Through Teaching Are We Learning? Learning Through Teaching: Facilitating Interprofessional Education Experiences
Full text
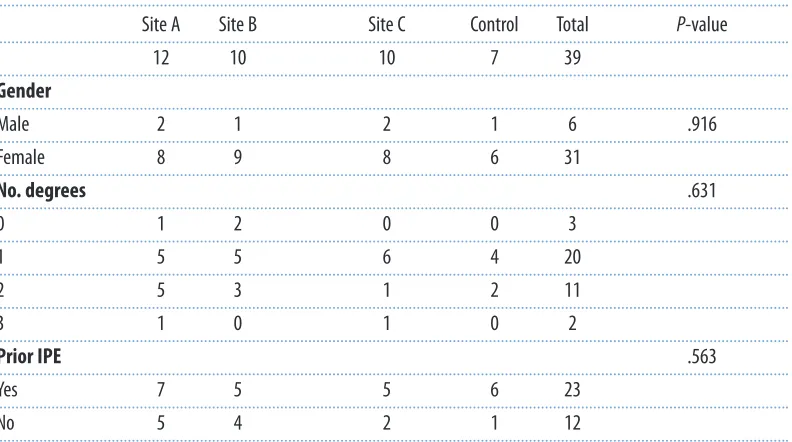
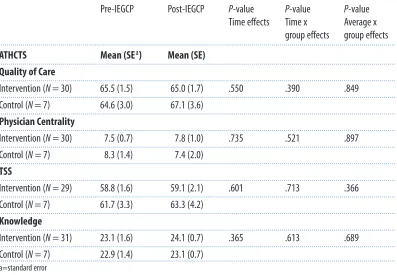
Figure
Related documents
So you have Type 2 diabetes and you have now been prescribed insulin to help your body to keep the blood glucose levels under good control.. Insulin can be prescribed in once
Companies like Sears and Southwest Airlines (USA) have been able to create a linkage between employee satisfaction and customer loyalty. This linkage helps to estimate
A before-after study of illuminance at intersections conducted by Oya, Ando and Kanoshima (2002) has showed a clear benefit of lighting at major urban
X The State determines eligibility for PACE enrollees under rules apply in g to instituti onal groups, but chooses not to apply post-e li gibility treatment of income
The main tasks will consist of (i) modeling of a typical electric power system in regional level in collaboration with electricity generation, capacity expansion, applica- tion of
Relevant comparison materials to assess a local production of the figurines at Saqqara include ceramic reference data obtained from mixed "silt and gebel" and mixed
However, it was claimed over a decade ago that budgetary, accounting and financial reporting formats and standards varied between Australian governments and that a lack of
Following the simulated Council meeting, the meeting discussed the exercise itself and considered matters arising from it. It was agreed that the Plan itself as a document worked