Effect of Neonatal Jaundice and Phototherapy on the
Frequency of First-Year Outpatient Visits
WHAT’S KNOWN ON THIS SUBJECT: Previous studies found that neonatal jaundice was associated with increased parental perceptions of infant vulnerability and significantly increased outpatient visit rates. It was not known whether these effects would be seen in a more recent cohort of infants.
WHAT THIS STUDY ADDS: Compared with infants who never had a bilirubin level⬎12 mg/dL, infants with bilirubin levels of 17.0 to 22.9 mg/dL averaged only 0.36 extra first-year visits when they did not receive phototherapy and 0.73 extra visits when they did.
abstract
OBJECTIVE:The objective of this study was to determine whether ei-ther hyperbilirubinemia or inpatient photoei-therapy is associated with increased subsequent outpatient visit rates, a possible effect of the “vulnerable child syndrome.”
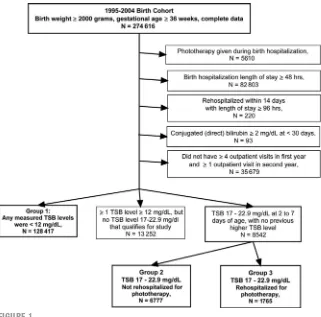
METHODS:We compared 3 groups of otherwise well term and late-preterm infants who were born between 1995 and 2004 in Northern California Kaiser hospitals: group 1 never had a documented total serum bilirubin (TSB) levelⱖ12 mg/dL (n⫽128 417); group 2 had a TSB levelⱖ17 and⬍23 mg/dL as outpatients between 48 hours and 7 days of age and did not receive inpatient phototherapy (n⫽6777); and group 3 met criteria for group 2 but did receive inpatient phototherapy (n⫽1765). We compared outpatient visit rates from 15 to 364 days of age adjusting for other predictors of visit rates by using Poisson and linear regression.
RESULTS:The mean total number of visits between 15 and 364 days was 9.83. Compared with group 1, adjusted total first-year visit rates were slightly increased in group 2 (adjusted incidence rate ratio: 1.04 [95% confidence interval: 1.02–1.05]) and group 3 (incidence rate ratio: 1.07 [95% confidence interval: 1.05–1.10]). The increases in visit rates were greatest for visits from 15 to 59 days of age, for specialty visits, and for unspecified diagnoses. These rates correspond to adjusted increases in total first-year visits (compared with group 1) of 0.36 visits in group 2 and 0.73 visits in group 3.
CONCLUSIONS:Neonatal jaundice and inpatient phototherapy are as-sociated with only small increases in first-year outpatient visit rates, consistent with mild or infrequent contribution to the vulnerable child syndrome in this population.Pediatrics2010;125:729–734
AUTHORS:Danielle Usatin, BA,aPetra Liljestrand, PhD,b,c
Michael W. Kuzniewicz, MD, MPH,c,dGabriel J. Escobar,
MD,c,eand Thomas B. Newman, MD, MPHb,c,d
aAlbert Einstein College of Medicine, Bronx, New York;
Departments ofbEpidemiology and Biostatistics anddPediatrics,
School of Medicine, University of California, San Francisco, San Francisco, California;cDivision of Research, Kaiser Permanente
Medical Care Program, Oakland, California; andeDepartment of
Pediatrics, Kaiser Permanente Medical Center, Walnut Creek, California
KEY WORDS
child health services/utilization, disease
susceptibility/psychology, jaundice, neonatal/therapy, mother-child relations, phototherapy/adverse effects
ABBREVIATIONS
TSB—total serum bilirubin ED— emergency department
KPMCP—Kaiser Permanente Medical Care Program ICD-9 —International Classification of Diseases, Ninth Revision
IRR—incidence rate ratio CI— confidence interval
This work was presented at the annual meeting of the Pediatric Academic Societies; May 5, 2008; Honolulu, HI.
