2001-2010
We firmly believe that knowledge is the key to patient safety.
Physical Therapy Liability
Contents
PART ONE: CNA HealthPro Physical Therapy Closed Claims Analysis . . . . 5
Introduction . . . . 7
Purpose . . . . 7
Database and Methodology . . . . 7
Scope . . . . 8
Terms . . . . 8
General Data Analysis . . . . 9
Analysis of Closed Claims by Insurance Source . . . 9
Severity of Physical Therapist Closed Claims by Year Closed . . . 10
Distribution of Closed Claims by Severity . . . 11
Analysis of Severity by Location . . . 12
Analysis of Severity by Allegation . . . . 13
Allegations by Category . . . 13
Allegations Related to Improper Management over the Course of Treatment . . . 14
Allegations Related to Failure to Monitor or Supervise. . . 15
Physical Therapy Closed Claim Scenario: Failure to Properly Monitor or Supervise . . . . 15
Allegations Related to Improper Performance Using Therapeutic Exercise . . . 16
Physical Therapy Closed Claim Scenario: Improper Performance Using Therapeutic Exercise . . . . 17
Allegations Related to Improper Performance of Manual Therapy . . . 17
Allegations Related to Inappropriate Behavior by Physical Therapist . . . 18
Allegations Related to Equipment . . . 19
Allegations Related to Improper Use of a Physical Agent . . . 19
Physical Therapy Closed Claim Scenario: Improper Use of a Physical Agent . . . . 20
Analysis of Severity by Injury . . . . 20
Comparison of Re-injury Versus Other Injuries . . . 22
Analysis of Severity by Re-injury . . . 23
Analysis of Re-injury by Affected Body Part . . . 23
Allegations Related to Re-injury . . . 24
Analysis of Claims Related to Burns . . . 26
Analysis of Severity Related to Burns by Body Part . . . 26
Analysis of Severity by Disability . . . 27
Summary Analysis of Physical Therapist Assistant Closed Claims . . . . 28
Severity by Allegation . . . 28
PTA and PT Closed Claims: Comparison of Top Three Elements by Severity . . . 29
Physical Therapy Closed Claim Scenario: Alleged Improper Care (a Success Story) . . . . 30
Risk Control Recommendations . . . . 31
Risk Control Self-assessment Checklist for Physical Therapists . . . . 36
PART TWO: Healthcare Providers Service Organization Analysis of Physical Therapy
License Protection Paid Claims January 1, 2001–December 31, 2010 . . . . 41
Introduction . . . . 43
Scope . . . . 43
Database and Methodology . . . . 43
License Protection Paid Claims . . . . 43
Claims by Insurance Coverage Type . . . 43
Claims by Licensure Type . . . 44
Claims by Location . . . 44
Allegations by Class . . . 45
Allegations Related to Improper Management over the Course of Treatment . . . 46
Allegations Related to Inappropriate Behavior . . . 47
Allegations Related to Fraudulent Billing . . . 48
Licensing Board Outcomes . . . 49
Recommendations . . . . 50
PART THREE: Highlights from Healthcare Providers Service Organization
2011 Qualitative Physical Therapist Work Profile Survey . . . . 51
Introduction . . . . 53
Survey Background and Methodology . . . . 53
Summary of Findings . . . . 55
Topic 1: Respondent Demographics . . . . 56
Physical Therapy Licensure . . . 56
Gender . . . 56
Age . . . 56
Highest Level of Education . . . 57
Topic 2: Practice Profile . . . . 58
Location of Practice . . . 58
Primary Language . . . 58
Annual Continuing Education (CE) Requirements . . . 59
Topic 3: About the Claim Submitted . . . . 60
Seeking PT Without a Referral . . . 60
Years of Practice at Time of Incident . . . 60
PART ONE
CNA HealthPro Physical Therapy
Closed Claims Analysis
PART ONE: Introduction
Through Healthcare Providers Service Organization (HPSO), CNA continues to be the nation’s largest underwriter of professional liability insurance coverage for physical therapy professionals, with over 70,000 policies in force in 2011. In collaboration with our business partners at HPSO, we at CNA are dedicated to educating physical therapy professionals regarding professional liability risk exposures relevant to their practice. Part One of this report focuses on risks faced by physical therapists (PTs), whether they are insured as individuals or as employees of physical therapy practices. A subsection of Part One addresses the specific professional liability risk exposures for physical therapist assistants (PTAs) insured by HPSO/ CNA and other healthcare professionals providing services on behalf of a HPSO/CNA-insured physical therapy practice.
Purpose
We firmly believe that knowledge is the key to enhancing patient safety and managing risk. Our goal is to help PTs enhance the quality of their patient care services by providing fact-based risk management information and guidance. The risk management information presented in this report is based upon an analysis of closed professional liability claims that resulted in sizable settlements or adverse judgments. Part One focuses on closed claims in order to identify the types of incidents most likely to have resulted in significant consequences for patients, therapists and practices. By offering data analysis, risk control recommendations and a self-assessment checklist, we strive to encourage our insureds to examine their own clinical practice and policies, discern areas of possible improvement, and dedicate themselves to maximizing patient safety and minimizing risk. We believe that physical therapy professionals in every type of practice setting will find this report a valuable educational resource.
Database and Methodology
There were 3,889 professional liability closed claims and incidents attributed to CNA-insured physical therapy professionals in the HPSO program from 2001 through 2010. Professional liability claims were included in the final data set only if they
-
involved a licensed PT or PTA whether insured independently or through a PT practice or other healthcare professional providing services on behalf of a PT practice-
resulted in a closure date between January 1, 2001 and December 31, 2010-
resulted in an indemnity payment equal to or greater than $10,000Closed claims with an indemnity payment of less than $10,000 were excluded for the reason that they typically reflect injuries that were less severe and/or resolved without extensive litigation.
These criteria generated a data set of 552 closed claims. There were 477 closed claims asserted against PTs, 49 closed claims asserted against PTAs and 26 closed claims asserted against other healthcare pro- fessionals providing services on behalf of an insured PT practice. Findings for closed claims asserted against PTs or PTAs insured as individuals or by a PT practice, and against other healthcare professionals insured by a PT practice, are summarized in Figure 1 and Figure 2 (page 9). Findings for all closed claims meeting the criteria noted above and asserted against PTAs are summarized in Figure 23 and Figure 24 (pages 28 and 29). The methodology used in this report differs from the 2007 CNA Physical Therapy Claims Study and PT claims studies developed by other organizations. For that reason, it is not advisable
Scope
Claim characteristics analyzed within the report include incident location, allegation, injury, re-injury and related disability. Also included is a summary review of closed claims comparing individually insured PTs with PTs providing services as employees of insured PT practices.
Noted indemnity payments or expenses were paid by CNA on behalf of an insured and do not represent any additional amounts paid by employers, other insurers or other parties in the form of direct or insur-ance payments. This analysis reflects CNA data only and is not necessarily representative of all closed claims for PTs, PTAs and/or PT practices.
The process of resolving a professional liability claim may take several years. Therefore, claims included in this report may have resulted from events that occurred prior to 2001, as long as the claim closed between January 1, 2001 and December 31, 2010.
