Original Article
Comparison of side effects of chemotherapy between
the elderly Uygur patients and the Han patients
with non-Hodgkin lymphoma
Xun Li*, Wei Liu*, Li Guo, Yan Li, Zhen-Hui Zhao, Xin Hu, Shun-E Yang
Department of Breast Cancer and Lymphoma, Affiliated Tumor Hospital of Xinjiang Medical University, Urumqi 830011, People’s Republic of China. *Equal contributors.
Received August 21, 2015; Accepted November 26, 2015; Epub February 15, 2016; Published February 29, 2016
Abstract: Purpose: This study is to detect whether the different side effects of the same amount chemotherapy drugs administered in elderly Uygur patients with non-Hodgkin lymphoma (NHL) and aged Han NHL patients are related to the levels of cytogenetic damage in the two ethnics. Methods: Sister chromatid exchanges (SCE) rate, hypoxanthine guanine phosphoribosyltransferase (HPRT) gene mutation rate, micronucleus (MN) rate, and white blood cell (WBC) count in 20 cases of two groups before and after chemotherapy were compared. Results: Before chemotherapy (at baseline level), the average SCE rate, HPRT gene mutation rate, MN rate were lower in elderly Uygur patients than that in aged Han patients, but the difference was not significant (P>0.05). After each cycle of chemotherapy,the average SCE rate, HPRT gene mutation rate, MN rate in elderly Uygur patients were lower thanthat in Han patients, but this difference was not statistically significant (P>0.05). However, the three indicators described above in two ethnics were significantly higher after each cycle of chemotherapy than those before each cycle of chemotherapy (P<0.05). In addition, the decreased level of average WBC in aged Uygur NHL patients was lower than that in Han patients after each cycle of chemotherapy, but this difference was not statistically significant (P>0.05). Spearman analysis showed that there is a negative correlation between the three indicators and the decrease of WBC counts. Conclusion: The difference of side effects of chemotherapy for NHL between Uygur and Han patients is related to the levels of cytogenetic damage.
Keywords: SCE rate, HPRT gene mutation rate, MN rate, the Uygur nationality, non-Hodgkin lymphoma
Introduction
Diffuse large B-cell lymphoma (DLBCL) is one of the most common subtypes of non-Hodgkin lymphoma (NHL), accounting for 30% to 40% of NHL patients [1-4]. The incidence of DLBCL increases with age [5]. The majority of patients with DLBCL are over the age of 60 years [6], with approximately 40% of patients aged over 70 years [7-9]. Xinjiang is a multi-ethnic region, with Uygur and Han population accounting for about 47% and 38.2% of the total population by the end of 2011, respectively, according to the statistical results by XIN JIANG office of Facts and Figures, indicating that the ethnic Uygur group is the majority in Xinjiang region [10]. Chemotherapy for non-Hodgkin’s lymphoma (NHL) acts in a dose-dependent manner gener-ally. During our clinical work, it was found that
the side effects of chemotherapy are nausea, vomiting and severe bone marrow suppression (I-II degree majority). Some others were all mild in the elderly Uygur patients with NHL group after chemotherapy using the same dosage as in the elderly Han case, in comparison with the elderly Han patients with NHL. This difference may be caused by cytogenetic diversity between the Uygur and Han population.
cannot enter mitosis with the child nucleus when cells enter the next division step, forming the round or oval micronucleus (MN) with com-pletely unequal sizes in the cytoplasm (diame-ter <1/3 of main nuclear). The hypoxanthine guanine phosphoribosyltransferase (HPRT) ge- ne is located on the X sex chromosome distal Xq26 region, encoding t HPRT protein. This pro-tein is a membrane enzyme in the purine sal-vage pathway involved in cell nucleotide syn-thesis in vivo. Lack of or reduced activity of this protein affects nucleic acid metabolism. SCE test, HPRT gene mutation, and MN test are often used due to the sensitive detection of cytogenetic damages. Therefore, they were widely used in the fields of chemical mutagen-esis, environmental monitoring, and cancer research.
In this work, we have investigated the differ-ence of cytogenetics in elderly Uygur and Han patients with NHL using detection of SCE rate, HPRT gene mutation rate, MN rate and the decrease level of white blood cells (WBC) counts before and after chemotherapy. Therefore, this study was to detect whether there were cytogenetics differences in periph-eral lymphocytes between the elderly Uygur and Chinese NHL before and after ch- emotherapy.
