Original Research Article
Different causes of prolonged unconjugated Jaundice in the newborns
Vijay Agrawal*, Alok Kumar Goyal, J. N. Sharma, Murli D. Yadav
INTRODUCTION
Prolonged unconjugated hyperbilirubinemia is a type of neonatal jaundice, which occurs in infants with high bilirubin levels (>10 mg/dl) persisting beyond 14-21 days.1 Prolonged unconjugated hyperbilirubinemia is a
common problem among new born, and the prevalence rate has been estimated at 2-15%. Although this condition is normally manageable, it may sometimes be a sign of other serious diseases. According to the literature, breastfeeding is a major cause of prolonged jaundice, and about 40% of infants who are exclusively breastfed are diagnosed with this disorder.2-5 Among other pathological
causes associated with prolonged hyperbilirubinemia are urinary tract infection (UTI), congenital hypothyroidism and hemolysis. Therefore, these factors should be taken into account in the evaluation of neonates for jaundice. Early diagnosis and treatment of hyperbilirubinemia could prevent further complications in term and preterm infant. Breast milk jaundice occurs later in the newborn period, with the bilirubin level usually peaking in the sixth to 14th days of life. This late-onset jaundice may develop in up to one third of healthy breastfed infants.6 It
has been suggested that bilirubin uptake in the gut (enterohepatic circulation) is increased in breast fed babies, possibly as the result of increased levels of
ABSTRACT
Background: Prolonged unconjugated hyperbilirubinemia is a type of neonatal jaundice, which occurs in infants with high bilirubin levels (>10 mg/dl) persisting beyond 14-21 days. Prolonged unconjugated hyperbilirubinemia is a common problem among newborns, and the prevalence rate has been estimated at 2-15%. According to the literature, breastfeeding is a major cause of prolonged jaundice, and about 40% of infants who are exclusively breastfed are diagnosed with this disorder. Among other pathological causes associated with prolonged hyperbilirubinemia are urinary tract infection (UTI), congenital hypothyroidism and hemolysis. So, this study was done to know the different causes of unconjugated jaundice in newborn.
Methods: This Hospital based prospective descriptive study was carried out at outpatients and inpatients in the Department of pediatrics, SMS medical college Jaipur. Total 100 cases were taken and these neonates were evaluated to know different causes of unconjugated hyperbilirubenemia.
Results: Most common cause of persistent jaundice in both term and preterm babies is breast milk jaundice (66%), other causes include isoimmunization (10%), cephalhematoma (7%), hypothyroidism (7%), sepsis (4%) and ABO incompatibility (3%). Etiology of persistent jaundice was not significantly different in term and preterm babies.
Conclusions: Although breast milk jaundice is considered as a major cause of prolonged unconjugated hyperbilirubinemia in neonates, identification of other etiological factors, such as UTI, congenital hypothyroidism and hemolysis is also of paramount importance. Early diagnosis and treatment of these disorder could effectively prevent further complication in neonates.
Keywords: Breast feeding, Neonates, Sepsis, Unconjugated bilirubin
Department of Pediatric Medicine, Sir Padampat Mother and Child Health Institute, SMS Medical College, Jaipur, Rajasthan, India
Received: 23 February 2017
Accepted: 28 March 2017
*Correspondence:
Dr. Vijay Agrawal,
E-mail: vijayagrawal30111974@gmail.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
epidermal growth factor (EGF) in breast milk.7 Second,
the breast-milk of some women contains a metabolite of progesterone called 3-alpha-20-beta pregnanediol.
This substance inhibits the action of the enzyme uridine diphosphoglucuronic acid (UDPGA) glucuronyl transferase responsible for conjugation and subsequent excretion of bilirubin. In the newborn liver, activity of glucuronyl transferase is only at 0.1-1% of adult levels, so conjugation of bilirubin is already reduced. Further inhibition of bilirubin conjugation leads to increased levels of bilirubin in the blood.8
Third, an enzyme in breast milk called lipoprotein lipase produces increased concentration of nonesterified free fatty acids that inhibit hepatic glucuronyl transferase, which again leads to decreased conjugation and subsequent excretion of bilirubin.9
Prolonged jaundice causes parental anxiety as well as difficulty for the clinician, partly because of the need for extreme and varied investigation.
