To access the audio portion:
Dial:
866-832-6378
Pass Code:
61592208
Note: The webinar will be archived and hosted on
www.GuidelineAdvantage.org
within one week
1
"Management of Hyperglycemia in T2DM: Update on
the New ADA-EASD Position Statement"
Silvio E. Inzucchi, M.D.
Yale University School of Medicine
Professor of Medicine
New ADA-EASD Type 2 Diabetes
Treatment Guidelines
July 13, 2012
• Providers can use several different technology platforms
• Technology vendor collect clinical data for The Guideline Advantage
• Data are processed,
analyzed and sent back to the providers or medical practices
1
2
3
• Performance is measured,
Professionals can set measureable goals and chart improvements in performance
4
Program Model
• Flexible data extraction model working directly with platform
• Accepts data currently collected for other programs – “give us what you’ve got”
• Provides quarterly reports on data quality and performance feedback on treatment to guidelines
• Includes access to valuable ACS/ADA/AHA resources, including professional education and patient education materials
Future opportunities
•Allows physicians to participate in key research that will change healthcare
•Offers national recognition for the work physicians do each day
Benefits of Participation
Silvio E. Inzucchi, M.D.
Yale University School of Medicine
Professor of Medicine
8
Silvio E. Inzucchi MD
Yale University
New ADA-EASD Type 2 Diabetes
Treatment Guidelines
insulin 1950 1960 1970 1980 1990 2000 2010 9 8 7 6 5 4 3 2 1 Nu mbe r of Med ica tion Cl asse s 10
11
Hypertension & Diabetes:
Drug Classes* in U.S.
over Past Half-Century
Sulfonylureas Biguanides Angiotensin II receptor blockers ACE Inhibitors Ca+ channel blockers - blockers diuretics central -2 agonists peripheral -1 blockers adrenergic neuronal blockers Renin inhibitors vasodilators -glucosidase inhibitors Thiazolidinediones „Glinides GLP-1 Receptor Agonists DPP-4 inhibitors Amylinomimetics Biguanides Bile acid sequestrants Dopamine agonists
+
peripheral
glucose
uptake
hepatic
glucose
production
pancreatic
insulin
secretion
pancreatic
glucagon
secretion
Main Pathophysiological Defects in T2DM
gut
carbohydrate
delivery &
absorption
incretin
effect
HYPERGLYCEMIA
?
2008 ADA / EASD Consensus Algorithm
Nathan DM, et al. Diabetes Care. 2008;31:1
At Diagnosis:
Lifestyle +
Metformin Lifestyle + Metformin
+ Sulfonylureaa Lifestyle + Metformin + Basal Insulin Lifestyle + Metformin + Intensive Insulin Lifestyle + Metformin + Pioglitazone Lifestyle + Metformin + GLP-1 agonistb Lifestyle + Metformin + Basal Insulin Lifestyle + Metformin + Pioglitazone + Sulfonylureaa
STEP 1
STEP 2
STEP 3
Tier 2: Less well-validated therapies Tier 1: Well-validated therapies
Reinforce lifestyle changes at every visit and check A1C every 3 months until < 7.0%, then at least every 6 months thereafter. Change interventions whenever A1C ≥ 7.0%.
aSulfonylureas other than glibenclamide (glyburide) or chlorpropamide. bInsufficient clinical use to be confident regarding safety.