Materials and methods
Patients
A sample size calculation was performed prior to the commencement of this study. Patients including 20 Uygur ethic cases and 20 Han pop-ulation cases were enrolled in this study after providing informed consent. These patients had been chemotherapy-naive patients with NHL from CancerHospital affiliated with Xinjiang Medical University in 2012-2015. They were aged 60 to 70 years old. All patients were received heparin to achieve systemic anticoag-ulation. Two microliters of peripheral blood samples were collected from patients before and after the end of chemotherapy within 24 hours. Blood samples were drawn into sterile tubes and stored at 4°C, inoculated within five hours. The patients who were not able to toler-ate the chemotherapy showing severe adverse effects, and the patients who received the adjusted chemotherapy, were calculated by the
cumulative period of CHOP (combination of cyclophosphamide, doxorubicin/hydroxydoxo-rubicin, vincristine and prednisone)-based che-motherapy. The patients treated with reduced CHOP-based chemotherapy were also inclu- ded.
Administration of CHOP chemotherapy
CHOP is commonly administered in 4 cycles of chemotherapy, including cyclophosphamide (CTX) 750 mg/m2, day 1, intravenous injection; doxorubicin/hydroxydoxorubicin 50 mg/m2, day 1, intravenous injection; vincristine 1.4 mg/m2 (maximum, 2 mg), 1st day intravenous injec-tion; prednisone tablets 100 mg/m2 first to the fifth day, oral, 21-days repeat. The patients were monitored for four cycles.
Inclusion criteria and exclusion criteria
The patients enrolled in this study were select-ed using stringent inclusion criteria as follows: 1. The new cases with pathological stage I-III of NHL proved histologically. 2. ECOG (Eastem Cooperative Oncology Group) score ≤2 points in Non-Hodgkin’s lymphoma patients. 3. No other complications, no poison, radiation expo-sure history. 4. Age ≥60 years old. 5. Long-term living in the Xinjiang region not less than 30 years. Exclusion criteria were as follows: 1. Age >70 years old. 2. NHL patients received chemo-therapy previously. 3. Smokers.
SCE assay
Cytokinesis-block micronucleus (CBMN) assay
Criteria for binucleated lymphocytes were as follows: a cell with two major micronuclei of substantially equal size; no more than 6 micro-nuclei in a cell; nuclear material possibly con-nected between the two major nuclei; and pos-sible overlap between the two major nuclei. In the dual-nuclei cells, micronucleus diameter was one sixteenth to one third of the main nucleus with no light refraction. No nuclear materials were connected between the major nuclei. There were possible overlaps with the border of the major nucleus. However, each nuclear membrane could be observed clearly. High magnification (×400 times) microscope was used. For each specimen, 1000 pairs of core lymphocytes were counted. The number of dual-nuclei cells was calculated to obtain the incidence of micronuclei (MNf, ‰) (Figure 1B). HPRT gene mutation frequency examined by multinucleated cells
Cells containing two or more nuclei were con-sidered as mutant cells. The number of sam-ples containing a 6-Thioguanine (6-TG) in every 1000 transformed cells were divided by the number of samples without 6-TG, which gave hprt gene mutation rate (‰) (Figure 1C). Statistical analysis
Quantitative data were given as mean ± stan-dard deviation. SCE rates before or after each chemotherapy, HPRT gene mutation rate, MN compare rates, Uygur and Chinese indexes were indicated by paired t test. Correlation be- tween SCE rate and WBC counts were analyzed by spearmancorrelation. P<0.05 was consid-ered as statistically significant.
Results
Comparison of SCE rate, HPRT gene mutation rate, and MN rate between the Han group and the Uygur group of elderly NHL patients before chemotherapy and after four-cycle chemo-therapy
To determine whether there is difference in SCE ratebetween the Han group and the Uygur group of elderly NHL patients before chemo-therapy and after four-cycle chemochemo-therapy, FPG method was used to evaluate the mean SCE ratein both groups. As given in Table 1, the average SCE rate was significantly lower in Uygur NHL elderly patients than in the Han patients before chemotherapy (at baseline) (P<0.05). With the increase of chemotherapy cycles, the average SCE rate was significant lower than in the aged Uygur NHL patients both before and after chemotherapy than in the Han patients (P<0.05), as indicated in Table 1. These results showed that the mean SCE rate in elderly Uygur was lower than in Han patients, indicating an ethnic-dependent pattern of NHL incidence.
