A Dissertation on
STUDY OF NEONATAL MORBIDITY AND MORTALITY
IN VERY LOW BIRTH WEIGHT NEONATES
ADMITTED IN NEONATAL INTENSIVE CARE
UNIT IN A TERTIARY CARE CENTRE
Dissertation submitted to
COIMBATORE MEDICAL COLLEGE COIMBATORE
in Partial fulfillment of the regulations for the award of the degree of M.D.PEDIATRIC MEDICINE
BRANCH
THE TAMILNADU Dr.M.G.R. MEDICAL UNIVERSITY CHENNAI- 600 032
CERTIFICATE
Certified that this dissertation entitled “STUDY OF NEONATAL MORBIDITY, MORTALITY IN VERY LOW BIRTH WEIGHT NEONATES ADMITTED IN NEONATAL INTENSIVE CARE UNIT IN A TERTIARY CARE CENTRE” is a bonafide work done by Dr. ABINAYA. G, M.D Post graduate student of Pediatric Medicine , Coimbatore Medical College & Hospital , Coimbatore – 641 018 during the
academic year 2016 – 2019.
Prof.Dr.V. Booma MD Professor and HOD of Pediatrics,
CERTIFICATE – II
This is to certify that this dissertation work titled “STUDY OF NEONATAL MORBIDITY, MORTALITY IN VERY LOW BIRTH WEIGHT NEONATES ADMITTED IN NEONATAL INTENSIVE CARE UNIT IN A TERTIARY CARE CENTRE” of the candidate Dr.ABINAYA. G, M.D with registration Number 201617301 for the award of
M.D Paediatrics, is personally verified by me from the urkund.com website for the purpose of plagiarism check. I found that the uploaded thesis file contains from introduction to conclusion 79 pages and result shows 3 % of plagiarism in the dissertation.
DECLARATION
I declare that this dissertation entitled “STUDY OF NEONATAL MORBIDITY AND MORTALITY IN VERY LOW BIRTH WEIGHT NEONATES ADMITTED IN NEONATAL INTENSIVE CARE UNIT IN A TERTIARY CARE CENTRE” has been conducted by me at NICU, Department of Pediatrics, Coimbatore Medical College and Hospital, under the guidance and supervision of my guide Prof.Dr.A.LAKSHMANASWAMY M.D., Dch., It is submitted in part of fulfillment of the award of the degree of M.D.Pediatrics for the MAY 2019 examination to be held under The Tamil Nadu Dr.M.G.R. Medical University, Chennai. This has not been submitted previously by me for the award of any degree or diploma from any other university.
ACKNOWLEDGEMENT
My sincere thanks to Prof.Dr.B.ASOKAN.M.S.Mch., DEAN, Coimbatore Medical College Hospital for allowing me to do this
ACKNOWLEDGEMENTS
I would like to express my sincere gratitude to Prof.Dr.V.Booma MD, Professor of Pediatrics, Coimbatore Medical College and Hospital for permitting me to undertake this study and for her guidance, invaluable help, encouragement and support throughout the study.
I am extremely thankful to Prof. Dr. A.Lakshmanaswamy MD.DCh, Prof.Dr.M.Geethanjali, MD.DCh, Prof. Dr. D. Rajkumar, M.D., for their guidance, encouragement and support throughout the study.
I would like to thank our Registrar, Dr.B.R.Sasi Kumar,MD.DCh., for his valuable guidance and support in doing this study.
I extend my sincere thanks to Assistant Professors Dr.N.Kumar MD, Dr.M.Senthil kumar.MD, Dr.A.Umashankar, Dr.P.Thiyagarajan.MD.Dch, Dr.A.Uma Maheswari.MD, Dr.S.Jayaprakash.MD,Dr.C.Karthikeyan,M.D, Dr.P.Senthil kumar.MD.DM, Dr.V.K.Sathyan.MD.DM, Dr.C.Suganya M.D. for their invaluable suggestion, help and support throughout the study.
I sincerely thank Mr.JOSHVA ALLEN SHEPHERD, for helping me in statistical analysis.
I sincerely thank all the parents of the neonates who gave consent to include their neonates in this study.
ABBREVIATIONS
VLBW - Very low birth weight
NNH - Neonatal hyperbilirubinemia
WHO - World health organization
GA - Gestational age
NICU - Neonatal intensive care unit
IVH - Intraventricular hemorrhage
HMD - Hyaline membrane disease
AAP - American association of pediatrics
NRP - Neonatal resuscitation program
PDA - Patent ductus arteriosus
NEC - Necrotising enterocolitis
AOP - Apnea of prematurity
SGA - Small for gestation
AGA - Appropriate for gestation
IUGR - Intrauterine growth restriction
RDS - Respiratory distress syndrome
GDM - Gestational Diabetes mellitus
PROM - Premature rupture of membranes
PIH - Pregnancy induced hypertension
CONTENTS
SL.NO TITLE PAGE NO:
1. INTRODUCTION
1
2. AIM & OBJECTIVES
8
3. JUSTIFICATION OF THE STUDY9
4. REVIEW OF LITERATURE10
5. METHODOLOGY
17
6. OBSERVATION & RESULTS
48
7. DISCUSSION
71
8. CONCLUSION
77
9. RECOMMENDATIONS
78
10. BIBLOGRAPHY
80
11. ANNEXURE
PROFORMA
83
CONSENT FORM
86
1
INTRODUCTION
Prematurity (Gestational age (GA) < 37 weeks) is the major cause
of morbidity in neonates especially very low birth weight (VLBW)
neonates.
The WHO defines Very low birth weight neonates as birth weight
less than 1500g at birth irrespective of gestational age.
Birth weight is the most important determinant of perinatal,
neonatal and postnatal outcomes. It is dependent on the length of the
gestation and the intrauterine growth of the fetus.
The Incidence of VLBW babies is less than 2 % of the births
globally. In India, VLBW babies constitute 4 % to 7 % of live births and
approximately 30 % of Neonatal death. The VLBW rate is an accurate
predictor of the infant mortality rate. VLBW infants account for more
than 50% of neonatal death.
Neonatal mortality rate is an important contributing factor for
underfive mortality rate. Out of the 26 lakh neonatal deaths occurring
2
Figure 1 shows birth weight specific neonatal mortality in united states, 1950, 1985 and 2008.
The main reason for increasing morbidity & mortality in VLBW
neonates is due to their physiologic & metabolic immaturity. These
neonates are prone for increased risk of hypoglycemia, jaundice, infection
& re-hospitalization during their neonatal period. VLBW is one of the
most serious challenges in Maternal and Child Health in developing
[image:13.595.107.502.78.406.2]3
Nearly half of neonates who survive to hospital discharge have
complications later which will affect the quality of their life.
Despite improvement in the neonatal care & facilities, neonatal
mortality remains high particularly in the developing countries.
By studying the factors associated with neonatal death, morbidity
& mortality in VLBW neonates can be reduced.
Hence my study will help to identify the factors contributing to the
morbidity and mortality in very low birth weight neonates admitted in
NICU. Necessary steps can be taken to reduce mortality in VLBW
neonates.