Terms
For purposes of this report, please refer to the definitions below:
-
Allegation – An assertion that the professional or organization has done something wrong or illegal, which has not yet been proven.-
Expense payment – Monies paid by CNA in the investigation, management or defense of a claim.-
Incurred – Costs or financial obligations, including indemnity payments and expense payments,resulting from the management and resolution of a claim.
-
Indemnity payment – Monies paid by CNA to a plaintiff on behalf of an insured in the settlement or judgment of a claim.-
Physical therapy practice (PT practice) – An organization insured through the HPSO/CNA physical therapy program that provides professional physical therapy services and whose employees may include PTs, PTAs, PT aides, massage therapists, athletic trainers and other healthcare providers.-
Referring practitioner – A licensed independent healthcare provider other than a PT – such as aphysician, dentist, advanced practice nurse, physician assistant, podiatrist or chiropractor – who is authorized to prescribe physical therapy treatments.
General Data Analysis
ANALySIS OF CLOSED CLAIMS By INSuRANCE SOuRCE
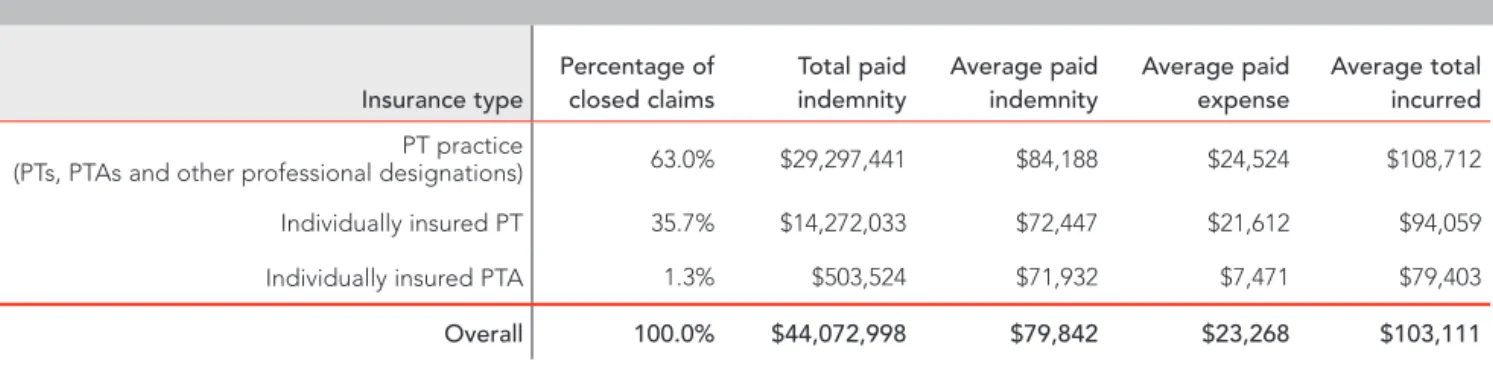
Figure 1 provides an overview of claim results based upon the type of insurance coverage. The first row describes claim results for PTs, PTAs and other healthcare providers who received their coverage through a PT practice. The second and third rows describe claim results of PTs and PTAs who were individually insured. This is the only chart that includes all 552 claims in the database. Figure 2 provides additional detail regarding the PT practices data reported in Figure 1.
-
The highest average paid indemnity and the highest average paid expenses involved PT practices. This result is expected, inasmuch as the coverage provided for a PT practice is the primary source (i.e., first dollar) of insurance coverage for the corporation, its employees and independent contractors. Conversely, individually insured PTs and PTAs may share financial responsibility with an employer, healthcare facility or others.-
Individually insured PTAs had an average paid indemnity similar to that of individually insured PTs.-
PTs experienced 80.5 percent of the closed claims within PT practices.-
The average paid indemnity for individually insured PTs (Figure 1) was $11,966 lower than for practice-insured PTs (Figure 2), while the average paid expense was $2,532 lower than for practice-practice-insured PTs. Therefore, the average total incurred was $14,498 less for PTs with their own individual coverage than for PTs receiving coverage through a PT practice.Claims by Insurance Source for All Physical Therapy Professionals
Chart reflects closed claims with paid indemnity of ≥ $10,000
1
Insurance type Percentage of closed claims Total paid indemnity Average paid indemnity Average paid expense Average total incurred PT practice(PTs, PTAs and other professional designations) 63.0% $29,297,441 $84,188 $24,524 $108,712
Individually insured PT 35.7% $14,272,033 $72,447 $21,612 $94,059
Individually insured PTA 1.3% $503,524 $71,932 $7,471 $79,403
Overall 100 .0% $44,072,998 $79,842 $23,268 $103,111
Claims by Providers Insured by a PT Practice
Chart reflects closed claims with paid indemnity of ≥ $10,000
2
Provider Percentage of practice-insured closed claims Total paid indemnity Average paid indemnity Average paid expense Average total incurred Athletic trainer 0.3% $350,000 $350,000 $23,521 $373,521 PT aide 6.6% $2,051,182 $89,182 $25,271 $114,453 PT 80.5% $23,635,663 $84,413 $24,144 $108,557 PTA 12.1% $3,210,596 $76,443 $26,962 $103,405 Massage therapist 0.6% $50,000 $25,000 $18,386 $43,386 Overall 100 .0% $29,297,441 $84,188 $24,524 $108,712SEvERITy OF PHySICAL THERAPIST CLOSED CLAIMS By yEAR CLOSED
-
While average paid indemnity varied considerably from year to year, the overall trend increased approximately 4 to 5 percent annually (as represented by the trend line) over the course of the 10-year period of the analysis.-
The increases in 2004 and 2009 were based on the high number of closed claims with paid indemnity equal to or greater than $200,000.3
Average Paid Indemnity and Average Paid Expense by year Closed
Chart reflects closed claims with paid indemnity of ≥ $10,000
Average paid by year closed 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010
Figure 4 displays average paid expenses for PT closed claims that closed with no indemnity payment. The data include closed claims with paid expenses of one dollar or greater for each of the 10 years included in the analysis.
A claim that resolved without an indemnity payment may incur costs associated with managing the claim. These costs, or claim expenses, include such items as attorney fees and costs incurred to investigate the claim. Claim expenses can vary due to the unique and sometimes complicated circumstances of each claim. While some individual claim expenses in these data exceeded $100,000, the 10-year average annual
Please note that from this point forward, the analysis solely reflects PT closed claims . Data inclusion and
exclusion criteria are explained on page 7 .
Average Paid Expenses for Closed Claims with No Indemnity Paid by year Closed
4
Average paid expenses 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010
DISTRIBuTION OF CLOSED CLAIMS By SEvERITy
-
Approximately 80 percent of the PT closed claims were resolved with an indemnity payment under $100,000.-
Only 0.4 percent of the PT closed claims incurred the policy limit of $1 million. These claims reflect treatment that resulted in severe injury and irreversible harm to the patient.Distribution of Closed Claims by Severity
Chart reflects closed claims with paid indemnity of ≥ $10,000
5
Paid indemnity Percentage of closed claims
$10,000 to $99,999 $100,000 to $249,999 $250,000 to $499,999 $500,000 to $749,999 $750,000 to $999,999 $1,000,000
SEvERITy OF PHySICAL THERAPIST CLOSED CLAIMS By yEAR CLOSED
-
While average paid indemnity varied considerably from year to year, the overall trend increased approximately 4 to 5 percent annually (as represented by the trend line) over the course of the 10-year period of the analysis.-
The increases in 2004 and 2009 were based on the high number of closed claims with paid indemnity equal to or greater than $200,000.3
Average Paid Indemnity and Average Paid Expense by year Closed
Chart reflects closed claims with paid indemnity of ≥ $10,000
Average paid by year closed 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010
Figure 4 displays average paid expenses for PT closed claims that closed with no indemnity payment. The data include closed claims with paid expenses of one dollar or greater for each of the 10 years included in the analysis.
