Hepatitis B and E Co-Primary Infections in an HIV-1-Infected Patient
Yanis Bouamra,aSouad Benali,cHervé Tissot-Dupont,cCatherine Tamalet,a,bPhilippe Colsona,b
Pôle des Maladies Infectieuses et Tropicales Clinique et Biologique, Fédération de Bactériologie-Hygiène-Virologie, Centre Hospitalo-Universitaire Timone, IHU Méditerranée Infection, Assistance Publique-Hôpitaux de Marseille, Marseille, Francea
; Aix-Marseille Université, Unité de Recherche sur les Maladies Infectieuses et Tropicales Emergentes (URMITE) UM 63 CNRS UMR 7278 IRD 198 INSERM U1095, Facultés de Médecine et de Pharmacie, Marseille, Franceb
; Pôle des Maladies Infectieuses et Tropicales Clinique et Biologique, Service de Maladies Infectieuses, Centre Hospitalo-Universitaire Conception, Assistance Publique-Hôpitaux de Marseille, Francec
We report an autochthonous hepatitis E virus (HEV)-hepatitis B virus co-primary infection in a 41-year-old man having sex with
men and infected with human immunodeficiency virus (HIV). This case prompts testing for HEV in HIV-infected patients with
acute hepatitis even if primary infection with another hepatitis virus is diagnosed.
CASE REPORT
A
41-year-old man having sex with men (MSM) diagnosed in
1997 with human immunodeficiency virus type 1 (HIV-1)
infection (
1
) presented asthenia, abdominal pain, and dark urine
specimens in September 2010. His CD4
⫹T-lymphocyte count
(CD4 count) was 222/mm
3, and his plasma HIV-1 RNA level was
⬍
40 copies/ml (RealTime HIV; Abbott, Wiesbaden, Germany)
under raltegravir, darunavir, and ritonavir. In June 2009, he was
seronegative for hepatitis C virus (HCV) and hepatitis B virus
(HBV) (Architect; Abbott), while primary hepatitis A virus
(HAV) infection was diagnosed by detecting anti-HAV IgM
(Ar-chitect; Abbott) and HAV RNA, as described previously (
2
). At
admission, the alanine aminotransferase level was 2,620 IU/ml,
bilirubinemia was 72
mol/liter, and the prothrombin index was
100% (
Table 1
). His antiretroviral drugs had not been modified
since June 2009. Infections with HCV (HCV serology, Architect
[Abbott]; HCV RNA, RealTime HCV [Abbott]), Delta agent
(DiaSorin, Saluggia, Italy), Epstein-Barr virus (DiaSorin Liaison),
cytomegalovirus (Vidas; bioMérieux, Meylan, France), and
her-Received2 October 2012Returned for modification31 October 2012
Accepted4 January 2013
Published ahead of print9 January 2013
Address correspondence to Philippe Colson, philippe.colson@ap-hm.fr.
Copyright © 2013, American Society for Microbiology. All Rights Reserved.
