The Effect of Respiratory
Therapist-Initiated Treatment Protocols on Patient
Outcomes and Resource Utilization*
Marin H. Kollef, MD, FCCP; Steven D. Shapiro, MD, FCCP;
Darnetta Clinkscale, MA; Lisa Cracchiolo, RRT; Donna Clayton, BS;
Russ Wilner, RRT; and Linda Hossin, RRT
Context:
Physicians frequently prescribe respiratory treatments to hospitalized patients, but the
influence of such treatments on clinical outcomes is difficult to assess.
Objective:
To compare the clinical outcomes of patients receiving respiratory treatments
managed by respiratory care practitioner (RCP)– directed treatment protocols or
physician-directed orders.
Design:
A single center, quasi-randomized, clinical study.
Setting:
Three internal medicine firms from an urban teaching hospital.
Patients:
Six hundred ninety-four consecutive hospitalized non-ICU patients ordered to receive
respiratory treatments.
Main outcome measures:
Discordant respiratory care orders, respiratory care charges, hospital
length of stay, and patient-specific complications. Discordant orders were defined as written
orders for respiratory treatments that were not clinically indicated as well as orders omitting
treatments that were clinically indicated according to protocol-based treatment algorithms.
Results:
Firm A patients (n
ⴝ
239) received RCP-directed treatments and had a statistically lower
rate of discordant respiratory care orders (24.3%) as compared with patients receiving
physician-directed treatments in firms B (n
ⴝ
205; 58.5%) and C (n
ⴝ
250; 56.8%; p
<
0.001). No
statistically significant differences in patient complications were observed. The average number
of respiratory treatments and respiratory care charges were statistically less for firm A patients
(10.7
ⴞ
13.7 treatments; $868
ⴞ
1,519) as compared with patients in firms B (12.4
ⴞ
12.7
treatments, $1,124
ⴞ
1,339) and C (12.3
ⴞ
13.4 treatments, $1,054
ⴞ
1,346; p
ⴝ
0.009
[treat-ments] and p
<
0.001 [respiratory care charges]).
Conclusions:
Respiratory care managed by RCP-directed treatment protocols for non-ICU
patients is safe and showed greater agreement with institutional treatment algorithms as compared
with physician-directed respiratory care. Additionally, the overall utilization of respiratory treatments
was significantly less among patients receiving RCP-directed respiratory care.
(CHEST 2000; 117:467–475)
Key words:asthma; chronic obstructive pulmonary disease; outcomes; protocols; respiratory careAbbreviations: APACHE⫽acute physiology and chronic health evaluation; BJH⫽Barnes-Jewish Hospital; CI⫽confidence interval; RCP⫽respiratory care practitioner
T
he administration of respiratory treatments is a
necessary component of the care of hospitalized
patients, especially those individuals with
thoracoab-dominal disease processes. However, a number of
clinical studies suggest that respiratory treatments are
often needlessly prescribed to patients who do not
derive benefit from their administration.
1–10To date,
few investigations have attempted to define the optimal
method for the utilization of respiratory treatments or
to determine the impact of various respiratory care
utilization strategies on patient outcomes.
11–13This
represents an important area of investigation because
of the potential complications associated with
inappro-priate use of respiratory treatments and the need to
conserve valuable medical resources for treatments
that are more likely to provide patient benefits.
14,15To better determine the optimal use of respiratory
*From the Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Washington University School of Medicine (Drs. Kollef and Shapiro), and Department of Respi-ratory Care Services, Barnes-Jewish Hospital (Mss. Clinkscale, Cracchiolo, Clayton, and Hossin, and Mr. Wilner), St. Louis, MO. This investigation was supported by a grant provided by the American Association of Respiratory Care.
Manuscript received March 5, 1999; revision accepted June 28, 1999.
Correspondence to: Marin H. Kollef, MD, FCCP, Pulmonary and Critical Care Medicine, Washington University School of Medi-cine, Campus Box 8052, 660 South Euclid, St. Louis, MO 63110; e-mail: mkollef@pulmonary.wustl.edu
treatments for hospitalized patients not requiring
ICU admission (
ie
, non-ICU patients), we
per-formed a clinical trial that had two main objectives.
The first goal of our study was to determine the
occurrence of administered respiratory treatments
that were discordant with the respiratory care
guide-lines of the hospital. Our second goal was to test the
hypothesis that the use of respiratory care
practi-tioner (RCP)-directed treatment protocols would
decrease the occurrence of discordant respiratory
treatments.
