J
OURNAL OFC
LINICALM
ICROBIOLOGY,
0095-1137/98/$04.00
1
0
July 1998, p. 2157–2163
Vol. 36, No. 7
Copyright © 1998, American Society for Microbiology. All Rights Reserved.
Fatal Hormonema dematioides Peritonitis in a Patient on
Continuous Ambulatory Peritoneal Dialysis: Criteria
for Organism Identification and Review of Other
Known Fungal Etiologic Agents
JONG HEE SHIN,
1SANG KU LEE,
1SOON PAL SUH,
1DONG WOOK RYANG,
1NAM HO KIM,
1MICHAEL G. RINALDI,
2,3ANDDEANNA A. SUTTON
3*
Departments of Clinical Pathology and Internal Medicine, Chonnam University Medical School, Kwangju, Korea,
1and
Audie L. Murphy Division, South Texas Veterans Health Care System,
2and Fungus Testing Laboratory,
Department of Pathology, University of Texas Health Science Center at San Antonio,
3San Antonio, Texas 78284
Received 2 January 1998/Returned for modification 9 March 1998/Accepted 7 April 1998
We report a fatal case a fungal peritonitis caused by the yeast-like dematiaceous mould Hormonema
dematioides in a 45-year-old woman. The woman had a 13-year history of insulin-dependent diabetes mellitus
and had been on continuous ambulatory peritoneal dialysis for chronic renal failure. H. dematioides was
repeatedly isolated from the dialysate culture specimens collected on days 3, 9, 16, and 20 of her hospital stay.
Preliminary culture reports on day 7 of the growth of a yeast-like fungus, a probable Candida species, prompted
the administration of fluconazole (FLU). Intraperitoneal and intravenous FLU failed to eliminate the mould,
and the patient expired on day 21 of her hospital stay. We use this case to present what appears to be the first
report of fungal peritonitis due to H. dematioides, to provide laboratorians with criteria for differentiating this
organism from the similar mould Aureobasidium pullulans and from various yeast genera, and to provide a
review of known fungal taxa inciting peritonitis.
Fungal peritonitis is a serious and potentially
life-threaten-ing complication of both intermittent peritoneal dialysis and
continuous ambulatory peritoneal dialysis (CAPD).
Investiga-tors reviewing significant numbers of CAPD-associated fungal
peritonitis episodes cite yeasts, particularly Candida species, as
the predominant etiologic agents (10, 12, 13, 20, 29, 37, 38, 50,
52, 53, 54, 58, 61, 63, 65, 66, 68, 73, 78). Filamentous fungi
complicating CAPD, although reported less frequently and
fewer in number, encompass a wide array of agents, from the
classic, systemic pathogens (4, 42, 45) to zygomycetous species
(55, 64) and members of numerous moniliaceous (3, 11, 16, 25,
27, 30, 33, 39, 40, 48, 51, 57, 67, 71, 75, 76, 77) and
dematia-ceous genera (1, 2, 6, 7, 14, 21, 28, 31, 34, 43, 44, 59, 69, 80). See
Table 1 for a listing of reported etiologic agents of fungal
peritonitis. Filamentous CAPD-associated fungi displaying
cream-colored (moniliaceous) colonies and yeast-like
synana-morphs may initially be considered Candida or Cryptococcus
species. Two such organisms, Hormonema dematioides
Lager-berg et Melin [teleomorph, Sydowia polyspora (von Tavel)
Mu¨ller], the subject of this report, and Aureobasidium pullulans
(deBary) Arnaud, an agent previously reported in fungal
peri-tonitis (7, 14), are both initially somewhat mucoid, yeast-like
(both macroscopically and microscopically), and hyaline. As
they mature, their filamentous nature becomes evident and
colonies become dematiaceous, with the production of brown,
thick-walled hyphae. McCarthy et al. observed that when
tested by conventional yeast identification systems, specifically
API 20C yeast identification system strips (bio Me´rieux, Marcy
l’Etoile, France), A. pullulans usually fails to give a code while
H. dematioides may code as Cryptococcus albidus (49). Both
organisms may present diagnostic or identification difficulties
in the setting of the CAPD-associated fungal peritonitis
pa-tient.
Case report.
A 45-year-old woman on CAPD presented at
the emergency room of Chonnam University Hospital on 19
March 1996 with nausea, anorexia, increased body weight
(from 56 to 74 kg), abdominal distention, and pitting edema.
She had a 13-year history of insulin-dependent diabetes
mel-litus and had had an arteriovenous shunt inserted in February
of 1995. Malfunction of the shunt required switching from
hemodialysis to CAPD in April 1995. On 1 March 1996, the
patient developed abdominal pain and her dialysate became
cloudy. Cefazolin and vancomycin were administered
intra-peritoneally for 20 days without clinical improvement. Upon
admission from the emergency room, the patient’s dialysate
cell count was 306/
m
l, with a predominance of
polymorphonu-clear neutrophils (70%). The hemoglobin level was 6.6 g/dl, the
leukocyte count was 6,700/
m
l, the blood urea nitrogen level was
12.1 mg/dl, and the serum creatinine level was 5.0 mg/dl. The
patient was initially treated with intraperitoneal ceftazidime
and imipenem. Fluconazole therapy was started on hospital
day 7, following a preliminary culture report indicating the
presence of a yeast-like fungus, probably a Candida species, in
the dialysate. Dialysate cell counts on day 6 were 2,600/
m
l, with
a predominance of polymorphonuclear neutrophils. On day 8,
the patient’s abdominal pain and fever slightly improved, but
vasopressive drug and O
2therapies were started due to the
occurrence of respiratory insufficiency and hypotension.