MET TZD 2 DPP4 1 AGI 3 A1C 6.5 – 7.5%** Monotherapy MET + GLP-1 or DPP4 1 TZD 2 Glinide or SU 5 TZD + GLP-1 or DPP4 1 MET + Colesevelam AGI 3 2 - 3 Mos.*** 2 - 3 Mos.*** 2 - 3 Mos.*** Dual Therapy MET + DPP4 or GLP-1 1,10 or TZD2 SU or Glinide 4,5 A1C 7.5 – 9.0% Dual Therapy 8 2 - 3 Mos.*** 2 - 3 Mos.*** Triple Therapy 9 MET + GLP-1 or DPP4 1 + TZD 2 Glinide or SU 4,7 MET + GLP-1 or DPP4 1 + TZD 2 GLP-1 or DPP41 + SU 7 TZD 2 A1C > 9.0% No Symptoms
Drug Naive Under Treatment
INSULIN ± Other Agent(s) 6 Symptoms INSULIN ± Other Agent(s) 6 INSULIN ± Other Agent(s) 6 Triple Therapy
AGI α-Glucosidase Inhibitor
DPP4 DPP-4 Inhibitor
GLP-1 Incretin Mimetic
Met Metformin
SU Sulfonylurea
TZD Thiazolidinedione FPG Fasting Plasma Glucose PPG Post-prandial Glucose A1C Goal ≤ 6.5%* MET + GLP-1 or DPP4 1 ± SU 7 TZD 2 GLP-1 or DPP4 1 ± TZD 2
Rodbard H et al. Endocrine Practice 2009
* May not be appropriate for all patients ** For patients with diabetes and A1C< 6.5,
pharmacologic Rx may be considered
*** If A1C goal not achieved safely
1 DPP4 if PPG and FBG or GLP-1 if
PPG
2 TZD if metabolic syndrome (MetS) and/or
non-alcoholic fatty liver disease (NAFLD)
3 AGI if PPG
4 Glinide if PPG or SU if FBG 5 Low dose secretagogue recommended 6 a) Discontinue insulin secretagogue with
multidose insulin b) Can use pramlintide with prandial insulin.
7 Decrease secretagogue by 50% when added
to GLP-1 or DPP-4
8 If A1c <8.5, combination Rx with agents that
cause hypoglycemia should be used with caution
9 If A1c> 8.5, in patients on Dual Therapy,
insulin should be considered
10 GLP-1 not approved for initial combination Rx INSULIN
± Other Agent(s) 6
HbA1c≥7.5%1 HbA 1c <7.5%1 Monitor HbA1c≥7.5%1 HbA 1c <7.5%1 Monitor
HbA1c≥6.5%1 after lifestyle trial
Metformin2 HbA1c ≥ 6.5%1 HbA
1c<6.5%1
Monitor
Add insulin2,8
(esp. if very hyperglycemic) Insulin + Metformin + SU4
1 Or individually agreed target.
2 With active dose titration.
3 See the NICE clinical guideline on obesity (www.nice.org.uk/CG43).
4 Offer once-daily sulfonylurea if adherence is a problem.
5 Only continue DPP-4 inhibitor or thiazolidinedione if reduction in HbA
1c
of at least 0.5 percentage points in 6 months.
6 Only continue exenatide if reduction in HbA
1c of at least 1 percentage point
and weight loss of at least 3% of initial body weight at 6 months.
Consider SU4 if:
• Not overweight3, or
• Metformin is not tolerated or contraindicated, or
• Rapid therapeutic response needed due to hyperglycemic symptoms. Consider glinide for people with erratic lifestyles.
Consider substituting DPP-4i9 or TZD10 for SU if significant risk of hypo-
glycemia (or its consequences) or SU contraindicated / not tolerated. Consider DPP-4i9 or TZD10 instead of insulin if insulin unacceptable (due to
employment, social, recreational, or other personal issues) Consider adding exenatide6 if:
•BMI ≥35, European descent7, & problems associated with high weight, or
•BMI <35 kg/m2 & insulin unacceptable because of occupational implications or
weight loss would benefit other comorbidities. Increase insulin dose & intensify regimen over time. Consider pioglitazone with insulin if:
• A TZD has previously had a marked glucose-lowering effect, or
• BG control is inadequate with high-dose insulin.