[image:3.612.89.524.73.178.2]To explore whether there is difference in MN ratebetween the Han group and the Uygur group of elderly NHL patients before chemo-therapy and after four-cycle chemochemo-therapy, the number of lymphocytes and micronuclei were counted using oil-immersion microscope to determine the mean MN ratein both groups. The average MN rate has no significant differ-ences between the aged Uygur NHL patients and the Han patients either before or after the first cycle of chemotherapy (P>0.05). However, after the first chemotherapy cycle, it was signifi-cantly lower in aged Uygur NHL patients than the Han patients either before or after chemo-therapy (P<0.05), as shown in Table 2. These
Table 1. Comparison of the average rates of SCE between the Han group and Uygur group of elderly NHL patients before chemotherapy and after chemotherapy of four cycles
Ethnicity
1st cycle (n=20) 2nd cycle (n=20) 3rd cycle (n=19) 4th cycle (n=19)
Before
chemo-therapy After chemo-therapy Beforech emo-therapy After chemo-therapy Before chemo-therapy After chemo-therapy Before chemotherapy After chemotherapy
Uygur 14.25±3.35 23.25±7.66 34.75±8.35 40.25±9.39 37.63±9.03 44.21±8.70 39.47±7.05 46.05±7.74 Han 18.25±6.34 30.25±8.03 42.50±10.07 48.00±10.18 45.00±8.33 52.11±7.33 46.84±7.49 53.68±6.42
t-value 2.49 2.82 2.65 2.50 2.61 3.03 3.12 3.31
P-value 0.017* 0.008* 0.012* 0.017* 0.013* 0.005* 0.004* 0.002*
[image:4.792.93.704.235.318.2]Note: Two-sample t-test (large sample approximations). *Significant at 5% level, P-value corrected up to three decimal. SCE: Sister chromatid exchanges rate.
Table 2. Comparison of the average rates of MN between the Han group and Uygur group of elderly NHL patients before chemotherapy and after
chemotherapy of four cycles
Ethnicity
1st cycle (n=20) 2nd cycle (n=20) 3rd cycle (n=19) 4th cycle (n=19)
Before
chemo-therapy After chemo-therapy Before chemotherapy After chemo-therapy Before chemo-therapy After chemo-therapy Before chemo-therapy After chemotherapy
Uygur 17.55±5.10 32.10±7.96 32.30±7.90 43.20±6.73 36.05±7.34 45.42±6.34 41.42±6.64 45.68±5.90 Han 20.15±11.44 30.15±9.29 37.75±8.57 48.15±7.18 41.63±6.71 52.16±6.38 46.53±5.86 53.26±6.28
t-value 0.93 -0.71 2.09 2.25 2.45 3.27 2.51 3.84
P-value 0.359 0.481 0.043* 0.031* 0.019* 0.002* 0.017* 0.000*
Note: Two-sample t-test (large sample approximations). *Significant at 5% level, P-value corrected up to three decimal. MN: micronucleus rate.
Table 3. Comparison of the average rates of HPRT between the Han group and Uygur group of elderly NHL patients before chemotherapy and
after chemotherapy of four cycles
Ethnicity
1st cycle (n=20) 2nd cycle (n=20) 3rd cycle (n=19) 4th cycle (n=19)
Before
chemo-therapy After chemo-therapy Before chemo-therapy After chemo-therapy Before chemo-therapy After chemo-therapy Before chemo-therapy After chemo-therapy
Uygur 83.93±36.27 148.10±45.98 95.85±33.26 159.10±45.53 108.84±32.71 172.42±47.04 108.53±32.80 162.11±41.60 Han 84.75±62.50 146.65±51.16 98.05±60.95 165.35±47.92 117.37±57.13 176.32±47.38 116.16±54.39 169.19±47.99
t-value 0.05 -0.09 0.142 0.42 0.57 0.27 0.52 0.48
P-value 0.960 0.925 0.893 0.675 0.582 0.793 0.603 0.631
[image:4.792.90.712.379.460.2]results suggest that there is no significant dif-ference in the mean MN rate between elderly Uygur and Han patients at the baseline level, however, it also denotean ethnic-dependent pattern of NHL incidence after chemotherapy. To clarify whether there is difference in HPRT ratebetween the Han group and the Uygur group of elderly NHL patients before chemo-therapy and after four-cycle chemochemo-therapy, HPRT rate was calculated to determine the mean HPRTratein both groups. There was no significant difference of the average HPRT gene mutation rate in the whole chemotherapy cycle in stages 1-4 between the two populations (P>0.05), as shown in Table 3. These results indicate that there is ethnic-independent in mean HPRT rate in both two groups.