Dia-lysate cell counts were 675 and 441/
m
l on days 9 and 17,
respectively. The same yeast-like fungus was cultured from the
dialysate on days 3, 9, 16, and 20. Fluconazole was
adminis-tered intraperitoneally (200 mg/day) for 15 days and
intrave-* Corresponding author. Mailing address: Fungus Testing
Labora-tory, Department of Pathology, University of Texas Health Science
Center at San Antonio, 7703 Floyd Curl Dr., San Antonio, TX
78284-7750. Phone: (210) 567-4131. Fax: (210) 567-4076. E-mail: suttond
@uthscsa.edu
2157
on May 15, 2020 by guest
http://jcm.asm.org/
nously (800 mg/day) for the last 2 days. The catheter tip was
removed on day 20. On day 21 the patient began to lose
consciousness, appeared to have signs of acute respiratory
in-sufficiency due to hypoxia and septic shock, and expired. Blood
cultures for the causative organism remained negative.
Mycology.
All four peritoneal fluid culture specimens
col-lected during the patient’s hospital stay (on days 3, 9, 16, and
20) revealed the same organism. Three of the dialysates were
inoculated onto Sabouraud dextrose agar (SDA) (Becton
Dickinson, Cockeysville, Md.), prepared in-house (Fig. 1),
while one was inoculated into BACTEC 16A and 17A bottles
(Becton Dickinson, Towson, Md.). Only the BACTEC 16A
[image:2.612.370.487.67.314.2]bottle (aerobic medium) was positive after 48 h of incubation.
Pure growth of cream-colored mucoid colonies was observed
on SDA and on the blood agar plate subculture from the
BACTEC 16A in 24 to 48 h at 35°C. Growth at 35°C was slow,
and a Gram stain of organisms from the colony revealed
oval-shaped yeast forms. API 20C yeast identification system strips,
tested a total of seven times with identical results, indicated
assimilation of glucose, glycerol, 2-keto-gluconate,
L-arabi-nose,
D-xylose, adonitol, xylitol, galactose, inositol, sorbitol,cellobiose, maltose, saccharose, trehalose, melibiose, and
raf-finose, giving a numerical code of 6773277. The API database,
which provides a list of species and their probabilities, with a
confidence estimate for each identification, indicated the code
as an unacceptable profile with no identification. Ancillary
testing on cornmeal agar (Difco Laboratories, Detroit, Mich.)
by the Dalmau method (17) indicated the presence of hyphae
and blastic conidia. Conidia occurred asynchronously from the
hyphae as viewed under the coverslip after 72 h of incubation
at 25°C (Fig. 2). Prolonged incubation of the isolates for 1, 2,
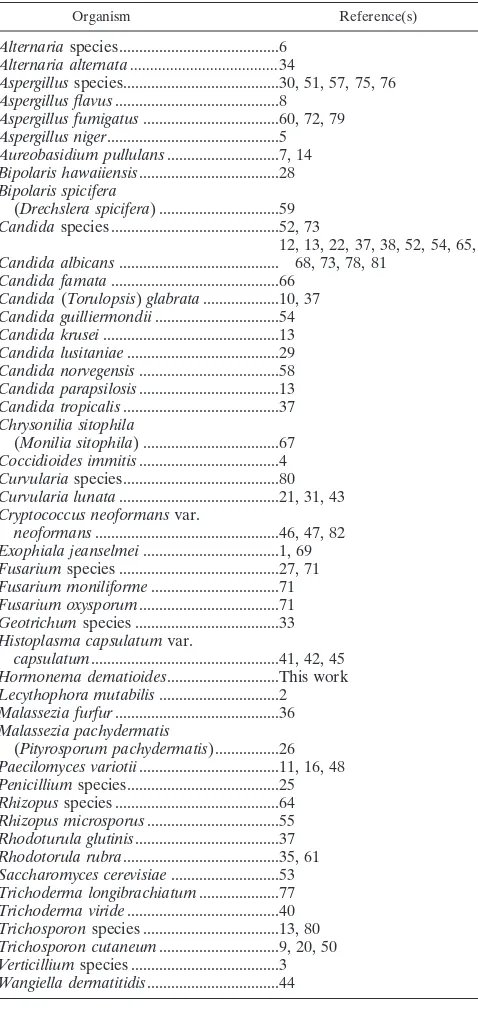
TABLE 1. Reported Etiologic Agents of Fungal Peritonitis
Organism Reference(s)
Alternaria species...6
Alternaria alternata ...34
Aspergillus species...30, 51, 57, 75, 76
Aspergillus flavus...8
Aspergillus fumigatus ...60, 72, 79
Aspergillus niger...5
Aureobasidium pullulans...7, 14
Bipolaris hawaiiensis...28
Bipolaris spicifera
(Drechslera spicifera) ...59
Candida species...52, 73
Candida albicans ...
12, 13, 22, 37, 38, 52, 54, 65,
68, 73, 78, 81
Candida famata ...66
Candida (Torulopsis) glabrata ...10, 37
Candida guilliermondii ...54
Candida krusei ...13
Candida lusitaniae ...29
Candida norvegensis ...58
Candida parapsilosis...13
Candida tropicalis ...37
Chrysonilia sitophila
(Monilia sitophila) ...67
Coccidioides immitis...4
Curvularia species...80
Curvularia lunata ...21, 31, 43
Cryptococcus neoformans var.
neoformans ...46, 47, 82
Exophiala jeanselmei ...1, 69
Fusarium species ...27, 71
Fusarium moniliforme ...71
Fusarium oxysporum...71
Geotrichum species ...33
Histoplasma capsulatum var.
capsulatum...41, 42, 45
Hormonema dematioides...This work
Lecythophora mutabilis ...2
Malassezia furfur ...36
Malassezia pachydermatis
(Pityrosporum pachydermatis)...26
Paecilomyces variotii...11, 16, 48
Penicillium species...25
Rhizopus species ...64
Rhizopus microsporus ...55
Rhodoturula glutinis...37
Rhodotorula rubra...35, 61
Saccharomyces cerevisiae ...53
Trichoderma longibrachiatum...77
Trichoderma viride...40
Trichosporon species ...13, 80
Trichosporon cutaneum...9, 20, 50
Verticillium species ...3
[image:2.612.51.290.78.590.2]Wangiella dermatitidis...44
FIG. 1. Slow-growing, cream-colored, mucoid colonies of H. dematioides on SDA (72 h; 35°C).