A claim that resolved without an indemnity payment may incur costs associated with managing the claim. These costs, or claim expenses, include such items as attorney fees and costs incurred to investigate the claim. Claim expenses can vary due to the unique and sometimes complicated circumstances of each claim. While some individual claim expenses in these data exceeded $100,000, the 10-year average annual expense where there is no associated indemnity payment is $13,710. The claims included in this chart represent PT professional liability matters that were resolved as follows:
-
successfully defended on behalf of the PT, resulting in a favorable jury verdict-
abandoned by the plaintiff during the investigative or discovery process-
dismissed in favor of the defendant PT by the court prior to trialANALySIS OF SEvERITy By LOCATION
-
The highest average paid indemnity resulted from closed claims that occurred in hospital inpatient PT areas. The high average paid indemnity for this complement of closed claims was driven by one claim that closed at the policy limit of $1 million.-
The highest total paid indemnity resulted from closed claims that occurred in PT offices or clinics, followed by patient homes and hospital inpatient PT areas.6
Analysis of Severity by Location
Chart reflects closed claims with paid indemnity of ≥ $10,000
Location Percentage of closed claims Total paid indemnity Average paid indemnity
Hospital inpatient PT area 1.9% $1,779,000 $197,667
Fitness center 0.2% $96,500 $96,500
Aging services facility 2.3% $973,911 $88,537
Acute medical/surgical hospital inpatient 1.0% $400,471 $80,094 PT office/clinic - non-hospital 82.0% $30,764,890 $78,683
Industrial/occupational health 0.2% $75,000 $75,000
School 2.7% $921,175 $70,860
Patient home 8.4% $2,716,749 $67,919
Acute rehabilitation hospital inpatient room/area 0.2% $50,000 $50,000
Hospital outpatient area 0.8% $115,000 $28,750
Practitioner office or private clinic 0.2% $15,000 $15,000
Overall 100 .0% $37,907,696 $79,471
The highest
average paid indemnity
resulted from closed claims that occurred in
hospital inpatient PT areas, while the highest
Analysis of Severity by Allegation
The analysis of allegations begins with Figure 7, which includes data for allegations by category. More detailed reviews are provided for categories of allegations that accounted for 5 percent or more of the PT closed claims. These categories include
-
improper management over the course of treatment, Figure 8-
failure to supervise or monitor, Figure 9-
improper performance using therapeutic exercise, Figure 10-
improper performance of manual therapy, Figure 11-
inappropriate behavior by the physical therapist, Figure 12-
equipment-related, Figure 13-
improper performance using a physical agent, Figure 14ALLEGATIONS By CATEGORy
-
Failure to properly test or treat the patient reflected the highest average paid indemnity, but accounted for less than 1 percent of the PT closed claims. Some examples of failure to properly test or treat the patient included-
using excessive weight when testing patient functional capacity-
extending traction beyond acceptable traction time periods-
including improper exercises in the patient’s treatment plan-
advancing the patient’s treatment plan too rapidly-
Examples of “environment of care” included equipment not mounted properly on the wall and cluttered treatment area resulting in patient falls.-
Improper performance using therapeutic exercise had the highest total paid indemnity at $10,600,774. The total paid indemnity was driven by how often this allegation occurred. This allegation category accounts for 26.6 percent of the PT closed claims.Severity of Allegations by Category
Chart reflects closed claims with paid indemnity of ≥ $10,000
7
Allegation category Percentage of closed claims Total paid indemnity Average paid indemnityFailure to properly test or treat 0.8% $1,893,805 $473,451 Improper management over the course of treatment 11.3% $6,459,346 $119,618
Environment of care 1.5% $636,792 $90,970
Failure to supervise or monitor 15.9% $6,508,342 $85,636 Improper performance using therapeutic exercise 26.6% $10,600,774 $83,471 Improper performance of manual therapy 14.0% $5,360,466 $80,007
Inappropriate behavior by PT 5.7% $1,537,018 $56,927
Equipment-related 6.7% $1,576,538 $49,267
Improper performance using a physical agent 17.4% $3,334,615 $40,176
Figures 8 through 14 examine in detail the categories of allegations that accounted for 5 percent or more of all
the PT closed claims . They are organized from highest to lowest average paid indemnity, as listed in Figure 7 .
The percentages are based on the number of claims for the specific category .
ALLEGATIONS RELATED TO IMPROPER MANAGEMENT OvER THE COuRSE OF TREATMENT
-
This allegation category produced the following findings:-
The average paid indemnity of $119,618 for closed claims was 50 percent higher than the average paid indemnity of $79,471 for all PT closed claims.-
Failure to report changes in the patient’s condition to the referring practitioner represented the highest average paid indemnity .-
Failure to cease treatment when the patient experienced excessive/unexpected pain constituted the highest total paid indemnity .-
Example of improper management of a surgical patient: A middle-aged man had undergone a hip arthroscopy and was referred for physical therapy by his surgeon. The patient canceled several ses- sions for vague reasons, and did not return to continue therapy. He reported to his surgeon that the PT had placed him prone, flexed his knee and extended his hip. The patient and surgeon alleged that, as a result of this therapy, the patient’s hip was dislocated, requiring additional surgery. The claim was settled for over $200,000.8
Severity by Allegations Related to Improper Management over the Course of Treatment
Chart reflects closed claims with paid indemnity of ≥ $10,000
Allegation Percentage of closed claims Total paid indemnity Average paid indemnity
Failure to report patient’s condition to referring practitioner 9.3% $1,397,125 $279,425 Failure to cease treatment with excessive/unexpected pain 29.6% $2,649,500 $165,594 Improper management of surgical patient 16.7% $962,721 $106,969 Failure to follow referring practitioner orders 20.4% $804,500 $73,136 Failure to complete proper patient assessment 14.8% $440,500 $55,063 Injury during training for assistive devices or equipment 5.6% $140,000 $46,667
Failure to refer/seek consultation 3.7% $65,000 $32,500
ALLEGATIONS RELATED TO FAILuRE TO MONITOR OR SuPERvISE
-
Failure to supervise or monitor other providers during patient care had the highest average paid indemnity in this allegation category.-
Failure to monitor the patient during treatment had the highest total paid indemnity .-
Example of failure to monitor or supervise: A female patient had nearly completed her course of treatment with the PT for therapy to her strained left quadriceps. In preparation for her continuing home-exercise program, she was asked to perform a leg stretch that involved putting her leg on the table. The PT was standing directly in front of the patient, but was unable to catch her when she lost balance and fell to the floor. She suffered a fractured femur requiring surgical insertion of a femoral rod. The claim was settled in excess of $350,000.Severity by Allegations Related to Failure to Monitor or Supervise
Chart reflects closed claims with paid indemnity of ≥ $10,000
9
Allegation Percentage of closed claims Total paid indemnity Average paid indemnityFailure to monitor or supervise other providers 9.2% $688,750 $98,393 Failure to monitor patient during treatment 85.5% $5,733,592 $88,209 Failure to maintain proper infection control 1.3% $27,500 $27,500
Failure to respond to patient 2.6% $40,500 $20,250
Failure to supervise patient assessment 1.3% $18,000 $18,000
Overall 100 .0% $6,508,342 $85,636
Physical Therapy Closed Claim Scenario: Failure to Properly Monitor or Supervise
A 45-year-old patient was referred to physical therapy with a history of traumatic brain injury, limited use of his extremities, and contractures of his left elbow and shoulder. Therapy was prescribed due to his decreased ability to perform activities of daily living, decreased range of motion and reduced functional mobility. The patient attended aquatic therapy twice a week, during which time his phys- ical therapist would typically work with him one-on-one in the pool. The patient was occasionally permitted to walk on his own alongside the pool while holding the handrail. At the time of the incident, the patient was unattended in the pool, but a lifeguard was on duty and the patient was wearing a flotation device around his chest attached to a lead rope. The physical therapist was assisting another client when the physical therapy aide noticed the patient was completely submerged. The physical therapy aide immediately pulled the patient out of the water and
per-formed cardiopulmonary resuscitation. It was determined that he had been submerged for several minutes before the physical therapy aide rescued him.
