55 Int J Res Med. 2015; 4(2);55-60 e ISSN:2320-2742 p ISSN: 2320-2734
Combination of Low Dose Isobaric Levobupivacaine 0.5% and Fentanyl
Compared With Isobaric Levobupivacaine 0.5% in Spinal Anaesthesia for
Lower Abdominal and Perineal Surgeries
Nimisha P. Brahmbhatt1*, Ila A. Prajapati2,M. R. Upadhyay3
1Associate Professor,2Ex Resident, 3Professor &Head of Department, Dept. of Anaesthesia, S.S.G. Hospital, Medical College, Vadodara
INTRODUCTION
Spinal anaesthesia is popular & commonly used worldwide. The advantages of an awake patient, minimal drug costs and rapid patient turnover has made this the method of choice for many surgical procedures including lower abdominal and perineal surgeries .1,2
As practice of medicine focuses increasingly on outpatient care,spinal anaesthetics should provide short acting and adequate anaesthesia without compromising early ambulation and discharge from day care surgery unit. However, spinal anaesthesia for ambulatory lower abdominal and perineal surgeries is more complicated (Kehlet et al 2003).3 A higher level of sensory block is
*Corresponding Author:
Dr. Nimisha P. Brahmbhatt B/2, Saikrupa Society, Near Sangam char rasta,
Harni Road, Fatehpura post office, Vadodara -390006 Gujarat India No. -09428764477
Email-nimishabrahmbhatt7@gmail.com
required but increasing the dose of long acting local anaesthetics may produce extensive sensory and motor block as well as arterial hypotention and this might result in delayed discharge from hospital. (Korhonen et al 2006). 1,4
At the same time ,short acting spinal anaesthesia with minimum motor block can be useful and assumed that recovery and mobilization of the patient could be faster, if the motor block is less intense. For this purpose, short acting or low doses of local anaesthetics can be used. (Kararmaz A et al 2003, Kuusniemi et al 2000). 5,6
Levobupivacaine is the S(-) enantiomer of racemic bupivacaine. Levobupivacaine has similar efficacy but an enhanced safety profile when compared to bupivacaine, a major advantage in regional anaesthesia.
7-9
Intrathecal opioids added to local anaesthetics enhance analgesia without intensifying motor and sympathetic block, and make it possible to achieve successful anaesthesia in spite of the use of a low dose local anaesthetic. 5,10-12
ORIGINAL ARTICLE
ABSTRACT
BACKGROUND: The aim of study was to evaluate the effects of fentanyl added to low dose levobupivacaine on sensory & motor blockade characteristics, post operative analgesia & complications if any. MATERIAL AND METHODS: A prospective randomised double blind study was conducted in 64 ASA grade I-II patients undergoing lower abdominal & perineal surgeries ,Group L(n=32) received intrathecal levobupivacaine 2 ml(10 mg) and normal saline 0.5 ml , Group LF (n=32) recieved levobupivacaine 1.5 ml (7.5mg) with fentanyl 0.5 ml(25g.) and normal saline 0.5 ml (total 2.5 ml in each ).Patients were assessed for sensory & motor block characteristics, period of analgesia, Time to ambulation & urination. RESULTS: Both groups were comparable in terms of onset and peak effects of sensory & motor blockade. Two segment regression times in Group LF (71.87 ± 7.49 mins) was shorter than Group L (77.5 ±5.76 mins). Duration of motor block in Group LF (170.62±16.05 mins) was shorter than Group L (190.62±17.58 mins). Duration of Effective Analgesia in Group LF (220.62±16.25 mins) was prolonged compared to Group L (185.65 ± 6.44 mins). Time to Ambulation in Group LF (242.5±16.26 mins) was shorter than Group L(336.25 ± 31.49 mins). Time to first voiding of urine in Group LF (265.62±20.46 mins) was shorter than Group L (365.93 ± 29.49 mins). CONCLUSION: We conclude that combination of intrathecal FENTANYL with low dose LEVOBUPIVACAINE provides good surgical anaesthesia but early motor recovery which is well suited for outpatient anaesthesia.