[image:1.585.47.542.431.651.2]doi:10.1128/JCM.02630-12
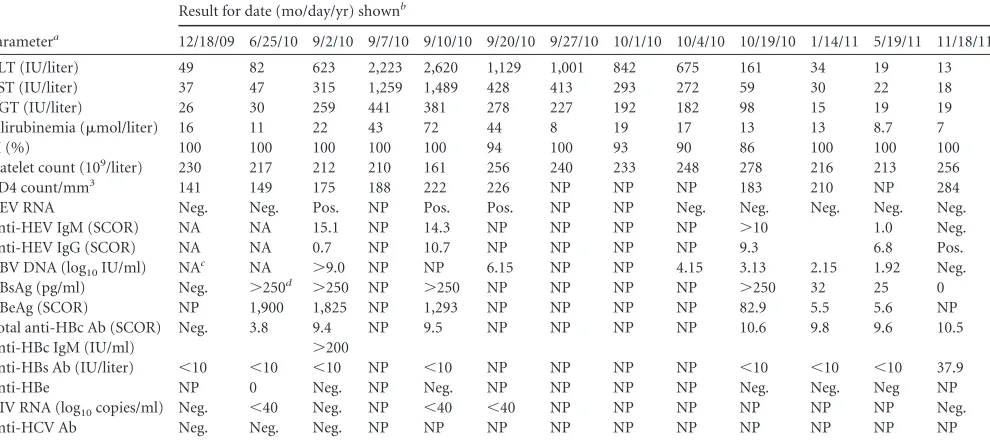
TABLE 1Longitudinal follow-up of biological and virological parameters
Parametera
Result for date (mo/day/yr) shownb
12/18/09 6/25/10 9/2/10 9/7/10 9/10/10 9/20/10 9/27/10 10/1/10 10/4/10 10/19/10 1/14/11 5/19/11 11/18/11
ALT (IU/liter) 49 82 623 2,223 2,620 1,129 1,001 842 675 161 34 19 13 AST (IU/liter) 37 47 315 1,259 1,489 428 413 293 272 59 30 22 18
GGT (IU/liter) 26 30 259 441 381 278 227 192 182 98 15 19 19
Bilirubinemia (mol/liter) 16 11 22 43 72 44 8 19 17 13 13 8.7 7
PI (%) 100 100 100 100 100 94 100 93 90 86 100 100 100
Platelet count (109/liter) 230 217 212 210 161 256 240 233 248 278 216 213 256 CD4 count/mm3 141 149 175 188 222 226 NP NP NP 183 210 NP 284 HEV RNA Neg. Neg. Pos. NP Pos. Pos. NP NP Neg. Neg. Neg. Neg. Neg. Anti-HEV IgM (SCOR) NA NA 15.1 NP 14.3 NP NP NP NP ⬎10 1.0 Neg. Anti-HEV IgG (SCOR) NA NA 0.7 NP 10.7 NP NP NP NP 9.3 6.8 Pos. HBV DNA (log10IU/ml) NAc NA ⬎9.0 NP NP 6.15 NP NP 4.15 3.13 2.15 1.92 Neg. HBsAg (pg/ml) Neg. ⬎250d ⬎250 NP ⬎250 NP NP NP NP ⬎250 32 25 0 HBeAg (SCOR) NP 1,900 1,825 NP 1,293 NP NP NP NP 82.9 5.5 5.6 NP Total anti-HBc Ab (SCOR) Neg. 3.8 9.4 NP 9.5 NP NP NP NP 10.6 9.8 9.6 10.5 Anti-HBc IgM (IU/ml) ⬎200
Anti-HBs Ab (IU/liter) ⬍10 ⬍10 ⬍10 NP ⬍10 NP NP NP NP ⬍10 ⬍10 ⬍10 37.9
Anti-HBe NP 0 Neg. NP Neg. NP NP NP NP Neg. Neg. Neg NP
HIV RNA (log10copies/ml) Neg. ⬍40 Neg. NP ⬍40 ⬍40 NP NP NP NP NP NP Neg.
Anti-HCV Ab Neg. Neg. Neg. NP NP NP NP NP NP NP NP NP NP
a
ALT, alanine aminotransferase level; AST, aspartate aminotransferase level; CD4 count, CD4⫹T-lymphocyte count; GGT, gammaglutamyltransferase; PI, prothrombin index; HCV, hepatitis C virus; HEV, hepatitis E virus; SCOR, signal/cutoff ratio; HBV, hepatitis B virus; HBsAg, hepatitis B surface antigen; HbeAg, hepatitis B e antigen; HBc, hepatitis B core; Ab, antibody; HIV, human immunodeficiency virus.
bThe antiviral therapy from 18 December 2009 through 10 September 2010 included raltegravir (RGV), darunavir (DRV), and ritonavir (RTV). The antiviral therapy from 20
September 2010 through 19 October 2010 included RGV, DRV, RTV, tenofovir-emtricitabine (TDF/FTC), and ribavirin (RBV). The antiviral therapy from 14 January 2011 through 18 November 2011 included RGV, DRV, RTV, and TDF/FTC. Neg., negative; Pos., positive; NP, not performed; NA, not available.
