109 Int J Res Med. 2014; 3(3);109-114 e ISSN:2320-2742 p ISSN: 2320-2734
A Comparative Study between sutureless and Lichtenstein inguinal Mesh
hernioplasty
Hitesh D. Patel1, Chirag B. Pandya2, V. P. Hathila3
1 Dr. Hitesh D. Patel (MS), Assistant professor. General surgery, medical college and SSG hospital, Vadodara, Gujarat. 2
Dr. Chirag B Pandya (MS), General surgery, ESIS General Hospital, Vadodara, Gujarat.
3 Dr V. P. Hathila (MS), Professor, general surgery, medical college and SSG hospital, vadodara, Gujarat.
INTRODUCTION
Inguinal hernias are one of the most common problems encountered by the surgeon, accounting for about 10-12% of all operations. An inguinal hernia can be defined as protrusion of a part or whole abdominal viscous into the inguinal canal either through the deep ring or through hasselbach's triangle.1 Approximately 75% of all hernias occur in the groin with a lifetime risk of 27% in men and 3% in
*Corresponding author
Dr. Hitesh D. Patel, Assistant Professor,
General surgery Department, Medical college and SSG hospital, Vadodara
mo: 9879722888
Email- hitesh_315@yahoo.co.in
women. About 2/3 of these hernias are indirect and one third direct.2 The weakness of the abdominal wall and the increase in abdominal pressure has been regarded as the main mechanism thus chronic cough (smokers or COPD) and constipation are major risk factors for hernia.3 Surgery is the treatment of choice varying from nylon darn, ice layered, Lichtenstein mesh to a laparoscopic repair. The gold standard for any hernia surgery is lowest recurrence rate. While numerous surgical approaches exist to treat inguinal hernias, the Lichtenstein tension-free mesh-based repair remains the standard for primary hernia. Laparoscopic repair is suggested for recurrent and bilateral inguinal hernias, though it may also be offered for primary inguinal hernia repair; have certain ABSTRACT
BACKGROUND: Present study conducted to assess the efficacy of suture less hernioplasty for inguinal hernia patients as compare with standard Lichtenstein hernioplasty. MATERIALS AND METHODS: this was randomized controlled trial conducted in department of surgery, sir sayaji general hospital, vadodara. Total 150 patients were included in study. Patients were randomly divided into two groups. Each group consists of 75 patients each. Those patients undergoing suture less was grouped as A and those undergoing Lichtenstein mesh repair was grouped as B. RESULTS: Mean age in group A and B was 40.34±7.2 and 43.26±7.2. In Group-A 24(16.7%) patients had direct and 31(83.3%) had indirect hernia. In Group-B 47(13.3%) patients had direct and 28(86.7%) had indirect hernia. At 7th day post operative in Group-A 3 patients had hematoma while in Group-B 12 patients had large scrotal edema. Large Scrotal edema formation in both treatment groups at 7th day was statistically significant i.e., p-value (7th day) =0.017 In Group-B rate of large scrotal edema formation was less as compared to Group-A. Post operative pain was assessed by visual analog score in both groups at 1st, 2nd, 4th, and 7th day. at 1st day mean pain score in group A was 5.8±1.9 and in group B was 7.1±2.3.mean pain score on 2nd day was 5.1±1.5 in group A and in group B was 6.5±1.8.at 4h day mean pain score in group A was 4.3±1.3 and in group B was 5.1±1.6.At 7TH day mean pain score in group A was 4.3±1.3 and in group B 5.1±1.6.patients in group A had less pain score as compare to group B patients. CONCLUSION: Suture less hernia repair is a superior approach as compared to Lichtenstein technique for inguinal hernia surgery in terms of post operative pain and large scrotal edema formation.