The patient eventually began breathing on his own and was transferred to a hospital by ambulance. Acute hospi-talization lasted approximately one month, while he was treated for adult respiratory distress syndrome and aspira-tion pneumonia. Following hospitalizaaspira-tion, the patient was admitted to a rehabilitation facility, where he required high levels of oxygen until his discharge. The patient suffered permanent lung damage and functions at approx- imately 50 percent of normal lung capacity. He resides in an assisted living facility, due to the level of care required on a daily basis. The patient and his wife sued the insured PT and the owners of the pool, alleging negligence of a dependent adult and failure to monitor the patient during treatment. The claim was settled in the high six-figure range.
ALLEGATIONS RELATED TO IMPROPER PERFORMANCE uSING THERAPEuTIC ExERCISE
-
As noted in Figure 7, improper performance using therapeutic exercise was the category with the highest total paid indemnity .-
Injury during gait or stair training accounted for the highest average paid indemnity .-
Improper technique reflected the highest total paid indemnity and the highest percentage of closed claims.-
Examples of claims that alleged improper performance using therapeutic exercise:-
A patient with a history of balance issues performed an exercise that required her to stand on one leg without being supported or braced while moving the alternate leg over an object.-
Patients suffered injuries resulting from exercises that were too advanced or aggressive, based upon their medical history.-
A PT conducting a functional capacity exam (FCE) required a male patient with an injured arm and a pre-existing neck injury to lift a weight that was heavier than the lifting require- ment for the patient’s job. The patient was later diagnosed with cervical herniation and underwent spinal fusion surgery. The claim settled for an amount in excess of $200,000.10
Severity by Allegations Related to Improper Performance using Therapeutic Exercise
Chart reflects closed claims with paid indemnity of ≥ $10,000
Allegation Percentage of closed claims Total paid indemnity Average paid indemnity
Injury during gait or stair training 12.6% $2,296,500 $143,531
Improper positioning 3.1% $367,500 $91,875
Injury from restrictive or elastic bandage/support/brace 0.8% $90,000 $90,000
Improper technique 35.4% $3,998,564 $88,857
Injury during active resistance or assistive range of motion exercises 15.0% $1,424,859 $74,993 Injury during endurance activities 12.6% $1,046,464 $65,404 Injury during resistance exercise or stretching 17.3% $1,248,387 $56,745 Injury during aquatic exercise/therapy 3.1% $128,500 $32,125
ALLEGATIONS RELATED TO IMPROPER PERFORMANCE OF MANuAL THERAPy
-
Injury during passive range of motion had the highest average paid indemnity in this category.-
Example of improper performance of manual therapy:The PT was treating a patient for lumbararthritis and chronic sciatica by performing a piriformis stretch, which required the patient to lie on her back while the PT drew the knee upward toward the opposite shoulder. The patient had under- gone right total hip replacement surgery approximately six years prior to this incident. She had a history of possible right hip instability and reported difficulty getting on and off the toilet due to right hip pain. During the exercise, the patient reported that she felt a sudden pain and experienced a “pop” in her right hip. Although the PT did not hear or feel a pop, the patient was unable to move her hip and could not sit or transfer immediately after the treatment. The patient was trans-ferred to the hospital where she underwent a repeat right hip replacement. The claim was settled in excess of $150,000.
Severity by Allegations Related to Improper Performance of Manual Therapy
Chart reflects closed claims with paid indemnity of ≥ $10,000
11
Allegation Percentage of closed claims Total paid indemnity Average paid indemnityInjury during passive range of motion 13.4% $783,000 $87,000 Injury during manual therapy - improper technique 67.2% $3,604,000 $80,089
Injury during traction 10.4% $529,125 $75,589
Injury during connective tissue manual therapy or massage 9.0% $444,341 $74,057
Overall 100 .0% $5,360,466 $80,007
Physical Therapy Closed Claim Scenario:
Improper Performance Using Therapeutic Exercise
A 9-year-old child with cerebral palsy, who had undergone extensive surgery for correction of bilateral ankle contrac-tures, was referred for physical therapy following removal of the casts from both of his legs. In addition to his surgery, the patient had a history of balance problems, as well as pain and weakness on his right side. The patient was well-known to the therapist, who had provided his care prior to surgery. The patient was correctly placed in bilateral orthotics that maintained the proper position of his ankles during his treatment. The physical therapist positioned the patient on a therapy ball placed against the wall, with chairs on both sides for added stabilization. The patient held the therapy ball handle with his left hand, and with his right hand tossed objects into a basket as instructed by the therapist. The physical therapist remained with the patient continuously, standing on his left side during the exercise. The patient suddenly slipped to his right and was momentarily unable to reach out to the chair to stabilize himself. The physical therapist reached him and eased him to the floor. The patient immediately complained of pain
in the back of his right knee. He was diagnosed with a non-displaced fracture of the right tibia and placed into an over-the-knee cast of the right leg. The physical thera-pist expert review was positive regarding the choice of exercise and confirmed that the exercise did not require two persons. However, the expert noted that, in view of the patient’s history of right-sided weakness and pain, the physical therapist could have anticipated that if the patient were to fall, it would be to the right. Therefore, the therapist would have been better positioned to the patient’s right during the exercise. The orthopedic expert opined that the orthotic acted as the fulcrum point of the fracture and that the fall was the cause of the injury. The orthopedic expert did not believe the fracture would lead to permanent injuries or joint deformity, and the fracture healed successfully. Given the facts of the case and the very sympathetic presentation of the child, the decision was made to attempt to settle the claim. The settlement was in the low six-figure range.