c
Negative on 24 July 2009.
dPerformed retrospectively.
on May 16, 2020 by guest
http://jcm.asm.org/
pes simplex virus (Siemens, Marburg, Germany) were ruled out
by serology and PCR testing. Acute hepatitis B was diagnosed by
detection in serum of HBV DNA (
⬎
9 log
10IU/ml) (RealTime
HBV; Abbott), hepatitis B surface antigen (HBsAg; Abbott), HBe
antigen (HBeAg; Abbott), and anti-HB core (anti-HBc) IgM (titer
of
⬎
200 IU/ml) (Vidas; bioMérieux) (
Table 1
). Retrospective
HBsAg and anti-HBc testing showed negativity in December 2009
and positivity in June 2010; HBV DNA testing was negative in July
2009. The HBV genotype, determined as described previously (
3
),
was G (
Fig. 1
). Concurrently with HBV diagnosis, hepatitis E virus
(HEV) testing on the serum sample collected in September 2010
showed positivity for anti-HEV IgM (Adaltis, Casalecchio di
Reno, Italy), and for HEV RNA using in-house assays as described
previously (
4
). Retrospective testing showed absence of HEV RNA
and anti-HEV IgM in June 2010. HEV RNA sequencing (
4
)
iden-tified genotype 3c (
Fig. 2
).
The patient did not travel abroad in 2010 but reported multiple
male sexual partners and frequent consumption of uncooked pig
liver sausage (PLS) in the 9-week period before hepatitis onset.
Tenofovir-emtricitabine and ribavirin (12 mg/kg of body weight/
day) were introduced to help control HBV and HEV, respectively.
HBV viremia and HBsAg titers progressively became undetectable
(
⬍
10 IU/ml and
⬍
0.05 pg/ml, respectively) 14 months post-HBV
diagnosis (
Table 1
). Anti-HBs antibodies became detectable at this
FIG 1Phylogenetic tree based on a 943-nucleotide (nt) fragment of the hepatitis B virus genome encoding the reverse transcriptase/hepatitis B surface antigen (nt 131 to 1073 in reference to GenBank sequence accession no.AF405706). HBV DNA from the present case is indicated by a boldface white font on a black background. Other sequence names in boldface indicate sequences with the highest BLAST scores (http://blast.ncbi.nlm.nih.gov/Blast.cgi) when searching in the NCBI GenBank nucleotide sequence database (BBHGbk; black frame) or our laboratory nucleotide sequence database (BBHTim; gray background); reference sequences with known genotypes and subtypes are indicated (3). Nucleotide sequence alignments were performed by using ClustalX version 2.0 (www.clustal .org/download/current). The tree was constructed by using MEGA5 (www.megasoftware.net) and the neighbor-joining method. Branches were obtained from 1,000 resamplings of the data; those with bootstrap values of⬎50% are labeled on the tree. The avian HEV sequence AY043166 was used as an out-group. The scale bar indicates the number of nucleotide substitutions per site. HEV sequences are labeled with GenBank accession number or laboratory number (for BBHTim and the present case), host, country where isolated, and collection or submission date. Av, avian; Hu, human; BBH, best BLAST hit; FRA, France; Gbk, GenBank; Mrs, Marseille; Tim, Timone laboratory.
Case Report
on May 16, 2020 by guest
http://jcm.asm.org/
[image:2.585.113.477.66.490.2]time point. HEV RNA became undetectable within 2 weeks
post-ribavirin introduction. Liver biochemical markers normalized
within 4 months after HBV-HEV diagnosis.
We report here, to our knowledge, the first observation of
HBV/HEV co-primary infection in an HIV-infected patient.
Oth-erwise, co-primary infections with other hepatitis viruses sharing
the same transmission routes have been described. One case of
HAV-HEV dual infection was recently reported in association
with aseptic meningitis in India, but diagnosis relied only on
pos-itive IgM to both viruses (
5
). In contrast, co-primary infections
with HBV and HCV or delta agent were more frequently described
(
6
–
8
). Besides, concurrent acute hepatitis E and HBV reactivation
has been described in an HIV-infected person (
9
).