Comparison of the average rate of SCE, MN rate, HPRT gene mutation rate before and after each cycle of chemotherapy in elderly Uygur and Han NHL patients themselves
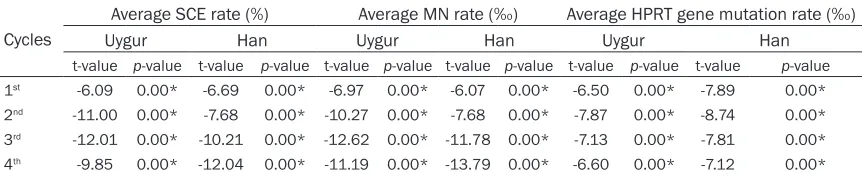
To verify whether SCE, MN rate, HPRT gene mutation ratecan reflect the cytogenetic man-age caused by chemotherapy drugs, compari-son of the average rate of SCE, MN rate, HPRT gene mutation rate before and after each cycle of chemotherapy in elderly Uygur and Han NHL patients themselves was performed. The mean SCE rate, MN rate, and HPRT gene mutation rate were significantly higher after each cycle of chemotherapy than before each cycle of che-motherapy in all the four cycles for both elderly Uygur NHL patients and Han patients (P<0.05), as shown in Table 4. These results indicate that SCE rate, MN rates, HPRT gene mutation rate can sensitively reflect cytogenetic damage induced by anti-tumor chemotherapy, which has a good dose-effect relationship with the cumulative dose chemotherapy, further dem-onstrating the reliability of the Tables 1-3.
Comparison of decrease level of WBC counts in elderly Uygur patients with NHL and Han patients
To determine whether there is significant differ-ence in blood toxicity caused by chemotherapy in elderly Uygur patients with NHL and Han patients, the decrease level of WBC counts was performed. The decreased level of average white blood cell count is lower in elderly patients with NHL Uighur than in Han patients after each cycle of chemotherapy for all the four cycles, but the difference was not statistically signifi-cant (P>0.05), as is shown in Table 5. These results suggested that WBC count was slightly higher in elderly Uygur NHL patients and the hematological toxicity degree due to chemo-therapy was a little lower than in Han patients, showing no significant.
Pair-wise correlation analysis of the average SCE rate, HPRT gene mutation rate, MN rate, and WBC count in the aged NHL patients Spearman correlation coefficient (R) and the value of probability P were shown in Figure 2. A moderately negative correlation was observed between the average SCE rate of every cycle and the correspondingly average WBC count in all the patients (R=-0.833, P=0.01, P<0.05) (Figure 2A). The linear regression equation was as follows: Y=-2.511X+48.297. We also observed a moderately negative correlation between the average MN rate of every cycle and the correspondingly average WBC count in all the patients (R=-0.833, P=0.01, P<0.05) (Figure 2B). The linear regression equation was as follows: Y=-3.062X+50.852. As shown in
Figure 2C, there was a moderately negative
[image:5.612.91.522.97.184.2]correlation betweenthe average HPRT gene mutation rate of every cycle and the corre-spondingly average WBC count in all the patients (R=-0.976, P<0.001). The linear
Table 4. Comparison of the average rate of SCE, MN rate, HPRT gene mutation rate before and after
each cycle of chemotherapy in elderly Uygur and Han NHL patients themselves
Cycles
Average SCE rate (%) Average MN rate (‰) Average HPRT gene mutation rate (‰)
Uygur Han Uygur Han Uygur Han
t-value p-value t-value p-value t-value p-value t-value p-value t-value p-value t-value p-value
1st -6.09 0.00* -6.69 0.00* -6.97 0.00* -6.07 0.00* -6.50 0.00* -7.89 0.00*
2nd -11.00 0.00* -7.68 0.00* -10.27 0.00* -7.68 0.00* -7.87 0.00* -8.74 0.00*
3rd -12.01 0.00* -10.21 0.00* -12.62 0.00* -11.78 0.00* -7.13 0.00* -7.81 0.00*
4th -9.85 0.00* -12.04 0.00* -11.19 0.00* -13.79 0.00* -6.60 0.00* -7.12 0.00*
Table 5. Comparison of the decreased levels of WBC count between elderly Uygur patients with NHL and Han patients before and after each chemotherapy cycle
cycles WBC count (10
9/l)
t-value P-value
Han (n1-2 cycles=20; n3-4 cycles=19) Uygur (n1-2 cycles=20; n3-4 cycles=19)
1st 4.34±1.61 3.91±1.59 0.86 0.396
2nd 4.45±1.55 3.94±1.28 1.12 0.272
3rd 3.28±0.99 3.22±0.91 0.204 0.840
4th 3.27±1.00 2.99±1.08 0.839 0.407
Note: Two-sample t-test (large sample approximations).
