Chronic low back pain: Osteopaths’ attitudes and management
Full text
(2) ABSTRACT Background: Chronic low back pain (CLBP) is one of the chief complaints seen by osteopaths. The management and care that practitioners provide for CLBP patients as well as their attitudes towards them are crucial in the overall wellbeing of the patient. Little is known about osteopaths’ management of CLBP and their attitudes towards such patients. Objective: To determine the non-manual management modalities commonly employed by osteopaths for CLBP, their view of the perceived effectiveness of these and other modalities and their attitudes towards treating CLBP patients. Methods: A random sample of 453 osteopaths in Australia received by mail a. ity. 26 item survey “Osteopath Pain Management and Attitude Survey”.. ct (c or ) ia 20 U 05 ni ve rs. Results: There was a 31.3% (N=142) response rate. Physical exercise and patient education were the most commonly prescribed non-manual management for CLBP and considered the most effective. Osteopaths’ incorporation into management of CLBP, the psychosocial factors appeared to be lacking. Ninety-four percent deemed physical therapy beneficial for CLBP.. patients”.. Vi. Eighty-four percent disagreed “there is nothing physically wrong with CLBP. Conclusion: Management of CLBP by osteopaths does not appropriately consider psychosocial aspects of pain. Osteopaths in this study did not believe that they had “negative feelings” towards their CLBP patients. There is insufficient evidence to conclude negative attitudes towards CLBP patients. However there is some indication a small number of osteopaths may have potentially undesirable attitudes towards CLBP patients. Keywords: low back pain, chronic pain, Osteopathic Medicine, Health knowledge, attitudes, practice 2.
(3) INTRODUCTION Chronic low back pain (CLBP) has been defined as low back pain that continues for more than three months.1-2 In 1991, Wolff et al.3 described chronic low back pain as a condition where pathology may not be identifiable. CLBP is often a transition from an acute injury, with 5-10% of back pain patients developing long term problems.4 CLBP is often associated with pain that is disproportionate to physical findings, progressive inactivity, failed treatments, distress and negative beliefs from the patient.1 CLBP which is of non-cancer origin, is “not just a physical disease but an illness combining the physical. ity. disorder with a multitude of somatic and psychosocial factors” 5. Chronic pain. ct (c or ) ia 20 U 05 ni ve rs. may be associated with anxiety, depression, helplessness and hopelessness, which can serve as a vicious cycle exacerbating the patient’s pain.6-8. Chronic low back pain is reported to have a substantial impact on the well being of an individual as well as being a source of major concern in today’s society. In the US it has been found that health care costs and the cost of managing. Vi. chronic low back pain are staggeringly high, typically associated with many failed treatments, loss of productive workdays (absenteeism) and disability.5,8 In 1998, Linton9 stated that absenteeism due to back pain costs the Netherlands an average of $1.5 million an hour. Accurate diagnosis and effectual treatment of chronic low back pain is a growing dilemma for primary health care practitioners, as a lack of a ‘pathological’ diagnosis and continued ineffectual treatments can potentially lead to poor attitudes towards patients suffering chronic low back pain and furthermore inadequate treatment and management of the problem by practitioners.8. 3.
(4) Health care practitioners such as physicians and physical therapists often handle chronic low back pain patients poorly.3,10-11 Many studies3,10-13 have concluded that a lack of knowledge and formal education of health care practitioners in the processes of pain management, particularly chronic pain, has led to negative professional attitudes towards the treatment of chronic pain patients, resulting in mediocre treatment and management programs and undue suffering of such patients. A possibility for better management of chronic pain could be greater education of health professionals.. ity. It has been found that many practitioners have a negative attitude towards. ct (c or ) ia 20 U 05 ni ve rs. treating and managing people with chronic conditions such as CLBP. 3,10-14 The negative attitudes often arise because of the inability to relieve pain and help the patient cope, thus leading to feelings of frustration and professional inadequacy.. It is important to note that studies and government publications15-17 in varying. Vi. countries indicate that manual therapy is effective in acute low back pain, however less so in chronic. Bogduk15 suggested that physiotherapy (manual therapy) either does not work or has limited efficacy in the treatment of CLBP.. There are currently many manual and non-manual modalities and strategies available to manage pain and pain related symptoms. Many studies6,8,18-21 have examined different non-manual techniques to help a patient suffering chronic pain and CLBP as it is thought these techniques will benefit the patient in the long term.. 4.
(5) Studies have suggested that physical exercise is important for building strength and flexibility as well as giving the sufferer a feeling of control over their physical functioning. 6,18 Exercise and reconditioning programs, which focus on functional restoration, may provide the most valuable therapy for a majority of CLBP patients. 8. Simple patient education in regards to their condition has been found to have a positive effect on coping with chronic pain.12,21-25 Patients who understand that their pain may not be cured learn to focus on managing their pain and. ct (c or ) ia 20 U 05 ni ve rs. ity. developing coping skills for everyday life. Coping skills are important in helping the patient come to terms with having a chronic condition and address some psychosocial factors. CLBP patients have a high incidence of anxiety and depression, which often results in them focusing purely on their pain and their body making them more sensitive to pain and heightened intensity.18 The problem lies in the assessment and. Vi. identification of psychosocial factors and determination of which factors are remediable, such that the patient experiences reduced pain and improved function.26 There are many types of coping strategies, such as relaxation, visualisation, meditation etc, and they do not all have the same effect on everyone. It would be difficult to ascertain which one coping strategy would be proven to be consistently beneficial or not, therefore it is important that practitioners tailor a management program appropriate to the individual patient and have knowledge of a variety of modalities that they can employ in doing so.26. 5.
(6) Mind body therapies, such as relaxation, visualisation, auditory distraction, imagery, hypnosis and meditation, although considered controversial and ‘alternative’ are behavioural, psychologic, social and spiritual approaches to medicine.20 Previously conducted studies 6,18,20,23,27 support the use of relaxation and auditory distraction as methods of coping with and reducing pain, particularly chronic pain.. Although mind body therapies are possibly gaining in credibility and acceptance. ity. they are not practiced nor incorporated as part of standard medical care and. ct (c or ) ia 20 U 05 ni ve rs. training today. Multi-component approaches including combinations of stress management, coping skills training, cognitive reconstructing and relaxation therapy may form an appropriate complementary therapy approach in the overall treatment and management of chronic low back pain.20,26. It is believed that the management of chronic pain is influenced by the health. Vi. care practitioner and their knowledge of the effectiveness of different management modalities.3,10,11,28. It has been well documented that patients suffering from chronic conditions often suffer from depression, anxiety, hopelessness and distress as they grapple to accept living with a chronic condition.1,2,4-8 Treatment of chronic pain patients is not successful if there is no attention paid to the treatment of psychosocial issues.3 In 2005, Lucas26 stated that the variance in pain. 6.