Materials and Methods
Study Location and Population
The study was conducted at a university-affiliated urban teaching hospital: Barnes-Jewish Hospital (BJH; 1,400 beds). During a 9-month period (February 1998 to October 1998), all patients ordered to receive respiratory treatments from the three internal medicine firms of the hospital (firms A, B, C) were potentially eligible for this investigation. The internal medicine firms are closed groups of internal medicine house officers, teaching physicians, and private attending physicians caring for patients on the medicine floors of BJH. Physicians are assigned to the firms so as to achieve a similar distribution of teaching and private attending physicians as well as a similar distribution of general internists and subspecialty-trained physicians, including pulmonary subspecialists. The patient populations served by the three firms are also similar in terms of their physicians’ practices (eg, general internal medicine vs subspecialty practices). There is no crossover of physicians between the internal medicine firms, which also have their own administrative structures (eg, chief residents, chiefs of service). Patients admitted to the internal medicine firms received their care on one of four hospital floors according to bed availability. Each of the medical floors involved in this study had a mixture of patients from the different medical firms. Patients were entered into the investigation if they were
⬎16 years old and excluded if they had a diagnosis of cystic fibrosis. The study was approved by the Washington University School of Medicine Human Studies Committee.
Study Design
Patients were assigned, at the time of hospital admission, to have their respiratory care managed by RCP-directed treatment protocols or by physician-directed orders. All patients assigned to firm A received RCP-directed treatments, whereas patients assigned to firms B and C received physician-directed respiratory care. Patient assignment to a medicine firm was based on their attending or clinic physician’s firm assignment. All patients without an attending or clinic physician were randomly assigned by the hospital admissions office to one of the medicine firms. The primary outcome measure was the occurrence of discordant respiratory care orders. Discordant respiratory care orders were defined as written orders that omitted clinically indicated treat-ments (eg, absence of an order for bronchopulmonary hygiene in a patient with lobar atelectasis), as well as orders for treatments that were not clinically indicated according to protocol-based treatment algorithms (eg, an order for bronchopulmonary hy-giene in a patient without an appropriate indication; Fig 1). Secondary outcome measures included the total number of respiratory care treatments per patient, charges for respiratory
care treatments, hospital length of stay, patient-specific compli-cations, and hospital mortality. All data were collected on a standardized data collection form by registered respiratory ther-apists who were blinded to patients’ firm assignments as well as to whether patients’ respiratory care orders were protocol guided. Respiratory Care Treatment Protocols
A series of respiratory care treatment protocols have been developed at BJH using a branched-chain logic format similar to that used at the Cleveland Clinic.12,13,16These protocols follow the recommendations of the American Association for Respira-tory Care Clinical Practice Guidelines.17,18 The protocols were developed by a working group of physicians and RCPs at BJH. Before their acceptance, each protocol underwent a trial period of utilization to determine its safety and effectiveness. The protocols were subsequently published as a hospital resource guide and made available to all physicians with admitting privi-leges to BJH, hospital nursing units, and hospital administrative staff. Additionally, each house officer and RCP was given a pocket-sized version of the resource guide before beginning the investigation. All RCPs underwent educational in-service training focused on the performance of patient assessments and the utilization of the treatment protocols. An example of a RCP treatment protocol is provided in Figure 1.
Two RCPs (L.C. and L.H.) prospectively evaluated all respi-ratory care orders to determine the presence of discordant orders. These two RCPs were blinded to patients’ firm assign-ments as well as to whether patients’ respiratory care orders were protocol guided, had no other clinical or administrative duties during their participation in the study, and contributed to the initial development and updating of the respiratory care treat-ment protocols used at BJH. Respiratory care orders were obtained daily by the two reviewers using an automated medical order communication system without having to directly review the medical record order sheets. This was done to minimize observer bias in regards to who wrote the original respiratory care orders (physician vs respiratory therapist). All respiratory care orders, discordant order assessments, and patient outcomes were subsequently reviewed by the medical directors of the respiratory care department (M.H.K. and S.D.S.). This was done to ensure that the discordant classification of respiratory care orders ad-hered to the explicit definitions described above.
RCP-Directed Respiratory Care
Each firm A patient ordered to receive RCP-directed treat-ments underwent formal assessment by a registered respiratory therapist who had⬎5 years of experience as a respiratory care supervisor. The respiratory therapist performing the patient assessment determined the patient’s respiratory care needs based on the institutional treatment protocols. A respiratory care plan was developed and orders were written. The patient’s treating physician requesting respiratory care was informed of the patient assessment. Treating physicians who disagreed with the assess-ment and orders of the RCP performing the evaluation were allowed to change the orders. However, all disagreements were subsequently reviewed by the medical directors of the respiratory care department for final discussion with the treating physicians. Physician-Directed Respiratory Care
All aspects of respiratory care were ordered by the treating physicians for patients assigned to firms B and C. Respiratory therapists could not make changes in the treatment orders without a physician’s order. However, respiratory therapists could
communicate their opinions and observations about patients’ needs for respiratory care to the treating physicians.