110 Int J Res Med. 2014; 3(3);109-114 e ISSN:2320-2742 p ISSN: 2320-2734 technical limitations. The object of hernia
repair is to prevent peritoneal protrusion, through the myopectineal orifice. The integrity of myopectineal orifice is restored by two different ways: aponeurotic closure or replacement of defective transversalis fascia with synthetic prostheses.1,4,5 We are concerning with anterior repair by inguinal incision using the method of anterior prosthetic hernioplasty or tension free hernioplasty which was coined by Lichtenstein to describe his prosthetic hernioplasty a technique which consist of a swatch of polypropylene mesh( 8-16cm) with part way slit on its upper edge to accumulate the spermatic cord and fashioned for the patient. The mesh is sutured circumferentially to the internal oblique abdominal muscle, the rectus sheath and shelving edge of inguinal ligament with or without mesh plug which is cylindrical and made from 2-2.5cm strip of polypropylene mesh. The plug is fixed firmly and sutured flush in place with non absorbable synthetic sutures. The suture less hernioplasty in which repair of posterior inguinal wall "Transversalis fascia" using a patch of polypropylene mesh without fixing it to the surrounding ligaments or aponeurotie structures, to evaluate the advantages and disadvantages of this method of repair by comparing it with 75 patients as a control group who were managed by conventional Lichtenstein repair in which fixation of the mesh by interrupted synthetic non absorbable suture. Two techniques have been described to use a mesh in open procedure i.e., sutured (traditional Lichtenstein) and suture less. Those advocating suture less mesh hernioplasty, are of the opinion that decrease tension in suture line and a better leveling leads to rapid embodiment of mesh without formation of dead space therefore chances of nerve entrapment
and post operative complications are reduced, so that post operative recovery and post operative hospital stay will be decreased. On the other hand some studies claim that chances of displacement, migration and folding of mesh are more in suture less mesh hernioplasty than traditional Lichtenstein technique, resulting in the failure of the whole procedure. The Tensions free suture less hernioplasty is especially appropriate for old men.6 They are usually not needed in woman with primary indirect inguinal hernias as simple obliteration of the deep ring always produce excellent results.1,2,4,7,9 Wide spread enthusiasm for tension free hernioplasty has been developed because they are easy to perform1 and has lowest recurrence rate. Furthermore suture less hernioplasty with its added simplicity, durability, quick recovery with comparable results to that of mesh fixation which is the prospect of study.
MATERIAL AND METHODS
From February 2005 to January 2007, 75 patients of different age groups attending vadodara teaching hospital who were suffered from inguinal hernia were managed by suture less tension free hernioplasty. Another 75 patients similarly of different age groups with primary inguinal hernia were managed by the standard Lichtenstein tension free where selected as control group.
Inclusion criteria: all patients aged 20-60 year of either gender with clinically reducible inguinal hernia diagnosed on clinical examination were included in the study.
Exclusion criteria: 1. congenital hernia
and hernia in patients up to 16 years. 2. Incarcerated, obstructed or strangulated
111 Int J Res Med. 2014; 3(3);109-114 e ISSN:2320-2742 p ISSN: 2320-2734 study. Patients were divided into two
groups randomly. Group-A for undergoing sutureless repair and group-B for lichenstain hernia repair. Hernioplasty was done by same consultant and follow by himself at 7th postoperative day for assessment.
Method: Following a preoperative
evaluation all patients were subjected to surgery Standard hernia incision was used, about 2 cm above and parallel to the medial half of the inguinal ligament. Skin and subcutaneous tissue cut along the line of incision up to external oblique. Anterior surface of external oblique was cleared off the superficial fascia, both fatty and membranous, above and below. Inguinal canal was opened by placing an incision over the external oblique about 2 cm from inguinal ligament extending from the superficial ring to about 1 cm past the deep ring. The upper and lower flaps were raised till the aponeurosis of internal oblique muscle and rectus sheath were seen superiorly and the upward curved portion of inguinal canal were exposed. The cord and its coverings were cleared off the inner aspect of inguinal ligament up to public tubercle. The spermatic nerve and ilioinguinal nerve were separated and safe guarded. The cord was "skeletonized" by removing its covering. The indirect sac was separated from the cord structures completely up to its neck and if direct sac present, it buried in to the posterior wall of inguinal canal. A snug internal ring was reconstructed after sac was ligated and transfixed by using suture material. Posterior wall of the inguinal canal repaired by tension free sutures and preshaped proline mesh was kept over the posterior wall of the inguinal canal with encircling the spermatic cord, depending on the condition of posterior wall. The spermatic cord was now placed over the newly constructed posterior wall. The anterior
wall of the inguinal canal was reconstituted by suturing the both flap of external oblique using continuous sutures starting from the lateral end reaching medially and ends to have a gap of adequate size so as to create new superficial ring and allow the passage of spermatic cord. In control group similar technique was adopted a mesh of similar size is fixed to strength transversalis fascia by 8 stitches, to the inguinal conjoined tendon and rectus sheath and pubic tubercle a small slit is made on the upper boarder so that two arms encircle the spermatic cord around the internal ring which are fixed by nonabsoable suture.
Follow up: all patients were followed for one year post operatively. Three parameter were assessed including post operative pain, post operative large scrotal hematoma and rate of hernia recurrence.