(7) attributable to psychosocial issues is between 15 and 30%, so in addressing these factors it could be hoped to vary the pain by up to 30%.. It is thought that practitioners as well as patients undervalue or completely ignore the relationship between the cognitive and emotional with the physical facets of pain.13 Physiotherapist treatments have been found to be biomechanically orientated even when psychological factors were apparent in the patient’s presentation.14 In the situation when, a patient’s psychological factors and pain remain unchanged referral for psychological intervention should be. ct (c or ) ia 20 U 05 ni ve rs. ity. considered by the treating professional.. Psychosocial issues should be more formally assessed for the wholistic management of an existing condition in order to meet the physical and emotional needs of the patient.26 The identification and treatment of underlying and developed psychosocial factors, such as depression and anxiety, in patients with CLBP is an important part of the management process.6-8,29. Vi. However it is important to consider the possibility that patients with CLBP do not necessarily have psychosocial factors attributing to their condition. 19 Management with more emphasis on psychosocial aspects of CLBP may in fact be more cost effective in that long-term suffering, health care utilization and absenteeism could be reduced.9. Owing to the high costs of CLBP to society and the undue suffering of CLBP patients it is therefore imperative that the management of chronic pain patients be examined to identify the barriers and gaps in the appropriate management. 7.
(8) of such problems. Past research has examined physician and physical therapists’ management of chronic pain, their attitudes towards treatment and management of chronic pain patients and the effectiveness of management approaches.3, 10-12,28 Despite the research focus of management of CLBP, the numbers of people suffering CLBP do not reflect adequate management of such a condition. This raises questions about how the practitioners are actually managing CLBP patients and whether they are taking into accounts all of the factors involved in the successful management of CLBP.. ity. There is, however, little or no research into the treatment and management of. ct (c or ) ia 20 U 05 ni ve rs. CLBP by osteopaths, which is surprising considering that CLBP is often treated by osteopaths. It is therefore important to determine how osteopaths are managing CLBP, and in particular to understanding their knowledge and use of varying pain non-manual management modalities and what their attitudes are towards such patients. Osteopaths in Australia currently undergo 5 years of training covering many disciplines and thus should have a sound knowledge of. Vi. pain mechanisms and non-manual management of chronic pain. While it is expected that manual techniques will form part of the initial approach by osteopaths to CLBP patients, it is important to determine what additional approaches could be used by osteopaths to help a CLBP patient.. 8.
(9) The aims of this study were to examine the management of chronic low back pain by practising osteopaths and their attitudes towards CLBP patients. In particular the aims were; 1) To measure the non-manual management modalities commonly employed by osteopaths for CLBP, whether they use modalities suggested by the literature. 2) To measure osteopaths’ perceptions of the effectiveness of the nonmanual management modalities for CLBP as suggested by the literature.. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. 3) To determine osteopaths attitudes towards people with CLBP.. 9.
(10) METHODOLOGY Participants The “Osteopath Pain Management and Attitude Survey” (Appendix 2) was sent to 453 practising osteopaths throughout Australia. Potential participants were selected randomly from public domain documents, and were mailed a general demographic information questionnaire that included the participant’s age, gender, years of experience and education details, as well as the “Osteopath Pain Management and Attitude Survey”. This study was approved by the Victoria University Faculty of Human Development Human Research Ethics. ity. Committee. The survey was voluntary and anonymous, as participants were not. ct (c or ) ia 20 U 05 ni ve rs. required to disclose their name or location of practice, and participants consented to taking part in this study by completing and returning the questionnaire.. Procedure. A three-page survey was developed to provide a quantitative analysis of CLBP. Vi. management by osteopaths in Australia (Appendix 2). The survey instrument for this study was one patterned after previously employed surveys and questions used to study physicians and physical therapists. 3,10-12,24 Items selected from the previous surveys were chosen based on their relation to the aims of this study and their appropriateness for use in the osteopathic profession. The survey contained questions regarding practitioner characteristics, opinions concerning patients with CLBP and osteopathic non-manual management modalities. The multi-item survey was designed to investigate the osteopaths. 10.
(11) use and perceptions of effectiveness of pain management modalities, satisfaction and confidence in management as well as attitudes and beliefs regarding CLBP patients. The survey was administered to a pilot group of 6 practising osteopaths. Items in the survey were refined based on feedback from the pilot sample. The final “Osteopath Pain Management and Attitude Survey” contained 26 items (Appendix 2). Items included in the survey asked the osteopaths; 1. Item 25 - Non-manual management modalities they utilise or teach their. ct (c or ) ia 20 U 05 ni ve rs. to 5 (always) on a five point Likert scale.. ity. CLBP patients with responses for each question ranging from 1 (never). 2. Item 26 - The specific effectiveness of individual non-manual management approaches. The osteopaths were requested to respond to each non-manual management modality by marking their response on a five-point Likert scale ranging from 1 (not effective) to 5 (very effective). 3. Item 14 to 24 - A series of statements regarding the osteopath’s beliefs. Vi. and attitudes concerning patients with CLBP. Participants were provided with a five point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) to respond to these items. 4. Items 9 to11 – About their level of confidence in regards to their management of CLBP versus acute low back pain (ALBP) patients, the responses also on a five point Likert scale ranging from 1 (not confident) to 5 (extremely confident). 11.
(12) 5. Item 13 - Their level of satisfaction with the management and care they provide CLBP patients on a five-point Likert scale ranging from 1 (very dissatisfied) to 5 (very satisfied).. Statistical Analysis Descriptive statistics were used to determine osteopaths attitudes towards CLBP patients and how they are managing CLBP patients. An Exploratory Factor Analysis with Oblimin rotation was performed on the “Osteopaths Beliefs” section (questions 14-24 of the survey). Extraction method Maximum. ity. Liklihood was performed due to assumption of correlations between items. All. ct (c or ) ia 20 U 05 ni ve rs. statistical analyses were performed using Microsoft Excel (2000) and SPSS for. Vi. Windows (Version 11.0) with α level set at 0.05.. 12.
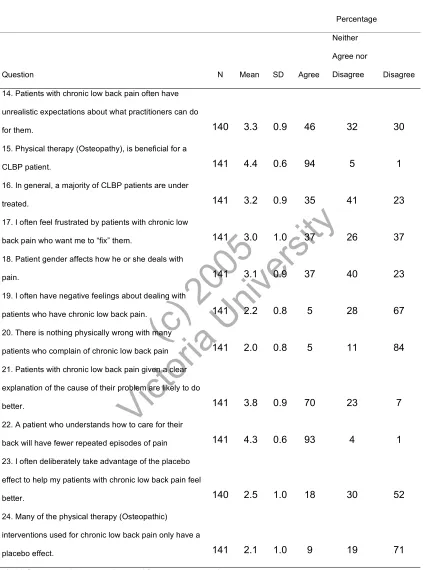
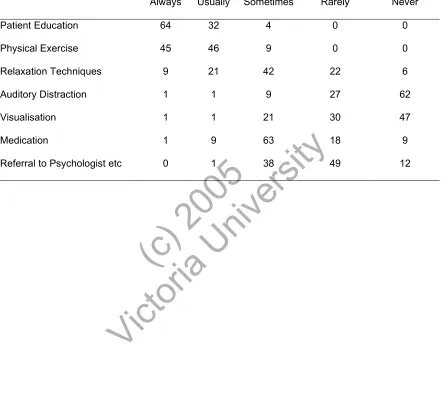
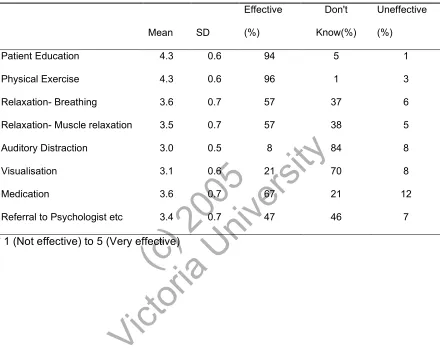
(13) RESULTS From the 453 surveys mailed, 143 surveys were returned. A total of 142 survey responses were entered into the database for analysis with 1 survey being returned unanswered. The overall response rate was 31.3%. Osteopaths management of CLBP (Items 25 + 26) Table 1 and figure 4 shows the percentage of osteopaths utilising the various different types of non-manual management modalities. The majority of osteopaths (64%) “always” use patient education as part of their management of CLBP patients. Physical exercise was the second most common. ity. management modality osteopaths “always” used (45%). For both patient. ct (c or ) ia 20 U 05 ni ve rs. education and physical exercise the least amount of utilisation indicated by osteopaths was “sometimes”. Relaxation techniques produced a wide spread of utilisation, depending on the individual osteopath. However 94% of osteopaths used relaxation techniques when managing CLBP patients, ranging from always to rarely. Only 6% of osteopaths did not use relaxation techniques as a. Vi. way to help chronic low back patients cope.. Auditory distraction was the management modality least used by osteopaths, 62% indicated they never employed auditory distraction as part of the management of CLBP patients. Visualisation was the second least employed modality with 47% indicating they never use it. Medication usage also produced a wide spread of results with osteopaths responses ranging from always to never. However the majority (63%) revealed they “sometimes” utilise this as management of CLBP, although the type of. 13.