Definitions
All definitions were selected prospectively as part of the original study design. We calculated acute physiology and chronic health evaluation (APACHE) II scores on the basis of clinical data available from the first 24-h period of hospitalization.19 Lifestyle scores were previously defined as follows20: 0 indicates employed; 1, independent, fully ambulatory; 2, restricted activi-ties, able to live on own and get out of home to do basic necessities, severe limitation in exercise ability; 3, housebound, cannot get out of house unassisted, cannot live alone or perform heavy chores; and 4, bed- or chair-bound. The diagnostic criteria for nosocomial pneumonia were modified from those established by the American College of Chest Physicians.21 Nosocomial
pneumonia was defined as the development of a new or progres-sive radiographic infiltrate in conjunction with two of the follow-ing: fever (temperature⬎38.3°C), leukocytosis (leukocyte count
⬎10⫻109/L), and purulent tracheal aspirate. Lobar atelectasis was defined as displacement of a fissure along with opacification of a lobe demonstrated radiographically. Immunosuppression was defined as patients receiving corticosteroids, having a positive serum HIV antibody, having received chemotherapy in the past 45 days, or having neutropenia (absolute neutrophil count
⬍0.5⫻109/L) resulting from the administration of chemother-apy, or as recipients of an organ transplant (kidney, liver, heart, lung, bone marrow) requiring immunosuppressive agents. Statistical Analysis
We estimated the sample size needed to provide 90% power to detect a difference in the rate of discordant orders of 20%. We Figure1. Treatment guideline for bronchial hygiene. IPPB⫽intermittent positive-pressure
used an␣error of 0.05 (two-tailed) and assumed a baseline rate of discordant orders of 50% on the basis of preliminary surveys conducted before performing the investigation. According to these assumptions, 269 patients were needed in each study group to provide the desired power. All comparisons were unpaired, and all tests of significance were two-tailed. Continuous variables were compared using the Student’sttest for normally distributed variables and the Wilcoxon rank sum test for non-normally distributed variables. The2or Fisher’s Exact Test were used to compare categorical variables. The primary data analysis was an intention-to-treat analysis, comparing the rate of discordant orders among patients assigned to receive RCP-directed treat-ments in firm A and the patients receiving physician-directed respiratory care in firms B and C.
Multiple logistic regression analysis, using a commercial statis-tical package, was used to identify predictor variables that were significantly related to the likelihood of having a discordant order for respiratory care (eg, presence of a discordant order as the dependent outcome variable).22 Baseline covariants were in-cluded in models that were judgeda priorito be clinically sound. This was prospectively determined to be necessary to avoid producing spuriously significant results with multiple compari-sons.23Potential predictor variables for model entry were iden-tified using univariate analysis, where a p value of 0.15 was used to determine entry into the logistic regression model. A stepwise
approach was used to enter new terms into the logistic regression model, and 0.05 was set as the limit for the acceptance or removal of these terms. Results of the logistic regression analysis are reported as adjusted odds ratios with 95% confidence intervals (CIs).
Results
Patients
Six hundred ninety-four consecutive patients
or-dered to receive respiratory treatments from firms A,
B, and C were enrolled into the study. At the time of
randomization, no statistically significant differences
were found among the three firms for age, sex,
ethnicity, lifestyle scores, APACHE II scores,
smok-ing status, presence of a do-not-resuscitate order,
tracheostomy at the time of hospital admission, and
the presence of COPD, congestive heart failure,
underlying malignancy, seropositivity for HIV, or an
immunocompromised state (Table 1). Patients in
firm B were statistically more likely to have an
Table 1—Patient Characteristics at Time of Hospital Admission*
Characteristics Firm A (n⫽239) Firm B (n⫽205) Firm C (n⫽250) p Value Age, yr 60.8⫾17.5 61.5⫾17.8 59.7⫾17.2 0.366 Male 96 (40.2) 82 (40.0) 108 (43.2) 0.726 Race White 106 (44.4) 85 (41.5) 114 (45.6) 0.574 Black 133 (55.6) 118 (57.5) 134 (53.6) Other 0 (0.0) 2 (1.0) 2 (0.8) Lifestyle score 2.0⫾1.1 1.8⫾1.2 2.0⫾1.1 0.450 APACHE II score 10.5⫾5.1 9.2⫾4.8 10.0⫾4.9 0.086 Smoking status Nonsmoking 68 (28.5) 56 (27.3) 62 (24.8) 0.859 Current smoker 55 (23.0) 53 (25.9) 62 (24.8) Ex-smoker 116 (48.5) 96 (46.8) 126 (50.4) Do-not-resuscitate order 16 (6.7) 8 (3.9) 14 (5.6) 0.433
Congestive heart failure 107 (44.8) 72 (35.1) 102 (40.8) 0.118
COPD 179 (74.9) 167 (81.5) 184 (73.6) 0.117 Underlying malignancy 38 (15.9) 22 (10.7) 30 (12.0) 0.230 HIV-positive 1 (0.4) 2 (1.0) 7 (2.8) 0.096 Immunocompromised 32 (13.4) 24 (11.7) 40 (16.0) 0.406 Tracheostomy 3 (1.3) 2 (1.0) 4 (1.6) 0.916 Admission diagnosis COPD/asthma 58 (24.3) 80 (39.0) 65 (26.0) 0.001
Congestive heart failure 44 (18.4) 26 (12.7) 41 (16.4) 0.254
Pneumonia 30 (12.6) 28 (13.7) 53 (21.2) 0.018 Myocardial ischemia 26 (10.9) 25 (12.2) 24 (9.6) 0.674 Gastrointestinal hemorrhage 12 (5.0) 14 (6.8) 8 (3.2) 0.202 Hepatitis/cirrhosis 1 (0.4) 1 (0.5) 0 (0.0) 0.538 Neurologic 7 (2.9) 3 (1.5) 6 (2.4) 0.567 Sepsis 18 (7.5) 9 (4.4) 13 (5.2) 0.327 Renal failure 6 (2.5) 1 (0.5) 6 (2.4) 0.211 Pulmonary fibrosis 2 (0.8) 0 (0.0) 5 (2.0) 0.128 Cancer 12 (5.0) 2 (1.0) 7 (2.8) 0.042 Pulmonary embolism 4 (1.7) 4 (1.9) 5 (2.0) ⬎0.999 Miscellaneous 19 (8.0) 12 (5.8) 17 (6.8) 0.683
admission diagnosis of COPD or asthma and
statis-tically less likely to have an admission diagnosis of
cancer compared with patients in firms A and C.
