To Tap or Not to Tap: High Likelihood of Meningitis Without Sepsis
Among Very Low Birth Weight Infants
Barbara J. Stoll, MD*; Nellie Hansen, MPH‡; Avroy A. Fanaroff, MD§; Linda L. Wright, MD㛳; Waldemar A. Carlo, MD¶; Richard A. Ehrenkranz, MD#; James A. Lemons, MD**;
Edward F. Donovan, MD‡‡; Ann R. Stark, MD§§; Jon E. Tyson, MD, MPH㛳㛳; William Oh, MD¶¶; Charles R. Bauer, MD##; Sheldon B. Korones, MD***; Seetha Shankaran, MD‡‡‡;
Abbot R. Laptook, MD§§§; David K. Stevenson, MD㛳㛳㛳; Lu-Ann Papile, MD¶¶¶; and W. Kenneth Poole, PhD‡
ABSTRACT. Context. Neonatal meningitis is associ-ated with significant morbidity and mortality. We spec-ulated that meningitis may be underdiagnosed among very low birth weight (VLBW) infants because of the failure to perform lumbar punctures (LPs) in infants with suspected sepsis.
Objective. This study was undertaken to review the epidemiology of late-onset meningitis in VLBW (401– 1500 g) infants and to evaluate the concordance of cere-brospinal fluid (CSF) and blood culture (BC) results.
Methods. VLBW infants (excluding those with intra-ventricular shunts) born at centers of the National Insti-tute of Child Health and Human Development Neonatal Research Network from September 1, 1998, through De-cember 31, 2001, were studied. Late-onset meningitis was defined by culture-based criteria and classified as men-ingitis with or without associated sepsis. Unadjusted comparisons were made using2tests and adjusted com-parisons using regression models.
Results. Of 9641 VLBW infants who survived >3 days, 2877 (30%) had>1 LPs, and 6056 (63%) had>1 BC performed after day 3. One hundred thirty-four infants had late-onset meningitis (1.4% of all patients; 5% of those with an LP). Pathogens associated with meningitis were similar to those associated with sepsis. One third
(45 of 134) of the infants with meningitis had negative BCs. Lower gestational age and prior sepsis increased risk for meningitis. Compared with uninfected infants, those with meningitis had a longer time on mechanical ventilation (28 vs 18 days), had longer hospitalizations (91 vs 79 days), were more likely to have seizures (25% vs 2%), and were more likely to die (23% vs 2%).
Conclusions. Meningitis is a serious complication among VLBW infants, associated with increased severity of illness and risk of death. Of note, one third of the infants with meningitis had meningitis in the absence of sepsis. Because CSF cultures were performed only half as often as BCs, this discordance in blood and CSF culture results suggests that meningitis may be under-diagnosed among VLBW infants. Pediatrics 2004;113: 1181–1186;meningitis, sepsis, lumbar puncture, very low birth weight infants.
ABBREVIATIONS. LP, lumbar puncture; VLBW, very low birth weight; LOM, late-onset meningitis; NICHD, National Institute of Child Health and Human Development; BC, blood culture; CSF, cerebrospinal fluid; CONS, coagulase-negative staphylococcus; GA, gestational age; IVH, intraventricular hemorrhage; PVL, periventricular leukomalacia; NEC, necrotizing enterocolitis; OR, odds ratio; CI, confidence interval.
N
eonatal meningitis is an uncommon but se-rious disorder with high rates of morbidity and mortality.1–5The importance of a lumbarpuncture (LP) as part of the diagnostic evaluation of the neonate with suspected sepsis has been the sub-ject of debate, and clinical practice varies.5–10
Neona-tologists often defer the LP when evaluating the very low birth weight (VLBW) infant. Reasons stated in-clude the perceived low risk of meningitis versus the risk of the procedure in the often unstable VLBW patient. This study was undertaken to review the epidemiology of late-onset meningitis (LOM) in VLBW infants (401–1500 g) cared for at the centers of the National Institute of Child Health and Human Development (NICHD) Neonatal Research Network and to evaluate the concordance of blood cultures (BCs) and cerebrospinal fluid (CSF) cultures.
