ESTIMATING THE PREVALENCE OF ELEVATED
PLASMA NEUTROPHIL GELATINASE
ASSOCIATED LIPOCALIN (NGAL) LEVEL IN
PATIENTS WITH ACUTE CORONARY
SYNDROMES, AND IT’S ASSOCIATION WITH
ESTIMATING THE PREVALENCE OF ELEVATED
PLASMA NEUTROPHIL GELATINASE
ASSOCIATED LIPOCALIN (NGAL) LEVEL IN
PATIENTS WITH ACUTE CORONARY
SYNDROMES, AND IT’S ASSOCIATION WITH
OUTCOME
A dissertation submitted in partial fulfillment of
D.M (Cardiology) Examination of the Tamil Nadu
Dr. M.G.R. UNIVERSITY, Chennai
CONTENTS
Certificate 4
IRB approval 7
Plagiarism certificate 8
Acknowledgements 9
Abstract 10
Aims 12
Literature review 13
Methodology 42
Results 49
Discussion 101
Limitations 105
Conclusions 106
References 107
Annexure 1 (Patient consent form) 113
Annexure 2 (Raw data collection sheet) 114
Annexure 3 (Master data sheet) 119
CERTIFICATE
This is to certify that the dissertation entitled “Estimating the prevalence of
elevated plasma neutrophil gelatinase associated lipocalin (NGAL) level in patients with acute coronary syndromes, and its association with outcome” is the bonafide original work of Dr. Anandaroop Lahiri, towards the DM (Cardiology), Degree Examination of the Tamil Nadu Dr. M.G.R University, Chennai to be conducted in 2015.
Signature:
Prof. Paul George (guide)
Professor and Head of Cardiology, Department of Cardiology Unit II, CHRISTIAN MEDICAL COLLEGE,
CERTIFICATE
This is to certify that the dissertation entitled “Estimating the prevalence of
elevated plasma neutrophil gelatinase associated lipocalin (NGAL) level in patients with acute coronary syndromes, and its association with outcome” is the bonafide original work of Dr. Anandaroop Lahiri, towards the DM (Cardiology), Degree Examination of the Tamil Nadu Dr. M.G.R University, Chennai to be conducted in 2015.
Signature:
Prof. Alfred Job Daniel Principal,
Department of Orthopaedics,
CERTIFICATE
I, Anandaroop Lahiri, solemnly declare that the dissertation entitled “Estimating the prevalence of elevated plasma neutrophil gelatinase associated lipocalin (NGAL) level in patients with acute coronary syndromes, and its association with outcome” is a bonafide original work done by me in the Christian Medical College
and Hospital, Vellore, towards the DM (Cardiology), Degree Examination of the Tamil Nadu Dr. M.G.R University, Chennai to be conducted in 2015.
Signature:
Anandaroop Lahiri Candidate, Resident
Department of Cardiology,
ACKNOWLEDGEMENTS
Right at the outset I want to thank my guide Prof. Paul George, with all my heart for meticulously and painstakingly guiding me through this entire process of completing my dissertation. I cannot thank him enough for all the patience with which he dealt with me even when I fell behind in my work.
I am also grateful to Prof. Jacob Jose, Prof. George Joseph, Prof. Oommen George, Prof. Bobby John, Prof. Viji Samuel, Prof. John Roshan and all my other teachers and colleagues in the Department of Cardiology for all the support I received in preparing this dissertation and throughout my three year course in Cardiology.
I would like to thank the departments of Biochemistry and Microbiology for processing the NGAL and HSCRP samples.
I would also like to thank the Department of Clinical Epidemiology and Biostatistics, and Ms. Reka in particular, who helped me with the analysis of the data.
At this point of time I would like to thank all my patients who agreed to be a part of this study without caring for the extra blood samples and their extra time that I wasted to fill up the forms.
ABSTRACT
Aims and objectives:
The principal objective of this study was to estimate the plasma levels of neutrophil gelatinase associated lipocalin (NGAL) in a cohort of patients with acute coronary syndromes across their entire spectrum, and to correlate them with outcomes.
Background:
NGAL has been studied in the past as a sensitive indicator of acute kidney injury and contrast induced nephropathy. Very recently some studies have indicated the possibility of elevated NGAL levels in various cardiac conditions with or without acute kidney injury. One such study has looked at this molecule in patients with ST elevation myocardial infarctions where they found elevated levels in these patients, as well as, prognostic benefit of the molecule.
Methods:
longitudinal strain by speckle tracking imaging. Plasma NGAL was studied for its predictive power for various defined outcomes.
Results:
Plasma NGAL levels were detectably elevated in 67% of patients with acute coronary syndromes without any significant proportion with renal dysfunction, sepsis or overt infection. Plasma NGAL was the strongest independent predictor of all cause hospital mortality in Cox regression multivariate analysis with an odds ratio of 8.353, p= 0.0237. Plasma NGAL did not correlate with HSCRP, severity of coronary artery disease or major adverse cardiac events at one month follow up.
Conclusion:
This is a small study that shows that plasma NGAL in patients admitted with acute coronary syndromes, can predict hospital mortality and forms the basis for consideration of this molecule as a possible new risk marker in acute coronary syndromes meriting further and more extensive investigation.
Keywords:
AIMS
The aims of this study were as follows:
1. Estimation of the proportion of patients with acute coronary syndromes, with elevated plasma neutrophil gelatinase associated lipocalin (NGAL) at admission to the hospital
2. Correlation of the values of plasma NGAL with markers of cardiac injury 3. Correlation of the values of plasma NGAL with markers of inflammation
4. Correlation of the values of plasma NGAL with severity of coronary artery disease in patients with acute coronary syndromes
LITERATURE REVIEW
Introduction
Recently there has been a lot of work done in the development of biomarkers in various fields. The concept that a simple assay or a bedside test for a particular molecule could predict complex endpoints has led to widespread work to uncover these molecules and make them readily detectable. The advantage lies in them being able to predict the complicated from the very basic.
Neutrophil gelatinase associated lipocalin (NGAL) is a molecule, that, as many in the past, have done the rounds and gone around in circles, to land up in fields, that are completely distinct from those associated with it, at its characterization. It continues to surprise us and appears to take up new roles every day in various pathways in the body.
Biology of NGAL
The lipocalin proteins, of which NGAL is one, are made of eight beta strands that form a beta barrel enclosing a calyx (4). The structure of the NGAL molecule was demonstrated by crystallography in the year 2000 by Goetz et al (5). The calyx transports and binds small molecules. Though NGAL was originally identified in neutrophils, later it was also found to be expressed in the liver, kidneys, and epithelial cells (4).
NGAL exists as a 25 kilodalton monomer – as well as a 45 kilodalton homodimer, and attached to gelatinase as a 135 kilodalton heterodimeric form (3). The monomeric form and sometimes the heterodimeric form are the predominant forms manufactured by the renal tubular epithelial cells - whereas the homodimeric form is usually specific to the neutrophils (6).