Metformin +SU4
National Institute for
Health and Clinical
Excellence (NICE)
TYPE 2 DIABETES
National clinical guideline for
management in primary &
secondary care (2009)
HbA1c ≥ 7.5%1 HbA 1c< 7.5%1 Monitor HbA1c≥7.5%1 HbA1c <7.5%1 Monitor HbA1c≥7.5%1 HbA 1c <7.5%1 Monitor
Consider adding DPP-4i9 or TZD10
if metformin contraindicated or not tolerated
HbA1c ≥ 6.5%1 HbA1c<6.5%1
Monitor
Sulfonylurea4
Metformin2 +DPP-4i5,9 or + TZD5,10
7 With adjustment for other ethnic
groups.
8 Continue with metformin and
sulfonylurea (and acarbose, if used), but only continue other drugs that are licensed for use with insulin. Review the use of sulfonylurea if hypoglycemia occurs. 9 DPP-4 inhibitor refers to sitagliptin or vidagliptin. 10 Thiazolidinedione refers to pioglitazone or rosiglitazone. SU4 +DPP-4i5,9 or + TZD5,10 HbA1c≥7.5%1 HbA1c <7.5%1 Monitor Metformin2 + SU4 + DPP4i5, or Metformin2 + SU4 + TZD5, 10, or Metformin2 + SU4 + GLP-1R agonist6 Start insulin2,8
National Institute for
Health and Clinical
Excellence (NICE
)
TYPE 2 DIABETES
National clinical guideline for
management in primary &
secondary care (2009)
Did We
Really
Need Another Guideline ?
1. Increasing number & variety of anti-hyperglycemic
agents.
2. New data re: benefits vs. risks of tight glycemic control.
3. Increasing concerns about drug safety.
4. Increasing discourse about personalized medicine and
‘patient
-
centered’ care.
5. Prior guidelines were consensus documents that did
not undergo formal Association review to become an
2010
2011
2012
ADA
EASD
ADA-EASD Organizational Meeting Teleconference #1 Teleconference #2 Live Meeting #1 (Washington, DC) Live Meeting #3 (Lisbon) (Draft 2.0) Writing GroupInvitations Draft Revisions
Literature Review
S O N D J F M A M J J A S O N D J
Live Meeting #2 (San Diego) (Draft 1.0) Writing Group Assignments2012
EASD
Live Meeting #3 (Lisbon) (Draft 2.0)S O N D J F M A M J
ADA-EASD Position Statement: Timeline
Hard copy publication Revisions Draft 5.4 to 25 Experts
Expert
Review
Teleconference #3 (Chairs) Revisions On-line publication Submission to journals (Draft 7.7)2011
PPC & POGS
Review
Exec Comms.
Review
Management of Hyperglycemia in Type 2
Diabetes: A Patient-Centered Approach
Position Statement of the American Diabetes Association (ADA) and
the European Association for the Study of Diabetes (EASD)
Diabetes Care 2012;35:1364–1379
Writing Group
American Diabetes Association Richard M. Bergenstal MD
Int’l Diabetes Center, Minneapolis, MN
John B. Buse MD, PhD
University of North Carolina, Chapel Hill, NC
Anne L. Peters MD
Univ. of Southern California, Los Angeles, CA
Richard Wender MD
Thomas Jefferson University, Philadelphia, PA
Silvio E. Inzucchi MD (co-chair)
Yale University, New Haven, CT
European Assoc. for the Study of Diabetes Michaela Diamant MD, PhD
VU University, Amsterdam, The Netherlands
Ele Ferrannini MD
University of Pisa, Pisa, Italy
Michael Nauck MD
Diabeteszentrum, Bad Lauterberg, Germany
Apostolos Tsapas MD, PhD
Aristotle University, Thessaloniki, Greece
David R. Matthews MD, DPhil (co-chair)
ADA-EASD Position Statement: Management of
Hyperglycemia in T2DM: A Patient-Centered Approach
1. PATIENT-CENTERED APPROACH
2. BACKGROUND
•
Epidemiology and health care impact•
Glycemic control & outcomes•
T2DM pathogenesis overview3. ANTIHYPERGLYCEMIC TX
•
Glycemic targets•
Therapeutic options- Lifestyle
- OAD s& non-insulin injectables - Insulin
•
Implementation Strategies- Initial drug therapy
- Advancing to dual combination tx - Advancing to triple combination tx - Transitions to / titrations of insulin
4. OTHER CONSIDERATIONS
• Age
•
Weight•
Sex/racial/ethnic/genetic differences•
Comorbidities (CAD, HF, CKD, LiverDisease, Hypoglycemia)
5. FUTURE DIRECTIONS /
RESEARCH NEEDS
Diabetes Care 2012;35:1364–1379 Diabetologia 2012;55:1577–1596ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
1. Patient-Centered Approach
“
...