ALLEGATIONS RELATED TO INAPPROPRIATE BEHAvIOR By PHySICAL THERAPIST
-
Failure to follow organizational policy represented the highest average paid indemnity .-
Abuse or misconduct by the PT reflected the highest total paid indemnity and the highest percentage of inappropriate behavior claims.-
Closed claims relating to a PT’s failure to notify the referring practitioner of the modified treatment plan involved the provision of services to patients that went beyond or differed from what the refer- ring practitioner had prescribed. The following examples illustrate this type of allegation:-
The referring practitioner ordered therapy only to the patient’s cervical spinal area, but the PT provided treatment to the cervical and lumbar spine areas without discuss- ing this additional therapy with the referring practitioner. The PT persisted despite the patient’s complaints of severe lower back pain. The patient suffered lower back injuries requiring hospitalization and extensive rehabilitation.-
The PT received an order to treat a patient’s fractured wrist twice a week for six weeks. However, the PT continued the therapy for several months without discussing the treatment with the referring practitioner. The patient suffered a permanent 40 percent loss of mobility in the treated wrist.-
The referring practitioner ordered specific treatment modalities to the patient’s ankle following surgery that involved insertion of hardware. The PT added several modalities – including electrical stimulation – without discussing them with the referring practitioner. These additional treatments resulted in severe burns, which required significant additional treatment.-
Allegations related to inappropriate behavior by the PT represented 5.7 percent of all PT closed claims in the analysis, as shown in Figure 7.12
Severity by Allegations Related to Inappropriate Behavior by Physical Therapist
Chart reflects closed claims with paid indemnity of ≥ $10,000
Allegation Percentage of closed claims Total paid indemnity Average paid indemnity
Failure to follow organizational policy 11.1% $205,000 $68,333 Failure to notify referring practitioner of modified treatment plan 18.5% $296,019 $59,204 Physical, sexual, emotional abuse and/or misconduct 70.4% $1,035,999 $54,526
ALLEGATIONS RELATED TO EQuIPMENT
-
The average paid indemnity for allegations relating to equipment was lower than the overall average for all closed claims.-
Equipment malfunction or failure had the highest percentage of closed claims, the highest total paid indemnity and the highest average paid indemnity in this category.Severity by Allegations Related to Equipment
Chart reflects closed claims with paid indemnity of ≥ $10,000
13
Allegation Percentage of closed claims Total paid indemnity Average paid indemnityEquipment malfunction or failure 53.1% $892,039 $52,473
Improper use of equipment 34.4% $568,499 $51,682
Failure to properly test equipment 6.3% $85,000 $42,500
Improper maintenance of equipment 6.3% $31,000 $15,500
Overall 100 .0% $1,576,538 $49,267
ALLEGATIONS RELATED TO IMPROPER uSE OF A PHySICAL AGENT
-
The term “physical agent” is defined by the American Physical Therapy Association’s Guide to Physical Therapist Practice (Second Edition, 2001) as “various forms of energy that are applied to tissues in a systematic manner and that are intended to [promote healing and/or improve the patient’s condition].”-
The average paid indemnity of $40,176 for this category was significantly less than the average paid indemnity of $79,471 for all PT closed claims in the analysis.-
Average paid indemnity for claims related to the use of heat therapy or hot packs was more than twice the average paid indemnity for claims related to the use of cold packs/ice massage.Severity by Allegations Related to Improper use of a Physical Agent
Chart reflects closed claims with paid indemnity of ≥ $10,000
14
Allegation Percentage of closed claims Total paid indemnity Average paid indemnityInjury during heat therapy or hot packs 61.4% $2,564,167 $50,278
Injury during electrotherapy 32.5% $651,948 $24,146
Injury from cold packs/ice massage 6.0% $118,500 $23,700
Analysis of Severity by Injury
-
Paralysis, physical assault, herniated disc and death reflected the highest average paid indemnity .-
Fractures reflected the highest percentage of injuries and total paid indemnity . The apparent causesof fractures were patient falls, improper use of equipment, unanticipated equipment failures, slips and trips that occurred during ambulation, improperly performed treatment, improper patient assess- ment, and failure to provide monitoring or supervision. The risk of fracture may be higher for patients who were more debilitated, suffered from chronic illness or failed to follow directions of the PT.
-
Burns followed by increase or exacerbation of injury/symptoms also accounted for a highpercent-age of injuries.
-
Burns were primarily associated with allegations of improper performance using a physical agent. However, there were also claims with allegations related to equipment and a low number of claims with five other categories of allegations. Therefore, the percentage of closed claims with the injury “burns” is greater than the percentage of closed claims with the allegation “improper performance using a physical agent” (see also Figure 7).-
Herniated disc was the only injury that had an average paid indemnity exceeding $175,000 while also accounting for more than 5 percent of the PT closed claims.-
In two claims, paralysis allegedly was related to the PT’s failure to report the patient’s condition.-
Delay in recovery resulted from the PT failing to order equipment needed to follow the physician’sorders while providing therapy in the patient’s home.
Physical Therapy Closed Claim Scenario: Improper Use of a Physical Agent
A 25-year-old male was referred to physical therapy with a history of diabetic neuropathy of his lower extremities. The patient had been undergoing heat therapy and par- affin baths at the PT office practice for approximately one month when he suffered a burn to his foot. The burn resulted in an infection, which led to gangrene and necrosis of the second toe. The patient underwent several surgical procedures, including insertion of a central catheter for the administration of antibiotics, debridements, skin graft, amputation of the right second toe, incision and drainage of a wound, resection of the right second metatarsal and a right posterior tibial common plantar artery bypass with vein graft.
The patient pursued a claim for pain and suffering, lost wages and lack of informed consent. The claim was difficult to defend, due to the absence of the physical therapist’s initial evaluation. In addition, documentation failed to demonstrate whether the physical therapist assistant – who was acting under the supervision of the physical therapist – had followed diabetic foot precautions. The claim was settled in the low six-figure range.
Severity by Injury
Chart reflects closed claims with paid indemnity of ≥ $10,000
15
Injury Percentage of closed claims Total paid indemnity Average paid indemnity Paralysis 0.6% $1,230,000 $410,000Physical injury resulting from abuse/assault 0.4% $401,000 $200,500
Herniated disc 5.5% $4,653,304 $178,973
Death 0.9% $632,125 $158,031
Traumatic brain injury 1.0% $640,288 $128,058
Loss of organ or organ function including hearing and sight 1.0% $544,000 $108,800 Increase or exacerbation of injury/symptoms 17.8% $7,611,980 $89,553
Fracture 26.4% $11,055,822 $87,745
Dislocation 2.3% $925,250 $84,114
Neurological - peripheral and all other 0.6% $247,500 $82,500
Muscle/ligament damage 9.0% $3,255,236 $75,703
Amputation 1.0% $344,492 $68,898
Infection/abscess/sepsis 0.9% $272,500 $68,125
Loss of use of limb 3.1% $1,009,000 $67,267
Bleeding/hemorrhage 0.2% $50,000 $50,000
Burn 20.1% $3,856,134 $40,168
Delay in recovery 0.2% $40,000 $40,000
Emotional distress resulting from sexual abuse/assault 3.6% $634,999 $37,353
Compartment syndrome 0.2% $35,000 $35,000 Sprain/strain 1.9% $222,000 $24,667 Cracked/broken tooth 0.9% $76,175 $19,044 Abrasion/irritation/laceration 1.3% $98,391 $16,399 Bruise or contusion 0.9% $62,500 $15,625 Cardiovascular injury 0.2% $10,000 $10,000 Overall 100 .0% $37,907,696 $79,471
COMPARISON OF RE-INJuRy vERSuS OTHER INJuRIES
The data were analyzed to determine the prevalence of re-injury during physical therapy. For the purposes of this analysis, a claim was classified as a “re-injury” if the condition or body part for which the patient was seeking physical therapy was harmed again during the therapy session. An example of “re-injury” would be a patient seeking therapy subsequent to rotator cuff surgery, whose same rotator cuff was injured during therapy.