This kind of study has not been done in our hospital so far and it
4 CAUSE OF PRETERM BIRTH: FETAL
Fetal distress
Multiple gestation
Erythroblastosis
Non immune hydrops
PLACENTAL
Placental dysfunction
Placenta previa
Abruptio placenta
UTERINE:
Bicornuate uterus
Incompetent cervix (premature dilation)
MATERNAL
Pre eclampsia
5
Infection( Listeria monocytogenes, group B streptococcus, urinary
tract infection, bacterial vaginosis, chorioamnionitis)
Drug abuse
OTHERS
Premature rupture of membranes
Polyhydramnios
Iatrogenic
Trauma
PROBLEMS IN PREMATURE LOW BIRTH WEIGHT NEONATES RESPIRATORY SYSTEM:
- Respiratory distress syndrome
- Broncho pulmonary dysplasia
- Pneumothorax
- Congenital Pneumonia
- Apnea
CARDIOVASCULAR SYSTEM:
- Patent ductus arteriosus
- Hypotension
6 HEMATOLOGICAL
- Anemia
GASTROINTESTINAL SYSTEM:
- Poor gastro intestinal function
- Necrotizing enterocolitis
- Hyperbilirubinemia
METABOLIC:
- Hypocalcaemia
- Hypoglycemia
- Hypothermia
CENTRAL NERVOUS SYSTEM:
- Intraventricular hemorrhage
- Periventricular leukemia
- Seizures
- Retinopathy of Prematurity
- Deafness
7 RENAL:
- Hyponatremia
- Hypernatremia
- Hyperkalemia
- Renal tubular acidosis
- Edema
8
AIM & OBJECTIVES
To study the morbidity and mortality profile in very low birth
weight neonates in Neonatal Intensive Care Unit in Coimbatore Medical
College Hospital.
OBJECTIVES
1) To study the morbidity and mortality pattern in very low birth
weight neonates.
2) To study the maternal risk factors leading to very low birth
weight neonates.
3) To establish targeted preventive and advanced treatment
strategies in specific areas.
4) To plan for future research in areas of increased admission and
9
JUSTIFICATION OF THE STUDY
In recent trends, there is increasing number of babies born with
very low birth weight. These VLBW babies are at risk of developing
Hypoglycemia, Sepsis, Hyperbilirubinemia, Respiratory distress when
compared to term babies. By studying the risk factors leading to very low
birth weight and their morbidities, health professionals will be able to
anticipate and manage them accordingly. As a result, we will be able to
prevent complications in these neonates.
Identification of morbidity and mortality in VLBW neonates will
help us in formulating and implementing interventions to reduce neonatal
10
REVIEW OF LITERATURE
Jaiswal et al2., has done a prospective cohort study to compare early neonatal morbidity (Within 7 days of life) in late preterm infants
with term infants. This study was conducted at the Fernandez hospital,
Hyderabad. 363 of late preterm infants and 2707 of term infants were
included in the study. 257 (70.8 %) of late preterm and 788 (29.1%) of
term infants had requiring inpatient morbidities admission within first 7
days of life. Neonatal jaundice requiring phototherapy (55.1%) followed
by respiratory morbidity (10.5%) and hypoglycemic (8.8%) were the
frequent identified morbidities in late preterm infants, while neonatal
Jaundice (24.8%) was the most frequently identified morbidity in term
infants. Compared with term infants, late preterm infants were at 5.5
time’s higher risk for over all morbidity. Cesarean delivery, IUGR and
multiple pregnancy status significantly Contribute to neonatal
morbidities.
Schindler et al3., did a retrospective analysis of prospectively collected data of all 10 NICU’s in New South Wales and Australian
Capital Territory. All Live born infants less than 32 weeks gestation
11
The most common cause of death across all gestational groups was major
IVH followed by Acute Respiratory Illness and Sepsis.
Kabilan et al4., did a cross sectional retrospective study at level three SNCU between October 2016 and September 2017 in Govt. Stanley
medical College, Chennai, Tamil Nadu. There were 154 VLBW infants
registered. 75 Females (48.7%) and 79 (51.3%). Majority of them were
in the gestational age 33-36 weeks (n=68, 44.2%), small for gestational
age (n=89, 57.8), delivered through normal vaginal delivery(n=95,
61.7%),maternal age 21-30 (n=95, 61.6%), on antenatal steroids (n=59,
38.3%), maternal disease were present in 55 mothers (33%) and
gestational hypertension being more common (n=14, 9.6%). The mean
birth weight is 1.198 (SD= 0.211). The mean gestational age in weeks
was 31.9(SD= 3.095). This study reveals that birth weight and
mechanical Ventilation are the 2 major factors responsible for mortality
in VLBW babies. Major cause of morbidity was RDS (n=56, 33.6%),
birth asphyxia (n=54, 32.4%) and Sepsis (n=46, 27.6%). Mortality of
40.3% (n=62) observed in this study. Most of the death occurred due to
12
Ghulam Nabi Rather et al5., done a prospective study in the Department of Pediatrics and Neonatology at G.B. Pant General Hospital,
from April 2012 to March 2013. This was undertaken to study the
incidence, early neonatal morbidity and mortality in late preterm infants
(34-36 6/7 weeks). A total of 4100 neonates were included in the study.
Incidence of late preterm neonates was 11.58%.365 (76.8%) late preterm
neonates and 965(28.3%) term neonates were admitted. Compared with
term infants, late preterm infants were at significantly higher risk for
Sepsis, Jaundice, Hypoglycemia, Mechanical Ventilation and Perinatal
Asphyxia. Jaundice (41.6% compared to 15.3%), Hypoglycemia (16%
compared to 6.5%), Respiratory morbidities (11.2% compared to 2.1%),
sepsis (4.8% compared to 1.53%), Perinatal asphyxia (2.9% compared to
1.9%) were all significantly higher in late preterm babies as compared to
term babies. Early neonatal mortality in late preterm neonates was 2.5%
or 25/1000 live births.
Rasania M et al6 had done a retrospective cohort study using previously collected data from neonates who were admitted at SNCU of
Dhiraj hospital, Gujarat, India between January 2015 to December 2015.
It was done to study the morbidity profile and immediate outcome of late
13
168 late preterm and 1025 term neonates were included in the
study. Of 122 late preterm admitted in SNCU, 16.39% had birth
asphyxia, 28.6% had sepsis, 7.37% had RDS and 32.78% had
hyperbilirubinemia. Morbidities were relatively higher in out born late
preterm neonates. Need for respiratory support was significantly higher in
moderate preterm compared to late preterm (47.8% versus 5.95%).
Thapar K et al7., has done a study about morbidity and mortality of very low birth weight babies in a tertiary level NICU. It was an
observational study and conducted in NICU of SGRDIMS&R, Amritsar,
over the period of 18 months (1st October 2013 to 31st march 2015). A total of 75 VLBW infants were observed during this period and neonatal
outcome was assessed.
Sepsis (77.3%) was the major cause of morbidity in VLBW
neonates followed by HMD (66.7%) and Jaundice (65.3%). Sepsis along
with other factors play an important role in neonatal mortality (p=0.083).
Out of the total nine mortality, three cases were associated with IVH (p
value< 0.001). Pneumothorax was an associated factor in three cases (p
value <0.001). Sepsis, HMD, metabolic complications like hypoglycemia
14
Another study8 was conducted at the University Hospital of the Institute of Medical Science, Banaras Hindu University, India over a
period of three years. It was a retrospective cohort study and its objective
was to determine the Pediatrics of mortality in VLBW neonates. A total
of 260 VLBW newborn were enrolled. 96 babies (36.9%) died. Survival
rate increased with increase in birth weight and gestational age. Perinatal
asphyxia, Apnea, neonatal sepsis and shock are the factors directly
responsible for neonatal mortality. The presence of maternal bleeding and
failure to administer steroids to the mother when premature delivery is
anticipated are the antenatal predictors of mortality.
Sangamam et al9. conducted a cross sectional study to assess the perinatal morbidity and mortality among low birth weight babies and to
determine the associated maternal health and socio demographic factors.