NGAL is normally expressed at constant albeit low rates in multiple cell types. Accordingly, in healthy individuals, NGAL levels are detectable in low concentrations in the circulation (4). In the kidneys, NGAL is filtered through the glomerular membrane, and luminal NGAL is subsequently readily reabsorbed into the proximal convoluted tubule by a megalin-dependent pathway (7,8). Hence, during steady state conditions, only low levels of NGAL are found in the urine.
downstream cellular responses (11,12). NGAL can produce bacteriostasis, anti-apoptotic effects and can cause enhanced proliferation of renal tubules. Renal proliferation may constitute a possible pathway of NGAL associated renal protection in acute kidney injury (AKI) (4).
NGAL levels maybe up-regulated in response to various pathological conditions, such as infection, inflammation, intoxication, ischaemia, acute kidney injury and even neoplastic transformation (5,13–16). Immediately after acute kidney injury, NGAL is significantly up-regulated in the thick ascending limb of the loop of Henle, distal convoluted tubule and collecting duct. This results in elevated urinary and plasma NGAL levels. This increase is presumably from both basolateral and apical secretion of the nephron epithelia. Proximal tubular reabsorption is impaired in the setting of proximal tubular injury – this may further potentiate the increase in NGAL levels in urine (8,17,18).
NGAL production, as has been pointed out before, is not restricted to renal tissues. Malignancies and septicemias are situations that have revealed elevated NGAL values (4). Urinary tract infections with leucocyturia can elevate NGAL levels as well (19). It has been shown in a large, heterogenous primary care study population, that urinary NGAL levels also depend on age, gender and hepatic function and that they vary positively with inflammatory parameters (20). 6.5% of
subjects demonstrated increased urinary NGAL levels in the absence of any signs of AKI (20).
failure (in the post myocardial infarction setting and in the chronic heart failure setting) and a rat model of post myocardial infarction heart failure. They found elevated myocardial expression of NGAL (up-regulation of NGAL mRNA) in human myocardial samples of the failing heart as well as from the myocardium of the rat model of post myocardial infarction heart failure. Latouche et al (22) studied a mouse model that over-expressed the mineralocorticoid receptor in the myocardium (termed MRcardio mice). A pan-genomic transcriptomic analysis on the hearts of these transgenic mice (MRcardio mice) identified the NGAL molecule as a gene that was highly induced. The induction of NGAL was essentially mineralocorticoid receptor dependent. The up-regulation of NGAL was up to the tune of about 150-times the values in control mice.
values being noted in the group of the STEMI patients. Interestingly, there was a significant positive correlation between serum-NGAL values and highly sensitive
CRP values (spearman coefficient rho = 0.685, P< 0.0001). It would appear that
NGAL levels correlate with the degree of inflammation as evidenced by correlation with rising values of highly sensitive CRP values.
The spectrum of atherosclerotic diseases includes the formation of abdominal aortic aneurysms which are also indirect manifestations of vessel inflammation. Ramos-Mozo et al (24) studied NGAL concentrations by Western blotting in conditioned media of polymorphonuclear neutrophils from abdominal aortic aneurysm patients (n = 22) and controls (n = 11). They also studied NGAL expression in aortic biopsies from abdominal aortic aneurysm patients and healthy controls (n = 10). Neutrophils isolated from abdominal aortic aneurysm patients secreted significantly greater amounts of NGAL as compared to neutrophils from control subjects. Furthermore, there was a positive direct correlation between plasma NGAL levels and abdominal aortic aneurysm growth (rho = 0.4, p = 0.01). This remained significant even after adjusting for other risk factors.
NGAL in renal dysfunction
bilateral ischaemia (15). If the maximum expression levels of NGAL mRNA were considered in injured kidneys, they were found to be elevated more than 1000-fold after 24–48 hours of injury (25). Urinary NGAL was undetectable in urine before ischaemia and subsequently became evident within 2–3 hours of clinically significant renal ischaemia. The time of occurrence, intensity and duration of
urinary NGAL up-regulation correlated well with the same parameters of the ischemic event. The highest NGAL levels following AKI displayed up to a 1000-fold increase in urine (from 0.04 to 40 mg/mL) and a 300-1000-fold increase in blood levels (from 0.1 to 30 mg/mL) (15,25). Interestingly when exogenous recombinant NGAL was administered in a mouse model of ischemia-reperfusion injury, it appeared to have renal protection from ischemic damage (8).
NGAL expression has also been studied in animal models of toxin injury to the kidneys such as with agents like cisplatin and gentamicin. These studies also showed similar outcomes with significant NGAL up-regulation fairly early into the stage of injury, to the tune of the first 2-3 hours following toxin exposure and kidney injury.
non-invasively. The luminescence was 10-fold increased 3–6 hours after renal artery clamping with maximum expression (around 25–80-fold) 12 hours after ischaemia. The intensity of the response correlated with the ischaemic dose. Interestingly, non-ischaemic kidneys as well as extra-renal tissues failed to show any luminescence. NGAL reporter expression in the kidneys and urinary NGAL levels correlated closely, both temporally and in terms of intensity of their responses – this implied that the protein originated in all probability from the kidneys.
kidneys were transplanted into NGAL-/- hosts. Consequently, only a mild increase in urinary NGAL was observed after ischaemia of NGAL-/- kidneys transplanted into NGAL+/+ mice, indicating that there could be some extra-renal source contributing to urinary NGAL levels. The increase was substantially lesser when compared with urinary NGAL values after ischaemia of an NGAL+/+ kidney, pointing to the fact that the majority of urinary NGAL is probably derived from the ischaemic kidney
Clinical utility of NGAL as a biomarker for AKI
In clinical practice, a diagnosis of AKI is currently based on serum creatinine and urine output, but these parameters have major limitations. Firstly, they do not differentiate between structural kidney damage and functional haemodynamic triggers of a reduced glomerular filtration rate. Secondly, the diagnosis gets delayed until creatinine has accumulated, which unavoidably delays treatment. The NGAL molecule could help in resolving these drawbacks due to its ability to detect actual tissue damage rather than renal dysfunction and due to its brisk induction in response to AKI triggers.
Multiple studies have addressed the potential clinical usefulness of NGAL in AKI. All these studies combined include in excess of 7000 patients. The studies reveal a remarkable heterogeneity regarding the patient groups studied, the biofluids analysed, the various assays used to measure NGAL levels, the definitions of clinical outcomes and the studied test characteristics. Most of these
31) and two other studies were done within a framework of multi-centric trials (32,33). AKI diagnosis was made according to current usual diagnostic criteria based on postoperative creatinine dynamics (>50% or >0.3 mg/dL elevation of creatinine).