Firm C patients were statistically more likely to have
an admission diagnosis of pneumonia compared with
patients in firms A and B.
Respiratory Care Treatments and Discordant
Orders
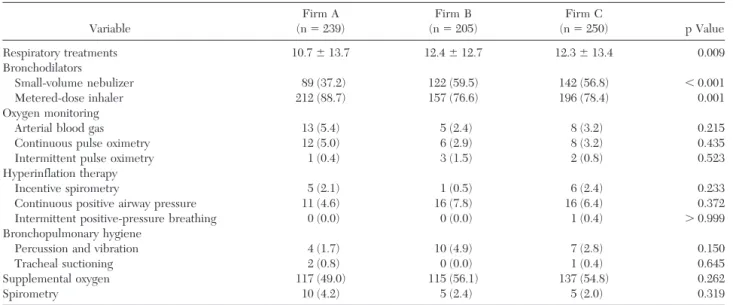
Patients in firm A received statistically fewer
respiratory treatments as compared with patients in
firms B and C (Table 2; Fig 2). The number of
patients receiving small-volume nebulizers was
sta-tistically less and the number of patients receiving
metered-dose inhalers was statistically greater for
firm A patients as compared with patients in firms B
and C (Table 2; Fig 3). The number of small-volume
nebulizer treatments per treated patient was
signif-icantly less in firm A (9.5
⫾
13.5 treatments) as
compared with patients in firms B (12.3
⫾
12.6
treatments) and C (12.7
⫾
13.2 treatments; p
⬍
0.001).
Conversely, the number of metered-dose inhaler
treat-ments per treated patient was statistically greater for
firm A patients (7.1
⫾
8.4 treatments) as compared
with patents in firms B (5.3
⫾
5.6 treatments) and C
(5.0
⫾
5.1 treatments; p
⫽
0.011).
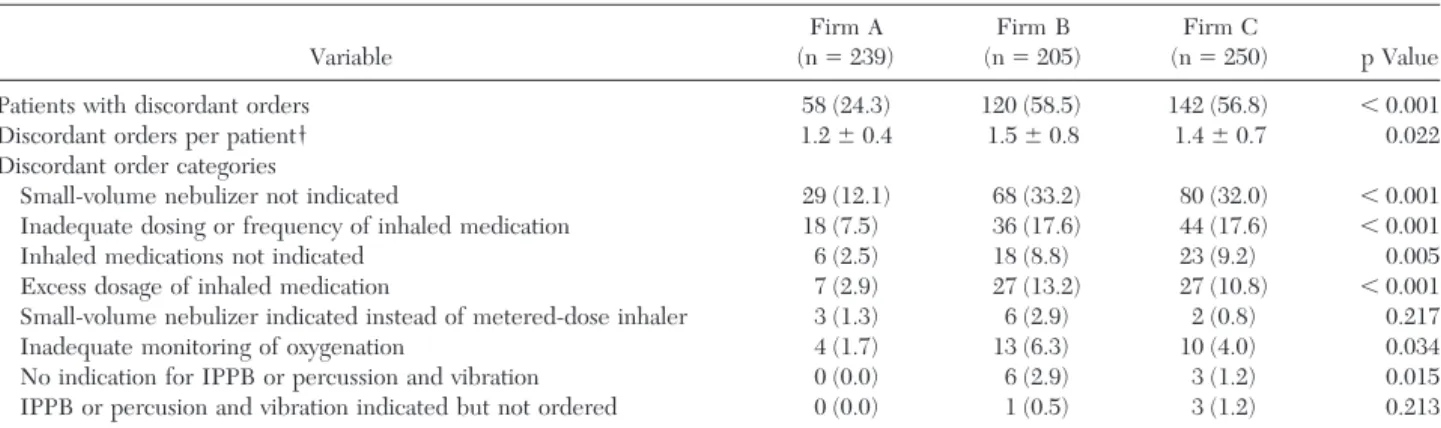
Three hundred twenty study patients (46.1%) had
at least one discordant order for respiratory care.