This study was done in KMCT medical college, Kerala. All the babies
with birth weight > 1000 g but less than 2500 g and their mothers were
included in the study. A total of 1002 low birth weight babies, 982
mothers were included in the study. Very low birth weight babies < 1500
g had 10 times more mortality rates when compared to babies with birth
weight between 1.5- 2.5 kg. Preterm and growth restricted babies had the
worst perinatal outcomes. The most common perinatal complication was
15
Hyaline membrane disease (14.86 %). The most common maternal
complications associated with LBW were anemia (43.36%) and
hypertensive disorders of pregnancy (17.6%).
There were 49 early neonatal deaths accounting to 5.29% of live
babies. The major causes of neonatal death were hyaline membrane
disease (3.56%) and birth asphyxia (1.11%).
Ballot et al10 conducted a retrospective review of patients’ records from a neonatal computer database for 562 VLBW infants. These
neonates weighed between 500 and 1500 g at birth, and were admitted
within 48 hours after birth between 01 January 2013 and 31 December
2013. This study aimed to review morbidity and mortality in very low
birth weight (VLBW) infants in 2013 compared with similar data from
2006/2007. Survival in 2013 was similar to that in 2006/2007 (73.4% vs
70.2%, p = 0.27). However, survival in neonates who weighed 750–900 g
significantly improved from 20.4% in 2006/2007 to 52.4% in 2013 (p =
0.001). The use of nasal continuous positive airway pressure (NCPAP)
increased from 20.3% to 62.9% and surfactant use increased from 19.2%
to 65.5% between the two time periods (both p < 0.001). The main
determinants of survival to discharge in 2013 were birth weight (odds
16
(2.673, 1.375–5.197), NCPAP (0.247, 0.109–0.560), necrotising
enterocolitis (4.555, 1.659–12.51), and mode of delivery, including
normal vaginal delivery (0.456, 0.231–0.903) and vaginal breech (0.069,
0.013–0.364). The major cause of mortality was Extreme prematurity
17
METHODOLOGY
STUDY DESIGN:
Prospective Cohort Study
STUDY PLACE:
Neonatal Intensive care unit, Coimbatore Medical College
Hospital.
STUDY POPULATION:
All VLBW neonates admitted in Neonatal Intensive Care Unit.
STUDY PERIOD:
January 2017 – December 2017.
SELECTION CRITERIA: Inclusion Criteria:
All very low birth weight neonates admitted in NICU between
January 2017 to December 2017.
Exclusion Criteria:
1. Neonates with major congenital anomalies.
18
All VLBW neonates were included in the study after getting
written informed consent from the parents for using their neonates’
clinical data for the study purpose. Ethical committee clearance were also
obtained.
All VLBW neonates admitted in our NICU were enrolled in the
study. Relevant details were collected which includes maternal details
like their age , address , socioeconomic status, educational status,
maternal weight, risk factors (Hypertension, Anemia, Gestational
Diabetes mellitus, Multiple gestation, Chronic medical illness,
Hypothyroidism, HIV status, Hepatitis B, Maternal fever), order of birth,
gestational age , Antenatal steroids, premature rupture of membranes,
mode of delivery and Baby’s details include their sex, need of
resuscitation, Apgar score, gestational age, birth weight and their illness ,
need of mechanical ventilation and surfactant therapy were recorded.
ROUTINE CARE IN DELIVERY ROOM:
Low risk neonates may initially be placed on mother’s abdomen
after delivery. Secretions from mouth can be cleared using a bulb syringe
or soft catheter. Spontaneously breathing neonates with no distress do not
need any assisted method to clear their airway. Delayed clamping of cord
19
Apgar score is a routine method of systematically assessing
newborn infants immediately after birth. It was not designed to predict
the neurological outcome. The incidence of cerebral palsy is low in
neonates with Apgar scores of 0-3 at 5 minutes, but higher than in infants
with Apgar scores of 7-10. Low Apgar score and umbilical artery blood
pH predict neonatal death.
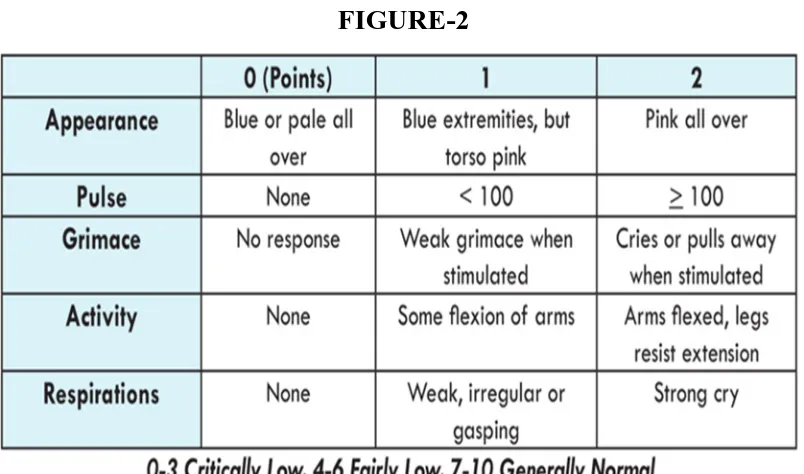
[image:30.595.114.516.352.589.2]APGAR SCORING11
20 Need for Resuscitation at birth:
- Resuscitation is carried out based on NRP Protocol.
- Apgar at 1st and 5th minute of birth.
- Need for PPV / Chest compression.
- Temperature regulation is the foremost goal.
22 Thermoneutral environment (TNE)
TNE refers to a narrow range of environmental temperature at
which the basal metabolic rate (BMR) of the baby is at a minimum,
oxygen consumption is at least and baby maintains its normal body
temperature is called thermoneutral range of temperature.
Warm chain:
The warm chain is a set of ten interlinked steps carried out at birth and
later which will reduce the chances of hypothermia in all newborns
1. Thermal care in delivery room
2. Warm resuscitation
3. Immediate drying
4. Skin to skin contact
5. Breastfeeding
6. Bathing
7. Clothing and bedding
8. Rooming in
23 10. Training and awareness rising
Apart from routine procedures, extra care is necessary to prevent
hypothermia in preterm babies.
Preterm babies < 34 weeks should be nursed in Incubator which
decreases the insensible water loss.
Mechanism :
Convective heat loss dependent on air flow, the incubators reduce
the exposure of babies to air currents. Evaporative process of heat loss
will be limited by providing maximum possible relative humidity within
the incubator. Radiative heat losses are minimized by the hood on the
baby or by using double walled incubators.
Perinatal Asphyxia:
Definition according to ACOG guidelines include
a) Profound metabolic or mixed academia (pH < 7) in Umbilical
cord blood.
b) Persistence of low Apgar score less than 3 for more than 5
24
c) Signs of neonatal neurologic dysfunction ( e.g. : seizures,
encephalopathy, tone abnormalities)
d) Evidence if multiple organ involvement.