We suspected that there would be center differ-ences in the frequency with which an LP was per-formed and speculated that meningitis may be un-derdiagnosed in VLBW infants because of the failure
From the *Department of Pediatrics, Emory University School of Medicine, Atlanta, Georgia; ‡Research Triangle Institute, Research Triangle Park, North Carolina; §Department of Pediatrics, Case Western Reserve Univer-sity, Cleveland, Ohio;㛳National Institute of Child Health and Human Development, Bethesda, Maryland; ¶Department of Pediatrics, University of Alabama, Birmingham, Alabama; #Department of Pediatrics, Yale Uni-versity School of Medicine, New Haven, Connecticut; **Department of Pediatrics, Indiana University School of Medicine, Indianapolis, Indiana; ‡‡Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, Ohio; §§Joint Program in Neonatology, Harvard University, Children’s Hospital Boston, Boston, Massachusetts;㛳㛳Center for Clinical Research and Evidence Based Medicine, University of Texas Health Science Center at Houston Medical School, Houston, Texas; ¶¶Department of Pe-diatrics, Brown University, Providence, Rhode Island; ##Department of Pediatrics, University of Miami, Miami, Florida; ***The Newborn Center, University of Tennessee, Memphis, Tennessee; ‡‡‡Division of Neonatal and Perinatal Medicine, Wayne State University, Detroit, Michigan; §§§Depart-ment of Pediatrics, University of Texas Southwestern Medical Center, Dal-las, Texas;㛳㛳㛳Division of Neonatology, Stanford University Medical Center, Palo Alto, California; ¶¶¶Department of Pediatrics, University of New Mexico School of Medicine, Albuquerque, New Mexico.
Received for publication Jul 24, 2003; accepted Oct 1, 2003.
Address correspondence to Barbara J. Stoll, MD, Department of Pediatrics, Emory University School of Medicine, 2040 Ridgewood Dr, NE, Atlanta, GA 30322
to routinely perform LPs in VLBW infants with sus-pected sepsis.
METHODS Population Database
The NICHD Neonatal Research Network is a consortium of tertiary neonatal centers. The network maintains a registry of all VLBW infants born and/or admitted to participating centers within 14 days of birth. Trained research nurses collect maternal data soon after birth and infant data until 120 days, discharge, or death.11The registry includes data on late-onset sepsis and men-ingitis, infecting organisms, maternal demographics, pregnancy, labor and delivery complications, infant characteristics, morbidi-ties, and final status. In September 1998, infection surveillance was expanded to include results of all BCs and CSF cultures, antibiotic therapy, and selected risk factors for infection. For this study, we excluded infants with intraventricular shunts and CSF cultures obtained from daily LPs or indwelling reservoirs that were per-formed only to treat posthemorrhagic hydrocephalus.
LOM was defined by a CSF culture positive for bacteria or fungi performed after 72 hours of age. Data on other CSF param-eters (cells, glucose, protein, and Gram stain) were not collected. CSF cultures positive for organisms generally considered to be contaminants were considered negative for this analysis. BCs taken within 7 days of each positive CSF culture were reviewed to classify meningitis further as: 1) meningitis without sepsis (2 positive CSF cultures for the same organism [within a week of each other] or a single positive CSF culture for an organism other than coagulase-negative staphylococcus [CONS] and BC negative for that organism); 2) meningitis with sepsis (CSF and BC positive for the same organism [included some cases in which the CSF was positive for 2 organisms and BC positive for at least 1 of the organisms]); or 3) probable contaminant (CONS in a single CSF culture and BC negative for CONS; a single CSF culture positive for multiple organisms and associated BC negative; or a single positive CSF culture thought to be a contaminant by the study site [ie, not treated]). All cases of meningitis (excluding probable con-taminants) were used to evaluate risk factors, infecting pathogens, and outcome.
Gestational age (GA), intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), and necrotizing enterocolitis (NEC) were assessed as described in previous network publica-tions.11,12The participating centers and the numbers of patients that each contributed to the study are listed in the Appendix 1.
Laboratory Methods
BCs and CSF cultures were processed by the clinical microbi-ology laboratories at each academic center using standard meth-ods. BCs were processed using either the Bactec (Becton Dickin-son, Sparks, MD) or BacT/Alert (Organon Teknika, Durham, NC) systems; 0.5 to 1 mL of blood was inoculated per BC.