Prolonged unconjugated jaundice is the most common form of prolonged jaundice. Even though breast milk jaundice, extravasated blood (cephalhematoma, bruises), subclinical hemolysis (G6PD deficience, Rh-incompatibility, ABO Rh-incompatibility, urinary tract infection (UTI), Congenital hypothyroidism, Sub acute intestinal obstruction, Increased enter hepatic circulation (functional intestinal obstruction), Idiopathic, Others (crigglar Najjar syndrome) have been described as common causes of prolonged unconjugated jaundice (PUJ), the relative contribution of various causes is not well documented.10
So, this study was plan to know the different causes of unconjugated jaundice in newborn.
The objective of the study was to etiological factors for prolonged unconjugated Jaundice in the newborns.
METHODS
This Hospital based prospective descriptive study was carried out at outpatients and inpatients in the Department of pediatrics, SMS medical college Jaipur.
Total 100 cases were taken. Nature of the study explained to the Parents and written informed consent was obtained. A detailed history and a thorough clinical examination were done for all the cases.
Following investigations were done according to patient’s clinical profile: Total serum bilirubin and conjugated fraction of bilirubin, complete blood count including PBF, Direct Coombs test, G6PD assay by methmoglobunemia reduction test T4 and TSH by radioimmunoassay, urine examination and culture for urinary tract infection (UTI) CRP and chest X-ray followed by blood culture, USG brain for occult hematoma, therapeutic trial of phenobarbitone in Criggler-Najjar syndrome.
Inclusion criteria
• Neonates presenting with clinical jaundice (Serum bilirubin ≥10 mg/dl) beyond 14 days of life.
Exclusion criteria
• Neonates with conjugated hyperbilirubinemia • Neonates with surgical conditions
RESULTS
Total 100 cases were taken out of them 64 were male, 36 were female.
About one third of both term and preterm babies were male and application of Chi square test showed that the two groups did not differ significantly in relation to their sex composition (p >0.05).
Table 1: Distribution of study subjects according to sex and gestation.
Sex Term baby Preterm baby Total
N % N % N %
Male 56 63.6 8 66.7 64 64
Female 32 36.4 4 33.3 36 36
Total 88 100.0 12 100.0 100 100
Chi-square = 0.013 with 1 degree of freedom; P = 0.908 (NS)
Table 2: Comparison of serum bilirubin in term and preterm babies with jaundice.
Group N Mean Std. deviation
Term 88 14.16 2.03 Preterm 12 13.47 1.88
Total 100 14.08 2.02
t = 1.113 with 98 degrees of freedom; P = 0.268 (NS)
DISCUSSION
Males have a higher incidence as compared to females in our study. Various studies have also shown similar result Table 4 shows that there was a male preponderance in
present study with males accounting for 64 (64%) cases. Comparable results were reported by N. with a male’s predominance. Incidence of prolonged unconjugated jaundice according to sex distribution in different studies.11-14
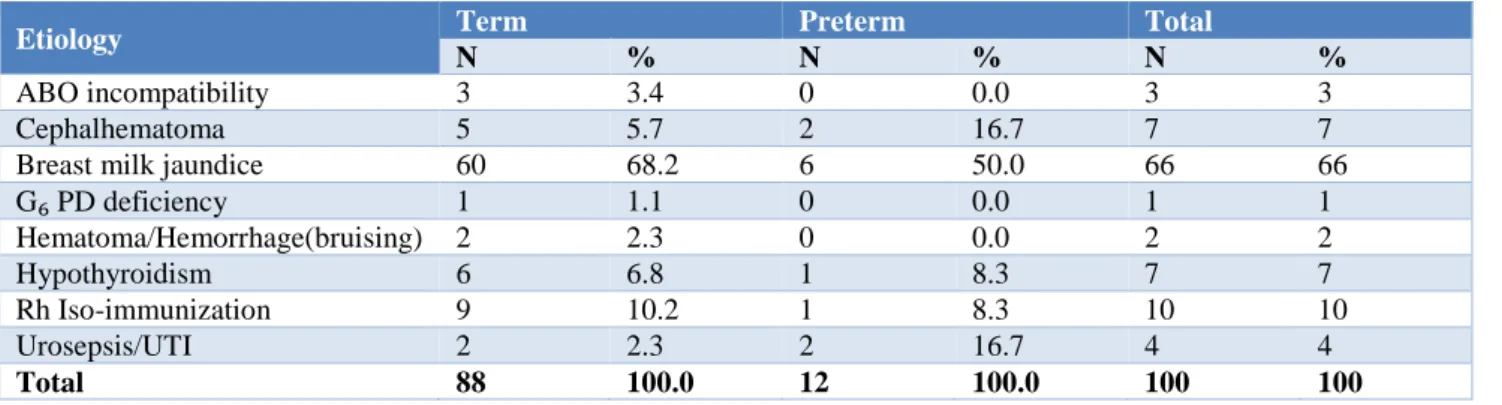
Table 3: Etiology of jaundice in term and preterm babies with jaundice.