25
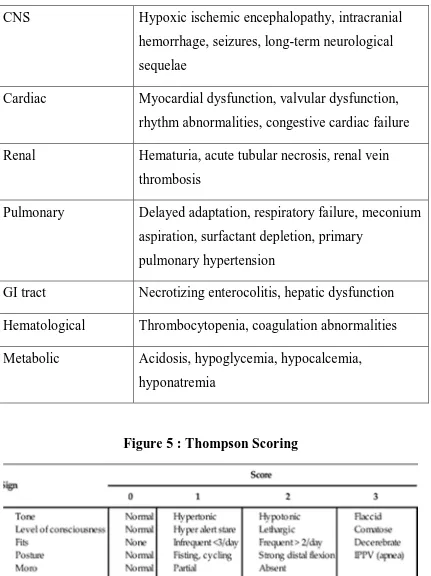
TABLE 1 : Organ system dysfunction in perinatal asphyxia CNS Hypoxic ischemic encephalopathy, intracranial
hemorrhage, seizures, long-term neurological sequelae
Cardiac Myocardial dysfunction, valvular dysfunction, rhythm abnormalities, congestive cardiac failure
Renal Hematuria, acute tubular necrosis, renal vein thrombosis
Pulmonary Delayed adaptation, respiratory failure, meconium aspiration, surfactant depletion, primary
pulmonary hypertension
GI tract Necrotizing enterocolitis, hepatic dysfunction
Hematological Thrombocytopenia, coagulation abnormalities
[image:36.595.105.536.95.671.2]Metabolic Acidosis, hypoglycemia, hypocalcemia, hyponatremia
26 Respiratory Distress:
a) Tachypnea ( RR ≥ 60/min )
b) Retractions
c) Grunting
d) Scoring – Silverman & Down score chart.
27
FIGURE-712 - DOWNE’S SCORE:
Indications for respiratory support
Indications for CPAP in Preterm infant:
Preterm infant with minimal respiratory distress and low
supplemental oxygen requirement.
Requirement of Fio2 above 30 % by hood with respiratory
distress
Fio2 above 40 % by hood
28
Initial management of premature infants with severe respiratory
distress.
Respiratory distress after extubation.
To maintain lung volume after extubation.
Indications for Mechanical Ventilation:
Prolonged Apnea
Pao2 <50 mmHg or Fio2 above 80 %
Paco2 above 60mmHg with persistent academia
General Anaesthesia.
SURFACTANT THERAPY:
Surfactant Replacement Therapy must be considered in all preterm
infants with ~28 week gestational age with a clinical suspicion of RDS.
Use in infants of gestational age 24 to 27 weeks may be decided on a
case-by-case basis. Early rescue therapy where surfactant is administered
early but after the onset of respiratory distress, is very effective in
decreasing the incidence of RDS and mortality in preterm infants. An
29
Administration. The optimal dose of surfactant for RDS is 100
mg/kg body weight of phospholipid.
ASSESSMENT OF GESTATIONAL AGE
Gestational age can be assessed by 3 methods.
First trimester Ultra sonogram:
- Done at 6- 12 weeks of gestation.
- Most reliable method of assessing age of gestation.
First day of last menstrual period.
New Ballard Scoring:
- Used to assess Gestation age 20 – 44 weeks
- Score ranges from -10 to + 50
- Consist of two components
1. Physical Maturity
30
31
FIGURE-9 : NEUROMUSCULAR MATURITY
KANGAROO MOTHER CARE:
Kangaroo mother care is a method of care of preterm or low birth
weight (LBW) infants by placing them in skin to skin (STS) contact with
mother or other caregiver in order to ensure optimum growth and
32 Components of KMC 6-8
1. Kangaroo position
- The kangaroo position consists of skin-to-skin contact (SSC)
between the mother and the infant in a vertical position, between
the mother’s breasts and under her clothes
- The provider must keep herself in a semi- reclining position to
avoid the gastric reflux in the infant
- The kangaroo position is maintained until the infant no longer
tolerates it- as indicated by sweating in the baby or baby refusing
to stay in KMC position
- When continuous care is not possible, the kangaroo position can
be used intermittently, providing the proven emotional and
breastfeeding promotion benefits
- The kangaroo position must be offered for as long as possible
33 2. Kangaroo nutrition
- Kangaroo nutrition is the delivery of nutrition to “kangarooed”
infants as soon as oral feeding is possible.
- Goal is to provide exclusive or nearly exclusive breastfeeding
with fortification, if needed.
3. Kangaroo discharge and follow up
- Early home discharge in the kangaroo position from the neonatal
unit is one of the original components of the KMC intervention.
- Mothers at home require adequate support and follow up hence a
follow-up program and access to emergency services must be
ensured.
34 Hypoglycemia:
a) WHO defines hypoglycemia as Blood glucose of less than 45
mg/dl.
b) Blood sugars are monitored by using glucometer and plasma
glucose.
Indication for routine blood screening:
Low birth weight infants
Preterm infants
Small for gestation
Large for gestation
Infant of Diabetic mother
Any sick neonate – perinatal asphyxia, sepsis, shock
Infants on total parental nutrition
Infant born to mother receiving oral propranolol, Labetalol, oral
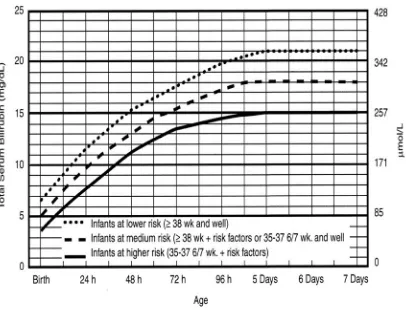
35 Neonatal Hyperbilirubemia:
a) Based on hour specific nomogram as per AAP guidelines,
phototherapy or exchange transfusion was given.
TABLE : 2 IMPORTANT RISK FACTORS FOR SEVERE HYPERBILIRUBINEMIA
Predischarge TSB or TcB measurement in high risk or high intermediate zone
Lower gestational age
Exclusive breastfeeding, especially if it is not going well and infant has excessive weight loss
Jaundice in the first 24 hours of age
Isoimmune or other hemolytic disease
Previous sibling with jaundice
Cephalohematoma or significant bruising
36
37
[image:48.595.107.545.388.676.2]Suggested Use of Phototherapy and Exchange Transfusion in Preterm Infants <35 Weeks Gestational Age
38 Neonatal Sepsis:
a) Neonatal Sepsis is a clinical syndrome characterised by signs and
symptoms of infection in the first month of life.
b) Classified into two categories.
1) Early onset Sepsis (EOS).
2) Late onset Sepsis. (LOS)
Sepsis is recorded as
Suspected sepsis- based on clinical symptoms and signs of
sepsis.Antibiotics given atleast for two days.
Probable sepsis- based on positive screening test for sepsis. CRP
is taken as 10 mg/dl
Culture positive sepsis
Risk Factors associated with early onset sepsis:
1) Low birth Weight (< 2500 g) or prematurity.
2) Febrile illness in the mother with evidence of bacterial infection
39
3) Foul smelling / meconium stained liquor.
4) Rupture of membranes > 24 hours.
5) Single unclean >3 sterile vaginal examinations.
6) Prolonged labor (sum of 1st & 2nd stage of labor ≥ 24 hours).
[image:50.595.97.533.344.593.2]7) Perinatal Asphyxia (Apgar score < 4 at 1minute).
TABLE 3 : SEPSIS SCREEN:
COMPONENTS ABNORMAL VALUE
Total leukocyte count <5000/mm3
Absolute neutrophil count Low counts
Immature / Total neutrophil >0.2
Micro – ESR >15 mm in 1st hour
40
TRANSIENT TACHYPNEA OF NEWBORN:
The incidence of TTN is 0.3% to 0.6% of term deliveries and 1%
of preterm deliveries.