RESULTS
Total 150 patients with inguinal hernia were selected for study and randomly divided into two groups each consist of 75 patients. Group-A for suture less and Group-B for Lichtenstein mesh repair.
Table 1: Age (years) of patients
Age Group
A
Group B
Total
Mean ± SD 43.26±7 40.34±6 .8
41.8± 7
Minimum 27 24 24
Maximum 60 58 60
Mean age of all patients (150) was 41.8±7years.while mean age of patients in group A and B was 40.34±7.2 and 43.26±7.2 years respectively. All patients in this study were male.
Table 2: Types of inguinal hernia
Type Group A
Group B
Total
indirect 24 (32%)
28 (37.3%)
75
direct 31 (41.3%)
47 (62.6%)
75
112 Int J Res Med. 2014; 3(3);109-114 e ISSN:2320-2742 p ISSN: 2320-2734 direct hernia.
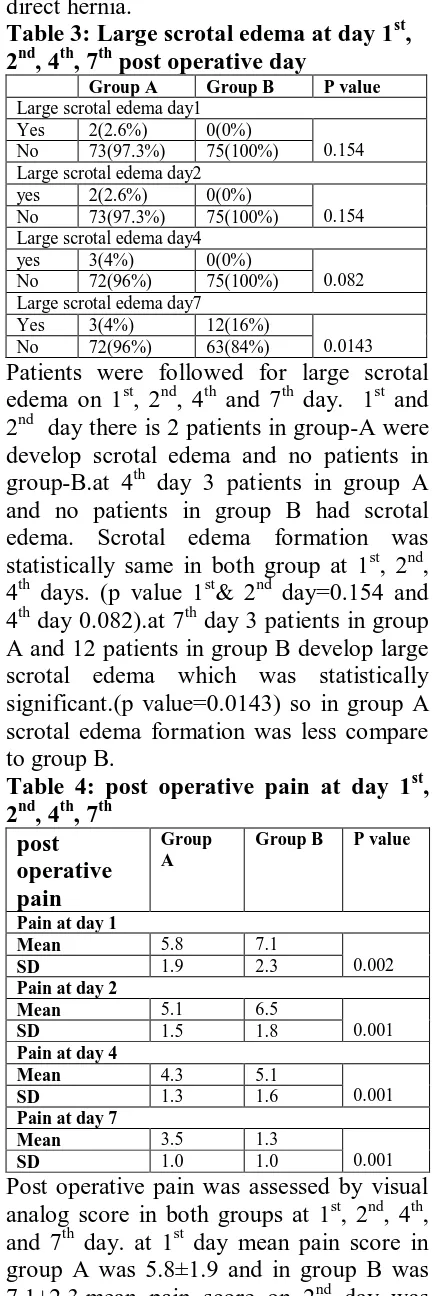
Table 3: Large scrotal edema at day 1st, 2nd, 4th, 7th post operative day
Group A Group B P value Large scrotal edema day1
Yes 2(2.6%) 0(0%)
0.154 No 73(97.3%) 75(100%)
Large scrotal edema day2 yes 2(2.6%) 0(0%)
0.154 No 73(97.3%) 75(100%)
Large scrotal edema day4 yes 3(4%) 0(0%)
0.082 No 72(96%) 75(100%)
Large scrotal edema day7
Yes 3(4%) 12(16%)
0.0143 No 72(96%) 63(84%)
Patients were followed for large scrotal edema on 1st, 2nd, 4th and 7th day. 1st and 2nd day there is 2 patients in group-A were develop scrotal edema and no patients in group-B.at 4th day 3 patients in group A and no patients in group B had scrotal edema. Scrotal edema formation was statistically same in both group at 1st, 2nd, 4th days. (p value 1st& 2nd day=0.154 and 4th day 0.082).at 7th day 3 patients in group A and 12 patients in group B develop large scrotal edema which was statistically significant.(p value=0.0143) so in group A scrotal edema formation was less compare to group B.
Table 4: post operative pain at day 1st, 2nd, 4th, 7th
post operative pain
Group A
Group B P value
Pain at day 1
Mean 5.8 7.1
0.002
SD 1.9 2.3
Pain at day 2
Mean 5.1 6.5
0.001
SD 1.5 1.8
Pain at day 4
Mean 4.3 5.1
0.001
SD 1.3 1.6
Pain at day 7
Mean 3.5 1.3
0.001
SD 1.0 1.0
Post operative pain was assessed by visual analog score in both groups at 1st, 2nd, 4th, and 7th day. at 1st day mean pain score in group A was 5.8±1.9 and in group B was 7.1±2.3.mean pain score on 2nd day was
5.1±1.5 in group A and in group B was 6.5±1.8.at 4h day mean pain score in group A was 4.3±1.3 and in group B was 5.1±1.6.At 7th day mean pain score in group A was 4.3±1.3 and in group B 5.1±1.6.patients in group A had less pain score as compare to group B patients. All patients were follow up for period one year and during this period none of the patients had recurrence of hernia.