Etiology Term Preterm Total
N % N % N %
ABO incompatibility 3 3.4 0 0.0 3 3
Cephalhematoma 5 5.7 2 16.7 7 7
Breast milk jaundice 60 68.2 6 50.0 66 66 G₆ PD deficiency 1 1.1 0 0.0 1 1 Hematoma/Hemorrhage(bruising) 2 2.3 0 0.0 2 2
Hypothyroidism 6 6.8 1 8.3 7 7
Rh Iso-immunization 9 10.2 1 8.3 10 10
Urosepsis/UTI 2 2.3 2 16.7 4 4
Total 88 100.0 12 100.0 100 100
Chi-square = 8.710 with 7 degrees of freedom; P = 0.284 (NS)
Table 4: Prolonged unconjugated jaundice study.
Worker/Country Male Female
Present study SMS
medical college, Jaipur 64 (64%) 36 (36%) N. Najati, M. M.
Gharebaghi et al, Iran 67 (67%) 33 (33%) Margaret Andre et al,
New Zealand 115 (69%) 52(31%) Khadije Sadat Najib et
al, Iran 99 (58.2%) 71 (41.8%)
Najati, M.M. Gharebaghi et al, Iran, Margaret Andre et al, New Zealand, Khadije Sadat Najib et al.11-13 A
probable explanation may be due to social bias, males being more cared for and promptly brought to medical attention.
In present study, mean serum bilirubin level at enrollment was 14.08±2.02 mg/dl, level was almost similar in both term (14.16±2.03) and preterm babies (13.47±1.88). Mohammad Kazem Sabzehei, Behnaz Basiri et al study reported serum bilirubin level in term babies was 17.4±3.6 mg /dl whereas in preterm babies was 17.6±5.0 mg/dl, which was slightly higher than our study.15
Comparable serum bilirubin level was reported in study by Gundur NM, Kumar P et al (mean SBr level at enrollment was 11.6±3.7mg/dl).16
The incidence of etiological causes of prolonged unconjugated jaundice in our study are following:
Breast milk jaundice 66% (66), Rh- isoimmunization 10% (10), hypothyroidism 7% (7), extravasated blood (cephalhematoma) 7%(7), UTI 4% (4), ABO incompatibility 3% (3), G6PD deficiency 1% (1), hemorrhage/bruising 2% (2).
N. Najati, M.M. Gharebaghi et al, Iran results in their study was comparable to our study.11 causes of prolonged
jaundice in their study was as breast milk jaundice 75% (75), G6PD deficiency 7% (7), UTI 7% (7), Hypothyroidism 4% (4), down syndrome 1% (1), ABO incompatibility 1% (1), unknown in 4% (4). In their study, most common cause was breast milk jaundice (75%), incidence of which was higher than present study. Incidence of G6PD deficiency was higher in their study compared to our study, other causes almost similar to our study.
Mohammad Kazem Sabzehei, Behnaz Basiri et al Iran had almost similar result in which etiologies as breast milk jaundice 70% (70), UTI 14% (14), congenital hypothyroidism 6% (6), G6PD deficiency 5% (5), ABO incompatibility 5% (5), incidence of UTI was higher in their study compare to our study.16
Shao-Wen Cheng, Ya-Wen Chiu et al studied 413 neonates with prolonged jaundice in Taiwan, also found similar etiological causes but the frequency of causes is different from our study.17 In their study, the causes as
exclusive breast feeding (38.5%), followed by G6PD deficiency (24.0%), and ABO incompatibility (21.8%),Idiopathic (15.3%), cephalhematoma (4.6%), massive bruising (0.7%), subgaleal hemorrhage (0.5%), adrenal hemorrhage (0.5%), ICH (0.2%), sepsis ( 2%), In their study most common causes of prolonged jaundice was breast feeding jaundice while in our study most common causes is breast milk jaundice. The incidence of G6PD deficience and ABO incompatibility in their study was much higher than our study.
milk jaundice (% 56.3), urinary tract infections (10.4%), blood group (ABO) incompatibility (6.9%), glucose-6-phosphate dehydrogenase deficiency (G6PDD) (5.9%), hypothyroidism (3.7%), Crikler-Najjar syndrome (2.1%), congenital heart disease (1.3%), and other causes (4.4%).