Risk factors for TTN include cesarean delivery with or without
labor, precipitous birth, and preterm birth. These conditions are thought
to result in delayed or abnormal fetal lung fluid clearance due to the
absence of the hormonal changes that accompany spontaneous labor. It is
characterized by
- Tachypnea
- Signs of mild respiratory distress
- Fio2 requirement < 40 %
- Signs of TTN persist for 12 to 24 hours in mild cases ; 72
hours in severe cases
- Chest radiograph reveals characteristic prominent perihilar
streaking (Sunburst pattern)
41
- Hyper aeration with widening of intercostal spaces, mild
cardiomegaly, widened and fluid-filled inter lobar fissure, and
mild pleural effusions may also be observed.
The radiographic findings in TTN usually improve by 12 to 18 hours and
resolve by 48 to 72 hours.
Treatment:
Treatment is mainly supportive with provision of supplemental
oxygen as needed. More severe cases may respond to continuous positive
airway pressure (CPAP) to improve lung recruitment
PATENT DUCTUS ARTERIOSUS:
PDA is commonly seen in preterm babies.
Clinical diagnosis of PDA:
- Bounding peripheral pulse
- Wide pulse pressure( 25 mm Hg )
- Hyperactive precordium
- Systolic murmur
42
Echocardiography is the gold standard for diagnosis as well as for
assessing severity of PDA. The features suggestive of patent ductus
arteriosus include
a) 2-D and color Doppler- short axis view: Direct visualization of
the ductus. In 2-D short axis view, in the presence of a patent
ductus, the appearance is classically described as ‘three-legged
stool’ appearance. In color Doppler, there is continuous flare in
the MPA.
b) Short axis view, Pulsed Doppler: Turbulence in main pulmonary
artery (MPA) due to left to right shunt jet flowing into MPA.
c) Four chamber view: Bowing of interatrial septum to right with
enlarged left atrium and left ventricle
d) Long axis view: LA/Ao ratio > 1.5:1
43
TABLE 4 : ECHOCARDIOGRAPHY - PDA Echocardiography
parameter* No PDA Mild Moderate Large Features of ductus arteriosus
Trans ductal diameter
(mm) 0 <1.5 1.5-3.0 >3.0
Ductal velocity Vmax
(cm/sec) 0 >2 1.5-2.0 < 1.5
Antegrade PA diastolic
flow (cm/sec) 0 >30 30-50 >50
Pulmonary overcirculation Left atrial /aortic root
width ratio 1.1 ± 0.2 <1.4:1 1.4-1.6 >1.6:1 Left ventricular/ aortic
root width ratio 1.9 ± 0.3 - 2.2 ± 0.4 2.27± 0.27
E wave/ A wave ratio <1 <1 1-1.5 >1.5
IVRT(ms) <55 46-54 36-45 <35
LVSTI 0.34 ± 0.09 - 0.26 ±
0.03 0.24 ± 0.07 Systemic hypoperfusion
Retrograde diastolic flow
(as % of forward flow) 10 < 30 30-50 > 50 Aortic Stroke Volume
(ml/kg) <2.25 - - >2.34
Left ventricular output
(ml/kg/min) 190-310 - - >314
44 Hemodynamically significant PDA:
Presence of PDA >1.5 mm with one of the following
- LA/Ao ratio >2.2:1
- Retrograde diastolic flow in descending aorta, celiac or
cerebral arteries > 30% of antegrade flow
- Left ventricular output > 320 ml/kg/min
RETINOPATHY OF PREMATURITY:
ROP is a vaso-proliferative disorder of the retina among
preterm infants. Neonates at less than 32 weeks of gestation are at risk of
developing ROP. Screening for ROP should be performed in all preterm
neonates who are born
< 34 weeks gestation and/or < 1750 grams birth weight ; in babies
34-366/7 weeks gestation or 1750-2000 grams birth weight if they have
risk factors for ROP. The first retinal examination should be performed
not later than 4 weeks of age or 30 days of life in infants born ~ 28 weeks
of gestational age. Infants born < 28 weeks or < 1200 grams birth weight
should be screened early, by 2-3 weeks of age, to enable early
45 FIGURE- 13
INTRAVENTRICULAR HEMORRHAGE:
IVH is common in preterm infants and the incidence is currently 15
to 20% in infants born at < 32 weeks of gestation.
46
TABLE-5 : VOLPE GRADING OF IVH
SEVERITY OF IVH FINDINGS
Grade 1 GMH with no or minimal IVH (10%
ventricular volume)
Grade 2 IVH occupying 10% - 50% of ventricular area on parasagittal view
Grade 3 IVH occupying > 50% of ventricular area on parasagittal view usually distends lateral ventricle (at the time of IVH diagnosis)
Grade 4 (separate notation)
Periventricular echodensity
APNEA OF PREMATURITY:
Apnea is defined as cessation of airflow for more than 20 seconds
accompanied by bradycardia or hypoxemia that is evident clinically
(cyanosis) or by oxygen saturation monitoring. Incidence of apnea
increases with decreasing gestational age. It is treated by caffeine
Caffeine- Loading dose of 20 mg/kg intravenous or orally over 30
minutes followed by maintenance dose of 10mg/kg of caffeine single
47 NECROTISING ENTEROCOLITIS:
NEC is the most common gastrointestinal emergency of the
neonate. Prematurity is the most common risk factor. Early enteral
[image:58.595.113.525.317.629.2]feeding, bovine milk based products may increase the risk of NEC
48
RESULTS
A total of 382 VLBW neonates were included in the study. Out of 382
[image:59.595.110.519.289.688.2]VLBW neonates, 199(52%) were males and 183(48%) were females.
TABLE 6 : AGE DISTRIBUTION
Gender
VLBW Neonates
n (%)
MALE 199 52%
FEMALE 183 48%
MALE 52%
Gender Distribution[N=382]
49
TABLE 7 : BIRTH LOCALITY
Locality
VLBW Neonates
n (%)
In Born 231 60%
Out Born 151 40%
Out of 382 VLBW neonates, 231(60%) were inborn and 151(40%) were out born.
In Born 60% Out Born
40%
50
TABLE 8 : MEAN BIRTH WEIGHT OF VLBW NEONATES MEAN BIRTH WEIGHT OF VLBW NEONATES
Mean SD Std. Error
MALE 1.250 0.120 0.008
FEMALE 1.274 0.125 0.009 Total 1.261 0.123 0.006
Mean birth weight was 1.25 kg in males and 1.27 kg in females with
standard deviation of 0.12.
Out of 382 VLBW babies, 195(51%) were born out of normal
51
TABLE 9 : MODE OF DELIVERY Mode of Delivery
Normal
VLBW Neonates
n (%)
LSCS 199 52%
FEMALE 183 48%
Among 382 VLBW neonates, 222(58%) were SGA, 92(24%) -AGA,
68(18%) were IUGR. The percentage of SGA babies were more among
them.
Normal 51% LSCS
49%
52
TABLE 10 : GESTATIONAL AGE
GA
VLBW Neonates
n (%)
SGA 222 58%
AGA 92 24%
IUGR 68 18%
Majority of VLBW neonates were in the gestational age group between
28-32 weeks (n = 224, 59%) and 32-34 weeks (n = 92, 24%)
0% 10% 20% 30% 40% 50% 60%
SGA AGA IUGR
53
TABLE 11 : GESTATIONAL AGE GESTATIONAL
AGE
VLBW Neonates
n (%)
< 28 weeks 24 6%
28-32 weeks 224 59%
32-34 weeks 92 24%
34-36 weeks 42 11%
The most common maternal risk factor associated with VLBW being
Gestational hypertension -210(55%) followed by Anemia – 63(17%),
Gestational diabetes mellitus- 8(2%), Hypothyroidism- 4(1%). 90 VLBW
54
TABLE 12 : MATERNAL RISK FACTORS
Maternal Risk
Factors Number (%)
No Risk 90 23.5
Gestational
Hypertension 210 55
Anemia 63 17
Hypothyroid 4 1
Gestational Diabetes 8 2
HIV 1 0.5
Multiple Gestation 0 0
Chronic Medical
Illness 0 0
55
Most of the mothers belong to low socioeconomic status. Table 13 shows
maternal age < 18 years were 10(2.5%) and most of the mothers were in
the age 18-21 years - 136(35.5%) followed by 194(51%) between 21-30
years, 42(11%) in the age > 30 years. Maternal hypertension being the
most common cause for VLBW babies. Only 2(0.5%) out of 382 were
meconium stained and 389(99.5%) had clear amniotic fluid. Antenatal
steroids coverage being 325(85%).