Compared to the general population, HIV-infected persons
are at higher risk of viral hepatitis, including with HBV, HCV, or
delta agent, due to common risk factors for these infections,
in-cluding intravenous drug use or sexual intercourse (
8
,
10
–
13
).
Regarding HEV, it is an emerging cause of autochthonous
hepa-titis in Europe (
14
) and a new causative agent of acute and chronic
hepatitis in HIV-infected persons (
15
–
19
). Nonetheless, HEV
se-roprevalence has not been found to date to differ statistically
sig-nificantly between HIV-seropositive and -seronegative patients
FIG 2Phylogenetic tree based on partial (281-nucleotide [nt]) sequences of open reading frame 2 of the hepatitis E virus (HEV) genome (nt 6034 to 6314 in reference to GenBank sequence accession no.AB291961). HEV RNA from the present case is indicated by a boldface white font on a black background. Other sequence names in boldface indicate sequences with the highest BLAST scores (http://blast.ncbi.nlm.nih.gov/Blast.cgi) when searching in the NCBI GenBank nucleotide sequence database (BBHGbk; black frame) or our laboratory nucleotide sequence database (BBHTim; gray background); reference sequences with known genotypes and subtypes are indicated (4). Nucleotide sequence alignments were performed by using ClustalX version 2.0 (www.clustal.org/download /current). The tree was constructed by using MEGA5 (www.megasoftware.net) and the neighbor-joining method. Branches were obtained from 1,000 resam-plings of the data; those with bootstrap values of⬎50% are labeled on the tree. The avian HEV sequence AY043166 was used as an out-group. The scale bar indicates the number of nucleotide substitutions per site. HEV sequences are labeled with GenBank accession number or laboratory number (for BBHTim and the present case), host, country where isolated, and collection or submission date. Av, avian; BEL, Belgium; Hu, human; BBH, best BLAST hit; COL, Colombia; FRA, France; Gbk, GenBank; GER, Germany; ITA, Italy; Mrs, Marseille; Tim, Timone laboratory; USA, United States of America.
on May 16, 2020 by guest
http://jcm.asm.org/
[image:3.585.74.507.62.477.2]and in HIV-infected patients according to CD4 count, gender, or
HIV transmission mode (
18
–
21
). HEV genotype 3c identified
here is among the most frequently described in autochthonous
cases in Europe, including France (
4
,
22
,
23
). Best matches in the
NCBI nucleotide sequence database were HEV sequences
ob-tained in France from humans in whom HIV status was not
doc-umented, while best matches in our laboratory sequence database
were HEV sequences from HIV-negative persons (
Fig. 2
).
Con-sumption of uncooked PLS reported by the case has been
docu-mented as an HEV source in southern France, and eating raw or
undercooked pork has been identified as a risk factor predictive of
anti-HEV seropositivity in HIV-infected persons (
4
,
19
,
24
,
25
).
This habit may explain the greater incidence and prevalence of
HEV infections reported in southern France than northern
France, including in HIV-infected persons (
26
,
27
). HEV
trans-mission through sexual intercourse between MSM had been
sus-pected in the 1990s but was not confirmed thereafter (
19
,
21
,
28
).
Nonetheless, HEV transmission may potentially occur through
sexual intercourse between MSM, as demonstrated for HAV or
HCV, particularly in HIV-seropositive persons (
29
–
31
), and HEV
infection has been described previously in several MSM and a
bisexual man infected with HIV (
9
,
17
,
21
,
32
,
33
). Here, the
pa-tient reported sexual intercourse with several men and
concur-rently acquired HBV as well as HAV and HIV earlier in his life. Of
note, he became infected with HBV genotype G, which is rare in
France and worldwide but has been described to be more frequent
in HIV-infected patients (
34
–
36
) and particularly among MSM
(
37
–
39
). Also, we searched for top hits in the NCBI sequence
database with the HAV sequence recovered from a patient’s serum
collected 1 year before HEV-HBV primary infection, and we
found three HAV sequences with 100% nucleotide identity that
were obtained from serum samples of MSM in Barcelona, Spain
(
40
).