A lot of investigators have looked at NGAL levels in cardiac surgery patients mainly in an attempt to hasten the detection of renal dysfunction (16,29,32,34).Studying patients in this setting gives the advantage of being able to identify with a fair degree of accuracy as to the possible exact time point of the initiation of renal injury. The majority of these investigations highlighted the fact that the levels of NGAL both in the urine and the plasma were able to predict renal injury in the acute setting. The sensitivity analyses among these studies yielded substantially varying area under the curve (AUC) – receiver operating characteristics (ROC) for the NGAL values.
the range of 0.95–0.998 for urine NGAL, and 0.91–0.96 for plasma NGAL n these studies.
A number of prospective studies on NGAL have also been performed on adult patients post cardiac surgery (29,30,32). Elevated urinary NGAL levels were observed as early as 1–3 hours after surgery. Peak levels of NGAL in urine and plasma were attained 6 hours after the operation (29,32). The predictive ability of NGAL depended considerably on the type of the NGAL assay, the time points reported and the definition of AKI in all these studies. AUC-ROC of urinary
NGAL spanned from 0.74 (36) to 0.88 (32). When plasma NGAL was considered the AUC-ROCs varied from 0.64 (30) to 0.89 (37).
When we consider serum creatinine as the gold standard for the diagnosis of AKI, then many a time it would be noticed that serum creatinine per say is a poor marker for true or intrinsic renal injury. “Prerenal AKI” where the serum
creatinine is markedly responsive to the correction and optimization of haemodynamic parameters in the body would appear to be a common phenomenon in day to day clinical practice. With this background, studies have tried to tease out actual intrinsic renal injury from “Prerenal AKI” with the use of
these papers was that the diagnosis of intrinsic kidney injury was based on clinical criteria rather than actual renal biopsy and histopathology.
There is additional data to demonstrate remarkable associations of NGAL values with adverse clinical outcomes. These include major endpoints such as worsening of AKI, need for renal replacement therapy and overall mortality (27,33,38,39). Interestingly, patient populations stratified by serum creatinine cut-offs were further effectively subdivided into high and low risk groups, when NGAL cut-offs were added (27,40). The levels of urinary NGAL predicted a composite endpoint of initiation of dialysis or death during hospitalization. NGAL was also able to identify a substantial sub-population of patients with low / normal serum creatinine at admission to the hospital, but who were later found to be at risk of adverse events. This so called “Creatinine-negative”, “NGAL-positive”
patient group, which cannot be classified to have AKI by conventional criteria and standards, may represent a unique group of patients exhibiting what may be classified as „subclinical‟ AKI. AKI has been found to be independently associated
with the length of hospital stay (41) and therefore can significantly add to the treatment expenses. Early diagnosis of AKI based on NGAL may aid in earlier, and thus more cost-effective management than the standard strategy (42).
the story when plasma NGAL was considered – in the ICU - plasma NGAL discriminated AKI with an AUC-ROC of 0.78–0.86 (44,45).
In critically ill septic patients the picture was somewhat less succinct. This was due to the fact that sepsis appears to be a major inducer of urinary and blood NGAL expression – and this is even in the absence of changes in creatinine. The origin of NGAL in the clinical situation of septicemia appears to be not only the injured kidneys but also the leucocytes and the liver. Bagshaw et al (46) studied patients with septic AKI versus non-septic AKI. They found that the levels of NGAL, both in the urine and the plasma, to be substantially elevated in the septic AKI group as compared to the non-septic AKI group, other conditions remaining similar. This fact may have some independent implications. For one thing, this leads us to believe that up-regulation of NGAL is not limited to renal injury – it may be a response to other processes within the body. It remains to be clearly elucidated as to what other processes could be reasons for NGAL expression – however inflammatory states and cardiac conditions like heart failure and acute coronary syndromes may be likely candidates for over-expression of NGAL – the possible cardiac conditions associated with elevation of NGAL will be discussed in a later section.
NGAL in epidemiologic studies of cardiovascular risk
The concept of the possible association of the NGAL molecule with the cardiovascular system is a fairly recent one. The fact that the NGAL molecule is not unique to the nephron and that it is expressed in the neutrophils which are an universal response to any form of injury, healing or inflammation raises the possibility of fluctuations of the levels of the molecule in various physiological and pathological processes involving the cardiovascular system, given the multitude of conditions involving inflammation, affecting the cardiovascular system. However, in contrast to the amount of literature about NGAL in the field of acute kidney injury (that may or may not stem from a primary cardiovascular problem or a procedure related to the cardiovascular system) work on NGAL levels in cardiovascular disease without kidney injury is scanty.
cardiovascular endpoint [defined as a composite of the first incidence of coronary
revascularization (coronary artery bypass graft surgery or percutaneous coronary intervention), cardiovascular disease mortality, and nonfatal myocardial infarction]. After adjusting for N-terminal pro–B-type natriuretic peptide (NT-proBNP) and C-reactive protein (CRP) levels, plasma NGAL remained an independent predictor marker of each of the above mentioned outcomes. NGAL was able to improve the C-statistic from 0.835 to 0.842, for prediction of cardiovascular disease deaths (p < 0.001). It was also noted in the analysis that participants with both NGAL and NT-proBNP above the median had higher risk of cardiovascular disease death as compared to those with only elevated NT-proBNP levels (hazards ratio: 1.43, 95% confidence interval: 1.12 to 1.82). This probably points towards the fact that plasma NGAL was able to re-stratify an already high cardiovascular disease risk population (as indicated by elevated NT-proBNP) into further low-risk and high-risk groups. This could indicate an additive stratification advantage of the NGAL molecule. This would obviously need to be further looked at in more studies for adequate validation. Also, the biology or the pathophysiological processes that may involve the NGAL molecule in cardiovascular disease processes was not delved into in this study, as this was an epidemiological follow-up.
NGAL in coronary artery disease
angina, non ST elevation myocardial infarction (NSTEMI) and ST elevation myocardial infarction (STEMI) and studied the levels of NGAL in the serum of such patients. The hypothesis was that, NGAL being a component of neutrophil granules in the human body, may reflect the degree of inflammation in these various cardiovascular clinical conditions that possibly reflect various degrees or stages in the spectrum of inflammatory reactivity of the cardiovascular system. They studied 140 patients - 40 with stable angina, 35 with unstable angina, 40 with NSTEMIs, 25 with STEMIs, and 20 that were healthy controls. There were significant differences that were observed in the median serum NGAL (ng/mL)
CRP (spearman rank correlation coefficient rho = 0.685, P< 0.0001) – the
correlation also held true for neutrophil counts (r = 0.511, P< 0.0001). Hence, in patients with coronary artery disease, serum levels of NGAL appear to increase with, and reflect, the extent of the inflammatory process, brewing within the
cardiovascular system. There is some demonstrable positive correlation of the NGAL molecule with a known robust risk predictor of cardiovascular disease (highly sensitive CRP levels) – this opens up the possibility of the use of NGAL as a novel independent cardiovascular risk predictor. These ideas however need to be studied further before any emphatic statement can be laid out.
