 Vision problems infirst year 217 .006 0.06 Total complications from 2 y to Vineland-II 21.03 .002 0.02
(P,.001) and socialization scales (P,.001) were significantly higher (better) for the study cohort
compared with the normative sample. A greater percentage of the study cohort had scores outside of the normal range than would be
anticipated for the general population (Table 1).
BASC-2
The BASC-2 behavioral symptoms index composite was not significantly different for the SVR participants compared with population norms (Fig 2A). Among the subscales contributing to the BASC-2 behavior symptoms index, somatization was significantly worse for the SVR cohort compared with the normative sample. For all other subscales contributing to the behavior symptoms index, either scores were similar or the SVR cohort scored better, with less or no difference in reported hyperactivity, aggression, anxiety, depression, atypicality, withdrawal, and attention problems. However, even in those subdomains for which the SVR cohort mean scores were similar or better than the normative scores, more individuals than expected for the standard population had scores more than 2 SDs lower than the normative mean score (Table 1, Fig 2A). The study cohort, compared with the normative sample, scored
significantly worse on the BASC-2 internalizing and externalizing behavior scales and the adaptive skills composite, with worse subscale scores on activities of daily living and functional communication (Table 1, Fig 2B).
QoL and Functional Status
QoL was reported to be lower for the SVR cohort compared with the normative sample. Among the PedsQL generic core scales, physical
functioning was most impaired in the study cohort compared with the normative sample (71623 vs 806 21;P,.001). In addition, the SVR cohort demonstrated less favorable
scores on the PedsQL psychosocial health summary (Table 1). The PedsQL cardiac module includes referent scores for cardiac patients with mild, moderate, surgically treated, and complex or severe congenital heart disease (CHD).13 Scores on this module for the SVR cohort were most similar to scores for those with complex or severe CHD and surgically treated CHD
(Supplemental Table 9). On the CHQ-PF50, the SVR cohort scored
significantly lower (worse) on the physical summary scale but,
interestingly, not on the psychosocial summary scale (Table 1). Among the subscales, the SVR cohort scored significantly lower on multiple domains, including physical functioning (81623 vs 97615;
P,.001), emotional functioning (89622 vs 95616;P,.001), self-esteem (85616 vs 87613;P= .04), general health perceptions (46618 vs 74619;P,.001), emotional impact on parents (61627 vs 806 20;P,.001) time impact on parents (83623 vs 89619;P,.001), and family activities (77623 vs 88620;
P,.001). On the FSII(R), the SVR cohort had worse functional status compared with the normative sample, consistent withfindings from the Vineland-II motor domain and the PedsQL physical functioning scores (Table 1).
Multivariable Analyses
Independent risk factors for lower scores on the Vineland-II adaptive behavior composite included male
TABLE 3Models for Each Outcome WithR2.0.10: BASC-2 Adaptive Skills Composite: Standard Score (n= 212, AdjustedR2= 0.20)
Variable Estimate P AdjustedR2
Male sex 25.3 .0006 0.04
Race .02 0.02
African American 24.25 — —
Other 7.56 — —
White Reference — —
Need for additional operations after Norwood procedure 27.3 .009 0.02 Seizures reported before 6 y 25.6 .01 0.02 Vision problems infirst year 28.2 .02 0.05
SES score 0.44 .005 0.04
WHO wtzscore at 14 mo 1.8 .02 0.01
Lowest temperature obtained during bypass 20.7 .05 0.01
SES, socioeconomic status; WHO, World Health Organization;—, not applicable.
TABLE 4Models for Each Outcome WithR2.0.10: PedsQL Physical Functioning Score at 6 Years (n= 209, AdjustedR2= 0.25)
Variable Estimate P AdjustedR2
Race .04 0.02
African American 1.83 — —
Other 20.02 — —
White Reference — —
Hollingshead score (SES) 0.22 .02 0.02
Cross-clamp time at Norwood procedure .0006 0.06
0.0–39.5 29.8 — —
.39.5–51.0 217.1 — —
.51.0–65.0 210.7 — —
.65.0–194.0 Reference — —
Steroids used during Norwood procedure 12.4 .005 0.03 Fontan procedure hospitalization duration 20.2 .04 0.05
Total surgeries 22.7 .001 0.04
Protein-losing enteropathy 229.2 .0007 0.04 Any early intervention services 7.4 .02 0.02
Ever had GJ tube 225.0 .008 0.03
sex, use of regional cerebral perfusion during the Norwood procedure, extracorporeal membrane oxygenation (ECMO) at any time, seizures at any time, performance of nonroutine catheterizations after stage 2 surgery, visual problems detected and reported by 1 year of age, and greater number of
complications reported between ages 2 and 6 years. However, only one-third of the variance in outcomes was explained by this model (adjusted
R2= 0.32; Table 2). Although some
point estimates are larger than expected, it is noteworthy that a small number of participants had some of these risk factors; for example, only 11 participants required ECMO, 7 had catheterizations after stage 2 surgery, and 10 had reported vision problems.