www.pediatrics.org/cgi/doi/10.1542/peds.2009-0172 doi:10.1542/peds.2009-0172
Accepted for publication Nov 6, 2009
Address correspondence to Thomas B. Newman, MD, MPH, Department of Epidemiology and Biostatistics, UCSF Box 0560, San Francisco, CA 94143. E-mail: newman@epi.ucsf.edu PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275). Copyright © 2010 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE:The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
ter birth.1Although in most cases jaun-dice is harmless, the need to monitor bilirubin levels with repeated visits and blood draws and occasionally to readmit infants to the hospital for pho-totherapy may cause parental anxiety and adversely affect the parent–infant relationship.2,3 Mothers, including those with previous experience with neonatal jaundice, may feel at fault for having caused the jaundice, worry when total serum bilirubin (TSB) levels increase, and have difficulty bonding with their infants.4
Green and Solnit5first coined the term “vulnerable child syndrome” in 1964 to refer to a pattern of parental overpro-tection and excessive medical con-cerns that followed children’s re-covery from life-threatening illness. Subsequent work has found that chil-dren may be perceived as vulnerable after less serious illnesses or events, even as minor as a febrile illness that led to a negative lumbar puncture,6 sickle cell trait,6,7or a false-positive re-sult on newborn screening.8–10Indeed, Shonkoff,11commenting on Green and Solnit’s classic article 34 years later, wrote, “The most important contribu-tion of this report is the extent to which it underscores the critical importance of what physicians say (and don’t say) to parents. . . . Anything that a pediatri-cian conveys to a mother or father, whether it is thought through clearly or not, can have enormous impact on them and their children. Moreover, the effect may not only be immediate, but it often can be long-lasting.”
Previous studies have raised concern that neonatal jaundice may be a cause of the vulnerable child syndrome. Kemper et al2,3found that mothers of infants with jaundice (TSB ⱖ12 mg/dL) were less likely than mothers of control infants to leave their infants with another person and more likely to bring them for
well-health care resources by children who are perceived as vulnerable has been re-ported by others as well6,12–15and is 1 of the hallmarks of the vulnerable child syndrome.16
The studies of Kemper et al2,3included only 85 infants who had jaundice and were born in 1987 and 1988. Our ac-cess to an integrated health care deliv-ery system has allowed us to analyze data for a larger and more recent co-hort of infants who were born in a set-ting in which considerable variation in the use of phototherapy has been doc-umented.17Although this study based on electronically available data cannot assess parental perceptions of vulner-ability directly, our very large sample size allows us to quantify precisely and objectively 1 important manifestation of perceived vulnerability: increased use of outpatient services for sick- and well-child care. Thus, the main goal of this study was to determine, by using a more recent cohort, whether either neonatal hyperbilirubinemia or its treatment with inpatient phototherapy is associated with an increase in sub-sequent outpatient visit rates.
METHODS
The study was approved by the Kaiser Permanente Medical Care Program (KPMCP) and the University of Califor-nia, San Francisco, institutional review boards for the protection of human subjects. This was a retrospective co-hort study of children who were born in the Northern California KPMCP hos-pitals between 1995 and 2004. We ob-tained data from KPMCP demographic, laboratory, outpatient visit, and hospi-talization databases as described elsewhere.18–20
Patients
Eligible patients were infants with ges-tational age ⱖ36 weeks and birth
nursery stays, we excluded newborns who received phototherapy during their birth hospitalization, those with a birth hospitalization length of stay
⬎48 hours, or a conjugated or direct bilirubin levelⱖ2 mg/dL in the first 30 days after birth. Patients were eligible when they either never had a TSB level
ⱖ12 mg/dL or when they had a TSB levelⱖ17 and⬍23 mg/dL at 2 to 7 days (48 –168 hours) after birth. This range was selected to identify a range at which phototherapy might be discre-tionary; we therefore excluded infants who previously had a TSB level ⱖ23 mg/dL, because the vast majority would be expected to receive photo-therapy. To avoid including infants who might be perceived as vulnerable for other reasons or who might have had an unusually complicated treatment course for neonatal jaundice, we ex-cluded those who were rehospitalized for any reason with a length of stayⱖ96 hours within the first 14 days after birth. To restrict attention to infants who were likely to have been covered by the health plan for their first year, we included only patients with at least 4 outpatient visits in first year and at least 1 visit in the second year after birth.