-
It was determined that 22.2 percent of the PT closed claims involved a re-injury.-
The financial impact was significantly higher when the claim involved a re-injury.-
The average paid indemnity for re-injury closed claims was $126,200, which is almost twice the aver- age paid indemnity for other injuries ($66,120) and almost 60 percent higher than the overall average paid indemnity of $79,471.16
Comparison of Re-injury versus Other Injuries
Chart reflects closed claims with paid indemnity of ≥ $10,000
Re-injury/Injury Percentage of closed claims Total paid indemnity Average paid indemnity Re-injury 22.2% $13,377,207 $126,200
Injury (other than re-injury) 77.8% $24,530,489 $66,120
Overall 100 .0% $37,907,696 $79,471
The
average paid indemnity
for re-injury closed
claims was $126,200, which is almost twice the
average paid indemnity
for other injuries ($66,120)
ANALySIS OF SEvERITy By RE-INJuRy
-
A claim that involved re-injury of the spine resulting in paralysis had the highest paid indemnity.-
Herniated disc, physical abuse/assault, muscle/ligament damage, and increase or exacerbation ofthe patient’s injury or symptoms were associated with an average paid indemnity higher than the overall average paid indemnity for PT closed claims.
Severity by Re-injury
Chart reflects closed claims with paid indemnity of ≥ $10,000
17
Re-injury Percent of re-injury closed claims Total paid indemnity Average paid indemnity Paralysis 0.9% $1,000,000 $1,000,000 Herniated disc 7.5% $2,758,000 $344,750Physical injury resulting from abuse/assault 1.9% $401,000 $200,500
Muscle/ligament damage 12.3% $1,664,166 $128,013
Increase or exacerbation of injury/symptom 74.5% $7,402,941 $93,708
Fracture 1.9% $111,600 $55,800
Sprain/strain 0.9% $39,500 $39,500
Overall 100 .0% $13,377,207 $126,200
ANALySIS OF RE-INJuRy By AFFECTED BODy PART
-
Re-injury of the lower back had significant average paid indemnity and total paid indemnity .-
Re-injury of the shoulder, including rotator cuff injury, had lower average paid indemnity than lowerback injury, but represented the highest percentage of re-injury closed claims.
18
Severity of Re-injuries by Affected Body Part
Chart reflects closed claims with paid indemnity of ≥ $10,000
Body part Percent of re-injury closed claims Total paid indemnity Average paid indemnity Nerve 0.9% $1,000,000 $1,000,000 Disc (thoracic) 0.9% $385,000 $385,000 Upper back 0.9% $285,000 $285,000 Lower back 21.7% $4,847,973 $210,781 Disc (lumbar) 2.9% $510,000 $170,000 Knee 18.9% $2,580,156 $129,008 Neck 2.9% $310,000 $103,333 Toe 0.9% $100,000 $100,000 Hand 0.9% $85,000 $85,000 Upper leg 2.9% $240,000 $80,000 Shoulder 34.0% $2,431,478 $67,541 Hip 2.9% $202,000 $67,333 Ankle 0.9% $65,000 $65,000 Wrist 1.9% $120,000 $60,000 Finger 0.9% $45,000 $45,000 Arm 1.9% $61,500 $30,750 Foot 1.9% $56,600 $28,300 Abdomen 0.9% $27,500 $27,500 Pelvis 0.9% $25,000 $25,000 Overall 100 .0% $13,377,207 $126,200
ALLEGATIONS RELATED TO RE-INJuRy
-
Examples of claims with the highest average paid indemnity:-
A PT allegedly failed to identify a thoracic fracture. The allegation was related to the PT’s failure to continue to communicate with the referring physician until the physician responded.Severity by Allegations Related to Re-injury
Chart reflects closed claims with paid indemnity of ≥ $10,000
19
Allegation Percent of re-injury closed claims Total paid indemnity Average paid indemnityFailure to report patient’s condition to referring practitioner 0.9% $1,000,000 $1,000,000
Abandonment 2.0% $1,631,305 $815,653
Injury during gait or stair training 2.0% $1,135,000 $567,500
Improper performance of test 0.9% $250,000 $250,000
Failure to cease treatment with excessive/unexpected pain 7.5% $2,000,000 $250,000 Physical, sexual, emotional abuse and/or misconduct 2.0% $401,000 $200,500 Failure to complete proper patient assessment 2.0% $322,500 $161,250 Injury during manual therapy - improper technique 13.2% $1,687,500 $120,536
Improper technique 18.9% $2,223,166 $111,158
Failure to follow organizational policy 2.0% $185,000 $92,500 Injury from restrictive or elastic bandage/support/brace 0.9% $90,000 $90,000
Injury during traction 0.9% $78,000 $78,000
Failure to properly test equipment 0.9% $70,000 $70,000
Failure to supervise physical therapist assistant/aide 0.9% $70,000 $70,000 Failure to follow referring practitioner orders 6.6% $462,000 $66,000 Injury during training for assistive devices or equipment 0.9% $65,000 $65,000 Failure to monitor patient during treatment 3.8% $257,198 $64,300
Improper management of surgical patient 2.8% $165,000 $55,000
Failure to provide safe environment 0.9% $55,000 $55,000
Injury during active resistance or assistive range of motion exercises 7.5% $413,412 $51,677 Injury during aquatic exercise/therapy 0.9% $49,500 $49,500 Injury during endurance activities 5.7% $249,375 $41,563 Injury during resistance exercise or stretching 9.4% $357,251 $35,725 Failure to notify referring practitioner of modified treatment plan 2.0% $57,500 $28,750
Failure to refer/seek consultation 0.9% $27,500 $27,500
Equipment malfunction or failure 2.8% $62,500 $20,833
Unnecessary treatment 0.9% $12,500 $12,500
ANALySIS OF CLAIMS RELATED TO BuRNS
20
Severity by Intensity of Burn
Chart reflects closed claims with paid indemnity of ≥ $10,000
Intensity of burn Percentage of closed claims Total paid indemnity Average paid indemnity
Severe: requires any type of surgery 63.5% $2,419,634 $39,666 Moderate: requires more treatment than “mild” burn but no surgery 31.3% $1,298,000 $43,267 Mild: requires only local treatment/comfort care 5.2% $138,500 $27,700
Overall 100 .0% $3,856,134 $40,168
ANALySIS OF SEvERITy RELATED TO BuRNS By BODy PART
-
Burns to the hip accounted for the highest average paid indemnity for closed claims related to burns.-
Burns to the lower extremities accounted for both the highest total paid indemnity and the highestpercentage of the closed claims related to burns.