Among firm A patients, 58 patients (24.3%) had
discordant orders for respiratory treatments; 262
patients (57.6%) in firms B and C combined had
discordant orders for respiratory treatments (relative
risk, 0.42; 95% CI, 0.33 to 0.53). Among patients
with discordant orders, those in firm A had
statisti-cally fewer discordant orders as compared with
patients in firms B and C (Table 3). When we used
multiple logistic regression analysis to control for all
relevant confounders, the adjusted odds ratio
assess-ing the relationship between the presence of
discor-dant orders and firm assignment (assignment to firm
A as compared with assignment to firms B or C) was
0.50 (95% CI, 0.45 to 0.55). Patients in firm A were
statistically less likely to have a discordant order as
compared with patients in firms B and C in six of the
eight specific categories examined (Table 3).
Physi-cians in firm A changed the orders of respiratory
therapists in 86 instances, which represented 3.4% of
all ordered respiratory treatments for firm A
pa-tients. The medical directors of respiratory therapy
overrode 37 (60.5%) of these physician orders.
Secondary Outcomes
No statistically significant differences in the
occur-rence of nosocomial pneumonia, lobar atelectasis,
pneumothorax, hospital mortality, transfer to an
ICU, or the hospital length of stay were observed
between the three internal medicine firms (Table 4).
Patients in firm A had statistically lower charges for
respiratory care as compared with patients in firms B
and C. Patients with at least one discordant order
had statistically greater charges for respiratory care
as compared with patients having no discordant
orders (Fig 4).
Discussion
Our investigation demonstrated that the use of
RCP-directed protocols significantly reduced the
number of prescribed respiratory treatments as
com-pared with physician-directed respiratory care. Use
of the RCP-directed protocols also significantly
de-creased total charges for respiratory care. These
outcomes were achieved without any increase in
adverse patient outcomes. RCP-directed treatments
were significantly more likely to conform to currently
recommended respiratory care practices at our
insti-tution. The overall rate of discordant respiratory care
orders and the number of discordant orders per
patient were significantly less among patients
receiv-ing RCP-directed treatments as compared with
pa-tients receiving physician-directed respiratory care.
Finally, we found a statistically significant association
between the administration of discordant respiratory
treatments and the charges associated with the
de-livery of respiratory care.
The main importance of our findings is that they
offer an additional strategy for more effectively using
respiratory care in hospitalized patients. Protocols
have previously been used to guide specific aspects
of respiratory care for hospitalized patients including
the weaning of mechanical ventilation,
24,25infection
control practices for the prevention of
ventilator-associated pneumonia,
26,27chest physiotherapy,
6the
clinical use of arterial blood gases,
10and inhaled
bronchodilator administration.
28,29Many of those
protocols were specifically designed for
implemen-tation by RCPs to achieve improvements in patient
outcomes, reduce unnecessary medical care costs,
and to unburden physicians from tasks that could be
performed by RCPs.
1The use of such protocols
represents an effective strategy for standardizing
medical practices within medical institutions. The
potential benefits associated with such
standardiza-tion of medical practices include improvements in
patient outcomes, reducing medical care costs,
en-abling the identification of clinical practices
requir-ing change or improvement, improvrequir-ing the quality of
nonblinded clinical research, and establishing a
foundation for the performance of quality
improve-ment efforts.
30,31Standardized medical practices and
protocols achieve such benefits primarily by helping
to create less variable or “chaotic” medical
environ-ments. This occurs by decreasing errors in clinical
management, improving the effectiveness of
avail-able treatments, increasing the accountability of
medical providers, and providing a reference of
measure to assess practices that deviate from the
accepted standard.
32The findings of this investigation are consistent
with the results of previous studies demonstrating
the ability of RCPs to prescribe and perform
respi-ratory treatments for hospitalized non-ICU patients.
Stoller and colleagues
13conducted a randomized
controlled trial comparing RCP-directed respiratory
care with physician-directed respiratory care. These
investigators found that RCP-directed respiratory
care demonstrated better agreement with the
“stan-dard care plan” of their institution and was associated
with lower costs as compared with
physician-di-rected respiratory care. These outcomes were
achieved without any increase in adverse events,
hospital mortality, or hospital length of stay. Similar
studies have been performed focusing on specific
aspects of respiratory care. Several clinical
investiga-tions have demonstrated the ability of RCPs to
Figure2. Box plots for respiratory treatments administered to patients assigned to the three internal medicine firms. Boxes represent 25th to 75th percentiles with 50th percentile (solid line) and mean (broken line) values shown within the boxes. The 10th and 90th percentiles are shown as capped bars, and closed circles mark the 5th and 95th percentiles.
Figure 3. The percentage of study patients receiving small-volume nebulizer treatments and metered-dose inhaler treat-ments according to their internal medicine firm assigntreat-ments, with upper 95% CIs, are shown.