We also constructed multivariable models for each of the primary scales of the BASC-2, PedsQL, and CHQ-PF50; thefinal models are detailed in Tables 2 through 6 for each domain model withR2.0.10. The variability explained by the models ranged from 7% to 32%. Some demographic and perfusion variables were included in these models, but we found that most of the predictive variables were measures of a complex course or greater morbidity (Tables 2 through 6, Fig 3).
DISCUSSION
Children with HLHS and related single right ventricular anomalies have a multitude of risk factors for impaired neurodevelopmental and behavioral outcomes, spanning innate factors (genetic abnormalities and impaired fetal cerebral oxygen delivery), operative and perioperative complexity, and long-term medical morbidities. The SVR Extension Study was designed to survey the SVR cohort through 6 years of age, providing an unparalleled opportunity to study subject characteristics, perioperative factors, and therapies that predict
longer-term neurodevelopmental, behavioral, QoL, and functional outcomes in a well-characterized population at high risk for neurodevelopmental morbidity.
We found that, by parent report at subject age 6 years, children with HLHS and other single right ventricle malformations had more
abnormalities in adaptive behavior and behavioral symptoms and lower health-related QoL and functional status than the normative population. In particular, subjects with HLHS and related disorders scored worse in measures of motor function, somatization, functional
communication, activities of daily living, adaptive skills, and QoL. Most independent predictors of adaptive behavior, behavioral symptoms, and QoL outcomes reflected greater course complexity and morbidity. Multivariable modeling predicted only 7% to 32% of variability in adaptive behavior, behavioral symptoms, and QoL domains despite the prospective study design and
collection of an extensive list of clinical factors beginning at birth.
In some domains, the mean score for the SVR cohort was actually better than the score for the normative sample, but the SDs were large, and the distribution of scores consistently skewed left, with a greater number of low scores than expected for the general population. Such
a distribution, combined with the limited explanation of the variance in our models, highlights the limitations of empirical prediction of
neurodevelopmental outcomes based on cardiac diagnosis and history alone. These data suggest that individual assessment is required to determine neurodevelopmental strengths and weakness in children with complex CHD. Evaluation of this cohort with an in-person
neurodevelopmental assessment at 10 to 12 years of life is in progress and should clarify if there are areas of strength for this cohort or if the positivefindings reflect parental underreporting of problems.
TABLE 5Models for Each Outcome With R2 .0.10: Multivariable Model for PedsQL Psychosocial Health Summary Score at 6 Years (n= 206, AdjustedR2= 0.17)
Variable Estimate P Adjusted
R2 Any early intervention up to Vineland-II 26.2 .005 0.03
Ever had G-tube 25.9 .03 0.02
WHO wtzscore before Norwood procedure 1.46 .03 0.02
Total support time 0.02 .03 0.02
Total complications from 2 y to Vineland-II 20.80 .0018 0.05
G-tube, gastric tube; WHO, World Health Organization.
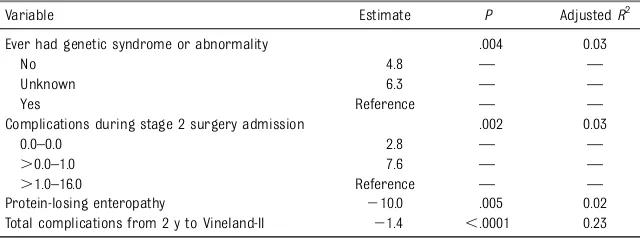
TABLE 6Models for Each Outcome WithR2.0.10: CHQ Physical Summary T-Score at 6 Years (n= 223, AdjustedR2= 0.31)
Variable Estimate P AdjustedR2
Ever had genetic syndrome or abnormality .004 0.03
No 4.8 — —
Unknown 6.3 — —
Yes Reference — —
Complications during stage 2 surgery admission .002 0.03
0.0–0.0 2.8 — —
.0.0–1.0 7.6 — —
.1.0–16.0 Reference — —
Protein-losing enteropathy 210.0 .005 0.02 Total complications from 2 y to Vineland-II 21.4 ,.0001 0.23
With this study, we provide the most extensive evaluation of adaptive behavior, behavioral symptoms, and QoL in early school-aged children with HLHS and related disorders. Our
findings are consistent with smaller studies that have revealed similar risk factors for adverse outcomes. Reich et al,16in a 2-center study, found that longer length of stay and a greater need for interventions were both
associated with lower scores on measures of neurodevelopment for patients with pre-Fontan single ventricle heart disease. Our study
findings also build on earlier evaluations of this same cohort. At age 14 months of age, lower scores on the Bayley Scales of Infant
Development, Second Edition were most highly associated with innate patient factors (eg, low birth weight,
genetic syndromes, lower maternal education) and greater overall morbidity in thefirst year than with intraoperative management
strategies.4,8At 3 years of age, lower scores on the Ages and Stages Questionnaire were associated with more clinical complications, abnormal growth, and evidence of feeding, vision, or hearing problems. However,
,30% of variation in scores could be explained by the models.5Future studies to determine the value of early measures in predicting later neurodevelopmental outcomes may be helpful as we search for improved prognosticators for individuals.