regression equation was as follows Y=-1- 6.62X+196.863.
Discussion
In this study, the statistical results showed that mean SCE rate was significantly lower in the aged Uygur patients than in elderly Han NHL patients before chemotherapy (baseline lev-els). However, MN rate, HPRT gene mutation rates were not significantly different between
the two population. Comparative studies of SCE rate, HPRT gene mutation rate, MN rate among different ethnic groups are rarely reported.
[image:6.612.91.521.214.587.2]Previous study has shown that frequency distri-bution of HLA alleles originated from Caucasian is higher in Xinjiang Uygur than in other ethnic groups, equivalent to the numerical of Caucasians, suggesting that Uighur groups have Caucasian blood, having different genetic
background with Han population [11]. That may be the reason why Uygur NHL patients have sig-nificant lower average SCE rate than Han patients when at baseline. However, there no significant differences of MN rate and HPRT gene mutation rate between the two popula-tions. This finding may be due to the following reasons: (i) although the Uighur patients con-tain Caucasian descent, and have different genetic backgrounds from Han patients, cyto-genetic characteristic is similar in the two popu-lations. Because all patients involving in this experiment were long-term residents in the Xinjiang region for not less than 30 years, and the common area, eating customs, living condi-tions may contribute to the similarity. HPRT gene mutation rate and MN rate are influenced by many factors [12-17], such as certain drugs, vitamins [18], chemical materials [19] etc, and wecannot exclude the confounders above com-pletely. (ii) The dynamics of the cell itself, lead-ing to some mutant cell loss [20]. (iii) Although the average MN rate and HPRT gene mutation rate did not show a significant difference between the two population before chemother-apy (at baseline), however, the indicators above were lower in elderly Uighur patients than in Han patients, possibly due to the sample size. (iv) The significant difference of SCE rate and the no significant difference of HPRT gene mutation rate and MN rate between Uighur elderly patients with NHL and Han patients before chemotherapy (at baseline) may reflect the particular difference of cytogenetics in Uighur elderly NHL patients and the polymor-phism of genetic material among different human ethics.
The average SCE rate was significantly higher after each cycle chemotherapy in both elderly Han patients and Uygur patients with NHL than before chemotherapy, from initial py to the end of the fourth cycle of chemothera-py (P<0.05). This is consistent with the find- ings of Silva [21], Mourelatos C et al. [22], Mourelatos et al. [23] and Suspiro A [24]. The average HPRT gene mutation rate, MN rate were significantly increased after each cycle of chemotherapy, which is consistent with the reports from Tates et al. [25] and Elsendoom et al [26]. These studies again show that the che-motherapy can cause cytogenetics damage. As shown in this study, the mean SCE rate, MN rate, HPRT gene mutation rate decreased
before each cycle of the second, third and fourth cycle chemotherapy compared to after each cycle of the first, second and third cycle chemotherapy in the two populations. However, these rates did not fully restore to the baseline (before the initial chemotherapy) level, which showed the repair of chemotherapy drugs to DNA damage was incomplete [27].
The average MN rate was shown the same results with the average SCE rate since the beginning of the second cycle chemotherapy. This suggests that elderly Uygur patients with NHL showed different degree of cytogenetic damage and DNA repair mechanisms from the Han patients. The complexity and polymor-phisms in the genetic materials between ethnic groups may lead to different clinical toxicity of chemotherapy drugs. spearman correlation analysis showed that the average SCE rate, MN rate, HPRT gene mutation rate were all moder-ately negatively correlated with WBC cells in elderly patients with NHL.