Predictor Variables
infant for the study (dichotomized at 17.0 –19.9 and 20.0 –22.9 mg/dL).
Outcome Variables
Our principal outcome variables were the total numbers of various types of outpatient visits at the following ages (in days): 15 to 59, 60 to 119, 120 to 179, 180 to 364, and total (15 to 364). We did not consider visits at ⬍15 days be-cause visits for follow-up of jaundice would be expected during that period. We grouped the visits into ED, spe-cialty, well-child, and illness on the ba-sis of the department and the first 5 International Classification of Dis-eases, Ninth Revision(ICD-9) codes for the visit diagnoses by using the follow-ing classification hierarchy: (1) any visit to the ED was coded as ED regard-less of ICD-9 code; (2) all visits to de-partments coded neither as ED nor as pediatrics were categorized as spe-cialty visits; and (3) all pediatrics visits were classified as well-child or illness on the basis of ICD-9 codes. Well-child included those with ICD-9 codes V20.1 (routine child health examination), V20.2 (care of healthy child), V40.9 (mental behavioral problem), V65.3 (dietary surveillance and counseling), V65.43 (counseling for injury prevention), V65.49 (other specified counseling), V67.9 (follow-up examination), V68.9 (administrative encounter), or V70.9 (general medical examination). The ill-ness category included all pediatrics visits that were not coded as well-child visits as defined.
Data Analysis
We compared demographic and clini-cal characteristics of infants in the 3 study groups by using t tests, rank sum, or 2 test as appropriate. To quantify the effects of jaundice and phototherapy on outpatient visit rates, we used Poisson regression. We exam-ined rates for the 5 types of outpatient visits in the 4 age groups, controlling for the potential confounders listed
al-ready and accounting for clustering of visits by infant. Poisson regression yields an adjusted incidence rate ratio (IRR), which is the ratio of the esti-mated underlying probability of a visit during a short period in 1 group com-pared with another, adjusting for con-founding variables. For comparisons of visit types associated with the 8 most common outpatient diagnoses, we calculated the adjusted effects of study groups and correspondingP val-ues by using multiple linear regres-sion models that included the same confounding variables listed already.
We did not adjust for multiple compar-isons,21butPvalues and confidence in-tervals should be interpreted with awareness that we compared 5 visit types and 4 time periods and 8 differ-ent diagnoses in 3 groups of patidiffer-ents. All statistical analyses were per-formed by using Stata 9.2 (Stata Corp, College Station, TX).
RESULTS
Figure 1 shows how the 3 study groups were extracted from the KPMCP birth cohort. Table 1 compares the demo-graphic characteristics of the 128 417 infants who never had a TSB levelⱖ12 mg/dL (group 1), the 6777 infants who had TSB levels of 17.0 to 22.9 mg/dL and were not rehospitalized for photo-therapy (group 2), and the 1765 infants who were reshospitalized (group 3). Groups 2 and 3 had slightly lower birth weight and gestational age, a higher proportion of Asian infants, and older mothers than group 1, with the differ-ences greater in group 3 than in group 2, consistent with their significantly higher maximum TSB levels. The aver-age total number of outpatient visits from 15 to 364 days was 9.83 ⫾4.90 (mean ⫾ SD; Table 2); however, the number of outpatient visits varied widely within each visit type and age bracket. For example, for the ED visit FIGURE 1
Definition of the study groups.
type, the mean was typically close to 0 (eg, the mean for the 15- to 59-day age range was 0.03 visits) but with an SD much larger than the mean (⫾0.19), indicating that the distribution of num-bers of ED visits were skewed to the right.
We found a small increase in total out-patient visit rates in group 2 compared with group 1 (overall adjusted IRR for days 15–364: 1.04 [95% CI: 1.02–1.05]). There was a slightly smaller additional increase with rehospitalization for phototherapy (adjusted IRR for group 3 versus group 2: 1.03 [95% CI: 1.01– 1.06]). This corresponds to adjusted in-creases in total first-year visits, when compared with group 1, of 0.36 visits in group 2 and 0.73 visits in group 3. Both increases in rates were greatest be-tween 15 and 59 days after birth; the additional effect of phototherapy in in-fants with jaundice (ie, comparison of group 3 and group 2) was not
statisti-cally significant in any of the other in-dividual periods.