FIG. 2. Basipetal, hyaline blastic conidia of H. dematioides produced asyn-chronously (one at a time) from hyaline hyphae on cornmeal agar by the Dalmau method (72 h; 25°C). Magnification,3710.
on May 15, 2020 by guest
http://jcm.asm.org/
[image:2.612.310.546.571.698.2]and 3 weeks on SDA revealed their dematiaceous nature (Fig.
3). Subsequent subcultures of the isolate at 25°C were totally
brown to black. A 5-day slide culture revealed the presence of
moniliaceous blastic conidia being produced from
dematia-ceous hyphae (Fig. 4).
Pathogenicity and identifying features.
Fungal peritonitis in
patients on CAPD, although significantly less frequent than
bacterial peritonitis (3 to 15% versus
.
80%, respectively), is a
well-documented clinical entity (13, 38, 54, 65, 78). Signs and
symptoms are essentially the same in both presentations and
may include cloudy dialysate effluent, dialysate leukocyte
counts greater than 100/mm
3, neutrophil counts greater than
50%, abdominal pain, distension, rigidity, nausea and
vomit-ing, diarrhea, and fever. Because of these similarities and the
higher incidence of bacterial peritonitis, fungal etiologies may
be overlooked and may have contributed, in part, to a delayed
antifungal regimen in the case of this patient. She received
cefazolin and vancomycin intraperitoneally for 20 days,
with-out improvement, followed by ceftazidine and imipenem
intra-peritoneally for another 7 days. Not until hospital day 7
(epi-sode day 28), with the report of a Candida species in the
dialysate, was fluconazole therapy started. Although the route
of infection is not clear, several reports have cited altered host
flora due to prior or prolonged use of broad-spectrum
antibac-terial therapy as a significant risk factor and/or as being
asso-ciated with the development of fungal peritonitis (13, 38, 54,
65, 78). Fungal cultures taken earlier in the course of this
patient’s episode or during the administration of antibacterial
agents would have provided direction for more appropriate or
additional antifungal therapy.
[image:3.612.50.289.69.602.2]The recovery of cream-colored, mucoid colonies from the
dialysate on hospital day 7 (episode day 28) provided the first
evidence of a fungal pathogen. Cream-colored mucoid
colo-nies are consistent with a variety of fungal genera, both
yeast-like and filamentous, including Candida, Cryptococcus,
Aureo-basidium, and Hormonema. In the genera Aureobasidium and
Hormonema, cream-colored colonies become brownish to
oli-vaceous black with time, thereby requiring extended
incuba-tion for recogniincuba-tion of their dematiaceous nature. The API
20C yeast identification system utilized with these colonies
failed to provide an identification, giving an unrecognizable
code of 6773277. McCarthy et al. recently reported on 4 of 11
isolates of H. dematioides coding as C. albidus by this method
(49). The remaining 7 isolates in their group revealed several
different unrecognizable codes, which did not include this
iso-late’s number, 6773277. Their results reinforce the necessity of
performing critical microscopic observations (for blastic
conidia, hyphae, pseudohyphae, etc.) and demonstrate the
fu-tility of relying solely on binary codes and/or physiologic
char-acteristics for these similar, cream-colored, mucoid taxa.
Be-cause the API 20C method failed to provide an identification,
the case isolate was subsequently identified by ancillary testing
utilizing the Dalmau method for determining the method of
conidiogenesis and extended incubation for revealing its
de-matiaceous affinities. Slide culture preparations normally used
for studying methods of conidiogenesis in filamentous fungi
FIG. 3. Macroscopic morphology of H. dematioides on SDA (1 week [A], 2 [image:3.612.310.548.70.198.2]weeks [B], and 3 weeks [C]; 25°C).
FIG. 4. Moniliaceous blastic conidia of H. dematioides being produced from conidiogenous loci (arrows) on dematiaceous hyphae. Magnification,3280.
V
OL. 36, 1998
NOTES
2159
on May 15, 2020 by guest
http://jcm.asm.org/
TABLE 2. Differentiation of similar species
Species Macroscopic morphologya Microscopic
morphologyb
Physiologyc
Comments Reference(s)
Cyclo-heximide 25°C 35°C 42°C Urease Nitrate fermentationGlucose Glucosidemethyl-a- D-Gluconate
Hormonema
dematioides Creamy, moist, mucoid, whiteto cream initially, becoming brown to black
Hyphae hyaline and dematiaceous; hyaline, oval-shaped blastic conidia, asynchronous, from hyaline and dematiaceous hyphae; nonbudding
2 1 V 2 V V 2 NG NG Cornmeal agar
Dalmau plate to determine method of conidiogenesis
18, 19, 32, 62
Aureobasidium
pullulans Creamy, moist, white tocream initially, becoming partly brown to black (frequently with a white, radiating fringe at the periphery)
Hyphae hyaline and dematiaceous; hyaline, oval-shaped blastic conidia, synchronous, from hyaline hyphae only; nonbudding
2 1 V 2 V V 2 G G Cornmeal agar
Dalmau plate to determine method of conidiogenesis
18, 19, 32, 62
Candida albicans
Cream colored, numerous phenotypes (dry, wrinkled, mucoid)
Variably sized, globose to oval budding yeast; pseudohyphae and true hyphae; germ tube positive
1 1 1 1 2 2 1 Numerous other
yeast species are etiologic agents of CAPD-associated fungal peritonitis
62, 74
Cryptococcus albidus
Cream-colored to beige to slight pink, mucoid colonies
Large, round budding yeast; no true hyphae or pseudo-hyphae
2 1 W 2 1 1 2 Some H.