-
A recurring theme in this category of closed claims was failure to properly monitor the patient dur-ing use of hot packs.21
Severity of Burns by Body Part
Chart reflects closed claims with paid indemnity of ≥ $10,000
Body part Percentage of closed claims Total paid indemnity Average paid indemnity Hip 3.1% $547,500 $182,500 Upper extremity 24.0% $872,448 $37,933 Lower extremity 50.0% $1,812,186 $37,754 Upper back/neck 4.2% $138,500 $34,625 Lower back 15.6% $416,500 $27,767 Face 1.0% $26,000 $26,000 Trunk 2.1% $43,000 $21,500 Overall 100 .0% $3,856,134 $40,168
ANALySIS OF SEvERITy By DISABILITy
-
The cost of providing immediate and future medical care, as well as compensation for economic and non-economic losses related to the injury, contributed to a higher average paid indemnity for permanent total disability.-
Permanent partial disability had the highest total paid indemnity, representing 24.5 percent of closed claims.-
Deaths related to care provided by physical therapists are rare, but they represented the second-highest average paid indemnity . Deaths were the result of cardiac arrest, traumatic brain injury and a post-operative cervical epidural abscess.Severity by Disability
Chart reflects closed claims with paid indemnity of ≥ $10,000
22
Disability Percentage of closed claims Total paid indemnity Average paid indemnityPermanent total disability from injury/illness 2.3% $3,242,195 $294,745
Death 0.8% $632,125 $158,031
Permanent partial disability from injury/illness 24.5% $14,737,208 $125,959 Temporary total disability from injury/illness 13.2% $5,533,548 $87,834 Temporary partial disability from injury/illness 59.1% $13,762,620 $48,804
Overall 100 .0% $37,907,696 $79,471
Deaths related to care provided by physical therapists
are rare, but they represented the second-highest
average paid indemnity
. Deaths were the result of
cardiac arrest, traumatic brain injury and a post-
operative cervical epidural abscess.
Summary Analysis of Physical Therapist Assistant Closed Claims
Figures 23 and 24 include both individually insured PTAs and PTA employees of PT practices.SEvERITy By ALLEGATION
-
The average paid indemnity for PTA and PT closed claims was similar. The associated medical costs and economic losses were similar, regardless of who was involved in the patient’s care.-
Improper use of equipment represented the highest average paid indemnity in PTA closed claims. The patient sustained a back injury allegedly resulting from the PTA’s failure to properly use equip-ment. There was no documentation to support the appropriateness of the PTA’s care.-
Failure to monitor the patient during treatment accounted for the highest percentage of PTA claims.-
Common themes in these claims included failure to take responsibility for the patient’s care, lack of communication with the healthcare team, improper assessment, failure to follow practitioner orders and improper monitoring of patients during treatment.23
Severity by Allegation Related to Physical Therapist Assistants
Chart reflects PTA closed claims with paid indemnity of ≥ $10,000
Allegation Percentage of PTA closed claims Total paid indemnity Average paid indemnity
Improper use of equipment 2.0% $650,000 $650,000
Failure to report patient’s condition to referring practitioner 2.0% $525,000 $262,500 Failure to complete proper patient assessment 4.1% $175,000 $175,000 Failure to follow practitioner orders 2.0% $427,500 $106,875
Improper positioning 8.2% $90,000 $90,000
Equipment malfunction or failure 2.0% $177,500 $88,750
Injury during manual therapy - improper technique 4.1% $243,335 $81,112 Injury during heat therapy or hot packs 6.2% $394,500 $65,750 Improper management of surgical patient 12.3% $55,000 $55,000 Injury during gait or stair training 2.0% $92,000 $46,000 Injury during resistance exercise or stretching 4.1% $45,000 $45,000 Failure to monitor patient during treatment 2.0% $403,006 $40,301 Failure to provide safe environment 20.5% $35,000 $35,000 PTA functioning outside accepted scope of practice 2.0% $158,689 $31,738
PTA AND PT CLOSED CLAIMS: COMPARISON OF TOP THREE ELEMENTS By SEvERITy
-
Locations with the highest average paid indemnity differed for PTA and PT closed claims.-
Improper management over the course of treatment (e.g., failure to report patient’s condition to the referring practitioner or failure to refer/seek consultation) was one of the top three allegations with the highest average paid indemnity for both PTAs and PTs. The other allegations differed.-
Injuries with the highest average paid indemnity differed for PTA and PT closed claims, with the exception of herniated disc.-
Causes of death with the highest average paid indemnity differed for PTAs and PTs.PTA and PT Claim Comparison of Top Three Elements by Severity
Chart reflects closed claims with paid indemnity of ≥ $10,000
24
Topic PTA PT
Percent of claims 9.3% 90.7%
Average paid indemnity $75,798 $79,471
Location
■ Physical therapy office/clinic - non-hospital ■ Aging services facility
■ Acute medical-surgical hospital inpatient
■ Hospital inpatient physical therapy area ■ Fitness center
■ Aging services facility
Allegations
■ Improper use of equipment
■ Improper management over the course of
treatment
■ Improper performance of manual therapy
■ Failure to test/treat
■ Improper management over the course of
treatment ■ Environment of care Injury ■ Herniated disc ■ Death ■ Muscle/ligament damage ■ Paralysis
■ Physical injury resulting from abuse/assault ■ Herniated disc Cause of death ■ Cardiopulmonary arrest ■ Burns ■ Pneumonia/respiratory infection ■ Paralysis
■ Traumatic brain injury ■ Cardiopulmonary arrest
Disability
■ Death
■ Permanent partial disability ■ Permanent total disability
■ Permanent total disability ■ Death
Physical Therapy Closed Claim: Alleged Improper Care (a Success Story)
A 65-year-old male was referred to physical therapy for treatment of work-related injuries that resulted in pain between his shoulder blades radiating to his lower back, numbness and tingling of both arms and left leg, and muscle spasms radiating from the spine. MRI had con-firmed degenerative lumbar disc disease and possible herniated thoracic discs. The physical therapy treatment plan included joint mobilization, electrical stimulation, aquatic and therapeutic exercises, posture exercises and ultrasound therapy. The PT discussed the plan of care, including joint mobilization, with the patient, who provided his written consent. Five therapy treatments were com-pleted, with joint mobilization performed only on the fifth visit. The patient offered no complaint at any time and admitted to feeling better at the time of his final treatment. The PT received a letter of legal representation alleging that during joint mobilization, the PT had forcefully and repeatedly bent the patient’s arms and shoulders, despite his complaints of intense pain resulting in a torn rotator cuff. The patient also alleged interruption of his back ther- apy to attend to his shoulder, including two surgeries and a referral to a neurosurgeon.
The defense expert supported the care provided by the PT as being within the standard of care. The expert further noted that the PT’s documentation was complete and appropriate, confirming the PT’s testimony and providing a solid basis for defending the claim.
The plaintiff’s orthopedic surgeon testified only that the patient’s shoulder surgery interrupted his back treatment. The patient’s neurosurgeon refused to attend his deposi-tion and legal counsel was unable to secure a PT expert witness to support the patient’s allegations.