The visit type that was associated with the largest increase in visit rates was specialty visits (Table 3), with the ef-fect apparently attributable to jaun-dice itself (group 2 versus group 1 IRR: 1.17 [95% CI: 1.08 –1.97]), with little or
[95% CI: 0.87–1.19]; Table 3). The in-crease in specialty visits in group 2 versus group 1 was statistically signif-icant and of similar magnitude in each of the 4 periods (IRR range: 1.14 –1.20). (Full cross-tabulations of adjusted IRRs by visit type and age group are available from the authors.) In models that examined the effect of photother-apy in the infants with jaundice (ie, comparing group 3 with group 2), there was no significant difference in any of the outcomes when the TSB level that qualified the infant for the study was 20.0 to 22.9 vs 17.0 to 19.9 mg/dL.
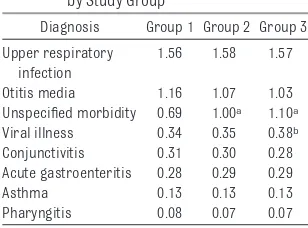
The average number of outpatient vis-its for most of the 8 most common sick-visit diagnosis codes did not vary by phototherapy use (Table 4). Only 1 diagnosis code, that for “unspecified morbidity,” had a difference of at least 0.1 visits in the first year between group 1 and groups 2 and 3; this is the code given when the physician writes text rather than checks a box on the encounter form. There was a statisti-cally significant increase in visits for “viral illness” in the phototherapy group compared with the group without jaundice, but the magnitude of the differ-ence was small (adjusted differdiffer-ence: 0.048 visits [95% CI: 0.016 – 0.079]).
(n⫽128 417) (n⫽6777) (n⫽1765)
Male,n(%) 62 573 (49) 3878 (57) 985 (56) .290
Race,n(%) .030
White 61 700 (48) 2667 (39) 690 (39) Asian 20 080 (16) 1963 (29) 569 (32) Hispanic 29 060 (23) 1517 (22) 353 (20) Black 9791 (8) 210 (3) 63 (4) Other 5039 (4) 269 (4) 59 (3) Missing 2747 (2) 161 (2) 31 (2)
Year of birth, % .180
1995–1999 53 49 47
2000–2004 47 51 53
Gestational age, mean⫾SD, wk 39.44⫾1.17 38.78⫾1.30 38.52⫾1.37 ⬍.001 Birth weight, mean⫾SD, kg 3.49⫾0.46 3.40⫾0.46 3.37⫾0.48 .003 Mother’s age at child’s birth, mean⫾SD, y 28.76⫾5.82 29.16⫾5.75 29.41⫾5.56 .013 Maximum TSB level, mean⫾SD, mg/dL 18.93⫾1.46 21.32⫾1.92 ⬍.001
Group 1: no bilirubin levelⱖ12 mg/dL; group 2: bilirubin 17.0 to 22.9 at 48 to 168 hours and no inpatient phototherapy; group 3: bilirubin 17.0 to 22.9 at 48 to 168 hours, received inpatient phototherapy.Pvalues for categorical variables based on2
tests; means compared with analysis of variance.