Statistical Methods
A binary variable was created to indicate infants who were and were not evaluated by CSF culture after day 3 of life, and statistical significance for comparisons of this variable across groups was determined by the2test. Most analyses focused on the subset of patients who were evaluated by CSF culture. LOM was treated as a binary variable. Statistical significance for unadjusted compari-sons (eg, the variation in incidence of meningitis across study centers) was determined by using the2test. Possible risk factors for meningitis were evaluated in logistic regression models fit to the binary outcome, and statistical significance of covariates was determined by Wald 2 tests. Characteristics included in the model were study center, GA, birth weight, race, sex, prior IVH grade 3 or 4, PVL, and prior sepsis. Infants with meningitis were considered to have prior IVH or prior sepsis if the diagnosis date was on or before the date of the positive CSF culture. Logistic regression models were used also to evaluate the relationship between meningitis (and other infection groups) and risk of sei-zures and death after adjusting for study center and GA. Mean days on mechanical ventilation, time to attain full feeds, and length of hospital stay were compared among infection groups using linear regression models, which included study center and GA in addition to the infection group.Pvalues⬍.05 were
con-sidered significant. Analyses were completed by using SAS soft-ware (SAS Institute, Cary, NC).13
RESULTS
Populations Studied and Incidence of Meningitis Between September 1, 1998, and December 31, 2001, 11 028 VLBW infants were born and/or cared for at network centers, and 9828 infants survived at least 72 hours. After excluding 187 infants with shunts (2%), 9641 were included in the analyses. Although 6056 of the 9641 infants (63%) had at least 1 BC performed after day 3 of life, only 2877 (30%) infants had an LP performed. Almost all infants who had an LP (98%) had an associated BC. The average age at the time of the first LP was 22 days (median: 16 days; range: 4 –120 days).
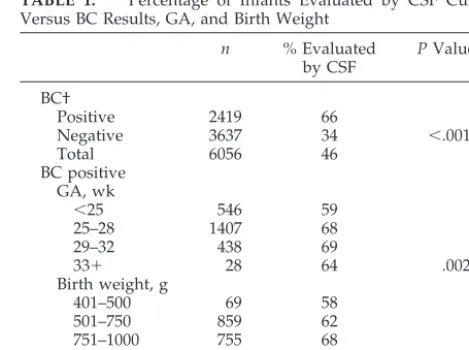
Among infants with a BC, the percentage that also had at least 1 CSF culture after day 3 varied signifi-cantly by clinical center, ranging from 22% to 85% (P ⬍ .001). Infants with a positive BC were signifi-cantly more likely than those with negative BCs to have an LP. Among those who had a positive BC after day 3, infantsⱖ25 weeks old and⬎750 g were most likely to have an LP performed (Table 1). In-fants with seizures were more likely to have an LP performed; 54% of those with seizures had an LP, compared with 29% of those without seizures (P⬍
.001).
Two hundred twenty-eight infants had a positive CSF culture after day 3; 94 infants whose results were considered probable contaminants were not counted as having meningitis. These 94 infants had 96 CSF cultures: 85 positive for CONS/negative BC; 2 posi-tive for bacillus; 1 posiposi-tive for aspergillus; and 8 positive for multiple organisms. Thus, using strict criteria, 134 infants had meningitis. This represents 1.4% of all infants (134 of 9641) and 5% of patients evaluated with a CSF culture after day 3 (134 of 2877).
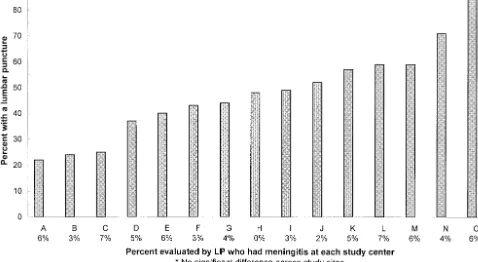
No significant differences were found in the per-centage of infants with meningitis by clinical center in the subgroup of infants evaluated with a CSF culture (Fig 1). Infants with a positive BC were
sig-TABLE 1. Percentage of Infants Evaluated by CSF Culture
Versus BC Results, GA, and Birth Weight
n % Evaluated by CSF
PValue*
BC†
Positive 2419 66
Negative 3637 34 ⬍.001
Total 6056 46
BC positive GA, wk
⬍25 546 59
25–28 1407 68
29–32 438 69
33⫹ 28 64 .002
Birth weight, g
401–500 69 58
501–750 859 62
751–1000 755 68
1001–1250 477 68
1251–1500 259 70 .02
* By the2square test.
nificantly more likely to have meningitis than those with a negative BC (7.2% vs 1.5%;P ⬍.001).