dema-tioides isolates
may code as C.
albidus by API
20C
49, 62, 74
Candida
parapsilosis Cream-colored, moist Branched pseudo-hyphae, oval budding yeast
2 1 1 2 2 2 1 A common yeast
negative for growth on cycloheximide yeast that could be confused with
H. dematioides
74
aOn SDA.
bCornmeal agar, Dalmau method.
cPhysiology was studied under the following conditions: on medium with cycloheximide; at 25, 35, and 42°C; on Christensen’s urea agar slant (Urease); and by the method of Pincus et al. (62) (Nitrate). Results are
reported as follows:2, negative;1, positive; V, variable; W, weak; NG, no growth; and G, growth.
NOTES
J.
C
LIN
.M
ICROBIOL
.
are generally less satisfactory than the Dalmau method for
visualizing the asynchronous or synchronous development of
conidia in Hormonema and Aureobasidium species,
respec-tively.
H. dematioides is an important wood-bluing fungus often
isolated from discolored coniferous wood or needles (32). It is
also appears to occupy an ecological niche in moist
environ-ments, as evidenced by the isolates submitted to the Fungus
Testing Laboratory (FTL) at the University of Texas Health
Science Center at San Antonio from high-humidity areas. Its
pathogenicity in humans has been previously documented as
an agent of subcutaneous phaeohyphomycosis of the hands of
an immunocompetent host (15). Additional human sites from
which the organism has been recovered include cerebrospinal
fluid, blood, stool, pleural fluid, a surgical wound, and a knee
(FTL isolates [unpublished data]).
Because authors have illustrated H. dematioides under the
name of A. pullulans, some cases of infection ascribed to A.
pullulans may actually have been caused by misidentified
iso-lates of H. dematioides. Recently Clark et al. described a case
of peritonitis caused by A. pullulans in a patient on CAPD (14).
Caporale et al. reported A. pullulans as an agent of peritoneal
catheter colonization and peritonitis (7). The present case
demonstrates that H. dematioides can also cause
CAPD-asso-ciated peritonitis. The pure growth of the organism from four
separate specimens from a patient who had diffuse abdominal
pain and turbid dialysates indicates that it was the cause of
peritonitis and not a contaminant.
Colonies on SDA at 25°C are white to cream, smooth, and
soon covered with a light slimy mass of blastoconidia. Poorly
conidiating cultures are olivaceous black with a wooly mycelial
mat. The optimum temperature for growth is 24°C, with a daily
growth rate of
.
6 mm; no growth is observed on media
con-taining cycloheximide. Isolates that have been subcultured
re-peatedly conidiate poorly and tend to grow faster than freshly
isolated strains (32). Microscopically, hyphae are septate,
hy-aline, and initially thin walled and soon become brown and
thick walled, with cells wider than they are long. Hyaline,
smooth, ellipsoidal blastic conidia (4.5 to 12
m
m by 3 to 4.5
m
m) are borne asynchronously by percurrent proliferation
(each successive conidium growing through the tip of the
co-nidiogenous cell) from mostly intercalary coco-nidiogenous loci
on hyaline as well as dematiaceous hyphae (Fig. 4). Older
conidia often swell and become brown and are frequently two
celled. Endoconidia (conidia formed inside hyphal cells) may
be present. The method of conidiogenesis for both A. pullulans
and H. dematioides is best studied by the Dalmau method. H.
dematioides is differentiated from A. pullulans by
asynchro-nous, basipetal (youngest conidium at the base) conidial
for-mation from both hyaline and dematiaceous hyphae rather
than synchronous (all at the same time) conidial formation
from only hyaline hyphae. Synchronous conidia appear as a
cluster, with each member attached to a separate denticle,
while asynchronous conidia appear as a detached cluster
around an individual conidiogenous aperture. Also note that
several other Hormonema species exist, but all grow
,
6 mm
per day at 24°C. Both H. dematioides and A. pullulans are
differentiated from hyaline, mucoid yeasts by the formation of
dematiaceous hyphae (Table 2).
Therapy.
Fungal peritonitis is associated with significant
morbidity and mortality. In the patient this report,
intraperi-toneal fluconazole (200 mg/day for 15 days) followed by
intra-venous fluconazole (800 mg/day for 2 days) therapy failed to
improve the clinical conditions. Retrospectively, higher
em-piric doses earlier may have been more efficacious, as judged
by data from yeast isolates that exhibit dose-dependent
sus-ceptibility to fluconazole and that therefore require maximum
dosing regimens (70). Catheter removal, considered a
neces-sary adjunct to antifungal therapy (11, 37, 38, 54, 77), was
delayed because there was no other therapeutic option for
renal failure in this patient. The patient had severe, frequent
hypotension histories associated with the arteriovenous shunt,
severe malnutrition, and extensive peritoneal adhesions.