Mahendra Kumar Banakar et al studied 36 healthy term babies with prolonged jaundice during Jan. 2005 to Dec. 2006 in United Kingdom.19 In their study causes were
almost similar but frequency different. The causes as Breast Milk Jaundice 14 (38%), Hemolytic Jaundice 3 (9%), Urinary Tract Infection 1(3%), Physiological Jaundice 1 (3%) and in their study, causes not documented in 17 (47%) babies. In this study breast milk had lower incidence compared to our study.
Merih Çetinkaya, Özkan Hilal et al studied 154 neonates with prolonged jaundice during Jan. 2007 to Dec. 2007 in Istanbul.20 Causes in their study was as breast milk
jaundice (53%). It was followed by urinary tract infections and clinical sepsis (29%), hemolytic causes due to blood group incompetency (10%) and congenital hypothyroidism (8%), in our study incidence of UTI was low in incidence (4%) compare to their study, other causes comparable with our study. Maruo Y, Nishizawa K et al analyzed 17 breastfed Japanese infants with apparent prolonged jaundice 3 weeks to 1 month after their birth.21
Sixteen infants had at least one mutation of the UGT1A1. Seven were homozygous for 211G >A (G71R), which is the most common mutation detected in the East Asian population, and the mutant enzyme had one third of the
normal activity. The results indicate that defects of UGT1A1 are an underlying cause of the prolonged unconjugated hyperbilirubinemia associated with breast milk. One or more components in the milk may trigger the jaundice in infants who have such mutations. Their result comparable with present study in which breast milk jaundice is most common etiology.
Prasad Adavappa Parvathammaet al studied 116 infants with prolonged unconjugated jaundice with normal urine and stool colour, the causes of prolonged unconjugated jaundice in their study were as breast-milk jaundice 83% (97), feeding difficulties 6% (7), UTI 1.7% (2) and hereditary spherocytosis0.8% (1), in their study the incidence of breast milk jaundice was higher than our study.22
Nader Pashapour, Ahmad Ali Nikibahksh et al analysed 100 neonates with prolonged jaundice, all of the neonates were breastfed. Out of them Six (6%) babies suffered from UTI (4 boys and 2 girls), the result is comparable to our study in which UTI is 4%.23
Gundur NM, Kumar P et al analysed 66 neonates with prolonged unconjugated jaundice, in their study causes as G6PD deficiency 16 (24%), ABO incompatibility 5 (8%), Rh incompatibility 2 (3%), UTI 3 (5%), Hypothyroidism in 2.6% of cases.16 The incidence of G6PD deficiency
was high in their study compared to present study in which incidence is 1%.
Table 5: Comparison of etiological factors of prolonged unconjugated jaundice in different studies with present study.
Worker Prematuty ABO
Incomp. Rh Incom.
Breast milk jaundice
Breast feeding jaundice
G6PD Def.
Cephal/ Brusing
Sepsis/ UTI
Hypoth- -roidism
Present study SMS MC (n=100) India
12% 3% 10% 66% - 1% 9% 4% 7%
N. Najati et al, n=100 Iran
- 1% - - 75% 7% - 7% 4%
MK Sabzehei
Iran n=100 31% 5% - 70 - 5% - 14% 6% MK Banakar,
n=36, UK - 9% - 38% - - - 3% -
Shao-wen Cheng et al n=413
- 21.8% - - 38.5% 24% 5% 2% -
Gundur NM et al
n=66 India 48% 8% 3% - - 24% - 5% 2.6% Merih Çetinkaya
et al
n=154 Istanbul
CONCLUSION
According to the result of this study, although breast milk jaundice is considered as a major cause of prolonged unconjugated hyperbilirubinemia in neonates, identification of other etiological factors, such as UTI, congenital hypothyroidism and hemolysis is also of paramount importance. Early diagnosis and treatment of these disorder could effectively prevent further complication in neonates.