Acknowledgements
This study was supported by the Innovative Foundation of Xinjiang Medical University (XJC201153).
Disclosure of conflict of interest
None.
Address correspondence to: Shun-E Yang, Depart- ment of Breast Cancer and Lymphoma, Affiliated Tumor Hospital of Xinjiang Medical University, Storey 16, Comprehensive Building, No. 789 Suzhou East Street, Xinshi District, Urumqi 830011, People’s Republic of China. Tel: +86-0991-7819362; Fax: 0991-7819366; E-mail: yangshune2015@sina.cn
References
[1] Nedomova R, Papajik T, Prochazka V, Indrak K, Jarosova M. Cytogenetics and molecular cyto-genetics in diffuse large B-cell lym- phoma(DLBCL). Biomed Pap Med FacUniv- Palacky Olomouc Czech Repub 2013; 157: 239-247.
[2] Raut LS, Chakrabarti PP. Management of re-fractory diffuse large B cell lymphoma. South Asian J Cancer 2014; 3: 66-70.
[4] Song CG, Huang JJ, Li YJ, Xia Y, Wang Y, Bi XW, Jiang WQ, Huang HQ, Lin TY, Li ZM. Epstein-Barr Virus-Positive Diffuse Large B-Cell Lymphoma in the Elderly: A MatchedCase-Control Analysis. PLoS One 2015; 10: e0133973.
[5] Yoshida M, Nakao T, Horiuchi M, Ueda H, Hagihara K, Kanashima H, Inoue T, Sakamoto E, Hirai M, Koh H, Nakane T, Hino M, Yamane T. Analysis of elderly patients with diffuse large B-cell lymphoma:aggressive therapy is a rea-sonable approach for “unfit” patients classi-fied by comprehensive geriatric assessment. Eur J Haematol 2015; [Epub ahead of print]. [6] Tucci A, Martelli M, Rigacci L, Riccomagno P,
Cabras MG, Salvi F, Stelitano C, Fabbri A, Storti S, Fogazzi S, Mancuso S, Brugiatelli M, Fama A, Paesano P, Puccini B, Bottelli C, Dalceggio D, Bertagna F, Rossi G, Spina M; Italian Lymphoma Foundation (FIL). Comprehensive geriatric as-sessment is an essential tool to support treat-ment decisions in elderly patients with diffuse large B-cell lymphoma: a prospective multi-center evaluation in 173 patients by the Lymphoma Italian Foundation (FIL). Leukemia Lymphoma 2015; 56: 921-926.
[7] Zhou Z, Sehn LH, Rademaker AW, Gordon LI, Lacasce AS, Crosby-Thompson A, Vanderplas A, Zelenetz AD, Abel GA, Rodriguez MA, Nademanee A, Kaminski MS, Czuczman MS, Millenson M, Niland J, Gascoyne RD, Connors JM, Friedberg JW, Winter JN. An enhanced international prognostic index(NCCN-IPI) for patients with diffuse large B-celllymphoma- treated in the rituximab era. Blood 2014; 123: 837-842.
[8] Ha H, Keam B, Kim TM, Jeon YK, Lee SH, Kim DW, Kim CW, Heo DS. Reduced Dose Intesities of Doxorubicin in Elderly Patients with DLBCL in Rituximab Era. Cancer Res Treat 2015; 9: 1-8.
[9] Williams JN, Rai A, Lipscomb J, KoffJL, Nastoupil LJ, Flowers CR. Disease chara- cteristics,patterns of care, and survival in very elderly patients with diffuse large B-cell lym-phoma. Cancer 2015; 121: 1800-1808. [10] Li X, Abulajiang G, Li J, et al. A clinicopathologic
study of extranodal NK/T cell lymphoma, nasal type occurring in Xinjiang multiple nationali-ties. China Oncology 2012; 22: 751-756. [11] Xu MY, Hong KX, Ma J, Deng XL, Li J, Peng H,
Ruan YH, Qin GM, Zhang YZ, Xing H, Xu XH, Shao YM. Analysis of HLA-B Locus Gene Polymorphism in Sichuan Yi Ethnic Group and Xinjiang Uygur Ethnic Group. Yi Chuan 2006; 28: 913-917.