No Risk Gestatio nal Hyperte nsion Anemia Hypothy roid Gestatio nal Diabetes HIV Multiple Gestatio n Chronic Medical Illness Hepatitis B
Number 90 210 63 4 8 1 0 0 0
(%) 23.5 55 17 1 2 0.5 0 0 0
0 50 100 150 200 250
56
TABLE 13 : MATERNAL DETAILS Maternal Details
Maternal Age (Years) Number (%)
<18 10(2.5%)
18-21 136(35.5%)
21-30 194(51%)
>30 42(11%)
Maternal Disease
Gestational Hypertension 210(55%)
Anemia 63(17%)
Hypothyroid 4(1%)
Gestational Diabetes 8(2%)
HIV 1(0.5%)
Multiple Gestation 0
Chronic Medical Illness 0
Hepatitis B 0
Aminotic Fluid
Clear 389(99.5%)
Meconium Stained 2(0.5)
Antenatal Steroids 325(85%)
Table 14 depicts the findings from the study. Most of them were in the
gestational age 28-32(n = 224, 59%) and 32-34 weeks (n = 92, 24%) and
small for gestational age (n = 222, 58%).out of 382 VLBW neonates,
183(48%) were females and 197(52%) were males, 231 (60%) were
57
TABLE 14 : CHARACTERISTIC FEATURES OF THE STUDY
Characteristic Features of the Study
Number (%)
Gender
Female 183 (48%)
Male 197 (52%)
Gestational Age
<28 Weeks 24 (6%)
28-32 weeks 224 (59%)
32-34 Weeks 92 (24%)
34-36 Weeks 42 (11%)
Place of Birth
Inborn 231 (60%)
Outborn 151 (40%)
SGA 222 (58%)
AGA 92 (24%)
IUGR 68 (18%)
Table 15 shows 195(51%) normal vaginal deliveries and 187(49%) were
born by LSCS. Resuscitation at birth required for 24(6.3%).Surfactant
therapy was given for 43(11%), NCPAP for 62(16%), Mechanical
58
TABLE 15 : DELIVERY & INTERVENTIONS
Delivery & Interventions
Number (%)
Mode of Delivery
Normal 195 (51%)
LSCS 187 (49%)
Resuscitation
Required 24 (6.3%)
Surfactant 43 (11%)
NCPAP 62(16%)
Mechanical
Ventilation 71 (18.5%)
Table 16, shows the morbidity pattern in very low birth weight neonates.
The most common morbidity among VLBW neonates being sepsis (n =
133, 35%), RDS (n = 105, 27%), TTN (n = 85, 22%), Hypoglycemia (n =
47, 12%), NNH (n = 31, 8%). Perinatal asphyxia (n = 24, 6%), meningitis
(n = 24, 6%) were the other major morbidities.
59
TABLE 16 : MORBIDITY PATTERN IN VLBW NEONATES
Disease
VLBW Neonates
n (%)
SEPSIS 133 35%
RESPIRATORY DISTRESS SYNDROME 105 27% TRANSIENT TACHYPNEA OF
NEWBORN 85 22%
HYPOGLYCEMIA 47 12%
NEONATAL HYPERBILIRUBINEMIA 31 8%
ASPHYXIA 24 6%
MENINGITIS 24 6%
INTRAVENTRICULAR HEMORRHAGE 15 4%
SHOCK 15 4%
PNEUMONIA 10 3%
HYDROCEPHALUS 8 2%
PATENT DUCTUS ARTERIOSUS 6 2%
APNEA OF PREMATURITY 9 2%
NECROTISING ENTEROCOLITIS 7 2%
RETINOPATHY OF PREMATURITY 5 1%
INFANT OF DIABETIC MOTHER 5 1%
PNEUMOTHORAX 2 1%
60
SEPSI
S RDS TTN HYP OGLY CEMI A NNHASPH YXIA MENI NGITI S IVH SHO CK PNE UMO NIA HYD ROCE PHAL US
PDA AOP NEC ROP IDM PNE UMO
THO RAX
MAS
Series1 133 105 85 47 31 24 24 15 15 10 8 6 9 7 5 5 2 2
Series2 35% 27% 22% 12% 8% 6% 6% 4% 4% 3% 2% 2% 2% 2% 1% 1% 1% 1%
0 20 40 60 80 100 120 140
61
TABLE 17 : RDS BABIES REQUIRING SURFACTANT
Out of 382 VLBW neonates, 105 neonates had RDS. Among them, 43
neonates (41%) received surfactant therapy.
0 20 40 60 80 100 120
RDS
SURF 41%
RDS SURF
n 105 43
RDS REQUIRING SURFACTANT THERAPY
RDS babies requiring surfactantDisease RDS SURF %
62
TABLE 18 :NNH BABIES REQUIRING EXCHANGE TRANSFUSION
NNH babies requiring Exchange transfusion
Disease NNH EXCHANGE %
n 31 4 13%
31 VLBW neonates were admitted for neonatal hyperbilirubinemia. Out
of 31 neonates, exchange transfusion was done for 13% (n = 4), others
received phototherapy.
0 5 10 15 20 25 30 35
13%
NNH EXCHANGE
Series1 31 4
EXCHANGE TRANSFUSION IN NNH BABIES
EXCHANGE
63
TABLE 19 :OUTCOME
Outcome
VLBW Neonates
n (%)
SURVIVAL 287 75%
DEATH 95 25%
Table 19 shows that 285(75%) VLBW neonates survived and 95(25%)
neonates died.
Survival 75%
Death 25%
[image:74.595.121.508.185.525.2]64
TABLE 20 : MORTALITY
Mortality Number (%)
Sepsis 49 52
RDS 38 40
Asphyxia 0 0
Meningitis 1 1
Pneumothorax 2 2
Pre-maturity 1 1
IVH 4 4
Table 20 shows the major cause of mortality in VLBW neonates were
found to be Sepsis 49 (52%), followed by Respiratory Distress syndrome
38 (40%). Other causes accounted to 8% of total VLBW neonatal death.
RDS 40%
Sepsis 52% Meningitis
1%
PneumoThorax 2%
IVH 4%
prematurity 1%
[image:75.595.136.496.477.722.2]65
TABLE 21 : TIME OF DEATH
Duration
VLBW Neonates
n (%)
< 24 hours 7 7%
24 - 48 hours 11 12%
48- 72 hours 12 13%
3 Days 65 68%
Table 21 shows out of 95 neonatal death, 7(7%) occurred within 24 hours
of birth, 11(12%) between 24- 48 hours, 12(13%) between 48- 72 hours,
65(68%) occurred after 3 days.
Most of the VLBW neonates were died after 3 days (68%).