The major complications of autochthonous HEV infection in
Europe are fatal outcome, which occurred mostly in patients with
underlying liver diseases, and progression to chronicity and
cir-rhosis (
14
,
17
,
20
,
32
,
41
–
43
). HIV-infected patients are at
partic-ular risk of both severe outcomes due to frequent liver injury
related to hepatitis virus coinfections or antiretroviral-induced
toxicity and to HIV-induced immunosuppression (
11
,
15
). The
present observation questioned if concurrent acute HEV-HBV
infections could be associated with more severe histopathology
than acute HEV or HBV monoinfection, as observed for
concur-rent acute infections with Delta agent and HBV (
7
), and if
recip-rocal inhibition of HEV and HBV replication, as suspected during
co-primary HBV-HCV infection, may occur (
6
). Then
introduc-tion of antiviral therapy for both viruses prevented speculaintroduc-tion on
these issues. Of note, HBV DNA clearance only occurred after 14
months on tenofovir-emtricitabine, while HEV RNA clearance
occurred within 1 month under ribavirin. Regarding progression
toward chronic hepatitis E in HIV-infected patients, its
occur-rence was previously observed in patients exhibiting a CD4 count
of
⬍
200/mm
3(
15
,
21
). Here, ribavirin therapy was administered
to avoid potential severe outcome due to concurrent HBV
infec-tion and progression toward chronicity because the patient’s CD4
count was around 200/mm
3. No treatment is currently
recom-mended for acute hepatitis E, but ribavirin led to HEV clearance
within 2 to 12 weeks in chronically infected solid organ transplant
recipients (
44
–
46
) and was associated with rapid HEV RNA
nega-tivation in nonimmunocompromised patients exhibiting severe
acute hepatitis E (
47
,
48
).
Overall, the present case prompts to test systematically for
HEV in HIV-infected patients with acute hepatitis regardless of
whether primary infection with another hepatitis virus has been
diagnosed. The indication for ribavirin therapy in similar contexts
remains to be clarified.
REFERENCES
1.Henry M, Tourres C, Colson P, Ravaux I, Poizot-Martin I, Tamalet C.
2006. Coexistence of the K65R/L74V and/or K65R/T215Y mutations on the same HIV-1 genome. J. Clin. Virol.37:227–230.
2.Motte A, Blanc J, Minodier P, Colson P.2009. Acute hepatitis A in a pregnant woman at delivery. Int. J. Infect. Dis.13:e49 – e51.
3.Panassie L, Borentain P, Nafati C, Bernardin G, Doudier B, Thibault V, Gerolami R, Colson P.2012. Fatal fulminant primary hepatitis B virus infections with G1896A precore viral mutants in southeastern France. Clin. Res. Hepatol. Gastroenterol.36:e1– e8.
4.Colson P, Borentain P, Queyriaux B, Kaba M, Moal V, Gallian P, Heyries L, Raoult D, Gerolami R.2010. Pig liver sausage as a source of hepatitis E virus transmission to humans. J. Infect. Dis.202:825– 834. 5.Naha K, Karanth S, Prabhu M, Sidhu MS.2012. Dual infection with
hepatitis A and E virus presenting with aseptic meningitis: a case report. Asia Pac. J. Trop. Med.5:587–588.
6.Coppola N, Marrocco C, Di Caprio D, Coviello G, Scolastico C, Filippini P, Sagnelli E.2003. Acute hepatitis B and C virus coinfection: a virological and clinical study of 3 cases. Clin. Infect. Dis.36:528 –532. 7.Wedemeyer H, Manns MP.2010. Epidemiology, pathogenesis and
man-agement of hepatitis D: update and challenges ahead. Nat. Rev. Gastroen-terol. Hepatol.7:31– 40.