The majority of infants had 1 episode of meningitis (only 7 of 134 [5%] had 2 episodes). The average age for the first episode was 26 days (median: 19 days; range: 4 –102 days). Sixty-seven percent of the infants (90 of 134) had a repeat LP performed. Of the 44 patients without a follow-up LP, 11 (25%) died within 6 days of their initial culture. For most pa-tients (70 of 90 [78%]), the follow-up LP was per-formed within 10 days of the original LP. Of the repeat LPs, 11 of 90 (12%) were positive. The same organism grew on the original and repeat cultures for 10 of these patients despite treatment with pre-sumably appropriate antimicrobial agents in 9 cases. One patient withCandida albicansmeningitis on both the original and repeat culture was not begun on anti-fungal therapy until after the second positive culture.
One third of those with meningitis (45 of 134) had a positive CSF culture without an associated positive BC, and two thirds (89 of 134) had meningitis with
sepsis (Table 2). Of note, none of the 45 patients with meningitis/no sepsis had an earlier episode of sepsis with the organism causing meningitis. Because CONS may be a contaminant, if we exclude cases with CONS in the CSF, the percentage of infants who had meningitis without sepsis is even greater (47% vs 34%). For the vast majority of infants, the BC and LP were closely linked. For 87 of the 134 (65%) in-fants with meningitis, the positive CSF culture was taken on the same day as the associated BC; for 37 patients (28%), the LP was performed 1 to 3 days after the BC. Among these 124 infants with menin-gitis and closely linked BCs and CSF cultures, the percentages with and without sepsis were similar to those overall: 83 with sepsis (67%) vs 41 without sepsis (33%).
Pathogen Distribution
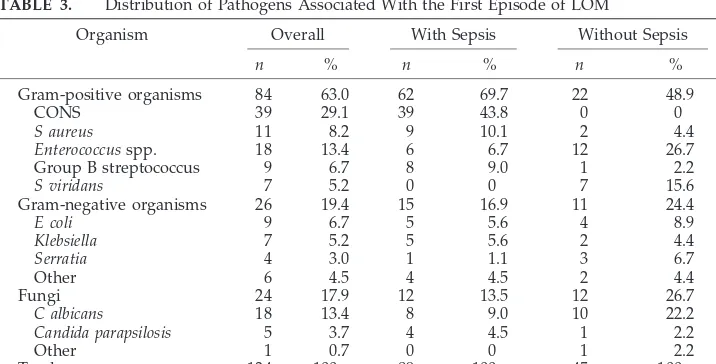
Gram-positive agents were the most frequent or-ganisms (63% of first episodes), with CONS account-ing for 29% of first episodes. Gram-negative
patho-Fig. 1. Percentage of infants by center evaluated by BC who also had an LP, and percentage with meningitis among those with an LP.
TABLE 2. Rates of LOM Determined by CSF Cultures Including and Excluding Patients With
CONS in the CSF
n Rates/1000 Patients 401–1500 g Studied
(n⫽9641)
Rates/1000 Patients 401–1500 g with
LP Performed (n⫽2877)
Meningitis (all patients) 134 14 47
Meningitis/sepsis 89 (66%) 9 31
Meningitis/no sepsis 45 (34%) 5 16
Meningitis (minus CONS in CSF) 96 10 33*
Meningitis/sepsis 51 (53%) 5 18
Meningitis/no sepsis 45 (47%) 5 16
gens accounted for 19% and fungal agents for 18% of cases (Table 3). Among 89 patients with meningitis/ sepsis, CONS (44%),Staphylococcus aureus(10%), and group B streptococci (9%) were the most common Gram-positive agents.Escherichia coli(6%) and Kleb-siella (6%) were the most frequent Gram-negative organisms, andC albicans(9%) was the most frequent fungal agent. Among the 45 infants with meningitis alone, Enterococcus species (27%), C albicans (22%), and Streptococcus viridans (16%) were the most fre-quent organisms.