providing care that is respectful of and responsive to
individual patient preferences, needs, and values - ensuring
that patient values guide all clinical decisions.”
•
Gauge patient’s preferred level of involvement.
•
Shared decision making
–
final decisions re: lifestyle choices
ultimately lies with the patient.
•
Explore, where possible, therapeutic choices.
•
Utilize decision aids.
Diabetes Care 2012;35:1364–1379
“We Need Minimally Disruptive Medicine”
The burden of treatment for many
people with complex, chronic,
comorbidities reduces their capacity
to collaborate in their care.
4 Principles
1. Establish the weight of burden.
2. Encourage coordination in
clinical practice.
3. Acknowledge comorbidity in
clinical evidence.
4. Prioritize from the
patient
perspective.
Impact of Intensive Therapy for Diabetes:
Summary of Major Clinical Trials
Study
Microvasc
CVD
Mortality
UKPDS
DCCT / EDIC*
ACCORD
ADVANCE
VADT
Long Term Follow-up Initial Trial
* in T1DM
Kendall DM, Bergenstal RM. © International Diabetes Center 2009
UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:854.
Holman RR et al. N Engl J Med. 2008;359:1577. DCCT Research Group. N Engl J Med 1993;329;977.
Nathan DM et al. N Engl J Med. 2005;353:2643. Gerstein HC et al. N Engl J Med. 2008;358:2545. Patel A et al.N Engl J Med 2008;358:2560. Duckworth W et al. N Engl J Med 2009;360:129. (erratum: Moritz T. NEnglJMed 2009;361:1024)
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
3. ANTI-HYPERGLYCEMIC THERAPY
•
Glycemic targets
-
HbA1c < 7.0%
(mean PG 150-160
mg/dl
[8.3-8.9
mmol/l
])
-
Pre-prandial PG <130
mg/dl
(7.2
mmol/l
)
-
Post-prandial PG <180
mg/dl
(10.0
mmol/l
)
-
Individualization
is key:
Tighter targets (6.0 - 6.5%) - younger, healthier