(14) medication osteopaths recommend their patients was not indicated by the sample. Table 2 demonstrates each management modality and the corresponding responses by the osteopaths, regarding their perceived effectiveness of that modality. The combined weighted sample estimated that patient education (mean 4.3± SD 0.6) and physical exercise (mean 4.3± SD 0.6) were perceived to be effective when managing CLBP patients, with 94% and 96% respectively of osteopaths revealing they perceived these modalities as effective. Over 50% of the combined weighted sample indicated they perceived both breathing and. ct (c or ) ia 20 U 05 ni ve rs. ity. muscle relaxation (of relaxation techniques) to be equally effective.. Medication usage (mean 3.6± SD 0.7) produced the most varied of responses by osteopaths. Over 67% of the combined sample perceived that medication usage is effective, 21% responded “Don’t Know” and the largest number of osteopaths (12%) out of all modalities indicated that medication usage is either. Vi. “less than effective” or “not effective”. Osteopaths indicated that they “don’t know” the effectiveness of auditory distraction (84%) and visualisation (70%). The perceived effectiveness of referral to a psychologist was mostly split between “effective” (47%) and “don’t know” (46%). Osteopath’s belief (Items 14-24) An Exploratory Factor Analysis was performed, alpha measure of 0.05, on this section of the survey (Q14-24), to determine if these items were reliable and whether items were tapping into the same concept. Correlation coefficients of 0.3 and greater were found suggesting that some of the statements were. 14.
(15) useable. The Bartlett test of sphericity for the correlation matrix was 234.840 with a significance level of 0.000 suggesting adequate correlations amongst the statements. The Kaiser-Meyer-Olkin (KMO) measure of sampling was 0.695 indicating that there was most likely a factor structure underlying the data. Insufficient correlations between question 18 and the other questions meant it was excluded from the exploratory factor analysis.. Table 3 shows the total variance explained by each factor. The variance of the first factor is 2.717 out of the total variance of 10. This means that the first. ity. factor explains 27.167% of the total variance. The variance of the second factor. ct (c or ) ia 20 U 05 ni ve rs. is 1.484 or 14.84% of the total variance; the variance of the third factor is 1.249 or 12.494% of the total variance; the variance of the fourth factor is 1.136 or 11.357% of the total variance etc. The first 4 factors already account for about 66% of the total variance and given that each of the subsequent factors have a variance of less than one (ie. smaller than the variables themselves) we choose to use just four factors to adequately describe the 10 statements. The ten items. Vi. of the osteopath belief section represent four factors, three strong factors (attitudes, understanding and treatment) and one factor that stands on its own (placebo usage).. Question 23 had its highest factor loading on factor one (Table 4). Q23 stands alone in this factor and was written to measure the use of the placebo effect, therefore it is the “placebo usage” factor. The pattern matrix (Table 5) shows no cross loading of this question on other factors suggesting it is a relatively “pure” measure of “placebo usage”. The structure matrix (Table 6) shows a high. 15.
(16) correlation (0.995) between Q23 and the factor therefore is a good measure of the factor, however there are no other questions as a measure of this factor thus the factor stands alone.. Questions 17, 19, 20 and 14 all have the highest factor loading on factor 2. These statements were written to measure osteopath attitudes and feelings towards patients, thus the “attitudes” factor. The cross loadings on other factors are low (only Q20 has a cross loading (0.229)) indicating that these measures are relatively pure measures of “attitudes”(Table 5). Furthermore correlations. ct (c or ) ia 20 U 05 ni ve rs. good measures of the factor (Table 6).. ity. between Q17, Q19, Q20 and Q14 and the factor are high suggesting they are. Questions 22 and 21 have the highest factor loading on factor 3. These statements were written to measure levels of patient understanding, thus the “understanding” factor. No cross loading is present and the correlations between the statements (Table 5 + 6) and the factor are high therefore these. Vi. questions are “pure” and a good measure of the factor.. Questions 15, 16 and 24 all have the highest factor loading on factor 4. Question 20 has a higher factor loading on the “attitudes” factor. These statements were written to measure belief about osteopathic treatment, in other words the “treatment” factor. Questions 15 and 16 are written in a positive manner in regards to treatment, whereas Q24 is written in a negative manner in regard to treatment. With the exception of Q20, the level of cross loading is low with high correlations (Table 6) between the factor and Q16, Q15 and Q24. 16.
(17) suggesting that these statements are a good measure of “treatment”. In summary, the exploratory factor analysis supported the basic grouping of the statements, in the “belief” section questions 14-24, regarding osteopaths’ beliefs’ of varying themes concerning CLBP patients.. Table 7 demonstrates the statements (items 14-24) and the corresponding responses by the osteopaths. The majority of osteopaths (46%) agreed that CLBP patients have unrealistic expectations about what osteopaths can do for them. The osteopaths were divided in their belief of the statement “I often feel. ity. frustrated by patients with CLBP who want me to “fix” them” 37% agreed, 37%. ct (c or ) ia 20 U 05 ni ve rs. disagreed and 26% neither agreed nor disagreed. In contrast the osteopaths had a strong belief in the statement “I often have negative feelings about dealing with patients who have chronic low back pain”. 67% either disagreed or strongly disagreed (mean 2.2± 0.8 SD) with this statement with only 5% agreeing. This pattern was also seen in response to the statement “There is nothing physically wrong with many patients who complain of chronic low back. SD).. Vi. pain”. 84% of osteopaths either disagreed or strongly disagreed (mean 2.0± 0.8. The most strongly supported statement was; ”Physical therapy (Osteopathy), is beneficial for a CLBP patient” a substantial 94% of osteopaths either agreed or strongly agreed with this statement (mean 4.4± 0.6 SD). The interpretation of this statement, however, leaves some questions. The way that the statement was worded did not clarify whether the term “Physical Therapy (Osteopathy)” referred only to the use of hands-on techniques, or whether it encompassed the. 17.