The overarching aim of the SVR was to determine if the Norwood procedure with the MBTS or the RVPAS resulted in better outcomes for children with HLHS and other related cardiac malformations. We did notfind that shunt type was associated with any of the adaptive behavior, behavioral symptoms, QoL, or functional status outcomes measured at 6 years. We also collected an in-depth array of variables related to intraoperative techniques and vital organ support during the Norwood operation as we sought to identify any modifiable risk factors. Interestingly, we found that a primary strategy of regional cerebral perfusion rather than deep
hypothermic circulatory arrest was associated with significantly worse scores on the Vineland-II adaptive behavior composite. Despite widespread use of regional cerebral perfusion as a neuroprotective approach, ourfinding of its association with worse outcomes is consistent withfindings of earlier single-center studies.17–19Because perfusion strategy was not randomly assigned but rather performed according to the center or surgeon’s preference, further study is warranted. No other
intraoperative variables were predictive of 6-year outcomes.
The suspected or definite presence of genetic abnormalities was an independent predictor of worse
FIGURE 3
scores on the mental development index of the Bayley Scales of Infant Development, Second Edition at age 14 months.4However, we did notfind a significant relation of genetic abnormalities to adaptive behavior, behavioral symptoms, or QoL outcomes at age 6 years. The absence of such a relation may be related, in part, to greater mortality before age 6 years in the group with genetic abnormalities, a smaller percentage variance contributed by genetic abnormalities to neurodevelopmental measures in the setting of important cumulative acquired neurologic morbidity, or the absence of assessment of all study subjects by a geneticist. Future analyses are underway to correlate
neurodevelopmentalfindings with results of whole-exome sequencing in a subset of subjects with HLHS. In addition, further study should be used to explore additional genetic and in utero factors in improving
prognostication for later
neurodevelopmental outcomes in this at-risk population.
Other limitations of our study should be noted. Participation in this midterm follow-up study of the SVR cohort was excellent (82% of eligible participants completed the primary outcome measure, and 86%
completed at least 1 of the measures). Participants had fewer risk factors (eg, low socioeconomic status) for impaired neurodevelopment compared with nonparticipants, suggesting that the
neurodevelopmental outcomes measured in this study likely underestimate the impairment burden for children with HLHS. This follow-up study of the SVR cohort did not include in-person evaluations, and outcome measures were based on parent-report instruments, which can be biased, and in some cases, may overestimate a child’s capabilities.20 Subjectivity of parent reports as well as differences in evaluation measures among instruments may account for a few discordantfindings, such as better-than-normal scores on socialization on the Vineland-II yet worse social functioning on the PedsQL.
Many risk factors were highly collinear, and some late postoperative morbidities may have been in the causal pathway of earlier risk factors. Models included some risk factors, such as ECMO and protein-losing enteropathy, that were rare among the study group, potentially
overestimating the influence of these factors. Finally, our study design permitted us to explore associations, but apart from the role of Norwood procedure shunt type, we cannot draw conclusions about causality.
CONCLUSIONS
We found that at 6 years of age, children with HLHS and other related single right ventricle malformations have more abnormalities in areas of adaptive behavior and behavioral symptoms and have lower scores on
health-related QoL than the general population. Predictive models for these outcomes included
sociodemographic and rare
modifiable intraoperative variables, but most risk factors were indicators of course complexity and overall morbidity. In-person evaluation for the SVR cohort at age 10 to 12 years is currently underway to better characterize their
neurodevelopmental profile and brain MRIfindings.