NGAL seepage from cardiovascular tissues
increased proteolytic activity may suggest a role for NGAL/24p3 in modulating and influencing the MMP-9-mediated remodeling of atherosclerotic plaques and infarcted hearts.
NGAL in heart failure
Yndestad et al. (21), looked at the dynamics of NGAL expression in the context of heart failure both in the post myocardial infarction setting as well as otherwise. Their main study subjects were as follows:
1. A subgroup of patients (around 236) from the OPTIMAAL trial registry (50) were included – these patients had post myocardial infarction heart failure.
2. 150 patients with stable chronic heart failure (greater than four months in NYHA class II-IV on optimal cardiovascular medications) – these patients were recruited from those attending the Department of Cardiology at Rikshospitalet University Hospital – 66 of them had ischemic heart disease and 84 had idiopathic dilated cardiomyopathy.
3. 20 healthy controls
obtained from age and sex-matched patients whose hearts were rejected for cardiac donation for various surgical reasons.
5. Male Wistar rats were considered at 2, 7, 28, and 64 days after ligation of the left coronary artery leading to the development of heart failure. A control group of rats with a sham operation without ligation of the left coronary artery was also considered. Myocardial NGAL expression was studied in both these groups.
Cardiomyocytes, endothelial cells and other non-cardiomyocytes were isolated from rats and humans as mentioned above and analysed for NGAL with the help of real time RT-PCR, immunohistochemistry and enzyme linked immunosorbent assays (ELISAs).
There was some immunoreactivity also, in the vascular smooth muscle cells and the adjoining endothelial cells. In the ischaemic area, the granulation tissue especially at the border zone between the non-ischaemic and ischaemic regions in post myocardial infarction rats, anti-NGAL/lipocalin-2 immunostaining was found to be present in microvascular endothelial cells as well as in some of the infiltrating cells that could represent granulocytes. Hence this study demonstrated
[image:33.612.92.408.431.655.2]the enhanced myocardial and systemic expression of the NGAL molecule in both clinical and experimental heart failure. This may thus indicate a possible supporting role of the NGAL molecule in the innate immune responses of the body in heart failure. This also goes on to demonstrate that the myocardium may well be one of the potential sources of over-expression of the NGAL molecule especially in situations like cardiac failure and myocardial infarction.
Activation of the mineralocorticoid receptor may be deleterious to the cardiovascular system, and mineralocorticoid receptor antagonists have been shown to improve mortality and morbidity of patients with heart failure. However, the exact pathophysiology of mineralocorticoid signaling in the heart remains fairly unknown. Latouche et al. (22) used a pan-genomic transcriptomic analysis, and identified the NGAL molecule as a highly induced gene in the cardiomyocytes of mice with conditional and targeted mineralocorticoid receptor over-expression (This induction was reduced in glucocorticoid receptor–over-expressing mice). NGAL mRNA levels were also elevated after stimulation by the mineralocorticoid receptor ligand aldosterone in cultured myocardial cells of wild-type mice. Mineralocorticoid pathological challenge caused by nephrectomy / aldosterone / salt treatment interestingly up-regulated NGAL expression in the aorta and the heart and it subsequently led to an increase in its plasma levels. They were able to show evidence for mineralocorticoid receptor binding to an NGAL promoter, hypothesising a potential mechanism for NGAL regulation. They proposed that NGAL may well be a marker of mineralocorticoid-dependent injury within the cardiovascular system in mice. Human studies in this area are however not forthcoming.
NGAL in ST elevation myocardial infarctions
prospective follow-up study in this field. Lindberg et al. (51) published a study recently where they prospectively studied the possible role if any of the NGAL molecule in predicting various outcomes in patients undergoing primary percutaneous intervention for ST segment elevation myocardial infarctions.
Lindberg et al. (51) prospectively recruited 584 patients with ST elevation myocardial infarctions presenting within 12 hours of symptom onset, from September 2006 through December 2008, treated with primary percutaneous coronary intervention at Gentofte University Hospital, Copenhagen, Denmark. Plasma NGAL was measured using an in-house time-resolved immunofluorometric assay based on antibodies to the NGAL molecule and recombinant NGAL from R&D Systems (Abingdon, United Kingdom) (52). Endpoints considered were all-cause mortality and major adverse cardiovascular events (MACE). MACE was defined as cardiovascular mortality or recurrent acute
myocardial infarctions or heart failure requiring hospital admission. Subjects with high NGAL levels had increased overall risk of all-cause mortality and MACE when compared with subjects with low NGAL levels (log-rank test, p < 0.001). After adjustment for confounding factors chosen by backward elimination by Cox regression analysis, high levels of NGAL remained an independent and significant predictor of all-cause mortality as well as MACE (hazard ratio: 2.00; 95% confidence interval: 1.16 to 3.44; p < 0.01 and hazard ratio: 1.51; 95% confidence
be a very sensitive marker of acute kidney injury. This also raises the possibility that NGAL may represent subclinical AKI in this particular group of patients. In this study the combination of high CRP with high NGAL conferred the highest risk of mortality, whereas low CRP with low NGAL conferred the lowest risk of mortality. Hence NGAL appeared to confer additional prognostic information over and above CRP levels. Interestingly, patients with high NGAL with low CRP had a significantly higher risk of mortality when compared with patients having low NGAL with high CRP. This indicates that NGAL probably possesses better prognostication efficiency when compared with CRP. With regard to MACE, subjects with high NGAL values had significantly high risk regardless of CRP levels. Hence overall, high NGAL levels were observed in patients with acute myocardial infarctions with ST segment elevation, and not all of them had AKI as defined by creatinine levels. Whether this increase in the levels of NGAL is caused by AKI (overt / subclinical), increased inflammation, or both and whether
Figure 3: Kaplan-Maier plots of all-cause mortality amongst the subjects dependent on NGAL levels stratified as high versus low (51)
[image:37.612.94.370.72.369.2] [image:37.612.93.370.426.703.2]NGAL in contrast induced nephropathy (CIN)
The search for indicators of contrast induced nephropathy has been on for a while now – work has concentrated on sharpening the sensitivity and specificity of these markers as well as to find molecules that would indicate renal injury as early as possible during the clinical course of contrast induced nephropathy so that adequate pre-emptive action could be taken. Work with regard to NGAL in the field of contrast induced nephropathy is fairly common in the literature.
McCullough et al. (53) performed a prospective blinded study that assessed blood samples collected from patients with estimated glomerular filtration rate (eGFR) <75 ml/min/1.73 square meter body surface area undergoing elective coronary intervention or angiography using iodinated contrast agents. Patients with renal transplants, dialysis patients, and patients who had received iodinated contrast in the prior 30 days were excluded from the analysis. The correlation between NGAL and eGFR was r = –0.61 (95% CI –0.74 to –0.44), p <0.001. When stratified according to baseline NGAL tertiles, the peak NGAL values observed for each group occurred at 29.0 +/- 22.2 hours and there appeared to be a twofold increase in the peak and mean change in NGAL values across the tertiles. NGAL was seen to begin to rise as early as 6 hours after contrast exposure. Rise of NGAL levels followed a similar course to serum creatinine and at 48 hours the overall mean NGAL value was still increasing.
exposure yielded a sensitivity of 0.78 and a specificity of 0.96 for making a diagnosis of contrast induced nephropathy with an AUC-ROC of 0.89.Overall NGAL appeared to be both of diagnostic as well as prognostic value in various clinical situations of acute kidney injury including contrast induced nephropathy.