113 Int J Res Med. 2014; 3(3);109-114 e ISSN:2320-2742 p ISSN: 2320-2734 up. The prevalence of post operative pain
syndrome after hernia surgery has been reported as high as 30% and some analyst estimate that 12% patient restricted their daily activities. Clinical studies have shown that both recurrence and chronic pain after hernia repair are influenced by the type of mesh implanted and its method of fixation. The ideal mesh fixation should produce no structural damage and be biocompatible in order to reduce the risk of hematoma and seroma. Conventionally, the mesh prosthesis is secured by either sutures or staple which may strangulate muscle fibers, compress regional nerves, or give rise to a lesion, leading to incapacitating pain. (12, 13, 14)
.at 1st day mean pain score in group A was 5.8±1.9 and in group B was 7.1±2.3.mean pain score on 2nd day was 5.1±1.5 in group A and in group B was 6.5±1.8.at 4h day mean pain score in group A was 4.3±1.3 and in group B was 5.1±1.6.at 7th day mean pain score in group A was 4.3±1.3 and in group B 5.1±1.6.patients in group A had less pain score as compare to group B patients. The difference may be due to less aggressive wound retraction needed in the suture less method as compared to the wound retraction needed for fixation of the mesh in the control group. The incidence of post operative heavy uncomfortable large scrotal swelling was interestingly less in the suture less method 6.5% as compared to the 21% in the control group again it may be due to less operative manipulation although it has no statistically significant.
CONCLUSION
Suture less hernia repair is a superior approach as compared to Lichtenstein technique for inguinal hernia surgery in terms of post operative large scrotal edema formation and pain status. Suture-less technique is effective and should be considered as first line of option as compared to Lichtenstein hernioplasty.
REFERENCES:
1. David C. Sabiston Text book of surgery the biological basis of modern surgica practices.
2. Jenkins JT, O’Dwyer PJ. Inguinal hernias.BMJ: British Medical JournaL 2008; 336(7638):269-72.
3. Queroz T, Sperandio WT, Soares RP, Kelmann G, Bernardo WM. What are the risks factors for inguinal hernia in adults? RevAssoc Médica Bras. 2008; 54(2):98.
4. David C. Sabiston Text book of surgery the biological basis of modern surgical practices.
5. Nyhus L.M. Klein and Roger's.F.B. inguinal hernia curr. Probl. Surg.1991. 6. Gilbert Al: sutureless repair of inguinal
hernia Am J surgery 163:331, 1992, Lichtenstein Il, Shul man Ag et al: The tension free hernioplasty American J. Surg. 157: 188, 1989.
7. Cooper A.P. the Anatomy and surgical treatment of inguinal and congenital hernia London Longman 1804.
8. Berlin, S. D.; An approach to grain hernia surg. Clin, North, Am 64:197. 1984.
9. Lichtenstein Il: Tension free technique held safe and effective for all hernia repairs General surgery news 9 (12)1, 1990
10. Read, R.C.i, college synthetic and direct inguinal herniation, advances or conversalis oxford, Radcliff medical press 1994.
11. Mac Fadyen B.V. and mathis C.R.: inguinal herniorrhaphy complications and recurrence. 1994.
12. Hidalgo M, Castillo M, Eymar J, Hidalgo A. Lichtenstein inguinal hernioplasty: sutures versus glue. Hernia. 2005; 9(3):242-4.
13. Junge K, Rosch R, Krones C, Klinge U, Mertens P, Lynen P, et al. Influence of polyglecaprone 25 (Monocryl)
supplementation on the
114 Int J Res Med. 2014; 3(3);109-114 e ISSN:2320-2742 p ISSN: 2320-2734 mesh for hernia repair. Hernia 2005;
9(3):212-7.
14. Mui WL-M, Ng CS, Fung TM-K, Cheung FKY, Wong C-M, Ma T-H, et al. Prophylactic ilioinguinal
neurectomy in open inguinalhernia repair: a double-blind randomized controlled trial. Annals of surgery.