Table 2—Respiratory Care Services Provided*
Variable Firm A (n⫽239) Firm B (n⫽205) Firm C (n⫽250) p Value Respiratory treatments 10.7⫾13.7 12.4⫾12.7 12.3⫾13.4 0.009 Bronchodilators Small-volume nebulizer 89 (37.2) 122 (59.5) 142 (56.8) ⬍0.001 Metered-dose inhaler 212 (88.7) 157 (76.6) 196 (78.4) 0.001 Oxygen monitoring
Arterial blood gas 13 (5.4) 5 (2.4) 8 (3.2) 0.215
Continuous pulse oximetry 12 (5.0) 6 (2.9) 8 (3.2) 0.435
Intermittent pulse oximetry 1 (0.4) 3 (1.5) 2 (0.8) 0.523
Hyperinflation therapy
Incentive spirometry 5 (2.1) 1 (0.5) 6 (2.4) 0.233
Continuous positive airway pressure 11 (4.6) 16 (7.8) 16 (6.4) 0.372
Intermittent positive-pressure breathing 0 (0.0) 0 (0.0) 1 (0.4) ⬎0.999 Bronchopulmonary hygiene
Percussion and vibration 4 (1.7) 10 (4.9) 7 (2.8) 0.150
Tracheal suctioning 2 (0.8) 0 (0.0) 1 (0.4) 0.645
Supplemental oxygen 117 (49.0) 115 (56.1) 137 (54.8) 0.262
Spirometry 10 (4.2) 5 (2.4) 5 (2.0) 0.319
successfully wean patients from mechanical
ventila-tion as compared with tradiventila-tional physician-directed
weaning.
24,25,33Similarly, Alexander and coworkers
6have shown that simple respiratory care guidelines,
based on clinical practices supported by
peer-re-viewed investigations, could be used to reduce the
performance of unnecessary respiratory treatments
without compromising patient care. Such reductions
were associated with significant cost savings and also
allowed RCPs to concentrate their efforts on
treat-ments that potentially were more likely to result in
beneficial patient outcomes. However, it is
impor-tant to note that most of the institutions involved in
the study of protocols and guidelines for respiratory
care (
eg
, Cleveland Clinic Foundation, Cedars-Sinai
Medical Center) have extensive experience with
protocol development and utilization. Therefore, the
results of clinical investigations examining
protocol-directed therapy from these institutions may, in part,
be related to their medical practice cultures (
ie
,
medical cultures accepting protocol- or
guideline-directed treatments). The importance of such an
environment for the successful implementation of
quality improvement efforts, including
protocol-based therapies, has recently been described.
34Our study has several limitations. First, it was
performed within a single institution using house
officers to write most of the treatment orders for
patients admitted to the internal medicine firms.
Therefore, these results may not be generalizable to
patients receiving respiratory care at other centers,
particularly nonteaching hospitals. Second, our
eco-nomic analysis only allowed us to examine
respira-tory care charges and not costs. However, these
charges are directly related to the number and type
of respiratory treatments provided to patients. This is
consistent with other study results showing that the
number of prescribed respiratory treatments is the
most important determinant of respiratory therapy
costs and charges.
6,10Reductions in administered
respiratory treatments may not necessarily reduce
the number of respiratory therapists needed at a
given institution. Therefore, the economic impact of
implemented respiratory therapy protocols should
ideally be assessed in terms of resource utilization as
well as manpower needs. Another important
limita-tion of our study is the possibility of bias on the part
of the RCPs performing the assessments for firm A
patients. It is possible that these RCPs altered their
normal practices to achieve better compliance with
the institutional respiratory care algorithms during
the study period. Lack of compliance with protocols
Table 3—Respiratory Care Orders Discordant From Standard Care*Variable Firm A (n⫽239) Firm B (n⫽205) Firm C (n⫽250) p Value
Patients with discordant orders 58 (24.3) 120 (58.5) 142 (56.8) ⬍0.001
Discordant orders per patient† 1.2⫾0.4 1.5⫾0.8 1.4⫾0.7 0.022
Discordant order categories
Small-volume nebulizer not indicated 29 (12.1) 68 (33.2) 80 (32.0) ⬍0.001 Inadequate dosing or frequency of inhaled medication 18 (7.5) 36 (17.6) 44 (17.6) ⬍0.001
Inhaled medications not indicated 6 (2.5) 18 (8.8) 23 (9.2) 0.005
Excess dosage of inhaled medication 7 (2.9) 27 (13.2) 27 (10.8) ⬍0.001 Small-volume nebulizer indicated instead of metered-dose inhaler 3 (1.3) 6 (2.9) 2 (0.8) 0.217
Inadequate monitoring of oxygenation 4 (1.7) 13 (6.3) 10 (4.0) 0.034
No indication for IPPB or percussion and vibration 0 (0.0) 6 (2.9) 3 (1.2) 0.015 IPPB or percusion and vibration indicated but not ordered 0 (0.0) 1 (0.5) 3 (1.2) 0.213 *Values given as mean⫾SD or No. (%). See Figure 1 for abbreviation.
†Discordant orders for patients having at least one discordant order identified.