(18) broad spectrum of osteopathic management approaches including the nonmanual ones. Osteopaths also strongly supported the statement; “A patient who understands how to care for their back will have fewer repeated episodes of pain” with 93% of them agreeing.. Only 18% of osteopaths admitted to consciously using the placebo effect, while the majority (52%) disagreed with using the placebo effect. A large 71% of the combined weighted sample either disagreed or strongly disagreed that “many of the physical therapy (osteopathic) interventions used for CLBP only have a. ct (c or ) ia 20 U 05 ni ve rs. a placebo effect if you are a useless osteopath”.. ity. placebo effect”. One osteopath commented “the interventions would only have. Practitioner confidence (Items 9-11). Upon entering practice 50% (mean 2.7± 0.9 SD) of osteopaths felt only moderately confident of managing CLBP, while at the time of survey the combined weighted sample estimated that 73% (mean 3.9±0.7) of osteopaths. Vi. felt either very or extremely confident of managing CLBP (Table 8). Slightly fewer osteopaths - 42% and 31% (mean 2.6± 0.9 SD) felt moderately confident or a little confident respectively, of managing ALBP upon entering practice. At the time of survey the combined weighted sample estimated that 88% (mean 4.2± 0.7 SD) felt either very or extremely confident of managing ALBP, slightly higher that that for CLBP. Figure 2 demonstrates the mean changing levels of confidence of the management of chronic and acute low back pain.. 18.
(19) Practitioner characteristics The average age of the respondents was 38 years (± 11 years), ranging from 23-69 years. There was an equal distribution of male (n=71) and female (n=71) respondents (Table 9). The mean number of years in practice was 12 (± 7 years) with a range of 0-37 years. (Table 9).. Solo osteopathic practice was the most common with n=65 respondents working in this type of setting. Group multi discipline settings were the second most common with n=59 respondents practising in this way (Table 10). Some. ity. osteopaths worked in more than one employment category.. ct (c or ) ia 20 U 05 ni ve rs. Of the 142 respondents 83 (60%) had undertaken further pain management education following graduation from osteopathic university/college (Table 9). 52% indicated that the level of chronic pain management education was only “briefly covered” in university/college (Table 11). The majority of osteopaths (53%) deemed this amount of chronic pain management adequate for entering practice (Table 12), yet graduate level education was perceived as the least. (Figure 3).. Vi. useful source of pain management information compared to the other sources. Most osteopaths considered a combination of different sources useful for professional education regarding pain management. However both “continuing education” and “reading current literature” were the most common types of useful professional education with 119 and 113 respondents respectively choosing these sources (Figure 3). Some osteopaths regarded other additional sources, which weren’t included in the survey, as useful. The following are. 19.
(20) sources in which some osteopaths thought useful in addition to the ones listed in the survey, including; “experience in practice” and “patient feedback and responses”, the internet, outcome measures, information from supplement manufacturers and reading wholistic health, osteopathy, self awareness and philosophical books. Forty-eight percent of the osteopaths estimated that 26-50% of their patients suffer from CLBP in comparison to 56% of osteopaths estimating that only 0-. Practitioner satisfaction (Item 13). ity. 25% of their patients suffer from acute low back pain (Table 13).. ct (c or ) ia 20 U 05 ni ve rs. The majority of osteopaths were satisfied (66%) or very satisfied (20%) with the management and care they give their CLBP patients, with consistent scores of 4 or more (mean 4.05± 0.6) (Table 14). Of the combined weighted sample only. Vi. 1% felt either dissatisfied or extremely dissatisfied.. 20.
(21) DISCUSSION It could be reasoned that CLBP is one of the most common conditions seen by many osteopaths in practice. However there has been limited consideration given to understanding the ways in which osteopaths are managing CLBP and their attitudinal barriers to optimal pain management. Even though there is evidence that poor practitioner knowledge of management and attitudes plays a role in the inadequate management and treatment of pain by physicians and physical therapists it is not known if this is the case for osteopaths. 3,10-12 This study has presented new information about osteopaths’ pain education,. ity. attitudes towards CLBP patients and perceived effectiveness of non-manual. ct (c or ) ia 20 U 05 ni ve rs. management modalities in an endeavour to gain insight into possible barriers to effective CLBP management by osteopaths.. It has been previously estimated that low back pain contributes between one third and one half of patients treated by physical therapists.11-12 The results of this study’s survey substantiate this estimate with the majority of osteopaths. Vi. indicating that CLBP accounts for 26-50% of all their patients. The higher percentage of patients with CLBP compared to ALBP in this study supports the belief that a substantial amount of health care resources are directed at CLBP.11 Key Findings Many studies have examined different techniques to help people with chronic pain and CLBP and from such studies there have been a wide range of nonmanual modalities proposed as being effective in the successful management of CLBP patients.6,8,12,18,20-26 Management modalities suggested in previous. 21.
(22) studies are not only directed at treatment of the physical symptoms but also at the management and development of coping strategies for chronic pain where a physical/biomechanical cause is not identifiable.. In the earlier study by Crites Battié et al.12 physical therapists were asked about their preferences on treatment modalities for CLBP, but they were mostly of a biomedical approach. They were found to most commonly prefer education and exercise in the treatment of CLBP. This present study, however, also included psychosocially focussed management approaches (relaxation, visualisation,. ity. auditory distraction and referral to a psychologist) as well as biomedical. ct (c or ) ia 20 U 05 ni ve rs. directed modalities (patient education, physical exercise and medication usage) corresponding to the present literature concerning management of chronic pain.. Even with the psychosocially focussed modalities included in this study the respondents agreed with those in the Crites Battié et al. 12 study with the majority of osteopaths most commonly using patient education and physical. Vi. exercise as the chief non-manual management modalities for CLBP. Astin20 suggested that, although mind body therapies are possibly gaining in credibility and acceptance they are not often practised or incorporated as part of standard medical care and training today. The result of this study is consistent with Astin20, as the osteopaths used mind body therapies far less then the other biomedically directed non-manual management modalities.. Despite the osteopaths’ confidence, it is possible they are in fact not always appropriately managing CLBP patients particularly those with psychosocial. 22.
(23) aspects to their pain. It is however beyond the scope of this study to determine whether osteopaths are not using the other techniques because they do not have any knowledge of these techniques or have inadequate knowledge of both the cognitive and physiologic mechanisms of pain, or whether they are aware of them but simply choose not to use them. It is encouraging to see that only 6% of osteopaths never used relaxation. However those that used relaxation did not employ it as often as education or exercise. The majority of osteopaths admitted to never using the other psychosocial directed. ity. management modalities auditory distraction and visualisation.. ct (c or ) ia 20 U 05 ni ve rs. Unfortunately, 12% of the respondents admitted they never referred to psychologists, which may suggest that they never identify depression, pathological anxiety or other psychological conditions that may accompany chronic pain. If osteopaths do not have the capacity to diagnose psychological conditions then they will never refer for appropriate treatment. On the other hand the majority of osteopaths indicated they can recognise when a chronic. Vi. pain patient requires further help for coping with and managing their condition, and are prepared to work with other professions for the benefit of their patients.. In respect of the osteopaths’ perception of the effectiveness of the specific nonmanual management modalities the majority perceived that physical exercise, patient education as well as breathing and muscle relaxation were effective non-manual management modalities for CLBP patients. The majority of respondents indicated that medication was an effective management modality, yet on the other hand medication usage also received. 23.