<24 Hrs
7% 24-48 Hrs 12%
48-72 hrs 13%
3 Days 68%
66
TABLE 22 :ASSOCIATION OF GENDER WITH OUTCOME
GENDER
OUT COME
TOTAL
SURVIVAL DEATH
MALE 135 64 199
FEMALE 152 31 183
TOTAL 287 95 382
No significant association of Gender with Outcome.
MALE FEMALE
ALIVE 47% 53%
DEATH 67% 33%
0% 10% 20% 30% 40% 50% 60% 70% 80%
67
TABLE 23 :ASSOCIATION OF BIRTH LOCALITY WITH OUTCOME
LOCALITY
OUT COME
TOTAL SURVIVAL DEATH
In Born 173 58 231
Out Born 114 37 151
TOTAL 287 95 382
Place of birth had no correlation with outcome of very low birth weight neonates.
In Born Out Born
ALIVE 60% 40%
DEATH 61% 39%
0% 10% 20% 30% 40% 50% 60% 70%
68
TABLE 24 :ASSOCIATION OF GESTATIONAL AGE WITH OUTCOME
Gestational Age
OUT COME
TOTAL SURVIVAL DEATH
<28wks 10 14 24
28-32wks 161 63 224
32-34wks 79 13 92
34-36wks 37 5 42
TOTAL 287 95 382
There is significant association of gestational age with outcome of very
69
TABLE 25 :ASSOCIATION OF MODE OF DELIVERY WITH OUTCOME
DELIVERY
OUT COME
TOTAL SURVIVAL DEATH
NORMAL 143 52 195
LSCS 144 43 187
TOTAL 287 95 382
Outcome of VLBW neonates was not affected by Mode of delivery.
NORMAL LSCS
ALIVE 50% 50%
DEATH 55% 45%
0% 10% 20% 30% 40% 50% 60%
70
TABLE 26 : Gestational Age with Time of Death Gestational
Age
Time of Death
48-72Hrs 3
Days Total < 24 Hrs 24 - 48 Hrs
28wks 2 3 1 8 14
28-32 4 5 9 45 63
32-34 0 3 2 8 13
34-36 1 0 0 4 5
TOTAL 7 11 12 65 95
There is significant association between gestational age and time of
death. 0% 10% 20% 30% 40% 50% 60% 70% 80%
< 24 Hrs 24 - 48 Hrs >72 Hrs 3 Days
28wks 29% 27% 8% 12%
28-32 57% 45% 75% 69%
32-34 0% 27% 17% 12%
34-36 14% 0% 0% 6%
71
DISCUSSION
This study includes 382 very low birth neonates admitted in NICU,
Coimbatore Medical College Hospital during the period from January
2017 – December 2017.
Out of 382 VLBW neonates, 199(52%) were males & 183 (48%)
were females; 231 (60%) were Inborn & 151 (40%) were Out born.
Their mean birth weight was 1.25 Kg in males & 1.27 kg in
females. 195(51%) were born out of Normal vaginal delivery & 187
(49%) were born by caesarean section.
Out of 382 neonates, 222(58%) were SGA, 92 (24%) were AGA
and 68(18%) were IUGR. SGA babies were among VLBW neonates.
Most of VLBW neonates were in the gestational age b/w 28-32
weeks (n=224, 59%) & (32-34 weeks (n = 92, 24%).
The most common maternal risk factor associated with VLBW was
gestational hypertension is 210 (55%) followed by anemia 63(17%).
Most of the mothers belong to low socio economic status (88.6%). This
leads to inadequate intake and increased risk of infections and leading to
72
In Jaiswal et al study, Neonatal jaundice requiring phototherapy (55.1%)
followed by respiratory morbidity (10.5%) and hypoglycemic (8.8%)
were the frequent identified morbidities in late preterm infants. In our
study, sepsis (35%) followed by RDS (27%), TTN (22%), NNH (8%).
Sepsis found to be the major morbidity in our study. Multiple gestation ,
IUGR and cesarean deliveries were found to be the risk factors for
morbidity in Jaiswal et al. study. But in our study, Gestational
hypertension (n =210, 55%) followed by anemia (n= 63, 17%) were the
major risk factors. Cesarean delivery and normal vaginal delivery were
found to be equal and does not contribute to morbidity in VLBW
neonates in our study.
The most common morbidity among VLBW neonates being sepsis
(n = 133, 35%) followed by RDS (n=105, 27%), TTN (n = 85, 22%),
hypoglycemia (n=47, 12%). In schinder et al. study, IVH followed acute
respiratory illness & sepsis were the most common cause of death.
In our study the major cause of mortality being Sepsis (n=49, 52%)
followed by RDS (respiratory distress syndrome) (n=38, 40%).
Kabilan et al. study reveals that birth weight & mechanical
ventilation are the two major factors responsible for mortality in VLBW
73
(n=54, 32.4%) and Sepsis (n=46, 27.6%). Most of the death occurred due
to RDS (n=43, 25.8%). RDS occurred in 90% of VLBW infants with
incidence of 33.6% and mortality rate of 76%. In our study, Sepsis and
RDS were the major cause of morbidity and mortality in VLBW
neonates. RDS accounts for 40% of mortality which is one of the major
cause of death in VLBW infants.
In Thapar K.et al study, sepsis was the major cause of morbidity
followed by HMD and Jaundice. Majority of them were in the gestational
age 33-36 weeks (n=68, 44.2%), small for gestational age (n=89, 57.8).
Similar to this study, Sepsis and RDS were the major cause of morbidity
in VLBW neonates in our study. But most of them were in the gestational
age between 28-32 weeks (n = 224, 59%) and 32-34 weeks (n = 92,
24%).
In Ghulam nabi et al. study, Jaundice was the major morbidity. But
in our study, jaundice constitutes 31(8%) of morbidity.
In Ballot et al study, major cause of mortality was Extreme
prematurity followed by HMD and NEC. In our study, Sepsis and RDS
74
In Sangamam et al. study, the most common morbidity was was
Hyperbilirubinemia (16.77%) followed by Hypoglycemia (14.99%) and
Hyaline membrane disease (14.86 %).The most common maternal
complications associated with LBW were anemia (43.36%) and
hypertensive disorders of pregnancy (17.6%). In our study, Sepsis and
RDS were the major morbidities among VLBW neonates. Maternal
hypertension and anemia being the most common risk factors leading to
VLBW in our study. Hypoglycemia accounts for 47(12%) of morbidity in
our study. Preterm infants are at risk of developing hypoglycemia after
birth, because they have immature hepatic glycogenolysis and adipose
tissue lipolysis, hormonal dysregulation and deficient hepatic
gluconeogenesis and ketogenesis.
In Rasania et al study, 16.39% had birth asphyxia, 28.6% had
sepsis, 7.37% had RDS and 32.78% had hyperbilirubinemia. Need for
respiratory support was significantly higher in moderate preterm (47.8%).
In our study, 35% had sepsis, 27% had RDS, 22 % had TTN followed by
hypoglycemia in 12%.
In another study done in Banaras university, Perinatal asphyxia,
75
neonatal mortality. In our study, Sepsis (n= 49, 52%), RDS contribute
40%, Prematurity 1%, IVH contribute 4% of mortality.
Out of 382 VLBW neonates, 105 neonates had respiratory distress
syndrome; 43 received surfactant therapy, 38 neonates with RDS
succumb to death.
Most of the VLBW neonates were in the gestational age group of
28-32 weeks and 32-34 weeks. Out of 382 VLBW neonates, 287 (75%)
were alive and 95 (25%) were died.
VLBW neonates (n = 71, 18.5%) were mechanically ventilated.
There was no association of gender, birth, locality and sex with outcome.