Table 4 —Secondary Clinical Outcomes*
Variable Firm A (n⫽239) Firm B (n⫽205) Firm C (n⫽250) p Value Nosocomial pneumonia 0 (0.0) 2 (1.0) 2 (0.8) 0.466 Lobar atelectasis 9 (3.8) 12 (5.9) 11 (4.4) 0.567 Pneumothorax 0 (0.0) 2 (1.0) 0 (0.0) 0.087 Hospital mortality 5 (2.1) 4 (2.0) 8 (3.2) 0.708 Transfer to ICU 10 (4.2) 10 (4.9) 12 (4.8) 0.927
Hospital length of stay, d 5.9⫾4.1 5.5⫾5.0 6.1⫾3.9 0.489
Respiratory care charges, $ 868⫾1,519 1,124⫾1,339 1,054⫾1,346 ⬍0.001 *Values are given as mean⫾SD or No. (%).
and guidelines, after they are initially tested and
implemented, is a common limitation of such
meth-ods aimed at standardizing medical practices.
35The
use of automated protocols using prompts and
re-quired inputs from bedside health-care providers
represents one strategy for ensuring more uniform
levels of protocol compliance over time.
36,37Another important limitation of this study is that
we only had experienced RCPs involved in
perform-ing patient assessments. This was purposely done to
obtain support for the performance of this study
from the admitting physicians. Therefore, these
re-sults may have differed if we had used
less-experi-enced individuals in this capacity. Additionally, the
numbers of treatments other than nebulizers and
metered-dose inhalers were small, limiting the
power of our results for those interventions. Lastly,
RCPs in the control arm of this study were not
impeded from communicating their clinical opinions
to the treating physicians. We did not track this
communication, nor did we monitor how often
phy-sicians deviated from the opinions of the RCPs in
firms B and C. A recent investigation suggests that
this may be an important barrier to the
implemen-tation of RCP-directed guidelines.
38In summary, the use of RCP-directed treatment
protocols decreased the overall use of respiratory
care and decreased respiratory care charges without
resulting in any detrimental clinical outcomes.
Pro-tocol-guided treatment represents an effective
strat-egy for standardizing medical practices and focusing
the efforts of health-care workers on specific tasks
needing to be performed in a timely manner.
Addi-tionally, protocols can serve as important educational
tools providing clinicians information on the
appro-priateness of various medical practices for specific
disease processes.
13However, the effective use of
protocol-directed therapies requires a dedicated
ef-fort on the part of the institution to ensure its
success. This implies that such protocols are
main-tained and updated on a regular basis to optimize
their clinical applicability, have adequate support
staff in place to perform the necessary treatments,
and do not impair or interfere with the ability of
clinicians to alter practices based on their own
experiences.
34,39References
1 Kollef MH. Outcomes research as a tool for defining the role of respiratory care practitioners in the ICU setting. New Horiz 1998; 6:91–98
2 Zibrak JD, Rossetti P, Wood E. Effect of reductions in respiratory therapy on patient outcomes. N Engl J Med 1986; 315:292–295
3 Celli BR, Rodriguez KS, Snider GL. A controlled trial of intermittent positive pressure breathing, incentive spirome-try, and deep breathing exercises in preventing pulmonary complications after abdominal surgery. Am Rev Respir Dis 1984; 130:12–15
4 Johnson D, Kelm C, To T, et al. Post-operative physical therapy after coronary artery bypass surgery. Am J Respir Crit Care Med 1995; 152:953–958
5 Hall JC, Tarala RA, Tapper J, et al. Prevention of respiratory complications after abdominal surgery: a randomized clinical trial. BMJ 1996; 312:148 –152
6 Alexander E, Weingarten S, Mohsenifar Z. Clinical strategies to reduce utilization of chest physiotherapy without compro-mising patient care. Chest 1996; 110:430 – 432
7 Dhand R, Jubran A, Tobin MJ. Bronchodilation delivery by metered-dose inhaler in ventilation-supported patients. Am J Respir Crit Care Med 1995; 151:1827–1833
8 Idris AH, McDermott MF, Raucci JC, et al. Emergency department treatment of severe asthma: metered-dose in-haler plus holding chamber is equivalent in effectiveness to nebulizer. Chest 1993; 103:665– 672
9 Colacone A, Afilalo M, Wolkove N, et al. A comparison of albuterol administered by metered dose inhaler (and holding chamber) or wet nebulizer in acute asthma. Chest 1993; 104:835– 841
10 Pilon CS, Leathley M, London R, et al. Practice guideline for arterial blood gas measurement in the intensive care unit decreases numbers and increases appropriateness of tests. Crit Care Med 1997; 25:1308 –1313
11 Kirby EG, Durbin CG Jr. Establishment of a respiratory assessment team is associated with decreased mortality in patients re-admitted to the ICU. Respir Care 1996; 41:903– 907
12 Stoller JK, Skibinski CI, Giles DK, et al. Physician-ordered respiratory care vs physician-ordered use of a respiratory therapy consult service: results of a prospective observational study. Chest 1996; 110:422– 429
13 Stoller JK, Mascha EJ, Kester L, et al. Randomized controlled trial of physician-directed versus respiratory therapy consult service-directed respiratory care to adult non-ICU inpatients. Am J Respir Crit Care Med 1998; 158:1068 –1075
14 Connors AF, Hammon WE, Martin RJ, et al. Chest physical Figure4. Box plots for respiratory care charges in patients with
and without discordant respiratory care orders. Boxes represent 25th to 75th percentiles, with 50th percentile (solid line) and mean (broken line) values shown within the boxes. The 10th and 90th percentiles are shown as capped bars, and closed circles mark the 5th and 95th percentiles.