56 Int J Res Med. 2015; 4(2);55-60 e ISSN:2320-2742 p ISSN: 2320-2734
In this study, we aimed to identify whether low dose of intrathecal levobupivacaine with fentanyl provides adequate surgical conditions as compared to intrathecal levobupivacaine alone without prolonging recovery for lower abdominal and perineal surgeries.
MATERIALS AND METHODS
The study was conducted at S.S.G. Hospital, Medical College, and Vadodara during period of January 2014 to October 2014 after obtaining ethical committee approval. After obtaining written & informed consent from the patients , a prospective , randomized , double - blind study was conducted on 64 patients of ASA I &II aged between 18-60 years of either sex scheduled for planned lower abdominal & perineal surgeries.
Exclusion Criteria:
1) Patients with allergy to local anaesthetics
2) Patients with history of drug or alcohol/ opioid abuse
3) Local infection in lumbar region 4) Morbid obesity (BMI>35 kg/ square
metre)
5) Patients with neurological disease, psychiatric illness ,epilepsy in past 6) Bleeding disorders /patients on
anticoagulants
7) Refusal and /or unable to give consent The procedure was explained to the patients. After taking the patient on operation table, an intravenous line was taken up using 18 G intracath & preloading was done with Inj. Ringer Lactate 10ml/kg IV . Blood pressure cuff, pulse oximeter and ECG electrodes were applied. The inital pulse, blood pressure, respiratory rate and oxygen saturation were noted. Premedication was given in form of Inj. Glycopyrrolate 0.2 mg IV, Inj. Ranitidine 50 mg IV & Inj. ondensetron 4mg IV.
Patients were randomly grouped in to Group L: Inj. Levobupivacaine 0.5% isobaric 2ml (10 mg) +Inj. Normal Saline 0.5 ml = 2.5 ml drug solution
Group LF: Inj. Levobupivacaine 0.5% isobaric 1.5 ml (7.5mg) + Inj. Normal Saline 0.5 ml+ Inj. Fentanyl 0.5ml (25 mcg)= 2.5 ml drug solution
The drug solution was prepared by another anaesthesiologist. Monitoring was done by the observer blinded to the identity of the drug given. Patient was placed in left lateral position for spinal anaesthesia. Under all aseptic and antiseptic precautions, painting and draping of the lumbo-sacral area was done. After skin infiltration with 2% Lignocaine, 23g spinal needle was inserted in L3/4 inter vertebral space. Correct needle placement was identified by free flow of CSF and then 2.5ml of study drug solution was injected over 10 seconds. Patient was turned to supine position soon after the injection. Surgery was started after establishment of block adequate for surgery.
Assessment of sensory block was done by using pin prick method . Sensory blockade was assessed every 1 min for 5 mins , every 5 mins for 30 mins and then every 30 min till end of surgery. Onset of sensory blockade at L1 level (in min) , highest sensory level achieved , time to achieve highest sensory level, two segment regression time & time for regression up to L1 from highest sensory level were recorded .
Motor block was assessed using bromage scale (Grade 0 - No motor block
Grade I - Unable to flex hip, Grade II - Unable to flex knee, Grade III- Unable to flex ankle). Onset of motor block, maximum motor block achieved, time to achieve maximum motor block (time interval from intrathecal injection to achievement of maximum motor block), duration of motor block (time interval from onset of motor block to regression of motor block to BROMAGE Grade 0) were recorded.
Vital Parameters like pulse rate, blood pressure and oxygen saturation were monitored. Recordings were done before giving the block and then at 1, 3,5, 10 and 15 minutes after giving spinal anaesthesia and then every 15 minutes till the end of surgery.
57 Int J Res Med. 2015; 4(2);55-60 e ISSN:2320-2742 p ISSN: 2320-2734
form of Inj Diclofenac Sodium 1.5mg/kg IM. Time to ambulation (time interval from intrathecal injection to first getting out of bed without assistance.) and time to first voiding of urine ( time interval from intrathecal injection to first spontaneous voiding of urine) were recorded.