TABLE 2 Use of Outpatient Care in Entire Study Population No. of Visits,
Mean⫾SD
Age, d
15–59 60–119 120–179 180–364 Total Well-child 1.04⫾0.78 0.94⫾0.61 0.90⫾0.57 1.83⫾0.91 4.71⫾1.47 Illness 0.54⫾0.88 0.58⫾0.97 0.70⫾1.07 2.60⫾2.61 4.43⫾3.87 Specialty 0.06⫾0.37 0.07⫾0.41 0.08⫾0.40 0.26⫾0.97 0.47⫾1.65 ED 0.03⫾0.19 0.03⫾0.19 0.03⫾0.19 0.13⫾0.40 0.23⫾0.56 Total 1.67⫾1.26 1.62⫾1.28 1.71⫾1.34 4.82⫾3.23 9.83⫾4.90
TABLE 3 Adjusted IRR (95% CI) for Comparisons Between Groups
Parameter Group 2 Versus Group 1 Group 3 Versus Group 2 Group 3 Versus Group 1 Age group, d
15–59 1.05 (1.04–1.08) 1.07 (1.03–1.12) 1.14 (1.10–1.18) 60–119 1.02 (1.00–1.04) 1.03 (0.99–1.08) 1.06 (1.02–1.10) 120–179 1.02 (1.00–1.04) 1.02 (0.98–1.07) 1.04 (1.00–1.08) 180–364 1.04 (1.03–1.06) 1.02 (0.99–1.06) 1.07 (1.04–1.10) Visit type
Well-child 1.01 (1.01–1.02) 1.02 (1.01–1.04) 1.04 (1.03–1.06) Illness 1.05 (1.03–1.07) 1.04 (0.98–1.09) 1.10 (1.05–1.14) Specialist 1.17 (1.08–1.27) 1.02 (0.87–1.19) 1.20 (1.05–1.38) ED 1.00 (0.94–1.06) 1.08 (0.93–1.24) 1.07 (0.95–1.21) Total of all types of visits,
15–364 d
1.04 (1.02–1.05) 1.03 (1.01–1.06) 1.07 (1.05–1.10)
DISCUSSION
We observed only a small increase in first-year outpatient visit rates in infants with hyperbilirubinemia, with the in-crease only slightly larger in those who received phototherapy than in those who did not. The increase in visit rates was greatest from 15 to 59 days of age, and specialty and illness visit rates were in-creased more than well-child or ED visit rates. A strength of this study is the large sample size, permitting narrow CIs around estimates of these small effects.
The study also has potential limita-tions. First, other factors that are as-sociated with either jaundice or photo-therapy might also be associated with subsequent outpatient use. The most important predictor of jaundice that we could not include in our models is breastfeeding. Breastfeeding provides protection against infectious diseases and therefore might be expected to at-tenuate any positive association be-tween jaundice and subsequent visit rates. Thus, if infants with jaundice were more likely to be breastfed and if jaundice led to discontinuation of breastfeeding (as it often did in the study by Kemper et al2), then the bene-ficial effect of breastfeeding on visit rates would be diminished or even re-versed in infants with jaundice. The comparison between infants who had jaundice and did and did not get pho-totherapy could be similarly affected if
phototherapy (more than just jaun-dice) led to discontinuation of breast-feeding. In addition, that comparison could be confounded by parental anxi-ety. For example, if newborns of anx-ious parents were more likely to re-ceive phototherapy at a given bilirubin level and gestational age, then there could be a subsequent increase in out-patient visits as a result of this parental anxiety, rather than of a causal effect of phototherapy itself; however, given the small magnitude of the differences that we observed, it seems unlikely that sig-nificant confounding by either breast-feeding or parental anxiety occurred.
Second, we studied infants who re-mained in the KPMCP for at least 1 year after birth. It is possible that some of the patients who left the system expe-rienced different perceptions of vul-nerability than those who remained in the health plan. Third, the particular visit type that was associated with the highest IRR, specialty visits, was the type of visit that we a priori believed was least likely to be affected by the vulnerable child syndrome. In the study by Kemper et al,2 infants with jaundice had an excess of well-child visits, sick visits, and ED visits; spe-cialty visits were not mentioned. Be-cause specialty visits often involve a referral from the primary care pro-vider, they seem less likely to be af-fected by parental anxiety. Because we excluded infants with high conjugated bilirubin levels and the increase in spe-cialty visits was not greater in the low-est age groups, it seems unlikely that a significant number of these specialty visits were directly related to jaundice. It seems more likely that they may have been related to physician anxiety or practice style (ie, physicians with a lower threshold for admission for pho-totherapy may have a lower threshold for subspecialty referral as well).
