The Impact of Opioids on the Endocrine System
By NA T H A N I E L KA T Z, M D , M S
“[Opium] has kept, and does now keep down the population: the women have fewer children than those of other countries… the feeble opium-smokers of Assam… are more effeminate than women.”
– Charles Alexander Bruce, “Report on the Manufacture of Tea and on the extent and produce of the tea plantations in Assam,” Calcutta, 1839. Opioids have been used for medicinal and analgesic purposes for millennia and today remain a critical part of the medical armamentarium against pain, diarrhea, cough, and other symptoms. Unfortunately, while barely discussed in the modern medical lexicon, opioids have negative effects on the endocrine system that have been observed for at least a century. These effects (Table 1) include decreased testosterone, with loss of libido and other expected effects, in men, and menstrual irregularities and infertility in women. In view of the increased use of opioids for chronic pain, it has become increasingly important to recognize and manage their endocrine complications.
PHYSIOLOGY OF OPIOID-ENDOCRINE INTERACTIONS
The hypothalamic-pituitary-gonadal process of controlling the secretion of gonadal hormones, testosterone, and estrogen, begins with secretion by the hypothalamus of gonadotropin-releasing hormone (GNRH) (Figure 1). GNRH stimulates the pituitary gland to secrete luteinizing hormone (LH) and follicle stimulating hormone (FSH). These two hormones are released into the systemic circulation and interact with the gonads, the testes and ovaries, to secrete testosterone or estrogen, respectively. These sex hormones then feed back to the hypothalamus and pituitary to form a com-plete feedback loop. Testosterone and estrogen support normal sexual and reproductive growth and behavior.
This system is modulated by a complex series of outside influences as well. Opioids are one of a number of such influences and evidence suggests that opioids – both endogenous and exogenous – can bind to opioid receptors primarily in the hypothalamus, but potentially also in the pituitary and the testes, to modulate gonadal function.1-6
Decreased release, or interference with the normal pulsatility of release of GNRH at the level of the hypothalamus, has been documented, with conse-quent decreased release of LH and FSH from the pituitary. Direct effects of opioids on the testes, including decreased secretion of testosterone and testicular interstitial fluid, have been docu-mented.7
Finally, opioids have been shown to increase pituitary release of prolactin in preclinical studies,8
with secondary effects of decreasing testosterone secretion (although, as indicated below, prolactin secretion is generally not affected in clinical studies).
ENDOCRINE CONSEQUENCES OF OPIOID USE
Investigations in animals have demonstrated the acute and chronic effects of opioids on the endocrine system,9including decreasing testosterone levels by central reductions of LH release (decreased hypothalamic release of luteinizing-hormone releasing hormone (LHRH), leading to reduced pituitary release of LH), and peripheral effects on the testicle as well.10-15
Studies in heroin
M G H PA I N C E N T E R
Jane C. Ballantyne, M.D.Chief, Division of Pain Medicine Editor, Pain Management Rounds Salahadin Abdi, M.D., Ph.D. Director, MGH Pain Center Martin Acquadro, M.D., D.M.D. Director of Cancer Pain Service Steve Barna, M.D.
Medical Director, MGH Pain Clinic Gary Brenner, M.D., Ph.D. Director, Pain Medicine Fellowship Lucy Chen, M.D.
Katharine Fleischmann, M.D. Director, Acute Pain Service Jatinder Gill, M.D. Karla Hayes, M.D.
Eugenia-Daniela Hord, M.D. Ronald Kulich, Ph.D. Jianren Mao, M.D., Ph.D. Director, Pain Research Group Seyed Ali Mostoufi, M.D.
Anne Louise Oaklander, M.D., Ph.D. Director, Nerve Injury Unit
Director, Center for Shingles and Postherpetic Neuralgia Gary Polykoff, M.D. Milan Stojanovic, M.D. Director, Interventional Pain Management MGH PAIN CENTER
15 Parkman Street, Suite 324 Boston, MA 02114
Fax : 617-724-2719
The editorial content of Pain Management Roundsis determined solely by the MGH Pain Center, Massachusetts General Hospital.