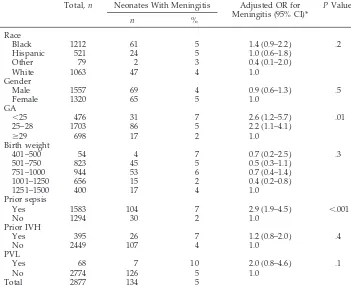
Risk Factors for Meningitis
Selected neonatal characteristics and the risk of meningitis among infants evaluated by LP are pre-sented in Table 4. No association was found between meningitis and an infant’s race, sex, birth weight, prior IVH, or PVL. However, lower GA was associ-ated with greater risk of meningitis, as was prior sepsis (7% vs 2%; odds ratio [OR]: 2.9; 95% confi-dence interval [CI]: 1.9 – 4.5;P⬍.001).
Hospital Course/Outcome
For the purpose of evaluating hospital outcomes, infants who had an LP performed were classified into the following groups: 1) LOM (n ⫽ 134); 2) culture-confirmed sepsis but no meningitis and no NEC (n ⫽ 1263); 3) NEC with or without culture-positive sepsis and no meningitis (n ⫽ 329); 4) cul-ture-negative clinical infection alone (n ⫽ 637); and 5) uninfected (no meningitis, no culture-positive or clinical sepsis, and no NEC [n⫽514]). Seizures were significantly more common in infants with LOM (25%) than in infants with sepsis alone (9%) or who were uninfected (2%) (P ⬍ .001). Adjusting for GA and study center, infants with meningitis were nearly 15 times more likely to have seizures (OR: 14.8; 95% CI: 6.5–33.8) than infants who were unin-fected. Compared with those who were uninfected, infants with meningitis spent more time on mechan-ical ventilation (28 ⫾ 1.9 vs 18 ⫾ 1.0 days), took longer to attain full feeds (31⫾1.5 vs 21⫾1.8 days), and had longer hospital stays (91⫾ 3.9 vs 79⫾ 2.1 days) (each:P⬍ .001).
Although “too sick to tap” and “risk of
complica-tions” are cited often as reasons to defer the LP, we found no difference in the risk of death between infants who did and did not have an LP (284 of 2877 [10%] vs 661 of 6764 [10%]). However, meningitis increased the risk of death substantially. Overall, 23% (31 of 134) of infants with meningitis died, com-pared with 9% (253 of 2743) of those who had an LP performed but did not have meningitis (P ⬍ .001). This relationship remained after adjustment for GA and study center (OR for death/meningitis versus no meningitis: 2.4; 95% CI: 1.6-3.8;P⬍ .001). The likeli-hood of death was increased in all 4 groups of in-fected patients (Table 5). The proportion of infants with meningitis who died was significantly higher for infants infected with Gram-negative (41%) and fungal (32%) agents than for those with gram-posi-tive (15%) (P ⫽ .01) agents. Three of the 31 infants with meningitis who died (10%) did so on the day of the CSF culture, 6 (19%) between 1 and 3 days, 5 (16%) between 4 and 7 days, and 17 (55%)⬎7 days after the diagnosis of meningitis.
DISCUSSION
Among VLBW infants, meningitis is associated with acute complications, increased risk of death, and late neurodevelopmental sequelae among survi-vors.14,15 This study reviews the epidemiology of
LOM in VLBW infants cared for at the centers of the NICHD Neonatal Research Network, with emphasis on the concordance of BCs and CSF cultures, rates of infection, infecting pathogens, risk factors for dis-ease, in-hospital morbidity, and mortality. Five per-cent of the infants evaluated with an LP had menin-gitis. Lower GA and prior sepsis increased risk of meningitis. One in 4 infants with meningitis had seizures, a clinical sign that could lead to earlier LP and diagnosis.