No indemnity payment was offered and the court issued a summary judgment dismissing the action against the insured PT. Significant legal and related expenses were paid to successfully defend this claim. While settlement may have been less costly, the PT’s appropriate treatment and careful documentation led to an aggressive and suc-cessful defense of the claim.
While settlement may have been less costly,
the PT’s appropriate treatment and careful
documentation led to an aggressive and successful
Risk Control Recommendations
While rare events may be difficult to foresee, analysis of the PT closed claims data suggests that many errors are both predictable and preventable. In order to protect patients and minimize liability, it is nec-essary to ensure that services meet established standards of care and that documentation practices are thorough and consistent. The following strategies can help both individual therapists and practices enhance safety while minimizing risk:
Communicate effectively with patients, families and colleagues . The following measures can help strengthen key relationships:
-
Consider the best method and form of communication, e.g., written versus spoken, words versus pictures, in person versus by telephone.-
Utilize translation/interpreter services when necessary, following organizational guidelines.-
Obtain the patient’s permission before sharing information with family members or significant others.-
Request that the patient and family members repeat back key information.-
Encourage questions from and open discussion with patients and family members.-
Recognize nonverbal cues from the patient, such as grimacing or flinching, as well as physical distress signs, such as pallor or diaphoresis.-
Notify the appropriate practitioner(s) and healthcare team members of the patient’s clinical responses to therapy, and swiftly convey any signs or symptoms of physiological or psychological changes that could indicate a new pathological condition or a change in an existing condition.-
Actively solicit feedback from the patient, and document the patient’s statements in the health infor- mation record.-
Employ effective handoff communication techniques whenever the therapist of record transfers the care of the patient to another therapist or provider.-
Actively involve the patient, family and/or caregiver in setting goals for therapy.Delegate patient therapy services only to the appropriate level of staff and provide appropriate super- vision for all delegated patient services .
-
It may be acceptable to delegate certain patient services to licensed/certified therapy personnel in accordance with the state scope of practice for each level of staff.-
Delegate only those services that can be legally and safely provided by another level of staff and only when the patient is stable and his/her ability to tolerate the service is known to the physical therapist.-
Never leave the therapy area when the patient is receiving services from another level of staff.-
Periodically assess the staff member’s technique and the patient’s response to the delegated servicethroughout the session, and document supervisory findings.
-
Cease the delegated services and directly evaluate the patient in the event of patient complaints of unanticipated pain, fatigue, or other signs and symptoms that demand the physical therapist’s direct attention.Adopt an informed consent process that includes discussion and teach-back from the patient, and demonstrates that the patient understands the risks associated with treatment .
Before engaging in treatments or interventions, the PT must obtain the patient’s informed consent, with all discussions carefully documented. At a minimum, informed consent discussions should include
-
known risks and benefits of the treatment plan, alternative treatment options and the likely consequences of declining the suggested therapy-
disclosure of clinically indicated touching and/or potential discomfort during treatment-
answers to patient and family questions-
repetition of important information by the patient to ensure understanding-
written confirmation that the patient agrees to the proposed treatment-
provision of pertinent patient education materials and corresponding documentationEnsure that clinical documentation practices comply with the standards promulgated by physical therapy professional associations, state practice acts and facility protocols .
The importance of complete, appropriate, timely, legible and accurate documentation cannot be over-stated, whether records are in electronic or handwritten form. At a minimum, records should include
-
date, time and signature for each entry-
patient complaints, statements and ongoing concerns related to the treatment plan, such as progress and pain levels-
findings of initial and ongoing patient assessments-
results of diagnostic procedures-
patient responses to therapy-
discussions regarding diagnosis, treatment options and expected outcomes with the patient, family and healthcare team members-
patient education and discharge instructions, including assessment of the patient’s ability to demonstrate self-care and correctly repeat instructions-
objective facts related to any patient accident, injury or adverse outcomeAvoid documentation errors that may weaken legal defense efforts in the event of litigation . The following documentation missteps can seriously compromise defensibility:
-
Refrain from documenting subjective opinions or conclusions, as well as making any derogatory statement about patients or other providers in the record.-
Never remove any page or section from a health information record or alter a written or electronic medical record.-
If it is necessary to correct documentation errors or make a late entry, ensure that alterations conform to organizational policies and procedures.Maintain clinical competencies specific to the relevant patient population .
If the practice does not offer continuing education opportunities, contact the appropriate regulatory agency or professional association to obtain information about classes, seminars and resources neces-sary to maintain competencies.
Be vigilant about protecting patients from the most common types of injuries .
Our analysis of closed claims indicates that re-injuries, burns and fractures should be a serious concern for all physical therapists and practices. The following guidelines can help minimize liability and increase defensibility in case of an adverse occurrence:
-
Re-injuries-
Adhere to organizational treatment protocols when available. If protocols are not available, refer to the applicable state practice act and professional organization guidelines, such as those of the American Physical Therapy Association.-
Review published evidence-based best practices.-
Cease treatment immediately if there are complaints of unexpected, sudden and/or severe pain, swelling or discoloration.-
Arrange emergency transportation to the nearest emergency room following any suspected injury.-
Determine the level of patient compliance with any prescribed exercise program.-
Discuss suspected noncompliance with the patient, emphasizing that it presents a risk of injury. Notify the referring practitioner of any noncompliance, and document both the notification and the practitioner’s response.-
Routinely monitor and document vital signs.-
Burns-
Be aware of the high risk of burns from certain commonly used treatments and interventions, such as whirlpool therapy, hot packs, paraffin, cold/ice packs and electrotherapy. Ensure that each of these treatments is clinically appropriate and that there are no clinical contraindications for their use.-
Evaluate and document each patient’s skin integrity, neurological status, and ability to perceive pain or discomfort, and convey problems to staff. Evaluation should be performed prior to the course of treatment and periodically thereafter.-
Closely supervise and/or monitor patients during treatment, including frequent skin checks.-
Discuss any perceived alterations in skin integrity with the referring practitioner and healthcare team.-
Routinely test, monitor and log temperatures of whirlpool water, hot-pack warmers, paraffin tanks and other equipment in accordance with organizational policies.-
Fractures-
Maintain a safe environment of care with dry, level and unobstructed walkways and therapy spaces.-
Assess patients initially and periodically thereafter for fall and fracture risk in light of underlying medical conditions.-
Evaluate patients’ ability to use equipment in a safe manner and participate in physical therapy treatments.-
Respond immediately to any signs or symptoms of a possible fracture by determining the need for additional medical evaluation and obtaining emergency medical services as needed.-
Observe high-risk patients closely to prevent falls and/or fractures, and never leave them unattended.-
Utilize appropriate safety devices, such as gait belts, floor and treatment table pads, and equipment alarms.-
Conduct and document regular equipment maintenance and check equipment for proper functioning before each patient use. Immediately remove and sequester any equipment that has malfunctioned or that does not meet safety standards.-
Always ensure that patients are correctly and securely positioned on treatment tables or equipment.-
Train staff and patients in the proper use of equipment and require an initial demonstra- tion of competency to avoid injury.-
Educate patients regarding the appropriate clothing and footwear that should be worn during treatment/intervention, and do not permit use of equipment without proper apparel and shoes.Recognize patients’ medical conditions, co-morbidities and any additional specific risk factors that may affect therapy .
Examples of pre-existing conditions include