MGH 1811
MASSACHUSETTS GENERAL HOSPITAL
Pain Management Roundsis approved by the Harvard Medical School Department of Continuing Education to offer continuing education credit
F R O M G R A N D R O U N D S A N D O T H E R C L I N I C A L C O N F E R E N C E S O F T H E M G H P A I N C E N T E R , M A S S A C H U S E T T S G E N E R A L H O S P I T A L
2005 Volume 1, Issue 9
addicts, compared to healthy controls, have demonstrated decreased testosterone levels in males, with an associated decrease in LH and/or FSH consistent with central hypogo-nadism.7,16-21In one study measuring hormonal status one month after cessation of heroin use, testosterone levels returned to normal.21
In methadone-maintained male patients, several studies have demonstrated decreased testos-terone levels consistent with central hypogonadism. One of these studies20
demonstrated a dose-response effect, in that patients on “low dose” methadone (10-60 mg/day) had no evidence of suppression compared with those on “high dose” (80-150 mg/day). The second study7demonstrated a periph-eral effect on the testicle, with decreased secretion of testos-terone and testicular interstitial fluid, and decreased sperm motility. One case series described amenorrhea and galactor-rhea in female heroin addicts.22
Several studies have compared patients undergoing intrathecal opioid treatment for nonmalignant pain with patients with a comparable pain syndrome, but not on opioid therapy. These studies have documented hypogonadism associated with low LH values and normal or low FSH levels in both males and females.23-28
When compared to the chronic pain control group, these laboratory findings were associated with decreased libido or impotence in males and irregular or absent menses in females. Interestingly, in one study, 15% of patients developed hypocorticism and 15% growth hormone deficiency.23
Although one patient with hypocorticism developed an Addisonian crisis, the clinical consequences of low cortisol observed in several studies of opioid therapy have not been confirmed in controlled stud-ies. Symptoms were reported to have improved in most patients with hormone supplementation. None of these studies reported elevation of prolactin levels, suggesting that prolactin is not significantly related to the mechanism by which opioids produce hypogonadism.
Three studies have been published on the effects of long-term oral opioid therapy in males with chronic pain.
•In the first,29
endocrine function was measured in 54 patients on sustained-release opioids and compared to 27 healthy controls. Hormone levels were much lower in opioid users than in control subjects in a dose-related pattern (P<0001 for all comparisons) and total testosterone levels were subnormal in 74% of the opioid group, with an appar-ent dose-response effect. Eighty-seven percappar-ent (39 of 45) of the opioid-ingesting men who reported normal erectile func-tion before opioid use, reported severe erectile dysfuncfunc-tion or diminished libido after beginning opioid therapy.
•The second study30
was a case series in cancer survivors with chronic pain taking opioids who had abnormally low testosterone levels. This was confirmed with a follow-up case-control study31 comparing 20 cancer survivors on opioids to 20 matched controls. Among the opioid group, 18/20 (90%) exhibited hypogonadism, compared to 8/20 controls (40%) (median testosterone levels were statistically significantly lower in the opioid group). LH, but not FSH levels, were statistically significantly lower in the cases. Importantly, clinically significant consequences of these lab-oratory abnormalities were also demonstrated. Sexual desire (measured by the Sexual Desire Inventory); anxiety and depression (measured by the Hospital Anxiety and Depres-sion Scale); and overall quality of life (measured by the Func-tional Assessment of Chronic Illness Therapy with general and fatigue subscales [FACT-G/FACIT-F]) were all signifi-cantly lower in the opioid group than in the controls.
•An unpublished study32
also compared endocrine status in male patients on opioid therapy to healthy controls and found that of 25 patients, 68% had either free or total testosterone values below the normal range. Among men over age 50, 87.5% had low free testosterone levels. Mean free and total testosterone and LH values were significantly lower than in normal controls. FSH and prolactin levels were normal.