Perhaps the most important finding of this study is that one third of the patients with meningitis had negative BCs within a week of the CSF culture. The importance of the LP in the evaluation of VLBW infants with suspected late-onset infection remains controversial. Because VLBW infants often suffer re-spiratory distress and cardiovascular instability, it has been argued that many infants are too ill to
TABLE 3. Distribution of Pathogens Associated With the First Episode of LOM
Organism Overall With Sepsis Without Sepsis
n % n % n %
Gram-positive organisms 84 63.0 62 69.7 22 48.9
CONS 39 29.1 39 43.8 0 0
S aureus 11 8.2 9 10.1 2 4.4 Enterococcusspp. 18 13.4 6 6.7 12 26.7
Group B streptococcus 9 6.7 8 9.0 1 2.2
S viridans 7 5.2 0 0 7 15.6 Gram-negative organisms 26 19.4 15 16.9 11 24.4
E coli 9 6.7 5 5.6 4 8.9
Klebsiella 7 5.2 5 5.6 2 4.4 Serratia 4 3.0 1 1.1 3 6.7
Other 6 4.5 4 4.5 2 4.4
Fungi 24 17.9 12 13.5 12 26.7
C albicans 18 13.4 8 9.0 10 22.2 Candida parapsilosis 5 3.7 4 4.5 1 2.2
Other 1 0.7 0 0 1 2.2
undergo an LP. In this study, only one half of all infants who had a BC performed also had an LP. Moreover, there were major practice differences: the percentage of infants who had a BC and an LP per-formed ranged from 22% to 85% across centers. Al-though LPs were performed more frequently in in-fants with positive BCs, only 66% of the inin-fants with culture-confirmed sepsis had an LP performed. We speculate that the failure to perform an LP routinely in infants with suspected late-onset sepsis might re-sult in an underdiagnosis of meningitis.
A possible limitation of this analysis is that there is physician variation in the decision to perform an LP. Because meningitis can be diagnosed only by LP, there may be selection bias in the patients diagnosed with meningitis. Infants with a positive BC were significantly more likely to have an LP performed at
all centers. We have no information on why an LP was not performed if a sepsis evaluation was done (ie, if a BC was drawn to rule out sepsis). Better understanding of why physicians do or do not per-form an LP and the diagnostic accuracy of factors used to make this decision might lead to improved patient care. However, among those patients who had an LP performed, there was no significant dif-ference across centers in the rate of positive CSF cultures. This finding suggests that, although there are LP practice differences across centers, they prob-ably are not explained by better clinical acumen (ie, some clinicians are not necessarily better at predict-ing which VLBW infant has menpredict-ingitis and therefore requires an LP).
A wide range of bacterial and fungal agents was associated with LOM in this cohort. The pathogens
TABLE 4. Neonatal Characteristics and Risk of Meningitis Among Infants Evaluated With an LP
Total,n Neonates With Meningitis Adjusted OR for Meningitis (95% CI)*
PValue*
n %
Race
Black 1212 61 5 1.4 (0.9–2.2) .2
Hispanic 521 24 5 1.0 (0.6–1.8)
Other 79 2 3 0.4 (0.1–2.0)
White 1063 47 4 1.0
Gender
Male 1557 69 4 0.9 (0.6–1.3) .5
Female 1320 65 5 1.0
GA
⬍25 476 31 7 2.6 (1.2–5.7) .01
25–28 1703 86 5 2.2 (1.1–4.1)
ⱖ29 698 17 2 1.0
Birth weight
401–500 54 4 7 0.7 (0.2–2.5) .3
501–750 823 45 5 0.5 (0.3–1.1)
751–1000 944 53 6 0.7 (0.4–1.4)
1001–1250 656 15 2 0.4 (0.2–0.8)
1251–1500 400 17 4 1.0
Prior sepsis
Yes 1583 104 7 2.9 (1.9–4.5) ⬍.001
No 1294 30 2 1.0
Prior IVH
Yes 395 26 7 1.2 (0.8–2.0) .4
No 2449 107 4 1.0
PVL
Yes 68 7 10 2.0 (0.8–4.6) .1
No 2774 126 5 1.0
Total 2877 134 5
* ORs (with 95% CIs) andP values from a logistic regression model, which included all variables shown and study center. GA and birth weight were included as categorical variables for estimating ORs and as continuous variables for determiningPvalues. Race was missing for 2 infants, prior IVH for 33, and PVL for 35.
TABLE 5. Infection Status Versus Risk of Death Among Infants Evaluated With an LP
Infection Status n % Died OR for Death (95% CI)*
LOM with sepsis† 89 26 12.1 (5.3–27.2)
LOM without sepsis 45 18 8.2 (2.9–23.1)
Sepsis/no meningitis/no NEC 1263 9 3.9 (2.0–7.6) NEC (with or without sepsis)‡/no meningitis 329 28 17.1 (8.6–34.1) Culture negative clinical infection only§ 637 6 2.6 (1.3–5.3)
Uninfected㛳 514 2 1.0
* OR for death in each group, compared with uninfected after adjusting for study center and GA in a logistic regression model.
† Culture confirmed.