ABBREVIATIONS
BASC-2: Behavior Assessment System for Children 2 CHD: congenital heart disease CHQ-PF50: Child Health
Questionnaire Parent Report Form50 ECMO: extracorporeal membrane
oxygenation
FSII(R): Functional Status Revised Second Edition
HLHS: hypoplastic left heart syndrome
MBTS: modified Blalock-Taussigshunt
PedsQL: Pediatric Quality of Life Inventory 4.0
QoL: quality oflife
RVPAS: right ventricle to pulmonary arteryshunt
SVR: Single Ventricle Reconstruction Trial
Vineland-II: Vineland Adaptive Behavior Scales, Second Edition
nCongenital Heart Institute of Florida, St Petersburg, Florida;oDepartment of Pediatrics, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio;pDepartment of Pediatrics, Medical University of South Carolina, Charleston, South Carolina;qDepartment of Neurology, Boston Children’s Hospital and Harvard Medical School, Boston, Massachusetts;rDepartment of Cardiology, Boston Children’s Hospital, Boston, Massachusetts; andsDepartment of Pediatrics, NewYork-Presbyterian Morgan Stanley Children’s Hospital, New York, New York
Drs Goldberg and Newburger conceptualized the study design, interpreted the results, drafted the manuscript, and worked with the other authors to revise the manuscript; Ms Hu and Dr Tractenberg were involved with the study design, conducted the analysis, and edited the manuscript; Drs Gaynor, Mahle, Miller, Mussatto, Sananes, Uzark, Pizarro, Lewis, Li, Jacobs, Cnota, Atz, Lai, and Ms Pemberton were involved with the study design and interpreting the results, and participated in critical editing of the manuscript; Dr Bellinger helped to determine the neuropsychological instruments to be used, was involved in the study design and interpreting the results, and participated in critical editing of the manuscript; and all authors approved thefinal manuscript as submitted and agree to be accountable for all aspects of the work.
Accepted for publication Aug 5, 2019
Address correspondence to Caren S. Goldberg, MD, Division of Pediatric Cardiology, C.S. Mott Children’s Hospital, University of Michigan, 1540 E Hospital Dr, Ann Arbor, MI 48109. E-mail: cgoldber@med.umich.edu
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2019 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE:The authors have indicated they have nofinancial relationships relevant to this article to disclose.
FUNDING:Supported by grants (HL068270, HL068290, HL109673, HL109737, HL109741, HL109741, HL109743, HL109777, HL109778, HL109781, HL109816, and HL109818) from the National Heart, Lung, and Blood Institute, National Institutes of Health. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST:The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER:A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2019-1664.
REFERENCES
1. Gaynor JW, Stopp C, Wypij D, et al; International Cardiac Collaborative on Neurodevelopment (ICCON)
Investigators. Neurodevelopmental outcomes after cardiac surgery in infancy.Pediatrics. 2015;135(5):816–825
2. Gaynor JW, Wernovsky G, Jarvik GP, et al. Patient characteristics are important determinants of
neurodevelopmental outcome at one year of age after neonatal and infant cardiac surgery.J Thorac Cardiovasc Surg. 2007;133(5):1344–1353, 1353–3
3. Morton PD, Ishibashi N, Jonas RA. Neurodevelopmental abnormalities and congenital heart disease: insights into altered brain maturation.Circ Res. 2017;120(6):960–977
4. Newburger JW, Sleeper LA, Bellinger DC, et al; Pediatric Heart Network Investigators. Early developmental outcome in children with hypoplastic left heart syndrome and related anomalies: the single ventricle reconstruction trial.Circulation. 2012; 125(17):2081–2091
5. Goldberg CS, Lu M, Sleeper LA, et al; Pediatric Heart Network Investigators. Factors associated with
neurodevelopment for children with single ventricle lesions.J Pediatr. 2014; 165(3):490–496.e8
6. Ohye RG, Sleeper LA, Mahony L, et al; Pediatric Heart Network Investigators. Comparison of shunt types in the Norwood procedure for single-ventricle lesions.N Engl J Med. 2010;362(21): 1980–1992
7. Ohye RG, Gaynor JW, Ghanayem NS, et al; Pediatric Heart Network
Investigators. Design and rationale of a randomized trial comparing the Blalock-Taussig and right ventricle-pulmonary artery shunts in the Norwood procedure.J Thorac Cardiovasc Surg. 2008;136(4):968–975