Finally, although the use of electronic data allowed a large sample size, it did
not allow us to address directly the vul-nerable child syndrome but rather just 1 manifestation of it: increased tient use. The small increase in outpa-tient visits that we observed does not rule out the presence of parental fear and vulnerable child syndrome se-quelae in the parent– child relation-ship at home. For example, other as-pects of the vulnerable child syndrome found by Kemper et al, such as reluc-tance to leave the child with a baby-sitter, were not examined in this study and might be greater in magnitude.
Although statistically significant, the differences that we observed in this study were much smaller than those reported by Kemper et al.2At 1 month of age, infants with jaundice in that study had risk ratios of 4.1 for⬎2 well-child visits, 3.1 for⬎1 sick visit, and 8 for any ED visit. Risk ratios for exces-sive well-child and sick visits and any ED visits had declined to 1.2, 1.3, and 2.4, respectively, by 6 months in that study, with only the last still statisti-cally significant,3but were still much higher than the rate ratios observed in this study. One reason for this may be that as a result of previous studies highlighting concern about the vulner-able child syndrome (cited in the American Academy of Pediatrics 1994 guideline1), clinicians who cared for the newborns in this study were sensi-tive to that possibility and were able to explain the importance of follow-up and/or phototherapy for jaundice while at the same time providing reassurance about the lack of any late sequelae.22
Despite the limitations of our study, our data will help to guide physicians in the future when making decisions about phototherapy. Although clini-cians should remain sensitive to the possibility of the vulnerable child syn-drome to avoid overly alarming par-ents of infants with jaundice, the small effect size and narrow CIs in this study suggest that concern about the
devel-TABLE 4 Mean Numbers of Visits Between 15 and 364 Days With the 8 Most Commonly Coded Illness Diagnoses, by Study Group
Diagnosis Group 1 Group 2 Group 3 Upper respiratory
infection
1.56 1.58 1.57 Otitis media 1.16 1.07 1.03 Unspecified morbidity 0.69 1.00a 1.10a
Viral illness 0.34 0.35 0.38b
Conjunctivitis 0.31 0.30 0.28 Acute gastroenteritis 0.28 0.29 0.29 Asthma 0.13 0.13 0.13 Pharyngitis 0.08 0.07 0.07
aP⬍.001 versus group 1. bP⫽.003 versus group 1.
or use of phototherapy for infants with jaundiced when it is indicated.
RO1 HD047557-01A1 from the Eunice Kennedy Shriver National Institute of
grant from the Glaser Pediatric Re-search Network.
REFERENCES
1. Practice parameter: management of hyper-bilirubinemia in the healthy term newborn. American Academy of Pediatrics. Provi-sional Committee for Quality Improvement and Subcommittee on Hyperbilirubinemia [published correction appears in Pediat-rics. 1995;95(3):458 – 461].Pediatrics.1994; 94(4 pt 1):558 – 665
2. Kemper K, Forsyth B, McCarthy P. Jaundice, terminating breast-feeding, and the vulner-able child.Pediatrics.1989;84(5):773–778 3. Kemper KJ, Forsyth BW, McCarthy PL.
Per-sistent perceptions of vulnerability follow-ing neonatal jaundice.Am J Dis Child.1990; 144(2):238 –241
4. Hannon PR, Willis SK, Scrimshaw SC. Persis-tence of maternal concerns surrounding neonatal jaundice: an exploratory study.
Arch Pediatr Adolesc Med.2001;155(12): 1357–1363
5. Green M, Solnit A. Reactions to the threat-ened loss of a child: a vulnerable child syndrome—pediatric management of the dying child, part III.Pediatrics.1964;34: 58 – 66
6. Levy JC. Vulnerable children: parents’ per-spectives and the use of medical care. Pe-diatrics.1980;65(5):956 –963
7. Hampton ML. Sickle cell “nondisease”: a po-tentially serious public health problem.
Am J Dis Child.1974;128(1):58 – 61 8. Tymstra T. False positive results in
screen-ing tests: experiences of parents of chil-dren screened for congenital hypothyroid-ism.Fam Pract.1986;3(2):92–96
9. Fyro¨ K, Bodegard G. Four-year follow-up of psychological reactions to false positive screening tests for congenital hypothyroid-ism. Acta Paediatr Scand. 1987;76(1): 107–114
10. Gurian EA, Kinnamon DD, Henry JJ, Wais-bren SE. Expanded newborn screening for biochemical disorders: the effect of a false-positive result. Pediatrics.2006;117(6): 1915–1921
11. Shonkoff CJ. Reactions to the threatened loss of a child: a vulnerable child syndrome, by Morris Green, MD, and Albert A. Solnit, MD, Pediatrics, 1964;34:58 – 66.Pediatrics.