TABLE 1:Endocrine effects of opioids
Cortisol deficiency Uncertain, ?Addisonian crisis Growth Hormone Uncertain
deficiency
The Hypothalamic-Pituitary-Gonadal Axis Hypothalamus Pituitary Testes Ovaries LHRH (GnRH) LH FSH + Testosterone Estrogen + _ _ LHRH = luteinizing-hormone releasing hormone GNRH = gonadotropin- hormone releasing hormone LH = luteinizing hormone FSH = follicle-stimulating hormone OPIOIDS _ _ _
FIGURE 1:Interactions between opioids and the
endocrine system Central hypogonadism •Decreased hypothalamic GNRH •Decreased pituitary LH, possibly FSH •Decreased testicular testosterone; ovarian estradiol •Decreased testicular interstitial fluid
•Loss of libido, impotence
•Infertility (males and females)
•Depression, anxiety, fatigue
•Loss of muscle mass and strength
•Amenorrhea, irregular menses, galactorrhea
ing testosterone suppression with increasing opioid doses. One study suggests that all opioids may not be alike in this regard. Two provocative studies, one in rats and one in women with AIDS wasting syndrome, suggest the possibility that decreased testosterone levels may be associated with increased pain. Opioids also appear to affect the endocrine system in other ways, including decreasing cortisol and growth hormone levels (Table 2).
DIAGNOSIS OF OPIOID-INDUCED ENDOCRINOPATHY
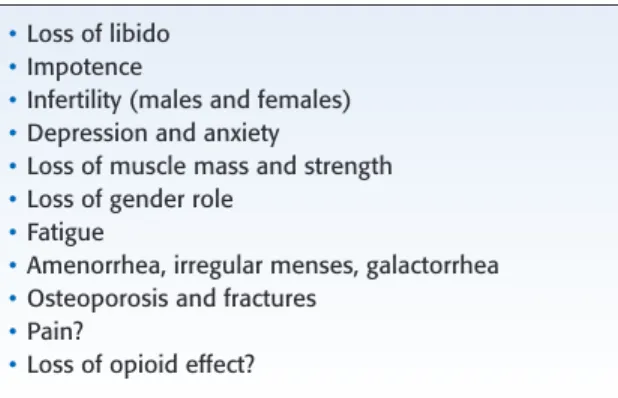
The signs and symptoms of hypogonadism are well known (Table 2), and include loss of sexual desire and per-formance, alterations in gender role, fatigue, mood alter-ations, loss of muscle mass and strength, abnormal menses, infertility, and finally, osteoporosis and fractures.31,41-43
Many of these symptoms are also widespread in patients with chronic pain.44-47 Therefore, it is unclear to what extent – on an epidemiologic basis – such symptoms in patients on opioids for chronic pain are due to opioid-induced hypogo-nadism or to chronic pain and its associated conditions. All patients with chronic pain on opioid therapy should be assessed prospectively for symptoms that could be potentially related to opioid-induced hypogonadism (Table 2).
While there are no available standards for laboratory monitoring of patients on opioids for chronic pain, the avail-able data suggest that endocrine monitoring should be rou-tine (Table 3). The usual laboratory studies include total testosterone, free testosterone (and/or sex hormone-binding globulin), estradiol, LH, and FSH. Monitoring of bone density should also be considered in at-risk patients, since patients with fractures associated with hypogonadism often have no other symptoms of hypogonadism.41
The diagnosis of hypogonadism is made by low levels of testosterone, with a customary cutoff of total (bound and free) testosterone <300 ng/dL. Whether hypogonadism in a patient on opioid therapy is due to opioids or some other cause becomes a pragmatic issue of whether any other causes of hypogo-nadism are present. If not; the presumptive diagnosis and
•A final study33
compared endocrine function in 17 men treated with buprenorphine for addiction, 37 men on high-dose methadone and 51 healthy blood donors served as controls. Patients treated with buprenorphine had signifi-cantly higher testosterone levels and a signifisignifi-cantly lower fre-quency of sexual dysfunction compared with patients treated with methadone. The testosterone level of buprenorphine-treated patients did not differ from that of the healthy controls. This is the first study to demonstrate the possibility that not all opioids may be alike in terms of endocrine effects, although it is not clear in this study that equivalent doses of methadone and buprenorphine were compared.