8.Yurdaydin C, Idilman R, Bozkaya H, Bozdayi AM.2010. Natural history and treatment of chronic delta hepatitis. J. Viral Hepat.17:749 –756. 9.Colson P, Gerolami R, Moreau J, Borentain P, Brouqui P. 2010.
Concurrent autochthonous acute hepatitis E and hepatitis B reverse sero-conversion in an HIV-1-infected patient: one virus may hide another. Int. J. Infect. Dis.14:e357. doi:10.1016/j.ijid.2009.04.007.
10. Larsen C, Pialoux G, Salmon D, Antona D, Le SY, Piroth L, Pol S, Rosenthal E, Neau D, Semaille C, Delarocque AE.2008. Prevalence of hepatitis C and hepatitis B infection in the HIV-infected population of France, 2004. Euro Surveill.13:18888.http://www.eurosurveillance.org /ViewArticle.aspx?Articleid⫽18888.
11. Sulkowski MS.2008. Viral hepatitis and HIV coinfection. J. Hepatol.
48:353–367.
12. Sulkowski MS, Thomas DL.2003. Hepatitis C in the HIV-infected per-son. Ann. Intern. Med.138:197–207.
13. Thio CL.2003. Hepatitis B in the human immunodeficiency virus-infected patient: epidemiology, natural history, and treatment. Semin. Liver Dis.23:125–136.
14. Kamar N, Bendall R, Legrand-Abravanel F, Xia NS, Ijaz S, Izopet J, Dalton HR.2012. Hepatitis E. Lancet379:2477–2488.
15. Colson P, Dhiver C, Poizot-Martin I, Tamalet C, Gerolami R.2010. Acute and chronic hepatitis E in patients infected with human immuno-deficiency virus. J. Viral Hepat.17:807– 815.
16. Crum-Cianflone NF, Curry J, Drobeniuc J, Weintrob A, Landrum M, Ganesan A, Bradley W, Agan BK, Kamili S. 2012. Hepatitis E virus infection in HIV-infected persons. Emerg. Infect. Dis.18:502–506. 17. Jagjit Singh GK, Ijaz S, Rockwood N, Farnworth SP, Devitt E, Atkins M,
Tedder R, Nelson M.2013. Chronic hepatitis E as a cause for cryptogenic cirrhosis in HIV. J. Infect.66:103–106.
18. Kaba M, Richet H, Ravaux I, Moreau J, Poizot-Martin I, Motte A, Nicolino-Brunet C, Dignat-George F, Menard A, Dhiver C, Brouqui P, Colson P.2011. Hepatitis E virus infection in patients infected with the human immunodeficiency virus. J. Med. Virol.83:1704 –1716.
19. Keane F, Gompels M, Bendall R, Drayton R, Jennings L, Black J, Baragwanath G, Lin N, Henley W, Ngui SL, Ijaz S, Dalton H.2012. Hepatitis E virus coinfection in patients with HIV infection. HIV Med.
13:83– 88.
20. Jardi R, Crespo M, Homs M, van den Eynde E, Girones R, Rodriguez-Manzano J, Caballero A, Buti M, Esteban R, Rodriguez-Frias F.2012. HIV, HEV and cirrhosis: evidence of a possible link from eastern Spain. HIV Med.13:379 –383.
Case Report
on May 16, 2020 by guest
http://jcm.asm.org/
21. Kenfak-Foguena A, Schöni-Affolter F, Bürgisser P, Witteck A, Darling KEA, Kovari H, Kaiser L, Evison JM, Elzi L, Gurter-De La Fuente V, Jost J, Moradpour D, Abravanel F, Izopet J, Cavassini M, Swiss HIV Cohort Study.2011. Hepatitis E virus seroprevalence and chronic infec-tions in patients with HIV, Switzerland. Emerg. Infect. Dis.17:1074 –1078. 22. Bouquet J, Tesse S, Lunazzi A, Eloit M, Rose N, Nicand E, Pavio N.
2011. Close similarity between sequences of hepatitis E virus recovered from humans and swine, France, 2008 –2009. Emerg. Infect. Dis.17:2018 – 2025.