Looser targets (7.5 - 8.0%
+
) - older, comorbidities,
hypoglycemia prone, etc.
-
Avoidance of hypoglycemia
Most Intensive Less Intensive Least Intensive
Patient Age
Disease Duration
40 45 50 55 60 65 70 75 5 10 15 20Other Comorbidities
None Few/Mild Multiple/Severe
Hypoglycemia Risk
Low Moderate High
8.0%
6.0%
7.0%
Established Vascular Complications
None
Early Micro Advanced Micro
Psychosocioeconomic Considerations
Highly Motivated, Adherent, Knowledgeable,
Excellent Self-Care Capacities, & Comprehensive Support Systems
Less motivated, Non-adherent, Limited insight, Poor Self-Care Capacities,
& Weak Support Systems
Cardiovascular
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
3. ANTI-HYPERGLYCEMIC THERAPY
•
Therapeutic options: Lifestyle
-
Weight optimization
-
Healthy diet
-
Increased activity level
Diabetes Care 2012;35:1364–1379
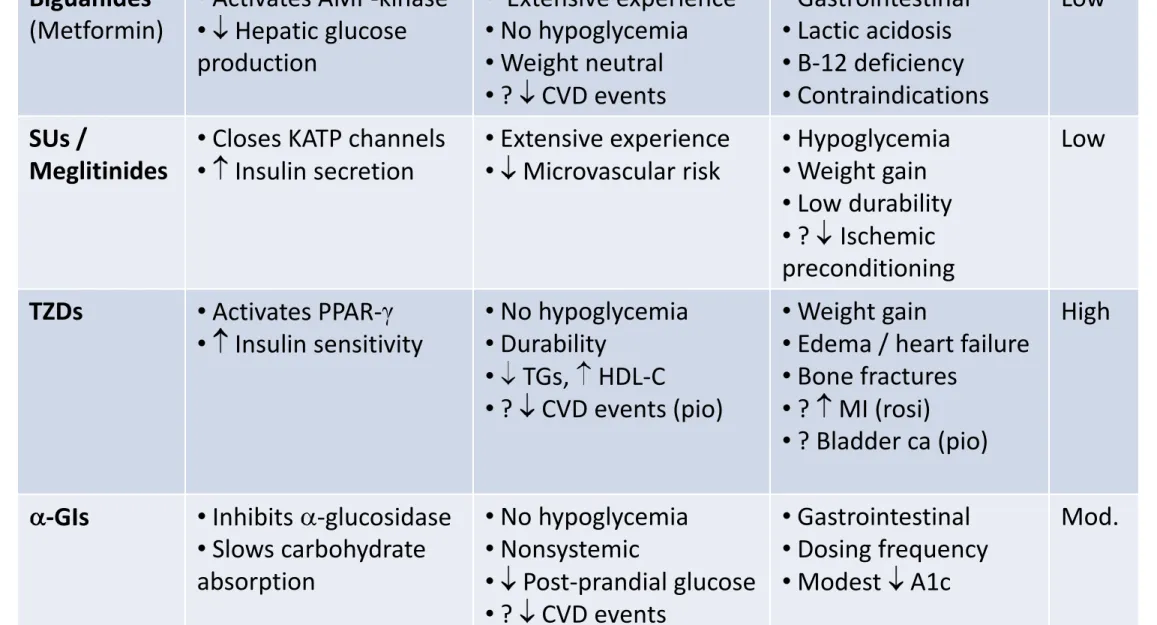
Class
Mechanism
Advantages
Disadvantages
Cost
Biguanides (Metformin) • Activates AMP-kinase • Hepatic glucose production • Extensive experience • No hypoglycemia • Weight neutral • ? CVD events • Gastrointestinal • Lactic acidosis • B-12 deficiency • Contraindications Low SUs / Meglitinides• Closes KATP channels
• Insulin secretion • Extensive experience • Microvascular risk • Hypoglycemia • Weight gain • Low durability • ? Ischemic preconditioning Low TZDs • Activates PPAR- • Insulin sensitivity • No hypoglycemia • Durability • TGs, HDL-C • ? CVD events (pio) • Weight gain
• Edema / heart failure
• Bone fractures
• ? MI (rosi)
• ? Bladder ca (pio)
High
-GIs • Inhibits -glucosidase
• Slows carbohydrate absorption • No hypoglycemia • Nonsystemic • Post-prandial glucose • ? CVD events • Gastrointestinal • Dosing frequency • Modest A1c Mod.