(24) the largest response for being ineffective of all the modalities in the management of CLBP. This suggests that medication usage for CLBP is controversial in the osteopathic profession. However it would be worth noting that this study did not specify what type of medication was to be used and thus all medications were assumed to be in the one category including analgesics, anti-depressants, herbal remedies and supplements. In future studies, specification of the types of medication may help resolve such controversy.. It is also important to consider that perhaps the osteopaths in this study thought. ity. that their all-round management, including “hands-on” management, was. ct (c or ) ia 20 U 05 ni ve rs. effective. This study’s intention was to investigate the non-manual management protocols for CLBP and the perceived effectiveness of those modalities listed. However, it was recognised at the time of data analysis that the wording of the questions may have left open the possibility of manual approaches also being included. If the osteopaths did indeed think manual treatment was effective as a way of managing CLBP it would require further investigation to determine if this. Vi. is in fact the case.. It has been found that many practitioners in past studies have a negative attitude towards treating and managing chronic conditions such as CLBP.3,10-14 In this study, despite the level of osteopaths’ confidence in their ability to manage CLBP, the majority of them agreed that CLBP patients have unrealistic expectations about what osteopaths can do for them, which is comparable to previous studies.12,24 Osteopaths in this study acknowledge the physical side of CLBP in that they believe CLBP patients have a physical condition and that osteopathy is beneficial for these patients. While 75% of respondents in the. 24.
(25) Wolff et al.3 study felt physical therapy is not beneficial for patients with chronic pain, a very convincing 94% of osteopaths in this study felt that physical therapy is in fact beneficial to such patients. However, this figure may have been skewed by the wording of the question, which did not differentiate between “hands-on” and non-manual management. Osteopaths also believe that educating CLBP patients about their condition together with manual therapy will help patients with their complaint. This belief was subsequently demonstrated with osteopaths’ choice of non-manual management modalities for CLBP patients, such as patient education, supporting the study by Crites. ct (c or ) ia 20 U 05 ni ve rs. ity. Battié et al.12. The majority of osteopaths in this study did not have “negative feelings” towards their CLBP patients. However some osteopaths did acknowledge that CLBP patients have “unrealistic expectations” about what osteopaths can do for them and that a considerable number of osteopaths feel frustrated by this attitude. Frustration has the potential to lead to mediocre treatment and. Vi. management programs for CLBP patients as suggested by the literature 3,10-14 In contrast to those studies 3,10-14 that conclude practitioners (not including osteopaths) have negative attitudes towards CLBP patients, this study found that there is insufficient evidence to reach such conclusions about the osteopathic profession.. Other Findings The results of this study contrast with previous conclusions, based on study of physicians and physical therapists, that pain management education is. 25.
(26) generally inadequate.3,10 Wolff et al. 3 and Green et al. 10 found that between 1/3 - 2/3 of practitioners deemed entry level pain education as less than adequate, compared to over half of the osteopaths in this study indicating their pain management education was adequate. Despite this however, over half of respondents described chronic pain management teaching as having been only briefly covered and indicated that they considered graduate level education as the least useful source of pain management information. It is possible that osteopaths believed they have gained adequate pain management education via its inclusion in a variety of subjects throughout all years of osteopathic. ity. education. Conversely some respondents may have considered their pain. ct (c or ) ia 20 U 05 ni ve rs. education as having been briefly covered due to the fact there is not a sole subject at university dedicated to pain management. However perhaps consideration should be paid to the type and quality of the pain education and whether it is addressing cognitive aspects of pain as well as the physiological aspects.. As for the sources of pain management information thought to be useful by. Vi. osteopaths, similarly to Wolff et al.3, they regarded continuing education as the most useful source, along with reading current literature and liaison with professional colleagues.. As with an earlier study by Crites Battié et al.12 who concluded fewer therapists were confident of affecting CLBP than ALBP, at the time of survey, nearly three quarters of osteopaths in this study felt very or extremely confident of managing CLBP compared to 88% feeling the same for ALBP. It is interesting though to see that although they felt less confident in managing CLBP now, upon entering. 26.
(27) practice the respondents felt slightly more confident in managing CLBP than ALBP. This finding may indicate a significant amount of on the job learning in regards to the management of ALBP, or it may suggest that with experience, practitioners found that CLBP was harder to mange than they had envisaged when entering practice.. Compared to a study by Green et al.10 who found that physicians were less satisfied with their care given to chronic pain as it produced the lowest score out of all types of pain, the respondents of this study were slightly more. ity. satisfied with the management and care they give CLBP patients. It is important. ct (c or ) ia 20 U 05 ni ve rs. to note that we did not ask the participants their satisfaction with management and care of other types of pain thus it is difficult to determine where their satisfaction lies in relation to other types of pain, particularly acute low back pain.. Vi. Limitations. The rate of return 31.3% is relatively low. With this return rate it limits the ability to generalise the results to the osteopathic profession in Australia. It is possible that the osteopaths who responded to the survey may not be fully representative of all osteopaths and constitute a positively or negatively biased sample. Due to the controversial topic and the potential fear of judgement professionally, it is likely that some participants may have under reported their attitudes towards CLBP patients and further not have truthfully answered some questions about their management of such patients. 27.
(28) CONCLUSION The study findings provide osteopaths with information about which management approaches others in the osteopathic field employ and value in the management of CLBP patients. Commonly used management approaches by osteopaths are identified as patient education and physical exercise and the non-manual management modalities identified as being less used were relaxation, visualisation and auditory distraction which are gaining more acceptance as appropriate management approaches for CLBP according to current literature. This study’s conclusion that management of CLBP patients is. ity. not appropriately considering psychosocial aspects of pain supports the current. ct (c or ) ia 20 U 05 ni ve rs. literature.. Osteopaths in this study did not believe that they had “negative feelings” towards their CLBP patients. The difficulty in testing attitudes makes it hard to give an accurate conclusion on the nature of the osteopaths attitudes towards CLBP patients, thus it is the belief of the researchers that there is insufficient. Vi. evidence to support claims that practitioners have negative attitudes towards CLBP patients. However there is some indication a small number of osteopaths may have potentially undesirable attitudes towards CLBP patients.. Further research is necessary to qualify the use of management modalities by osteopaths in the management of CLBP. Additionally, the potential role of attitudes of osteopaths towards CLBP patients and hence adequate management could be the focus for future study.. 28.
(29) REFERENCES 1. Waddell G. The back pain revolution. Edinburgh: Churchill Livingstone;1998. 2. Turk DC, Okifuji A, Sherman JJ. Physiologic aspects of back pain: Implications for physical therapists. In Twomey LT, Taylor JR, editors. Physical therapy of the low back. 3rd ed. Philadelphia: Churchill Livingstone;2000. 3. Wolff MS, Hoskins Michel T, Krebs DE, Watts NT. Chronic painAssessment of orthopedic physical therapists’ knowledge and attitudes.. ity. Physical Therapy 1991;71:207-14.. ct (c or ) ia 20 U 05 ni ve rs. 4. Linton SJ. Cognitive-behavioral approach to the prevention of chronic back pain. In Turk DC, Gatchel RJ, editors. Psychological approaches to pain management: A practitioners handbook. 2nd ed. New York: The Guilford Press; 2002, p.317-32. 5. Werneke MW, Harris DE, Lichter RL. Clinical effectiveness of the behavioural signs for screening chronic low back pain patients in a work-. Vi. oriented physical rehabilitation program. Spine 1993;18:2412-18. 6. Turk DC, Gatchel RJ. Editors. Psychological approaches to pain management: A practitioners handbook. 2nd ed. New York:The Guilford Press; 2002. 7. Polatin PB, Kinney RK, Gatchel RJ, Lillo E, Mayer TG. Psychiatric illness and chronic low-back pain. The mind and the spine-which goes first?. Spine 1992;18:66-71 8. Rauck RL. Chronic low back pain. In Rawal N. ed Management of acute and chronic pain, London: BMJ Books;1998, p.139-171. 29.