23. Legrand-Abravanel F, Mansuy JM, Dubois M, Kamar N, Peron JM, Rostaing L, Izopet J.2009. Hepatitis E virus genotype 3 diversity, France. Emerg. Infect. Dis.15:110 –114.
24. Legrand-Abravanel F, Kamar N, Sandres-Saune K, Garrouste C, Dubois M, Mansuy JM, Muscari F, Sallusto F, Rostaing L, Izopet J. 2010. Characteristics of autochthonous hepatitis E virus infection in solid-organ transplant recipients in France. J. Infect. Dis.202:835– 844.
25. Mansuy JM, Bendall R, Legrand-Abravanel F, Saune K, Miedouge M, Ellis V, Rech H, Destruel F, Kamar N, Dalton HR, Izopet J. 2011. Hepatitis E virus antibodies in blood donors, France. Emerg. Infect. Dis.
17:2309 –2312.
26. Renou C, Lafeuillade A, Cadranel JF, Pavio N, Pariente A, Allegre T, Poggi C, Penaranda G, Cordier F, Nicand E.2010. Hepatitis E virus in HIV-infected patients. AIDS24:1493–1499.
27. Renou C, Moreau X, Pariente A, Cadranel JF, Maringe E, Morin T, Causse X, Payen JL, Izopet J, Nicand E, Bourliere M, Penaranda G, Hardwigsen J, Gerolami R, Peron JM, Pavio N.2008. A national survey of acute hepatitis E in France. Aliment. Pharmacol. Ther.27:1086 –1093. 28. Montella F, Rezza G, Di Sora F, Pezzotti P, Recchia O.1994. Association between hepatitis E virus and HIV infection in homosexual men. Lancet
344:1433. doi:10.1016/S0140-6736(94)90598-3.
29. Bordi L, Rozera G, Scognamiglio P, Minosse C, Loffredo M, Antinori A, Narciso P, Ippolito G, Girardi E, Capobianchi MR.2012. Monophyletic outbreak of hepatitis A involving HIV-infected men who have sex with men, Rome, Italy 2008 –2009. J. Clin. Virol.54:26 –29.
30. Urbanus AT, van Houdt R, van de Laar TJ, Coutinho RA. 2009. Viral hepatitis among men who have sex with men, epidemiology and public health consequences. Euro Surveill. 14:19421. http://www .eurosurveillance.org/ViewArticle.aspx?ArticleId⫽19421.
31. van de Laar TJ, van der Bij AK, Prins M, Bruisten SM, Brinkman K, Ruys TA, van der Meer JT, de Vries HJ, Mulder JW, van Agtmael M, Jurriaans S, Wolthers KC, Coutinho RA.2007. Increase in HCV inci-dence among men who have sex with men in Amsterdam most likely caused by sexual transmission. J. Infect. Dis.196:230 –238.
32. Dalton HR, Bendall RP, Keane FE, Tedder RS, Ijaz S.2009. Persistent carriage of hepatitis E virus in patients with HIV infection. N. Engl. J. Med.
361:1025–1027.
33. Sellier P, Mazeron MC, Tesse S, Badsi E, Evans J, Magnier JD, Sanson-Le-Pors MJ, Bergmann JF, Nicand E.2011. Hepatitis E virus infection in HIV-infected patients with elevated serum transaminases levels. Virol. J.
8:171. doi:10.1186/1743-422X-8-171.
34. Dao DY, Balko J, Attar N, Neak E, Yuan HJ, Lee WM, Jain MK.2011. Hepatitis B virus genotype G: prevalence and impact in patients
co-infected with human immunodeficiency virus. J. Med. Virol.83:1551– 1558.