Liu et al. (55) studied patients with suspected or established coronary artery disease who had estimated glomerular filtration rates (eGFR) between 30 and 90 ml/min/1.73 square meter body surface area. Such patients were enrolled continuously. A total 311 patients were included, among whom 39 (12.5%) developed contrast induced acute kidney injury (CIAKI). Plasma NGAL values were seen to start increasing by 2 hours and were seen to reach a peak at 4 hours post procedure. The plasma NGAL value at 4 hours after contrast medium exposure showed the largest area under curve (AUC) of 0.662 [95% confidence interval (CI): 0.565–0.758, P=0.002] with a sensitivity of 51.5% and a specificity of 80.6%. Relative increase in the NGAL value of about 25% from the baseline value showed the best specificity and sensitivity of 0.808 and 0.872 respectively for a diagnosis of contrast induced acute kidney injury. In the same study they also studied serum cystatin levels concurrently and found that the combination of cystatin and NGAL may be an even better indicator of this condition.
Global strain as a marker for left ventricular dysfunction
The most extensively investigated echocardiographic parameter for systolic function of the left ventricle is the left ventricular ejection fraction (LVEF). Most studies have established it to be a fairly powerful predictor of mortality among patients with systolic heart failure (57,58). Some reports however have characterized the relationship between mortality and LVEF in heart failure patients with rather inconsistent results (59–61). The fact also remains that the assessment of left ventricular systolic function by echocardiogram often remains subjective – more so when the endocardial border of the left ventricle cannot be clearly delineated. The fairly recently developed tool utilizing 2-dimensional (2D) strain based on speckle tracking is an interesting method providing information about multidimensional myocardial mechanics – these involve rotational, longitudinal and circumferential motion of the left ventricle.
METHODOLOGY
Study design
This study was modeled like a observational cross-sectional study with a defined period of follow up.
Setting
The study was conducted in the Department of Cardiology, in the Christian Medical College and Hospital, Vellore. This is a tertiary care hospital in south India with a dedicated twenty four hours emergency chest pain unit and cardiac catheterization laboratory service.
Patients
Inclusion criteria:
1. Patients with any form of acute coronary syndrome. 2. Age more than 18 years
3. Valid consent
Exclusion criteria 1. Any overt infection 2. Sepsis
Procedures
Patients with acute coronary syndrome meeting the inclusion and exclusion criteria as specified, presenting to the emergency department or chest pain unit of the Christian Medical College and Hospital, Vellore were included in the study after taking informed consent. At the time of admission the patients underwent all the usual routine work-up that is followed as a protocol in the department of Cardiology. Thus the patients had an electrocardiogram taken They had blood drawn for clinical pathology parameters like haemoglobin and blood counts, and clinical biochemistry parameters like estimation of troponin T and CKMB mass, and estimation of renal functions, serum electrolytes, serum lipid profile and HBA1C. Apart from those, blood was drawn for estimation of plasma neutrophil gelatinase associated lipocalin (NGAL). and serum high sensitivity C reactive protein (HSCRP) at admission. Plasma NGAL and serum HSCRP, being investigations not part of the routine work up of such patients, were not charged for. The details of the assays are discussed in a subsequent section.
parameters and global longitudinal strain (GLS) by speckle tracking, were determined for all patients during hospitalisation on a GE Vivid 9E machine. Data was also collected of the angiograms of the patients, if they had one and the type of interventions that they underwent. SYNTAX and Gensini scores were calculated on all the performed angiograms.
The patients were followed up at an interval of one month from the discharge of index admission on an out-patient department / office basis or in the emergency department or chest pain unit if they underwent readmission. A repeat conventional echocardiographic examination was performed and an attempt was made to repeat the GLS measurements. Patients were interviewed for clinical events and examined for features of ischemia or heart failure.
Outcomes
1. Proportion of patients with acute coronary syndromes with elevated plasma NGAL levels.
2. Endpoints in hospital
Progression to cardiogenic shock Development of reinfarction
Development of recurrent post infarction angina Mechanical and electrical complications of a STEMI In-hospital all-cause mortality
ECHO: Left ventricular function by conventional echocardiographic methods and GLS
Correlation with angiographic severity of coronary artery disease and TIMI risk percentage
3. Correlation of plasma NGAL with biomarkers: Troponins
CKMB HSCRP
4. Endpoints at follow up
Total mortality up till one month Major adverse cardiac events
ECHO: Left ventricular function by conventional echocardiographic methods and GLS
Laboratory and assay considerations
particle enhanced turbidimetric immunoassay for the quantitative determination of NGAL. The minimum level of detection of the test is 10 ng/mL.
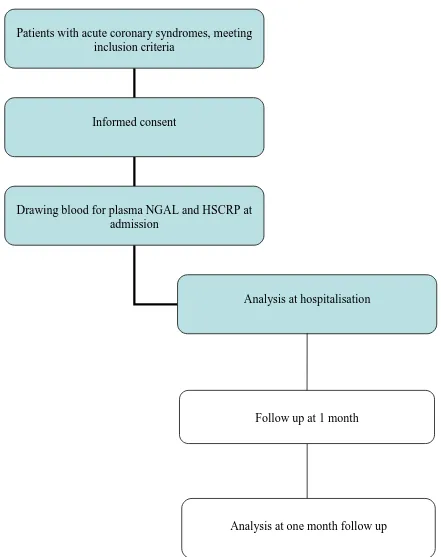
Summary of study
Figure 1: STROBE diagram (blue coded boxes represent the parts during hospitalisation) Patients with acute coronary syndromes, meeting
inclusion criteria
Informed consent
Drawing blood for plasma NGAL and HSCRP at admission
Analysis at hospitalisation
Follow up at 1 month
Statistical analysis
The sample size in accordance with a prevalence study (51), was calculated by the following formula.
n= z2 p (1-p) d2
where n = sample size,
z = z statistic for a level of confidence, p = expected prevalence or proportion and d = precision
According to existing data the prevalence of elevated NGAL levels in acute coronary syndromes was taken as 30%, the precision was taken as 10%, z statistic was taken as 1.96 for a confidence interval of 95%. With the above figures a sample size of 80 was arrived at. The aim of the study is to get a total of 100 people as the sample population.