(30) 9. Linton SJ. The socio-economic impact of chronic back pain: is anyone benefiting? Pain 1998;75:163-8 10. Green CR, Wheeler JRC, Marchant B, LaPorte F, Guerrero E. Analysis of the physician variable in pain management. Pain Medicine 2001;2:317-27 11. Green CR, Wheeler JRC, Marchant B, LaPorte F, Guerrero E. How well is chronic pain managed? Who does it well? Pain Medicine 2002;3:56-65 12. Crites Battié M, Cherkin DC, Roxanne D, Clol MA, Wheeler KJ. Managing low back pain: Attitudes and treatment preferences of physical. ity. therapists. Physical Therapy 1994;74:219-26. ct (c or ) ia 20 U 05 ni ve rs. 13. Wittink H, Hoskins Michel T. Chronic pain management for physical therapists. 2nd ed. USA: Butterworth Heinemann;2002 14. Daykin A, Richardson B. Physiotherapists’ Pain Beliefs and Their Influence on the Management of Patients With Chronic Low Back Pain. Spine 2004;29:783-95. 15. Bogduk N. Management of chronic low back pain. Medical Journal of. Vi. Australia 2004;180:79-83. 16. Rasmussen-Barr E, Nilsson-Wikmar L, Arvidsson I. Manual Therapy 2003;8:233-41 17. Australian Acute Musculoskeletal Pain Guidelines Group. Acute Low Back Pain. In: Australian Acute Musculoskeletal Pain Guidelines Group Evidence-Based Management of Acute Musculoskeletal Pain. Bowen Hills: Australian Academic Press Pty. Ltd; 2003, p. 25-62 18. French S. Physiotherapy: a psychosocial approach. Oxford: Reed Educational and Professional Publishing Ltd;1997. 30.
(31) 19. Turner JA, Jensen MP, Romano JM. Do beliefs, coping and catastrophizing independently predict functioning in patients with chronic pain?. Pain 2000;85:115-25 20. Astin J. Mind-Body Therapies for the Management of Pain. Clinical Journal of Pain 2004;20:27-32 21. Frost H, Lamb S, Doll H, Taffe Carver P, Stewart-Brown S. Randomised controlled trial of physiotherapy compared with advice for low back pain. BMJ, doi:10.1136/bmj.38216.868808.7C (published 17 September 2004) 22. Burton K, Waddell G, Tillotson M, Summerton N. Information and Advice. ct (c or ) ia 20 U 05 ni ve rs. 1999;24:2484-91. ity. to Patients With Back Pain Can Have a Positive Effect. Spine. 23. Harding V, Williams AC de C. Extending physiotherapy skills using a psychological approach: Cognitive-behavioural management of chronic pain. Physiotherapy 1995;81:681-7. 24. Verbeek J, Sengers M, Riemens L, Haafkens J. Patient Expectations of Treatment for Back Pain. Spine 2004;29:2309-18. Vi. 25. Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 2000;85:317-32 26. Lucas N. Psychosocial factors in the osteopathic practice: To what extent should they be assessed?. International Journal of Osteopathic Medicine 2005;8:49-59 27. McCormack GL. Pain management by occupational therapists. American Journal of Occupational Therapy 1998;42:582-90. 31.
(32) 28. Green CR, Wheeler JRC, LaPorte F. Clinical decision making in pain management: Contributions of physician and patient characteristics to variations in practice. Pain 2003;4:29-39 29. Feuerstein M, Beattie, P. Biobehavioral factors affecting pain and disability in low back pain: Mechanisms and assessment. Physical. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. Therapy 1995;75:267-80. 32.
(33) TABLES AND FIGURES. Table 1. Percentage usage of varying management modalities indicated by osteopaths for CLBP patients (N=142). Usually. Sometimes. Rarely. Never. Patient Education. 64. 32. 4. 0. 0. Physical Exercise. 45. 46. 9. 0. 0. Relaxation Techniques. 9. 21. 42. 22. 6. Auditory Distraction. 1. 1. 9. 27. 62. Visualisation. 1. 1. 21. 30. 47. Medication. 1. 9. 63. 18. 9. Referral to Psychologist etc. 0. 1. 38. 49. 12. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. Always. 33.
(34) Table 2. Osteopaths’ perceived effectiveness of management modalities for the management of CLBP patients.* (N=142). Effective Mean. SD. (%). Don't Know(%). Uneffective (%). 4.3. 0.6. 94. 5. 1. Physical Exercise. 4.3. 0.6. 96. 1. 3. Relaxation- Breathing. 3.6. 0.7. 57. 37. 6. Relaxation- Muscle relaxation. 3.5. 0.7. 57. 38. 5. Auditory Distraction. 3.0. 0.5. 8. 84. 8. Visualisation. 3.1. 0.6. 21. 70. 8. 3.6. 0.7. 67. 21. 12. 3.4. 0.7. 47. 46. 7. ct (c or ) ia 20 U 05 ni ve rs. Medication. ity. Patient Education. Referral to Psychologist etc. Vi. * 1 (Not effective) to 5 (Very effective). 34.
(35) Table 3. Total Variance Explained (Items 14-24 Belief section). Initial Eigenvalues Total 2.717. % of Variance 27.167. Cumulative % 27.167. Total 1.190. % of Variance 11.903. Cumulative % 11.903. Total 1.275. 2. 1.484. 14.840. 42.007. 2.005. 20.052. 31.954. 1.945. 3. 1.249. 12.494. 54.500. .893. 8.931. 40.886. .839. 4. 1.136. 11.357. 65.858. .621. 6.212. 47.098. 1.230. 5. .765. 7.654. 73.512. 6. .631. 6.307. 79.819. 7. .600. 5.999. 85.818. 8. .530. 5.301. 91.119. 9. .460. 4.596. 95.715. ity. .428 4.285 100.000 Extraction Method: Maximum Likelihood. a When factors are correlated, sums of squared loadings cannot be added to obtain a total variance.. ct (c or ) ia 20 U 05 ni ve rs. 10. Vi. Factor 1. Extraction Sums of Squared Loadings. Rotation Sums of Squared Loadings(a ). 35.
(36) Table 4. Factor Matrix (Items 14-24 Belief section) 1 23. I often deliberately. 2. Factor 3. 4. .999. take advantage of the placebo effect to help my patients with CLBP feel better.. .693. 17. I often feel frustrated. .262. -.212. by patients with CLBP who want me to "fix" them. .675. 20. There is nothing physically wrong with many patients who complain of CLBP. .593. 19. I often have negative. -.216. feelings about dealing with patients who have. .499. expectations about what practitioners can do for them 15. Physical therapy (osteopathy) is beneficial for a CLBP patient 24. Many of the physical therapy (Osteopathic) interventions used for chronic low back pain only have a placebo effect. 22. A patient who. -.434. .313. .232. .371. .403. Vi. often have unrealistic. ct (c or ) ia 20 U 05 ni ve rs. 14. Patients with CLBP. ity. chronic low back pain. -.261. -.224. .336. .568. .313. .405. .310. .320. -.374. understands how to care for their back will have fewer repeated episodes of pain 21. Patients with CLBP given a clear explanation of the cause of their problem are likely to do better. 16. In gerneral, a majority. -.222. of CLBP patients are undertreated. Extraction Method: Maximum Likelihood. a. 4 factors extracted. 12 iterations required. 36.