35. Desire N, Sanchis T, Ben MF, Stitou H, Katlama C, Thibault V.2011. Development and validation of a specific method for relative HBV-genotype G (G-HBV) quantification in the context of co-infection with other genotypes. Pathol. Biol. (Paris)59:e13– e19. (In French.) 36. Mata Marin JA, Arroyo Anduiza CI, Calderon GM, Cazares RS, Fuentes
Allen JL, Arias FR, Gaytan MJ.2012. Prevalence and resistance pattern of genotype G and H in chronic hepatitis B and HIV co-infected patients in Mexico. Ann. Hepatol.11:47–51.
37. Bottecchia M, Souto FJ, O KM, Amendola M, Brandao CE, Niel C, Gomes SA.2008. Hepatitis B virus genotypes and resistance mutations in patients under long term lamivudine therapy: characterization of geno-type G in Brazil. BMC Microbiol.8:11. doi:1471-2180-8-11.
38. Chu CJ, Keeffe EB, Han SH, Perrillo RP, Min AD, Soldevila-Pico C, Carey W, Brown RS, Jr, Luketic VA, Terrault N, Lok AS.2003. Hepatitis B virus genotypes in the United States: results of a nationwide study. Gas-troenterology125:444 – 451.
39. Sanchez LV, Tanaka Y, Maldonado M, Mizokami M, Panduro A.2007. Difference of hepatitis B virus genotype distribution in two groups of Mexican patients with different risk factors. High prevalence of genotype H and G. Intervirology50:9 –15.
40. Perez-Sautu U, Costafreda MI, Cayla J, Tortajada C, Lite J, Bosch A, Pinto RM.2011. Hepatitis a virus vaccine escape variants and potential new serotype emergence. Emerg. Infect. Dis.17:734 –737.
41. Colson P, Kaba M, Moreau J, Brouqui P. 2009. Hepatitis E in an HIV-infected patient. J. Clin. Virol.45:269 –271.
42. Dalton HR, Hazeldine S, Banks M, Ijaz S, Bendall R.2007. Locally acquired hepatitis E in chronic liver disease. Lancet369:1260. doi:10.1016 /S0140-6736(07)60596-0.
43. Peron JM, Bureau C, Poirson H, Mansuy JM, Alric L, Selves J, Dupuis E, Izopet J, Vinel JP.2007. Fulminant liver failure from acute autochtho-nous hepatitis E in France: description of seven patients with acute hepa-titis E and encephalopathy. J. Viral Hepat.14:298 –303.
44. Chaillon A, Sirinelli A, De Muret A, Nicand E, d’Alteroche L, Goudeau A.2011. Sustained virologic response with ribavirin in chronic hepatitis E virus infection in heart transplantation. J. Heart Lung Transplant.30:841– 843.
45. Kamar N, Rostaing L, Abravanel F, Garrouste C, Lhomme S, Esposito L, Basse G, Cointault O, Ribes D, Nogier MB, Alric L, Peron JM, Izopet J. 2010. Ribavirin therapy inhibits viral replication on patients with chronic hepatitis E virus infection. Gastroenterology139:1612–1618. 46. Mallet V, Nicand E, Sultanik P, Chakvetadze C, Tesse S, Thervet E,
Mouthon L, Sogni P, Pol S.2010. Brief communication: case reports of ribavirin treatment for chronic hepatitis E. Ann. Intern. Med.153:85– 89. 47. Gerolami R, Borentain P, Raissouni F, Motte A, Solas C, Colson P.
2011. Treatment of severe acute hepatitis E by ribavirin. J. Clin. Virol.
52:60 – 62.
48. Peron JM, Dalton H, Izopet J, Kamar N.2011. Acute autochthonous hepatitis E in western patients with underlying chronic liver disease: a role for ribavirin? J. Hepatol.54:1323–1324.

![FIG 2 Phylogenetic tree based on partial (281-nucleotide [nt]) sequences of open reading frame 2 of the hepatitis E virus (HEV) genome (nt 6034 to 6314 insequence names in boldface indicate sequences with the highest BLAST scores (reference to GenBank sequ](https://thumb-us.123doks.com/thumbv2/123dok_us/8284956.849084/3.585.74.507.62.477/phylogenetic-nucleotide-sequences-hepatitis-insequence-indicate-sequences-reference.webp)