8. Mahle WT, Lu M, Ohye RG, et al. A predictive model for
neurodevelopmental outcome after the Norwood procedure.Pediatr Cardiol. 2013;34(2):327–333
9. Newburger JW, Sleeper LA, Gaynor JW, et al; Pediatric Heart Network Investigators. Transplant-free survival and interventions at 6 years in the SVR trial.Circulation. 2018;137(21): 2246–2253
10. Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales: Survey Forms Manual, 2nd ed. Minneapolis, MN: NCS Pearson; 2005
11. Reynolds CR, Kamphaus RW.Behavior Assessment System for Children, 2nd ed. Circle Pines, MN: American Guidance Service, Inc; 2004
12. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations.Med Care. 2001; 39(8):800–812
13. Uzark K, Jones K, Slusher J, et al. Quality of life in children with heart disease as perceived by children and parents.Pediatrics. 2008;121(5). Available at: www.pediatrics.org/cgi/ content/full/121/5/e1060
14. Landgraf JM, Abetz L, Ware JA.The CHQ User’s Manual. Boston, MA: The Health
Institute, New England Medical Center; 1996
15. Stein RE, Jessop DJ. Functional status II(R). A measure of child health status [published correction appears inMed Care. 1991;29(5):490–491].Med Care. 1990;28(11):1041–1055
16. Reich B, Heye K, Tuura R, et al. Neurodevelopmental outcome and health-related quality of life in children with single-ventricle heart disease before Fontan procedure.Semin Thorac Cardiovasc Surg. 2017;29(4):504–513
17. Visconti KJ, Rimmer D, Gauvreau K, et al. Regional low-flow perfusion versus circulatory arrest in neonates: one-year neurodevelopmental outcome. Ann Thorac Surg. 2006;82(6):
2207–2211–2213
18. Goldberg CS, Bove EL, Devaney EJ, et al. A randomized clinical trial of regional cerebral perfusion versus deep hypothermic circulatory arrest: outcomes for infants with functional single ventricle.J Thorac Cardiovasc Surg. 2007;133(4):880–887
19. Algra SO, Jansen NJ, van der Tweel I, et al. Neurological injury after neonatal cardiac surgery: a randomized, controlled trial of 2 perfusion techniques.Circulation. 2014;129(2): 224–233
DOI: 10.1542/peds.2019-1010 originally published online October 18, 2019;
2019;144;
Pediatrics
Jane W. Newburger and PHN INVESTIGATORS
Jeffrey P. Jacobs, James Cnota, Andrew M. Atz, Wyman W. Lai, David Bellinger,
Trachtenberg, Christian Pizarro, Victoria L. Pemberton, Alan B. Lewis, Jennifer S. Li,
Mahle, Thomas Miller, Kathleen A. Mussatto, Renee Sananes, Karen Uzark, Felicia
Caren S. Goldberg, Chenwei Hu, Cheryl Brosig, J. William Gaynor, William T.
Heart Syndrome
Behavior and Quality of Life at 6 Years for Children With Hypoplastic Left
Services
Updated Information &
http://pediatrics.aappublications.org/content/144/5/e20191010
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/144/5/e20191010#BIBL
This article cites 16 articles, 5 of which you can access for free at:
Subspecialty Collections
http://www.aappublications.org/cgi/collection/cardiac_surgery_sub
Cardiac Surgery
http://www.aappublications.org/cgi/collection/cardiology_sub
Cardiology
rning_disorders_sub
http://www.aappublications.org/cgi/collection/cognition:language:lea
Cognition/Language/Learning Disorders
al_issues_sub
http://www.aappublications.org/cgi/collection/development:behavior
Developmental/Behavioral Pediatrics following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.2019-1010 originally published online October 18, 2019;
2019;144;
Pediatrics
Jane W. Newburger and PHN INVESTIGATORS
Jeffrey P. Jacobs, James Cnota, Andrew M. Atz, Wyman W. Lai, David Bellinger,
Trachtenberg, Christian Pizarro, Victoria L. Pemberton, Alan B. Lewis, Jennifer S. Li,
Mahle, Thomas Miller, Kathleen A. Mussatto, Renee Sananes, Karen Uzark, Felicia
Caren S. Goldberg, Chenwei Hu, Cheryl Brosig, J. William Gaynor, William T.
Heart Syndrome
Behavior and Quality of Life at 6 Years for Children With Hypoplastic Left
http://pediatrics.aappublications.org/content/144/5/e20191010
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
http://pediatrics.aappublications.org/content/suppl/2019/10/17/peds.2019-1010.DCSupplemental
Data Supplement at:
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.