[12] Kareli DE, Pouliliou SE, Nikas IH, Psillaki AN, Galazios GC, Liberis VA, Lialiaris TS. Cytogenetic evaluation of pre-pregnancy smoking in mater-nal and newborn lymphocytes. Eur J Obstet Gynecol ReprodBiol 2012; 165: 205-209.
[13] Costa C, Costa S, Silva S, Coelho P, Botelho M, Gaspar J, Rueff J, Laffon B, Teixeira JP. DNA damage and susceptibility assessment in in-dustrial workers exposed to styrene. J Toxicol Environ Health A 2012; 75: 735-746.
[14] Kurtoglu EL, Yuksel S. Genotoxic effects of ta-crolimus on human lymphocyte cells. Genetika 2012; 48: 762-767.
[15] Tug E, Kayhan G, Kan D, Guntekin S, Ergun MA. The evaluation of long-term effects of ionizing radiation through measurement of current sis-ter chromatid exchange (SCE) rates in radiolo-gy technologists, compared with previous SCE values. Mutat Res 2013; 757: 28-30.
[16] Wagner KH, Reichhold S, Hölzl C, Knasmüller S, Nics L, Meisel M, Neubauer O. Well-trained, healthy triathletes experience no adverse health risks regarding oxidative stress and DNA damage by participating in an ultra-en-durance event. Toxicology 2010; 278: 211-216.
[17] Litviakov NV, Goncharik OO, Freidin MB, Sazonov AE, Vasil‘eva EO, Mezheritskiĭ SA, Khaliuzova MV, Bondariuk AA, Al‘bakh EN, Karpov AB, Takhauov RM. [The estimate of as-sociation between gene polymorphisms and the frequency and spectrum of cytogenetic ab-normalities in the cohort of Siberian Group of Chemical Enterprises employees exposed to professional irradiation (microarray studies)]. Radiats Biol Radioecol 2013; 53: 137-150. [18] Alzoubi K, Khabour O, Hussain N, Al-Azzam S,
Mhaidat N. Evaluation of vitamin B12 effects on DNA damage induced by pioglitazone. Mutat Res 2012; 748: 48-51.
[19] Costa C, Costa S, Silva S, Coelho P, Botelho M, Gaspar J, Rueff J, Laffon B, Teixeira JP. DNA damage and susceptibility assessment in in-dustrial workers exposed to styrene. J Toxicol Environ Health A 2012; 75: 735-746.
[20] Hakoda M, Akiyama M, Kyoizumi S, Awa AA, Yamakido M, Otake M. Increased somatic cell mutent frequency in atomic bomb survivors. Mutat Res 1988; 201: 39-48.
[21] Silva LM, Takahashi CS, Carrara HH. Study of chromosome damage in patients with breast cancer treated by two antineoplastic treat-ments. Teratog Carcinog Mutagen 2002; 22: 257-269.
[22] Mourelatos C, Kareli D, Dafa E, Argyraki M, Koutsourea A, Papakonstantinou I, Fousteris M, Pairas G, Nikolaropoulos S, Lialiaris TS. Cytogenetic and antineoplastic effects by new-ly synthesised steroidal alkylators in new- lympho-cytic leukaemia P388 cells in vivo. Mutat Res 2012; 746: 1-6.
com-bined action of esteric steroidal derivatives of nitrogen mustards. Genet Test Mol Biomarkers 2012; 16: 558-562.
[24] Suspiro A, Prista J. Biomarkers of occupational exposure do anticancer agents: a minireview. Toxicol Lett 2011; 207: 42-52.
[25] Tates AD, van Dam FJ, Natarajan AT, Zwinderman AH, Osanto S. Frequenceis of HPRT mutants and micronuclei in lymphocytes of cancer patients under chemotherapy: a pro-spective study. Mutat Res 1994; 307: 293-306.
[26] Elsendoorn TJ, Weijl NI, Mithoe S, Zwinderman AH, Van Dam F, De Zwart FA, Tates AD, Osanto S. Chemotherapy induced chromosomal dam-age in peripheral blood lymphocytes of cancer patients supplemented with antioxidants of placebo. Mutat Res 2001; 498: 145-158. [27] Koishi S, Kubota M, Sawada M, Hirota H,