Class
Mechanism
Advantages
Disadvantages Cost
DPP-4 inhibitors • Inhibits DPP-4 • Increases GLP-1, GIP • No hypoglycemia • Well tolerated • Modest A1c • ? Pancreatitis • Urticaria High GLP-1 receptor agonists • Activates GLP-1 receptor • Insulin, glucagon • gastric emptying • satiety • Weight loss • No hypoglycemia• ? Beta cell mass
• ? CV protection • GI • ? Pancreatitis • Medullary ca • Injectable High Amylin mimetics
• Activates amylin receptor
• glucagon • gastric emptying • satiety • Weight loss • Post-prandial glucose • GI • Modest A1c • Injectable • Hypo w/ insulin • Dosing frequency High Bile acid sequestrants
• Binds bile acids
• Hepatic glucose production • No hypoglycemia • Nonsystemic • LDL-C • GI • Modest A1c • TGs • Dosing frequency High Dopamine-2 agonists • Activates DA receptor • Modulates hypothalamic control of metabolism • Insulin sensitivity • No hypoglycemia • ? CVD events • Modest A1c • Dizziness/syncope • Nausea • Fatigue High
Class
Mechanism
Advantages
Disadvantages
Cost
Insulin • Activates insulin
receptor • Glucose disposal • Hepatic glucose production • Universally effective • Unlimited efficacy • Microvascular risk • Hypoglycemia • Weight gain • ? Mitogenicity • Injectable • Training requirements • “Stigma” Variable
©2011 by American College of Physicians
Figure 1. Pooled between-group differences in HbA1c level
with monotherapy and combination therapies
140 head-to-head trials+26 observational studies of mono, combo therapy with intermed./ long-term clinical outcomes and harms reported
Bennett WL, et al. Ann Intern Med 2011;154:602
Agency for Healthcare Research & Quality:
©2011 by American College of Physicians
Figure 2. Pooled between-group difference in body weight
with monotherapy and combination therapies
Bennett WL, et al. Ann Intern Med 2011;154:602
Agency for Healthcare Research & Quality:
©2011 by American College of Physicians
Figure 4. Pooled odds of mild or moderate hypoglycemia
with monotherapy and combination therapies.
Agency for Healthcare Research & Quality:
Comparative Effectiveness & Safety of T2DM Medications
Bennett WL, et al. Ann Intern Med 2011;154:602
“
Evidence on long-term clinical outcomes
(all-cause
mortality, cardiovascular disease, nephropathy, and
neuropathy)
was of low strength or insufficient. Most
medications decreased A1c level by about 1% and most
2-drug combinations produced similar reductions.”
“Evidence supports
metformin as a first-line
agent to treat
T2DM. Most 2-drug combinations similarly reduce A1c
levels, but some increased risk for hypoglycemia and other
adverse events.”
Diabetes Care 2012;35:1364–1379
Diabetes Care 2012;35:1364–1379
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Age: Older adults
-
Reduced life expectancy
-
Higher CVD burden
-
Reduced GFR
-
At risk for adverse events from polypharmacy
-
More likely to be compromised from hypoglycemia
Less ambitious targets
HbA1c <7.5
–
8.0% if tighter targets
not easily achieved
Focus on drug safety
Diabetes Care 2012;35:1364–1379
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Weight
-
Majority of T2DM patients overweight / obese
-
Intensive lifestyle program
-
Metformin
-
GLP-1 receptor agonists
-
? Bariatric surgery
-
Consider LADA in lean patients
Diabetes Care 2012;35:1364–1379
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Sex/ethnic/racial/genetic differences
-
Little is known
-
MODY & other monogenic forms of diabetes
-
Latinos: more insulin resistance
-
East Asians: more beta cell dysfunction
-
Gender may drive concerns about adverse effects
(e.g., bone loss from TZDs)
Diabetes Care 2012;35:1364–1379
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Comorbidities
-
Coronary Disease
-
Heart Failure
-
Renal disease
-
Liver dysfunction
-
Hypoglycemia
Metformin: CVD benefit (UKPDS)
Avoid hypoglycemia
? SUs & ischemic preconditioning
? Pioglitazone &
CVD events
? Effects of incretin-based
therapies
Diabetes Care 2012;35:1364–1379