therapy: the immediate effect on oxygenation in acutely ill patients. Chest 1980; 78:559 –564
15 Kollef MH. Prolonged use of ventilator circuits and ventila-tor-associated pneumonia: a model for identifying the optimal clinical practice. Chest 1998; 113:267–269
16 Stoller JK, Haney D, Burkhart J, et al. Physician-ordered respiratory care versus physician-ordered use of a respiratory therapy consult service: early experience at the Cleveland Clinic Foundation. Respir Care 1993; 38:1143–1154 17 Hilling L, Bakow E, Fink J, et al. Postural drainage therapy:
American Association for Respiratory Care practice guideline. Respir Care 1991; 36:1418 –1426
18 American Association for Respiratory Care. AARC clinical practice guideline: assessing response to bronchodilator ther-apy at point of care. Respir Care 1995; 40:1300 –1307 19 Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a
severity of disease classification system. Crit Care Med 1985; 13:818 – 829
20 Menzies R, Gibbons W, Goldberg P. Determinants of wean-ing and survival among patients with COPD who require mechanical ventilation for acute respiratory failure. Chest 1989; 95:398 – 405
21 Pingleton SK, Fagon JY, Leeper KV Jr. Patient selection for clinical investigation of ventilator-associated pneumonia: cri-teria for evaluating diagnostic techniques. Chest 1992; 102: 553S–556S
22 SAS Institute. SAS/STAT User’s Guide (vol 2). Cary, NC: SAS Institute, 1990; 1071–1126
23 Concato J, Feinstein AR, Holford TR. The risk of determin-ing risk with multivariable models. Ann Intern Med 1993; 118:201–210
24 Wood G, Macleod B, Moffatt S. Weaning from mechanical ventilation: physician-directed versus a respiratory-therapist-directed protocol. Respir Care 1995; 40:219 –224
25 Kollef MH, Shapiro SD, Silver P, et al. A randomized, controlled trial of protocol-directed versus physician-directed weaning from mechanical ventilation. Crit Care Med 1997; 25:567–574
26 Joiner GA, Salisbury D, Bollin GE. Utilizing quality assurance as a tool for reducing the risk of nosocomial ventilator-associated pneumonia. Am J Med Qual 1996; 11:100 –103 27 Kelleghan SI, Salemi C, Padilla S, et al. An effective
contin-uous quality improvement approach to the prevention of ventilator-associated pneumonia. Am J Infect Control 1993; 21:322–330
28 Goldberg R, Chan L, Haley P, et al. Critical pathway for the emergency management of acute asthma: effect on resource utilization. Ann Emerg Med 1998; 31:562–567
29 Ford RM, Phillips-Clar JE, Burns DM. Implementing ther-apist-driven protocols. Respir Care Clin North Am 1996; 2:51–76
30 Peterson WL, Cook DJ. Using a practice guideline for safely shortening hospital stay for upper gastrointestinal tract hem-orrhage. JAMA 1997; 278:2186 –2187
31 Grimshaw JM, Hutchinson A. Clinical practice guidelines: do they enhance value for money in health care? Br Med Bull 1995; 51:927–940
32 Clemmer TP, Spuhler VJ. Developing and gaining acceptance for patient care protocols. New Horiz 1998; 6:12–19 33 Horst HM, Mouro D, Hall-Jenssens RA, et al. Decrease in
ventilation time with a standardized weaning process. Arch Surg 1998; 133:483– 488
34 Clemmer TP, Spuhler VJ, Berwick DM, et al. Cooperation: the foundation of improvement. Ann Intern Med 1998; 128:1004 –1009
35 Pearson SD, Goulart-Fisher D, Lee TH. Critical pathway as a strategy for improving care: problems and potential. Ann Intern Med 1995; 123:941–948
36 Lobach DF. Electronically distributed, computer-generated, individual feedback enhances the use of a computerized practice guideline. Proc AMIA Annu Fall Symp 1996; 493– 497
37 Nilasena DS, Lincoln MJ. A computer-generated reminder system improves physician compliance with diabetes preven-tion care guidelines. Proc Annu Symp Comput Appl Med Care 1995; 640 – 645
38 Ely EW, Bennett PA, Bowton DL, et al. Large scale imple-mentation of a respiratory therapist-driven protocol for ven-tilator weaning. Am J Respir Crit Care Med 1999; 159:439 – 446
39 Thorens JB, Kaelin RM Jolliet P, et al. Influence of the quality of nursing on the duration of weaning from mechan-ical ventilation in patients with chronic obstructive pulmonary disease. Crit Care Med 1995; 23:1807–1815