(37) Table 5. Pattern Matrix(a) (Items 14-24 Belief section). Factor 1. 3. 4. 1.016. Q.17. 0.809. Q.19. 0.633. Q. 20. 0.591. Q. 14. 0.501. 0.229. Q. 22. 0.633. Q. 21. 0.513 -0.563. Q. 15. -0.511. Q. 24. 0.265. ct (c or ) ia 20 U 05 ni ve rs. Q. 16. ity. Q. 23. 2. 0.485. Vi. Extraction Method: Maximum Likelihood. Rotation Method: Oblimin with Kaiser Normalization. a Rotation converged in 7 iterations.. 37.
(38) Table 6. Structure Matrix (Items 14-24 Belief section). Factor 1. 3. 0.995. Q.17. 0.766. Q. 20. 0.663. Q. 19. 0.623. Q. 14. 0.520. 0.405. 0.245. Q. 22. 0.677. Q. 21. 0.509 -0.245. -0.315. Q. 24. 0.352. 0.340. 0.231. -0.220. -0.584. ct (c or ) ia 20 U 05 ni ve rs. Q.15. Q. 16. 4. ity. Q. 23. 2. 0.553. -0.526. Vi. Extraction Method: Maximum Likelihood. Rotation Method: Oblimin with Kaiser Normalization.. 38.
(39) Table 7. Osteopath’s Beliefs Concerning Patients with CLBP (%). Percentage Neither Agree nor Question. Disagree. N. Mean. SD. Agree. Disagree. 140. 3.3. 0.9. 46. 32. 30. 141. 4.4. 0.6. 94. 5. 1. 141. 3.2. 0.9. 35. 41. 23. 141. 3.0. 1.0. 26. 37. 14. Patients with chronic low back pain often have unrealistic expectations about what practitioners can do for them. 15. Physical therapy (Osteopathy), is beneficial for a CLBP patient.. treated. 17. I often feel frustrated by patients with chronic low. 37. ct (c or ) ia 20 U 05 ni ve rs. back pain who want me to “fix” them.. ity. 16. In general, a majority of CLBP patients are under. 18. Patient gender affects how he or she deals with pain.. 141. 3.1. 0.9. 37. 40. 23. 141. 2.2. 0.8. 5. 28. 67. 141. 2.0. 0.8. 5. 11. 84. 141. 3.8. 0.9. 70. 23. 7. 141. 4.3. 0.6. 93. 4. 1. 140. 2.5. 1.0. 18. 30. 52. 141. 2.1. 1.0. 9. 19. 71. 19. I often have negative feelings about dealing with patients who have chronic low back pain.. 20. There is nothing physically wrong with many patients who complain of chronic low back pain. 21. Patients with chronic low back pain given a clear. better.. Vi. explanation of the cause of their problem are likely to do. 22. A patient who understands how to care for their back will have fewer repeated episodes of pain 23. I often deliberately take advantage of the placebo effect to help my patients with chronic low back pain feel better. 24. Many of the physical therapy (Osteopathic) interventions used for chronic low back pain only have a placebo effect.. * 1( Strongly Disagree) to 5 (Strongly Agree). 39.
(40) Table 8. Practitioner Confidence in management of chronic compared to acute low back pain. Practitioner Confidence. Percentage Extremely. Very. Moderately. A Little. Not. Mean. SD. Confident. Confident. confident. Confident. Confident. graduation). 2.7. 0.9. 1. 13. 50. 26. 9. CLBP (now). 3.9. 0.7. 20. 53. 26. 0. 0. graduation). 2.6. 0.9. 1. 14. 42. 31. 12. ALBP (now). 4.2. 0.7. 31. 57. 11. 1. 0. CLBP (upon. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. ALBP (upon. 40.
(41) Table 9. Osteopath Characteristics. Characteristic. Mean. SD. Range. Age. 37.6. 11. 23-69. Percentage of females. 50%. Percentage of males. 50% 7. 0-37. Years in practice. 12. Percentage of practitioners undertaking 60%. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. further pain management education. 41.
(42) Table 10. Employment Type. n. Solo. 65. Group single discipline. 38. Group multi discipline. 59. Hospital. 0. Academic salaried. 4. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. Employment. 42.
(43) Table 11. Description of chronic pain management teaching at university/college. Chronic pain management teaching. % 23. Briefly Covered. 52. None. 16. Can't Remember. 9. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. Covered in Depth. 43.
(44) Table 12. Perceived Adequacy of Pain Education by Osteopaths*. Percentage Very. Less than. Very. Adequate. Adequate. Neutral. Adequate. Inadequate. 6. 53. 18. 18. 4. Mean. 3.4. SD. 1.0. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. *1 (very inadequate) to 5 (very adequate). 44.
(45) Table 13. Estimated percentage of patients with chronic and acute low back pain*. Percentage of patients estimated by osteopaths n(%) 0-25%. 26-50%. 51-75%. 76-100%. Chronic Low Back Pain. 141. 40(28). 68(48). 29(21). 4(3). Acute Low Back Pain. 140. 79(56). 15(32). 15(11). 1(1). Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. N. 45.
(46) Table 14. Practitioner Satisfaction with CLBP Management*. Practitioner Satisfaction N=140 n Percentage(%) Mean SD. Very satisfied 28 20. Satisfied 93 66. Neither Satisfied nor Dissatisfied 17 12. Dissatisfied 2 1. Very Dissatisfied 0 0. 4 0.6. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. * 1 (Very Dissatisfied) to 2 (Very Satisfied). 46.
(47) 70 60 Percentage. 50 40. Alw ays. 30. Sometimes. Usually Rarely. 20. Never. 10 0. Patient. Physical. Relaxation. Auditory. Education. Exercise. Techniques. Distraction. Visualisation. Medication. Referral to Psychologist. ct (c or ) ia 20 U 05 ni ve rs. ity. CLBP Non-Manual Managem ent Modalities. Figure 1. Non-manual pain management modalities utilized by osteopaths in. Vi. the management of CLBP. 47.
(48) Mean level of confidence. 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0 CLBP (upon CLBP (now ) ALBP (upon ALBP (now ) graduation) graduation) Osteopaths' confidence in their ability to m anage CLBP vs ALBP. Figure 2. Osteopaths’ confidence in their ability to manage chronic vs acute. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. low back pain. 48.
(49) Number of Responses (n). 140 120 100 80 60 40 20 0 Continued Education. Professional Colleagues. Reading Current Literature. Graduate Level Education. ity. Sources of Pain Management Information. Vi. Most Useful.. ct (c or ) ia 20 U 05 ni ve rs. Figure 3. Sources of Pain Management Information Osteopaths Consider. .. 49.
(50) APPENDIX 1. Acknowledgements. The authors wish to sincerely thank Philip Holmes-Smith, Principal Researcher, School Research, Evaluation and Measurement Services for his guidance and assistance with the statistical analysis for this paper. We acknowledge the advice provided by Dr Brian Sharpley, Director, BriTer Solutions The authors would also like to thank the 142 osteopaths who took the time to. Vi. ct (c or ) ia 20 U 05 ni ve rs. ity. complete and return the survey.. 50.