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Comorbidities
-
Coronary Disease
-
Heart Failure
-
Renal disease
-
Liver dysfunction
-
Hypoglycemia
Diabetes Care 2012;35:1364–1379 Diabetologia 2012;55:1577–1596
Metformin: May use unless
condition is unstable or severe
Avoid TZDs
? Effects of incretin-based
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Comorbidities
-
Coronary Disease
-
Heart Failure
-
Renal disease
-
Liver dysfunction
-
Hypoglycemia
Diabetes Care 2012;35:1364–1379 Diabetologia 2012;55:1577–1596
Increased risk of hypoglycemia
Metformin & lactic acidosis
US: stop
@SCr
≥ 1.5 (1.4 women)
UK: half-dose
@GFR < 45 &
stop
@GFR < 30
Caution with SUs (esp. glyburide)
DPP-4-
i’s –
dose adjust for most
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Comorbidities
-
Coronary Disease
-
Heart Failure
-
Renal disease
-
Liver dysfunction
-
Hypoglycemia
Diabetes Care 2012;35:1364–1379 Diabetologia 2012;55:1577–1596
Most drugs not tested in advanced
liver disease
Pioglitazone may help steatosis
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
4. OTHER CONSIDERATIONS
•
Comorbidities
-
Coronary Disease
-
Heart Failure
-
Renal disease
-
Liver dysfunction
-
Hypoglycemia
Diabetes Care 2012;35:1364–1379 Diabetologia 2012;55:1577–1596
Emerging concerns regarding
association with
increased
morbidity / mortality
Proper drug selection is key in
Guidelines for Glucose, BP, & Lipid Control
American Diabetes Assoc. Goals
HbA1C
< 7.0%
(individualization)
Preprandial
glucose
70-130
mg/dL (3.9-7.2 mmol/l)
Postprandial
glucose
< 180
mg/dL
Blood pressure
< 130/80
mmHg
Lipids
LDL: < 100
mg/dL (2.59 mmol/l)
< 70
mg/dL (1.81 mmol/l)
(with overt CVD)
HDL: > 40
mg/dL (1.04 mmol/l)
> 50
mg/dL (1.30 mmol/l)
TG: < 150
mg/dL (1.69 mmol/l)
ADA. Diabetes Care 2012;35:S11–S63 HDL = high-density lipoprotein; LDL = low-density
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
KEY POINTS
•
Glycemic targets & BG-lowering therapies must be individualized.
•
Diet, exercise, & education: foundation of any T2DM therapy program
•
Unless contraindicated, metformin = optimal 1st-line drug.
•
After metformin, data are limited. Combination therapy with 1-2 other
oral / injectable agents is reasonable; minimize side effects.
•
Ultimately, many patients will require insulin therapy alone / in
combination with other agents to maintain BG control.
•
All treatment decisions should be made in conjunction with the patient
(focus on preferences, needs & values.)
•
Comprehensive CV risk reduction - a major focus of therapy.
Diabetes Care 2012;35:1364–1379
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
Contrasts to 2008 ADA-EASD Treatment Algorithm
•
Not as prescriptive / algorithmic
•
Calibration of treatment targets to patient needs
•
Acknowledgement of the role of lifestyle change
prior
to
metformin (in selected patients)
•
Individualization of treatment options
•
Harmonization of 5 dual therapy options
after
metformin
•
Recognition of role for initial combination therapy (A1c>9%)
•
Endorsement of triple therapy, when required
ADA-EASD Position Statement: Management of Hyperglycemia in T2DM
Invited Reviewers
Professional Practice Committee, American Diabetes Association
Panel for Overseeing Guidelines and Statements, European Association for the Study of Diabetes American Association of Diabetes Educators
The Endocrine Society American College of Physicians James Best, The University of Melbourne, Australia
Henk Bilo, Isala Clinics, Zwolle, Netherlands
John Boltri, Wayne State University, Detroit, MI
Thomas Buchanan, Univ of So California, LA, CA
Paul Callaway, University of Kansas,Wichita, KS
Bernard Charbonnel, University of Nantes, France
Stephen Colagiuri, The University of Sydney, Australia
Samuel Dagogo-Jack, Univ of Tenn, Memphis, TN
Margo Farber, Detroit Medical Center, Detroit, MI
Cynthia Fritschi, University of Illinois, Chicago, IL
Rowan Hillson, Hillingdon Hospital, Uxbridge, U.K.