Interestingly, one preclinical study34
in rats demon-strated that reducing testosterone levels by castration signifi-cantly increased sensitivity to pain (as measured by two standard assays: tail flick and hot plate). This increase in pain sensitivity was reversed by testosterone supplementation. This raises the provocative possibility that in chronic pain patients on opioid therapy, opioid-induced hypogonadism – which occurs in a majority of male patients on opioids – could potentially have the undesirable effect of increasing pain sensitivity.
The only evidence addressing this hypothesis in humans is quite indirect. A randomized, placebo-controlled study35 of 53 female patients with AIDS wasting syndrome was con-ducted that compared transdermal testosterone to placebo. This syndrome is known to be associated with markedly decreased serum androgen levels. Pain scores were captured incidentally with the pain item on the SF-36 quality of life survey. A trend towards improved pain score (p = 0.059) was observed in 1 of the 2 testosterone treatment groups com-pared to placebo.
Several studies have examined the possibility of opioid-induced alterations of other endocrine functions. In general, it does not appear that opioids alter thyroid function in any meaningful way.36,37Opioids have been found in several studies to decrease cortisol levels, as well as cortisol responses to adrenocorticotropin (ACTH) challenges.23,38,39
The clinical significance of this is unclear. One study also documented decreased growth hormone secretion in the setting of opioid therapy, also of unclear significance. Hypogonadism from any cause may also affect serum lipid profiles, although the con-sistency and clinical importance of these effects is uncertain.40
In summary, a number of lines of evidence – including preclinical studies, heroin addiction, methadone mainte-nance – indicate that intrathecal and oral opioids in both cancer and non-cancer pain suppress testosterone secretion, primarily via central mechanisms (although a peripheral component may be important as well). This suppression appears to have important clinical consequences, including decreased sexual desire and performance, potentially increased anxiety and depression, and reduced quality of life. Some studies have found a dose-response effect, with
increas-TABLE 2:Symptoms of hypogonadism
•Loss of libido
•Impotence
•Infertility (males and females)
•Depression and anxiety
•Loss of muscle mass and strength
•Loss of gender role
•Fatigue
•Amenorrhea, irregular menses, galactorrhea
•Osteoporosis and fractures
•Pain?
management options point to opioids as the focus of attention.
MANAGEMENT OF OPIOID-INDUCED ENDOCRINOPATHY
There are no accepted standards for the manage-ment of presumptive opioid-induced hypogonadism. Therefore, clinical judgment must be relied upon. In patients who appear to have opioid-induced hypo-gonadism, several considerations will influence treat-ment decisions (Table 4).
The first issue is to determine to what extent the laboratory abnormalities are clinically important by assessing sexual function, mood, and the other symp-toms noted above. For patients with sympsymp-toms, or even laboratory abnormalities and unclear clinical status, the first question is whether to switch opioids. It is presently unknown if all opioids at equi-analgesic doses cause an equal degree of endocrine dysfunction. In some patients, opioid rotation is fairly straightforward and a reasonable first step. In others, such as those on high doses or who have failed multiple opioids, opioid rotation is difficult and testosterone supplementation will be more appropriate. Serum total (bound and free) testosterone concentrations <300 ng/dL are generally considered indicative of hypogonadism in men and the biochemical goal of hormone replacement therapy with testosterone is to increase serum total testosterone con-centrations to within the normal physiologic range of 300-1200 ng/dL.48-50
Several formulations of testosterone are available, including intramuscular injections, transdermal patches, and transdermal gel. Most of the clinical trial data and experience that have accumulated is with
intramuscular injections, but transdermal formulations are more acceptable to most patients. Therefore, a reasonable approach is to begin with a transdermal for-mulation and then switch to injections in patients who are unable to normalize testosterone levels with the transdermal formulations. It must be remembered that testosterone supplementation is not free of side effects, including local site reactions, sleep apnea, abuse and misuse, and various hematologic abnormalities, parti-cularly polycythemia. Oligospermia, priapism, male pattern baldness, and gynecomastia may occur in men, while menstrual irregularities and virilization may occur in women.