(51) 2. Osteopath Pain Management and Attitude Survey 1. Your present age________ years 2. Gender:. Male Female. 3. Year of graduation from osteopathic education ______________ 4. Which term/s best describe your employment? You may choose more than one Solo practitioner Group single discipline Group multi discipline Hospital salaried employee Academic salaried employee Other (please describe) ___________________________________________ 5. Which best describes the teaching of chronic pain management you received at university/osteopathic college? Covered in depth. Briefly covered. None. Can’t remember. . . . . 6. How do you perceive the adequacy of your pain education upon entering osteopathic practice? Neutral. Less than Adequate. Very Inadequate. . . . . . ity. Adequate. ct (c or ) ia 20 U 05 ni ve rs. Very Adequate. 7. Have you undertaken any further education regarding pain management since graduating? Yes. No. 8. What sources of pain management information, for professional education do you consider useful? You may choose more than one.. Vi. Continuing education Professional colleagues Reading current literature Graduate level education Other (please describe) ___________________________________________. CONFIDENCE Answer these questions by marking the response that best describes your confidence. Extremely Confident. Very Confident. Moderately. A Little Confident. Not Confident. a. Chronic low back pain. . . . . . b.. . . . . . . . . . . . . . . . 9. What is your level of confidence in being able to help patients with:. Acute low back pain. 10. Upon entering practice how confident did you feel to manage: a. Chronic low back pain. 51.
(52) b. Acute low back pain 11. At present time, how confident do you feel to manage: a. Chronic low back pain. . . . . . b. Acute low back pain. . . . . . 12. Estimate the percentage of patients you treat/manage that suffer from: 0 – 25 %. 26 – 50 %. 51 – 75 %. 76 – 100 %. a. Chronic low back pain. . . . . b. Acute low back pain. . . . . 13. How satisfied are you with the management and care you provide to patients with CLBP? Very satisfied. Satisfied. . . Neither Satisfied Nor Dissatisfied. Dissatisfied. Very dissatisfied. . . . ct (c or ) ia 20 U 05 ni ve rs. ity. OSTEOPATH’S BELIEF. Answer these questions by marking the response that best describes your belief Agree. Neither Agree or Disagree. Disagree. Strongly Disagree. 14. Patients with chronic low back pain often have unrealistic expectations about what practitioners can do for them.. . . . . . 15. Physical therapy (Osteopathy), is beneficial for a CLBP patient.. . . . . . 16. In general, a majority of CLBP patients are under treated.. . . . . . 17. I often feel frustrated by patients with chronic low back pain who want me to “fix” them.. . . . . . 18. Patient gender affects how he or she deals with pain.. . . . . . 19. I often have negative feelings about dealing with patients who have chronic low back pain.. . . . . . 20. There is nothing physically wrong with many patients who complain of chronic low back pain.. . . . . . 21. Patients with chronic low back pain given a clear explanation of the cause of their problem are likely to do better.. . . . . . 22. A patient who understands how to care for their back will have fewer repeated episodes of pain.. . . . . . 23. I often deliberately take advantage of the placebo effect to help my patients with chronic low back pain feel better.. . . . . . Vi. Strongly Agree. 52.
(53) 24. Many of the physical therapy (Osteopathic) interventions used for chronic low back pain only have a placebo effect.. . . . . . Management Modalities 25. Apart from manual osteopathic techniques, which management modalities do you utilise or teach your chronic pain patient to help them cope with their pain? Answer by marking the response that best describes your use of these modalities. Rarely. Sometimes. Usually. a. Patient education. . . . . . b. Physical exercise. . . . . . . . . . . d. Auditory distraction (Music). . . . . . e. Visualisation. . . . . . f. Medication. . . . . . . . . c. Relaxation techniques - (Breathing, Muscle. ct (c or ) ia 20 U 05 ni ve rs. relaxation etc). ity. Never. g. Referral to Psychologist/Psychiatrist/counsellor etc. . . Always. 26. How do you perceive the effectiveness of the following coping strategies for patients with CLBP? Very Effective. Effective. Don’t know. Less than Effective. Not Effective. . . . . . . . . . . . . . . . . . . . . d. Auditory distraction (Music). . . . . . e. Visualisation. . . . . . f. Medication. . . . . . g. Referral to Psychologist/Psychiatrist etc.. . . . . . a. Patient education b. Physical exercise. i. Breathing. Vi. c. Relaxation techniques:. ii. Muscle relaxation. h. Other (as specified above) _________________________________________________________________ _________________________________________________________________________________________. THANKYOU FOR YOUR PARTICIPATION Please include any questions or comments regarding this study on the back of this survey.. 53.
(54) 3. Information to Participants. INFORMATION TO PARTICIPANTS. ct (c or ) ia 20 U 05 ni ve rs. ity. We invite you to be a part of a study investigating the management of chronic low back pain by practising osteopaths and their attitudes towards chronic low back pain patients. This study will involve a short questionnaire (approximately 10 minutes completion time), which will examine factors such as the osteopath’s attitudes concerning patients with chronic low back pain, the osteopath’s confidence with their management/treatment of chronic low back pain and the osteopath’s opinions on perceived effectiveness of management modalities used for chronic low back pain patients. This study aims to • Determine management modalities employed, in the management of chronic low back pain, and their perceived effectiveness. • Determine osteopaths’ attitudes towards treating chronic low back pain patients and confidence in treating them. The outcomes of this study may demonstrate how the practitioners are actually managing chronic low back pain patients. Further understanding of the ways in which osteopaths are managing chronic low back pain patients may be of benefit in the development of the profession and determine where osteopaths stand in relation to other professions, regarding this area. There are no hidden agendas involved in this research.. Vi. In the event that any potential issues arise, participants will be provided with written feedback from the investigator. The data from this research may be published. In this case, your confidentiality will be protected by the use of an alphanumerical coding system. The completion of this questionnaire and subsequent return in the reply paid envelope provided, implies consent to participation in this study. The researchers will not be able to identify individual participants. Participation in this study is voluntary. A counselling psychologist may be contacted should you require one as a result of completing the survey. Counselling Psychologists contact details: Mark Andersen 9919 5413 If participants have any queries regarding the study they can forward any questions to the researchers at Victoria University City Flinders Campus Please return the questionnaire by 30th May 2005. If you have any queries or complaints about the way you have been treated, you may contact the Secretary, University Human Research Committee, Victoria University, PO Box 14428 MCMC, Melbourne, 8001 (telephone: (03) 9688 4710). 54.
(55)
Figure


Related documents
Given the social conditions that have been proved to be characteristic of solo mothers – solo breadwinners in a sex-segregated labour market, and largely solo caregivers – this
To evaluate the prognostic role of above-mentioned mutations in stage II colon cancer, we aimed to determine the status of the BRAF V600E mutation, MSI status, KRAS mutation
Military veterans in the federal civil service: a qualitative Military veterans in the federal civil service: a qualitative descriptive study using Schlossberg's transition theory
Therefore, the effect of subsidies on both R&D input and R&D output is compared between independent high-tech young firms (NTBFs), independent low-tech young firms (LTBFs)
Instructor will: - Notify student they are unable to return to clinical setting until successful remediation is complete -Have a plan of action identified on conference form
In spite of the many ongoing and evolving challenges associated with cloud forensic extraction and analysis, UFED Cloud Analyzer offers a unique solution to investigators who
Thus Functionally graded materials (FGMs) are spatial composites that display discrete or continously varying composition as in [1] over a geometrical length.The segregation
Despite these promising findings, the results of our sensory evaluation indicate that gamma irradiation causes undesirable changes to the sensory characteristics of