Patients were monitored for various perioperative complications like bradycardia (defined as pulse rate less than 20% of pre procedure value or <50 beats/min. It was treated with Inj Atropine 0.6mg iv.), hypotension (Systolic blood pressure less than 20% of pre procedure value or <80 /60mmhg was considered as hypotension and was treated with IV fluids, oxygen and Inj. Ephedrine 5mg IV Bolus.), respiratory depression( decrease in respiratory rate <10 / min or SpO2 to less than 90% was defined as hypoxia and treated with supplemental oxygen if required. ) nausea and vomiting , pruritus & urinary retention .
All qualitative data were analyzed using Chi Square test and quantitative data using the Student’s t-test. Results were expressed as Mean ± SD. ‘p’ value <0.05 was taken as statistically significant. ‘ p’ value <0.01 was taken as highly significant.
RESULTS
Table: 1 Demographic Data
Parameters GROUP LF (Mean ± SD)
GROUP L (Mean ± SD)
p value
AGE (years) 44.46±8.91 45.5±9.38 >0.05 SEX
(Male: Female)
30:2 30:2 >0.05
WEIGHT (kg) 52.62±7.34 53.64±7.31 >0.05 ASA I ASA II 20 12 1814 >0.05 DURATION
OF SURGERY (mins)
57.96±15.07 57.5±11.84 >0.05
Table: 2 Assessment of Sensory Block
Parameters GROUP LF (MEAN±SD)
GROUP L (MEAN±SD)
p value
Onset of sensory
block (mins) 1.71 ± 0.52 1.72 ±0.53 >0.05 Highest sensory
level achieved T10:T8:T68:20:4
T12:T10:T8 2:12:18 >0.05 Time to achieve
highest sensory level(mins)
4.26±0.97 4.28±1.31 >0.05
Two segment regression time(min)
71.87 ± 7.49 77.5 ± 5.76 <0.01
Time for regression upto L1 level(min)
134.34 ± 9.13 145.62 ± 9.73 P<0.001
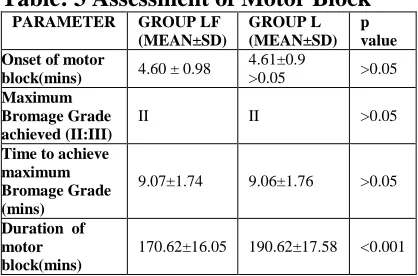
Table: 3 Assessment of Motor Block
PARAMETER GROUP LF (MEAN±SD)
GROUP L (MEAN±SD)
p value Onset of motor
block(mins) 4.60 ± 0.98
4.61±0.9
>0.05 >0.05
Maximum Bromage Grade achieved (II:III)
II II >0.05
Time to achieve maximum Bromage Grade (mins)
9.07±1.74 9.06±1.76 >0.05
Duration of motor block(mins)
170.62±16.05 190.62±17.58 <0.001
Table 1 show that there was no statistically significant difference among two groups in terms of demographic data.
Table 2 shows that onset of sensory block & times to achieve highest sensory level were comparable between two groups. The Time taken for two segment regression of level was 71.87 ± 7.49 minutes in Group LF as compared to 77.5 ±5.76 minutes in Group L. Thus it was shorter in group LF than in group L and the difference was statistically highly significant. ( p <0.01).Regression time to L1Level was 134.34 ± 9.13 minutes in Group LF, whereas it was 145.62 ± 9.73 minutes in Group L. Thus it was shorter in group LF than in group L and the difference was statistically highly significant. (p<0.001) Table 3 shows that onset of motor block, maximum Bromage grade achieved and time to achieve it were comparable between two groups. However, the duration of motor block was 170.62±16.05 minutes in Group LF, while it was 190.62±17.58 minutes in Group L. Thus it was shorter in group LF than Group L and the difference was statistically highly significant ( p < 0.001).