Perhaps the most worrisome side effect is the poten-tial for stimulation of growth, benign or otherwise, of the prostate gland. While exogeneous testosterone has not been firmly linked to the development of prostate cancer, patients must be monitored (rectal examinations and prostate specific antigen [PSA]) for such effects (Table 5). Similarly, the possibility of abnormalities in serum lipids should be monitored, although there are no definite links between testosterone supplementation and clinically significant lipid abnormalities.
CONCLUSIONS
Opioid-induced hypogonadism due to central suppression of hypothalamic secretion of GNRH is
TABLE 3:Diagnosis of opioid-induced
endocrinopathy Clinical evaluation
•Symptoms (Table 2) Laboratory evaluation
•Free and total testosterone, LH, FSH, estradiol
•Consider growth hormone, morning cortisol
•Consider bone densitometry
Rule-out other causes of central hypogonadism
•Idiopathic gonadotropin or gonadotropin-releasing hormone (luteinizing hormone releasing
hormone) deficiency •Pituitary-hypothalamic injury •Tumors •Trauma •Radiation Corticosteroid therapy
TABLE 4:Management of opioid-induced
hypogonadism Consider opioid rotation
Consider strategies that allow opioid dose reduction
•Concomitant non-opioid analgesics
•Non-pharmacologic modalities Testosterone supplementation
•Consider consultation with an endocrinologist
•Choose formulation and dose – Intramuscular injection – Transdermal patch – Transdermal gel
•Monitor prostate specific antigen (PSA) in males
•Monitor clinical and laboratory results
TABLE 5:Monitoring of patients on testosterone
supplementation
•Symptoms of hypogonadism
•Free and total testosterone, sex hormone binding globulin
•Rectal examinations and prostate specific antigen (PSA)
•Complete blood count
likely common in both male and female patients on long-term opioid therapy because of addiction or chronic pain. Potential symptoms include loss of libido, infertility, fatigue, depression, anxiety, loss of muscle strength and mass, alteration of gender role, osteoporo-sis, and compression fractures and, in men, impotence, and, in females, menstrual irregularities, galactorrhea, and infertility. Therefore, patients on opioid therapy should have routine screening for such symptoms, which may be difficult to distinguish from symptoms that are common in patients with chronic pain or addiction and for associated laboratory abnormalities. Patients with opioid-induced hypogonadism should probably undergo opioid rotation if this is likely to be straightforward. In patients who cannot easily be rotated or who have failed opioid rotation, testosterone supplementation should be offered after consideration of likely risks and benefits. Patients who undergo testos-terone supplementation require appropriate monitoring of both benefits and potential risks.
Dr. Nathaniel Katz is a Neurologist and Pain Manage-ment Specialist. He is currently Director, Pain and Opioid Research, Inflexxion, Inc. Between 1990 and 2001, Dr. Katz provided patient care at Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston. He has a longstanding interest in the use of opioids for acute and chronic pain, including their complications.
References
1. Cicero T. Effects of exogenous and endogenous opiates on the hypo-thalamic-pituitary-gonadal axis in the male. Fed Proc1980;39(8):2551-4. 2. Drolet G, Dumont EC, Gosselin I, Kinkead R, Laforest S, Trottier JF. Role of endogenous opioid system in the regulation of the stress response. Prog Neuropsychopharmacol Biol Psychiatry2001;25(4): 729-41.
3. Genazzani AR, Genazzani AD, Volpogni C, et al. Opioid control of gonadotrophin secretion in humans. Hum Reprod1993;8(Suppl 2): 151-3.
4. Grossman A, Moult PJ, Gaillard RC, et al. The opioid control of LH and FSH release: effects of a met-enkephalin analogue and naloxone. Clin Endocrinol(Oxf ) 1981;14(1):41-7.
5. Jordan D, Tafani JAM, Ries C, et al. Evidence for multiple opioid receptors in the human posterior pituitary. J Neuroendocrinol1996; 8:883-7.