‡ Among infants with NEC, 234 had sepsis and 95 did not.
were similar to those reported in network patients with late-onset sepsis.12 Although Gram-positive
agents were most frequent overall, Gram-negative and fungal agents were more common among pa-tients with meningitis alone than in those with both meningitis and sepsis (24% vs 17% and 27% vs 14%, respectively). One third of infants with meningitis did not have a follow-up LP; 11 of these 44 patients (25%) died within 6 days of the initial culture and were likely very sick. Of concern is the fact that 10 of 90 repeat LPs grew the same organism as the original CSF culture, underscoring the importance of a repeat LP to determine that meningitis is being appropri-ately treated.
VLBW infants with meningitis were significantly more likely to die (23%), compared with infants with sepsis alone (9%) or those who were uninfected (2%). Infants with Gram-negative or fungal meningitis were at particularly high risk for death (41% and 32%, respectively). Moreover, infants with meningi-tis were significantly more likely to have seizures, longer time on mechanical ventilation, longer time to reach full feeds, and longer hospital stays than in-fants who were uninfected.
CONCLUSIONS
Neonatal meningitis remains a serious complica-tion among VLBW infants that is associated with increased severity of illness and risk of death. Be-cause at least one third of infants with meningitis had an associated negative BC, these data suggest that LOM may be underdiagnosed in VLBW neona-tal intensive care unit patients, many of whom do not have an LP performed because they are considered too sick to tap. These data support the need to per-form an LP as part of the diagnostic evaluation of the VLBW infant with suspected late-onset infection. An LP is warranted, because meningitis may occur with-out a positive BC. Furthermore, the identification of Gram-negative or fungal agents in the CSF may in-fluence the choice of drug and length of therapy. Finally, novel strategies to decrease the risk of men-ingitis among VLBW infants would reduce
short-and long-term neonatal morbidity, the high cost of VLBW infant care, and improve survival.
ACKNOWLEDGMENTS
Financial support was provided by National Institutes of Health grants U10 HD27851, U01 HD36790, U10 HD21364, U10 HD34216, U10 HD27871, M01 RR 06022, U10 HD27856, M01 RR 00750, U10 HD27853, M01 RR 08084, U10 HD34167, M01 RR 02635, M01 RR 02172, M01 RR 01032, U10 HD21373, U10 HD27904, U10 HD21397, U10 HD21415, U10 HD21385, U10 HD40689, U10 HD27880, M01 RR 00070, U10 HD27881, and M01 RR 00997.
We thank Mazie Tinsley for manuscript preparation.
REFERENCES
1. Davies PA, Rudd PT.Neonatal Meningitis. London, United Kingdom: MacKeith Press; 1994:1–177
2. Holt DE, Halket S, de Louvois J, Harvey D. Neonatal meningitis in England and Wales: 10 years on.Arch Dis Child Fetal Neonatal Ed.
2001;84:F85–F89
3. Harvey D, Holt DE, Bedford H. Bacterial meningitis in the newborn: a prospective study of mortality and morbidity.Semin Perinatol.1999;23: 218 –225
4. de Louvois J. Acute bacterial meningitis in the newborn.J Antimicrob Chemother.1994;34(suppl A):61–73
5. Hristeva L, Booy R, Bowler I, Wilkinson AR. Prospective surveillance of neonatal meningitis.Arch Dis Child.1993;69:14 –18
6. McIntyre P, Isaacs D. Lumbar puncture in suspected neonatal sepsis.J Paediatr Child Health.1995;31:1–2
7. Schwersenski J, McIntyre L, Bauer CR. Lumbar puncture frequency and cerebrospinal fluid analysis in the neonate.Am J Dis Child.1991;145: 54 –58
8. MacMahon P, Jewes L, de Louvois J. Routine lumbar punctures in the newborn—are they justified?Eur J Pediatr.1990;149:797–799 9. Kumar P, Sarkar S, Narang A. Role of routine lumbar puncture in
neonatal sepsis.J Paediatr Child Health.1995;31:8 –10
10. Visser VE, Hall RT. Lumbar puncture in the evaluation of suspected neonatal sepsis.J Pediatr.1980;96:1063–1066
