Improving care for people with dementia: development and initial feasibility study for evaluation of life story work in dementia care
331
0
0
Full text
Figure
+7
Outline
Conclusions
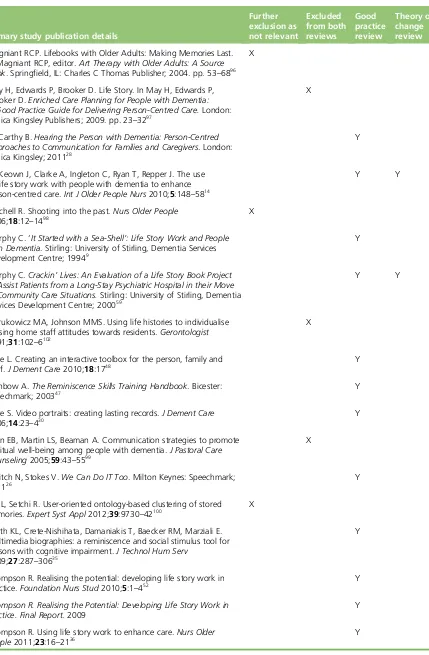
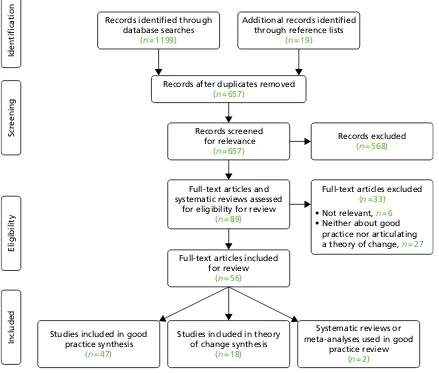
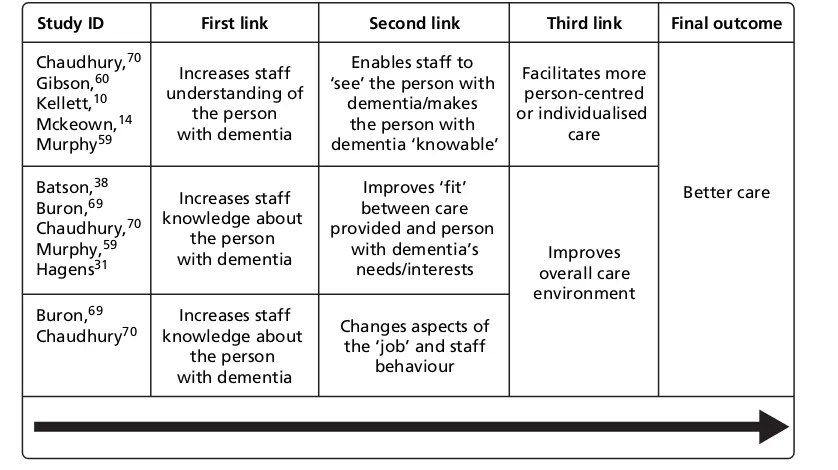
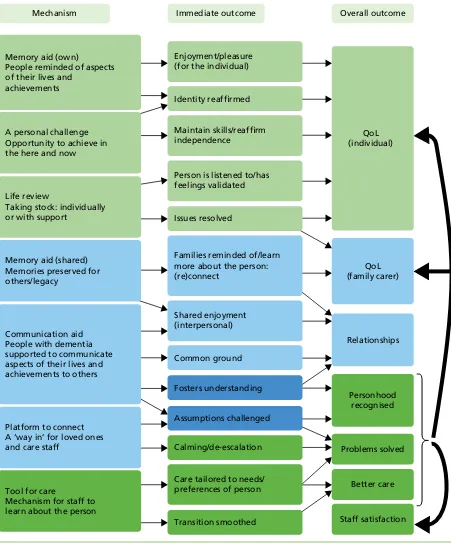
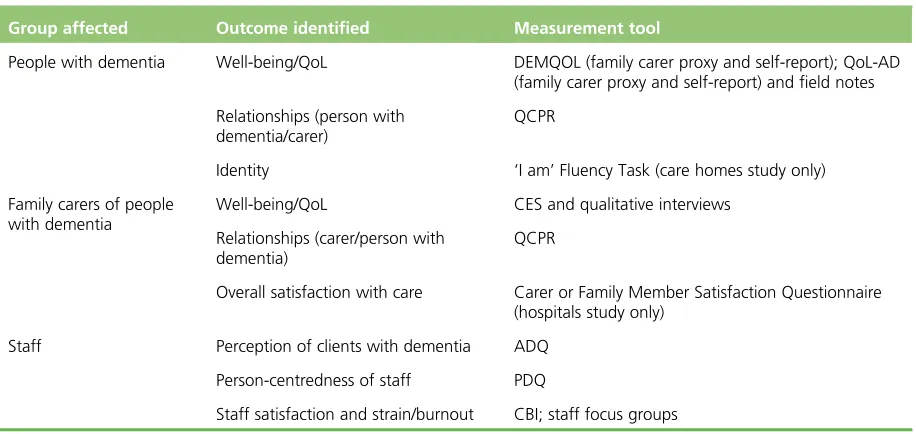
Data synthesis
Life story work outcomes, challenges and good practice: findings from the focus groups
Exploring feasibility
Findings of the feasibility studies
The costs of life story work
Doing life story work in care homes and hospitals: findings from qualitative interviews
Acceptability of the research
Discussion of findings
Strengths and limitations
Related documents