6. Veldhuis JD, Rogol AD, Samojlik E, et al. Role of endogenous opiates in the expression of negative feedback actions of androgen and estrogen on pulsatile properties of luteinizing hormone secretion in man. J Clin Invest1984;74:47-55.
7. Cicero TJ, Bell RD, Wiest WG, Allison JH, Polakoski K, Robins E. Function of the male sex organs in heroion and methadone users. N Engl J Med1975;292(17):882-7.
8. Yen SSC, Quigley ME, Reid RL, et al. Neuroendocrinology of opioid peptides and their role in the control of gonadotropin and prolactin secretion. Am J Obstet Gynecol1985;152:485-93.
9. Pfeiffer A, Herz A. Endocrine actions of opioids. Horm Metab Res 1984;16(8):386-97.
10. Adams ML, Sewing B, Forman JB, Meyer ER, Cicero TJ. Opioid-induced suppression of rat testicular function. J Pharmacol Exp Ther 1993;266(1):323-8.
11. Cicero TJ, Meyer ER, Bell RD, et al. Effects of morphine on the secondary sex organs and plasma testosterone levels of rats. Res Commun Chem Pathol Pharmacol1974;7:17-24.
12. Cicero TJ, Wilcox CE, Bell RD, et al. Acute reduction in serum testo-sterone levels by narcotics in the male rat: stereospecificity, blockade by naloxone and tolerance. J Pharmacol Exp Ther1976;198:340-6. 13. Clark JT, Gabriel SM, Simpkins JW, et al. Chronic morphine and
testosterone treatment. Effects on sexual behaviour and dopamine metabolism in male rats. Neuroendocrinology1988;48:97-104. 14. Wiesenfeld-Hallin Z, Sodersten P. Spinal opiates affect sexual behavior
in rats. Nature1984;309:257-8.
15. Yilmaz B, Knoar V, Kutlu S, et al. Influence of chronic morphine expo-sure on serum LH, FSH, testosterone levels, and body and testicular weights in the developing male rat. Arch Androl1999 Nov-Dec 31;43(3):189-96.
16. Daniell HW. Narcotic-induced hypogonadism during therapy for heroin addiction. J Addict Dis2002;21(4):47-53.
17. Fachinetti F, Volpe A, Farci G, et al. Hypothalamus-pituitary-adrenal axis of heroin addicts. Drug Alcohol Depend1985;15:361-6. 18. Khan C, Malik SA, Iqbal MA. Testosterone suppression by heroin.
J Pak Med Assoc1990;40(7):172-3.
19. Malik SA, Khan C, Jabbar A, Iqbal A. Heroin addiction and sex hormones in males. J Pak Med Assoc1992 Sep;42(9):210-2. 20. Mendelson JH, Mendelson JE, Patch VD. Plasma testosterone levels in
heroin addiction and during methadone maintenance. J Pharmacol Exp Ther1975; 192(1):211-17.
21. Mendelson JH , Mello NK. Plasma testosterone levels during chronic heroin use and protracted abstinence. A study of Hong Kong addicts. Clin Pharmacol Ther 1975;17(5):529-33.
22. Pelosi MA, Sama JC, Caterini H, Kaminetzky HA. Galactorrhea-amenorrhea syndrome associated with heroin addiction. Am J Obstet Gynecol1974;118(7):996-70.
23. Abs R, et al. Endocrine consequences of long-term intrathecal adminis-tration of opioids. J Clin Endocrinol Metab2000;85(6):2215-22. 24. Doleys DM, Dinoff BL, Page L, et al. Sexual dysfunction and other
side effects of intraspinal opiate use in the management of chronic non-cancer pain. AJPM1998;8:5-11.
25. Finch PM, Roberts LJ, Price L, Hadlow NC, Pullan PT. Hypogo-nadism in patients treated with intrathecal morphine. Clin J Pain 2000;16(3):251-4.
26. Paice JA, Penn RD, Ryan WG. Altered sexual function and decreased testosterone in patients receiving intraspinal opioids. J Pain Symptom Manage1994;9:126-31.