Treat-ment of fungal peritonitis caused by rare fungi such as H.
dematioides is complicated by problems in identification, the
lack of in vitro antifungal susceptibility data, empiric therapy
which may not be appropriate (24), and the reluctance to
initiate amphotericin B therapy until a final identification is
made. Although standardization of susceptibility testing for
filamentous fungi is only commencing (23) and in vivo-in vitro
correlations are lacking, a significant number of dematiaceous
moulds appear to be susceptible, in vitro, to itraconazole (74).
Although the case isolate was not available for testing against
antifungal agents, data from the FTL for five similar
dematia-ceous A. pullulans isolates tested by a modified National
Com-mittee for Clinical Laboratory Standards reference method
(56) suggest greater in vitro susceptibility to itraconazole. Had
the filamentous and dematiaceous nature of the etiologic agent
been known earlier, the institution of itraconazole therapy,
with or without amphotericin B, may have facilitated
deferves-cence. Several reports cite its use in CAPD-associated fungal
peritonitis (12, 22, 28, 39, 67, 77).
Although filamentous fungal organisms in CAPD-associated
peritonitis are low in incidence, they are often associated with
significant morbidity and/or mortality. As this case emphasizes,
consideration of a fungal etiology early in the course of the
disease, particularly in patients unresponsive to antibacterial
therapy, is crucial. Early recognition and identification of the
etiologic agent, coupled with appropriate, aggressive therapy
(antifungal therapy and catheter removal, when possible),
ap-pear tantamount to a successful outcome. H. dematioides is yet
another dematiaceous agent that incites CAPD-associated
fun-gal peritonitis.
REFERENCES
1. Agarwal, S., N. L. Goodman, and H. H. Malluche. 1993. Peritonitis due to Exophiala jeanselmei in a patient undergoing continuous ambulatory perito-neal dialysis. Am. J. Kidney Dis. 21:673–675.
2. Ahmad, S., R. J. Johnson, S. Hillier, W. R. Shelton, and M. G. Rinaldi. 1985. Fungal peritonitis caused by Lecythophora mutabilis. J. Clin. Microbiol. 22: 182–186.
3. Amici, G., S. Grandesso, A. Mottola, G. Virga, T. Teodori, M. C. Maresca,
and C. Bocci.1994. Verticillium peritonitis in a patient on peritoneal dialysis. Am. J. Nephrol. 14:216–219.
4. Ampel, N. M., J. D. White, U. R. Varanasi, T. R. Larwood, D. B. Van Wyck,
and J. N. Galgiani.1988. Coccidioidal peritonitis associated with continuous ambulatory peritoneal dialysis. Am. J. Kidney Dis. 11:512–514.
5. Bibashi, E., A. Papagianni, A. Lelesidis, R. Antoniadou, and M.
Papadimi-triou.1993. Peritonitis due to Aspergillus niger in a patient on continuous ambulatory peritoneal dialysis shortly after kidney graft rejection. Nephrol. Dial. Transplant 8:185–187.
6. Buchanan, W. E., M. J. Quinn, and J. A. Hasbargen. 1994. Peritoneal colonization with Alternaria: successful treatment with catheter preservation. Periton. Dial. Int. 14:91–92.
7. Caporale, N. E., L. Calegari, D. Perez, and E. Gezuele. 1996. Peritoneal catheter colonization and peritonitis with Aureobasidium pullulans. Periton. Dial. Int. 16:97–98.
8. Carpenter, J. L., C. J. Goulks, and M. H. Weiner. 1982. Peritoneal dialysis complicated by Aspergillus flavus peritonitis: a role for fungal antigen sero-diagnosis. Nephron 32:258–260.
9. Carr, M. E., A. O’Brien, D. Moore, and J. A. Keogh. 1987. Trichosporon cutaneum C.A.P.D. peritonitis. Postgrad. Med. J. 663:1008. (Letter.) 10. Cecchin, E., S. De Marchi, G. Panarello, A. Franceschin, V. Chiaradia, G.
Santini, and F. Tesio.1984. Torulopsis glabrata peritonitis complicating con-tinuous ambulatory peritoneal dialysis: successful management with oral 5-fluorocytosine. Am. J. Kidney Dis. 4:280–284.
11. Chan, T. H., A. Koehler, and P. K. Li. 1996. Paecilomyces variotii peritonitis in patients on continuous ambulatory peritoneal dialysis. Am. J. Kidney Dis.
27:138–142.
V
OL. 36, 1998
NOTES
2161
on May 15, 2020 by guest
http://jcm.asm.org/
12. Chan, T. M., C. Y. Chan, S. W. Cheng, W. K. Lo, C. Y. Lo, and I. K. Cheng. 1994. Treatment of fungal peritonitis complicating continuous ambulatory peritoneal dialysis with oral fluconazole: a series of 21 patients. Nephrol. Dial. Transplant 9:539–542.
13. Cheng, I. K. P., G.-X. Fang, T.-M. Chan, P. C. K. Chan, and M.-K. Chan. 1989. Fungal peritonitis complicating peritoneal dialysis: report of 27 cases and review of treatment. Q. J. Med. 71:407–416.
14. Clark, E. C., S. M. Silver, G. E. Hollick, and M. G. Rinaldi. 1995. Continuous ambulatory peritoneal dialysis complicated by Aureobasidium pullulans peri-tonitis. Am. J. Nephrol. 15:353–355.
15. Coldiron, B. M., E. L. Wiley, and M. G. Rinaldi. 1990. Cutaneous phaeohy-phomycosis caused by a rare fungal pathogen, Hormonema dematioides: successful treatment with ketoconazole. J. Am. Acad. Dermatol. 23:363–367. 16. Crompton, C. H., R. C. Summerbell, and M. M. Silver. 1991. Peritonitis with Paecilomyces complicating peritoneal dialysis. Pediatr. Infect. Dis. J. 10:869– 871.