1998;102(1 pt 2):239 –241
12. Forsyth BW, Horwitz SM, Leventhal JM, Burger J, Leaf PJ. The child vulnerability scale: an instrument to measure parental perceptions of child vulnerability.J Pediatr Psychol.1996;21(1):89 –101
13. Forsyth BW, Canny PF. Perceptions of vul-nerability 3 1/2 years after problems of feeding and crying behavior in early in-fancy.Pediatrics.1991;88(4):757–763 14. Spurrier NJ, Sawyer MG, Staugas R, Martin
AJ, Kennedy D, Streiner DL. Association be-tween parental perception of children’s vul-nerability to illness and management of children’s asthma.Pediatr Pulmonol.2000; 29(2):88 –93
15. Thomasgard M, Metz WP. Differences in health care utilization between parents who perceive their child as vulnerable versus overprotective parents.Clin Pediatr (Phila).
1996;35(6):303–308
16. Kokotos F. The vulnerable child syndrome.
Pediatr Rev.2009;30(5):193–194
17. Atkinson L, Escobar G, Takayama J, New-man T. Phototherapy use in jaundiced newborns in a large managed care organization: do physicians adhere to the guideline?Pediatrics.2003;111(5). Avail-able at: www.pediatrics.org/cgi/content/ full/111/5/e555
18. Newman TB, Escobar GJ, Gonzales V, Arm-strong MA, Gardner M, Folck B. Frequency of neonatal bilirubin testing and hyperbiliru-binemia in a large health maintenance or-ganization [published correction appears in Pediatrics. 2001;1(2):126].Pediatrics.
1999;104(5 pt 2):1198 –1203
19. Newman TB, Liljestrand P, Escobar GJ. Com-bining clinical risk factors with serum bili-rubin levels to predict hyperbilibili-rubinemia in newborns.Arch Pediatr Adolesc Med.
2005;159(2):113–119
20. Newman TB, Kuzniewicz MW, Liljestrand P, Wi S, McCulloch C, Escobar GJ. Numbers needed to treat with phototherapy according to Amer-ican Academy of Pediatrics guidelines. Pediat-rics.2009;123(5):1352–1359
21. Newman TB, Kohn MA.Evidence-based Diag-nosis. New York, NY: Cambridge University Press; 2009:220 –238
DOI: 10.1542/peds.2009-0172 originally published online March 15, 2010;
2010;125;729
Pediatrics
Thomas B. Newman
Danielle Usatin, Petra Liljestrand, Michael W. Kuzniewicz, Gabriel J. Escobar and
Outpatient Visits
Effect of Neonatal Jaundice and Phototherapy on the Frequency of First-Year
Services
Updated Information &
http://pediatrics.aappublications.org/content/125/4/729 including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/125/4/729#BIBL This article cites 20 articles, 8 of which you can access for free at:
Subspecialty Collections
b
http://www.aappublications.org/cgi/collection/hyperbilirubinemia_su
Hyperbilirubinemia
sub
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_
Fetus/Newborn Infant
vices_sub
http://www.aappublications.org/cgi/collection/community_health_ser
Community Health Services
_sub
http://www.aappublications.org/cgi/collection/community_pediatrics
Community Pediatrics
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
DOI: 10.1542/peds.2009-0172 originally published online March 15, 2010;
2010;125;729
Pediatrics
Thomas B. Newman
Danielle Usatin, Petra Liljestrand, Michael W. Kuzniewicz, Gabriel J. Escobar and
http://pediatrics.aappublications.org/content/125/4/729
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.