27. Paice JA, Penn RD. Amenorrhea associated with intraspinal morphine. J Pain Symptom Manage1995;10:582-3.
28. Winkelmuller M, Minkelmuller W. Long-term effects of continuous intrathecal opioid treatment in chronic pain of nonmalignant etiology. J Neurosurg1996;85:458-67.
29. Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain2002;3(5):377-84.
30. Rajagopal A, Vassilopoulou-Sellin R, Palmer JL, Kaur G, Bruera E. Hypogonadism and sexual dysfunction in male cancer survivors receiv-ing chronic opioid therapy. J Pain Symptom Manage 2003;26(5):1055-61.
31. Rajagopal A, Vassilopoulou-Sellin R, Palmer JL, Kaur G, Bruera E. Symptomatic hypogonadism in male survivors of cancer with chronic exposure to opioids. Cancer2004;100(4):851-8.
32. Sherburne S, Adler G, Mutter G, Katz N. The effects of long-term opioid therapy on endocrine function in male patients with chronic pain. Submitted.
33. Bliesener N, Albrecht S, Schwager A, Weckbecker K, Lichtermann D, Klingmuller D. Plasma testosterone and sexual function in men on buprenorphine maintenance for opioid dependence. J Clin Endocrinol Metab 2005;(1):203-6.
34. Forman LJ, Forman LJ, Tingle V, Estilow S, Cater J. The response to analgesia testing is affected by gonadal steroids in the rat. Life Sci 1989;45(5):447-54.
35. Miller K, Corcoran C, Armstrong C, et al. Transdermal testosterone administration in women with acquired immunodeficiency syndrome wasting: a pilot study. J Clin Endocrinol Metab 1998;83(8):2717-25. 36. Chan V, Wang C, Yeung RT. Effects of heroin addiction on thyrotrophin, thyroid hormones and prolactin secretion in men. Clin Endocrinol(Oxf ) 1979;10(6):557-65.
RESULTS:Comparing the opioid group with the control group, 18 of the 20 patients (90%; 95% confidence interval [CI], 65-98%) exhibited hypogonadism, compared with 8 of the 20 control patients (40%; 95% CI, 19-64%). The median testosterone level was 145 ng/dL versus 399.5 ng/dL (5.0 nmol/L vs. 13.9 nmol/L; P < 0.0001), the median FSH level was 2.85 milli-International Units (mIU)/mL versus 5.3 mIU/mL (P = 0.08), the median LH level was 1.8 mIU/mL versus 4.2 mIU/mL (P = 0.0014), the median SDI-dyadic score was 18.5 versus 40 (P = 0.01), the median SDI-solitary score was 0 versus 5 (P = 0.007), the HADS (anxiety) score was 8.5 versus 5.5 (P = 0.053), the HADS (depres-sion) score was 7.5 versus 1.5 (P = 0.0002), the FACT-G score was 64 versus 96.3 (P = 0.0001), and the FACIT-F score was 24 versus 46 (P = 0.0003).
CONCLUSIONS:Survivors of cancer who chronically consumed opioids experienced symptomatic hypogonadism with significantly higher levels of depression, fatigue, and sexual dysfunction. With the increasing use of opioids among patients with cancer, further research in improving quality-of-life outcomes is warranted. Copyright 2004 American Cancer Society.
Upcoming Scientific Meetings
30 March – 2 April, 2005
24thAnnual Meeting of the American Pain Society American Pain Society
Hynes Convention Center, Boston, Massachusetts CONTACT: www.ampainsoc.org
http://www.ampainsoc.org 23-25 June, 2005
47thAnnual Scientific Meeting of the American Headache Society
Philadelphia, PN
CONTACT: American Headache Society Tel: (856) 423-0043 Fax: (856) 423-0082 Website: www.ahsnet.org 37. Rasheed A, Tareen IA. Effects of heroin on thyroid function, cortisol and
testosterone level in addicts. Pol J Pharmacol1995;47(5):441-4.
38. Allolio B, Deuss U, Kaulen D, et al. FK 33-824, a met-enkephalin analog, blocks corticotropin-releasing hormone-induced adrenocorticotropin secre-tion in normal subjects but not in patients with Cushing’s disease. J Clin Endocrinol Metab 1986;63:1427-31.
39. Taylor T, Dluhy RG, Williams GH. beta-Endorphin suppresses adrenocorti-cotropin and cortisol levels in normal human subjects. J Clin Endocrinol Metab1983;57: 592-96.
40. von Eckardstein A, Kliesch S, Nieschlag E, Chirazi A, Assmann G, Behre HM. Suppression of endogenous testosterone in young men increases serum levels of high density lipoprotein subclass lipoprotein A-I and lipoprotein(a). J Clin Endocrinol Metab1997;(10):3367-72.
41. Anderson FH, Francis RM, Selby PL, Cooper C. Sex hormones and osteo-porosis in men. Calcif Tissue Int1998;62(3):185-8.
42. Ebeling PR. Osteoporosis in men. New insights into aetiology, pathogenesis, prevention and management. Drugs Aging1998;13(6):421-34.
43. Jackson JA, Riggs MW, Spiekerman AM. Testosterone deficiency as a risk factor for hip fractures in men: a case-control study. Am J Med Sci 1992;304(1):4-8.
44. Flor H, Turk DC, Schotz OB. Impact of chronic pain on the spouse: marital, emotional and physical consequences. J Psychosom Res1987;31:63-71. 45. Maruta T, Osborne D, Swanson DW, et al. Chronic pain patients, and
spouses: marital and sexual adjustment. Mayo Clin Proc1981;56:307-10. 46. Monga TN, Tan G, Ostermann HJ, et al. Sexuality and sexual adjustment of
patienets with chronic pain. Disabil Rehabil 1998;20:317-29.
47. Sjogren K, Fugl-Meyer AR. Chronic back pain and sexuality. Int Rehabil Med 1981;3:19-25.
48. Gooren LJ, Bunck MC. Androgen replacement therapy: present and future. Drugs2004;64(17):1861-91.
49. Behre HM, Kliesch S, Leifke E, Link TM, Nieschlag E. Long-term effect of testosterone therapy on bone mineral density in hypogonadal men. J Clin Endocrinol Metab1997;82(8):2386-90.
50. Mc Clure RD, Oses R, Ernest ML. Hypogonadal impotence treated by trans-dermal testosterone. Urology1991;37(3):224-8.
Abstract of Interest
Symptomatic hypogonadism in male survivors of cancer with chronic exposure to opioids
RA J A G O P A L A , VA S S I L O P O U L O U- SE L L I N R , PA L M E R J L , KAU RG, BRU E R A E. CA N C E R 2004;100(4):851-8.
BACKGROUND:Profound hypogonadism has been noted in patients receiving intrathecal opioids. The purpose of the current study was to determine whether chronic consumption of oral opioids by male survivors of cancer also would lead to central hypo-gonadism and whether this hypohypo-gonadism was associated with symptoms of sexual dysfunction, fatigue, anxiety, and depression.
METHODS:A case-control study was conducted at The Univer-sity of Texas M. D. Anderson Cancer Center (Houston, TX), in which 20 patients who were chronically consuming opioids were compared with 20 matched controls. Patients completed the Sexual Desire Inventory (SDI), the Hospital Anxiety and Depression Scale (HADS), the Functional Assessment of Chronic Illness Therapy with general and fatigue subscales (FACT-G/FACIT-F), and the Edmonton Symptom Assessment System (ESAS) questionnaires. Serum samples were collected for testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH).
© 2005 The MGH Pain Center, Massachusetts General Hospital, which is solely responsible for the contents. The opinions expressed in this publication do not necessarily reflect those of the publisher or sponsor, but rather are those of the authoring institution based on the available scientific literature. Publisher: SNELL Medical Communication Inc.in cooperation with the MGH Pain Center, Massachusetts General Hospital. All rights reserved. The administration of any therapies discussed or referred to in Pain Management Roundsshould always be consistent with the recognized prescribing information as required by the FDA.SNELLMedical Communication Inc.is committed to the development of superior Continuing Medical Education.
This publication is made possible by an educational grant from
Pfizer, Inc.
314-009 S N E L L