Gestational age and Mechanical ventilation had positive correlation with
outcome. As the gestational age decreases, both morbidity and mortality
increases.
Since RDS and sepsis are the major cause of mortality, quality of
care in the antenatal, perinatal and postnatal periods of newborn to be
improved.
We need to strengthen the ongoing trainings of health care
personnel like NRP and to provide appropriate antenatal education and
76
LIMITATION
This study was done in very low birth weight neonates weighing
1000- 1500 g. If babies weighing < 1000 g are also included, the results
would have been better.
77
CONCLUSION
Uplifting the socioeconomic status of women, Nutritional
counselling to reduce anemia should be considered to reduce the
incidence of very low birth weight babies. Antenatal steroid therapy
needs to be more vigorously implemented.
Sepsis and Respiratory distress syndrome were the major cause of
death.
Prematurity is the primary cause behind these neonatal death. This
emphasizes the need to prevent preterm deliveries. Effective preventive
strategies to decrease the preterm birth can only be the next big step to
78
RECOMMENDATION
By proper health education and strengthening of antenatal services
along with awareness of neonatal problems in low birth weight babies,
the incidence of very low birth weight and their complications can be
reduced.
FUTURE PERSPECTIVES:
This include preventive strategies at many levels with special
emphasis on the prevention ,early detection and effective
management of Pregnancy Induced Hypertension(PIH) which is
found to be the leading cause of preterm delivery in our Centre.
Antenatal steroid therapy needs to be more rigorously
implemented.
Policies at government level to implement strict Aseptic measures
in delivery rooms, Early CPAP administration, Good neonatal
transport facilities are essential to further raise our Neonatal health
79 WHAT THIS STUDY ADDS?
Prematurity is the primary cause behind all the leading cause of
neonatal deaths.
Preventing premature births is the single most important step in
reducing our neonatal mortality rate.
Government policies aimed at implementing strict aseptic measures
in delivery rooms, Early CPAP administration, Good neonatal
transport facilities can make a great leap in raising our Neonatal
80
BIBLIOGRAPHY
1) Predictive ability of a predischarge hour-specifi c serum bilirubin
for subsequent signifi
2) cant hyperbilirubinemia in healthy term and near-term newborns.
Pediatrics 1999;103:6–14.)
3) Jaiswal A, Murki S, Gaddam P, Reddy A.
4) Early Neonatal Morbidities in Late Preterm infants, Indian
Pediatrics.2011; 48:607.11
5) Tim Schindler, Louise Koller Smith , Kei Lui, Barbare Bajuk ND
Srinivas Bolisetty , Causes of death in very preterm infants cared
for in Neonatal intensive care units : a population – based
retrospective cohort study , BMC Pediatrics,17,1,(2017)
6) Kabilan S,Kumar Ms . Morbidity and mortality pattern of very low
birth weight infants admitted in SNCU in a south Asian tertiary
care centre.
81
8) Ghulam Nabi Rather, Muzafar Jan, Wasim Rafiq,Imran
Gatoo,Sheikh Quyoom Hussain,Mohamad Latief. Morbidity and
mortality pattern in late preterm infants as a tertiary care hospital in
Jammu and Kashmir, Northern India. J Clinic Diagnos Res.2015;
9(12) : SC 01 – SC04
9) Rasania M, Muley P. Morbidity profile and immediate outcome of
late preterm neonates compared to term neonates in a rural tertiary
care hospital of Gujarat. Int J Contemp Pediatr 2017;4:1329-33.
10) Kaur A , Thapar K, Chhabra GS, Jaslean. Morbidity and Mortality
of very low birth weight babies in a Tertiary level NICU. J.Nepal
Pediatrics.Soc 2015;35(3) :257-263
11) Basu S, Rathore P, Bhatia BD . Predictors of mortality in very low
birth weight neonates in India. Singapore Med J . 2008 Jul ;
49(7):556.
12) Ballot DE, Chirwa T, Ramdin T, et al. Comparison of morbidity
and mortality of very low birth weight infants in a Central Hospital
in Johannesburg between 2006/2007 and 2013. BMC Pediatrics.
82
13) Apgar V. A proposal for a new method of evaluation of the
newborn infant. Curr Res Anesth Analg 1953;32:260-267.
14) Weiner, G.M., & Zaichkin, J. (2016). Textbook of neonatal
resuscitation. Elk Grove village IL: American Academy of
Pediatrics.
15) Silverman WC, Anderson DH. Controlled clinical trial on effects of
water mist on obstructive respiratory signs, death rate and necropsy
findings among premature in fants. Pediatrics 1956; 17: 1-4.
16) Wood DW, Downes’JJ, Locks HI. A clinical score for the
diagnosis of respiratory failure. Amer J Dis child 1972; 123: 227-9.
17) New Ballard score. (From Ballard JL, Khoury JC, Wedig K et al.
New Ballard score, expanded to include extremely premature
infants. J Pediatr 1991;119: 417-423.)
18) Predictive ability of a predischarge hour- specific serum bilirubin
for subsequent significant hyperbilirubinemia in healthy term and
near term newborns. Pediatrics 1999; 103:6-14.)
19) The International Classification of Retinopathy of prematurity
83
PROFORMA
NAME:
AGE:
RESIDENCE:
CONTACT NO:
RURAL/URBAN/SEMI-URBAN:
OCCUPATION:
SOCIO-ECONOMIC STATUS:
EDUCATED/UNEDUCATED:
ANTENATAL VISITS:
1) BOOKED - YES/ NO
2) IMMUNISED – YES/ NO
HEMOGLOBIN:
BLOOD GROUP:
WEIGHT:
CONSANGUINITY: YES / NO
GRAVIDA: PARA: LIVE:
84 LMP: EDD:
RISK FACTORS:
1. ANEMIA -
2. HYPERTENSION -
3. DIABETES MELLITUS -
4. RH NEGATIVE -
5. MULTIPLE GESTATION -
6. HIV -
7. HEPATITIS – B -
8. SYPHILIS -
9. OTHER MEDICAL PROBLEMS -
10.HYPOTHYROID -
DRUG INTAKE:
ANTENATAL STEROIDS: YES / NO
MATERNAL FEVER:
FOUL SMELLING LIQUOR:
POSTNATAL HEMORRHAGE:
85 MODE OF DELIVERY:
1. CAESEREAN
2. LABOUR NATURAL
PRESENTATION: VERTEX / BREECH:
BABY’S DETAILS:
CRIED IMMEDIATELY AFTER BIRTH: YES / NO
BIRTH WEIGHT:
RESUSCITATION REQUIRED: YES / NO
(BAG & MASK VENTILATION / TACTILE STIMULATION /
ENDOTRACHEAL INTUBATION)
TERM / PRETERM (37 WEEKS):
APGAR SCORE:
PROBLEMS :
MECHANICAL VENTILATION:
86
CONSENT FORM
I have come to know that Dr.ABINAYA. G, Postgraduate in the Department of Paediatrics is conducting a study on the topic," STUDY OF NEONATAL MORBIDITY AND MORTALITY IN VERY LOW BIRTH WEIGHT NEONATES ADMITTED IN NEONATAL INTENSIVE CARE UNIT IN A TERTIARY CARE CENTRE" I understand that my child will not have to suffer any harmful consequences as a result of the study nor will I have any financial constraints.
It is understood that blood will be collected from my child for the purpose of conducting this study.
I also understand that I can withdraw myself from this study at any point of time and by doing so it will not affect the treatment in any manner. Understanding all these, I wholeheartedly agree to take part in this study.
Signature
Name of the Guardian: Relation: