EFFECTIVENESS OF SECONDARY PREVENTION STRATEGIES
ON KNOWLEDGE, PRACTICE AND SELECTED
PHYSIOLOGICAL AND PSYCHOLOGICAL PARAMETERS
AMONG POST MYOCARDIAL INFARCTION PATIENTS
AT SELECTED HOSPITALS,
KANYAKUMARI DISTRICT,
TAMIL NADU
THESIS
Submitted to
THE TAMILNADUDR.M.G.RMEDICALUNIVERSITY, CHENNAI
for the award of the degree of
DOCTOR OF PHILOSOPHY
IN
NURSING
By
Mrs.C.R.MERLIN SUJA, M.Sc. (N)
ON KNOWLEDGE, PRACTICE AND SELECTED
PHYSIOLOGICAL AND PSYCHOLOGICAL PARAMETERS
AMONG POST MYOCARDIAL INFARCTION PATIENTS
AT SELECTED HOSPITALS,
KANYAKUMARI DISTRICT,
TAMIL NADU
THESIS
Submitted to
THE TAMILNADUDR.M.G.RMEDICALUNIVERSITY, CHENNAI
for the award of the degree of
DOCTOR OF PHILOSOPHY IN
NURSING
By
Mrs.C.R.MERLIN SUJA, M.Sc. (N)
Under the Guidance of
Dr.C.SUSILA M Sc N., PhD,
PRINCIPAL
BILLROTHCOLLEGE OF NURSING CHENNAI
ON KNOWLEDGE, PRACTICE AND SELECTED
PHYSIOLOGICAL AND PSYCHOLOGICAL PARAMETERS
AMONG POST MYOCARDIAL INFARCTION PATIENTS
AT SELECTED HOSPITALS,
KANYAKUMARI DISTRICT,
TAMIL NADU
THESIS
Submitted to
THE TAMILNADUDR.M.G.RMEDICALUNIVERSITY, CHENNAI
for the award of the degree of
DOCTOR OF PHILOSOPHY
IN
NURSING
By
Mrs.C.R. MERLIN SUJA
Guided By
Dr.C.SUSILA, M.SC N., PhD, Ph.D RESEARCH GUIDE
PRINCIPAL
BILLROTH COLLEGE OF NURSING CHENNAI
CERTIFICATE
This is to certify that the thesis entitled “ASSESS THE LIVED IN EXPERIENCE AND EVALUATE THE EFFECTIVENESS OF SECONDARY PREVENTION STRATEGIES ON KNOWLEDGE, PRACTICE AND SELECTED PHYSIOLOGICAL AND PSYCHOLOGICAL PARAMETERS AMONG POST MYOCARDIAL INFARCTION PATIENTS AT SELECTED HOSPITALS, KANYAKUMARI DISTRICT, TAMIL NADU” submitted by
Mrs.C.R.MERLIN SUJA for the award of the degree of Doctor of Philosophy in Nursing, is a bonafide record of research done by her during the period of study, under my supervision and guidance and that it has not formed the basis for the award of any other Degree, Diploma, Associateship, Fellowship or other similar title. I also certify that this thesis is her original independent work. I recommend that this thesis should be placed before the examiners for their consideration for the award of Ph.D. Degree in Nursing.
Research Guide
Dr.C.SUSILA, M.SC N., PhD,
Ph.D Guide,
Billroth College of Nursing,
Chennai.
CERTIFICATE
This is to certify that the thesis entitled “ASSESS THE LIVED IN EXPERIENCE AND EVALUATE THE EFFECTIVENESS OF SECONDARY PREVENTION STRATEGIES ON KNOWLEDGE, PRACTICE AND SELECTED PHYSIOLOGICAL AND PSYCHOLOGICAL PARAMETERS AMONG
POST MYOCARDIAL INFARCTION PATIENTS AT SELECTED
HOSPITALS, KANYAKUMARI DISTRICT, TAMIL NADU” submitted by Mrs.C.R.MERLIN SUJA for the award of the degree of Doctor of Philosophy in Nursing, is a bonafide record of research done by her during the period of study under my supervision and co-guidance and that it has not formed the basis for the award of any Degree, Diploma, Associateship, Fellowship or other similar title. I also certify that this thesis is her original independent work. I recommend that this thesis should be placed before the examiners for their consideration for the award of Ph.D. Degree in Nursing
Research Co - Guide
Dr.CIBY JOSE, M.Sc (N)., PhD,
PRINCIPAL,
Venkateswara College of Nursing,
Chennai
DECLARATION
I hereby declare that this thesis entitled “ASSESS THE LIVED IN EXPERIENCE AND EVALUATE THE EFFECTIVENESS OF SECONDARY PREVENTION STRATEGIES ON KNOWLEDGE, PRACTICE AND SELECTED PHYSIOLOGICAL AND PSYCHOLOGICAL PARAMETERS AMONG POST MYOCARDIAL INFARCTION PATIENTS AT SELECTED HOSPITALS, KANYAKUMARI DISTRICT, TAMIL NADU” is my own work carried out under the guideship of Dr.C.SUSILA, M.Sc N., PhD, Research Guide, Billroth College of Nursing which is approved by the Research Committee, The Tamil Nadu Dr.M.G.R.Medical University, Guindy, Chennai.
I further declare that to the best of my knowledge the thesis does not contain any part of any work which has been submitted for the award of any degree either in this University or in any other University / DeemedUniversity without proper citation.
Mrs.C.R. Merlin suja Research Scholar
Place :
Praise is to god for bestowing on me the ability, poise, and strength to walk successfully through the laborious path of completing this project. First of all, I praise and thank Almighty God for his abundant grace, blessings and unconditional love showered on me throughout the study.
I owe my profound gratitude to Vice Chancellor and Research Department of the Tamil Nadu Dr.M.G.R Medical University, Guindy, Chennai, for giving me an opportunity to undertake my Ph.D at this esteemed University.
It’s my honour and privilege to offer my heartfelt gratitude to Mrs. Valli Alagappan, Managing Trustee and Chairperson of the Governing
Council, Mr. A.R. Kasiviswanathan, Trustee and Mrs. Seetha Subbiah, Member Trustee, Omayal Achi College of Nursing, for offering me an opportunity to pursue the Ph D. (N) programme in this renowned institution.
Help is an essential factor to reach the summit; these words are true of my Guide and Mentor Dr. C. Susila M.Sc(N), Ph.D(N), Principal, Billroth college of Nursing. Her constant encouragment guidance and valuable suggestions helped in the fruitful outcome of this study.
My special heartfelt gratitude and sincere thanks to Dr. A.Judie, M.Sc(N), Ph.D former guide for her efficient guidance valuable suggestions which helped me to lay a strong foundation for this study.
My sincere thanks and appreciation to the co-guide Dr. Ciby Jose, M.Sc(N), Ph.D, Principal, Venkateswara College of Nursing for her guidance and help to complete my study on time.
spared their valuable time for the ethical clearance in intervention tool.
I would like to extend my sincere thanks to the Advisory committee members Dr. Hemalatha. J, M.Sc(N) Ph.D, HOD, Medical Surgical Nursing, Dr. Shankar Shanmugam, M.Sc(N), Ph.D, for there enthusiastic help and critical comment and guidance throughout the study.
My deepest gratitude to Dr.Jayanthi MSc.(N), Ph.D, Research Coordinator for her helping hand in successful completion of the study.
I am indebted to the experts who contributed their valuable time and for their constructive judgments while validating the tool.
I owe my thanks to Dr. Arumugam Msc, Ph.D, Bio-Statistician, for his support, guidance valuable suggestions in analysis of data.
I acknowledge the positive response of my participants during their break hours is the great patience to complete my entire project without who this project would be next to nothing.
I extend my sincere thanks to the Asaripallam, Govt. Medical College and Hospital for permitting me to conduct the research work.
I express my sincere gratitude to librarian, Asst. librarian, Office Staff for their support and encouragement which helped me to complete this task.
Mr.Fredrick and Aunt Mrs. Doreen who was the corner stone to do this programme and lay a lending hand in all aspects of the study. I owe a great to deal to my uncle Y.Christudhas, my uncle Mr.Thiyagarajan, Mrs. Premavathy Aunt, Grandmother Mrs.Padma for their relentless support and concern to this endeavor.
Words fail to acknowledge the love and understanding of my lovable husband Mr. T. Samuel Trivalaine who gave me confidence and motivation to achieve the goal. His dedication, persistent confidence in me has taken the load off my shoulder; I owe him my heart full thanks.
I have no words to pen the love and sacrifice of my beloved children master S.M.Jemerson Nyhan, S.M. Linson Abarron Nyhan, who led me to this run on the ladder of my scholastic career and I am ever grateful to them for the smooth sail in my Endeavour.
I express my sincere thanks to the editors of Tamil and English for their timely help in editors the manuscripts.
I would like to thank Mr.G.K.Venkatraman, Elite Computers, and Ms.Manjusha Nyhan Travels for their enthusiastic help and sincere efforts in typing the manuscripts meticulously with much valued computer skills.
I thank my colleagues Mrs. Angelin, Mrs.Starmine, Research scholars, and friends in C.S.I college of Nursing, Marthandam who have helped me in making this work possible.
AMI - Acute Myocardial Infarction AHA - American Heart Association ACS - Acute coronary syndrome ANCOVA - Analysis of CoVariance test BGL - Blood Glucose Level
BP - Blood Pressure
BB - Beta Blockers
BMI - Body Mass Index CAD - Coronary Artery Disease CME - Continuing Medical Education CR - Cardiac Rehabilitation
CVD - Cardio Vascular Diseases CPK-MB - Creatinine Phospokinase(MB) CPX - Cardio pulmonary Exercise Testing CHD - Coronary Heart Disease
DALYS - Disability Adjusted Life Years DBP - Diastolic Blood Pressure DNA - Deoxyribo Nucleic Acid
EB - Evidence Based
ESC - European Society of Cardiology FG - Fasting Glucose
IEC - Information Education Communication IHD - Ischemic Heart Disease
K-DPP - Kerala-Diabetes Prevention Programme LDL - Low Density Lipoprotein
MI - Myocardial Infarction
MINAP - Myocardial ischemia national audit project NCEP - National Cholestrol Education Programme NICE - National Institute of clinical excellence NP - Nurse Practitioner
NS - Non significant
NV - Non Vegetarian
NSTEMI - Non ST elevation Myocardial Infarction PTSD - Post traumatic stress disorder
Po Gr - Post Graduate
STEMI - ST elevation Myocardial Infarction SES - Socio Economic Status
Semi Prof - Semi Professional SBP - Systolic Blood Pressure SD - Standard Deviation
CHAPTER NO.
TITLE PAGE
NO.
1 INTRODUCTION 1
1.1 Background of the study 2
1.2 Significance and Need for the study 20
1.3 Conceptual framework 31
2 AIMS AND OBJECTIVES 39
2.1 Title 39
2.2 Statement of the problem 39
2.3 Objectives 39
2.4 Operational definitions 40
2.5 Null hypotheses 41
2.6 Assumptions 42
2.7 Delimitations 42
3 REVIEW OF LITERATURE 43
3.1 General concepts of myocardial infarction 43 3.2 Research studies related to
3.2.1 Prevalence of myocardial infarction 48 3.2.1 Knowledge on myocardial infarction 51
3.2.3 Diet & Co-morbidities 52
3.2.4 Education on myocardial infarction 58 3.2.5 Exercise & weight management 58
3.2.6 Medication 59
3.2.7 Stress reduction 60
3.2.8 Habits 61
3.2.9 Cardiac rehabilitation 62
3.2.10 Secondary prevention 63
4 MATERIALS AND METHODS 68
CHAPTER NO.
TITLE
NO.
4.2 Research design 68
4.3 Variables 70
4.4 Research setting 70
4.5 Population 70
4.6 Sample & sample size 71
4.7 Criteria for selection of samples 71
4.8 Sampling technique 72
4.9 Development of the tool 72
4.10 Content validity 77
4.11 Reliability 77
4.12 Ethical considerations 77
4.13 Pilot study 79
4.14 Modifications after pilot study 79
4.15 Data analysis procedure 79
5 RESULTS AND ANALYSIS 81
5.1 Qualitative study 81
5.2 Description of the demographic variables of the samples. 91 5.3 Assessment of pre test, post test knowledge, practice,
physiological and psychological parameters in study and control group
93
5.4 Effectiveness of secondary prevention strategies on knowledge, practice, physiological and psychological parameters among post myocardial infarction patients
97
5.5 Comparison of pre test, post test knowledge, practice, physiological and psychological parameters between study and control group
110
5.6 Correlation among knowledge, practice, physiological and psychological Parameters in study and control group
CHAPTER NO.
TITLE
NO. 5.7 Association between knowledge, practice, physiological and
psychological parameters with demographic variables in study and control group.
116
6 DISCUSSION 125
7 SUMMARY, CONCLUSION, IMPLICATIONS,
RECOMMENDATIONS AND LIMITATIONS
133
8 REFERENCES 139
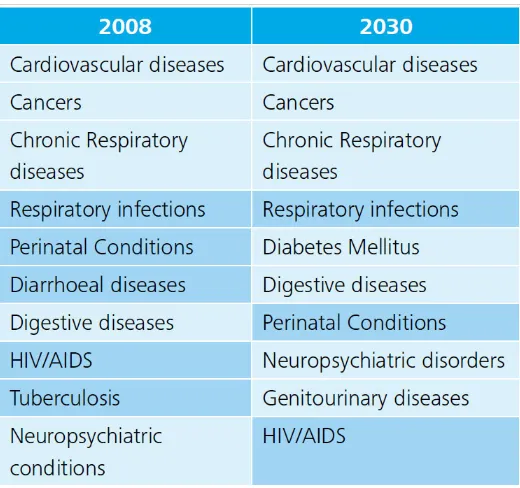
Table No. Title Page No. 1.1.1 Top 10 causes of mortality (Non-communicable diseases) 4 5.2.1 Frequency distribution of study and control groups in respect
of their demographic profiles
91
5.3.1 Frequency and percentage distribution of pre and post test level of knowledge in study and control group
93
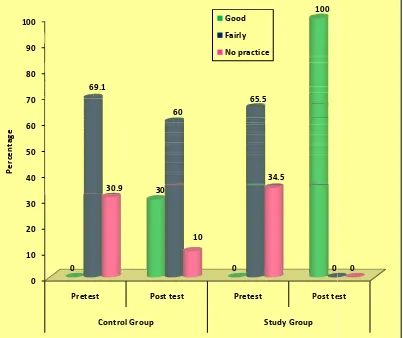
5.3.2 Frequency and percentage distribution of practice in pre and post test of study and control group.
94
5.3.3 Mean standard deviation of pre test physiological variables in study and control group.
95
5.3.4 Frequency distribution of psychological parameter (stress) among study and control group in pre and Post tests.
96
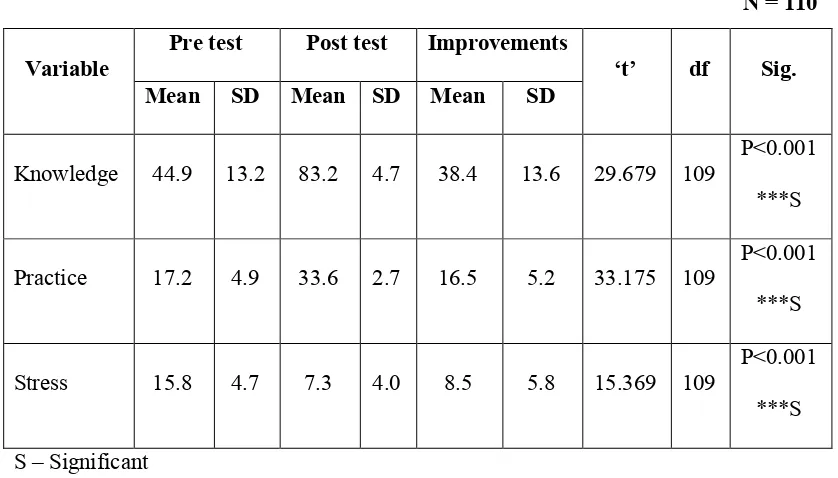
5.4.1 Comparison of mean and standard deviation of knowledge, practice and psychological parameter (Stress) within control group.
97
5.4.2 Comparison of mean and standard deviation of knowledge, practice and psychological parameter (stress) within study group.
98
5.4.3 Comparison of mean, standard deviation of Physiological variables within control group.
99
5.4.4 Comparison of mean, standard deviation of physiological variables within study group.
100
5.4/5 Systolic BP –comparison of mean, standard deviation of 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA.
101
5.4.6 Diastolic BP- Improvements at different levels- 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA .
102
5.4.7 BGL- Improvements at different levels- 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA.
5.4.8 Cholesterol- Improvements at different levels- 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA.
104
5.4.9 Triglycerides- Improvements at different levels- 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA.
105
5.4.10 HDL-Improvements at different levels- 5th day 1 month and 6 months within study and control group. using repeated measures of ANOVA
106
5.4.11 LDL- Improvements at different levels- 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA.
107
5.4.12 VLDL- Improvements at different levels- 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA.
108
5.4.13 CpKMB- Improvements at different levels- 5th day 1 month and 6 months within study and control group using repeated measures of ANOVA.
109
5.5.1 Comparison of knowledge, practice and psychological parameter between study and control group.
110
5.5.2 Comparison of waist hip ratio improvements between study and control group.
111
5.5.3 Comparison of physiological variables between study and control group.
112
5.6.1 Correlation of knowledge and practice with Psychological Variable (stress) and BMI with waist hip Ratio.
113
5.6.2 Comparison of correlated variables between study and control group.
114
5.7.1 Association between demographic variables with knowledge of Study and control group.
116
5.7.2 Association between demographic variables with pre test Practice of both groups.
5.7.3 Association between demographic variables with pre test psychological parameter (Stress) of both groups.
119
5.7.4 Association between demographic variables with systolic BP of both groups.
120
5.7.5 Association between demographic variables with diastolic BP of both groups.
121
5.7.6 Association between demographic variables with cholesterol of both groups.
122
5.7.7 Association between demographic variables with Blood Glucose Level of both groups.
123
5.7.8 Association between demographic variables with Cpk MB of both groups.
FIGURE NO. TITLE 1.1.1 Deaths worldwide stem from NCDs
1.1.2 Mortality from major communicable and non-communicable diseases, 2030
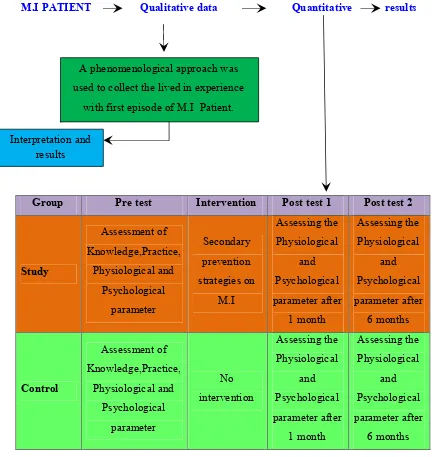
1.1.3 Shifting disease burden – from communicable diseases to NCDs 1.2.1 Disease Burden Estimates – 1990, Disease Burden Estimates – 2020 1.3.2 Conceptual framework based on Betty Newman’s System Model 4.2.1 Monograph of the study design
4.9.2 Schematic representation of Research Design
5.3.2 Frequency and percentage distribution of practice in pre and post test of control and study group
5.3.4 Frequency distribution of psychological parameter (stress) among study and control groups in pre and Post tests.
5.4.5 Comparison of Systolic BP trends between two groups at 5th day, 1 month and 6 months (Systolic Blood pressure)
5.4.6 Comparison of Diastolic BP trends between two groups at 5th day, 1 month and 6 months.
5.4.7 Comparison of BGL trends between two groups at 5th day, 1 month and 6 months
5.4.8 Comparison of Cholesterol trends between two groups at 5th day, 1 month and 6 months
5.4.9 Comparison of Triglycerides trends between two groups at 5th day, 1 month and 6 months.
5.4.10 Comparison of HDL trends between two groups at 5th day, 1 month and 6 months
5.4.12 Comparison of VLDL trends between two groups at 5th day, 1 month and 6 months
S. No. Title
A Provisional Registration for Full Time Ph.D Degree B Full Time Ph.D Research Programme Proforma C Advisory Committee Certificate
D Ph D Execution Plan – Gantt Chart E Ethical Clearance Certificate F IEC Approval Certificate
G Permission for conducting the study in the Data Collection Setting H Plagiarism Certificate
I Certificates
J Related Research Work Executed K Content validity experts
L Content validity certificates
M English and Tamil Editing Certificates N Tool in English and Tamil
O Intervention Tool – English & Tamil
A study to assess the lived in experience and evaluate the effectiveness of secondary prevention strategies on knowledge, practice, selected physiological and psychological parameters among post myocardial infarction patients at selected hospitalS, Kanyakumari District, Tamil Nadu.
Cardiovascular disease (CVD) is a major global health problem reaching epidemic proportions in the Indian subcontinent and developing countries, it is accounting for 78% of all deaths1. High risk of CVD has been reported among South Asians, regardless of whether they live overseas or in their native lands.2Presence of conventional risk factors such as smoking, diabetes mellitus, hypertension and dyslipidemia are clearly associated with coronary artery disease (CAD) among them. Upto 45% of deaths following myocardial infarction could be prevented with the appropriate secondary prevention strategy3.
Acute myocardial infarction (AMI) is frequent and the associated mortality is high in this group. One person dies every 33 seconds owing to a heart attack in India, India is currently witnessing nearly two million heart attacks per year and majority of the victims are youngsters. In developing countries such as India, cardiovascular disease is a major cause of mortality, Mehta 4.
stress, and a lack of consumption of fruit and vegetables lead to more than 90% of acute myocardial infarctions events among South Asians. Reducing morbidity and mortality in post myocardial infarction patients needs implementation of effective secondary measures. Thus the investigator interested to do this study.
The objectives of the study were
1. To assess the lived in experience of first episode of Myocardial Infarction among post myocardial infarction patients in study group.
2. To assess the pre test, post test knowledge, practice, physiological and psychological parameters in study and control group.
3. To compare the knowledge, practice, physiological and psychological parameters between pre and post test in study and control group.
4. To evaluate the effectiveness of secondary prevention strategies on knowledge, practice, physiological and psychological parameters among post myocardial infarction patients.
5 To correlate the relationship among knowledge, practice, physiological and psychological parameters in study and control group
6 To find out the association between knowledge, practice, physiological and psychological parameters with demographic variables in study and control group.
The Null hypotheses formulated for the study were:
physiological and psychological parameters between study and control group among post MI patients.
NH3- There is no significant correlation among knowledge, practice, physiological, psychological parameters in study and control group
The research process for this study was guided by the conceptual framework based on Betty Newman’s System model
A Mixed method research approach was adopted for the study.In qualitative research design the phenomenological approach, was taken in which sequential exploratory design was used for this study.In quantitative research approach true experimental design was used.The study was conducted in ICU’at Government Medical College and Hospital, Asaripallam. The population includes persons who got admitted with first episode of myocardial Infarction in tertiary care hospitals and follow up were done in their residents of selected villages.
The Sample size consists of 220 patients with first episode of myocardial infarction with 110 patients for study group and110 patient for control group by Block Randomization as a method of sampling technique. For qualitative research design 5 patients were selected conveniently to assess their lived in experience.
glucose level, Lipid profile and Creatinine Phospo Kinase (MB) through lab report, Body mass index and waist hip ratio through calibrated height weight machines. Psychological parameter was level of stress and it was assessed through modified perceived stress scale.
The Study findings were as follows:
In Qualitative study 5 patients were selected and asked to verbalize their feelings and it is autotaped and verbatim was formed. The content was analyzed and themes were formulated based on the following, pain experience, loss of control, Fear of future, mutual communication ,fear of death, fear of environment, Isolation, anxious about the disease, social stigma, dependency, loss of acceptance.Hopelessness, fear of another episode of M.I, Deficient knowledge, curiosity about secondary prevention strategies. The study shows that M.I is a condition that creates fearfulness about the disease, prognosis and future.It also showed that patient were curious in preventing another episode of M.I.
between the two group was statistically very highly significant (P<0.001).
The psychological parameter (stress) in both groups were moderate in pre test and improved as mild in posttest in study group and no improvement in control group. In pretest they were not practicing secondary measures in both groups but during post test in study group it was improved to fair and in control group still they were not practicing.
The effectiveness of secondary prevention strategies within control and study group in respect of physiological variables showed that, the mean BMI and Waist hip ratio of study group in pre and post test difference was highly significant where as in control group BMI mean difference was not significant but waist hip ratio mean difference was statistically significant.The cholesterol level LDL,VLDL,systolic and diastolic bloodpressure, bloodglucose in study group was differed from 5th day to 6 th month.But it was fluctuating in control group. The triglycerides, HDL trends were equal in all levels in control group whereas in study group it was statistically differed from 5th day to 6 months.
group was associated with age, educational status, occupation and religion (p<0.01).Also in practice the age was strongly associated likewise education and occupation. But the study group did not associate with this.In the association between the age of the subjects with stress of both groups were strongly associated (p<0.05).In study group the occupation had statistically significant association with stress.
The association between demographic variables with systolic BP of control group was associated with education, type of family, diet habit, sources of information, and family history and diastolic B.P of control group was associated with Age, gender, education, occupation, family type, religion and sources of information. The association between demographic variables with blood glucose levels of control group was associated with Age, occupation, family type, religion, diet habit, sources of information, family history. The association between demographic variables with cholesterol in study group was associated with residence.
CHAPTER – 1
INTRODUCTION
Cardiovascular disease (CVD) is a major global health problem reaching epidemic proportions in the Indian subcontinent and developing countries, it is accounting for 78% of all deaths. High risk of CVD has been reported among South Asians, regardless of whether they live in overseas or in their native lands.Presence of conventional risk factors such as smoking, diabetes mellitus, hypertension and dyslipidemia are clearly associated with coronary artery disease (CAD) among them.
According to a recent estimate by WHO1, 30% of deaths in India is due to Heart Diseases. Coronary causes may increase from about 2.9 crore in 2000 to 6.4 crore in 2015. 1 in 5 deaths is due to Heart diseases in the U.S. It is more common in developing countries, such as 32% in India. It is expected to raise from 1.59 million in 2000 to 2.03 million in 2010. The mortality rates in various states are 10% in Meghalaya, 49% in Punjab, 42% in Goa, 36% in Tamilnadu and 31% in Andhra Pradesh. The differences are found to be the prevailing dietary risk factors in the states.
The mortality of IHD related death in Tamil Nadu is 36%. It is associated with few modifiable and several modifiable risk factors. The drastic rise in the stress due to the sedentary lifestyle, food intake (food rich in carbohydrates, fat etc.), smoking and lack of physical activities which leads to obesity and tend to cause a sharp increase in the risk even in the developing countries.
myocardial infarction are susceptible to heart failure, re-infarction, arrythmias and sudden cardiac death. Most deaths occur in the first six months after infarction.
Reducing morbidity and mortality among post-myocardial infarction (MI) patients requires the implementation of effective secondary measures. A survey examined current practice by assessing the adherence to National Institute for Health and Clinical Excellence (NICE) guidance on MI secondary prevention in a sample of general practitioners and cardiologists. Although drug treatment for post-MI generally compiled with NICE recommendations, diet and lifestyle aspects were not implemented fully. There appeared to be sub-optimal integration between primary and secondary healthcare providers.
Most cardiovascular diseases can be prevented by curtailing the behavioral risk factors such as unhealthy diet, physical inactivity and obesity and use of alcohol. People with cardiovascular disease need early detection and medicine management with counseling.
1.1 BACKGROUND OF THE STUDY
to occur. Muscle continues to die for six to eight hours at the time of heart attack usually completes, Wikepedia2.
According to Global Burden of Diseases3 the deaths from Non Communicable Disease rises expected from 28.1 million in a year in 1990 to 49.7 million by 2020.By the year 2020, non communicable diseases are expected to account for seven out of every ten deaths in the developing regions, compared with less than half today.
[image:30.612.137.414.389.665.2]Non-communicable diseases4 (NCDs) impose a large burden on human health worldwide. Currently, more than 60% of all deaths worldwide stem from NCDs (Figure 1.1.1)
The Fig 1.1.1 depicts that majority of 30% deaths were due to cardiovascular diseases when compared to other conditions.
The Global status on Non-Communicable diseases Report5 has reported that there were more than 2.5 million deaths from CVD in India in 2008, two-thirds due to CHD and one third to stroke. These estimates show a rapid increase in the mortality rates of India.
[image:31.612.186.446.403.647.2]A report by the World Economic Forum and the Harvard School of Public Health September 20114, the Global Burden of Disease reported that, Non-communicable diseases (NCDs) impose a large burden on human health worldwide. Currently, more than 60% of all deaths worldwide stem from NCDs. In 2008, roughly four out of five NCD deaths occurred in low- and middle-income countries (WHO, 2011a)6.
The above table 1.1.1 shows that cardiovascular diseases are the top most causes of Mortality.
IHD was the leading cause of deaths and life-years lost from any cause worldwide in 2010, and IHD was the leading cause of death and disability among the major cardiovascular diseases. IHD is not only a disease of the elderly in wealthy countries, but past analyses by the GBD7,3 (Global Burden of Diseases, Injuries, and Risk Factors) study and other studies indicate that IHD has a major global impact on working-age adults and is a growing problem in low- and middle-income countries.IHD is among the major diseases globally, but regional importance varies due to differences in IHD incidence, prevalence, and mortality, as well as the impact of competing diseases.
MI is a symptom of advanced or severe heart disease, and the major modifiable risk factors for MI includes high blood pressure, high blood cholesterol, diabetes (mellitus), smoking/tobacco use, obesity and being overweight, poor nutrition diet, physical inactivity and (no or excessive) alcohol use. Stress has also been shown to be an important (modifiable) risk factor for MI. The major non-modifiable risk factors for MI includes sex, age, family history and race, but not all individuals with these risk factors experience a MI8.
cholesterol, diabetes, stroke, high blood pressure and family history) and women (diabetes, high cholesterol, being unmarried, dissatisfaction with financial situation, physical inactivity and high blood pressure). The interactions among MI-associated factors have a large influence on MI, factors associated with MI change and associations weaken after 65 years of age in both sexes and the interaction of factors can be associated with large reductions in MI prevalence, to near zero, even in the presence of one or more of the 4 key risk factors for MI and also study found one unidentified factor associated with MI (exposure to dangerous conditions at work) among the participants, which may represent a ‘new’ risk factor for MI.9
Fig.1.1.2: Mortality from major communicable and non-communicable diseases, 2030
Source: Global Burden of Diseases 2004. Projected Deaths 2030, Baseline Scenario.World Health Organization, 2008. Number of deaths in '000s
The above figure 1.1.2 shows that cardiovascular diseases shows the highest mortality rate.
countries. WHO projects that diabetes will be the seventh leading cause of death in 2030 (WHO fact sheet) 10
Recent studies have shown that an elevated admission or fasting glucose (FG) level is common in patients with acute myocardial infarction (AMI) and is associated with an increased short-term mortality. Study demonstrated that FG level was also a long term independent predictor of outcomes in patients with AMI and diabetes11.
[image:34.612.148.480.406.617.2]Most cardiovascular diseases can be prevented by curtailing the behavioral risk factors such as unhealthy diet, physical inactivity and obesity and use of alcohol. People with cardiovascular disease need early detection and medicine management with counseling. It is also needed to have a plan for 25% reduction in the prevalence of blood pressure defined as systolic and/or diastolic pressure≥140/90 mmHg, as it is one of the leading risk factors of cardiovascular disease in adults aged 18 years in 2014 12.
Fig.1.1.3: Shifting disease burden – from communicable diseases to NCDs Source: 1. Global Burden of Diseases 2004. Projected Deaths 2030, Baseline Scenario.World Health Organization, 2008.
Fig 1.1.3 shows that, In 2008 63% ofpeople were suffered with NCDs raises to 73% by 2020.
Fig.1.1.4: Disease Burden Estimates – 1990, Disease Burden Estimates - 2020
Fig.1.1.4 Source: Nutrition Transition in India, 1947-2007. Ministry of Women and Child Welfare.
This figure shows that, in 1990 29% of NCDs rises to 57% during 2020.
The WHO criteria were used to classify hypertension people a Type I, Type II, Type III. About 71% of people had 140 above systolic and above 90 mm Hg considered to be the Type I .20.3 % people with the systolic BP of 160 – 179 mm Hg and diastolic BP of 150-109 mm Hg.In Body Mass Index more than 23 were found to be positively related to hypertension.Tamil Nadu Health System project13 (TNHSP) has started to do study in 13 districts. This programme provides treatment to people to those who suffer from hypertension.
total-risk approach needs to be adopted for early detection and cost-effective management of hypertension in order to prevent myocardial infarctions and other complications.
Salt is the major factor that increases blood pressure and is responsible for myocardial infarction .In meta-analysis, it was estimated that a reduction of 6 g of salt per day would reduce coronary heart disease by 18%. This would prevent approximately 35,000 of CHD deaths a year in the UK and approximately 2.5 million deaths worldwide. Two large randomized trials (Trials of Hypertension Prevention (TOHP) I and II) looked at the long-term effects of salt reduction on CVD in more than 3000 participants over an 18 months (TOHP I) or 36-48months (TOHP II) period. A fall in BP of 1.7/0.9 mm Hg and a fall of 1.2/0.7 mm Hg were found in TOHP I and TOHP II respectively. The follow-up study taken after 10 – 15 years later showed a reduction of 25% in the incidents of cardiovascular events. The National Institute of Health and Clinical Excellence (NICE) 14,53,suggest a salt intake of 6g by 2015 and 3g by 2025 to prevent cardiovascular diseases. .
Tobacco production and consumption has increased significantly. Smoking is increasing among young subjects (20-35 years), according to second and third National Family Health Surveys 16(NFHS). In urban populations, smoking is increasing among the low educational status subjects. The prevalence of hypertension has increased in both urban and rural subjects and presently in 25%-40% of urban adults and 10%-15% of rural adults.
Lipids levels are increasing and serial studies from a north Indian city reported that increasing mean levels of total, low density lipoprotein and non-high density lipoprotein (HDL) cholesterol and triglycerides, and decreasing HDL cholesterol.
Although there are large regional variations in the prevalence of diabetes it has quadrupled in the last 20 years from < 1%-3% to 10%-15% in urban areas and 3%-5% in rural areas.
Studies have reported that, increasing obesity as well as truncal obesity due to sedentary lifestyles, and psychosocial stress in the country.
Atherogenesis and thrombogenesis is also believed to be lower in vegetarians as their platelet phospholipid linoleate and antioxidant concentrations are higher, which is likely to lead to reduced oxidation of LDL. From the study, it can be considered that following a nonvegetarian diet may lead to an increased risk of IHD and hence encouraging a vegetarian diet among Indians may help bring about a lower incidence of AMI.
Cardiovascular disease (CVD) is the leading cause of death globally: the majority dying from ischemic heart disease. Overweight and obesity, most commonly defined according to body mass index (BMI), has been characterized as a major modifiable risk factor for cardiovascular (CV) morbidity and mortality by the American Heart Association and the American College of Cardiology18.In the study the association between BMI and risk of incident acute myocardial infarction (AMI), CV death and all-causes of mortality in a large population of men and women with suspected CAD was assessed.BMI and risk of AMI, CV death and all causes of mortality in men and women shows strong associations between overweight/obesity and risk of CVD and death .
IHD is becoming a more common cause of death in the developing world. In India IHD had become the leading cause of death by 2004, accounting for 1.46 million deaths (14% of total deaths) and deaths due to IHD were expected to double during 1985–2015 Globally, disability adjusted life years20 (DALYs) lost to ischemic heart disease are predicted to account for 5.5% of total DALYs in 2030, making it to the second-most-important cause of disability as well as the leading cause of death by this date.
Many risk factors for myocardial infarction are potentially modifiable, with the most important being tobacco smoking (including secondhand smoke). Smoking appears to be the cause of about 36% and obesity the cause of 20% of coronary artery disease.21Lack of physical activity has been linked to 7–12% of cases. Less common causes include stress-related causes such as job stress, which accounts for about 3% of cases, and chronic high stress levels.At any age, men are more at risk than women, particularly before menopause22.High levels of blood cholesterol, particularly high (increased levels of) low-density lipoprotein, low (reduced levels of) high-density lipoprotein, high (increased levels of) triglycerides.Transfats do appear to increase risk.
Type 2 Diabetes Mellitus has become a major public health challenge in India. Factors relevant to the development and implementation of diabetes prevention programmes in resource-constrained countries, such as India, have been under-studied. The purpose of this study is to describe the findings from research aimed at informing the development and evaluation of a Diabetes Prevention Programme in Kerala26, India (K-DPP).Prevalence of risk factors for diabetes is very high and increasing in Kerala. This situation is largely attributable to rapid changes in the lifestyle of people living in this state of India. India’s National Programme for the prevention and control of major non-communicable diseases (NCD) also provide a supportive environment for further community-based efforts to prevent diabetes.
Psychological factors are strong risk factors for CHD and adversely affect recovery after major CHD events. Although most of the attention has been directed at depression, other adverse psychological characteristics, including anxiety and hostility, may also be significant CHD risk factors. Studies have demonstrated that 40% to 70% of prevalence of depression, anxiety, and hostility even after cardiac rehabilitation .Studies have also shown that depressed patients with CHD who attended a formal cardiac rehabilitation program, had nearly a 70% reduction in mortality risk. It has been found that only small improvements in exercise capacity may produce improvements in depression and depression-related mortality27,72.
CAD patients is 30 to 60 minutes of moderate intensity aerobic PA at least 5 days of the week, to elicit a heart rate of 60–85% of maximum. The duration, frequency, and intensity of aerobic Exercise Training are the key variables in the “dose” of exercise training that is optimally therapeutic. Highly controlled modes of Physical Activity include brisk walking, running, cycling, or swimming that involves large muscle groups which can increase peak aerobic capacity and are inversely related to all causes of mortality in patients with CAD28.Exercise-based CR programs have a 27% reduction in total mortality than patients receiving usual care.
A healthy diet and aerobic exercise are regarded as mainstays in prevention of CVD, with accumulating evidence on the impact of the Mediterranean diet on cardiovascular risk. Yoga, a form of physical activity that involves physical postures, breath work, and meditation or relaxation, is becoming more prevalent in the United States; In 2012 National Center for Health Statistics survey29 showing that 9.5% of adults (21 million) used yoga in the previous 12 months. Three recent systematic reviews and meta‐analyses suggested that meditation may significantly reduce the risk factors for CVD such as body weight, lipid profile, and BP30.
breathlessness. Patients who are not achieving this should be advised to increase their activity in a gradual, step-by-step way, aiming to increase their exercise capacity53.
Cardiovascular Disease (CVD) is a major cause of mortality worldwide32. Studies have proven that control and reduction of cardiovascular risk factors such as elevated blood pressure, high cholesterol levels, excess of body weight, smoking and lack of exercise can contribute to a reduction of CVD mortality of around 40-60% .The European Society of Cardiology and American Heart Association, National High Blood Pressure Education Program committee (JNC 7) and National Cholesterol Education Panel (ATP III) are some of them33.
Cardiac rehabilitation should be equally accessible and relevant to all patients after an MI, particularly people from groups that are less likely to access this service. These include people from black and ethnic minority groups, older people, people from lower socio-economic groups, women, people from rural communities and people with mental and/or physical co- morbidities.
breathlessness for 20–30 minutes every day, stop smoking, and trying to achieve a healthy weight 35. Exercise is both safe and effective even if people have had stents or heart failure.
A Mediterranean dietary pattern has been associated with reduced cardiovascular (CV) and total mortality in large epidemiological studies, and in two prevention trials, CV events were lower in subjects randomized to a Mediterranean dietary intervention compared with control subjects following a low-fat diet. The traditional Mediterranean diet is characterized by a high proportion of healthy foods, including fruit, vegetables, legumes, whole grains, fish, moderate alcohol, and little meat. Clinical practice guidelines from the European Society of Cardiology36 and the American Heart Association recommend frequent consumption of fruit, vegetables, fish, and other whole foods. In addition to encouraging healthy foods, these guidelines recommend restricting sodium, sugar, saturated fats, and refined carbohydrates, which are often included in processed foods, and are more typical of a Western dietary pattern.
vocational state of the patient. Cardiac rehabilitation is assuming an increasingly important role in secondary prevention.
In essence, cardiac rehabilitation services are comprehensive programs involving education, exercise, risk factor modification and counseling, designed to limit the physiological and psychological effects of heart disease, reduce the risk of death or recurrence of the cardiac event, and enhance the psychosocial and vocational state of patients.The goals of inpatient Rehabilitation are to assist the patient in becoming ambulatory; to prepare the patient and family to cope with the psychological and emotional stress that accompanies a coronary event; and to educate the patient about coronary risk factor modification.37
Cardiac rehabilitation programs were first developed in the 1960s, once the benefits of ambulation during prolonged hospitalization for coronary events had been recognized, cardiac rehabilitation programs have evolved, to comprehensive cardiovascular risk reduction programs, with exercise being an integral component of the program, but not the only component. Since, the hospital says that, MI has dramatically decreased over time, thereby reducing the opportunity for in-hospital risk factor interventions, outpatient cardiac rehabilitation programs have gradually broadened their scope to become an important avenue for secondary prevention38,.
resistant training. Prescribed and supervised residence training enhances muscular strength and endurance, functional capacity and independence, and quality of life while reducing disability in persons with CHD.Endurance training induces greater improvements in aerobic capacity and associated cardiopulmonary and metabolic variables and more effectively modifies CHD risk factors. Resistant training enhances muscular strength, endurance, and muscle mass to a greater extent39.
Nutrition Counseling37 is necessary to assess the dietary habits of the patient to obtain an estimate of total caloric intake, as well as daily consumption of saturated fat, cholesterol, sodium, and other nutrients. Patients should be recommended a diet low in fat (especially saturated fat), and high in complex carbohydrates.As a general guideline40, the diet should consist of 50-60% calories from carbohydrates, up to 30% from fat (with saturated fat forming 10% or less), and 10-15% from protein. Individualized plans should be formulated, depending on the presence of risk factors, such as diabetes, hypertension, and hypercholesterolemia.
After an MI, some of the common psychological reactions that patients may experience are: low mood, fearfulness, sleep disturbance, irritability, anxiety, acute awareness of minor somatic sensations or pains, poor concentration and memory.It should be explained to the patient that these symptoms are normal, that they are universal, and are part of the natural course of recovery following any potentially life threatening event41.
continuing medical education programs, Sri Lanka is a developing country and there is no established compulsory continuous medical education program or revalidation process at present. There is a National Continuous Professional Development Program to find out. No studies have been done on knowledge assessment on secondary prevention of cardiovascular disease in Sri Lanka42.
Counseling may be an effective tool in reducing behavioral risk factors for CVD, doctors do not counsel their patients about lifestyle changes to prevent CVD. In this study the knowledge about prevention with regard to diet was inadequate and exercise and lipids were adequate but not good. Only few physicians knew about the exact dietary recommendations of fat and salt and the frequency of exercise needs. Blood pressure control plays a vital role in the prevention of CVD. In a recent meta-analysis it was found that blood pressure reduction of 10 mmHg systolic or 5 mmHg diastolic reduced the rate of coronary heart disease by 22%.43
The educational and vocational counseling components of cardiac rehabilitation programs should further improve the ability of a patient to return to work.Therefore, the time to return to work, after an MI can vary greatly from about two weeks, to upwards of six weeks. Patient Participation in Cardiac Rehabilitation International guidelines and experts recommend the use of cardiac rehabilitation after MI.
to assess the patients’ out-of-hour care needs and to reduce the frequency of check-ups. Using telephone not only reduces the costs and facilitates to effective healthcare, but it also improves the relationship between patients and healthcare providers.
Research has shown that telephone-delivered interventions could improve self-efficacy among patients. Telephone-based interventions could result in clinically important reductions in hospital readmissions. Several studies in Iran have also reported that such interventions could improve the patients’ quality of life after pacemaker implantation, reduce readmissions in patients with heart failure, reduce glycosylated hemoglobin, and play an effective role in controlling the glycemic level.
The study aimed to investigate the effect of nurse-led telephone follow-up on medication and dietary adherence among patients after myocardial infarction. The results of the study confirmed the positive effects of tele-nursing intervention on improvement of adherence to dietary and medication regimen in the patients with MI. Telephone-delivered follow-ups and consultation can be applied as a useful method for self-assessment, monitoring, making decisions, and providing patients with the necessary advice45.
1.2 SIGNIFICANCE AND NEED FOR THE STUDY
sufferers die before reaching the hospital, the risk of further myocardial infarction is not to be taken slightly, with 10% death rate in the year after discharge46.
According to Lopez, Mathew, Jamison and Murray47 found cardiovascular diseases, especially coronary heart disease are the leading cause of mortality in the developing world. The CHD prevalence in South Asia is 3.2%. It is 10% in New Delhi and 11% in Chennai. This alarming rate signifies the importance of the need for effective preventive health measures. Different studies have reported that the prevalence of the risk factors of ischemic heart disease in Delhi are as follows: smoking 59%, obesity 41%, hypertension 22%, positive family history 17%, diabetes 10% and hypercholesterolemia 8%.
The eighth target in the global NCD48 action plan states at least 50% of eligible people should receive drug therapy and counseling to prevent myocardial infarctions and strokes. The UN general assembly will convene a third high 1evel meeting on NCD in 2018 to take stock of national progress in attaining the voluntary global target by 2025.
Times of India May 19 2016 50says every 33 seconds 1 person is dying become of M.I in India.Life style health and fitness men living in cities are there times more prone to heart attacks then people lining village. As for women the risk rises after menopause says Dr.Mehta senior consultant cardiologist 51.According to the World Health Organization’s Global Status Report of NCD 2010. Geneva52: the incidence of MI in India is 64.37/1000 people in men aged 29-69 years, alcohol intake led to 30% lower CHD incidence.
The prognosis after MI varies greatly depending on a person's health, the extent of the heart damage, and the treatment given. In those who have an STEMI in the United States, between 5 and 6 percent die before leaving the hospital and 7 to 18 percent die within a year. Morbidity and mortality from myocardial infarction has improved over the years due to earlier and better treatment.According to NICE53 twice as many men had MIs as women.
Cardiovascular disease (CVD) remains the leading cause of death globally54, with an estimated 17 million deaths from CVD in 2011, or about 3 in every 10 deaths of CVD deaths, 7 million deaths are due to coronary heart disease (CHD) and 6.2 million due to stroke. The annual number of people who die from CVD is predicted to reach 23.3 million by 2030 and CVD is projected to remain the single leading cause of death by Information and Trial Modification study55.
were significant regional variations. Goa, Tamil Nadu, Andhra Pradesh, Punjab had high CVD mortality compared to the low mortality rate in the central states of Uttar Pradesh, Madhya Pradesh and Rajasthan.
The Inter Heart study57, performed in 27,000 cases of acute myocardial infarction and controls in 52 countries reported that standard risk factors such as smoking, abnormal lipids, hypertension, diabetics, high waist-hip ratio, sedentary life style, psychological stress, and a lack of consumption of fruit and vegetables, in both multiple cardiovascular psychological and biological risk factor groups is more than 90% in India than in South Asians.
Coronary Artery Diseases (CADs), which have been consistently ranked among the most common Cardiovascular Diseases (CVDs), are the leading cause of mortality and morbidity in both developed and developing countries. CADs account for 21% of mortality and morbidity worldwide in both men and women. In Iran, also, CAD is the leading cause of mortality and morbidity and almost 138,000 Iranians die due to such diseases annually. Almost 50% of such deaths occur due to Myocardial Infarction (MI). According to the report published by World Health Organization 44,59(WHO), approximately 14 million people globally die due to MI. However, recent surgical and pharmaceutical interventions have reduced the mortality resulting from MI. But, prognosis of patients with acute MI is still poor.
Patients with MI are commonly advised to take lots of medications for long periods of time to reduce the complications, morbidity, and mortality. Despite health care providers’ advice, medication and dietary adherence is still poor among the patients with MI that can increase the risk of disease recurrence and re hospitalization. Moreover, 48% of all readmission in patients with MI are due to lack of adherence to dietary and medication regimen. It is essential for clinicians and caregivers to encourage the patients to adhere to appropriate methods which modify the risk factors of CVDs60.
part of nursing care. Nurses’ optimal selection of the type of nursing education and consultation is of great importance which leads to patients’ adherence to treatment regimen, delay progression of the disease, and reduction of the disease-related complications61.
According to the USA National Cholestrol Education Program62 (NCEP), Dyslipiderma was defined as criteria (high LDL cholestrol ≥100 mg/dl and low HDL cholesterol as < 40 mg/dl in males and < 50 mg/dl in females). The cut off value was 200 mg/dl for hypercholesterolemia and 150 mg/dl for hypertriglyceridemia. Either of above mentioned criteria was used for lipid profile disorders (NCEP, 2002).The study showed a decline in lipid profile disorders at six months in the study group as compared to baseline whereas an increase was observed in lipid profile disorders at six months compared to baseline in the control group although the difference was not significant. There was a significant reduction in lipids at six months in the study group as compared to the control group.
Poor knowledge of patients was considered a major problem by our respondents. To educate patients, patent information leaflets can be utilized. Self care diary maintenance can be promoted. To educate patients, patent information leaflets can be utilized. Self care diary maintenance can be promoted Lower the serum LDL-cholesterol level, the better it is for cardiovascular disease prevention. The knowledge on lipids was inadequate. This was also revealed by a study done by Freedman et al63.
reduce the risk of cardiovascular death or acute myocardial infarction (AMI) by about 30% in post AMI population.65,53 However, non-adherence to prescribed medication is a problem with potentially large public health implications that has received increasing attention in the last years.
Studies assessing the knowledge and efforts of doctors in secondary prevention have found that doctors do not stress enough on the role of secondary prevention to their patients .Lack of awareness about prevention guidelines and lack of motivation could be possible reasons. The lack of adherence to guidelines leads to erroneous or suboptimal management of risk factors66.
In the analysis by Taksler et al67 by the Institute of Medicine (US) Committee on Preventing the Global Epidemic of Cardiovascular Disease among US Preventive Services Task Force recommendations for preventive care, tobacco cessation, diabetes control, weight loss, and BP reduction were consistently ranked among the top guidelines for increases in life expectancy across patients.
Tobacco cessation ranked high in their study as well as the INTERHEART study68, which demonstrated that acute myocardial infarction almost tripled for a current smoker versus a nonsmoker. Study states successful smoking cessation is the most effective of all lifestyle changes for current smokers. The analysis supports the findings of several large‐scale studies that CVD risk can be modified by lifestyle changes.
similar to two other cohort studies of patients with a history of CHD. Considering that 15% of this sample of US adults was smoking despite having a history of CHD, smoking cessation should continue to be a high priority to lower recurrent CHD and mortality risk in individuals with CHD69.
Knowledge of secondary prevention, especially lifestyle modification, for coronary disease was poor among the group of physicians from tertiary hospitals. Jiang et al57Study suggested that efforts must be made to educate physicians to improve their knowledge and improve patient care70.
Prevalence of the following risk factors for myocardial infarction: Age, sex, diet, smoking, alcohol consumption, history of hypertension, history of diabetes mellitus, and lipid profile were studied. The study stated that Smoking and heavy drinking cessation, treatment of hypertension and reduction in blood glucose, correction of abnormal lipid profile either through use of statins or by dietary modification may be important in preventing IHD in Asian Indians71,72.
The incidence of myocardial infarction (MI) in the world varies greatly. According to a Spanish study,72 the crude coronary heart disease (CHD) incidence rate was 300.6/100,000 person-years for men and 47.9/100,000 person-years for women. The incidence of MI in India is 64.37/1000 people in men aged 29-69 years, alcohol intake led to 30% lower CHD incidence.
are neglecting their health and follow a life style according to the western standards which leads them to become victims of heart diseases. In recent trends, the emergence of unhealthy life style, modernization and lack of knowledge and unawareness about the risk failures has led to the deterioration of the discuses causing mortality and morbidity rates and cost to the society and in turn leads to anxiety and stress due to the lack of proper knowledge and psychological support. Many people are anxious about their life after the first acute myocardial infarction incident and have very little knowledge about AMI which initiates anxiety and leads to stress.
Nurses working in cardiac unit can impart knowledge about M.I that will help the clients to cope up with the situation psychologically as well as physiologically. In India cardiovascular mortality is likely to rise by 103% in men and 90% in women during the period of 1985-2015 and the cardiovascular disease will be the greatest killer by the year 202073.
According to Chopra 74(heart care foundation) in India nearly 3 crores of the people in our county are estimated to be the patients of CAD. In Delhi alone 2.5 lakhs of people in the age group between 25 to 64 suffered from coronary problems leading to angina and heart attack.Most of the M.I patients do not have adequate knowledge regarding their disease particularly in developing county live India, where very little attention being paid to health of MI patients.
Asian countries including India and is estimated to be as high as in European population. The world health organization estimates 16.7 million people around the globe die every year. WHO76 report says that ischemic causes of global burden of diseases on economics of the world in the year 2020.
.
John G.Ganto ,Cataning I kiefe (2011)77 conducted number of coronary artery disease mortality rise in patients with first M.I .The design was observed from the natural registry of M.I patients were examined the presence and absence of 5 major traditional coronary heart disease rise factors (hypertension) (smoking, dyslipidemia, diabetes and family history of coronary disease).Results was majority 85.6% of patient who presented with initial M.I had at least 1 of the 5 coronary heart disease risk factors, 14.4 % had none of the 5 risk factors. Age varied inversely with the number of coronary heart disease risk factors, from mean age of 71.5 years with ‘o’ risk factors to 56.5 years with 5 risk factors.
World health organization78 says cardiovascular diseases are the major cause of mortality globally, as well as in India. They are caused by disorders of heart and blood vessels. Common modifying factors werephysical inactivity, unhealthy diet , harmful use of tobacco and alcohol.Low density lipoprotein , (LDL-C) bad cholesterol is the leading cause of heart attacks. Diabetes , smoking, high blood pressure, genetic history, life style ,especially higher intake of carbohydrate rich foods and lack of physical exercise are other factors that leads are heart attack.
diseases are preventable.Healthy eating with consumption of fresh fruit and vegetables, coupled with daily exercise and a stress free environment also can ward off heart attack risks, lifestyle changes like stress reduction checkups including lipid profile and adherence to medications are very important.
Cardio vascular diseases have now become the leading cause of mortality in India. The global burden of disease study estimate of age standardized CVD death rate of 272per 100000 population in India is higher than the of 235 per 100000 population.International Journal of Public health80 reported that 21.4% hypertension prevalence in aged 25-64 in 11 village in the state in which the prevalence was nearly the same in both sex.Dr. Pradeep kaur44 the scientist at National Institute of Epidemiology Chennai stated that about 75% of people with hypertension were immigrant of their condition and more person belongs to younger age. Hypertension is one of the major risk factors for cardio vascular disease, 24.5% of death in aged 45-59 year in Tamil Nadu are caused by disease of the circulatory system. The fact is 6.6% of people on treatment for B.P.
The Hindu – Dec 201381 says that winter mornings may be rustier time for heart attack. Heart attack can occur at every time. A recent study shows that 53% were heart attack occurs during winter than other seasons stated by Wikepedia.
on their physical and psychological parameters which helped the investigator to bring additional data for nursing knowledge.
1.3 CONCEPTUAL FRAMEWORK
Betty Newmans System model was utilized to guide the researcher in conducting the proposed research work.
1.3.1 General concepts of Betty Newman’s system model
Conceptualization refers to the process of developing and refining abstract.A conceptual model provides for logical thinking, for systematic observation and interpreting the observed data.The frame work of this study was based on Betty Newman’s system models, which consider the researcher is an open system who interacts with the work environment. Newman System mainly focuses the client system response to stressors from the internal and external environment and primarily concerned with effects of stress on health.
Basic core structure
The person has a core consisting of Basic structures that compares the factors of energy resources necessary to client survival. Three lines surround the basic structure in first, the line of resistance and then the normal line of defense and the outer most is the flexible line of defense.
Line of resistance
Normal line of defense
A solid line outside the lines of resistance is called normal line of defense.It is the person’s usual level of wellness.
The flexible line of defense
The flexible line of defense depicted in the model as a broken line outside the normal line of defense.The flexible line of defense means the person is able to protect them from the stressors breaking through the normal line of defense
Stressors
Newman defines stressors as stimuli that produce tensions and cause system instability. Stressors are present both outside and within the system. The stressors are classified as intra, inter, extra personal in nature.
Reaction to stressors
If the flexible line of defense cannot protect a person from the stressor,the stressor can break through the normal line of defense, causing a reaction. The resulting reaction depends on the Client’s line of resistance.
Degrees of Reaction
Reaction
Newman does not point that reactions and outcomes may be positive or negative and discusses system movement toward illness or death.
Environment
Newman (2002) defines environment as all the Internal and External factors influences the client system. The Internal environment exists within the client system and is intrapersonal. The External environment exists outside the client system and is inter and extra personal.
Health
Newman (2002) identifies health as optimal system stability,harmony among the Physiological, psycological, developmental, Socio cultural, Spiritual variables or optimal state of wellness at a given time. The client system move towards illness and death or towards wellness in healthillness continuum and the nurse uses the balance or harmony needed through primary, secondary and tertiary interventions to reduce client’s stressors and help to attain maximum level of wellness.
Primary prevention
It refers to the intervention before the reaction occurs. According to Newman the stressor is suspected or identified and viewed as a possible risk of normal line of defense.
Secondary prevention
Tertiary prevention
It refers to the interventions after the active treatment of a reaction.
Nursing
Newman describes the nursing is to help the patient to attain, maintain or retain system stability.