RESULTS
A total of 107 consequent patients were deemed fit for inclusion into this study. 10 patients had to be excluded as they did not provide consent. A further 10 patients had to be excluded owing to inappropriate sampling methods for high sensitivity C- reactive protein (HSCRP) and neutrophil gelatinase associated lipocalin (NGAL), degradation of samples and unsatisfactory processing. Hence a total of 87 patients were considered for the final analysis.
Figure 5: Recruitment of patients and exclusion 107 patients eligible
97 patients
10 patients did not give consent, hence excluded
87 patients analysed
Age
[image:50.612.95.433.238.533.2]The mean age of the surveyed population was 57.9 years and the median age was 58 years. The minimum age was 32 years and the maximum age was 89 years. Given below is the age distribution of the population which appears to be a normal distribution.
Gender
[image:51.612.89.454.135.357.2]74% of the subjects were males and 26% were females.
Figure 7: Gender distribution in the population
Region
Habits
[image:52.612.91.460.165.391.2]Data regarding smoking, alcohol and tobacco chewing was assimilated during the study.
Figure 8: Distribution of smoking in the population
33% of the patients were current smokers and 5% were ex-smokers. 62% were non-smokers. Cigarettes were the commonest form of smoked tobacco (57.6%). 75.9% of the patients had never consumed alcohol. 5.7% of the patients were tobacco chewers.
Dyslipidemia
Hence in this study the definition of dyslipidemia has been arbitrarily taken to be either of the following:
1. LDL value of more than 70mg/dL
2. Total cholesterol value of more than 200mg/dL
Using the above definition, 89.7% of the patients qualified to be labeled as dyslipidemics. The mean value of LDL in the population was 107.17 mg/dL. The distribution of LDL in the population is shown below. The mean values of total cholesterol, triglycerides and HDL were 160.64 mg/dL, 144.23 mg/dL and 35.16 mg/dL respectively. 74.7% of the patients had an HDL value of less than 40mg/dL. Low HDL has traditionally been taken as a coronary risk factor, but the last ACC/AHA guidelines have declared that there is no benefit in treating to optimize HDL cholesterol goals. (1) Hence the significance of this high proportion of patients possessing low HDL has not been clarified. Incidentally low HDL has been quoted in the literature to be commoner in the Asians and may have a greater bearing towards cardiovascular risk determination in Asians preferentially, as compared to Non-Asians. (2)
Diabetes mellitus
51.7% of the patients had diabetes mellitus. Serum glycosylated haemoglobin (HBA1C) was tested for all patients at admission, irrespective of their diabetic status. The mean level of HBA1C amongst diabetics was 8.447g/dL (95% confidence interval 7.685 – 9.209), whereas the mean level of HBA1C amongst non-diabetics was 5.717g/dL (95% confidence interval 5.597 – 5.836). The distribution of HBA1C in the entire study population is shown below.
Figure 10: Distribution of HBA1C in g/dL in the population
Hypertension
History of cardiovascular disease
Data was collected for evidence of past history suggestive of coronary artery disease. 23% of the patients in the study had evidence of some form of coronary artery disease (CAD) in the past. 77% had no history suggestive of CAD. Amongst the patients who had a history of CAD in the past, the most common form of the disease was ST elevation myocardial infarction (STEMI) that was noted in 10 patients, and the next most common form of the disease was stable angina in 5 patients.
Figure 11: History of CAD in the patients
Of the patients who had a history of CAD, 7 patients had undergone angiograms in the past. 3 patients had triple vessel disease, 1 patient had left main disease with triple vessel disease, 2 patients had double vessel disease and one patient had single vessel disease. The median SYNTAX score of these patients was 19 and the median Gensini score of these patients was 46.
Apart from coronary artery disease, one other patient had a history of bradyarrhythmia in the past and one patient had a history of an atrial septal defect in the past.
History of renal disease
Type of acute coronary syndrome
[image:57.612.94.524.113.603.2]The distribution of the types of acute coronary syndromes is given below.
unit and in view of the absence of high risk features would have been discharged home with conservative management. However, in view of our hospital chest pain unit, being a very busy one with limited patient beds, there would have been a hidden admission bias in that the sicker patients would have been admitted preferentially as compared to the patients with low risk. This would not interfere with the implications of the results from this study owing to the fact that the low risk population is not really a concern when we consider issues like risk stratification and prognostication knowing that these patients would not register serious adverse cardiac events.
20% of the patients had non ST segment elevation myocardial infarctions. There were 2 patients who presented with acute coronary syndromes with acute onset left bundle branch blocks. Nobody was recruited with pure posterior wall myocardial infarction.
There were a total of 66 patients that were admitted with ST segment elevation myocardial infarctions (STEMI). Of them 52% had anterior infarctions and 48% had inferior infarctions. In the group with anterior infarctions there were 4 patients with qRBBB anterior wall myocardial infarctions. The commonest subtype of STEMI was anterolateral wall myocardial infarction – this was seen in 16.1% of the total number of recruited subjects.
Duration of symptoms
Figure 15: Distribution of the duration of symptoms at the time of presentation amongst the patients
There was no statistically significant difference in the mean duration of symptoms at presentation between patients with UA/NSTEMI versus patients with STEMI. The duration of symptoms at presentation was 12.19 hours for patients with STEMI and 13.63 hours for patients with UA/NSTEMI (p=0.749).
Clinical features at presentation
Figure 16: NYHA class amongst the dyspnoeic patients (n=26)
Figure 17: Distribution of heart rates amongst the population
presentation were not statistically different between patients with STEMI and UA/NSTEMI.
The mean systolic blood pressure was 119.79 mm Hg. There was no difference in the mean systolic blood pressures in the patients presenting with STEMI as opposed to UA/NSTEMI. Cardiogenic shock, defined as a systolic blood pressure of less than 90mm Hg was present in 11.5% of the patients at presentation.
On auscultation a left ventricular third heart sound was noted in 5.7% of the population. Left ventricular fourth heart sounds were not reliably noted amongst the patients that were recruited.
Pulmonary oedema at admission, was noted in 35.6% of the total population. 47.3% of the patients with an UA/NSTEMI had pulmonary oedema at admission and 32.3% of the patients with STEMI had pulmonary oedema at admission. The proportions of patients with pulmonary oedema in the two groups were not statistically different. 4 patients in the entire cohort had developed ventricular tachycardia / ventricular fibrillation in the entire duration of the hospitalization.
Neutrophil gelatinase associated lipocalin (NGAL)
Blood for plasma NGAL was drawn at the time of admission of all the patients in EDTA coated test tubes and sent immediately to the department of biochemistry where it was immediately logged and frozen for analysis in batches at a later date. 10 samples had to be excluded prior to the analysis in view of unsatisfactory sample quality or processing or both.
Figure 19: Distribution of NGAL values in the entire population
Figure 20: NGAL levels in the populations – detectable versus undetectable
Table 1: Mean NGAL values in major population groups
Mean NGAL
(ng/mL)
p value
STEMI 159.88 0.893
UA/NSTEMI 150.74
Renal failure at
admission
277.8 0.018*
No renal failure at
admission
122.09
With the above consideration of low versus high NGAL values, we looked at certain baseline characteristics to study whether they differed significantly between the groups.