Funding: No funding sources Conflict of interest: None declared
Ethical approval: The study was approved by the Institutional Ethics Committee
REFERENCES
1. Mackinlay GA. Jaundice persisting beyond 14 days after birth. BMJ. 1993;306(6890):1426-7.
2. Hannam S, McDonnell M, Rennie JM. Investigation of prolonged neonatal jaundice. Acta Paediatr. 2000; 89(6):694-7.
3. Schneider AP. Breast milk jaundice in the newborn: A real entity. JAMA. 1986;255(23):3270-4.
4. Hargreaves T. Breast-milk jaundice. BMJ. 1970; 3(5723):647.
5. Alonso EM, Whitington PF, Whitington SH, Rivard WA, Given G. Enterohepatic circulation of nonconjugated bilirubin in rats fed with human milk. J Pediatr. 1991;118(3):425-30.
6. Practice parameter: management of hyperbilirubinemia in the healthy term newborn. Pediatr. 1994;944(1):558-62.
7. Kumral A, Ozkan H, Duman N. Breast milk jaundice correlates with high levels of epidermal growth factor. Pediatr Res. 2009;66: 218-21. 8. Arias IM, Gartner LM, Seifter S, Furman M.
Prolonged neonatal unconjugated hyperbilirubinemia associated with breast feeding and a steroid, pregnane-3(alpha), 20(beta)-diol in maternal milk that inhibits glucuronide formation in vitro. J Clin Invest. 1964;43:2037-47.
9. Poland, RL, Schultz GE, Gayatri G. High milk lipase activity associated with breastmilk jaundice. Pediatr Res. 1980;14:1328-31.
10. Agarwal R, Deorari AK. Unconjugated hyperbilirubinemia in newborn. Indian Pediatr. 2002;39:30-42.
11. Najati N, Gharebaghi MM and Mortazavi F. Underlying Etiologies of Prolonged Icterus in Neonates Pak J Biologic Sci. 2010;13(14):711-4. 12. Margaret A, Andrew S. Day causes of prolonged
jaundice in infancy. New Zealand Med J. 2016;129:1429.
13. Najib KS, Saki F. Incidence, Risk Factors and Causes of Severe Neonatal Hyperbilirubinemia in the South of Iran. Iran Red Crescent Med J. 2013;15(3).
14. Mladenović M, Radlović N. Arias icterus-prolonged unconjugated hyperbilirubinemia caused by breast milk. Srp Arh Celok Lek. 2007;135 11-12.
15. Sabzehei MK, Basiri B, Gohari Z. Etiologies of prolonged unconjugated hyperbilirubinemia in neonates Iranian J Neonatol. 2015;6(4):37-42 16. Gundur NM, Kumar P. Natural history and
predictive risk factors of prolonged unconjugated jaundice in the newborn. Pediatr Int. 2010;52(5):769-72.
17. Cheng SW, Ya-Wen Chiu MD, Weng YH. Etiological Analyses of Marked Neonatal Hyperbilirubinemia in A Single Institution in Taiwan; Chang Gung Med J. 2012;35:148-54. 18. Boskabadi H. Goudarzi M. Prevalence and etiology
of prolonged neonatal jaundice. Scientific J Kurdistan Univ Med Sci. 2016;21(1)84-92.
19. Banakar MK and Subbarayan A, A study of prolonged jaundice screen in healthy term babies; Indian J Clini Biochem. 2008;23(3) :286-2891. 20. Merih Çetinkaya, Özkan Hilal. The Distribution of
Etiology in Newborns with Prolonged Jaundice. J Curr Pediatr. 2008;6:99-103.
21. Maruo Y, Nishizawa K. Prolonged unconjugated hyperbilirubinemia associated with breast milk and mutations of the bilirubin uridine diphosphate- glucuronosyl transferase gene. Pediatr. 2000;106(5):59.
22. Parvathamma PA, Brockbank EP, Abourahma Y. Three-year experience with prolonged neonatal jaundice screening in a district general hospital. International J Contemp Pediatr. 2016 Dec 21;4(1):1-4.
23. Pashapour N, Nikibahksh AA. Urinary Tract Infection in Term Neonates with Prolonged Jaundice. Urol J. 2007;4:91-4.