17. Dalmau, L. M. 1929. Remarques sur la technique mycologique. Ann. Para-sitol. 7:536–545.
18. de Hoog, G. S., and J. Guarro. 1995. Atlas of clinical fungi. Centraalbureau voor Schimmelcultures, Baarn, The Netherlands.
19. de Hoog, G. S., and N. A. Yurlova. 1994. Conidiogenesis, nutritional physi-ology and taxonomy of Aureobasidium and Hormonema. Antonie Leeuwen-hoek 65:41–54.
20. De Saedeleer, B., J. Sennesael, P. Van der Niepen, and D. Verbeelen. 1994. Intraperitoneal fluconazole therapy for Trichosporon cutaneum peritonitis in continuous ambulatory peritoneal dialysis. Nephrol. Dial. Transplant
9:1658–1659.
21. DeVault, G. A., Jr., S. T. Brown 3rd., J. W. King, M. Fowler, and A. Oberle. 1985. Tenckhoff catheter obstruction resulting from invasion by Curvularia lunata in the absence of peritonitis. Am. J. Kidney Dis. 6:124–127. 22. Edwards, R., L. N. Birrell, and R. G. Finch. In vitro evaluation of antifungal
agents in the treatment of yeast peritonitis complicating continuous ambu-latory peritoneal dialysis (CAPD). 1987. Chemioterapia 6:3–7.
23. Espinel-Ingroff, A., K. Dawson, M. Pfaller, E. Anaissie, B. Breslin, D. Dixon,
A. Fothergill, V. Paetznick, J. Peter, M. Rinaldi, and T. Walsh.1995. Com-parative and collaborative evaluation of standardization of antifungal sus-ceptibility testing for filamentous fungi. Antimicrob. Agents Chemother.
39:314–319.
24. Fabris, A. M. V. Pellanda, C. Gardin, A. Contestabile, and R. Bolzonella. 1993. Pharmacokinetics of antifungal agents. Periton. Dial. Int. 13(Suppl.)2: S380–S382.
25. Fahhoum, J., and M. S. Gelfand. 1996. Peritonitis due to Penicillium sp. in a patient receiving continuous ambulatory peritoneal dialysis. South. Med. J.
89:87–88.
26. Fine, A., D. Churchill, H. Guult, and P. Furdy. 1983. Pityrosporum pachy-dermatis peritonitis in a CAPD patient on long term intraperitoneal antibi-otics. Periton. Dial. Bull. 3:108–109.
27. Flynn, J. T., D. Meislich, B. A. Kaiser, M. S. Polinsky, and H. J. Baluarte. 1996. Fusarium peritonitis in a child on peritoneal dialysis: case report and review of the literature. Periton. Dial. Int. 16:52–57.
28. Gadallah, M. F., R. White, M. A. el-Shahawy, F. Abreo, A. Oberle, and J.
Work.1995. Peritoneal dialysis complicated by Bipolaris hawaiiensis perito-nitis: successful therapy with catheter removal and oral itraconazole without the use of amphotericin B. Am. J. Nephrol. 15:348–352.
29. Garcia-Martos, P., J. Diaz, M. Castano, M. Perez, and P. Marin. 1991. Peritonitis caused by Candida lusitaniae in a patient on continuous ambula-tory peritoneal dialysis (CAPD). Clin. Nephrol. 36:50. (Letter.)
30. Geiss, H. K. 1995. Peritoneal aspergillosis—pitfalls in the diagnosis of a rare disease. Nephrol. Dial. Transplant 10:1124–1125.
31. Guarner, J., C. Del Rio, P. Williams, and J. E. McGowan, Jr. 1989. Fungal peritonitis caused by Curvularia lunata in a patient undergoing peritoneal dialysis. Am. J. Med. Sci. 298:320–323.
32. Hermanides-Nijhof, E. J. 1977. Aureobasidium and allied genera. Stud. My-col. 14:144–176.
33. Hernandez Jaras, J., L. Martinez-Martinez, J. L. Gallego, J. Fernandez
Fernandez, and J. Botella.1987. Geotrichum sp. as an agent of peritonitis in continuous ambulatory peritoneal dialysis (CAPD). Clin. Nephrol. 28:210. (Letter.)
34. Horisberger, J.-D., J. Bille, and J.-P. Waters. 1984. Fungal eosinophilic peritonitis due to Alternaria in a patient on continuous ambulatory peritoneal dialysis. Periton. Dial. Bull. 4:255–256.
35. Isenberg, E. S., B. E. Alpert, R. A. Weiss, N. Mittman, and R. Soeiro. 1983. Rhodotorula rubra peritonitis in patients undergoing continuous ambulatory peritoneal dialysis. Am. J. Med. 7755:349–352.
36. Johnson, A. S., E. Bailey, P. A. Wright, and L. Solomon. 1996. Malassezia furfur: a possible cause of culture-negative CAPD peritonitis. Periton. Dial. Int. 16:187–188.
37. Johnson, R. J., P. G. Ramsey, N. Gallagher, and S. Ahmad. 1985. Fungal peritonitis in patients on peritoneal dialysis: incidence, clinical features and prognosis. Am. J. Nephrol. 5:169–175.
38. Kerr, C. M., J. R. Perfect, P. C. Craven, J. H. Jorgensen, D. J. Drutz, J. D.
Shelburne, H. A. Gallis, and R. A. Gutman.1983. Fungal peritonitis in
patients on continuous ambulatory peritoneal dialysis. Ann. Intern. Med.
99:334–337.
39. Kitiyakara, C., A. Sakulsaengprapha, and S. Domrongkitchaiporm. 1966. The role of surgery and itraconazole in Aspergillus peritonitis in CAPD. Nephrol. Dial. Transplant 11:1498. (Letter.)
40. Loepky, C. B., R. F. Sprouse, J. V. Carlson, and E. D. Everett. 1983. Tricho-derma viride peritonitis. South. Med. J. 76:798–799.
41. Lopez, J. O., S. H. Alves, J. P. Benevenga, and A. C. Rosa. 1994. The second case of peritonitis due to Histoplasma capsulatum during continuous ambu-latory peritoneal dialysis in Brazil. Mycoses 37:161–163.
42. Lopez, J. O., S. H. Alves, J. P. Benevenga, O. R. Regio, and A. Calil. 1993. Histoplasma capsulatum peritonitis associated with continuous ambulatory peritoneal dialysis. Mycopathologia 122:101–102.
43. Lopez, J. O., S. H. Alves, J. P. Benevenga, F. B. Brauner, M. S. Castro, and
E. Melchiors. 1994. Curvularia lunata peritonitis complicating peritoneal dialysis. Mycopathologia 127:65–67.
44. Lye, W. C. 1993. Peritonitis due to Wangiella dermatitidis. Periton. Dial. Int.
13:319–320.
45. Ma, K. W. 1985. Disseminated histoplasmosis in dialysis patients. Clin. Nephrol. 24:155–177.
46. Mabee, C. L., S. W. Mabee, R. B. Kirkpatrick, and S. L. Koletar. 1995. Cirrhosis: a risk factor for cryptococcal peritonitis. Am. J. Gastroenterol.
90:2042–2045.
47. Mansoor, G. A., and D. B. Ornt. 1994. Cryptococcal peritonitis in peritoneal dialysis patients: a case report. Clin. Nephrol. 41:230–232.
48. Marzec, A., L. G. Heron, R. C. Pritchard, R. H. Butcher, H. R. Powell, A. P.
Disney, and F. A. Tosolini.1993. Paecilomyces variotii in peritoneal dialysate. J. Clin. Microbiol. 31:2392–2395.
49. McCarthy, D. I., A. W. Fothergill, D. A. Sutton, and M. G. Rinaldi. 1997. Possible misidentification of Hormonema dematioides which code as Crypto-coccus albidus on API 20C, abstr. F88, p. 275. In Abstracts of the 97th General Meeting of the American Society for Microbiology 1997. American Society for Microbiology, Washington, D.C.
50. Melez, K. A., J. Cherry, C. Sanchez, R. B. Ettinger, and T. J. Walsh. 1995. Successful outpatient treatment of Trichosporon beigelii peritonitis with oral fluconazole. Pediatr. Infect. Dis. J. 14:1110–1113.
51. Miles, A. M., and R. H. Barth. 1995. Aspergillus peritonitis: therapy, survival, and return to peritoneal dialysis. Am. J. Kidney Dis. 26:80–83.
52. Montenegro, J., R. Aguirre, O. Gonzales, I. Martinez, and R. Saracho. 1995. Fluconazole treatment of Candida peritonitis with delayed removal of the peritoneal dialysis catheter. Clin. Nephrol. 44:60–63.
53. Mydlik, M., E. Tkacova, K. Szovenyiova, P. Mizla, and K. Derzsiova. 1996. Saccharomyces cerevisiae peritonitis complicating CAPD. Periton. Dial. Int.
16:188.
54. Nagappan, R., J. F. Collins, and W. T. Lee. 1992. Fungal peritonitis in continuous ambulatory peritoneal dialysis: the Auckland experience. Am. J. Kidney Dis. 20:492–496.
55. Nakamura, M., W. B. Weil, Jr., and D. B. Kaufman. 1989. Fatal fungal peritonitis in an adolescent on continuous ambulatory peritoneal dialysis: association with deferoxamine. Pediatr. Nephrol. 3:80–82.
56. National Committee for Clinical Laboratory Standards. 1997. Reference method for broth dilution antifungal susceptibility testing of yeasts. Ap-proved standard M27-A. National Committee for Clinical Laboratory Stan-dards, Wayne, Pa.
57. Nguyen, M. H., and P. R. Muder. 1994. Aspergillus peritonitis in a continuous ambulatory peritoneal dialysis patient. Case report and review of the liter-ature. Diagn. Microbiol. Infect. Dis. 20:99–103.
58. Nielsen, H., J. Stenderup, B. Bruun, and J. Ladefoged. 1990. Candida nor-vegensis peritonitis and invasive disease in a patient on continuous ambula-tory peritoneal dialysis. J. Clin. Microbiol. 28:1664–1665.
59. O’Sullivan, F. X., B. R. Stuewe, J. M. Lynch, J. W. Brandsberg, T. B.
Wiegman, R. V. Patak, W. G. Barnes, and G. R. Hodges.1981. Peritonitis due to Drechslera spicifera complicating continuous ambulatory peritoneal dial-ysis. Ann. Intern. Med. 94:213–214.
60. Park, S. B., K. H. Kim, I. Joo, and H. C. Kim. 1996. Scanning electron microscopy studies of peritoneal catheter in CAPD peritonitis due to As-pergillus fumigatus. Periton. Dial. Int. 16:81–83.
61. Pennington, 3rd, J. C., K. Hauer, and W. Miller. 1995. Rhodotorula rubra peritonitis in an HIV1patient on CAPD. Del. Med. J. 67:184.
62. Pincus, D., M. Kemna, and I. Salkin. 1988. Modification of potassium nitrate assimilation test for identification of clinically important yeasts. J. Clin. Microbiol. 26:1300–1302.
63. Piraino, B., and R. J. Hamburger. 1995. Complicated multiorganism peri-tonitis. Periton. Dial. Int. 15:394–400.
64. Polo, J. R., J. Luno, C. Menarguez, E. Gallego, R. Robles, and P. Hernandez. 1989. Peritoneal mucormycosis in a patient receiving continuous ambulatory peritoneal dialysis. Am. J. Kidney Dis. 13:237–239.
65. Powel, D., E. San Luis, S. Calvin, R. McDaid, and D. Potter. 1985. Peritonitis in children undergoing continuous ambulatory peritoneal dialysis. Am. J. Dis. Child. 139:29–32.
66. Quindos, G., F. Cabrera, M. C. Arilla, A. Burgos, R. Ortiz-Vigon, J. L.
Canon, and J. Ponton.1994. Fatal Candida famata peritonitis in a patient
on May 15, 2020 by guest
http://jcm.asm.org/
undergoing continuous ambulatory peritoneal dialysis who was treated with fluconazole. Clin. Infect. Dis. 18:658–660.
67. Radix, A. E., V. M. Bieluch, and C. W. Graeber. 1996. Peritonitis caused by Monilia sitophila in a patient undergoing peritoneal dialysis. Int. J. Artif. Organs 19:218–220.
68. Rault, R. 1983. Candida peritonitis complicating chronic peritoneal dialysis: a report of five cases and review of the literature. Am. J. Kidney Dis.
2:544–547.
69. Remon, C., I. J. de la Calle, F. Vallejo Carrion, S. Perez-Ramos, and E.
Fernandez Ruiz. 1996. Exophiala jeanselmei peritonitis in a patient on CAPD. Periton. Dial. Int. 16:536–538.
70. Rex, J. H., M. A. Pfaller, J. N. Galgiani, M. S. Bartlett, A. Espinel-Ingroff,
M. A. Ghannoum, M. Lancaster, F. C. Odds, M. G. Rinaldi, T. J. Walsh, A. L. Barry, and Subcommittee on Antifungal Susceptibility Testing of the National Committee for Clinical Laboratory Standards.1997. Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro-in vivo correlation data for fluconazole, itraconazole, and Candida infections. Clin. Infect. Dis. 24:235–247. 71. Rippon, J. W., R. A. Larson, D. M. Rosenthal, and J. Clayman. 1988.
Disseminated cutaneous and peritoneal hyalohyphomycosis caused by Fusar-ium species; three cases and review of the literature. Mycopathologia 101: 105–111.
72. Sartin, J. S., M. P. Wilhelm, M. R. Keating, K. Batts, and R. A. Krom. 1994. A case of Aspergillus fumigatus peritonitis complicating liver transplantation. Eur. J. Clin. Microbiol. Infect. Dis. 13:25–28.
73. Struijk, D. G., E. W. Boeschoten, R. T. Krediet, and E. J. Kuijper. 1995. Fluconazole in Candida peritonitis in CAPD: an alternative proposal. Neph-rol. Dial. Transplant 10:426.
74. Sutton, D. A., A. W. Fothergill, and M. G. Rinaldi. 1998. Guide to clinically significant fungi. Williams & Wilkins, Baltimore, Md.
75. Tanis, B. C., C. A. Verburgh, J. W. van’t Wout, and J. W. van der Pijl. 1995. Aspergillus peritonitis in peritoneal dialysis: case report and a review of the literature. Nephrol. Dial. Transplant 10:1240–1243.
76. Tanis, B. C., C. A. Verburgh, J. W. van der Pijl, and J. W. van’t Wout. 1996. Aspergillus peritonitis in peritoneal dialysis. Nephrol. Dial. Transplant 11: 752. (Letter.)
77. Tanis, B. C., H. Van der Pijl, M. L. van Ogtrop, R. E. Kibbelaar, and P. C.
Chang.1995. Fatal fungal peritonitis by Trichoderma longibrachiatum com-plicating peritoneal dialysis. Nephrol. Dial. Transplant 10:114–116. 78. Tapson, J. S., H. Mansy, R. Freeman, and R. Wilkinson. 1986. The high
morbidity of CAPD fungal peritonitis—description of 10 cases and review of treatment strategies. Q. J. Med. 61:1047–1053.
79. Tsoufakis, G. E., C. E. Iatrou, M. Petropoulou, S. C. Zerbala, H. S.
Vayia-kou, C. A. Polychronopoulou, and P. N. Ziroyanis.1995. Aspergillus fumiga-tus peritonitis in a patient on CAPD. Periton. Dial. Int. 15:184–185. 80. Ujhelyi, M. R., R. H. Raasch, C. M. van der Horst, and W. D. Mattern. 1990.
Treatment of peritonitis due to Curvularia and Trichosporon with amphoter-icin B. Rev. Infect. Dis. 112:621–627.
81. Vincent, F., T. A. Bensousan, and B. Leclercq. 1995. Fungal peritonitis complicating continuous ambulatory peritoneal dialysis: use of high dosages of fluconazole or solely removal of the catheter? Nephrol. Dial. Transplant
10:141–142.
82. Yinnon, A. M., A. Solages, and J. J. Treanor. 1993. Cryptococcal peritonitis: report of a case developing during continuous ambulatory peritoneal dialysis and review of the literature. Clin. Infect. Dis. 17:736–741.
![FIG. 3. Macroscopic morphology of H. dematioides on SDA (1 week [A], 2weeks [B], and 3 weeks [C]; 25°C).](https://thumb-us.123doks.com/thumbv2/123dok_us/8226564.823912/3.612.50.289.69.602/fig-macroscopic-morphology-dematioides-sda-week-weeks-weeks.webp)