Table 2: Baseline characteristics
Parameters Low NGAL High NGAL p value
Age (years) 55.97 63.92 0.008*
Troponin T at
admission (pg/mL)
739.48 1461.32 0.228
CKMB Mass at
admission (ng/mL)
51.33 58.03 0.805
HSCRP at
admission (mg/L)
22.15 19.68 0.810
eGFR at admission
(ml/min/1.732 sq m
BSA)
65.72 49.95 0.002*
Serum creatinine
(mg/dL)
1.17 1.43 0.027*
Duration of
presentation
(hours)
12.32 13.07 0.860
Hospital LVEF
(%)
43.98 42.68 0.580
In the baseline characteristics, age was found to be significantly higher in the group of patients with high NGAL as opposed to the group of patients with low NGAL. The mean age in the low NGAL group was 55.97 years while that in the high NGAL group was about 8 years higher at 63.92 years. Mean estimated glomerular filtration rate (as calculated by the Cockcroft-Gault equation) was found to be significantly lower at admission in patients with high NGAL versus patients with low NGAL. The mean value in patients with high NGAL was 49.95 ml/min/1.732 square meter body surface area, whereas amongst patients with low NGAL the mean value was 65.72 ml/min/1.732 square meter body surface area. Similarly mean serum creatinine at admission was also significantly higher amongst patients with high NGAL as opposed to patients with low NGAL. Mean admission values of cardiac injury biomarkers like serum Troponin T and serum CKMB were not statistically different in the low and high NGAL groups. The mean value at admission of the inflammatory marker HSCRP was also not statistically different in the high and the low NGAL group. The numbers of PCIs done in the two NGAL groups were statistically similar with a p value of 0.806.
Serum markers of cardiac injury
At admission all the patients had their serum Troponin T and CKMB mass analysed. Further estimations of these serum biomarkers were ordered based upon the discretion of the treating clinician.
value amongst patients with UA/NSTEMI was 190.87 pg/mL and amongst patients with STEMI was 1126.30 pg/mL (p=0.001).
Figure 21: Distribution of troponin T levels in pg/mL in the population
Figure 22: Statistically significant correlation of admission plasma NGAL levels with admission serum Troponin T values
This study was neither geared nor powered towards the study of Troponin T as a risk predictor of poor outcome. Hence analyses to that effect were not performed. Besides, the risk predicting ability of serum troponin T has been well studied and documented in the literature with robust evidence.
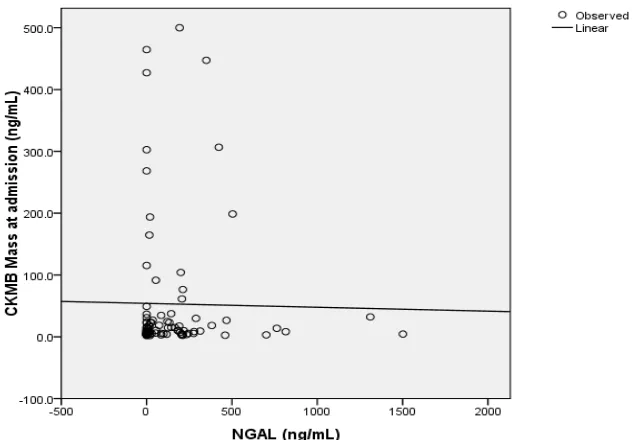
[image:70.612.105.457.77.444.2]Figure 23: Distribution of CKMB mass at admission in ng/mL in the population
Unlike the significant correlation with Troponin T, admission NGAL values did not seem to correlate significantly with admission values of CKMB mass as depicted below.
High sensitivity C reactive protein (HSCRP)
[image:72.612.98.453.326.631.2]HSCRP is an inflammatory marker that has been extensively studied in the field of cardiovascular medicine and especially coronary artery disease in the specific field of risk stratification. HSCRP values greater than 3mg/L have been deemed to indicate high risk and poor prognosis in cardiovascular disease. In our patient population the overall HSCRP value appeared to be higher than what would be normally expected in a cohort of patients with acute coronary syndromes.
Figure 25: Distribution of HSCRP in the population
UA/NSTEMI was 25.6 mg/L and in patients with STEMI was 20.3 mg/L. There was no statistical difference between these values with a p value of 0.623.
HSCRP values of more than 3mg/L in our cohort of patients failed to significantly predict all-cause mortality in hospital, total mortality up to one month of follow up and major adverse cardiac events up to one month of follow up. The values of HSCRP did not correlate significantly with admission values of Troponin T and CKMB mass. Interestingly, HSCRP failed to correlate significantly with the levels of plasma NGAL as well. This may indicate that variations in the values of NGAL in this population of patients with acute coronary syndromes may quite possibly be a mechanism not related to the inflammatory cascade. Hence plasma NGAL could potentially form an independent risk predictor of acute coronary syndromes – one that is independent of the inflammatory cascade.
When the correlation of HSCRP with TIMI risk percentage was plotted, it was noted that there was no statistical correlation between the HSCRP values and the TIMI risk percentage. HSCRP was not able to conclusively predict outcomes in our cohort.
Figure 26: Statistically significant negative correlation of HSCRP levels with LVEF during hospitalisation
Killip’s class
Traditionally the Killip‟s functional class at the presentation of an acute coronary syndrome correlates significantly and strongly with outcomes. In our cohort of patients with acute coronary syndromes, most patients (64%) were in Killip‟s class I. 10% was in Killip‟s class IV. The distribution of Killip‟s class in
[image:75.612.90.455.284.506.2]our population is depicted below.
Figure 28: Distribution of Killip‟s functional class amongst study patients
making it a better risk stratification tool in the cohort of patients with acute coronary syndromes. A high NGAL value however was not able to significantly predict Killips class I versus the higher or worse outcome groups. This may actually be due to the fact that the NGAL molecule is a predictor for the worst categories of outcome in preference to the other less critical outcomes. This may actually be an aid towards risk stratifying the sickest patients from the others.
Thrombolysis
in
myocardial
infarction
(TIMI)
risk
stratification system
The TIMI group has laid down two tried and tested risk stratification systems for patients with acute coronary syndromes. The first is for UA/NSTEMI and the second is for STEMI. These scores are derived from ascertaining values to a composite of factors that summate to provide an integer which would be the corresponding risk score of adverse cardiac events and mortality for that particular patient. The methods of scoring are different for UA/NSTEMI and STEMI. However each of the integers that represent the TIMI risk score, correspond to a particular TIMI risk percentage that is independent of the manner of scoring.
Figure 29: Distribution of TIMI risk percentages in the population
In our cohort of patients we tried to correlate the TIMI risk percentage with the values of HSCRP of the subjects in an effort to test whether HSCRP predicts risk in a similar fashion. However there was no statistically significant correlation between HSCRP levels and TIMI risk percentage.