Graph:1Duration of Effective Analgesia
58 Int J Res Med. 2015; 4(2);55-60 e ISSN:2320-2742 p ISSN: 2320-2734
Graph 1 shows that, the duration of effective analgesia was 220.62±16.25 minutes in group LF and that in group L was 185.65 ± 6.44 minutes. Thus it was significantly longer in Group LF than Group L. The difference was statistically highly significant (p<0.001)
Graph 2 shows that, time to Ambulation was 242.5±16.26 minutes in group LF and that in group L was 336.25 ± 31.49 minutes. Thus it was significantly shorter in Group LF than Group L. The difference was statistically highly significant (p<0.001).
Time to first voiding of urine was 265.62±20.46 minutes in group LF and that in group L was 365.93 ± 29.49 minutes. Thus it was significantly shorter in Group LF than Group L. The difference was statistically highly significant (p<0.001).
Haemodynamic parameters were comparable between two groups.
In Group LF total 4 patients while in Group L total 10 patients requiring rescue analgesia. Thus it was significantly less in Group LF than Group L. The difference was statistically highly significant ( p<0.001).
Perioperatively, in group LF, 2 patients had bradycardia, 4 patients had hypotension and 3 patients had nausea/vomiting and 3 patients had pruritus. While in group L, 2 patients had bradycardia, 5 patients had hypotension and 2 patients had nausea/vomiting and no pruritus was seen in any patient.
DISCUSSION
In recent years, efforts have been made to improve spinal anaesthetic technique for ambulatory surgery by reducing the dose of local anaesthetic and introducing the use of additional spinal opioids to improve pain relief.11
The ideal agent for Day Care Anaesthesia is the one which when injected intrathecally would produce a rapid onset of a reliable block providing adequate surgical anaesthesia of appropriate duration and followed by a rapid regression of the motor and sensory block with minimal side-effects or residual effects. Levobupivacaine is a novel local anaesthetic which is S enantiomer of
bupivacaine and reported to have less frequent cardiovascular and central nervous system side effects. An up and down sequential study design recommends a minimum effective local anaesthetic dose of levobupivacaine is 11.7 mg. Smaller doses (5-10mg) have been used in ambulatory surgery allowing a more rapid recovery and early discharge to home (Breebart et al 2003, Capelleri et al 2005).9,16 By using low dose of levobupivacaine, one can limit the distribution of spinal block but could not provide an adequate level of sensory block.( Kararmaz A et al 2003).5
59 Int J Res Med. 2015; 4(2);55-60 e ISSN:2320-2742 p ISSN: 2320-2734
both groups, but the density and duration of motor block were more in bupivacaine group.5Ben -David et al found that a small dose of fentanyl (10µg) added to dilute bupivacaine (3ml of 0.17% solution)in ambulatory patients undergoing knee arthroscopies intensified and increased the sensory block without increasing the intensity of motor block or prolonging recovery.10 Lee et al used 2.6 ml 0.5% levobupivacaine alone and 2.3 ml 0.5% levobupivacine with 15µg fentanyl for TURP surgery. They found no difference between characteristics of motor and sensorial block. 15 Although Lee et al found that highest level of sensory block was similar between two groups, in our study, however the combination of levobupivacaine with fentanyl reached a higher level of sensory block. The resolution of motor block was faster in this combination group than in the levobupivacaine group. Low dose local anaesthetic used in levobupivacaine with fentanyl group, offered the advantage of shorter duration of motor block. The clinical significance of a reduced duration of motor block resulting from lower dose levobupivacaine plus fentanyl would be early ambulation. Basar et al found that levobupivacaine plus fentanyl solution is more hypobaric than the pure levobupivacaine solution. Opioids such as fentanyl are hypobaric when added to a local anaesthetic will render the subsequent mixture even more hypobaric.12 Parlow et al stated that the addition of opioids to isobaric local anaesthetics alters the density of the resulting solutions, as well as the direction and extent of spread in a spinal model.17 We also found higher level of sensory block in LF group due to hypobaricity of resultant mixture.
Pruritus was the most common adverse effect in patients who received intrathecal fentanyl as reported by N K Girgin et al, Kararmaz et al. & Borazen et al.1,5,14 We get pruritus in 3 patients of group LF related to addition of opioid which does not require any treatment.