11. Hack M, Horbar JD, Malloy MH, Tyson JE, Wright E, Wright L. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Network. Pediatrics. 1991;87: 587–597
12. Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network.Pediatrics.2002;110:285–291
13. SAS Institute.SAS/STAT User’s Guide, Version 8. Cary, NC: SAS Institute Inc; 1999
14. Doctor BA, Newman N, Minich NM, Taylor HG, Fanaroff AA, Hack M. Clinical outcomes of neonatal meningitis in very-low birth-weight in-fants.Clin Pediatr (Phila).2001;40:473– 480
15. Klinger G, Chin CN, Beyene J, Perlman M. Predicting the outcome of neonatal bacterial meningitis.Pediatrics.2000;106:477– 482
APPENDIX 1. NICHD Neonatal Research Network (1996 –2000)
Center Principal Investigator Study Coordinator No. of Patients Studied
Brown University William Oh, MD Angelita Hensman, RN 703 Case Western Reserve University Avroy A. Fanaroff, MB, BCh Nancy Newman, RN 541 Emory University Barbara J. Stoll, MD Ellen Hale, RN 652 Harvard University Ann R. Stark, MD Kerri Fournier, RN 456 Indiana University James A. Lemons, MD DeeDee Appel, RN 972 Stanford University David K. Stevenson, MD Bethany Ball, BS 476 University of Alabama Waldemar A. Carlo, MD Monica Collins, RN 873 University of Cincinnati Edward F. Donovan, MD Marcia Mersmann, RN 1080 University of Miami Charles R. Bauer, MD Amy Mur Worth, BSN 691 University of New Mexico Lu-Ann Papile, MD Conra Backstrom, RN 367 University of Tennessee Sheldon B. Korones, MD Tina Hudson, RN 474 University of Texas at Dallas Abbot R. Laptook, MD Susie Madison, RN 554 University of Texas at Houston Jon E. Tyson, MD, MPH Georgia McDavid, RN 808 Wayne State University Seetha Shankaran, MD Gerry Muran, BSN 567 Yale University Richard A. Ehrenkranz, MD Pat Gettner, RN 427 NICHD Linda L. Wright, MD Beth B. McClure, MEd
Research Triangle Institute W. Kenneth Poole, PhD Betty Hastings
DOI: 10.1542/peds.113.5.1181
2004;113;1181
Pediatrics
Abbot R. Laptook, David K. Stevenson, Lu-Ann Papile and W. Kenneth Poole
Jon E. Tyson, William Oh, Charles R. Bauer, Sheldon B. Korones, Seetha Shankaran,
Carlo, Richard A. Ehrenkranz, James A. Lemons, Edward F. Donovan, Ann R. Stark,
Barbara J. Stoll, Nellie Hansen, Avroy A. Fanaroff, Linda L. Wright, Waldemar A.
Very Low Birth Weight Infants
To Tap or Not to Tap: High Likelihood of Meningitis Without Sepsis Among
Services
Updated Information &
http://pediatrics.aappublications.org/content/113/5/1181
including high resolution figures, can be found at:
References
http://pediatrics.aappublications.org/content/113/5/1181#BIBL
This article cites 13 articles, 5 of which you can access for free at:
Subspecialty Collections
b
http://www.aappublications.org/cgi/collection/infectious_diseases_su
Infectious Disease
http://www.aappublications.org/cgi/collection/neonatology_sub
Neonatology
sub
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_
Fetus/Newborn Infant
following collection(s):
This article, along with others on similar topics, appears in the
Permissions & Licensing
http://www.aappublications.org/site/misc/Permissions.xhtml
in its entirety can be found online at:
Information about reproducing this article in parts (figures, tables) or
Reprints
http://www.aappublications.org/site/misc/reprints.xhtml
DOI: 10.1542/peds.113.5.1181
2004;113;1181
Pediatrics
Abbot R. Laptook, David K. Stevenson, Lu-Ann Papile and W. Kenneth Poole
Jon E. Tyson, William Oh, Charles R. Bauer, Sheldon B. Korones, Seetha Shankaran,
Carlo, Richard A. Ehrenkranz, James A. Lemons, Edward F. Donovan, Ann R. Stark,
Barbara J. Stoll, Nellie Hansen, Avroy A. Fanaroff, Linda L. Wright, Waldemar A.
Very Low Birth Weight Infants
To Tap or Not to Tap: High Likelihood of Meningitis Without Sepsis Among
http://pediatrics.aappublications.org/content/113/5/1181
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.