Faramarz Ismail-Beigi, CWR Univ, Cleveland, OH
Devan Kansagara, Oregon H&S Univ, Portland, OR
Ilias Migdalis, NIMTS Hospital, Athens, Greece
Donna Miller, Univ of So California, LA, CA
Robert Ratner, MedStar/Georgetown Univ, DC
Julio Rosenstock, Dallas Diab/Endo Ctr, Dallas, TX
Guntram Schernthaner, Rudolfstiftung Hosp, Vienna, Austria
Robert Sherwin, Yale University, New Haven, CT
Jay Skyler, University of Miami, Miami, FL
Geralyn Spollett, Yale University, New Haven, CT
Ellie Strock, Int’l Diabetes Center, Minneapolis, MN
Agathocles Tsatsoulis, University of Ioannina, Greece
Andrew Wolf, Univ of Virginia Charlottesville, VA
Type question into the Q&A tab at the top of your screen.
Additional questions email
laura.jansky@heart.org
Download this slide deck within 5-7 working days from:
GuidelineAdvantage.org
Questions?
Join us August 21st for our next webinar:
“Cardiovascular Risk Reduction in People with Type 2 Diabetes” Presented by Dr. Jay Shubrook
Find registration information online at: GuidelineAdvantage.org
The Guideline Advantage will be attending the following conferences:
•eHI National Forum on Data Analytics in National Harbor, MD August 9, 2012
•Community Health Institute (CHI) and Expo in Orlando, FL September 9-12, 2012
•AAFP‟s Scientific Assembly in Philadelphia, PA October 18-20, 2012
For more information please contact Laura Jansky at laura.jansky@heart.org
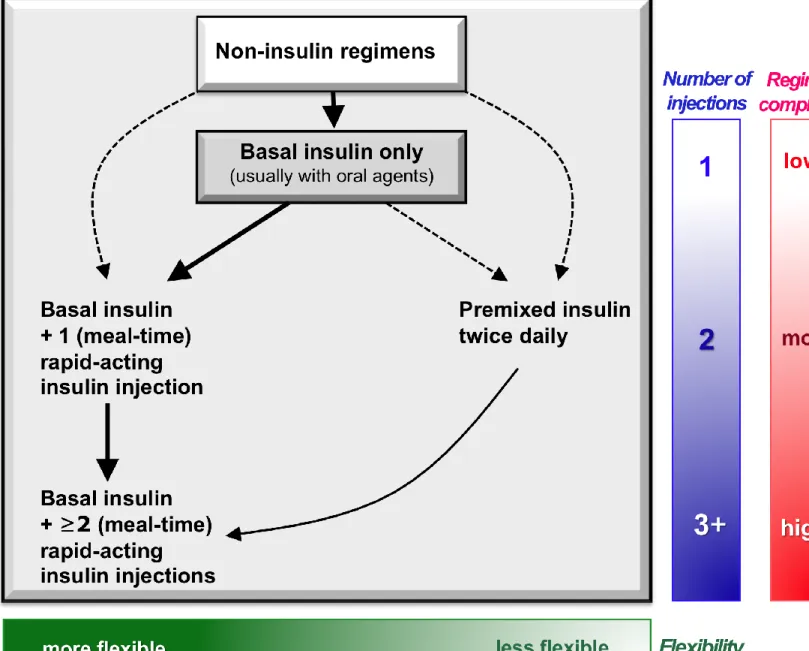
![Figure 1 Diabetes Care, Diabetologia. 19 April 2012 [Epub ahead of print]](https://thumb-us.123doks.com/thumbv2/123dok_us/1835153.2765712/26.1170.159.997.61.764/figure-diabetes-diabetologia-april-epub-ahead-of-print.webp)
![Figure 1 Diabetes Care, Diabetologia. 19 April 2012 [Epub ahead of print]](https://thumb-us.123doks.com/thumbv2/123dok_us/1835153.2765712/28.1170.159.997.61.764/figure-diabetes-diabetologia-april-epub-ahead-of-print.webp)