In conclusion, Combination of intrathecal FENTANYL 25µg with low dose LEVOBUPIVACAINE 7.5 mg provides
good quality surgical anaesthesia but early motor recovery with extended period of analgesia which is well suited for outpatient anaesthesia.
REFERENCES
1.NK Girgin, A Gurbet, G Turker,T Bulut, S Demir, & A Cinar. The combination of low dose levobupivacaine and fentanyl for spinal anaeshesia in ambulatory inguinal herniorraphy. The Journal of International Medical Research: 2008; 36:1287-1292.
2.Gupta A, Axelsson K, Thorn SE, et al.: Low dose bupivacaine plus fentanyl for spinal anaesthesia during ambulatory inguinal herniorrhaphy: a comparison between 6 mg and 7.5mg bupivacaine. Acta Anaesthesiology Scand 2003;47:13-9
3.Kehlet H, Niesen M: Anaesthetic practice for groin hernia repair - a nation wide study in Denmark 1998-2003.Acta Anaesthesiology Scand 2005;49:143-146
4.Korhonen AM: Use of spinal anaesthesia in day surgery. Curr Opin Anaesthesiology 2006;19: 612-616. 5.Kararmaz A Kaya S, Turhanoglu S,
Ozyilmaz MA.Low dose bupivacaine and fentanyl in spinal anaesthesia for transurethral prostatectomy. Anaesthesia: 2003:58(6); 526-530.
6.Kuusniemi KS, Pihlajamakin KK, Pitkanen MT, Helenius HY, Kirvela OA: The use of bupivacaine and fentanyl for spinal anaesthesia for urologic surgery. Anaesth Analog;2000,91:1452-6.
7.Mcleod GA, Burke D: Levobupivacaine. Anaesthesia; 2001, 56(4):331-41
8.Casati A, Moizo E, Marchetti C, Vinciguerra F. A prospective, randomized, double-blind comparison of unilateral spinal anesthesia with hyperbaric bupivacaine, ropivacaine, or levobupivacaine for inguinal herniorrhapy. AnesthAnalg 2004; 99:1387-92.
60 Int J Res Med. 2015; 4(2);55-60 e ISSN:2320-2742 p ISSN: 2320-2734
between lidocaine, ropivacaine , and levobupivacaine . Br. J. Anaesth 2003; 90: 309-313
10. Ben -David B, Solomon E , Levin H , Admoni H, Goldik Z : Intrathecal fentanyl with small dose dilute bupivacaine: better anaesthesia without prolonging recovery. Anaesth Analog 1997, 85: 560-65
11. Ben-David B, Frankel R, Arzumonov T, Marchevsky Y, Volpin G : Mini dose bupivacaine - fentanyl spinal anaesthesia for surgical repair of hip fracture in the aged. Anaesthesiology ; 2000, 92 :6-10
12. Cuvas O, Basar H, Yeygel A,Turkyilmaz E, Sunay MM. Spinal anaesthesia for transurethral resection operations: Levobupivacaine with or without fentanyl. Middle East j Anaesth 2010; 20:547-552.
13. Erkan Yavuz Akcaboy,Zeynep Nur Akcaboy,Nermin Gogus. Low dos levobupivacaine 0.5%with fentanyl in spinal anaesthesia for transurethral resection of prostate surgery. Journal
of Research in Medical Science :2011;16(1): 68-73
14. Hale Borazen, Isil Davarci, Ahmet Kececiaglu, Seref Otelcioglu. The effects of low dose levobupivacaine with or without sufentanil intrathecally in trans urethral resection of prostate. European J. Gen Med:2011;8(2) : 134-40
15. Lee.y.y.k,. Manchal,C K Chan& A.S.P. Chaung. Levobupivacaine and fentanyl for spinal anaesthesia :A Randomised Trial. European Journal of anaesthesiaology. 2005: 12;899-903. 16. Cappelleri G, Aldegheri G, Danelli G,
et al. Spinal anesthesia with hyperbaric levobupivacaine and ropivacaine for outpatient knee arthroscopy: a prospective, randomized, double-blind study. Anesth Analg 2005; 101:77-82. 17.