The admission troponin T levels also failed to show a significant correlation with the TIMI risk percentage in our cohort, indicating inability to predict TIMI risk class.
Figure 31: Non-significant correlation of Troponin T with TIMI risk percentage (p=0.632)
[image:78.612.102.508.191.562.2]Conventional echocardiography
Echocardiography was performed for all patients in the cohort during the admission for the acute coronary syndrome. The mean left ventricular ejection fraction in the group was found to be 43.6%, and the median value was 42%. There was a slight statistical trend towards a higher mean ejection fraction of 47.3% amongst patients with UA/NSTEMI as opposed to patients with STEMI who had a mean ejection fraction of 42.6% (p=0.054). 51 of the 87 patients (58.6%) of patients had an ejection fraction less than 45%. Echocardiography was repeated for the subjects at a follow up of one month.
Overall there was no statistically significant correlation between either the hospital left ventricular ejection fraction or the follow up left ventricular ejection fraction with the admission values of plasma NGAL or for that matter with any of the other biomarkers or inflammatory markers.
Figure 33: Negative correlation between ST deviation and hospital LVEF (p=0.05)
Strain echocardiography
laboratory, had their global longitudinal strains measured by speckle tracking on the GE machine (Vivid 9) at hospital admission. An attempt was made to do a similar strain echocardiography at follow up – however we were not able to do that in a significant proportion of the patients.
[image:82.612.109.451.317.678.2]81 of the 87 recruited patients (93.1%) had their global longitudinal strains measured on the GE machine. The mean global longitudinal strain value was -11.34 and the medium value was -11.4. The distribution of global longitudinal strain in the population is shown below.
The mean global longitudinal strain in the patients with STEMI was -11.07 and the mean value amongst patients with UA/NSTEMI was -12.23, the p value being non-significant at 0.195. Longitudinal strain correlated perfectly with the ejection fraction as determined by conventional echocardiography. The Pearson‟s correlation coefficient was -0.777 with a highly selective p value <0.001.
Figure 35: Statistically significant correlation of ejection fraction and strain
statistically significant correlation with strain, with a Pearson‟s correlation
[image:84.612.101.491.188.562.2]coefficient of 0.263 with a p value of 0.018 – the higher the value of troponin T the nearer the value of strain was towards zero.
Figure 36: Significant correlation of strain with admission Troponin T values
Coronary anatomy and interventions
was an observational cross-sectional study. However data was collected in all those patients who underwent angiography with respect to the coronary anatomy and any interventions if performed.
[image:85.612.89.454.428.668.2]68 (78.1%) of the 87 patients recruited in the study underwent coronary angiography. Of these 2 patients had minor disease or recanalised infarct related vessels with underlying minor disease. Single vessel disease was the most common form of angiographic finding with 38% of the patients undergoing angiograms, showing single vessel disease. Triple vessel disease was seen in 22% of the patients. Left main disease was noted in 5% of the patients. The mean values of plasma NGAL in the different categories of vessel disease was not found to be significantly different – in other words plasma NGAL values did not correlate with or predict progressively increasing number of vessel disease.
Figure 38: Distribution of the mean values of plasma NGAL and their dispersion in the various categories of angiographic vessel disease
Figure 39: Infarct related arteries according to the angiogram
[image:87.612.106.515.364.686.2]SYNTAX and Gensini scores were calculated for each of the significant angiograms of the cohort under study. The mean SYNTAX score was 16.14 and the median value was 15.75. Similarly the corresponding values for Gensisni score were 50.65 and 47 respectively. The distributions of SYNTAX scores and Gensini scores in the population are depicted below.
Figure 42: Distribution of Gensini scores in the population
Figure 43: Significant correlation between Gensini and SYNTAX scores
Figure 44: PCI categories
[image:91.612.89.454.353.576.2]Renal function
NGAL, as it is secreted by the nephrons, is expected to be elevated in kidney injury. As expected, in our cohort as well, it correlated significantly with the creatinine clearance calculated at admission. The Pearson‟s correlation
coefficient was -0.352, with a p value of 0.001.
[image:92.612.103.500.245.612.2]Clinical outcomes
In this study we had looked for certain defined clinical outcomes. Data regarding these outcomes were obtained at the time of admission to the hospital and subsequently each of the subjects was followed up through the entire course of hospitalization of the patient. Discharge characteristics were noted. The subjects were followed up once at one month interval. There was follow up beyond that period as well but such clinical follow up was not complete or exhaustive.
The following clinical outcomes are going to be analysed below: 1. All cause hospital mortality
2. All cause total mortality at one month inclusive of hospital mortality 3. Cardiogenic shock at presentation
4. Cardiogenic shock anytime during hospitalisation
5. Electrical and mechanical complications during hospitalisation 6. Duration of hospitalisation
7. Major adverse cardiac events up to one month after discharge.
All cause hospital mortality
Admission serum HSCRP was tested for its predictive power towards hospital mortality. However HSCRP failed to provide statistically significant odds ratios for predicting mortality in hospital.
Interestingly, high NGAL as opposed to low NGAL was able to
significantly predict all-cause mortality in the hospital on the bivariate
analysis. The calculated odds ratio of high NGAL to predict hospital all cause
hospital mortality was 6.078 (95% confidence intervals 1.318 – 28.033), p=
0.023, which was statistically significant.
All cause total mortality at one month inclusive of hospital mortality
There were 2 deaths in our study cohort in the following month after initial discharge – both were cardiovascular deaths. In our cohort, admission serum HSCRP was unable to significantly predict total mortality till one month follow up. The study was not powered to look for that particular endpoint, with respect to Troponin T and CKMB mass values.
High NGAL again was able to significantly predict all cause total
mortality at the end of one month in bivariate analysis. The odds ratio of high
NGAL to predict total mortality at one month was 5.8 (95% confidence
intervals 1.449 – 23.209), p=0.014, which was statistically significant.
Cardiogenic shock at presentation
High NGAL was able to significantly predict cardiogenic shock at
admission on the bivariate analysis. The odds ratio was 5.719 (95%
confidence interval 1.439 – 22.725), p= 0.015, which was statistically
significant.
Cardiogenic shock anytime during hospitalisation
Apart from the 10 patients with cardiogenic shock at presentation in our cohort, there were 11 more patients who developed cardiogenic shock during the duration of hospitalisation. Hence there were a total of 21 (24.1%) patients who suffered cardiogenic shock at some point in time during their admission. HSCRP at admission was not able to significantly predict this outcome.
Again high NGAL was able to successfully and significantly predict
this outcome on bivariate analysis. The odds ratio of high NGAL against this
particular outcome was 4.091 (95% confidence interval 1.417 – 11.814), p=
0.010, which was statistically significant.
Electrical and mechanical complications during hospitalisation
regurgitation. HSCRP and NGAL values were no